Abstract
Background:
The pathomechanism of anterolateral ankle impingement (ALAI) due to the distal fascicle of the anterior inferior tibiofibular ligament (DF-AITFL) has not been fully elucidated. In addition, because of its rarity, no definitive diagnostic criteria have been established for ALAI due to DF-AITFL.
Purpose:
To document the symptom characteristics and magnetic resonance imaging (MRI) and and arthroscopic findings as well as postoperative clinical outcomes of ALAI due to DF-AITFL.
Study Design:
Case series; Level of evidence, 4.
Methods:
Included were 12 patients (5 male and 7 female; mean age, 34.4 years [range, 21-76 years]) who were diagnosed with ALAI due to DF-AITFL and underwent excision of the DF-AITFL from November 2017 to August 2021. Symptom characteristics and symptom-related medical histories were evaluated, as were MRI and arthroscopic findings. Clinical outcomes were assessed using the visual analog scale for pain, American Orthopaedic Foot & Ankle Society ankle-hindfoot functional scale, and Foot Function Index.
Results:
All 12 patients had a history of ankle sprain before symptom onset. DF-AITFL was confirmed by MRI in all patients. Bone edema of the talus was observed in 2 patients (16.7%), and cartilage abnormalities in 3 patients (25%). Arthroscopy showed that the DF-AITFL contacted the anterolateral aspect of the talar dome during range of motion in all patients and that the AITFL was bent where it contacted the anterolateral dome of the talus in 3 patients (25%). Partial tear or adhesion of the DF-AITFL was noted in 7 patients (58.3%), and cartilage deformation at the anterolateral talar dome in 4 patients (33.3%). Mean visual analog scale pain, American Orthopaedic Foot & Ankle Society, and Foot Function Index scores improved significantly from preoperatively to postoperatively.
Conclusion:
ALAI due to DF-AITFL should be considered a possible cause of anterolateral ankle pain after an ankle sprain. The diagnosis can be reliably made with a thorough clinical examination and imaging studies. Half of the patients in this series also had lateral ankle instability. Surgical resection of the DF-AITFL and ligament reconstruction, if necessary, resulted in significant symptom improvement.
Keywords: ankle, ligament, impingement, anterolateral
The anterior inferior tibiofibular ligament (AITFL) is a flat band that connects the tibia and fibula and plays an important role in syndesmosis stability. 19 The AITFL may also have a distal fascicle (Bassett ligament); the incidence of this distal fascicle of the AITFL (DF-AITFL) has been reported to range from 82.9% to 100%.1-3,8,13 Furthermore, the DF-AITFL contacts the anterolateral dome of the talus during dorsiflexion of the ankle, and this contact is more prominent during dorsiflexion eversion.2,13
The DF-AITFL is the weakest structure of the syndesmotic ligament, and because it is distal to the AITFL, it is the first structure to be injured in cases of ankle sprain of the external rotation type. 26 This vulnerability can lead to pathologies after ankle sprain. Bassett et al 3 first reported anterolateral ankle impingement (ALAI) due to DF-AITFL after ankle sprain, and subsequently, cadaveric and imaging studies were conducted on the issue. However, the pathomechanism of this disease has not been fully elucidated.2,8,9,13,21,22 In addition, due to its rarity, no definitive diagnostic criteria have been established for ALAI by DF-AITFL. Although 3 clinical trials have been conducted,1,3,10 these focused on treatment and outcomes, and little is known about imaging or arthroscopic findings.
The purpose of this study was to document the symptom characteristics, magnetic resonance imaging (MRI) and arthroscopic findings, and postoperative clinical outcomes of ALAI due to DF-AITFL.
Methods
The protocol for this study received approval by our institutional review board, which waived the requirement for informed consent because of its retrospective design. Patients diagnosed with ALAI due to DF-AITFL and were treated surgically from November 2017 to August 2021 were included in the study.
The DF-AITFL is present in almost all individuals. It is currently difficult to detect pathologic DF-AITFL based on MRI findings alone, and no clear diagnostic criteria for impingement due to DF-AITFL have been established. Based on the diagnostic criteria used in previous reports,1,3,10,22 ALAI due to DF-AITFL was diagnosed when all of the following conditions were met: (1) persistent pain despite treatment for anterolateral ankle pain for >3 months, (2) tenderness of the anterolateral joint line, (3) anterolateral ankle pain with no causative bony spur on radiographs, (4) the detection of DF-AITFL on MRI, (5) pain exacerbation during ankle dorsiflexion and eversion, and (6) based on our clinical experience, pain disappearance or reduction when lidocaine was injected into the tender area.
Patients with ankle arthritis with bony spurs at the anterolateral joint, flatfoot with hindfoot valgus, an osteochondral lesion of the talus (OLT) with bone edema, or tarsal coalition were excluded. A total of 12 patients satisfied the study criteria and were included. There were 5 men and 7 women with a mean age of 34.4 years (range, 21-76 years). The mean follow-up period was 37.5 months (range, 24-62 months).
OLT without bone edema was diagnosed on preoperative MRI in 2 of the study patients (16.7%). One patient had been diagnosed with calcaneonavicular coalition at another hospital and underwent surgery, and another patient had been diagnosed with OLT and underwent surgery, but the symptoms did not improve in either patient.
Surgical Technique
Surgery was performed under general or spinal anesthesia in the supine position with a leg holder. The leg was exsanguinated with an elastic bandage, and a tourniquet was applied to the thigh. A 2.5-mm and 30° scope were used with ankle distraction. Before creating the arthroscopic portal, the joint was distended by saline loading. A standard anteromedial portal was created just medial to the tibialis anterior tendon. Then, under direct vision, an anterolateral portal was created just lateral to the peroneus tertius tendon. Synovitis around the DF-AITFL was checked using the anteromedial portal, and if present, synovectomy was performed. After confirming the presence of DF-AITFL and cartilage deformation, ankle ROM was performed to check for ligament to AL talar dome contact, and the ligament was also checked for bending of the DF-AITFL (without applying any force to the ankle).
After arthroscopic examination, DF-AITFL resection was performed using the anterolateral portal as the working portal. First, the ligament midsubstance was excised using an arthroscopic cutter (Figure 1A), and remnants were then completely removed using a shaver and an electrosurgical device (Figure 1B). In addition, the modified Broström procedure (MBP) was performed in patients with ankle instability after arthroscopic resection of DF-AITFL, as previously described. 15
Figure 1.
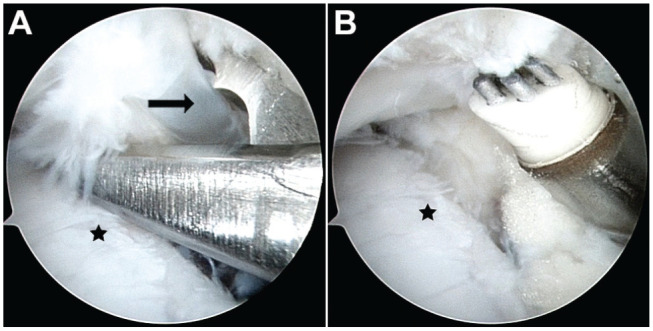
Cartilage injury was observed in the lateral dome of the talus (star) in contact with the distal fascicle of the anterior inferior tibiofibular ligament (DF-AITFL) (arrow). DF-AITFL resection was performed using the anterolateral portal as the working portal. (A) The ligament midsubstance was excised using an arthroscopic cutter, and (B) ligamentous remnants were completely removed using a shaver and an electrosurgical device.
Postoperatively, when the MBP was not performed, a short-leg splint was applied for 1 to 2 days. Patients were allowed to perform active exercises and full weightbearing as soon as tolerated. When MBP was performed, a short-leg walking cast was applied in the neutral position for 4 weeks postoperatively, followed by an air-stirrup brace for an additional month. Range of motion and peroneal strengthening exercises were started at 4 weeks, and full weightbearing with an air-stirrup brace was allowed at 4 weeks.
MRI Evaluation
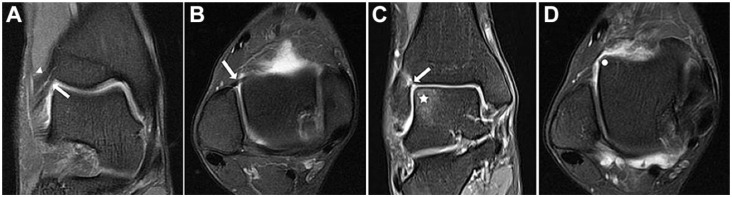
MRI examinations were performed using a 3.0-T instrument (Magnetom Skyra; Siemens Healthcare) and a standard ankle coil. Patients underwent the same routine ankle MRI in the supine position with the ankle in a neutral position. The MRI protocol consisted of fast spin-echo proton density–weighted sequences. Imaging was initially performed in the standard axial, coronal, and sagittal planes, and additional images were acquired in the coronal and axial oblique planes, as described previously, 5 to accurately assess the presence of DF-AITFL. The coronal oblique planes were prescribed using standard axial planes parallel to the orientation of the AITFL (Figure 2A), and the axial oblique planes were prescribed using coronal oblique planes parallel to the orientation of the AITFL (Figure 2B). In addition, abnormal findings such as synovitis, bone edema (Figure 2C), and cartilage abnormalities related to DF-AITFL were also evaluated by MRI (Figure 2D). Images were retrieved using a picture archiving and communication system (IMPAX; Agfa HealthCare).
Figure 2.
The distal fascicle of the anterior inferior tibiofibular ligament (DF-AITFL) (arrow) as assessed on magnetic resonance imging. (A) The coronal oblique plane was prescribed for the DF-AITFL using standard axial planes parallel to the AITFL (arrowhead). (B) The axial oblique plane was prescribed using coronal oblique planes parallel to the AITFL. The DF-AITFL was in contact with the anterolateral dome of the talus. (C and D) Abnormal findings related to DF-AITFL, including bone edema (star in [C]) and cartilage abnormalities (dot in [D]).
To assess the intra- and interobserver reliabilities for DF-AITFL detection by MRI, 51 patients, including the 12 study patients, were randomly selected based on sample size calculated using the Bonett approximation. 4 Before evaluating MRI findings, 2 orthopaedic surgeons (C.H.P., H.D.N.) reached consensus under the supervision of a musculoskeletal radiologist. These 2 surgeons independently assessed the blinded MRI scans, and repeated the assessments 3 weeks later. Kappa statistics were used to analyze reliability for the detection of DF-AITFL.
Talar tilt angle and anterior talar displacement were measured from stress radiographs with the ankle positioned at 15° plantarflexion using a Telos SE 2000 stress device (ARD Medizin Produkte) with 150 N force. Talar tilt angle was defined as the angle between the skeletal surfaces of the talus and tibia in the varus stress view. Varus instability was regarded as positive when the talar tilt angle was >10°, or the difference between both ankles was >6°. 15 Anterior talar displacement was defined as the shortest distance between the posterior lip of the tibia and the talar dome in the anterior drawer stress view. Anterior instability was regarded as positive when the anterior talar displacement was >4 mm or the difference between both ankles was >3 mm. 15
In addition, a manual anterior drawer test was performed to accurately assess the anterior shift of the talus. The test was performed in the operating room under anesthesia. Patients were categorized into 3 grades based on the degree of instability observed during testing. 1 Grade 1 (mild) was defined as a slight anterior translation compared with the contralateral ankle, grade 2 (moderate) was defined as a significant anterior translation exceeding that of the contralateral ankle but with a firm endpoint, and grade 3 (severe) was defined as significant anterior translation without an endpoint. Ankle instability was diagnosed when radiologic examination showed instability and the manual anterior drawer test showed grade 2 and 3 instability.
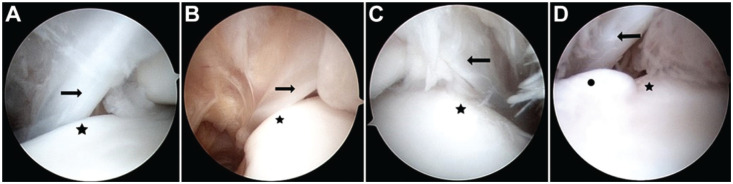
Arthroscopic Evaluation
Arthroscopic findings were evaluated for all 12 patients by classifying them by contact or bending of the DF-AITFL, ligament tear, or cartilage deformation. Contact was defined as contact between the DF-AITFL and the anterolateral talar dome during ankle range of motion (Figure 3A). Bending of the DF-AITFL was defined as bending in the area where the ligament contacted the anterolateral dome of the talus (Figure 3B). 2 Akseki et al 2 defined impingement of the ligament and talus as the presence of noticeable bending of the DF-AITFL between the lateral domes of the talus. A ligament tear was defined as the presence of a tear or adhesion around the DF-AITFL, regardless of severity (Figure 3C). Cartilage deformation was defined as the presence of cartilage degeneration at the anterolateral talar dome contacting the DF-AITFL (Figure 3D).
Figure 3.
(A) Ligament contact was defined as contact between the distal fascicle of the anterior inferior tibiofibular ligament (DF-AITFL) (arrow in all images) and the anterolateral talar dome (star in all images). (B) Bending of the ligament was defined as a bending in the area where the ligament contacted the anterolateral dome of the talus. (C) A ligament tear was defined as the presence of a tear or adhesion around the DF-AITFL, regardless of severity. (D) Cartilage deformation (dot) was defined as cartilage degeneration in the anterolateral talar dome in contact with the DF-AITFL.
Clinical Evaluation
Symptom characteristics and symptom-related medical histories were evaluated preoperatively. Clinical outcomes were assessed using a visual analog scale for pain, the American Orthopaedic Foot & Ankle Society ankle-hindfoot functional scale, 11 and the Foot Function Index 6 preoperatively and at the final follow-up. To avoid potential bias, clinical scores were assessed by research assistants not part of the surgical team.
Statistical Analysis
Continuous data are expressed as means and ranges. Dependent variables were tested for distribution normality and equality of variances. Nonparametric tests were used for the analysis because variables had a non-normal distribution. The Wilcoxon signed-rank test was used to evaluate changes in clinical outcomes. The Mann-Whitney U test was used to compare the radiographic results between patients with and without ankle instability. For all tests, P values of < .05 were considered significant. The analysis was performed using SPSS software (Version 12.0; IBM).
Results
All 12 of the study patients had a history of ankle sprain before symptom onset, and 8 of the patients had a history of ≥2 sprains. The mean symptom duration at presentation was 18.2 months (range, 3-36 months). All 12 patients had pain and tenderness in the anterolateral aspect of the ankle, which improved after lidocaine injection, and they experienced pain exacerbation when the ankle was dorsiflexed and everted. In addition, 3 patients (25%) experienced snapping during ankle range of motion.
The intra- and interobserver reliabilities for the detection of DF-AITFL were 1.0 and 0.99, respectively, in the axial oblique plane and 0.92 and 0.83, respectively, in the coronal oblique plane. These values indicated almost perfect reliability.
In 6 of the 12 patients, ankle instability with clunk was observed on manual anterior drawer test as well as stress radiographs (Table 1). In all 6 patients with ankle instability, an additional MBP was performed. DF-AITFL was confirmed in all 12 patients on axial oblique MRI, and in 6 patients (50%), DF-AITFL was identified on coronal oblique MRI as a distinct structure inferior and parallel to the AITFL (Figure 4). Synovitis with fluid collection around the DF-AITFL, regardless of the degree, was observed in all patients. Bone edema without an osteochondral lesion on the lateral dome of the talus was observed in 2 patients (16.7%), and cartilage abnormalities of the talar dome were observed in 3 patients (25%).
Table 1.
Comparison of Radiographic Findings Between Patients With and Without Ankle Instability a
| Ankle Instability (n = 6) | No Ankle Instability (n = 6) | P | |
|---|---|---|---|
| Talar tilt angle, deg | 10.7 ± 0.8 | 3.3 ± 1.5 | <.001 |
| Anterior talar displacement, mm | 6 ± 1.4 | 2.2 ± 0.8 | <.001 |
Values are presented as mean ± SD.
Figure 4.
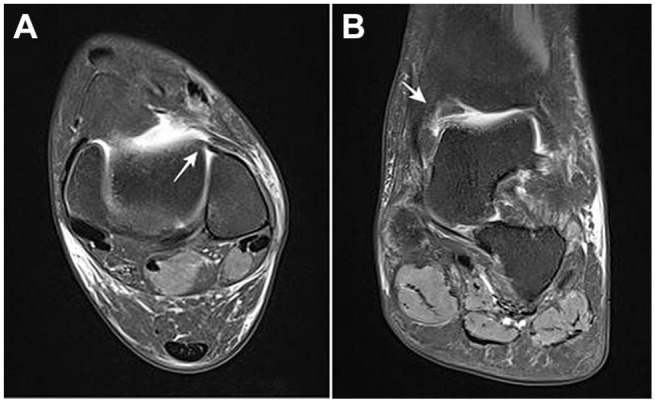
(A) The distal fascicle of the anterior inferior tibiofibular ligament (DF-AITFL) (arrow) was identified on axial oblique magnetic resonance imaging (MRI) as ligament contact with the anterolateral dome of the talus. (B) The distal fascicle (arrow) was identified below the AITFL on coronal oblique MRI.
Arthroscopic findings showed that the DF-AITFL contacted the anterolateral aspect of the talar dome during range of motion in all patients and that bending of the ligament occurred in 3 patients (25%). Partial tear or adhesion of the DF-AITFL was noted in 7 patients (58.3%) and cartilage deformation at the anterolateral talar dome in 4 patients (33.3%). In 5 patients (41.7%), the DF-AITFL was distinctly separated from the AITFL, and in 7 patients, the proximal part of the DF-AITFL was distinctly separated from the AITFL, but the distal part was attached.
The mean visual analog scale for pain (P < 0.001), American Orthopaedic Foot & Ankle Society score (P < 0.001), and Foot Function Index (P < 0.001) improved significantly from 5.4 (range, 4-8), 61.7 (range, 45-77), and 47 (range, 32.7-84) preoperatively to 1.3 (range, 0-3), 93.4 (range, 87-100), and 8.3 (range, 4.9-16.3), respectively, at last follow-up. No symptom recurrence or postoperative complications were reported at last follow-up.
Discussion
Ankle impingement was considered to be a bony impingement before the late 1980s.14,17,18,20 However, in 1990, Bassett et al 3 reported on soft impingement caused by DF-AITFL, and several cadaveric studies have since been conducted to identify the pathomechanism responsible for ALAI due to DF-AITFL.2,8,9,13,22 However, most of the studies were performed in vitro and did not consider muscular tonus or the effects of weightbearing. In a clinical study by Akseki et al, 1 all patients diagnosed with ALAI due to DF-AITFL showed ankle instability of various degrees. Bassett et al reported that all patients had a history of ankle sprain before the onset of impingement symptoms but did not describe the degree of instability. Nonetheless, based on the results of these studies, ankle instability is considered to be one of the most important pathomechanisms. When the anterior talofibular ligament (ATFL) is intact, it prevents anterior displacement of the talus and impingement between the talus and tibia during ankle dorsiflexion. However, when the ATFL is damaged, anterior displacement of the talus may result in impingement between the DF-AITFL and the anterolateral dome of the talus. 2 In the present study, all patients had a history of ankle sprain before symptom onset, and 50% of all patients had ankle instability with clunking on physical examination. In addition, all patients had pain that worsened with ankle dorsiflexion and eversion.
Another hypothesis addressed anatomic variations of the DF-AITFL 2 : namely, that a more distal fibular insertion of the DF-AITFL is more likely to cause impingement. In a cadaveric study by Akseki et al, 2 the distance between the joint level and fibular insertion of the DF-AITFL was significantly greater in the specimens with a bent DF-AITFL. MRI provides an excellent means of confirming this phenomenon before surgery, although bending of the DF-AITFL is difficult to confirm on standard axial and coronal planes. Therefore, in patients with suspected ALAI due to DF-AITFL, acquisition of axial and coronal oblique planes with focus on the AITFL may be helpful. 5 Furthermore, it is important to note that DF-AITFL is best identified on fat-saturated T2-weighted sequences, especially in the axial oblique plane. 21
Patients who experience persistent lateral or anterolateral ankle pain after an ankle sprain are commonly encountered in clinics. However, it is often difficult to make an accurate diagnosis in such cases because there are several differential diagnoses, including OLT, sinus tarsi syndrome, or tarsal coalition.16,22 To accurately diagnose ALAI due to DF-AITFL, it is most important to differentiate between the conditions that can cause anterolateral ankle pain. In the present study, 1 patient misdiagnosed as having OLT and another misdiagnosed with calcaneonavicular coalition presented at our hospital due to no improvement in symptoms after surgery.
To date, only 3 clinical studies have been performed on ALAI due to DF-AITLF,1,3,10 and as a result, there are no clear diagnostic criteria for ALAI due to DF-AITLF. Based on the clinical studies reported to date, the 5 diagnostic criteria described in the present study could be used empirically. 22 However, to hone the diagnosis further, we diagnosed ALAI due to DF-AITFL if the 5 diagnostic criteria were met and pain decreased after ultrasound-guided lidocaine injection. Since pain relief after lidocaine injection is commonly used to diagnose other musculoskeletal disorders, we suggest that it be used to increase the accuracy of diagnosing ALAI due to DF-AITFL.
Treatment of ALAI due to DF-AITFL, as with other musculoskeletal diseases, initially requires conservative treatment such as medication, injection, physical therapy, and bracing. 22 The duration of conservative treatment has not been established, but 3 to 6 months is generally recommended. However, it has been reported that longer periods of conservative treatment for anterior ankle impingement are associated with poorer postoperative outcomes. 23 Therefore, surgical treatment should be considered after an appropriate time if conservative treatment fails to elicit an improvement. The most common surgical treatment is resection of the DF-AITLF, the structure responsible for the pain. However, the role of DF-AITFL and the impact of resection on the ankle joint is still controversial. According to a study by Yeo et al, 25 many type 1 mechanoreceptors exist in the DF-AITFL, and their preservation should be considered. However, on the other hand, dissection and clinical studies have shown that DF-AITFL resection does not affect syndesmotic stability.10,18 In addition, when performing arthroscopic MBP, which is now being commonly performed, the DF-AITFL is commonly removed to secure a surgical view.7,12,24 Thus, DF-AITFL resection may be the simplest and most definitive treatment method.
It may be controversial to perform surgery for ankle instability at the same time as DF-AITFL resection. In the 3 clinical studies reported to date,1,3,10 only DF-AITFL resection was performed, postoperative results were good, and there was no recurrence. In a study by Akseki et al, 1 3 of 4 patients with severe ankle instability preoperatively were able to return to their previous activity levels without ligament repair, though 1 patient required additional surgery for moderate instability 6 months after surgery. In the present study, MBP was performed simultaneously with DF-AITFL resection for ankle instability with a clunk in the anterior drawer test, based on consideration of the risk of symptom recurrence due to soft tissue adhesion or hypertrophy after DF-AITFL resection. However, it is unknown if MBP alone would have resolved the symptoms in the patients with chronic ankle instability. Further studies are needed to determine the best surgical treatment method for ALAI due to DF-AITFL.
Strengths and Limitations
The strength of this study was that it is the first to evaluate arthroscopic findings in ALAI due to DF-AITFL. Although studies have been conducted to analyze the imaging findings of ALAI due to DF-AITFL, little is known about its arthroscopic findings. This study also had some limitations. First, the number of patients included was a major weakness of this study. However, considering that the incidence of symptomatic DF-AITFL is small and that only 21, 7, and 9 patients, respectively, were included in the 3 clinical studies reported to date,1,3,10 the number of patients included was meaningful. Second, we evaluated only surgical treatment for DF-AITFL due to ALAI. It was expected that more patients may have responded to nonsurgical treatment than those who underwent surgical treatment, but this study does not provide information on that. Third, there was no analysis of the ability to detect pathologic DF-AITFL on MRI evaluation. Last, there was no control group, which is the biggest limitation of this study. The lack of a control group made it difficult to definitively answer the question of whether pathologic arthroscopic findings seen in patients with ALAI due to DF-AITFL were truly caused by DF-AITFL. Therefore, a randomized case-control study with a well-designed control group involving a larger number of patients is needed to overcome these limitations.
Conclusion
ALAI due to DF-AITFL should be considered a possible cause of anterolateral ankle pain after an ankle sprain. Half of the patients in this study also had lateral ankle instability. The diagnosis can be made reliably with a thorough clinical examination and imaging studies. In this study, surgical resection of the DF-AITFL and ligament reconstruction, when necessary, resulted in improvement of symptoms.
Footnotes
Final revision submitted February 27, 2024; accepted March 18, 2024.
One or more of the authors has declared the following potential conflict of interest or source of funding: This research received no external funding. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Yeungnam University Hospital (ref No. 2023-10-060).
ORCID iD: Chul Hyun Park  https://orcid.org/0000-0002-3101-8655
https://orcid.org/0000-0002-3101-8655
References
- 1. Akseki D, Pinar H, Bozkurt M, Yaldiz K, Arac S. The distal fascicle of the anterior inferior tibio-fibular ligament as a cause of anterolateral ankle impingement: results of arthroscopic resection. Acta Orthop Scand. 1999;70(5):478-482. [DOI] [PubMed] [Google Scholar]
- 2. Akseki D, Pinar H, Yaldiz K, Akseki NG, Arman C. The anterior inferior tibiofibular ligament and talar impingement: a cadaveric study. Knee Surg Sports Traumatol Arthrosc. 2002;10(5):321-326. [DOI] [PubMed] [Google Scholar]
- 3. Bassett FH, 3rd, Gates HS, 3rd, Billys JB, Morris HB, Nikolaou PK. Talar impingement by the anteroinferior tibiofibular ligament. A cause of chronic pain in the ankle after inversion sprain. J Bone Joint Surg Am. 1990;72(1):55-59. [PubMed] [Google Scholar]
- 4. Bonett DG. Sample size requirements for estimating intraclass correlations with desired precision. Stat Med. 2002;21(9):1331-1335. [DOI] [PubMed] [Google Scholar]
- 5. Boonthathip M, Chen L, Trudell DJ, Resnick DL. Tibiofibular syndesmotic ligaments: MR arthrography in cadavers with anatomic correlation. Radiology. 2010;254(3):827-836. [DOI] [PubMed] [Google Scholar]
- 6. Budiman-Mak E, Conrad KJ, Roach KE. The Foot Function Index: a measure of foot pain and disability. J Clin Epidemiol. 1991;44(6):561-570. [DOI] [PubMed] [Google Scholar]
- 7. Cottom JM, Richardson PE. The “all-inside” arthroscopic Broström procedure augmented with a proximal suture anchor: an innovative technique. J Foot Ankle Surg. 2017;56(2):408-411. [DOI] [PubMed] [Google Scholar]
- 8. Dalmau-Pastor M, Malagelada F, Kerkhoffs G, et al. The anterior tibiofibular ligament has a constant distal fascicle that contacts the anterolateral part of the talus. Knee Surg Sports Traumatol Arthrosc. 2020;28(1):48-54. [DOI] [PubMed] [Google Scholar]
- 9. Edama M, Takeishi M, Kurata S, et al. Morphological features of the inferior fascicle of the anterior inferior tibiofibular ligament. Sci Rep. 2019;9(1):10472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Horner G, Liu S. Arthroscopic treatment of talar impingement by the accessory anteroinferior tibiofibular ligament. Arthroscopy. 1996;12:384-385. [Google Scholar]
- 11. Kitaoka HB, Alexander IJ, Adelaar RS, et al. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15(7):349-353. [DOI] [PubMed] [Google Scholar]
- 12. Nery C, Fonseca L, Raduan F, et al. Prospective study of the “Inside-Out” arthroscopic ankle ligament technique: reliminary result. Foot Ankle Surg. 2018;24(4):320-325. [DOI] [PubMed] [Google Scholar]
- 13. Nikolopoulos CE, Tsirikos AI, Sourmelis S, Papachristou G. The accessory anteroinferior tibiofibular ligament as a cause of talar impingement: a cadaveric study. Am J Sports Med. 2004;32(2):389-395. [DOI] [PubMed] [Google Scholar]
- 14. O’Donoghue DH. Impingement exostoses of the talus and tibia. J Bone Joint Surg Am. 1957;39(4):835-852. [PubMed] [Google Scholar]
- 15. Park CH, Park J. Effect of modified Broström procedure with periosteal flap augmentation after subfibular ossicle excision on ankle stability. Foot Ankle Int. 2019;40(6):656-660. [DOI] [PubMed] [Google Scholar]
- 16. Park JW, Park J, Park CH. Accessory talar facet impingement and sinus tarsi pain associated with accessory anterolateral talar facet. Foot Ankle Int. 2021;42(8):1060-1067. [DOI] [PubMed] [Google Scholar]
- 17. Parkes JC, 2nd, Hamilton WG, Patterson AH, Rawles JG., Jr. The anterior impingement syndrome of the ankle. J Trauma. 1980;20(10):895-898. [DOI] [PubMed] [Google Scholar]
- 18. Rasmussen O, Tovborg-Jensen I, Boe S. Distal tibiofibular ligaments: analysis of function. Acta Orthop Scand. 1982;53(4):681-686. [DOI] [PubMed] [Google Scholar]
- 19. Ray RG, Kriz BM. Anterior inferior tibiofibular ligament. Variations and relationship to the talus. J Am Podiatr Med Assoc. 1991;81(9):479-485. [DOI] [PubMed] [Google Scholar]
- 20. St Pierre RK, Velazco A, Fleming LL. Impingement exostoses of the talus and fibula secondary to an inversion sprain. A case report. Foot Ankle. 1983;3(5):282-285. [DOI] [PubMed] [Google Scholar]
- 21. Subhas N, Vinson EN, Cothran RL, et al. MRI appearance of surgically proven abnormal accessory anterior-inferior tibiofibular ligament (Bassett’s ligament). Skeletal Radiol. 2008;37(1):27-33. [DOI] [PubMed] [Google Scholar]
- 22. van den Bekerom MP, Raven EE. The distal fascicle of the anterior inferior tibiofibular ligament as a cause of tibiotalar impingement syndrome: a current concepts review. Knee Surg Sports Traumatol Arthrosc. 2007;15(4):465-471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. van Dijk CN, Tol JL, Verheyen CC. A prospective study of prognostic factors concerning the outcome of arthroscopic surgery for anterior ankle impingement. Am J Sports Med. 1997;25(6):737-745. [DOI] [PubMed] [Google Scholar]
- 24. Vega J, Poggio D, Heyrani N, et al. Arthroscopic all-inside ATiFL's distal fascicle transfer for ATFL's superior fascicle reconstruction or biological augmentation of lateral ligament repair. Knee Surg Sports Traumatol Arthrosc. 2020;28(1):70-78. [DOI] [PubMed] [Google Scholar]
- 25. Yeo ED, Rhyu IJ, Kim HJ, et al. Can Bassett's ligament be removed? Knee Surg Sports Traumatol Arthrosc. 2016;24(4):1236-1242. [DOI] [PubMed] [Google Scholar]
- 26. Zalavras C, Thordarson D. Ankle syndesmotic injury. J Am Acad Orthop Surg. 2007;15(6):330-339. [DOI] [PubMed] [Google Scholar]