Abstract
Background:
Despite a growing body of literature regarding anterior cruciate ligament reconstruction (ACLR), there remains a wide diversity in surgical technique and clinical practice across providers.
Purpose:
To (1) describe current ACLR practice preferences among members of the Herodicus society and (2) determine whether these preferences are influenced by years in practice and overall surgical volume.
Study Design:
Cross-sectional study.
Methods:
A 24-question survey investigating surgeons’ practices and preferred ACLR surgical techniques was sent via email to all active Herodicus Society members. Survey responses were subdivided by years of experience and overall ACLR annual case volume. Descriptive statistics were compiled and chi-square testing was utilized to determine the significance of experience and case volume on survey responses.
Results:
Of the 113 invited Herodicus Society members who perform ACLR, 69 (61%) completed the survey. Respondents had a mean ± SD of 30.9 ± 9.8 years of experience in clinical practice and performed a mean of 96.0 ± 50.7 primary and 21.6 ± 16.9 revision ACLR annually. Of revision cases, 72.1% were performed using a single-stage technique. Mean frequency of graft usage by surgeon was bone–patellar tendon–bone autograft (58.6%), quadriceps autograft (14.6%), hamstring tendon autograft (14.0%), and allograft (11.8%). The plurality of surgeons responded that they used anterolateral augmentation “rarely” in primary ACLR (39.1%) and “sometimes” in revision ACLR (31.9%), with the majority performing lateral extra-articular tenodesis (66.7%) rather than anterolateral ligament reconstruction (14.5%). Most surgeons would not allow a 20-year-old football player to return before 7 months after ACLR (71.0%) but highly valued return-to-sports testing to determine readiness (94.2%). Higher volume surgeons performed single-stage revision ACLR at a significantly higher rate (79.8% vs 62.9%, P = .02) and significantly differed in return-to-sports criteria, with a greater proportion relying primarily on biometric testing (P = .01).
Conclusion:
The survey demonstrated that, in the Herodicus Society, a wide range of preferences exist regarding ACLR surgical technique. Bone–patellar tendon–bone autograft is the most frequent primary ACLR graft choice. Most participants have not embraced newer techniques such as anterolateral or suture tape augmentation. Return to sports is generally not allowed before 7 months and heavily factors-in return-to-sports testing metrics, suggesting that purely time-based criteria for return to sports is not modern practice among elite sports medicine surgeons.
Keywords: ACL, ACLR, graft choice, Herodicus Society, knee ligaments
As one of the most thoroughly researched topics in sports medicine, anterior cruciate ligament (ACL) reconstruction (ACLR) has seen many advances in techniques, such as patient-specific graft choice, independent femoral tunnel drilling, and anatomic tunnel placement. With an abundance of knowledge from decades of literature, surgeons could be expected to have converged on a narrow breadth of evidence-based techniques. However, multiple techniques and ideologies continue to persist regarding optimal ACLR techniques. 34
Previous studies on surgeon preferences regarding ACLR have mostly focused on international surgeons,17,34,37 with limited data available on surgeons in the United States. 4 These have shown heterogeneity in many facets of ACLR, as well as trends that depart from the most common practices in the United States—most notably in the frequent use of hamstring tendon autograft.29,33,34,37 Therefore, evaluation of predominantly US surgeons provides a different view that may be more applicable to surgeons in the country.
The Herodicus Society is a small society of orthopaedic sports medicine surgeons who are among the most experienced and well-respected practitioners in the field. Membership to the Herodicus Society is by invitation only, and, although most members practice in the United States, a minority of surgeons in the society practice in other countries. Their opinions and techniques are shared widely in conferences, taught to trainees, and described in textbooks. A synthesis of Herodicus Society members’ preferences regarding ACLR would be a valuable reflection on the state of ACLR in the present day from those who have deep knowledge of, and often have written, the literature on the procedure. This is especially valuable at a time when there are many new techniques in the literature, such as anterolateral or suture tape augmentation, and surgeons may wish to know which techniques the leaders in the field have adopted.
The purpose of this study was to (1) describe current ACLR practice preferences among members of the Herodicus society and (2) determine whether these preferences are influenced by years in practice and overall surgical volume. It was hypothesized that (1) there would be a heterogeneous array of responses not associated with surgeon characteristics, and (2) most ACLR preferences would be consistent with evidence in the literature.
Methods
In June 2022, an electronic survey invitation was distributed through email to all active Herodicus Society members and narrowed to those who perform ACLR. The survey was prepared and distributed using QualtricsXM services (Qualtrics) and consisted of 25 total questions (Appendix Figure A1). The first 5 questions involved general demographics for each surgeon, including years in practice, practice setting, and total annual ACLR case volume. The next 15 questions investigated aspects of the surgeon's preferred surgical technique, including graft selection, tunnel drilling technique, fixation preference, and anterolateral augmentation. The final 5 questions focused on postoperative care and rehabilitation preferences. Participation was voluntary, and replies were kept confidential. The questions were chosen to highlight the most significant and variable aspects of management after ACL injury, from ACLR through the end of rehabilitation. The goal was to obtain a comprehensive understanding of provider-based variability in surgical techniques and postoperative rehabilitation.
Survey responses were compiled after a 30-day response period and analyzed and reported as percentage frequencies for each question. Survey responses were then categorized by years of experience (threshold of 30 years in practice) and overall ACLR annual case volume (threshold of 100 cases). Normal (Gaussian) distribution of the response data was determined. The influence of operative volume and surgical experience on survey responses with continuous variable responses (graft selection and staged revision preference) was assessed using Student t tests or Mann-Whitney U tests as appropriate. Pearson chi-square testing was used to compare categorical survey responses by experience and case volume. Statistical analysis was performed using the SPSS software package (SPSS Version 28.0.1.1, IBM).
Results
Survey Participants
Of the 113 Herodicus Society members who perform ACLRs, 69 members (61.1%) completed the survey. The mean ± SD time in clinical practice was 30.9 ± 9.8 years, and 85.5% were in an academic or privademic practice. Respondents performed a mean of 96.0 ± 50.7 primary and 21.6 ± 16.9 revision ACLR annually, with a mean of 72.1% of revision cases performed using a single-stage technique.
Surgical Technique
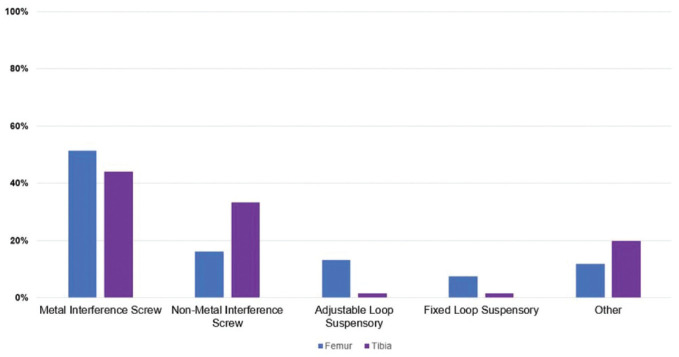
Regarding graft choice, the frequency of graft usage across all ACLRs showed bone–patellar tendon–bone (BPTB) autograft was most frequent, followed by quadriceps autograft, hamstring tendon autograft, and then allograft (Figure 1).
Figure 1.
Graft choice frequency for ACLR among Herodicus members. ACLR, anterior cruciate ligament reconstruction; BPTB, bone–patellar tendon–bone.
Most surgeons reported using BPTB autograft in over half of their ACLRs (Table 1). The preferred allograft was BPTB (50.8%), followed by Achilles (15.4%) and tibialis anterior or posterior (12.3%). Semitendinosus or other allografts were less common (total 18.5%). Most surgeons preferred not to soak grafts in vancomycin solution (63.8%). Femoral tunnel drilling was primarily independent of tibial tunnel drilling (82.6%), and most surgeons used an anteromedial approach (Table 1).
Table 1.
Descriptive Characteristics of Surgical Preferences a
| Variable | Total Respondents (n = 69) |
|---|---|
| Preferred graft | |
| ≥50% BPTB | 47 (68.1) |
| ≥50% quadriceps | 9 (13.0) |
| ≥50% hamstring | 8 (11.6) |
| ≥50% allograft | 5 (7.2) |
| Peripheral nerve block | |
| Yes (femoral) | 14 (20.3) |
| Yes (adductor) | 36 (52.2) |
| Never | 19 (27.5) |
| Femoral tunnel technique | |
| Anteromedial | 36 (52.2) |
| Accessory anteromedial | 11 (15.9) |
| Outside-in | 10 (14.5) |
| Transtibial | 12 (17.4) |
| Single-stage revision, % b | 72.1 ± 29.5 |
Data are presented as n (%) or mean ± SD.ACLR, anterior cruciate ligament reconstruction; BPTB, bone–patellar tendon–bone.
Reported as mean percentage of total revision ACLRs performed annually.
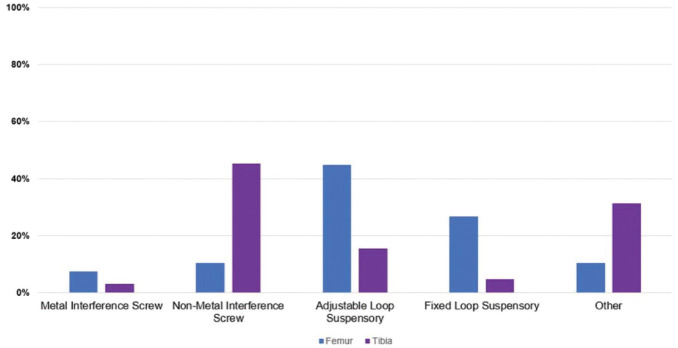
Regarding graft fixation, interference screws were most common for BPTB grafts on the femoral (66.6%) and tibial (73.9%) sides, with metal more commonly used than nonmetal (bioabsorbable or PEEK) screws (Figure 2).
Figure 2.
Preferred BPTB graft fixation techniques for ACLR, with the y axis representing percentage of survey respondents. ACLR, anterior cruciate ligament reconstruction; BPTB, bone–patellar tendon–bone.
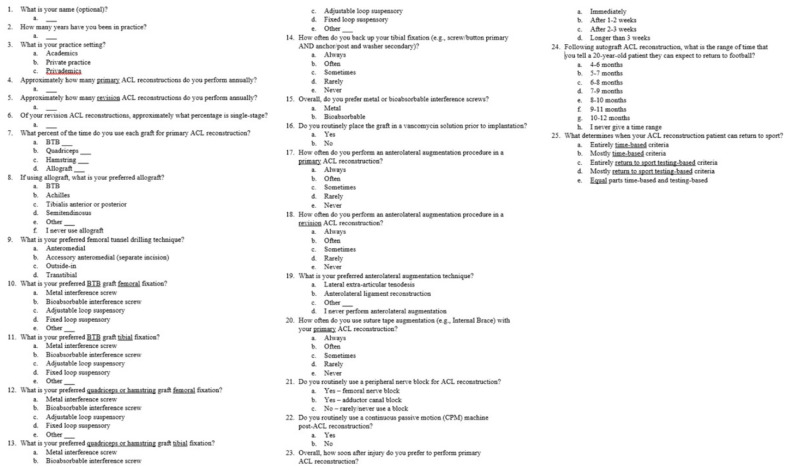
For soft tissue grafts, adjustable loop suspensory fixation was the most common preference on the femur (43.5%), with most surgeons (69.6%) using suspensory fixation of some type. On the tibia, nonmetal interference screw fixation was used by most surgeons (42.0%; Figure 3). Overall, there was a roughly even divide between preferring nonmetal (55.1%) and metal screws (44.9%). Back-up tibial fixation was used rarely or never among 55.9% of respondents.
Figure 3.
Preferred soft tissue (quadriceps and hamstring) graft fixation techniques for ACLR, with the y axis representing percentage of survey respondents. ACLR, anterior cruciate ligament reconstruction.
Surgeons most commonly reported using anterolateral augmentation “rarely” in primary ACLR and “sometimes” in revision ACLR, with most performing lateral extra-articular tenodesis technique versus anterolateral ligament reconstruction (Table 2). Suture tape augmentation was deemed to be used “never” by 76.8% of surgeons and “rarely” by 15.9% of surgeons.
Table 2.
Descriptive Characteristics of Anterolateral Augmentation Use and Technique During ACLR a
| Response | Total Respondents (n = 69) | |
|---|---|---|
| Anterolateral Augmentation Use | ||
| Primary ACLR | Revision ACLR | |
| Always | 0 (0.0) | 7 (10.1) |
| Often | 7 (10.1) | 21 (30.4) |
| Sometimes | 18 (26.1) | 22 (31.9) |
| Rarely | 27 (39.1) | 9 (13.0) |
| Never | 17 (24.6) | 10 (14.5) |
| Anterolateral Augmentation Technique | ||
| LET | 46 (66.7) | |
| ALLR | 10 (14.5) | |
| Other | 2 (2.9) | |
| None | 10 (14.5) | |
Data are presented as n (%). ACLR, anterior cruciate ligament reconstruction; ALLR, anterolateral ligament reconstruction; LET, lateral extra-articular tenodesis.
Surgical Timing, Perioperative Care, and Postoperative Rehabilitation
The most preferred surgical timing of primary ACLR was within 2 to 3 weeks of injury, followed by >3 weeks (Table 3). Most surgeons (72.5%) used a perioperative peripheral nerve block, with most utilizing adductor canal (52.2%), while the majority of surgeons did not use postoperative continuous passive motion (CPM) (82.6%). Regarding return to play, most of the respondents highly valued biometric return-to-sports testing to determine readiness (94.2%), with most weighing time and testing equally. For a hypothetical 20-year-old football player, return-to-sports timing varied widely, primarily between 6 and 10 months postoperatively; 7 months or longerwas the minimum time criteria for most surgeons (71.0%, Table 3).
Table 3.
Descriptive Characteristics of Surgical Timing and Postoperative Rehabilitation After ACLR a
| Variable | Total Respondents (n = 69) |
|---|---|
| Time to primary ACLR | |
| Immediately | 4 (5.8) |
| 1-2 weeks | 16 (23.2) |
| 2-3 weeks | 26 (37.7) |
| >3 weeks | 22 (31.9) |
| CPM (yes) | 12 (17.4) |
| Time until 20-year-old patient returns to football after surgery | |
| 4-6 months | 2 (2.9) |
| 5-7 months | 1 (1.5) |
| 6-8 months | 15 (21.7) |
| 7-9 months | 18 (26.1) |
| 8-10 months | 15 (21.7) |
| 9-11 months | 8 (11.6) |
| 10-12 months | 8 (11.6) |
| No timeline | 1 (1.5) |
| RTS criteria | |
| All time-based | 1 (1.5) |
| Mostly time-based | 3 (4.3) |
| Entirely RTS testing based | 7 (10.1) |
| Mostly RTS testing based | 21 (30.4) |
| Equal time-based and RTS testing-based | 37 (53.6) |
Data are presented as n (%). Time intervals posed to respondents intentionally overlapped; respondents could select the interval that best described their preference. ACLR, anterior cruciate ligament reconstruction;CPM, continuous passive motion; RTS, return to sports.
Results by Surgeon Volume and Experience
Higher volume surgeons (>100 ACLR annually) reported performing single-stage revision ACLR at a significantly higher rate (79.8% vs 62.9%, P = .02). Responses also significantly differed on return-to-sports criteria (P = .01), with higher volume surgeons more commonly reporting “entirely” or “mostly” utilizing biometric return-to-sports testing (57.0%) compared with lower volume surgeons (20.0%). No significant difference in responses was observed in selection of graft type by years of experience (P = .17) and volume (P = .58).
Discussion
The primary finding of this study is that substantial variation exists in surgeon preferences regarding most facets of ACLR, even among a small group of leaders in the field of sports medicine. Members of the Herodicus Society have helped establish much of the literature on ACLR, implying that their techniques are evidenced-based. This reflects the heterogeneity of the ACLR literature and the difficulties that surgeons face when selecting the optimal technique or approach to postoperative management.
Although frequent contradictory findings in the ACLR literature limit evaluating the “best practice” for many techniques, the literature does largely align on some variables. BPTB autograft, with a long track record of low revision rates, was the most common graft (58%), followed by similar rates of quadriceps (15%) and hamstring tendon (14%) autograft. Extensive research has compared failure rates by graft type, with consistent low retear rates in BPTB and inconsistent findings over whether hamstring has higher retear rates.14,31,32 Recent literature has also shown low failure rates following quadriceps autograft as well, comparable with those of BPTB and hamstring tendon autografts, although prospective, high-quality data remain lacking.9,28,30 Allograft, shown most conclusively to have higher retear rates in specific populations,7,19,40 was correspondingly the graft used least frequently (12%). Much literature supports using independent femoral tunnel drilling,12,21,26 which most respondents use (82%). As a greater understanding of ACL anatomy and biomechanical properties has developed, there has been a trend among surgeons to move from transtibial to independent femoral tunnel drilling.35,36 Regarding CPM use, most Herodicus respondents did not use CPM in the postoperative period (83%). This is in line with a recent systematic review of 12 comparative studies demonstrating no significant clinical benefit of CPM usage after ACLR. 8
Most respondents also aligned with literature suggesting away from return to football before 7 months (71%) and utilizing both time- and testing-based criteria for returning to sports (88%).5,20 Literature over the past several years has shown higher rerupture rate with early return to sports,2,22 and there has been a trend toward incorporating biometric testing into clearance for sports that was less common in years past.10,16 Historical studies surveying members of the AOSSM in 2001 and 2006 found that most members allowed return to full sports activity between 5 and 7 months.11,13 In light of these results, the findings of our study suggest that the past 2 decades of literature have established new norms among the leaders of the sports medicine community regarding timing of return to sports.
Regarding newer techniques with less literature, anterolateral augmentation procedures were mostly used “rarely” or “never” in primary ACLR (64%). While some studies do show reduced retear rates with anterolateral augmentation, especially in the high-risk populations and with hamstring tendon autograft,15,23 data on adding it to primary BPTB or quadriceps autograft ACLR are sparse. With minimal data guiding lateral extra-articular tenodesis versus anterolateral ligament reconstruction, most surgeons opted for lateral extra-articular tenodesis (67%), perhaps because of the cost-effectiveness and use of autograft tissue. Suture tape augmentation, which similarly has limited literature consisting of only short-term results, 25 was generally used “rarely” or “never” (93%). This shows that Herodicus surgeons have largely not adopted more recent techniques that are extensively discussed in the recent literature. In discussing with study participants, multiple surgeons cited the lack of mid- to long-term data showing improved outcomes as the reason for not employing these techniques.
Herodicus surgeons diverged from several evidence-based practices in ACLR. Nearly two-thirds of Herodicus surgeons did not soak their graft in vancomycin solution (64%), despite evidence suggesting decreased infection rates with this additional measure.1,3 Similarly, a survey of the ACL study group found that 62% of surgeons did not use a vancomycin solution. 39 The authors of that study noted that the surgeons’ main reason for not using an antibiotic solution was decreased mechanical properties, though the validity of this concern remains debated. 24
Single-stage versus two-stage revision ACLR remains an unsettled topic in the literature,6,27 with justifications for each; however, respondents showed a strong preference toward single-stage revision (72%). The greater rate of single-stage revision ACLR among higher volume surgeons could illustrate reuse of their own correctly placed tunnels, their comfort with the outcomes of single-stage reconstruction, and the efficiency of a single-stage procedure in their busy practice.
The most recent previous large study of the preferences of elite ACLR surgeons surveyed 140 international members of the ACL Study Group and also found significant heterogeneity in surgeon preferences. 34 This variability could be assumed in a widely international group of surgeons, but the present study shows similar inconsistency in a predominantly US surgeon cohort. In that study, Sherman et al 34 found a majority usage of hamstring tendon autograft (53%), in comparison with the predominant usage of BPTB autograft in the present study.
Another international survey study of members of the International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine found that, among 2107 respondents, 80% preferred hamstring tendon autograft and 79% used medial portal femoral drilling. 37 Similar to the present study, antibiotic-soaking of grafts (45%) and anterolateral augmentation (10% in primary ACLR) were used in a minority of cases, and mean time to fully resume sports was 8.9 months. That report varies from the present study in its largely international respondents and polling of a more general population of sports medicine surgeons. An overview of previous similar studies is provided in Table 4.
Table 4.
Survey Studies of ACLR Since 2016 a
| Year | Authors | Participants | Preferred Graft | Tunnel Drilling | Femoral Fixation | Tibial Fixation | IS Screw Type | AL Augment | CPM | RTP |
|---|---|---|---|---|---|---|---|---|---|---|
| 2016 | Grassi et al 18 | SIGASCOT (Italy) | HS 81% | NR | NR | NR | NR | NR | NR | 6-8 months 69% |
| 2016 | Vaishya et al 38 | DAS (India) | HS 83% | AM 90% | Button 94% | IS 96% | Bio 97% | NR | NR | NR |
| 2017 | Budny et al 4 | AOSSM and AANA (US) | HS 45%, BPTB 41% | AM 61% | BPTB: IS 79% ST: Button 79% |
BPTB: IS 98% ST: IS 41% |
NR | NR | 23% | 6-9 months 66% |
| 2021 | Sherman et al 34 | ACL Study Group (International) | HS 53%, BPTB 36% | AM 73% | Button 50% | IS 50% | NR | Rare/never 54% | NR | 6-8 months 44% |
| 2023 | Tuca et al 37 | ISAKOS (Intl) | HS 80% | AM 79% | BPTB: IS 93% ST: Button 83% |
BPTB: IS 95% ST: IS 77% |
BPTB: Metal 49% ST: Bio 81% |
Never 45% | NR | 9 months 33% |
| 2024 | Engler et al, this study | Herodicus (US+) | BPTB 59%, Quad 15% | AM 67% | BPTB: IS 79% ST: Button 80% |
BPTB: IS 77% ST: IS 78% |
Nonmetal 55% | Rare/never 64% | 17% | 7-9 months 26% |
AANA, Arthroscopy Association of North America; ACL, anterior cruciate ligament; ACLR, ACL reconstruction; AL, anterolateral; AM, anteromedial; AOSSM, American Orthopaedic Society for Sports Medicine; Bio, bioabsorbable; BPTB, bone–patellar tendon–bone; CPM, continuous passive motion; DAS, Delhi Arthroscopy Society; HS, hamstring; IS, interference screw; ISAKOS, International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine; NR, not reported; Quad, quadriceps tendon; RTP, return to play; SIGASCOT, Italian Society of Arthroscopy, Knee, Upper Limb, Sports, Cartilage and Orthopaedic Technologies; ST, soft tissue.
Limitations
There are limitations to this study. Respondents were very experienced surgeons, often with an academic component of their practice, which may limit the generalizable nature of the results. The years of surgeon experience could suggest that they may be less inclined to change their surgical techniques over time compared with younger surgeons with less established techniques. Nevertheless, the widespread use of independent femoral tunnel drilling does show a likely evolution in technique over time. Not all Herodicus Society members responded to the survey, introducing possible selection bias. Survey studies inevitably oversimplify clinical scenarios, so use of these data in the care of an individual patient may be limited. The authors recognize that the Herodicus Society is a limited group of surgeons, and there are other experts across the world not included in this survey whose perspectives may differ and are important. Eliciting the opinions of these surgeons in future studies would be a valuable contribution to the literature and would make for more generalizable results.
Conclusion
Our survey demonstrated that a wide range of preferences exist regarding ACLR surgical technique in the Herodicus Society. BPTB autograft is the most frequent primary ACLR graft choice. Participants have broadly not embraced newer techniques such as anterolateral or suture tape augmentation. Return to sports is generally not allowed before 7 months and heavily factors in return-to-sports testing metrics, suggesting that purely time-based criteria for return to sports are not modern practice among elite sports medicine surgeons. Surgeons may use the data from this study as a guide in identifying the appropriate graft type and surgical techniques during ACLR.
Appendix
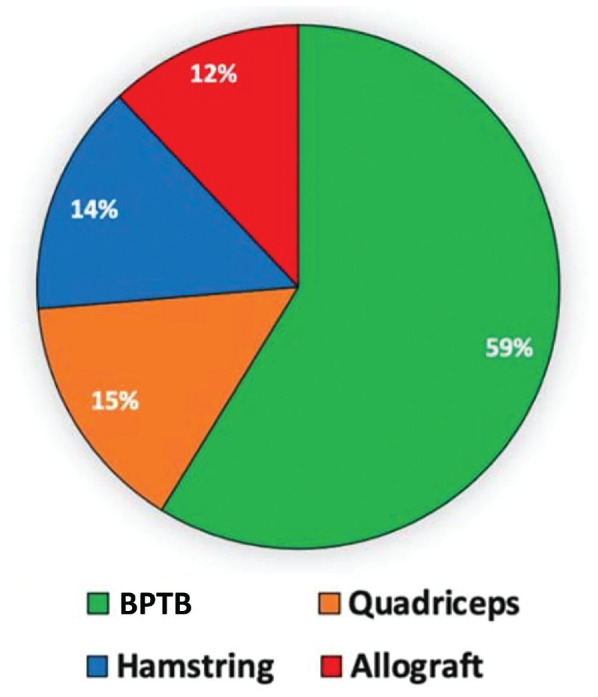
Appendix Figure A1.
Survey administered to the Herodicus Society.
Footnotes
Final revision submitted February 12, 2024; accepted March 5, 2024.
One or more of the authors has declared the following potential conflict of interest or source of funding: I.D.E. has received education payments from Arthrex, Mid-Atlantic Surgical Systems, Smith+Nephew; hospitality payments from Stryker; and a grant from Arthrex. M.A.F. has received education payments from Mid-Atlantic Surgical Systems. A.J.C. has received education payments from Arthrex, Medwest Associates, Mid-Atlantic Surgical Systems, Smith+Nephew, Supreme Orthopedic Systems; hospitality payments from Stryker; and a grant from Arthrex. J.W.A. has received education payments from Mid-Atlantic Surgical Systems; hospitality payments from Arthrex, Mid-Atlantic Surgical Systems, Smith+Nephew; and grants from Arthrex and DJO. V.M. has received nonconsulting fees from Smith & Nephew and Synthes GmbH; and consulting fees from Smith & Nephew. J.P.B. has received consulting fees from Arthrex and DJO; nonconsulting fees from Arthrex; royalties from Arthrex; and education payments from Fones Marketing Management. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
ORCID iDs: Sahil Dadoo  https://orcid.org/0000-0003-0397-6220
https://orcid.org/0000-0003-0397-6220
Justin W. Arner  https://orcid.org/0000-0002-7007-4596
https://orcid.org/0000-0002-7007-4596
References
- 1. Baron JE, Shamrock AG, Cates WT, et al. Graft preparation with intraoperative vancomycin decreases infection after ACL reconstruction: a review of 1,640 cases. J Bone Joint Surg Am. 2019;101(24):2187-2193. [DOI] [PubMed] [Google Scholar]
- 2. Beischer S, Gustavsson L, Senorski EH, et al. Young athletes who return to sport before 9 months after anterior cruciate ligament reconstruction have a rate of new injury 7 times that of those who delay return. J Orthop Sports Phys Ther. 2020;50(2):83-90. [DOI] [PubMed] [Google Scholar]
- 3. Bohu Y, Klouche S, Sezer HB, et al. Vancomycin-soaked autografts during ACL reconstruction reduce the risk of post-operative infection without affecting return to sport or knee function. Knee Surg Sports Traumatol Arthrosc. 2020;28(8):2578-2585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Budny J, Fox J, Rauh M, Fineberg M. Emerging trends in anterior cruciate ligament reconstruction. J Knee Surg. 2017;30(1):63-69. [DOI] [PubMed] [Google Scholar]
- 5. Burgi CR, Peters S, Ardern CL, et al. Which criteria are used to clear patients to return to sport after primary ACL reconstruction? A scoping review. Br J Sports Med. 2019;53(18):1154-1161. [DOI] [PubMed] [Google Scholar]
- 6. Colatruglio M, Flanigan DC, Long J, DiBartola AC, Magnussen RA. Outcomes of 1- versus 2-stage revision anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2021;49(3):798-804. [DOI] [PubMed] [Google Scholar]
- 7. Cruz AI, Jr, Beck JJ, Ellington MD, et al. Failure rates of autograft and allograft ACL reconstruction in patients 19 years of age and younger: a systematic review and meta-analysis. JB JS Open Access. 2020;5(4):e20.00106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. D’Amore T, Rao S, Corvi J, et al. The utility of continuous passive motion after anterior cruciate ligament reconstruction: a systematic review of comparative studies. Orthop J Sports Med. 2021;9(6):23259671211013841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dai W, Leng X, Wang J, Cheng J, Hu X, Ao Y. Quadriceps tendon autograft versus bone-patellar tendon-bone and hamstring tendon autografts for anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2022;50(12):3425-3439. [DOI] [PubMed] [Google Scholar]
- 10. Dan MJ, Lun KK, Dan L, et al. Wearable inertial sensors and pressure MAT detect risk factors associated with ACL graft failure that are not possible with traditional return to sport assessments. BMJ Open Sport Exerc Med. 2019;5(1):e000557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Delay BS, Smolinski RJ, Wind WM, Bowman DS. Current practices and opinions in ACL reconstruction and rehabilitation: results of a survey of the American Orthopaedic Society for Sports Medicine. Am J Knee Surg. 2001;14(2):85-91. [PubMed] [Google Scholar]
- 12. Duffee A, Magnussen RA, Pedroza AD, Flanigan DC, MOON Group, Kaeding CC.Transtibial ACL femoral tunnel preparation increases odds of repeat ipsilateral knee surgery. J Bone Joint Surg Am. 2013;95(22):2035-2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Duquin TR, Wind WM, Fineberg MS, Smolinski RJ, Buyea CM. Current trends in anterior cruciate ligament reconstruction. J Knee Surg. 2009;22(1):7-12. [DOI] [PubMed] [Google Scholar]
- 14. Gabler CM, Jacobs CA, Howard JS, Mattacola CG, Johnson DL. Comparison of graft failure rate between autografts placed via an anatomic anterior cruciate ligament reconstruction technique: a systematic review, meta-analysis, and meta-regression. Am J Sports Med. 2016;44(4):1069-1079. [DOI] [PubMed] [Google Scholar]
- 15. Getgood AMJ, Bryant DM, Litchfield R, et al. Lateral extra-articular tenodesis reduces failure of hamstring tendon autograft anterior cruciate ligament reconstruction: 2-year outcomes from the STABILITY study randomized clinical trial. Am J Sports Med. 2020;48(2):285-297. [DOI] [PubMed] [Google Scholar]
- 16. Gokeler A, Welling W, Zaffagnini S, Seil R, Padua D. Development of a test battery to enhance safe return to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):192-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Grassi A, Carulli C, Innocenti M, et al. New trends in anterior cruciate ligament reconstruction: a systematic review of national surveys of the last 5 years. Joints. 2018;6(3):177-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Grassi A, Vascellari A, Combi A, et al. Return to sport after ACL reconstruction: a survey between the Italian Society of Knee, Arthroscopy, Sport, Cartilage and Orthopaedic Technologies (SIGASCOT) members. Eur J Orthop Surg Traumatol. 2016;26(5):509-516. [DOI] [PubMed] [Google Scholar]
- 19. Kaeding CC, Aros B, Pedroza A, et al. Allograft versus autograft anterior cruciate ligament reconstruction: predictors of failure from a MOON prospective longitudinal cohort. Sports Health. 2011;3(1):73-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kaplan Y, Witvrouw E. When is it safe to return to sport after ACL reconstruction? Reviewing the criteria. Sports Health. 2019;11(4):301-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Keller TC, Tompkins M, Economopoulos K, et al. Tibial tunnel placement accuracy during anterior cruciate ligament reconstruction: independent femoral versus transtibial femoral tunnel drilling techniques. Arthroscopy. 2014;30(9):1116-1123. [DOI] [PubMed] [Google Scholar]
- 22. Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50(15):946-951. [DOI] [PubMed] [Google Scholar]
- 23. Lai S, Zhang Z, Li J, Fu WL. Comparison of anterior cruciate ligament reconstruction with versus without anterolateral augmentation: a systematic review and meta-analysis of randomized controlled trials. Orthop J Sports Med. 2023;11(3):23259671221149403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lamplot JD, Liu JN, Hutchinson ID, et al. Effect of vancomycin soaking on anterior cruciate ligament graft biomechanics. Arthroscopy. 2021;37(3):953-960. [DOI] [PubMed] [Google Scholar]
- 25. Mackenzie CEA, Huntington LS, Tulloch S. Suture tape augmentation of anterior cruciate ligament reconstruction increases biomechanical stability: a scoping review of biomechanical, animal, and clinical studies. Arthroscopy. 2022;38(6):2073-2089. [DOI] [PubMed] [Google Scholar]
- 26. Mao Y, Zhang K, Li J, Fu W. Transtibial versus anteromedial portal technique for femoral tunnel drilling in primary single-bundle anterior cruciate ligament reconstruction: a meta-analysis of level 1 and 2 evidence of clinical, revision, and radiological outcomes. Am J Sports Med. 2023;51(1):250-262. [DOI] [PubMed] [Google Scholar]
- 27. Mitchell JJ, Chahla J, Dean CS, Cinque M, Matheny LM, LaPrade RF. Outcomes after 1-stage versus 2-stage revision anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45(8):1790-1798. [DOI] [PubMed] [Google Scholar]
- 28. Mouarbes D, Menetrey J, Marot V, Courtot L, Berard E, Cavaignac E. Anterior cruciate ligament reconstruction: a systematic review and meta-analysis of outcomes for quadriceps tendon autograft versus bone-patellar tendon-bone and hamstring-tendon autografts. Am J Sports Med. 2019;47(14):3531-3540. [DOI] [PubMed] [Google Scholar]
- 29. Musahl V, Engler ID, Nazzal EM, et al. Current trends in the anterior cruciate ligament part II: evaluation, surgical technique, prevention, and rehabilitation. Knee Surg Sports Traumatol Arthrosc. 2022;30(1):34-51. [DOI] [PubMed] [Google Scholar]
- 30. Perez JR, Emerson CP, Barrera CM, et al. Patient-reported knee outcome scores with soft tissue quadriceps tendon autograft are similar to bone-patellar tendon-bone autograft at minimum 2-year follow-up: a retrospective single-center cohort study in primary anterior cruciate ligament reconstruction surgery. Orthop J Sports Med. 2019;7(12):2325967119890063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Persson A, Fjeldsgaard K, Gjertsen JE, et al. Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: a study of 12,643 patients from the Norwegian Cruciate Ligament Registry, 2004-2012. Am J Sports Med. 2014;42(2):285-291. [DOI] [PubMed] [Google Scholar]
- 32. Samuelsen BT, Webster KE, Johnson NR, Hewett TE, Krych AJ. Hamstring autograft versus patellar tendon autograft for ACL reconstruction: is there a difference in graft failure rate? A meta-analysis of 47,613 patients. Clin Orthop Relat Res. 2017;475(10):2459-2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Shelton WR, Fagan BC. Autografts commonly used in anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2011;19(5):259-264. [DOI] [PubMed] [Google Scholar]
- 34. Sherman SL, Calcei J, Ray T, et al. ACL Study Group presents the global trends in ACL reconstruction: biennial survey of the ACL Study Group. J ISAKOS. 2021;6(6):322-328. [DOI] [PubMed] [Google Scholar]
- 35. Tejwani SG, Prentice HA, Wyatt RWB, Jr, Maletis GB. Femoral tunnel drilling method: risk of reoperation and revision after anterior cruciate ligament reconstruction. Am J Sports Med. 2018;46(14):3378-3384. [DOI] [PubMed] [Google Scholar]
- 36. Tibor L, Chan PH, Funahashi TT, Wyatt R, Maletis GB, Inacio MC. Surgical technique trends in primary ACL reconstruction from 2007 to 2014. J Bone Joint Surg Am. 2016;98(13):1079-1089. [DOI] [PubMed] [Google Scholar]
- 37. Tuca M, Valderrama I, Eriksson K, Tapasvi S. Current trends in anterior cruciate ligament surgery. A worldwide benchmark study. J ISAKOS. 2023;8(1):2-10. [DOI] [PubMed] [Google Scholar]
- 38. Vaishya R, Agarwal AK, Ingole S, Vijay V. Current practice variations in the management of anterior cruciate ligament injuries in Delhi. J Clin Orthop Trauma. 2016;7(3):193-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Xiao M, Sherman SL, Safran MR, Abrams GD. Surgeon practice patterns for pre-soaking ACL tendon grafts in vancomycin: a survey of the ACL Study Group. Knee Surg Sports Traumatol Arthrosc. 2021;29(6):1920-1926. [DOI] [PubMed] [Google Scholar]
- 40. Zeng C, Gao SG, Li H, et al. Autograft versus allograft in anterior cruciate ligament reconstruction: a meta-analysis of randomized controlled trials and systematic review of overlapping systematic reviews. Arthroscopy. 2016;32(1):153-163.e18. [DOI] [PubMed] [Google Scholar]