Abstract
Objectives:
This review aimed to report the estimated pooled level of prevalence, risk factors, and birth outcome of hypertensive disorder of pregnancy in Ethiopia, in 2024.
Design:
A systematic review and meta-analysis approach was utilized.
Data Sources and Methods:
PubMed/MEDLINE, Google Scholar, African Index Medicus, Web of Science, and CINHAL (EBSCO) search was carried out. The result was written according to the PRISMA-updated guidelines. To estimate the pooled prevalence and effect sizes, a random-effect model was used. Heterogeneity was assessed and investigated using I2 test statistics and meta-regression, respectively. Publication bias was assessed using funnel plot and Egger’s test statistics. Statistical tests result at p-value < 0.05 were declared as having significance.
Result:
From a total of 52 primary studies with a total sample size of 269, 158 were included in this systematic review and meta-analysis. The pooled prevalence of hypertensive disorder in pregnancy was 8%. Egger’s test statistics (p = 0.8013) showed there is no publication bias. Having a history of kidney disease (AOR: 3.47), being rural resident (AOR: 2.5), having fruit intake during pregnancy (AOR: 0.39), being overweight (AOR: 2.24), and having multiple pregnancy (AOR: 2.1) were found to have a significant association with hypertensive disorder of pregnancy.
Conclusion:
Overall, the level of prevalence of hypertensive disorders of pregnancy in Ethiopia was significantly increasing. Having a history of kidney disease was found to have a strong association with hypertensive disorders of pregnancy among factors. The most common or dominant adverse maternal and childbirth outcomes were low birth weight, preterm birth, fifth minute low APGAR score; and eclampsia, hemolysis, elevated liver enzymes, and low platelets syndrome, and acute kidney injury. The governments and other stakeholders should work to broaden and strengthen the existing maternal and child health (MCH) practice by incorporating all possible risk factors of hypertensive disorders of pregnancy in MCH guidelines. In addition, a large-scale study is required that considers those important missed variables, especially, in the eastern part of Ethiopia.
Keywords: Preeclampsia, eclampsia, hypertensive disorder of pregnancy, pregnant women
Introduction
Hypertension (HTN) during pregnancy is defined as systolic blood pressure above 140 mmHg and/or diastolic blood pressure above 90 mmHg. Severe HTN is indicated by blood pressure measurements above 170 and 110 mmHg.1,2 HTN during pregnancy is typically diagnosed at least two times, 4 h apart, in previously normotensive women and is often accompanied by new-onset conditions after 20 weeks of gestation.3,4 Hypertensive disorders of pregnancy (HDP), including preexisting and gestational HTN, preeclampsia, and eclampsia, complicate up to 10%–21% of pregnancies, causing significant maternal and perinatal morbidity and mortality.5–9
Maternal mortality globally is alarmingly high, with 810 women dying daily from preventable pregnancy and childbirth causes, with 94% of all deaths occurring in low and lower-middle-income countries.10–12 HDP are a significant global cause of preventable maternal and fetal morbidity, accounting for 15%–18% of maternal deaths and posing a critical health threat.8,9,13,14
Globally, an estimated 2.6 million stillbirths annually, approximately 16%, occur in pregnancies complicated by pregnancy HTN. 15 Also, prematurity, fetal growth restriction, and fetal overgrowth, and the HDPs are identifiable risk factors for newborn morbidity like respiratory distress and neonatal hypoglycemia.16,17 Consequences of HDP were maternal and fetal adverse outcomes which usually characterized or include placental abruption, pulmonary edema, thrombocytopenia, hemolytic anemia, stroke, recurrent seizure, kidney damage, and liver injury intrauterine growth.9,18,19
In the past half-century, the incidence of preeclampsia and maternal mortality has decreased significantly in developed countries. However, in developing countries, the incidence rates of preeclampsia and maternal mortality are still very high. 20 The incidence increased from 16.30 to 18.08 million globally, with a total increase of 10.92 % from 1990 to 2019. Preeclampsia incidence and maternal mortality rates, however, continue to be relatively high in the developing nations.20,21
In sub-Saharan African region, pregnancy-related HTN diseases accounted for 27.2% of maternal deaths in East and Central Africa, 22.7% in Southern Africa, and 17.2% in West Africa region between 2015 and 2020. 22 Similarly, other studies conducted in Ethiopia revealed that HTN disorders during pregnancy accounted for 16%–32.5% of the causes of direct maternal deaths.23–29 Furthermore, perinatal and maternal death rates were shown to be greater in pregnant women with one of the hypertensive disorders than in the majority of low- and middle-income countries and high-income countries. 24
In Ethiopia, different primary studies indicated that the prevalence of HDP ranged from 12.5% to 25.4%.30–35 Also, there are different reports from various systematic reviews conducted in Ethiopia that reported the pooled prevalence of HDP were from 6.8% to 8%.36–38
Several studies have analyzed the risk factors for HDP, and the identified risk factors include maternal age ⩾35, rural residential area, prim gravida, null parity, positive history of abortion, twin pregnancy, lack of ANC follow-up, obesity, a family history of HTN, alcohol intake, heart failure, stroke and left ventricular hypertrophy, smoking, and positive history of diabetes mellitus (DM) were risk factors for hypertensive disorders during pregnancy.39–43
Hypertensive disorder of pregnancy among pregnant women is an outstanding public health problem and an important contributing factor for maternal and prenatal morbidity and mortality in the world especially in developing countries, especially, in Ethiopia. Goal 3 of the Sustainable Development Goals (SDGs) or agenda is to bring down the rate of maternal death worldwide to less than 70 per 100,000 live births by 2030. 44 In line with this, the government of Ethiopia has a plan to reduce maternal mortality from 401 to 140 per 100,000 live births in 2030. 45 Thus, reducing the maternal mortality ratio is one of the SDGs which is a top priority of Ethiopian government health policy. Therefore, prompt detection and handling of the fundamental aspect of obstetric care in Ethiopia is the assessment of HDP and its associated variables in pregnant women attending ANC clinics.46–48
In Ethiopia, the existing systematic review published in 2017, 2018, and 2020 focused only on either of one condition (prevalence, risk factors, or fetomaternal outcome), and they included research articles published up to 2019. After 2019, there were more than 35 primary research that were published regarding burden (incidence), risk factors, and birth outcome among women with HDP in Ethiopia, and reported inconsistent results on the prevalence, incidence, and risk factors.
The inconsistent findings that were reported in these studies are inconvenient for decision-makers, planners, programmers, legislators, and other stakeholders to identify the existing situation. Developing the right interventions and tactics to enhance mother and child health may prove difficult in this regard.
This review is crucial for improving maternal and child health, survival, social capital, and sustainable economic growth in Ethiopia. It will reveal the burden, risk factors, and fetomaternal outcomes among pregnant women with HDP, aiding existing programs. This study will provide insights into obstetrics care, aid in designing a new strategy for better outcomes, detect and track pregnant women with HTN, and serve as a baseline for further research. Therefore, this review aimed to report the overall estimated pooled level of prevalence and identify risk factors and birth outcome of hypertensive disorder of pregnancy which were not reported by other reviews in Ethiopia.
Methods
Protocol approval and registration
This review has been registered with the International Prospective Register of Systematic Reviews (PROSPERO) and registered https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42023482111.
Study design, setting, and period
This study uses a systematic review and meta-analysis which included only studies conducted in Ethiopia up to 12 July 2023.
Eligibility criteria
Inclusion criteria
The Condition, Context, and Population (CoCoPop) 49 format was used to define the study question to be included as follows: Condition outcomes reported “Preeclampsia, Eclampsia, Gestational HTN, pregnancy-induced HTN, HTN during pregnancy, and Chronic HTN during pregnancy.” The context was geographical area “studies conducted in Ethiopia” and the population of interest was “Pregnant women.” Also, the population, exposure, and outcome (PEO) framework was used as follows: Population “pregnant women, and pregnant mother,” exposure “hypertensive disorder of pregnancy,” outcome “adverse birth outcome or fetomaternal outcome.” Articles reported or published only in the English language up to July 2023 were eligible for this systematic review and also unpublished studies or articles were considered.
Exclusion criteria
After careful reviewing of the searched articles, primary studies that were not relevant to the topic or did not focus on the hypertensive disorder of pregnancy, those that did not report the outcome of interest, and those that were not conducted in Ethiopia were excluded from this systematic review. In addition, during the article selection process, studies that were not fully accessible (full text not available) were excluded. However, before excluding the articles, the primary author attempted to contact them at least one time through email.
Data source and search strategy
To identify articles, a comprehensive search of PubMed/MEDLINE, Google Scholar, African Index Medicus (AIM), Web of Science, and CINHAL (EBSCO) search was carried out. In general, the following searching key terms were applied during the search and to combine searching terms using the BOOLEAN operator: “OR” and “AND” designing a search strategy, to be as comprehensive as possible (Annex I), so it is necessary to include a wide range of synonyms key terms for the each of selected terms.
Data quality assessment and extraction
The database search and selection process were processed using EndNote X20 software and Covidence online web-based software and then removing duplicates, and extracting characteristics from each article. Primary studies were screened and assessed for eligibility and quality, which was done independently by two investigators. Conflicts in this process were resolved by consensus. The JBI Critical Appraisal checklist50,51 was used for quality assessment of cross-sectional, case-control, and cohort studies, articles that scored ⩾ 75% were included in the systematic review (Annex II). Data extraction was also employed by the two investigators and also quality and consistency of the review were checked by the investigators. Variables such as authors, region, study year, sample size, proportion of HDP, and effect size are extracted.
Assessment of publication bias and heterogeneity
Examination of publication bias for each meta-analysis was checked by running a funnel plot. Significance test statistics for publication bias were assessed using Egger’s regression test. Based on the regression test result, conclusion was made whether there is publication bias or not. After analyzing and running a forest plot analysis, the heterogeneity was assessed. To assess the degree of heterogeneity cut off I2.
Data synthesis
The overall process and result of this systematic review were written according to the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) updated guidelines. Analysis of the variable with two outcome dichotomous data were combined to get pooled prevalence and odds ratio, as well as predictors such as pooled effect and confidence interval, based on the results obtained from the included article.
All data analysis was done using Stata Crop MP v.17 software. A forest plot with an overall effect size was utilized to describe the results quantitatively for each outcome, and tabulation was employed. The strength of the statistical evidence for the relationship, as indicated by the p-value, and the consistency of the evidence across studies formed the basis of the quantitative assessment of the pooled evidence. In instances where study heterogeneity is identified, a random effect model is utilized. Additionally, a subgroup analysis was carried out according to the area or the location of the study in which the study was conducted, as well as sensitivity analysis was performed.
Results
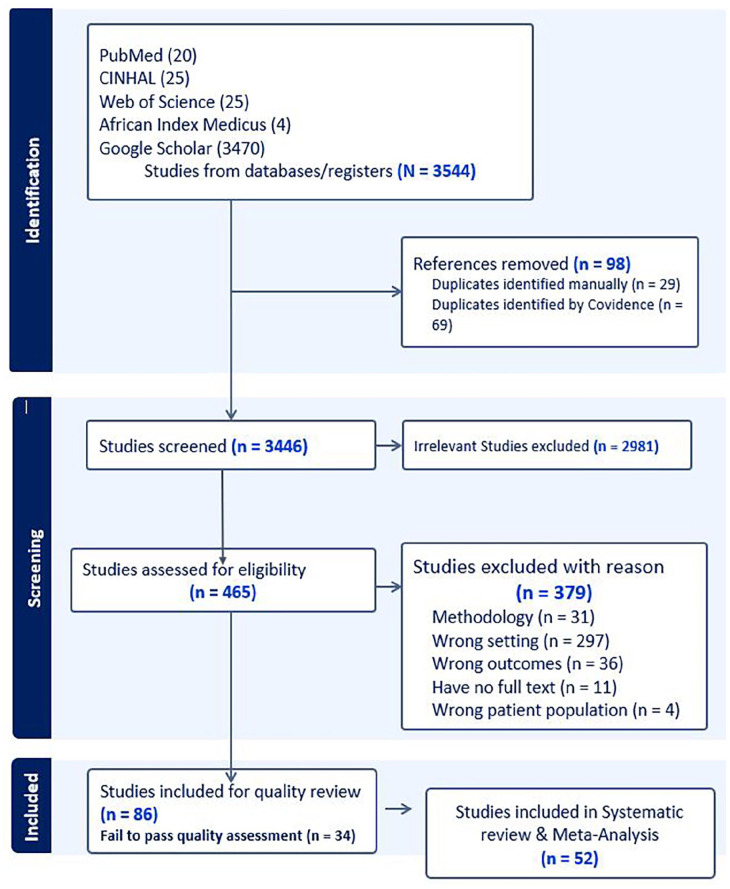
The process of selecting studies for systematic review and meta-analysis
A comprehensive search strategy on different databases, including PubMed, CINHAL, Web of Science, AIM, and Google Scholar, was used to retrieve the published articles. A total of 3544 articles were identified. Out of a total of 3544 articles generated from different databases (CINHAL = 25, African Index Medicus = 4, Google Scholar = 3470, PubMed = 20, Web of Science = 25) (Figure 1).
Figure 1.
Prisma flow chart of study selection for systematic review and meta-analysis of burden, risk factors, and adverse birth outcomes of hypertensive disorder of pregnancy in Ethiopia, 2024.
Characteristics of included studies in systematic review
Finally, after quality assessment, there were a total of 52 published articles included in this systematic review that consisted of cross-sectional (28), case–control (16), and cohort (8) studies with a total sample size of 269,158. Of these, the largest sample size was 174,561 from a national survey, while the smallest sample size was 129 from the Oromia region. The majority of these studies were conducted in Amhara (17) and Southern (15) Ethiopian regions. The study included research articles published between 2011 and 2013, and 65% of these were published after 2019. The highest prevalence of HDP reported was 17.25% in Harari and the lowest rate was 1.2% reported by a multicenter survey. Among the studies included 22 that reported prevalence rates, 33 included risk factors, and 19 reported adverse birth outcomes (Table 1).
Table 1.
Descriptive summary of 52 studies included in the systematic review of burden, risk factor, and birth outcome of HDP in Ethiopia 2024.
| Author, year | Pub/year | Study design | Study region | Sample size | HDP (%) | Associated factors reported (OR; 95% CI) | Birth outcome | Quality score (%) |
|---|---|---|---|---|---|---|---|---|
| Amare, Olani, et al., 2021 52 | 2021 | Cross–sectional | Southern Ethiopia | 215 | — | Being primipara (AOR = 4.6; 95% CI:1.6–13.2), multipara (AOR = 3.1; 95% CI:1.09–9.17), lack of antenatal care visit (AOR = 4.2; 95% CI: 1.2–15.01), late provision of drug (AOR = 3.9;95% CI: 1.9–7.9) | Preterm birth, low birth weight, stillbirth, and IUFD | 88.8% |
| Andarge, Anshebo, et al., 2020 53 | 2020 | Cross–sectional | Southern Ethiopia | 242 | 9.9% | Previous history of preeclampsia (AOR = 8.9; 95% CI: 1.03, 16.61), gestational diabetes mellitus (AOR = 5.8, (1.38, 17.54)) and twin pregnancy (AOR = 1.72; 95% CI: 1.05, 3.71) | — | 87.50% |
| Asefa, Hunde, et al., 2020 54 | 2020 | Cross–sectional | Oromia Region | 1980 | 10.2% | — | HELLP syndrome, abruptio placenta, aspiration pneumonia, pulmonary edema | 87.50% |
| Asfaw, 2014 55 | 2014 | Cross–sectional | Addis Ababa | 3351 | 7.8% | — | HELLP syndrome, eclampsia, pregnancies terminated, stillbirth and put under conservative management | 87.50% |
| Asres, Daga, et al., 2022 56 | 2022 | Case–control study | Southern Ethiopia | 1047 | — | A family history of HTN ((AOR = 11.5; 95% CI: 6.46–20.41), family history of diabetes mellitus (AOR = 2.1; 95% CI: 1.10–3.90), having two or multiple pregnancies (AOR = 6.33; 95% CI: 2.28–17.51), primigravida (AOR = 1.49; 95% CI: 1.01–2.21), and being gravida 5–9 (AOR = 2.47; 95% CI: 1.34–4.58)) | — | 80% |
| Asres, Daga, et al., 2020 57 | 2020 | Case–control study | Amhara Region | 330 | — | Multiple pregnancies (AOR = 2.75; 95% CI: 1.20–6.28), implant contraceptive method (AOR = 0.39; 95% CI: 0.13–0.96) | — | 80% |
| Asres, Tilahun, et al., 2023 58 | 2023 | Case–control study | Amhara Region | 330 | — | History of abortion (AOR = 3.17; 95% CI: 1.31–7.70); change of paternity (AOR = 3.16; 95% CI: 1.47–6.83); previous use of implants (AOR = 0.41; 95% CI: 0.13–0.96); and fruit intake during pregnancy (AOR = 0.36; 95% CI: 0.18–0.72) | — | 80% |
| Asseffa and Demissie, 2019 59 | 2019 | Cross–sectional | Southern Ethiopia | 7347 | 2.3% | — | Eclampsia, hemolysis, elevated liver enzyme syndrome, acute kidney injury, postpartum hemorrhage, DIC, and pulmonary edema | 88.80% |
| Ayalew, Bantie, et al., 2019 60 | Preprint | Cross–sectional | Amhara Region | 193 | 13% | Having a family history of HTN (AOR = 4.61 (1.06, 20.07)), Gestational diabetes mellitus (AOR = 11.41 (1.40, 92.83)), using traditional medicine during pregnancy (AOR = 26.29 (3.68, 187.84)) | — | 75% |
| Ayele and Tilahun, 2022 31 | 2022 | Cross sectional | Amhara Region | 261 | 15.7% | Age at menarche (10–15 years) (AOR = 4.79; 95% CI: 2.07–15.27), unwanted pregnancy (AOR:1.29; 95% CI: 1.59–8.44), history of chronic HTN (AOR:2.93; 95% CI: 1.00–6.20), BMI ⩾ 30 kg/m2 (AOR: 1.79; 95% CI: 1.06–3.65), and alcohol consumption (AOR:2.12; 95% CI: 4.00–14.14) | — | 75% |
| Melese, Aynalem, et al., 2021 61 | 2021 | Cross–sectional | Amhara Region | 456 | — | — | Abruptio placenta, DIC, HEELPS syndrome, acute renal failure, PPH, death aspiration pneumonia, pulmonary embolism, pulmonary edema | 75% |
| Beketie, Tafese, et al., 2022 62 | 2022 | Case–control study | Southern Ethiopia | 426 | — | Nulliparity (AOR 3.81; 95% CI: 1.55,9.34); multiplicity of pregnancy (AOR 3.62; 95% CI: 1.08–12.13) having preeclampsia history (AOR 10.11; 95% CI: 4.06–25.21); parents’ history of HTN had (AOR 2.95; 95% CI: 1.11–7.68); and drinking alcohol (AOR 4.42; 95% CI: 2.15–9.08) | — | 90% |
| Belay and Wudad, 2019 63 | 2019 | Cross–sectional | Oromia Region | 129 | 12.4% | Age (AOR = .009; 95% CI: 0.000–0.317), current multiple pregnancy (AOR = .071; 95% CI: 0.007, 0.773) and history of diabetes mellitus (AOR = .058; 95% CI: 0.007–0.465) | — | 75% |
| Belayhun, Kassa, et al., 2021 64 | 2021 | Case–control study | Southern Ethiopia | 283 | — | Rural residents (AOR:2.25; 95% CI: 1.09–4.65), illiterate (AOR: 3.12; 95% CI: 1.20–8.08), having a history of pregnancy–induced HTN (AOR:6.62; 95% CI: 2.4–17.7), history of kidney disease (AOR: 3.14; 95% CI: 1.05–9.38), and family history of HTN (AOR:5.59; 95% CI: 2.73–11.45) eating vegetables and fruit (AOR: 0.23; 95% CI: 0.06–0.79) | — | 80% |
| Berhan and Endeshaw, 2015 65 | 2015 | Cohort study | Southern Ethiopia | 1015 | — | — | Maternal deaths, eclampsia | 81.80% |
| Berhe, Ilesanmi, et al., 2020 66 | 2020 | Cohort study | Tigray Region | 782 | — | — | Low birth weight, birth asphyxia, small for gestational age, preterm delivery, stillbirth, admission to neonatal intensive care unit, and perinatal death | 100% |
| Birhanu, Temesgen, et al., 2020 67 | 2020 | Cohort study | Amhara Region | 242 | — | Having a preexisting history of diabetes mellitus (AHR = 2.7; 95% CI: 1.43–8.81), having a history of multiple pregnancies (AHR = 3.4 (95% CI = 2.8–6.9)) and being ⩾35 years old age (AHR = 2.5; 95% CI: 1.42–3.54) | — | 81.80% |
| Chemeda, Gurmesa, et al., 2022 68 | 2022 | Cross–sectional | Southern Ethiopia | 403 | 6.8% | Being rural residents (AOR: 2.35; 95% CI: 1.45–3.88), Age > 35 years (AOR: 4.06; 95 %CI: 1.38–11.95), unable to read and write (AOR: 2.15; 95% CI: 1.18–3.90), multipara (AOR: 1.96; 95% CI: 1.16–3.34) and multigravida (AOR: 2.08; 95% CI: 1.16–3.72) | — | 87.50% |
| Endeshaw and Berhan, 2015 69 | 2015 | A case–control study | Amhara Region | 453 | — | Taking coffee daily during pregnancy, (AOR = 1.78; 95% CI: 1.20–3.05), taking fruit or vegetable (AOR = 0.51; 95% CI: 0.29–0.91), intake of folate (AOR = 0.16; 95% CI: 0.08–0.29). | — | 80% |
| Endeshaw, Abebe, et al., 2016 70 | 2016 | A case–control study | Amhara Region | 453 | — | Advanced maternal age (AOR = 4.79; 95% CI: 1.031–22.18), family history of HTN (AOR = 11.16; 95% CI: 5.41–41.43), history of diabetes mellitus (AOR = 6.17; 95% CI: 2.11–20.33), UTI in the current pregnancy (AOR = 6.58; 95% CI: 2.93–14.73), failure to comply with iron and folic acid supplements during pregnancy (AOR = 8.32; 95% CI: 3.35–20.62), lack of exercise (AOR = 3.33; 95% CI: 1.35–8.17), multiple pregnancies (AOR = 4.05; 95% CI: 1.57–12.27), anemia (AOR = 4.19;95% CI 1.27–13.92), and periodontal disease or gingivitis (AOR = 3.51; 95% CI: 1.14–10.83) | — | 80% |
| Endeshaw, Abebe, et al., 2016 71 | 2016 | A case–control study | Amhara Region | 453 | — | Obesity (AOR = 3.63; 95% CI: 1.89, 6.97), women age ⩽24 (AOR = 2.31, 95 % CI: 1.06–5.12), women age 25–29 years (AOR = 3.66; 95% CI: 1.37–10.87) | — | 80% |
| Figa, Temesgen, et al., 2021 72 | 2021 | Cross–sectional study | Southern Ethiopia | 295 | — | Rural residence (AOR = 5.038; 95% CI 1.971–12.879), gestational age ⩽33 weeks (AOR = 3.67; 95% CI: 1.829–7.364), and admission of women with a diagnosis of severe preeclampsia (AOR = 6.42;95% CI: 2.017–21.103) | HELLP syndrome, DIC, and renal failure | 87.50% |
| Fikadu, 2021 73 | 2020 | A case–control study | Southern Ethiopia | 527 | — | Primary relatives who had a history of chronic HTN (AOR 2.1; 95% CI: 1.06–4.21), family history of diabetes mellitus (AOR 2.35; 95% CI: 1.07–5.20), preterm gestation (AOR = 1.56; 95% CI: 1.05–2.32), and pre–conception smoking exposure (AOR = 4.16; 95% CI: 1.1–15.4) | — | 87.50% |
| Gaym, Bailey, et al., 2011 74 | 2011 | Cross–sectional study | Country wise | 174561 | 1.2% | — | — | 100% |
| Getahun, Benti, et al., 2022 75 | 2023 | Cross–sectional study | Addis Ababa | 313 | 11.5% | Maternal age (AOR = 3.15, 1.13, 8.79), diabetic mellitus (AOR = 7.35, 1.79, 30.02), chronic HTN (AOR = 3.26, 1.17, 9.06), family history of pregnancy-induced HTN (AOR = 4.18, 1.37, 12.77), and history of kidney disease (AOR = 3.62, 1.21, 10.88) | — | 75% |
| Tessema, Tekeste, et al., 2015 76 | 2015 | Cross–sectional study | Amhara Region | 490 | 8.4% | Having family history of HTN ((AOR) = 7.19 (95% CI: 3.24–15.2)), chronic HTN (AOR = 4.3 (95% CI: 1.33–13.9)), age ⩾ 35 years (AOR = 4.5 (95% CI: 1.56–12.8)), family history of diabetes mellitus (AOR = 2.4 (95% CI: 1.09–5.6)) and being unmarried (AOR = 3.03 (95% CI: 1.12–8.2)) | — | 75% |
| Godana, Dessalegn, et al., 2021 77 | 2021 | Cohort study | 217 | — | Lack of ANC follow-up (AHR: 1.75; 95% CI: 1.22–2.51), presence of maternal leukocytosis (AHR: 1.53; 95% CI: 1.12–2.09), elevated serum creatinine (AHR: 1.51; 95% CI: 1.05–2.17), and maternal age of 20–35 years (AHR: 0.61; 95% CI: 0.41–0.90) | — | 90.9% | |
| Gudeta and Regassa, 2019 78 | 2019 | Cross–sectional study | Oromia Region | 422 | 7.9% | Positive family history of pregnancy HTN (AOR5.25 (1.39–19.86)), kidney diseases (AOR 3.32 (1.04–10.58)), having asthma (AOR 37.95 (1.41–1021)) and gestational age (AOR 0.096 (0.04–0.23)) | — | 87.50% |
| Jaleta, Gebremedhin, et al., 2021 79 | 2021 | Cohort study | Oromia Region | 777 | — | — | Low birth weight, preterm birth, fifth-minute low Apgar score, admission to neonatal intensive care unit, stillbirth and perinatal mortality | 91% |
| Birhanu Jikamo, 2022 80 | 2022 | A case–control study | Southern Ethiopia | 816 | — | Having a low wealth status (AOR: 1.98; 95% CI: 1.34–2.92), women who had early neonatal deaths (AOR: 5.09; 95% CI: 1.69–9.36), women who did not attend school (AOR: 3.00; 95% CI: 1.10–8.19) | — | 80% |
| Jikamo, Adefris, et al., 2022 81 | 2022 | Cohort study | Southern Ethiopia | 1015 | — | — | Maternal death, maternal ICU admission, postpartum hemorrhage, antepartum hemorrhage, and blood transfusion | 90.90% |
| Jikamo, Adefris, et al., 2022 82 | 2022 | Cohort study | Southern Ethiopia | 733 | — | — | Perinatal death, stillbirth, small for gestational age, preterm birth, birth asphyxia and low birth weight | 90.90% |
| Kahsay, Gashe, et al., 2018 83 | 2018 | A case–control study | Tigray Region | 330 | — | Consume fruits regularly (AOR = 5.1 95% CI: 2.4,11.15). Overweight (BMI > 25 kg/m2 (AOR = 5.5 95% CI: 1.12, 27.6) diabetic (AOR = 5.4, 95% CI: 1.1, 27.0) | — | 90% |
| Kahsay, Gashe, et al., 2018 84 | 2018 | Cross–sectional study | Tigray Region | 45,329 | 3% | — | — | 88.80% |
| Kibret, Chojenta, et al., 2020 85 | 2020 | A case–control study | Amhara Region | 340 | — | High dietary diversity (AOR) = 0.45; 95% CI: 0.21, 0.93) Being merchant (AOR = 3.71 (95% CI: 1.16, 11.89), having a previous history of HDP (AOR = 27.58; 95% CI: 4.53, 168) and high hemoglobin level (AOR = 2.26; 95% CI: 1.66, 3.09) | — | 80% |
| Kidane, Eshete, et al., 2022 86 | 2022 | A case–control study | Oromia Region | 333 | — | Plant source food-based dietary pattern (AOR = 0.36 95% CI: 0.15–0.82), balanced type of dietary pattern (AOR = 0.24 95% CI: 0.11–0.51), and folate intake (AOR = 0.17 95% CI: 0.06–0.48), Previous history of pregnancy-induced HTN (AOR = 3.76 95% CI: 1.67–8.37), twin pregnancy (AOR = 3.69 95% CI: 1.52–8.96), history of abortion (AOR = 2.37 95% CI: 1.10–5.12), presence of anemia at the first visit (AOR = 7.12 95% CI:2.30–21.98), gestational diabetes (AOR = 3.12 95% CI: 1.002–9.72) and highest wealth index (AOR = 4.17 95% CI: 1.27–13.66) | — | 80% |
| Legesse, Berhe, et al., 2019 87 | 2019 | Cross–sectional study | 8502 | 5.1% | — | Maternal death, eclampsia, renal failure, stillbirth, early neonatal deaths, and low APGAR score | 75.00% | |
| Jiregna, Assefa, et al., 2023 88 | Unpublished | Cross–sectional study | Harari Region | 400 | 17.25% | Maternal age ⩾ 35 ((AOR = 4.50; 95% CI 1.89–10.76)), history of preeclampsia (AOR = 2.42; 95% CI 1.16–5.04); family history of chronic HTN (AOR = 4.54;95% CI 2.23–9.23); anemic (AOR = 2.62; 95% CI 1.35–5.09); and chewing khat (AOR = 2.98; 95% CI 1.50–5.91) | Stillbirth, low birth weight | 87.50% |
| Mekie, Mekonnen, et al., 2020 89 | 2020 | A case–control study | Amhara Region | 330 | — | Short cohabitation duration (AOR = 2.13, 95% CI (1.104.1), unplanned pregnancy (AOR = 2.35, 95% CI (1.01, 5.52), high body weight (AOR = 2.00, 95% CI (1.10, 3.63), antenatal advice about nutrition (AOR = 0.52, 95% CI (0.29, 0.96), vegetable intake (AOR = 0.42, 95% CI (0.22, 0.82) and fruit intake during pregnancy (AOR = 0.45, 95% CI (0.24, 0.87)) | — | 80% |
| Melese, Badi, et al., 2019 90 | 2019 | Cross–sectional study | Amhara Region | 456 | — | — | Eclampsia, stillbirth, low birth weight | 75% |
| Sium, Lucero-Prisno, et al., 2022 91 | 2022 | A case–control study | Addis Ababa | 173 | — | — | Preterm birth, respiratory distress syndrome, early neonatal death, and low Apgar score | 80% |
| Syoum, Abreha, et al., 2022 92 | 2022 | Cross–sectional | Tigray Region | 497 | — | — | Low Apgar score, low birth weight, preterm, intensive care unit admissions, IUGR, Neonatal asphyxia | 87.50% |
| Tesfa, Munshea, et al., 2023 93 | 2022 | A case–control study | Amhara Region | 336 | — | Being primiparous (AOR): 3.19 at 95% CI: 1.71, 5.97), family history of HTN (AOR: 4.14; 95% CI: 1.71, 10.05), previous history of PE (AOR: 7.97; 95% CI: 2.42, 26.63), number of ANC visits (AOR: 5.43 at 95% CI: 2.86, 10.33), not taking iron and folic acid supplement (AOR: 4.46; 95% CI: 1.59, 12.48), body mass index ⩾25 kg/m2 (AOR: 3.47; 95% CI: 1.78, 6.77), not consuming vegetables (AOR: 1.99; 95% CI: 1.07, 3.69) and not consuming egg, milk and milk products (AOR: 3.00; 95% CI: 1.47, 6.11) | — | 90% |
| Tesfahun, Tadesse, et al., 2023 94 | 2023 | Cross–sectional | Addis Ababa | 235 | 5.5% | Age > 35 years, (AOR = 2.1,95% CI: 1.3–3.4), history of preeclampsia (AOR = 8.5; 95% CI: 1.2–10.3), history of HTN (AOR = 2.9; 95% CI: 3.0–7.3), ANC visit <3 times (AOR = 8.5; 95% CI: 3.1–13.4), and family history of HTN (AOR = 2.2; 95% CI: 1.24.3) | — | 75% |
| Tesfaye, Tefera, et al., 2018 95 | 2018 | Cross–sectional | Oromia Region | 356 | 10.3% | Rural residence (AOR) = 5.3,95% CI: 1.518–18.5), positive family history of HTN (AOR = 9.9, 95% CI: 2.31–42.4), positive family history of pregnancy-induced HTN (AOR = 9.13 (2.33–35.78)), kidney diseases (AOR = 3.97, 95% CI: 1.36–11.56) and psychological stress (AOR = 5.79; 95% CI: 1.6–20.2) | — | 87.50% |
| Tlaye, Endalifer, et al., 2021 96 | 2021 | Cross–sectional | Amhara Region | 8764 | 2.76% | Being multigravida (AOR) 0.154, 95% CI 0.029–0.831) and spontaneous onset of labor (AOR 5.628; 95% CI: 1.1247 –9.401) | — | 75% |
| Walle and Azagew, 2019 46 | 2019 | Cross–sectional | Amhara Region | 422 | 16.8% | Age < 24 (AOR = 0.31; 95% CI: 0.05, 0.027). Have family history of HTN (AOR = 7.77; 95% CI: 3.037–19.62), alcohol users (AOR = 1.984; 95% CI: 0.77–5.108) | — | 75% |
| Wassie and Anmut, 2021 97 | 2021 | Cross–sectional | Addis Ababa | 185 | 6.2% | — | Abruption of the placenta, postpartum hemorrhage and HELLP syndrome, stillbirth, NICU admission | 75% |
| Obsa and Wolka, 2018 98 | 2018 | Cross–sectional | Southern Ethiopia | 225 | — | — | IUGR, still birth, Fetal asphyxia, Meconium aspiration | 75% |
| Welesemayat, Taye, et al., 2020 99 | 2020 | Cohort study | Tigray Region | 715 | — | — | SGA, low birth weight, poor gestational weight gain | 81.80% |
| Wodajo, 2016 100 | 2016 | Cross–sectional | Amhara Region | 320 | 8.8% | Rural residence (AOR: 4.409; 95% CI: (1.459, 13.324)). zero parity (AOR: 11.363; 95% CI: (3.991, 28.35)). multiple pregnancies (AOR: 3.37; 95% CI: (1.18, 10.44)). history of renal disease (AOR: 3.5; 95% CI: (1.96, 20.63)). history of cardiac disease (AOR: 6.56; 95% CI: (4.065, 32.219)) | — | 87.50% |
| Yesuf, 2018 101 | Unpublished | Cross–sectional | Southern Ethiopia | 353 | 9.6% | Previous history of preeclampsia (AOD = 3.85; (95% CI: 1.19–12.49)), preexisting chronic HTN (AOD = 4.84; (95 % CI: 1.02–22.94)), preexisting renal disease (AOD = 4.91; (95% CI: 1.42–16.95)), family history of HTN (AOD = 7.90; (95% CI: 2.59–24.15)) and family history of preeclampsia (AOD = 6.45; (95% CI: 1.50–27.76)) | — | 87.50% |
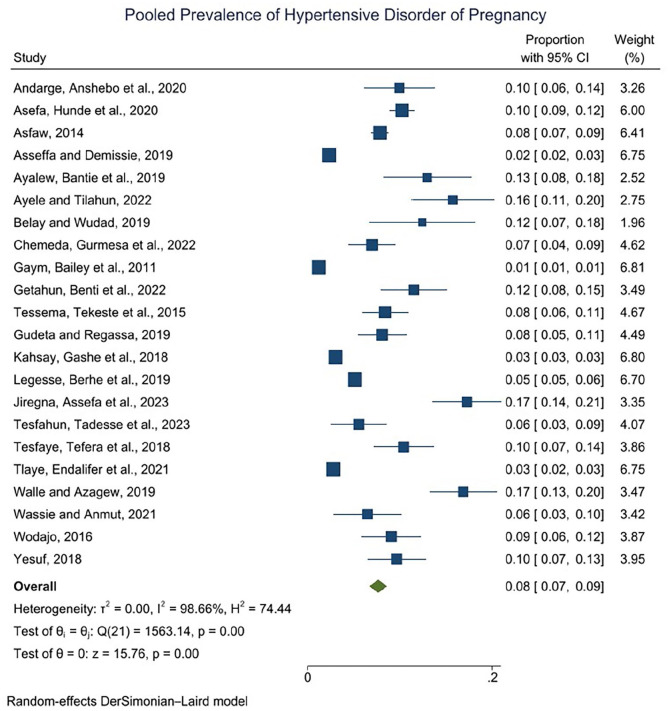
Pooled prevalence of hypertensive disorder of pregnancy in Ethiopia
The pooled prevalence of hypertensive disorder of pregnancy among pregnant women in Ethiopia was 8% (95% CI: 7–9). There was high heterogeneity between the included studies which were exhibited by I2 = 98.66%, p = 0.001) (Figure 2). Therefore, to deal with and investigate the source of heterogeneity subgroup analysis, meta-regression and sensitivity analysis were done.
Figure 2.
Pooled prevalence of hypertensive disorder of pregnancy among pregnant women in Ethiopia, 2024.
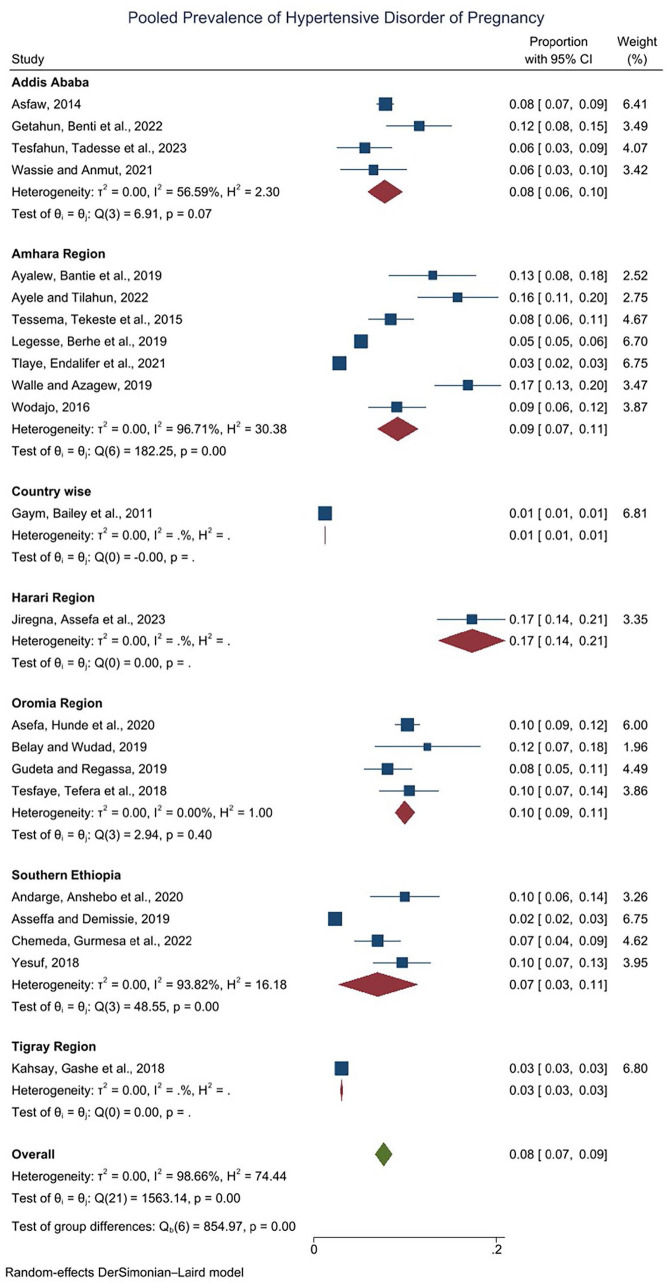
Subgroup analyses of pooled estimated prevalence of HDP.
Subgroup analyses of the pooled estimated prevalence of HDP were performed according to the study region to explore the source of heterogeneity. There is high heterogeneity within studies conducted in the Amhara Region and Southern Ethiopia which is I2 = 96.7% and 93.8%, respectively (Figure 3).
Figure 3.
Subgroup analyses of pooled estimated prevalence of hypertensive disorder of pregnancy, 2024.
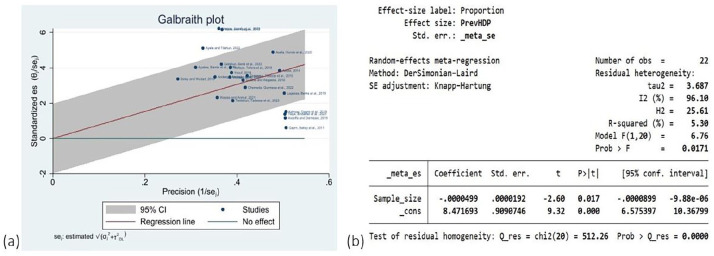
Heterogeneity investigation through Galbraith plot and meta-regression
Galbraith plot shows a visual impression of the amount of heterogeneity in meta-analysis, As shown in the figure majority of the studies are out of the line of regression above and below line ±2 or 95% boundaries of the overall standardized, so this means they are a source of heterogeneity. The meta-regression r-square result indicates that around 5.3% of heterogeneity in the meta-analysis was introduced due to sample size differences in the study (Figure 4).
Figure 4.
(a) Galbraith plot shows the source of heterogeneity, (b) meta-regression to investigate the source of heterogeneity in pooled estimate of hypertensive disorder of pregnancy among pregnant women in Ethiopia, 2024.
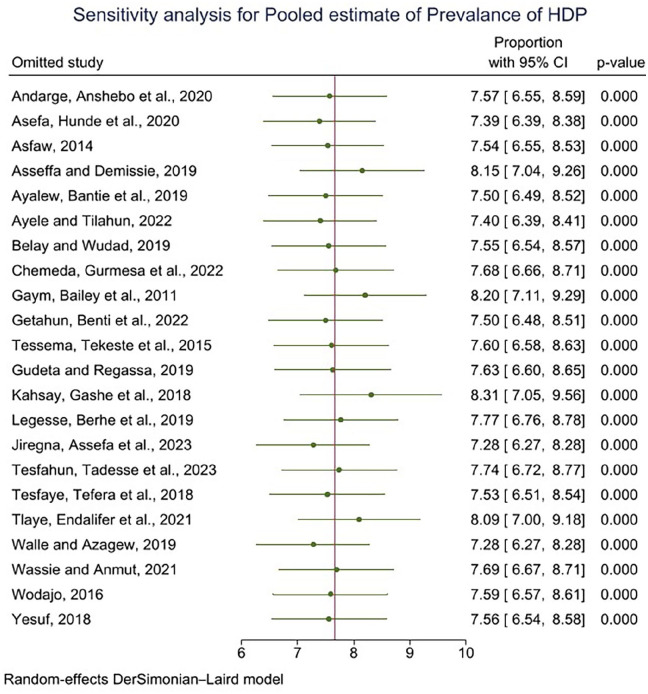
Sensitivity analysis on the pooled prevalence of hypertensive disorder of pregnancy
The displayed effect size for each study corresponds to an overall effect size computed from a meta-analysis excluding that study. The omission of study 13 83 or 9 74 seems to have a relatively larger influence (when compared with other studies) on the estimation of the overall prevalence. Omitting study 13 causes the overall prevalence to increase by roughly 0.3% (from 8% to 8.3%, whereas omitting studies 15 and 19 causes the overall prevalence to decrease by roughly 0.72% (8%–7.28%) (Figure 5).
Figure 5.
Sensitivity analysis on the pooled prevalence of hypertensive disorder of pregnancy, 2024.
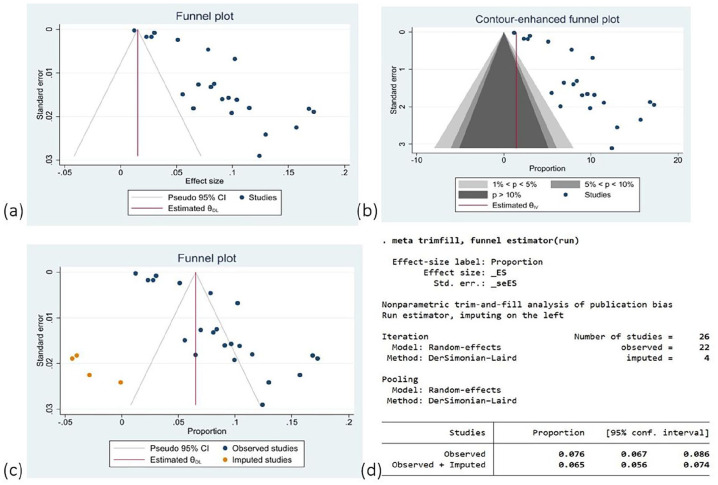
Assessment of publication bias in the pooled prevalence of hypertensive disorder of pregnancy
There is evidence of publication bias from the visual inspection of the funnel plot and statistical significance. Also, the nonparametric (Trim and fill method) test indicates evidence of publication bias. Based on the contour-enhanced funnel plot, it appears that a lot of studies were missing from both the significant and nonsignificant regions of the funnel plot. Under the funnel plot, more studies are missing in both regions. Therefore, the asymmetry in this meta-analysis is due to other factors such as heterogeneity (Figure 6).
Figure 6.
(a) Funnel plot, (b) counter-enhanced plot, (c and d) Funnel plot and trim-and-fill method for assessment of publication bias in the pooled prevalence of hypertensive disorder of pregnancy, 2024.
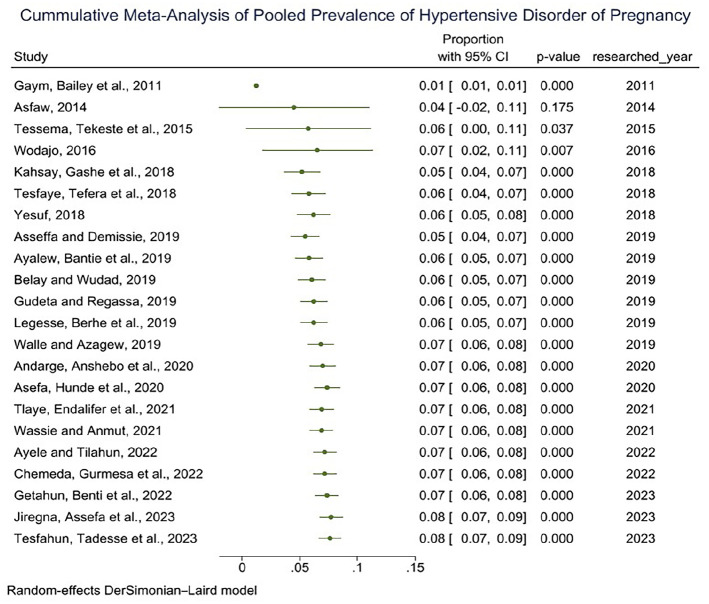
Cumulative meta-analysis (trend analysis) of pooled prevalence of HTN disorder of pregnancy
To explore the trend in the proportion or prevalence rate, we have used a year in which research was conducted. From year to year when more research was conducted, the overall prevalence of HTN disorder in pregnancy significantly (p-value) increases (Figure 7).
Figure 7.
Cumulative meta-analysis (trend analysis) of pooled prevalence of HTN disorder of pregnancy, 2024.
Risk factors associated with hypertensive disorder of pregnancy and assessment of publication bias
The finding of this meta-analysis showed several significant factors associated with HDP among these factors and the following were those variables that showed a strong association with HDP. Women having a history of kidney disease were 3 (AOR: 3.47; 95% CI: 1.2–5.7) times more likely to develop HDP than women who have no history of kidney disease. Women who have a family history of HTN were 3 (AOR: 3.57; 95% CI: 2.3–4.8) times more likely to develop HDP than women who have no family history of HTN. Those women who have a history of preeclampsia were 5 (AOR: 5.5; 95% CI: 2.7–8.2) times more likely to develop HDP than women who have no history of preeclampsia (Table 2).
Table 2.
Determinant factors associated with hypertensive disorder of pregnancy among pregnant women in Ethiopia 2024.
| Determinants of HDP | First author | OR (95% CI) | POR (95% CI) | Heterogeneity test | Publication bias | |
|---|---|---|---|---|---|---|
| I2 = % | p−Value | Egger test p−value | ||||
| Having history of kidney disease | Wodajo, 2016 100 , Tesfaye, Tefera et al., 2018 95 , Gudeta and Regassa, 2019 78 , Belayhun, Kassa et al., 2021 64 , Getahun, Benti et al., 2022 75 | 3.5 (5.82, 12.82), 3.97 (1.13, 9.07), 3.32 (1.45, 6.87), 3.14 (1.02, 7.3), 3.62 (1.22, 8.46) | 3.47 (1.20, 5.74) | 0.00% | <0.0001 | 0.9392 |
| Pregnant women age > 35 years | Chemeda, Gurmesa et al., 2022 68 , Endeshaw, Abebe et., 2016 71 , Tessema, Tekeste et al., 2022 76 , Jiregna, Assefa et al., 2023 88 , Tesfahun, Tadesse et al., 2023 94 | 4.06 (−1.2, 9.32), 4.79 (−5.75, 15.3), 3.15 (0.68, 6.98), 4.5 (1.12, 10.12), 4.5 (0.07, 8.93) | 2.43 (1.48, 3.38) | 0.00% | <0.0001 | 0.4524 |
| Being overweight | Ayele and Tilahun, 2022 31 , Endeshaw, Abebe et al., 2016 71 , Kahsay, Gashe et al., 2018 83 , Mekie, Mekonnen et al., 2020 89 , Tesfa, Munshea et al., 2023 93 | 1.79 (0.49, 3.08), 3.63 (1.09, 6.17), 5.5 (−7.74, 18.74), 2 (0.73, 3.27), 3.4 (0.9, 5.89) | 2.24 (1.44, 3.05) | 0.00% | <0.0001 | 0.1920 |
| Being rural resident | Belayhun, Kassa et al., 2021 64 , Chemeda, Gurmesa et al., 2022 68 , Figa, Temesgen et al., 2021 72 , Tesfaye, Tefera et al., 2018 95 , Wodajo, 2016 100 | 2.25 (0.47, 4.03), 2.35 (1.14, 3.56), 5.04 (0.42, 10.49), 5.3 (3.2, 13.8), 4.4 (1.53, 10.32) | 2.5 (1.53, 3.47) | 0.00% | <0.0001 | 0.2091 |
| Having family history of HTN | Asres, Daga et al., 2022 56 , Ayalew, Bantie et al., 2019 60 , Beketie, Tafese et al., 2022 62 , Belayhun, Kassa et al., 2021 64 , Endeshaw, Abebe et al., 2016 71 , Fikadu, 2021 73 , Getahun, Benti et al., 2022 75 , Tessema, Tekeste et al., 2022 76 , Gudeta and Regassa, 2019 78 , Tesfa, Munshea et al., 2023 93 , Tesfahun, Tadesse et al., 2023 94 , Tesfaye, Tefera et al., 2018 95 , Walle and Azagew, 2019 46 , Yesuf, 2018 101 | 11.5 (4.73, 18.27), 4.6 (−4.92, 14.12), 2.95 (0.34, 6.23), 5.59 (1.23, 9.95), 11.16 (−6.8, 29.2), 2.1 (0.52, 3.67), 4.18 (−1.49, 9.84), 7.19 (1.19, 13,19), 5.25 (−3.99, 14.5), 4.14 (−0.03, 8.31), 2.2 (0.65, 3.75), 9.9 (−10.2, 29.95), 7.77 (−0.51, 16.1), 7.9 (−2.88, 18.68) | 3.57 (2.33, 4.81) | 17% | 0.00 | 0.0009 |
| Fruit intake during pregnancy | Asres, Tilahun et al., 2023 57 , Belayhun, Kassa et al., 2021 64 , Endeshaw, Abebe et al., 2016 71 , Kahsay, Gashe et al., 2018 83 , Kidane, Eshete et al., 2022 86 , Mekie, Mekonnen et al., 2020 | 0.36 (0.09, 0.63), 0.23 (−0.14, 0.59), 0.51 (0.20, 0.82), 5.1 (0.72, 9.47), 0.36 (0.03, 0.69), 0.45 (0.14, 0.77) | 0.39 (0.24, 0.55) | 16.39% | 0.00 | 0.0522 |
| Having multiple pregnancy | Andarge, Anshebo et al., 2020 53 , Asres, Daga et al., 2022 56 , Asres, Tilahun et al.,2023 57 , Belay and Wudad, 2019 63 , Endeshaw, Abebe et al., 2016 71 , Kidane, Eshete et al., 2022 86 , Wodajo, 2016 100 | 1.72 (0.39, 3.05), 6.33 (−1.28, 13.9), 2.75 (0.20, 5.30), 0.07 (−0.31, 0.45), 4.05 (−1.3, 9.40), 3.69 (−0.03, 7.41), 3.37 (−1.26, 8.00) | 2.06 (0.53, 3.58) | 67.48% | 0.01 | <0.0001 |
| Having history of preeclampsia | Andarge, Anshebo et al., 2020 53 , Beketie, Tafese et al., 2022 62 , Figa, Temesgen et al., 2021 72 , Kibret, Chojenta et al., 2020 85 , Jiregna, Assefa et al., 2023 88 , Tesfa, Munshea et al., 2023 93 , Tesfahun, Tadesse et al., 2023 94 , Yesuf, 2018 | 8.9 (1.11, 16.68), 10.11 (−0.47, 20), 6.42 (−3.12, 15.9), 27.58 (−54.1, 109), 2.42 (0.48, 4.36), 7.97 (−4.14, 20.1), 8.5 (3.95, 13.05), 3.85 (−1.8, 9.5) | 5.48 (2.77, 8.18) | 30.63% | 0.00 | 0.0158 |
| Having history of chronic HTN | Ayele and Tilahun, 2022 31 , Getahun, Benti et al., 2022 75 , Tessema, Tekeste et al., 2022 76 , Kidane, Eshete et al., 2022 86 , Jiregna, Assefa et al., 2023 88 , Yesuf, 2018 101 | 2.93 (0.33 5.53), 3.26 (−0.69, 7.21), 4.3 (−1.99, 10.59), 3.76 (0.41, 7.11), 4.54 (1.04, 8.04), 4.84 (−6.1, 15.78) | 3.6 (2.05, 5.14) | 0.00% | 0.00 | 0.6537 |
| Having history of gestational DM | Andarge, Anshebo et al., 2020 53 , Ayalew, Bantie et al., 2019 60 , Belay and Wudad, 2019 63 , Endeshaw, Abebe et al., 2016 71 , Getahun, Benti et al., 2022 75 , Kahsay, Gashe et al., 2018 83 , Kidane, Eshete et al., 2022 86 | 5.8 (−2.26, 13.86), 11.41 (−33.8, 56), 0.06 (−0.17, 0.29), 6.17 (−3.08, 15.4), 7.35 (−6.76, 21.4), 5.4 (−7.55, 18.35), 3.12 (−1.19, 7.43) | 1.72 (0.52, 3.97) | 19.54% | 0.28 | 0.0094 |
CI: confidence interval; OR: odds ratio; POR: pooled odds ratio; Bold: p-value < 0.05; I2 > 50% heterogeneity and Egger test for publication bias.
Adverse fetomaternal outcome among pregnant women with HDP in Ethiopia
In this systematic review of included studies, 19 of them reported different adverse fetomaternal outcomes among pregnant women with HDP. The most common adverse fetal outcomes were low birth weight, preterm birth, and fifth-min low Apgar score. The dominant adverse maternal outcome was eclampsia, hemolysis, elevated liver enzymes and low platelets (HELP) syndrome, acute kidney injury pulmonary edema, and disseminated intravascular coagulation (DIC) (Table 1).
Discussion
According to the results of this meta-analysis, the pooled prevalence of HDP in Ethiopia was estimated to be 8%, which is higher than a systematic review and meta-analysis published in 2018 which included 13 primary studies that pooled the prevalence of HDP in Ethiopia that was 6.07%, 38 similarly, other review published in 2020 which included 22 primary studies reported the pooled prevalence of HDP in Ethiopia was 6.82%. 37
Regional variation in HDP was observed, and the highest prevalence of HDP (17%) was reported in a study done in Harari Region. The lowest prevalence of HDP (3%) was observed in the Tigray Region. These regional variations may result from variations in lifestyle, educational attainment, and use of MCH services.
In addition, most of the studies included in this meta-analysis were conducted in the Amhara Region which shows that the prevalence of HDP was 9% with a high source of heterogeneity between studies.
The finding of this meta-analysis also showed the risk of HDP increased with increasing age. Women aged > 35 years old were 2.43 times more likely to develop HDP than women aged < 35 years old during their pregnancy. This finding is consistent with results reported from similar studies in Ethiopia, Kenya, Asia, China, and Latin America, women aged > 35 years were having a risk of developing HDP than women aged < 35 years during their pregnancy.37,102–105 This is due to the fact that there is a higher risk of cardiovascular problems in this age group compared to younger women.104,106
In this meta-analysis, women who have had a previous history of preeclampsia were five times more vulnerable to develop HDP as compared with those women who have no previous history of preeclampsia. This was consistent with the findings reported from the study conducted in Ethiopia and China.37,102
Similarly, having a family history of HTN and a family history of DM could also increase the risk of developing HDP compared with their counterparts. These findings are in line with the studies conducted in Ethiopia, China, Swedish Medical Center, and US hospitals.37,102,107,108
Limitation of the study
There is geographical and selection bias, which means there was an underrepresentation of certain areas and the included or selected studies may not be representative. Also, there was high heterogeneity reported in this review, which is reported from the result of pooled estimates of the prevalence of hypertensive disorder in pregnancy. Even if meta-regression was computed to explore sources of heterogeneity, the conclusions drawn from highly heterogeneous studies are less generalizable, specifically for the eastern part of Ethiopia because there were a low number of articles included or found from the eastern part of Ethiopia. The underrepresentation of studies from the eastern part of Ethiopia means that the pooled estimates may not accurately reflect the prevalence of hypertensive disorders in pregnancy in this region.
Conclusion and recommendation
Conclusion
This systematic review and meta-analysis revealed that the level of prevalence of HDP in Ethiopia is increasing. Having a history of kidney disease, having a family history of HTN, having a history of preeclampsia, and having a history of chronic HTN, were found to have a strong association with HDP factors.
The most common adverse fetal outcomes were low birth weight, preterm birth, and a fifth-min low APGAR score. The dominant adverse maternal outcomes were eclampsia, HELP syndrome, acute kidney injury pulmonary edema, and DIC.
In the eastern part of Ethiopia, this condition was not well studied when compared to other areas, this is a high gap. There is a lack of articles conducted at the community level, and those published studies missed some very important variables that need attention or focus such as maternal mental health status, quality of life, and some specific modifiable socioeconomic variables. The majority of the studies that failed to pass quality assessment were those published in low-quality journals.
Recommendation
The finding of this review suggests the need to strengthen the existing strategies for prevention, effective intervention, and developing policy to decrease the burden and adverse birth outcome of hypertensive disorder of pregnancy by working on identified risk factors with a collaboration of nongovernmental organizations, and other stakeholders.
The study recommends enhanced screening and monitoring for hypertensive disorders in pregnancy, particularly among high-risk groups such as kidney disease, overweight individuals, and multiple pregnancies. Rural healthcare providers should be vigilant in HDP monitoring. Increased fruit intake during pregnancy can protect against HDP, and nutritional counselling should be incorporated into prenatal care programs. Encourage further research in underrepresented regions, particularly the eastern part of Ethiopia, to gain a more comprehensive understanding of HDP prevalence and risk factors. Support longitudinal studies to track the long-term outcomes of HDP on maternal and child health, which can inform future healthcare strategies and interventions.
In addition, the Ethiopian Ministry of Health should develop and disseminate educational materials, particularly on health Information dissemination about the importance of a balanced diet during pregnancy, with a focus on the benefits of fruit intake, the importance of preconception care, antenatal care (ANC), and early detection and management of HTN during pregnancy to reduce the unwanted or negative impact of hypertensive disorder of pregnancy on the health of the mother and her child.
Supplemental Material
Supplemental material, sj-docx-1-smo-10.1177_20503121241274741 for Burden, risk factors, and maternal postpartum and birth outcomes of hypertensive disorder of pregnancy in Ethiopia, 2024: A systematic review and meta-analysis by Astawus Alemayehu, Abebaw Demissie, Ibsa Ibrahim, Addisalem Geremew, Feysal Mohammed, Mogos Gudeta, Lamessa Oljira, Yadeta Dessie and Nega Assefa in SAGE Open Medicine
Supplemental material, sj-docx-2-smo-10.1177_20503121241274741 for Burden, risk factors, and maternal postpartum and birth outcomes of hypertensive disorder of pregnancy in Ethiopia, 2024: A systematic review and meta-analysis by Astawus Alemayehu, Abebaw Demissie, Ibsa Ibrahim, Addisalem Geremew, Feysal Mohammed, Mogos Gudeta, Lamessa Oljira, Yadeta Dessie and Nega Assefa in SAGE Open Medicine
Supplemental material, sj-docx-3-smo-10.1177_20503121241274741 for Burden, risk factors, and maternal postpartum and birth outcomes of hypertensive disorder of pregnancy in Ethiopia, 2024: A systematic review and meta-analysis by Astawus Alemayehu, Abebaw Demissie, Ibsa Ibrahim, Addisalem Geremew, Feysal Mohammed, Mogos Gudeta, Lamessa Oljira, Yadeta Dessie and Nega Assefa in SAGE Open Medicine
Acknowledgments
First of all, we would like to express our thanks to the almighty God. We would also like to extend our gratitude to Haramaya University, College of Health and Medical Science for giving us this chance to conduct this study. Finally, we thank Mr. Merga Hirko for editing the language and grammatical flow.
Footnotes
Author contribution: All authors contributed significant work to this review: AA, NA, and LO participated in the study from inception to design, acquisition of data, analysis, and interpretation of the results. AA, AD, NA, YD, LO, AG, MG, II, and FM participated in the methods, analysis, interpretation, and writing of the manuscript of the results. Finally, all authors approved the manuscript for publication and the journal to which it has been submitted.
Availability of data and materials: At any time, the corresponding author provides an additional resource on request.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics approval and consent to participate: Not applicable.
Consent for publication: Not applicable.
ORCID iDs: Astawus Alemayehu  https://orcid.org/0000-0003-1384-7123
https://orcid.org/0000-0003-1384-7123
Mogos Gudeta  https://orcid.org/0000-0002-0804-2569
https://orcid.org/0000-0002-0804-2569
Nega Assefa  https://orcid.org/0000-0003-0341-2329
https://orcid.org/0000-0003-0341-2329
Supplemental material: Supplemental material for this article is available online.
Reference
- 1. Welfare AIoHa. National maternity data development project: hypertensive disorders. Research brief 2016; 4. [Google Scholar]
- 2. Brown MA, Magee LA, Kenny LC, et al. Hypertensive disorders of pregnancy. Hypertension 2018; 72: 24–43. [DOI] [PubMed] [Google Scholar]
- 3. American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics. ACOG practice bulletin no. 203: Chronic hypertension in pregnancy. Obstet Gynecol 2019; 133: e26–e50. [DOI] [PubMed] [Google Scholar]
- 4. Poon LC, Shennan A, Hyett JA, et al. The International Federation of Gynecology and Obstetrics (FIGO) initiative on pre-eclampsia: a pragmatic guide for first-trimester screening and prevention. Int J Gynecol Obstetr 2019; 145: 1–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Roberts JM, August PA, Bakris G, et al. Hypertension in pregnancy. Report of the American college of obstetricians and gynecologists’ task force on hypertension in pregnancy. Obstet Gynecol 2013; 122: 1122–1131. [DOI] [PubMed] [Google Scholar]
- 6. Mammaro A, Carrara S, Cavaliere A, et al. Hypertensive disorders of pregnancy. J Prenat Med 2009; 3: 1–5. [PMC free article] [PubMed] [Google Scholar]
- 7. Zareian Z. Hypertensive disorders of pregnancy. Int J Gynecol Obstetr 2004; 87: 194–198. [DOI] [PubMed] [Google Scholar]
- 8. Say L, Chou D, Gemmill A, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health 2014; 2: e323–333. [DOI] [PubMed] [Google Scholar]
- 9. ACOG. Hypertension in pregnancy. Report of the American college of obstetricians and gynecologists’ task force on hypertension in pregnancy. Obstet Gynecol 2013; 122: 1122–1131. [DOI] [PubMed] [Google Scholar]
- 10. Committee on Practice Bulletins-Obstetrics. Practice bulletin no. 183: postpartum hemorrhage. Obstet Gynecol 2017; 130: e168–e186. [DOI] [PubMed] [Google Scholar]
- 11. UNICEF. One small step in technology, one giant leap for mothers, https://www.unicef.org/supply/stories/one-small-step-technology-one-giant-leap-mothers (2020, accessed 9 August 2022).
- 12. UNICEF. Maternal mortality, https://data.unicef.org/topic/maternal-health/maternal-mortality/ (2021, accessed 09 August 2022).
- 13. Garovic VD, White WM, Vaughan L, et al. Incidence and long-term outcomes of hypertensive disorders of pregnancy. J Am College Cardiol 2020; 75: 2323–2334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Khan KS, Wojdyla D, Say L, et al. WHO analysis of causes of maternal death: a systematic review. Lancet 2006; 367: 1066–1074. [DOI] [PubMed] [Google Scholar]
- 15. Lawn JE, Blencowe H, Waiswa P, et al. Stillbirths: rates, risk factors, and acceleration towards 2030. Lancet 2016; 387: 587–603. [DOI] [PubMed] [Google Scholar]
- 16. Backes CH, Markham K, Moorehead P, et al. Maternal preeclampsia and neonatal outcomes. J Pregnancy 2011; 2011: 214365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pinar H, Goldenberg RL, Koch MA, et al. Placental findings in singleton stillbirths. Obstetr Gynecol 2014; 123: 325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ukah UV, De Silva DA, Payne B, et al. Prediction of adverse maternal outcomes from pre-eclampsia and other hypertensive disorders of pregnancy: a systematic review. Pregnancy Hypertens 2018; 11: 115–123. [DOI] [PubMed] [Google Scholar]
- 19. Chappell LC, Bramham K, Shennan AH. Short-term prediction of preeclampsia: how close are we? Biomark Med 2014; 8: 455–458. [DOI] [PubMed] [Google Scholar]
- 20. Abalos E, Cuesta C, Grosso AL, et al. Global and regional estimates of preeclampsia and eclampsia: a systematic review. Eur J Obstetr Gynecol Reprodu Biol 2013; 170: 1–7. [DOI] [PubMed] [Google Scholar]
- 21. Wang W, Xie X, Yuan T, et al. Epidemiological trends of maternal hypertensive disorders of pregnancy at the global, regional, and national levels: a population-based study. BMC Pregnancy Childbirth 2021; 21: 364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Musarandega R, Nyakura M, Machekano R, et al. Causes of maternal mortality in Sub-Saharan Africa: a systematic review of studies published from 2015 to 2020. J Glob Health 2021; 11: 04048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Central Statistical Agency—CSA/Ethiopia and ICF. Ethiopia demographic and health survey 2016. Addis Ababa, Ethiopia: CSA and ICF, 2017. [Google Scholar]
- 24. Mersha AG, Abegaz TM, Seid MA. Maternal and perinatal outcomes of hypertensive disorders of pregnancy in Ethiopia: systematic review and meta-analysis. BMC Pregnancy Childbirth 2019; 19: 458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mekonnen W, Gebremariam A. Causes of maternal death in Ethiopia between 1990 and 2016: systematic review with meta-analysis. Ethiop J Health Develop 2018; 32(4). [Google Scholar]
- 26. Tessema GA, Laurence CO, Melaku YA, et al. Trends and causes of maternal mortality in Ethiopia during 1990–2013: findings from the global burden of diseases study 2013. BMC Public Health 2017; 17: 160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Legesse T, Abdulahi M, Dirar A. Trends and causes of maternal mortality in Jimma University Specialized Hospital, southwest Ethiopia: a matched case-control study. Int J Womens Health 2017; 9: 307–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Tesfaye G, Loxton D, Chojenta C, et al. Magnitude, trends and causes of maternal mortality among reproductive aged women in Kersa health and demographic surveillance system, eastern Ethiopia. BMC Womens Health 2018; 18: 198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Shiferaw MA, Bekele D, Surur F, et al. Maternal death review at a tertiary hospital in Ethiopia. Ethiop J Health Sci 2021; 31: 35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Belay AS, Wudad T. Prevalence and associated factors of pre-eclampsia among pregnant women attending anti-natal care at Mettu Karl referal hospital, Ethiopia: cross-sectional study. Clin Hypertens 2019; 25: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ayele AD, Tilahun ZA. Magnitude of preeclampsia and associated factors among women attending delivery service in Debre Tabor Specialized Hospital. Ethiop J Health Sci 2022; 32: 279–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Walle TA, Azagew AW. Hypertensive disorder of pregnancy prevalence and associated factors among pregnant women attending ante natal care at Gondar town health institutions, North West Ethiopia 2017. Pregnancy Hypertens 2019; 16: 79–84. [DOI] [PubMed] [Google Scholar]
- 33. Mekonen L, Shiferaw Z, Wubshet E, et al. Pregnancy induced hypertension and associated factors among pregnant women in Karamara Hospital, Jijiga, Eastern Ethiopia, 2015. J Pregnancy Child Health 2018; 5: 1–4. [Google Scholar]
- 34. Firisa W, Onsongo L, Mugo J. Prevalence of hypertensive disorders among pregnant women attending antenatal care in selected public hospitals in Addis Ababa, Ethiopia. J Health Med Nurs 2021; 7: 19–44. [Google Scholar]
- 35. Mengistu MD, Kuma T. Feto-maternal outcomes of hypertensive disorders of pregnancy in Yekatit-12 Teaching Hospital, Addis Ababa: a retrospective study. BMC Cardiovasc Disord 2020; 20: 173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gemechu KS, Assefa N, Mengistie B. Prevalence of hypertensive disorders of pregnancy and pregnancy outcomes in Sub-Saharan Africa: a systematic review and meta-analysis. Womens Health (Lond) 2020; 16: 1745506520973105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Tesfa E, Nibret E, Gizaw ST, et al. Prevalence and determinants of hypertensive disorders of pregnancy in Ethiopia: a systematic review and meta-analysis. PLoS One 2020; 15: e0239048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Berhe AK, Kassa GM, Fekadu GA, et al. Prevalence of hypertensive disorders of pregnancy in Ethiopia: a systemic review and meta-analysis. BMC Pregnancy Childbirth 2018; 18: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Shey Wiysonge CU, Ngu Blackett K, Mbuagbaw JN. Risk factors and complications of hypertension in Yaounde, Cameroon. Cardiovasc J S Afr 2004; 15: 215–219. [PubMed] [Google Scholar]
- 40. Pridjian G, Puschett JB. Preeclampsia. Part 1: clinical and pathophysiologic considerations. Obstet Gynecol Surv 2002; 57: 598–618. [DOI] [PubMed] [Google Scholar]
- 41. Leeners B, Rath W, Kuse S, et al. BMI: new aspects of a classical risk factor for hypertensive disorders in pregnancy. Clin Sci (Lond) 2006; 111: 81–86. [DOI] [PubMed] [Google Scholar]
- 42. Hinkosa L, Tamene A, Gebeyehu N. Risk factors associated with hypertensive disorders in pregnancy in Nekemte referral hospital, from July 2015 to June 2017, Ethiopia: case-control study. BMC Pregnancy Childbirth 2020; 20: 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kidane R, Eshete T, Sintayehu T, et al. Dietary patterns and hypertensive disorders among pregnant women attending antenatal and delivery care in public hospitals of Jimma Zone, Southwest Ethiopia. J Multidiscip Healthc 2022; 15: 1645–1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Liu L, Oza S, Hogan D, et al. Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet 2016; 388: 3027–3035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. FMOH. Health Sector Transformation Plan II (HSTP II) 2020/21–2024/25. FMOH, 2021. [Google Scholar]
- 46. Walle TA, Azagew AW. Hypertensive disorder of pregnancy prevalence and associated factors among pregnant women attending ante natal care at Gondar town health Institutions, North West Ethiopia 2017. Pregnancy Hypertens 2019; 16: 79–84. [DOI] [PubMed] [Google Scholar]
- 47. Gudeta TA, Regassa TM. Pregnancy induced hypertension and associated factors among women attending delivery service at Mizan-Tepi University Teaching Hospital, Tepi General Hospital and Gebretsadik Shawo Hospital, Southwest, Ethiopia. Ethiop J Health Sci 2019; 29: 831–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Belayhun Y, Kassa Y, Mekonnen N, et al. Determinants of pregnancy-induced hypertension among mothers attending public hospitals in Wolaita Zone, South Ethiopia: findings from unmatched case-control study. Int J Hypertens 2021; 2021: 6947499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Munn Z, Moola S, Lisy K, et al. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc 2015; 13: 147–153. [DOI] [PubMed] [Google Scholar]
- 50. Porritt K, Gomersall J, Lockwood C. JBI’s systematic reviews: study selection and critical appraisal. Am J Nurs 2014; 114: 47–52. [DOI] [PubMed] [Google Scholar]
- 51. Munn Z, Stone JC, Aromataris E, et al. Assessing the risk of bias of quantitative analytical studies: introducing the vision for critical appraisal within JBI systematic reviews. JBI Evid Synth 2023; 21: 467–471. [DOI] [PubMed] [Google Scholar]
- 52. Amare M, Olani A, Hassen H, et al. Perinatal outcomes and associated factors among women with hypertensive disorders of pregnancy delivered in Jimma Zone Hospitals, Southwest Ethiopia. Ethiop J Health Sci 2021; 31: 1145–1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Andarge RB, Anshebo AA, Halil HM, et al. Prevalence and associated factors of pre-eclampsia among pregnant women at antenatal booking in the Halaba Kullito General Hospital, Southern Ethiopia. J Womens Health Care 2020; 9: 2167-0420.2120. [Google Scholar]
- 54. Asefa F, Hunde A, Siraneh Y. Outcome of hypertensive disorders of pregnancy and associated factors among pregnant women admitted to Jimma University Medical Center, Southwest Ethiopia. Ethiop J Reprod Health 2020; 12: 12. [Google Scholar]
- 55. Asfaw M. Severe preeclampsia: effect of timing of termination of pregnancy on maternal and perinatal outcome, Addis Ababa University. http://thesisbank.jhia.ac.ke/ideprint/6996 (2014, accessed 24 October 2018). [Google Scholar]
- 56. Asres AW, Daga WB, Samuel S, et al. Determinants of preeclampsia among pregnant women in public hospitals of Wolaita and Dawuro Zones, Southern Ethiopia: a case-control study. Womens Health Rep 2022; 3: 964–970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Asres AW, Tilahun AW, Addissie A. Factors associated with preeclampsia among pregnant women in Gojjam zones, Amhara region, Ethiopia: a case-control study. Blood Pressure 2023; 32: 2255687. [DOI] [PubMed] [Google Scholar]
- 58. Asres AW, Tilahun AW, Teklu S, et al. Association between preeclampsia and hormonal contraceptive use among pregnant women in Northwest Ethiopia: a case-control study. J Womens Healthcare Midwifery Res SRC/JWHMR-116 2023; 2: 2–6. [Google Scholar]
- 59. Asseffa NA, Demissie BW. Perinatal outcomes of hypertensive disorders in pregnancy at a referral hospital, Southern Ethiopia. PLoS One 2019; 14: e0213240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Ayalew AF, Bantie GM, Kassa TB, et al. Prevalence of pre-eclampsia and associated factors among women attending antenatal care services in Felege-Hiwot referral hospital, Bahir Dar city, Northwest Ethiopia, 2019, 10.21203/rs.2.11607/v1 [DOI]
- 61. Melese MF, Aynalem GL, Badi MB. Factors Associated With Unfavourable Maternal Outcomes of Severe Preeclampsia/Eclampsia, North West Ethiopian Context, 2018. Clinics Mother Child Health S 2021; 10. [Google Scholar]
- 62. Beketie ED, Tafese WT, Shiferaw BZ, et al. Determinants of preeclampsia among mothers attending perinatal care in Gurage zone public hospitals, Ethiopia, matched case control study. Int J Afr Nurs Sci 2022; 17: 100453. [Google Scholar]
- 63. Belay AS, Wudad T. Prevalence and associated factors of pre-eclampsia among pregnant women attending anti-natal care at Mettu Karl Referral hospital, Ethiopia: cross-sectional study. Clin Hypertens 2019; 25: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Belayhun Y, Kassa Y, Mekonnen N, et al. Determinants of pregnancy-induced hypertension among mothers attending public hospitals in wolaita zone, south Ethiopia: findings from unmatched case-control study. Int J Hypertens 2021; 2021: 6947499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Berhan Y, Endeshaw G. Maternal mortality predictors in women with hypertensive disorders of pregnancy: a retrospective cohort study. Ethiop J Health Sci 2015; 25: 89–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Berhe AK, Ilesanmi AO, Aimakhu CO, et al. Effect of pregnancy induced hypertension on adverse perinatal outcomes in Tigray regional state, Ethiopia: a prospective cohort study. BMC Pregnancy Childbirth 2020; 20: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Birhanu MY, Temesgen H, Demeke G, et al. Incidence and predictors of pre-eclampsia among pregnant women attending antenatal care at debre markos referral hospital, North West Ethiopia: prospective cohort study. Int J Womens Health 2020; 12: 1013–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Chemeda WC, Gurmesa TS, Gedefa AG, et al. Factors associated with hypertensive disorders among pregnant mothers attending antenatal care services at public health facilities in Gambella Town, Southwest Ethiopia: Cross-sectional study. Int J Afr Nurs Sci 2022; 17: 100478. [Google Scholar]
- 69. Endeshaw G, Berhan Y. Perinatal outcome in women with hypertensive disorders of pregnancy: a retrospective cohort study. Int Sch Res Notices 2015; 2015: 208043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Endeshaw M, Abebe F, Bedimo M, et al. Diet and pre-eclampsia: a prospective multicenter case-control study in Ethiopia. Midwifery 2015; 31: 617–624. [DOI] [PubMed] [Google Scholar]
- 71. Endeshaw M, Abebe F, Bedimo M, et al. Family history of hypertension increases risk of preeclampsia in pregnant women: a case-control study. Universa Medicina 2016; 35: 181–191. [Google Scholar]
- 72. Figa Z, Temesgen T, Belekle E, et al. Assessment of maternal outcome among preeclamptic women at Dilla University Referral Hospital, Dilla Ethiopia. Int J Biomed Eng Clin Sci 2021; 7: 65. [Google Scholar]
- 73. Fikadu K, G/Meskel F, Getahun F, et al. Determinants of pre-eclampsia among pregnant women attending perinatal care in hospitals of the Omo district, Southern Ethiopia. J Clin Hypertens Greenwich Conn 2021; 23: 153–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Gaym A, Bailey P, Pearson L, et al. Disease burden due to pre-eclampsia/eclampsia and the Ethiopian health system’s response. Int J Gynecol Obstetr 2011; 115: 112–116. [DOI] [PubMed] [Google Scholar]
- 75. Getahun GK, Benti Y, Woldekidan F, et al. Prevalence of pregnancy-induced hypertension and associated factors among women receiving antenatal care in Addis Ababa, Ethiopia, 2022. Biomed J Scie & Tech Res (BJSTR) 2023; 48: 007587. DOI: 10.26717/BJSTR.2023.48.007587 [Google Scholar]
- 76. Tessema GA, Tekeste A, Ayele TA. Preeclampsia and associated factors among pregnant women attending antenatal care in Dessie referral hospital, Northeast Ethiopia: a hospital-based study. BMC Pregnancy Childbirth 2015; 15: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Godana A, Dessalegn D, Adem F, et al. Treatment outcomes and determinants of eclampsia and severe preeclampsia among pregnant women admitted to selected tertiary hospitals in Ethiopia: a cohort study. Int J Womens Health 2021; 13: 781–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Gudeta TA, Regassa TM. Pregnancy induced hypertension and associated factors among women attending delivery service at Mizan-Tepi University Teaching Hospital, Tepi General Hospital and Gebretsadik Shawo Hospital, southwest, Ethiopia. Ethiop J Health Sci 2019; 29: 831–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Jaleta DD, Gebremedhin T, Jebena MG. Perinatal outcomes of women with hypertensive disorders of pregnancy in Jimma Medical Center, southwest Ethiopia: retrospective cohort study. PLoS One 2021; 16: e0256520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Jikamo B, Adefris M, Azale T, et al. Risk factors for preeclampsia and eclampsia in Sidama region, southern Ethiopia: a nested case-control study. Pan Afr Med JOne Health 2022; 9: 1–17. [Google Scholar]
- 81. Jikamo B, Adefris M, Azale T, et al. The effect of preeclampsia on adverse maternal outcomes in Sidama region, Ethiopia: a prospective open cohort study. Scient Rep 2022; 12: 19300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Jikamo B, Adefris M, Azale T, et al. Incidence of adverse perinatal outcomes and risk factors among women with pre-eclampsia, southern Ethiopia: a prospective open cohort study. BMJ Paediatr Open 2022; 6: e001567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Kahsay HB, Gashe FE, Ayele WM. Risk factors for hypertensive disorders of pregnancy among mothers in Tigray region, Ethiopia: matched case-control study. BMC Pregnancy Childbirth 2018; 18: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Kahsay HB, Gashe FE, Ayele WM. Patterns of hypertensive disorders of pregnancy in selected hospitals of Tigray, Ethiopia. J Adv Med Med Res 2018; 27: 1–14. [Google Scholar]
- 85. Kibret KT, Chojenta C, D’Arcy E, et al. The effect of dietary patterns on hypertensive disorders of pregnancy in North Shewa, Ethiopia: a propensity score matched case-control study. Pregnancy Hypertens 2020; 22: 24–29. [DOI] [PubMed] [Google Scholar]
- 86. Kidane R, Eshete T, Sintayehu T, et al. Dietary patterns and hypertensive disorders among pregnant women attending antenatal and delivery care in public hospitals of Jimma Zone, Southwest Ethiopia. J Multidiscipl Healthcare 2022; 15: 1645–1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Legesse AY, Berhe Y, Mohammednur SA, et al. Prevalence and determinants of maternal and perinatal outcome of preeclampsia at a tertiary hospital in Ethiopia. Ethiop J Reprod Health 2019; 11: 8. [Google Scholar]
- 88. Jiregna A, Assefa N, Kenay A. Magnitude and factors associated with preeclampsia among pregnant women admitted in hiwot fana comprehensive specialized university hospital, eastern Ethiopia: a retrospective study. Eur J Midwifery 2023; 6: 49. [Google Scholar]
- 89. Mekie M, Mekonnen W, Assegid M. Cohabitation duration, obstetric, behavioral and nutritional factors predict preeclampsia among nulliparous women in West Amhara Zones of Ethiopia: age matched case control study. PLoS One 2020; 15: e0228127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Melese MF, Badi MB, Aynalem GL. Perinatal outcomes of severe preeclampsia/eclampsia and associated factors among mothers admitted in Amhara Region referral hospitals, North West Ethiopia, 2018. BMC Res Notes 2019; 12: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Sium AF, Lucero-Prisno DE, III, Gudu W. Perinatal outcomes of twin pregnancies complicated with preeclampsia at a tertiary hospital in Ethiopia: a case-control study. Public Health Chall 2022; 1: e37. [Google Scholar]
- 92. Syoum FH, Abreha GF, Teklemichael DM, et al. Fetomaternal outcomes and associated factors among mothers with hypertensive disorders of pregnancy in Suhul Hospital, Northwest Tigray, Ethiopia. J Pregnancy 2022; 2022: 6917009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Tesfa E, Munshea A, Nibret E, et al. Determinants of pre-eclampsia among pregnant women attending antenatal care and delivery services at Bahir Dar public hospitals, northwest Ethiopia: a case-control study. Health Sci Rep 2023; 6: e1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Tesfahun E, Tadesse S, Hailu A, et al. Prevalence of preeclampsia and associated factors among antenatal care attending mothers at Tirunesh Beijing General Hospital, Addis Ababa, Ethiopia. Adv Public Health 2023; 2023: 1132497. [Google Scholar]
- 95. Tesfaye A, Tefera B, Sena B. Pregnancy induced hypertension and associated factors among pregnant women receiving antenatal care service at Jimma town public health facilities, south west Ethiopia. Gynecol Womens Health 2018; 10: 555792. [Google Scholar]
- 96. Tlaye KG, Endalifer ML, Getu MA, et al. A five-year trend in pre-eclampsia admission and factors associated with inpatient eclampsia: a retrospective study from a resource-limited hospital in northeast Ethiopia. BMJ open 2021; 11: e040594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Wassie AY, Anmut W. Prevalence of eclampsia and its maternal-fetal outcomes at Gandhi Memorial Hospital, Addis Ababa Ethiopia, 2019: retrospective study. Int J Womens Health 2021; 13: 231–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Obsa MS, Wolka E. Maternal outcome of pregnant mothers with hypertensive disorder of pregnancy at hospitals in Wolaita Zone, Southern Ethiopia. J Pregnancy Child Health 2018; 4: 4–9. [Google Scholar]
- 99. Welesemayat ET, Taye G, Seid Y, et al. Effect of preeclampsia on the incidence rate of small-for-gestational-age of the fetuses among pregnant women in selected public hospitals in Tigray, Northern Ethiopia. Ethiop J Health Develop 2020; 34(3). [Google Scholar]
- 100. Wodajo S. Hypertensive disorders of pregnancy and associated factors among admitted pregnant cases in Dessie town referral hospital, North East Ethiopia, 2015. Medico Res Chron 2016; 3: 297–306. [Google Scholar]
- 101. Yesuf M. Magnitude of preeclampsia and associated factors among pregnant women in Yirgalem General Hospital Southern Ethiopia, (Doctoral dissertation, HU), 2018. [Google Scholar]
- 102. Ye C, Ruan Y, Zou L, et al. The 2011 survey on hypertensive disorders of pregnancy (HDP) in China: prevalence, risk factors, complications, pregnancy and perinatal outcomes. PLoS One 2014; 9: e100180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Conde-Agudelo A, Belizán JM. Maternal morbidity and mortality associated with interpregnancy interval: cross sectional study. BMJ 2000; 321: 1255–1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Conde-Agudelo A, Belizán JM. Risk factors for pre-eclampsia in a large cohort of Latin American and Caribbean women. BJOG Int J Obstetr Gynaecol 2000; 107: 75–83. [DOI] [PubMed] [Google Scholar]
- 105. Logan G, Njoroge P, Nyabola L, et al. Determinants of preeclampsia and eclampsia among women delivering in county hospitals in Nairobi, Kenya. F1000Research 2020; 9: 192. [Google Scholar]
- 106. Umesawa M, Kobashi G. Epidemiology of hypertensive disorders in pregnancy: prevalence, risk factors, predictors and prognosis. Hypertens Res 2017; 40: 213–220. [DOI] [PubMed] [Google Scholar]
- 107. Qiu C, Williams MA, Leisenring WM, et al. Family history of hypertension and type 2 diabetes in relation to preeclampsia risk. Hypertension 2003; 41: 408–413. [DOI] [PubMed] [Google Scholar]
- 108. Zhang Z, Corke H. Trypsin inhibitor activity in vegetative tissue of sweet potato plants and its response to heat treatment. J Sci Food Agri 2001; 81: 1358–1363. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-smo-10.1177_20503121241274741 for Burden, risk factors, and maternal postpartum and birth outcomes of hypertensive disorder of pregnancy in Ethiopia, 2024: A systematic review and meta-analysis by Astawus Alemayehu, Abebaw Demissie, Ibsa Ibrahim, Addisalem Geremew, Feysal Mohammed, Mogos Gudeta, Lamessa Oljira, Yadeta Dessie and Nega Assefa in SAGE Open Medicine
Supplemental material, sj-docx-2-smo-10.1177_20503121241274741 for Burden, risk factors, and maternal postpartum and birth outcomes of hypertensive disorder of pregnancy in Ethiopia, 2024: A systematic review and meta-analysis by Astawus Alemayehu, Abebaw Demissie, Ibsa Ibrahim, Addisalem Geremew, Feysal Mohammed, Mogos Gudeta, Lamessa Oljira, Yadeta Dessie and Nega Assefa in SAGE Open Medicine
Supplemental material, sj-docx-3-smo-10.1177_20503121241274741 for Burden, risk factors, and maternal postpartum and birth outcomes of hypertensive disorder of pregnancy in Ethiopia, 2024: A systematic review and meta-analysis by Astawus Alemayehu, Abebaw Demissie, Ibsa Ibrahim, Addisalem Geremew, Feysal Mohammed, Mogos Gudeta, Lamessa Oljira, Yadeta Dessie and Nega Assefa in SAGE Open Medicine