Abstract
Background
Prostate cancer is among prevalent cancers in men. Numerous strategies have been proposed to intervene with the important prostate cancer-related signaling pathways. Among the most promising strategies is CRISPR/Cas9 strategy. This strategy has been used to modify expression of a number of genes in prostate cancer cells.
Aims
This review summarizes the most recent progresses in the application of CRISPR/Cas9 strategy in modification of prostate cancer-related phenotypes with an especial focus on pathways related to androgen receptor signaling.
Conclusion
CRISPR/Cas9 technology has successfully targeted several genes in the prostate cancer cells. Moreover, the efficiency of this technique in reducing tumor burden has been tested in animal models of prostate cancer. Most of targeted genes have been related with the androgen receptor signaling. Targeted modulation of these genes have affected growth of castration-resistant prostate cancer. PI3K/AKT/mTOR signaling and immune response-related genes have been other targets that have been successfully modulated by CRISPR/Cas9 technology in prostate cancer. Based on the rapid translation of this technology into the clinical application, it is anticipated that novel treatments based on this technique change the outcome of this malignancy in future.
Keywords: Prostate cancer, Androgen receptor, CRISPR/Cas9
Introduction
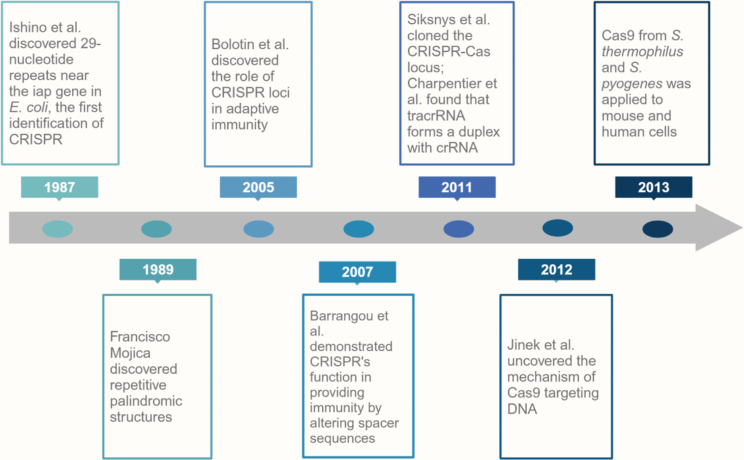
The CRISPR system is an innovative genome editing apparatus that is able to reform the outline of cancer research and treatment. Its capacity to accurately target and edit certain genetic mutations that initiate the growth and spread of cancer cells has offered new prospects for the design of more effective and personalized options for treatment of cancer. Historically, it was discovered in the prokaryotes. In 1987, Ishino et al. made a groundbreaking discovery that revolutionized the medical and biological sciences: the recognition of the prokaryotic immune response mechanism CRISPR (Clustered Regularly Interspaced Short Palindromic Repeats). While conducting their research on the iap enzyme and its role in converting the alkaline phosphatase isozymes in the periplasm of E. coli K-12, they came across a certain set of 29 nucleotide repeats located downstream of the iap gene. These repeats were interspersed with five 32-nucleotide non-repetitive sequences [1–3]. This discovery, sparked intense curiosity and laid the foundations for the subsequent impressive progress in CRISPR research.
In 1989, Francisco Mojica, a researcher from the University of Alicante, discovered an outstanding feature of the CRISPR system. Two years following the discovery of Ishino et al., Mojica discovered a strange structure with a roughly palindromic pattern. This repetitive structure comprised a section of about 30 bases alternating with a spacer of 36 bases [4]. Mojica also observed the same repeats in the intimately associated organism H. volcanii, highlighting the intriguing nature of these sequences. He called these structures Short Regular Spaced Repeats (SRSRs). But as the scientific community investigated their function, they were eventually renamed “clustered regularly interspaced palindromic repeats” (CRISPR) [5].
In 2005, the role of CRISPR loci in adaptive immunity was discovered independently by three groups of researchers: Bolotin et al.; Mojica et al. and Pourcel et al. [6]. Their joint observations revealed an intriguing pattern: the spacer sequences of CRISPR loci were not randomly arranged; instead, they appeared to be originated from phage DNA and conjugative plasmids. This discovery implied that the unique spacer regions actually serve as a kind of immune memory and provide protection against invading phage or plasmid DNA [6].
The theory that CRISPR contributed to the adaptive immunity was additionally confirmed by Barrangou et al. They artificially altered the spacer sequences of the CRISPR clusters of phage-resistant S. thermophiles. By deleting the spacer, the phage-resistant strains converted susceptible to phage infection again, demonstrating that CRISPR loci play a direct role in adaptive immunity [7].
At the same time, Horvath and his team conducted another experiment that provided further evidence for the CRISPR-adapted immune system notion. They integrated the new phage DNA into the CRISPR array and demonstrated effective protection against further phage attacks [8].
These primitive hypotheses provided intriguing clues about the potential mechanism of CRISPR-encoded defense against phage invasion. In addition, the findings of subsequent research showed that the CRISPR/Cas systems incorporate tiny fragments of foreign DNA into the CRISPR locus. In-depth transcriptional analysis of small RNAs revealed that the spacer sequences between CRISPR loci and certain repetitive sequences were transcribed as an elongated transcript and processed into small CRISPR-associated transcripts, named CRISRR RNA (crRNAs) [6].
Subsequently, Siksnys et al. cloned the complete CRISPR-Cas locus from S. thermophiles [9]. Their experiments confirmed the capacity of this system to deliver resistance against foreign plasmids [9]. They also explained how the RuvC domain of Cas9 cuts the non-complimentary DNA strand, while the HNH domain cuts the complementary strand. It was further shown that Cas9 can be trained to target a specific site by altering the crRNA sequence [10]. At the same time, another group found that trans-activating CRISPR RNA (tracrRNA) creates a duplex with crRNA and directs Cas9 to its targets [11]. In 2012, Jinek et al. made a significant scientific contribution with their groundbreaking research [12]. The main focus of their study was on the exact mechanism of Cas9 protein binding to the foreign DNA and its cleavage. They identified the essential components required for the CRISPR/Cas system to operate in genome editing. It turned out that Cas9, the mature crRNA, and the protospacer-adjacent motif (PAM) alone do not trigger the Cas9-mediated cleavage of plasmid DNA. Nevertheless, the inclusion of tracrRNA, a crRNA that attaches to the target DNA, together with magnesium resulted in successful cleavage reactions. Jinek and his colleagues conducted various experiments to understand the function of Cas9 and tracrRNA in the CRISPR/Cas system [12]. After understanding the process, they designed small guide RNAs (sgRNA) that resembled the tracrRNA-crRNA complex, and simplified the process of an adaptable system. Since Cas9 is an RNA-programmed enzyme, it permit targeting and cleavage of certain DNA sequences [12].
In 2013, another major breakthrough was accomplished. In fact, it was development of two orthologs of Cas9 from S. thermophilus and S. pyogenes, which were successfully applied to mouse and human cells [13]. During the same year, another group developed type II bacterial CRISPR/Cas system with modified gRNA in human cells, which opened up new opportunities for CRISPR technology [14].
The CRISPR/Cas9 system has been further modified and adapted for various types of genomic applications, including genome regulation [15]. This development illustrates the power and flexibility of the CRISPR/Cas9 system in a wide diversity of genome-related studies [15]. Figure 1 shows a schematic representation of different milestones in the application of CRISPR/Cas9 technology.
Fig. 1.
Timeline of important events leading to application of CRISPR/Cas9 technology
CRISPR/Cas structures and mechanisms
There are three major types of CRISPR/Cas systems described as Type I (Cas3), Type II (Cas9) and Type III (Cas 10) [16]. Type I Cas genes encode helicases having ATPase activity on single-stranded DNA [17]. Type II Cas genes encode a multiple-domain protein working for the DNA cleavage and crRNA maturation [12]. In combination with Cas9, all CRISPR/Cas systems with Type II genes contain Cas1 and Cas2. Type III CRISPR/Cas genes encode Cas10, a multiple domain protein with palm domain [18]. In addition to Cas10 which is the active unit of this type of systems, other subunits exist in Type III loci, including a subunit that encodes Cas5 groups and numerous RAMP subunits for Cas7 [19]. While Cas9 is helpful for editing purposes, the method of cleavage of Cas3 makes it unsuitable for this purpose. In fact, Cas3 pinpoints its target sequence and starts single stranded DNA degradation in a way that can continue up to multiple kilobases [20]. Finally, Type III effector systems specifically spot and cleave RNA molecules [21].
The CRISPR/Cas systems exist on both chromosomal and plasmid DNA [22]. These systems are a portion of adaptive immune systems evolved by bacteria and archaea to guard themselves against invading phages and are made up of diverse CRISPR and Cas genes. The large Cas effector protein, which has one multidomain per protein, forms a complex with crRNA during the interference process [23].
CRISPRs contain a leader (which is adjacent to the first repeat of the CRISPR loci and is the promoter of CRISPR arrays), short direct repeats (which form hairpin configuration to stabilize the secondary structure of the RNA), and non-repetitive spacers (which capture foreign DNA sequences) [24, 25].
The CRISPR/Cas9 class II systems expressed by bacteria and archaea can hold a small section of the viral gene, a so-called spacer, in to the CRISPR array. When the same virus re-invades the cells, the bacteria can distinguish the virus from the spacer and lyse the virus by cutting its DNA. This process includes three phases, namely adaptation, expression and interference. When the foreign DNA enters the host cell, Cas1 and Cas2 proteins distinguish the PAM in the foreign DNA structure, and afterwards catch the DNA sequence neighboring the PAM as a protospacer [26]. Then, the Cas1/2 protein complex cuts the protospacer from the foreign DNA to make a spacer that is incorporated between two repeat sequences at the 5’ end of the CRRSPR array [27, 28]. At the expression phase, CRISPR array is transcribed to create tracrRNA and crRNA precursor. The latter is trimmed into mature crRNA by the assistance of RNase III nuclease and Cas9. Then, repeats and tracrRNA make a double-stranded RNA (tracrRNA-crRNA) through pairing of complementary bases. This structure accumulates into the effector complex with the nuclease and Cas9 [29]. When the tracrRNA: crRNA duplex is processed, it can direct Cas9 to DNA sequences corresponding to the crRNA guide sequence [30]. In the interference phase, the Cas9 effector protein binds to the guide RNA before target recognition and cleavage. Afterwards, Cas9 protein is directed to the appropriate PAM sequence in a sequence-specific manner [31]. PAMs have a crucial role in the discrimination of self DNA from foreign DNA, since they are present only in the exogenous DNA, preventing the activation of the CRISPR mechanism for self-deletion. In fact, protospacer sequences inserted into the CRISPR locus are not cut since they are not adjacent to a PAM sequence [32].
In brief, pairing of crRNA with the complementary bases on the target strand creates an R-loop configuration that ultimately causes cutting of the target and nontarget strands by Cas9, leading to flat-end cut at three nucleotides upstream of the PAM [33]. This cleavage leads to formation of a double-strand break in the target sequence which in turn triggers two repair mechanisms: (1) non-homologous end joining (NHEJ) and (2) Homology directed repair (HDR). NHEJ pathway is an error-prone repair mechanism that repairs DNA double-strand break by inserting indels, thereby leading to diverse mutations in the open reading frames of the targets region [34, 35]. HDR is an innate DNA repair mechanism, which is triggered by double-strand DNA breaks [36]. This DNA repair mechanism could be used to repair the DNA double-strand breaks mediated by CRISPR [33, 37]. The DNA cleavage induced by sgRNA can be repaired by introducing a donor template into the target cells. The donor DNA harbors the intended insertions or modifications. The insertions are flanked with DNA segments that are homologous to the cleaved DNA. Therefore, the cells HDR mechanism inserts the desired gene into the targeted DNA segment by utilizing the donor template [14, 38].
CRISPR/Cas9 in cancer treatment
Although there has been considerable advancement in cancer treatment in recent decades, the continued mortality rate from this disease demonstrates the critical necessity for novel and more competent therapeutic modalities. CRISPR/Cas9-mediated genome editing is a potent research tool which provides vast promise in cancer therapeutic application, and it has been widely utilized in the research laboratories, due to its high specificity, efficiency, and accuracy, which have facilitated detection of the role of various oncogenes and tumor suppressors in the cancer cells [39–43]. The CRISPR/Cas9 tool has been also exploited to specifically target tumor-suppressors in order to suppress or diminish the tumorigenesis by reestablishing the functions of these genes [44]. It has also been used to recognize the heterogeneity of cancer cells and possible therapeutic targets for diverse cancer cells [45]. This technique has a potential to be used for repair of specific mutations, gene editing, knockdown of specific oncogenes, and engineered T cell immunotherapy [46]. In addition, CRISPR/Cas9 tool was used as a programmable base editing system to telomerase in order to demonstrate that base-editing of TERT rigorously affects cancer cell survival. In fact, haploinsufficiency of TERT resulted in telomere abrasion and growth retardation, showing the potential of TERT inactivation in cancer therapy [47]. The capacity of CRISPR/Cas9 system for editing of oncogenic mutations has also been confirmed [46]. CRISPR/Cas9 has also been applied in the clinical settings. In a phase I clinical trial, CRISPR/Cas9 PD-1-edited T cells were used in patients with advanced lung cancer. Results confirmed the feasibility and safety of this technique [48]. Here, we discuss the novel therapeutic aspects of this technology in the treatment of prostate cancer.
Prostate cancer
Prostate cancer is a very complicated disease with different genetic factors contributing to its pathogenesis [49]. Recent advancements in CRISPR technology offer a novel approach to targeting the specific genes associated with prostate cancer, leading to the development of new therapeutic strategies [50]. We discuss these studies in different sections of this article.
CRISPR-mediated modification of androgen receptor (AR) signaling
Due to the importance of AR in the pathogenesis prostate cancer, different methods were used to modulate this signaling pathway in prostate cancer. At the gene level, small interference RNA was used with great success [51, 52]. In addition, next-generation AR signaling inhibitors, bone-targeting substances, and poly(ADP-ribose) polymerase inhibitors have also been developed for such purpose [53]. CRISPR technology was also used by several groups as a tool for modification of this pathway (Table 1). For instance, Wei et al. employed the CRISPR/Cas method to effectively eliminate the AR gene in androgen- positive prostate cancer cells. Three distinct single sgRNAs were developed to target various regions of the AR gene. The investigators discovered the optimal sgRNA that effectively targeted the AR gene, leading to the inhibition of androgen-sensitive prostate cancer development. The AR sgRNA-guided CRISPR/Cas method induced targeted breaks in the AR gene, leading to cellular apoptosis and inhibition of the cell proliferation. The results showed that the CRISPR/Cas system might be an effective weapon for the treatment of this cancer [54].
Table 1.
CRISPR-mediated modification of AR signaling in prostate cancer
| Target gene | Study type | Cell line | Vector | Screening/verification | Experimental data | Ref |
|---|---|---|---|---|---|---|
| AR | In vitro | LNCaP | Lentiviral | PCR, CCK-8 assay, annexin V apoptosis assay | Reduced cell proliferation due to enhanced apoptosis | [54] |
| LNCaP, R1-AD1 | Plasmid | QPCR, sequencing, western blotting | High levels of tumor-specific AR variants and resistance to endocrine treatments in cell lines with AR gene rearrangements | [86] | ||
| PacMet-UT1 | Lentiviral | T7 endonuclease I assay, western blotting | Increased activity in the FGF and MAPK pathways | [87] | ||
| C4-2, CWR22Rv1 | Plasmid | Western blotting, qRT-PCR | Decreased cell proliferation | [88] | ||
| LN-95 | Plasmid | FACS, genotyping, western blotting, RNA-seq, IHC | Not necessarily leading to neuroendocrine differentiation | [89] | ||
| In vitro, in vivo | LNCaP | Plasmid | IHC, RNA-Seq, qRT-PCR, luciferase assay, clonal and clonogenic assays, BrdU incorporation assays | Distinctive biological and tumorigenic characteristics, showing contrasting responses to enzalutamide as a therapeutic target | [90] | |
| AR, NKX3-1 | In vitro | LNCaP | Lentiviral | QPCR | Validation of the regulatory roles of specific enhancers in the expression of NKX3-1 and AR genes | [91] |
| AR, FABP5 | In vitro | PC3-M, DU145, 22RV1 | CRISPR/Cas9 | Flow cytometry, western blotting, PCR, DNA sequencing, RNA sequencing | Inhibition of malignant cell characteristics, partly by disrupting the VEGF signaling pathway | [92] |
| AR-FL | In vitro | CWR22Rv1 | Plasmid | Nucleofection, SURVEYOR assay, PCR and sequencing, FACS, western blotting, qPCR, RNA sequencing | AR variants drive cell growth and androgenic gene expression independently of FL-AR loss | [93] |
| AR-FL, AR-V7 | In vitro | LNCaP-95 | Plasmid | FACS, western blotting, genotyping, RNA sequencing, IHC | Identification of the necessity of AR-FL and AR-V7 in conferring resistance to abiraterone and enzalutamide | [94] |
| ERG | In vitro | Pten−/− R26-ERG organoids | Lentiviral | Histology, IHC, RNA-seq, ChIP-seq, ATAC-seq, proteomics, RIME | Significantly reduced AR-dependent gene expression | [95] |
| TMPRSS2-ERG | In vitro | Mouse prostate organoids | psCas9 plasmid | Puromycin selection, qPCR | Overexpression of ERG due to AR activity | [62] |
| GATA2 | In vitro | 22Rv1 | Plasmid | Western blotting, qRT-PCR, single clone isolation, genotyping | Identification of GATA2 amplification’s role in enhancing TGFβ1 and AR signaling pathways | [96] |
| GREB1 | In vitro, in vivo | LNCaP/AR | Lentiviral | Single-cell cloning, flowcytometry | Restoration of enzalutamide sensitivity in cells with high AR output | [97] |
| TLE3 | In vitro | LNCaPCWR-R1, 22Rv1, LAPC4 | Lentiviral | Real-time live cell proliferation monitoring, colony formation assays, RNA-seq, ChIP-seq, ChIP-qPCR, western blotting, (IHC), qPCR | Increased resistance to AR inhibitors, including apalutamide and enzalutamide | [98] |
| DOT1L | In vitro | LNCaP, PC3 | Lentiviral, plasmid | QRT-PCR, RNA-seq, Microarray, ChIP, PCR, LC–MS/MS | Reduced viability of AR-positive prostate cancer cells | [99] |
| SF3B2 | In vitro | 22Rv1, LNCaP95 | Plasmid | Western blotting, PAR-CLIP | Identification of SF3B2 as a key factor in the expression of AR-V7 | [100] |
| TGM2 | In vitro | PC3 | Plasmid | Sequencing, western blotting | Increased AR transcription and decreased MUC1 expression | [101] |
| LCMT1 | In vitro | HAP1, LNCaP, VCaP, LNCaP-AR, LAPC4 | lentiviral | Immunoblotting | Enhanced AR activity, promoting the growth of castration-resistant prostate cancer | [102] |
| PARP-1, PARP-2 | In vitro, in vivo | LNCaP | Lentiviral, plasmid | ChIP assay, RNA-seq, ChIP-seq, cell viability, soft agar colony formation assay | Selective inhibition of PARP-2 disrupts its interaction with FOXA1, leading to reduced AR-mediated gene expression and inhibited growth of AR-positive prostate cancer | [103] |
| IP6K2, XPO4, DRG1, PRKAB1, RP2 | In vitro | C4, LNCaP, PC3, DU145, LAPC-4 | Lentiviral, plasmid | Sanger sequencing, RT-qPCR, dose-response assays, AlamarBlue assay, quant-seq analysis | Altered response to enzalutamide following IP6K2 and XPO4 knockout due to deregulation of AR, mTORC1, and E2F signaling pathways | [104] |
| AREM1, AREM2 | In vitro | C4-2B | CISPR/Cas9 | Flow-sorting, qPCR, ChIP-qPCR, ChIP-seq | Significant decrease in AR mRNA levels | [105] |
| hnRNP A1 | In vitro | CWR22Rv1 | Plasmid | Puromycin selection, FACS, genomic PCR, western blotting | Increased expression of AR3 | [106] |
| CAMKK2 | In vitro | LNCaP, 22Rv1 | Lentiviral, plasmid | Western blotting, immunofluorescence microscopy | Demonstrating that AR can utilize the CAMKK2-AMPK-ULK1 signaling pathway to stimulate prostate cancer by enhancing autophagy | [107] |
| LNCaP | Plasmid | Western blotting, qRT-PCR | Decreased expression of two important lipogenic enzymes, acetyl-CoA carboxylase and fatty acid synthase | [108] | ||
| In vitro, in vivo | C4-2 | Lentiviral, plasmid | Western blotting | Impaired tumor growth | [109] | |
| SOX2 | In vitro | CWR22-R1 | CRISPR/Cas9 | Western blotting | Modified gene expression profiles, particularly in pathways associated with resistance to AR antagonists | [110] |
| YAP1 | In vitro | LNCaP | Plasmid | Western blotting, qRT-PCR, immunofluorescence and microscopy | Revealing that androgen differentially regulates YAP1-dependent gene expression | [111] |
| G3BP1 | In vitro | LNCaP, 22Rv1 | Lentiviral, plasmid | Immunoblot, CellTiter96, xenograft studies, RNA-seq, qRT-PCR | Revealing a G3BP1-SPOP ubiquitin signaling axis that promotes PCa progression through activating AR signaling | [112] |
| EZH2 | In vitro | 16DCRPC | Plasmid | GeneArt genomic cleavage detection, FACS, western blotting, sanger sequencing | Establishing a collaborative role for AR and EZH2 in promoting drug resistance | [113] |
| In vitro, in vivo | PC-3 | Plasmid | SURVEYOR assay, western blotting, MTT assay, wound healing and proliferation assays, qRT-PCR, annexin V-PI assay | Decreased H3K27me3 levels and increased apoptosis | [114] | |
| EZH2, SETD2 | In vitro, in vivo | C4-2, LNCaP | PX330 plasmid | QRT-PCR | Demonstrating the role of the SETD2-EZH2 axis in linking metabolic and epigenetic signaling pathways to suppress prostate cancer metastasis | [115] |
| PSA | In vitro | LNCap, PC3, AT3B-1, DU145, RWPE1 | Plasmid | Luciferase assay, qRT-PCR, MTT assay, colony formation assay, cell migration assay, transwell migration assay, annexin V-PI assay | Reduced cell proliferation and migration, enhanced apoptosis | [56] |
| Survivin | In vitro | PC3 | Plasmid | Colony PCR, sequencing, qRT-PCR, XTT assay, annexin V-PE/7- AAD assay, CCK-8 assay | Induced apoptosis and downregulation of FBXO5 and RRM2 | [59] |
| SPOP | In vitro | LNCaP, | Plasmid | Genomic DNA and cDNA sequencing | Elevated GLI3 protein levels, indicating decreased degradation | [116] |
| In vitro, in vivo | DU145 | Lentiviral | Western blotting, real-time quantitative PCR, IP, in vivo xenograft assay | Identifying SPOP as a tumor suppressor that promotes the ubiquitination and degradation of NANOG | [117] | |
| SPOP, Caprin1 | In vitro | 293T, LNCaP, 22Rv1, PC-3, DU-145, C4-2 | PX459 plasmid | Western blot, sanger sequencing, cell cycle distribution and cell death, qRTPCR, EdU incorporation assay, immunofluorescence, migration assay | Resistance to cell death induced by stress granule inducers (e.g., docetaxel, sodium arsenite, and H2O2) | [118] |
| SPOP, HIPK2 | In vitro, in vivo | PC-3, DU145 | PX459 plasmid | Western blot, sanger sequencing, CCK-8 assay, colony formation assay | High levels of genomic instability | [119] |
| SPOP, SQSTM1/p62, ATG3, ATG5, ATG7, NFE2L2 | In vitro | PC-3, DU145 | PX459 plasmid | Western blotting, sanger sequencing | Increased autophagy and activation of Nrf2 | [120] |
| FOXA1 | In vitro | LNCaP | Plasmid | Western blotting, dot blotting | Altered expression of Casp-9, Bax, CCND1, CDK4, and fibronectin; no changes observed in Casp-3, Bcl-2, survivin, β-catenin, c-Myc, and GSK-3B; inhibition of CCND1 protein expression in LNCaP cells | [121] |
| LNCaP, 22Rv1 | Lentiviral, plasmid | Western blotting, cell proliferation assay, luciferase reporter assay, allele-specific ChIP-qPCR | Reduction in FOXA1 expression, leading to decreased cell growth | [122] | ||
| LNCaP, 22RV1 | Lentiviral, plasmid | Sanger sequencing, ChIP-seq | Reaffirming FOXA1 central role in mediating androgen receptor-driven oncogenesis | [123] | ||
| LNCaP, LNCaP 42D, LNCaP 42 F | Lentiviral | Immunoblot, western blotting, immunohistochemistry | Inhibited cell proliferation | [124] | ||
| LNCaP | Lentiviral | Puromycin selection, PCR, qRT-PCR, sanger sequencing | Upregulation of TGFB3, a gene encoding a ligand in the TGF-β pathway | [125] | ||
| In vitro, in vivo | Mouse prostate organoids, Rosa26-Cas9 organoids | Lentiviral, plasmid | Western blotting, RNA-seq, ATAC-seq, ChIP-seq | Disruption of normal luminal epithelial differentiation programs | [126] | |
| FOXA1, FOXP1, PTEN | In vivo | MEF cells from LSL-Cas9 mice, HEK293T | AAV-plasmid | Histochemical analysis, PCR | Induction of epithelial plasticity due to FOXA1 loss and increased cell proliferation due to FOXP1 loss | [127] |
| NANOG and NANOGP8 | In vitro, in vivo | DU145 | PX330 plasmid | PCR, genotyping, western blotting | Reduced malignant potential, diminished sphere formation, anchorage-independent growth, migration ability, and chemoresistance | [61] |
| SRD5α2 | In vitro | DU145 | A cationic liposome preparation carrying sgRNA on its surface | QRT-PCR | Discovery of a novel gene-editing approach targeting SRD5α2 to offer alternative treatments for prostate cancer without the adverse effects of current medications | [57] |
| CHD1 | In vitro | 22Rv1 | CRISPR/Cas9 | Immunoblotting, IHC, FISH, DNA sequencing | Improved response rate and extended efficacy during abiraterone treatment | [128] |
| In vitro, in vivo | 22Rv1, RWPE-1 | Plasmid | FACS, SURVEYOR mutation assay, PCR, sanger sequencing | Increased vulnerability to DNA damage, reduced efficiency of error-free HR repair, and elevated reliance on error-prone NHEJ repair, leading to genomic instability | [129] | |
| BRCA2 | In vitro | LNCaP | Lentiviral | Western blotting | Heightened sensitivity to SPA, resulting in increased DNA damage and apoptosis | [130] |
| LNCaP | Lentiviral | Sanger sequencing, qPCR | Elevated SRC phosphorylation and greater responsiveness to SRC inhibitors like dasatinib, bosutinib, and saracatinib | [131] | ||
| BRCA2, RB1 | In vitro | LNCaP, 22RV1 | Lentiviral | FISH, western blotting, qPCR, RNA sequencing | Induced epithelial-to-mesenchymal transition, leading to greater invasiveness and a more aggressive cancer phenotype | [132] |
| TP53, RB1 | In vitro, in vivo | LNCaP | Lentiviral, plasmid | Western blotting | High proliferation rates, resistance to different therapies | [133] |
| HOXB13 | In vitro | 22Rv1, DU145, LNCaP, C4-2, PC3, RWPE-1, VCaP, C4-2B | Plasmid, CRISPR/Cas9 constructs (GFP expressing) | Western blotting, qPCR, immunofluorescence studies, MTT assay, BrdU assay, wound scratch assay | Induction of apoptosis and strong suppression of tumor cell proliferation and migration | [134] |
| CWR22Rv, LAPC4 | Lentiviral, plasmid | Western blotting | Altered cell proliferation patterns | [135] | ||
| CTCF | In vitro | 22Rv1 | Lentiviral, plasmid | PCR, sanger sequencing, western blotting | Reorganization of CTCF looping and changes in H3K27ac loops at the MYC region | [136] |
| SMYD2 | In vitro | CWR-R1ca | Plasmid | Western blotting, wound-healing assay, colony formation assay, transwell assay | Decreased viability, reduced migration and invasion capacity, and fewer colonies formed | [137] |
| SYNCRIP | In vitro | LNCaP/AR, CWR22Pc, MDA-PCa-2b | Lentiviral, plasmid | CellTiter-Glo, flowcytometry, western blotting | Increased APOBEC-driven mutagenesis | [138] |
| p54/nrb (NONO) | In vitro, in vivo | CWR22Rv1 | Plasmid | Western blotting, qRT-PCR, FACS, genomic PCR | Lowered PCGEM1 expression, leading to reduced tumor growth | [139] |
| ARNTL | In vitro, in vivo | LNCaP, LNCaP-42D, LNCaP-ResA | Lentiviral, plasmid | Western blotting, puromycin selection, cell viability and xenograft studies | Inhibited growth of prostate cancer cells | [140] |
| (N-terminal domain of) PIP5K1α | In vitro, in vivo | LNCaP C4-2, LNCaP C4-2 SG | CRISPR/Cas9 | Sequencing | Reduced ability of cancer cells to grow and migrate | [141] |
| NKX3.1 | In vivo | C57BL6, Swiss-Webster, B6D2F1 mice | PX330 plasmid | Genotyping, histologic analysis, in situ TUNEL staining | Allelic loss of Nkx3.1 led to decreased Nkx3.1 protein level and increased proliferation | [64] |
Several other genes were found to be regulated by AR signaling. For instance, prostate-specific antigen (PSA) is among androgen-responsive genes [55]. This proto-oncogene is widely found in embryonic and prostate cancer cells, and is absent in normal prostate cells. A research team inspected the conditional transcriptional regulation of the PSA promoter and its application for the gene therapy. A CRISPR/dCas9-KRAB system was constructed using the PSA promoter to repress transcription of the PSA gene. This inhibition consequently resulted in the blockage of tumor growth and migration, and induction of apoptosis. Therefore, this study underlined the ability of the CRISPR-dCas9-KRAB system to control PSA expression as a therapeutic strategy for the prostate cancer gene therapy [56].
The steroid type II 5-alpha-reductase (SRD5α2) enzyme facilitates the conversion of testosterone to dihydrotestosterone, which are hormones associated with prostate cancer and benign prostatic hyperplasia. Suppression of SRD5α2 activity is regarded as a possible therapy for these disorders; however, current pharmacological treatments have certain side effects, and novel therapeutic modalities are desirable. Akbaba et al. established a cationic liposome preparation that encapsulates Cas9 protein and carries sgRNA on its surface. Such well-structured liposome exhibited favorable physicochemical characteristics, stability, low cytotoxicity, efficient cellular intake, and high gene knockout efficiency. The Lipo/Cas9 with sgRNA resulted in a 29.7% reduction in relative SRD5α2 mRNA expression. The research indicated mentioned liposomal formulation is a promising method for treating prostate cancer or BPH while avoiding the side effects associated with current medications [57].
Survivin is another molecule that plays a role in both AR-dependent and AR-independent drug resistance in prostate cancer. Its expression was up-regulated by androgen in both AR-positive LNCaP and AR-negative prostate cancer cells [58]. CRISPR-mediated silencing of Survivin induced apoptosis of prostate cancer cells [59].
NANOG is another factor that is involved in AR signaling. It can reprogram prostate cancer cells to castration resistance through suppressing the AR/FOXA1 signaling route [60]. In another study, Kaneda and colleagues demonstrated the role of NANOG and its pseudogenes in prostate cancer. Using the CRISPR/Cas9 technology, researchers obtained NANOG- and NANOGP8-knockout DU145 cells and examined their malignant features. Knockout of NANOG and NRFP8 significantly inhibited various malignant characteristics of these cells, namely sphere construction, anchorage-independent growth, migration ability, and chemoresistance. NANOG and NANOGP8 knockout did not suppress in vitro cell proliferation. However, the tumorigenic ability of cells was reduced significantly. It was revealed that both NANOG and NANOGP8 have an equivalent role in the aggressiveness of prostate cancer. This study highlighted the possibility of CRISPR-based targeting of NANOG and NANOG88 for the treatment of prostate cancer by inhibiting the malignant characteristics of cancer cells [61].
Another group achieved a great success by developing mice prostate models with the TMPRSS2-ERG gene fusion, a common genetic alteration in prostate cancer. Gene fusion was successfully induced by a CRISPR/Cas9-based technique, leading to the overexpression of ERG, a crucial factor in prostate development, in cancer cells. Treatment with the AR antagonist nilutamide led to the restoration of the fusion transcript expression to normal ERG levels. This novel model offered a helpful platform for studying the underlying processes of TMPRSS2-ERG fusion and exploring potential therapeutic interventions [62].
NKX3.1 is a homeodomain transcription factor that has androgen-responsive regions in its 3’ untranslated region [63]. The suppressor gene NKX3.1 has a crucial role in prostate cancer by acting as a gatekeeper. NKX3.1 is haplo-insufficient, and pathogenic decrease in its protein level might be due to genetic loss, reduced transcription, and elevated protein degradation resulting from inflammatory reactions or PTEN loss. CRISPR/Cas9 method was used to introduce a missense mutation in murine Nkx3.1 to substitute alanine with serine at aminoacid 186, the region that is target for Dyrk1b phosphorylation. The Nkx3.1S186A/− mouse exhibited elevated Nkx3.1 protein levels, decreased prostate size, normal histology, decreased cell growth as well as enhanced DNA labeling. The findings demonstrated that modification of only Nkx3.1 can lead to longstanding control over precancerous alterations related to DNA damage in the prostate. This also displayed the feasibility of CRISPR-guided modulation of NKX3.1 as a therapeutic strategy for prostate cancer [64].
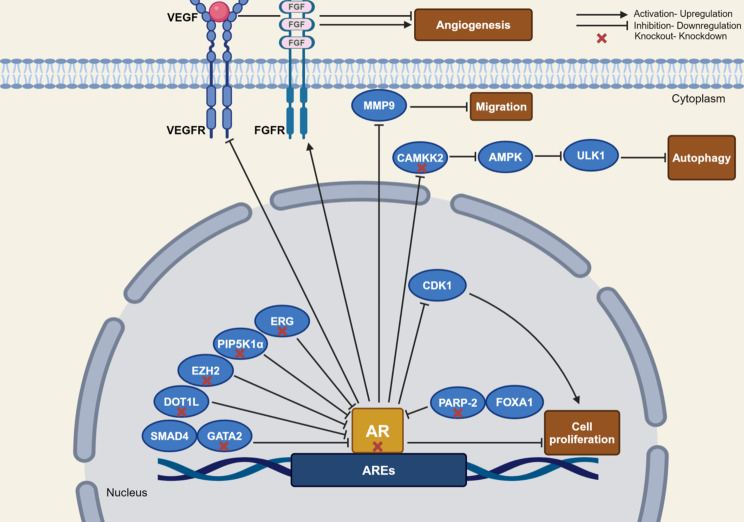
Figure 2 demonstrates a number of genes in the AR signaling that were targeted by CRISPR/Cas9 in prostate cancer.
Fig. 2.
An overview of different genes in the AR signaling targeted by CRISPR/Cas9 in prostate cancer, and consequences of gene editing on cell proliferation, autophagy, migration and angiogenesis. Figure was depicted using BioRender
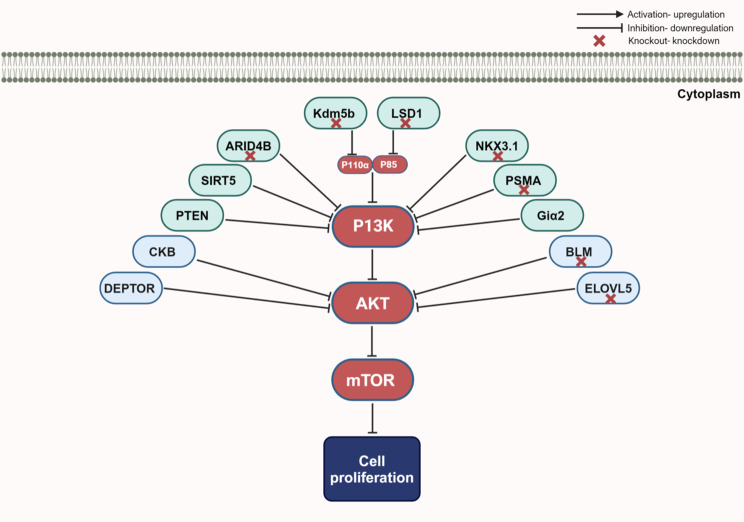
CRISPR-mediated modification of PI3K/AKT/mTOR pathway
PI3K/AKT/mTOR pathway as one of the important pathways in the carcinogenesis of prostate cancer has been the focus of several CRISPR-mediated knockout studies in this field (Table 2). PI3K/AKT pathway is hyperactivated in nearly all advanced prostate cancers, mostly via PTEN loss [65, 66]. The serine/threonine protein kinase mTOR belongs to the PI3K/AKT/mTOR pathway and controls cell growth, proliferation, survival, autophagy, and metabolism [67]. This protein establishes two distinctive complexes, namely mTORC1 and mTORC2. Notably, DEPTOR is a common constituent of both complexes that directly binds to mTOR to inhibit the activity of both complexes [68]. DEPTOR expression was considerably reduced in prostate cancer samples, in correlation with disease progression. CRISPR-mediated depletion of DEPTOR enhanced proliferation, survival, migration, and invasive capacity of these cells. This intervention led to activation of cell proliferation and survival, and induction of an AKT-dependent epithelial–mesenchymal transition (EMT) and nuclear translocation of β-catenin leading to cell migration and invasive features. Most notably, Deptor knockout speeded prostate tumor growth in animal models through activation of mTOR signaling. Therefore, reactivation DEPTOR might be suggested as a therapeutic strategy for prostate cancer [69].
Table 2.
CRISPR-mediated modification of PI3K/AKT/mTOR pathway in prostate cancer
| Target gene | Study type | Cell line | Vector | Screening/verification | Experimental data | Ref |
|---|---|---|---|---|---|---|
| DEPTOR | In vitro | DU145, 22RV1 | PX459 plasmid | Puromycin selection | Enhanced cell proliferation, survival, migration, and invasion, activated AKT-dependent EMT, and nuclear translocation of β-catenin | [69] |
| BLM | In vitro | PC-3 | Plasmid | Immunohistochemistry, western blotting, T7 endonuclease I assay, PCR | Lower level of phosphorylated AKT (Ser473) and PRAS40 (Thr246) | [143] |
| ELOVL5 | In vitro, in vivo | C4-2 | Plasmid | Western blotting, qRT-PCR | Reduced AKT-mTOR signaling activity | [144] |
| SIRT5 | In vitro | PC-3 | Plasmid | Western blotting, FACS | Elevated IL-1β expression and increased PI3K/AKT/NF-κB signaling | [145] |
| In vitro | PC-3 | Plasmid | Western blotting, FACS, wound-healing assay, transwell assay, CCK-8 assay | Increased cell invasion capability | [146] | |
| AKT 1/2 | In vitro, in vivo | CWR22rv1 | Lentiviral, plasmid | Puromycin screening, western blotting, sequencing | Suppressed metastasis | [147] |
| KDM1A (LSD1) | In vitro | 22Rv1 | Lentiviral | Puromycin screening, immunoblotting | Inhibited PI3K/AKT signaling | [148] |
| ATF3 | In vitro | LNCaP, DU145, PC3 | Plasmid | Western blotting, Surveyor mutation detection assay, qRT-PCR, zymography | Promoted AKT activation, resulting in enhanced cell proliferation | [149] |
| CKB | In vitro | PC3 | PX458 plasmid | Sanger sequencing, western blotting, flow cytometry | Activation of AKT, driving EMT and cell migration | [150] |
| ARID4B | In vitro, in vivo | PC3, DU145 | Plasmid | Western blotting, MTT assay | Identification of ARID4B as a key regulator in the PTEN-PI3K pathway | [151] |
| NKX3.1 | In vivo | C57BL/6 mice | Cas9 protein and sgRNA | Western blotting, IF staining, IHC staining | Inhibition of the PI3K/AKT/mTOR pathway | [73] |
| PSMA | In vitro | TRAM,22RV1 | Lentiviral, plasmid | Puromycin selection, sequencing, TIDE | Decreased PI3K-AKT signaling, with increased MAPK-ERK1/2 signaling | [152] |
| PPARG | In vitro, in vivo | PC3-M | Plasmid | Puromycin selection | Identification of a functional impact of PPARG on AKT3, associated with a more aggressive disease phenotype | [153] |
| PTEN | In vitro, in vivo | MSK-PCa1, MSK-PCa2, MSK-PCa3, MSK-PCa8, MSK-PCa11, MSK-PCa12, MSK-PCa15, MSK-PCa16, LNCaP, DU145, CWR22Pc, CWR22Pc-EP | Lentiviral | Sequencing | Effective pan-PI3K inhibition, with upregulation of IGF1R and promoted resistance | [154] |
| In vitro | 2924 V | PX459 plasmid | DNA sequencing, western blotting, MTT assay | Enhanced phosphorylation of RAC alpha serine/threonine protein kinase and increased cyclin D1 level | [155] | |
| PTEN, Fos, Jun | In vivo, in vitro | BPH-1, PC-3, DU145, murine prostate epithelium | Lentiviral, plasmid, AAV | Validation of guide RNA efficiency, Histology, IHC, qRT-PCR, sanger sequencing | Loss of Fos contributing to disease progression through accelerated proliferation and invasiveness, partly via Jun activation | [156] |
| PTEN, α6-integrin, β4-integrin, plectin | In vitro, in vivo | RWPE1, DU145, PC3, 22Rv1, LNCaP, VCaP, JIMT-1 | Lentiviral, plasmid | Western blotting, qRT-PCR, proliferation assay, soft agar assay, RNA-Seq | Activation of EGFR/PI3K/Akt and FAK/Src | [157] |
| WHSC1 | In vitro, in vivo | PC3 | Plasmid | Western blotting, qRT-PCR, ChIP | Condensed chromatin structure at the RAC1 gene locus, leading to reduced transcription | [158] |
| Giα2 | In vitro | PC3 | Plasmid | Sanger sequencing, western blotting, flow cytometry | Impaired lamellipodia establishment at the leading edge of migrating cells and attenuation of TGFβ1 signaling | [159] |
| KDM5B | In vitro | LNCaP, C4–2B, PC3 | Lentiviral, plasmid | QPCR, western blotting, IF staining, | Significant reduction in P110α and PIP3 levels, leading to decreased cell proliferation | [160] |
| PLK-1 | In vitro | PC-3 | Plasmid | Western blotting | Suppression of tumor growth | [161] |
| In vitro, in vivo | LNCap, PC-3 | Aptamer-liposome-CRISPR/Cas9 chimera | Apoptosis assay, MTT assay | Noticeable regression of prostate cancer | [70] | |
| ATM | In vitro | DU145, 22Rv1, LNCaP | Lentiviral, plasmid | Immunoblotting, NGS | Altered DNA damage response signaling | [162] |
| C4-2 | Lentiviral, plasmid | Puromycin selection, western blotting | Increased sensitivity to Enzalutamide | [163] | ||
| 22Rv1 | Plasmid | Immunostaining, sanger sequencing | Heightened sensitivity to ATR inhibition | [164] | ||
| MCL1 | In vitro, in vivo | LNCaP | Plasmid | Western blotting | Significant sensitization of cancer cells to apoptosis induced by navitoclax, but not by venetoclax | [165] |
| GPRC5A | In vitro, in vivo | PC3, DU145 | Guide-it™ CRISPR/Cas9 System | Real-Time RT-PCR, MTT and BrdU assays, cell cycle assay, RNA-seq | Decreased cell proliferation | [166] |
In another recent study, a flexible aptamer-liposome CRISPR/Cas9 chimera was developed for effective and targeted transfer of CRISPR/Cas9 into specific cells. The chimera had an RNA aptamer that precisely bound cells that expressed the prostate-specific membrane antigen. Conjugating cationic liposomes with aptamers enabled directed delivery of therapeutic CRISPR/Cas9 molecules to tumor cells, resulting in significant gene silencing effects in vitro. Besides, in vivo assays demonstrated that prostate cancer regressed following gene silencing. This innovative approach offers a universal method for cell-type-specific transfer of CRISPR/Cas9, addressing an important challenge for the extensive therapeutic application of CRISPR/Cas9 and other nucleic acid agents [70].
In addition, CRISPR/Cas9 technology was employed to simultaneously modify several genes in mouse prostate cells. The researchers focused on investigating the function of the activating protein-1 (AP-1) transcription factor, which is composed of JUN and FOS subunits and has a crucial role in several types of cancer. They discovered that loss of either JunB or Fos, in conjunction with Pten loss, resulted in the progression of prostate cancer to an invasive stage. On the contrary, lack of Fos enhanced the expression of Jun and CRISPR knockout of Jun also reduced cell proliferation in this context. In brief, JunB and Fos exhibited tumor suppressor functioned by suppressing invasive disease. However, Jun functioned as an oncogene and increased cell proliferation. This demonstrated that AP-1 factors are involved in the different stages of progression of this type of cancer and displayed dual functions as tumor suppressor and oncogene in this process [71].
In another study, GPRC6A, a gene associated with prostate cancer, was investigated, focusing on a polymorphism known as “Y.K” situated in the third intracellular loop that evolved in most humans and replaced the ancestral RKLP. Notably, this variant is prevalent in all human-originated prostate cancer cell lines. The researchers created GPRC6A-deficient PC-3 cells using CRISPR/Cas9 technique and examined its consequences on cell proliferation and migration. Their findings demonstrated that these cellular responses were blocked by targeting GPRC6A in vitro. At the same time, in a xenograft mouse model, their evidence indicated that the proliferation of GPRC6A-deficient PC-3 cells and their resistance to osteocalcin-related progression of prostate cancer was reduced compared to control cells that expressed GPRC6A. The results suggested that GPRC6A might be a potential antagonist for treating prostate cancer, particularly in addressing racial disparities in the disease [72].
The androgen-responsive gene, NKX3.1 can also affect the activity of PI3K/AKT pathway. CRISPR-mediated deletion of exon 1 of this gene led to increased weight of prostate. Ki67 was densely stained in the epithelial cells of these animals, while p53 levels were suppressed in these cells. In addition, PI3K/AKT/mTOR pathway was inhibited in NKX3.1-knockout cells [73]. Figure 3 shows selected genes from PI3K/AKT/mTOR pathway that have been targeted by CRISPR/Cas9 in prostate cancer.
Fig. 3.
Targeting PI3K/AKT/mTOR pathway by CRISPR/Cas9 in prostate cancer. Modification of expression of these targets has led to reduction of prostate cancer cell proliferation. Figure was depicted using BioRender
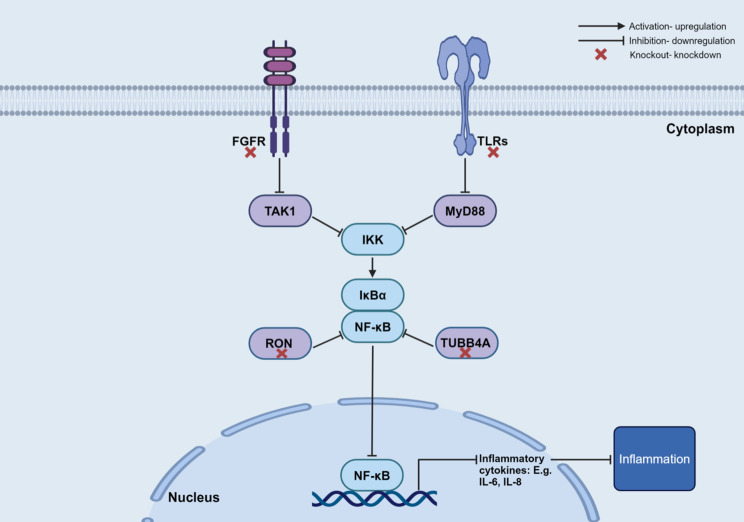
CRISPR-mediated modification of immune-related genes
A group of other genes, namely those related to immune function has been the target of CRISPR-mediated editing in the prostate cancer (Table 3). Most of these genes were enriched in the NF-κB signaling pathway. TUBB4A is an over-expressed gene in human prostate cancer, whose expression is related with aggressive phenotype and poor patient survival. CRISPR-mediated TUBB4A knockout reduced cell growth and migration but induced DNA damage through elevating γH2AX and 53BP1 levels. Notably, TUBB4A knockout led to severe DNA damage, reduced NF-κB signaling response, and retardation of tumor growth and metastases. Mechanistically, TUBB4A knockout reduced MYH9-mediated GSK3β ubiquitination and degradation, resulting in inactivation of β-catenin signaling and its pertinent EMT [74].
Table 3.
CRISPR-mediated modification of immune-related genes
| Target gene | Study type | Cell line | Vector | Screening/verification | Experimental data | Ref |
|---|---|---|---|---|---|---|
| TUBB4A | In vitro, in vivo | DU145 | PX458 plasmid | Western blotting, PCR, sanger sequencing, flow cytometry | Induced DNA damage, reduced NF-κB signaling response | [74] |
| FGFR1 | In vitro, in vivo | DU145 | Lentiviral | Puromycin selection, western blotting | Abolished both FGF activity and NF-κB signaling | [75] |
| ARID1A | In vitro | Myc-CaP | Lentiviral, plasmid | IHC, transwell assay | Unleashed CXCR2 ligand-mediated MDSC chemotaxis by silencing the enhancer of A20 deubiquitinase, a critical negative regulator of NF-κB signaling | [167] |
| RON | In vitro, in vivo | LMyc-CaP | PX458 plasmid | Western blotting, qRT-PCR | Demonstrating the role of RON in activating β-catenin and NF-κB |
[168] [169] |
| IL30 | In vitro, in vivo | PIN-SCs, DU145, PC3 | PX458 plasmid, CRISPRMAX™ Cas9 transfection reagent | Real-time PCR, western blotting, ELISA | Significant downregulation of BCL2, NF-κB, STAT3, IGF1 and CXCL5 expression, upregulation of SOCS3 | [170] |
| In vitro, in vivo | PIN-SC | Lentiviral, CRISPR/Cas9 | ELISA, western blotting | Decreased tumor onset, proliferation | [171] | |
| SEPT5 | In vitro, in vivo | RM1 | Lentiviral, plasmid | Western blotting, real-time PCR | Inhibited cancer progression, increased CD8 + T cell infiltration, elevated expression of CCL5, CXCL5, CXCL9, CXCL10, and INFGR1 | [172] |
| TLR3 | In vitro, in vivo | DU145 | Lentiviral, plasmid | Western blotting, DNA sequencing | Lower motility | [173] |
| IL-8/CXCL15 | In vitro, in vivo | Myc-CaP | Plasmid | ELISA, PCR, sanger sequencing | Increased density of polyfunctional CD8 T cells, delay in the onset of castration resistance | [174] |
| LEDGF/p75 | In vitro | HEp-2 | PX458 plasmid | FACS, immunofluorescence assay | Identified the role of LEDGF/p75 in inducing inflammatory processes | [175] |
| NEK6 | In vitro | DU-145 | PX459 plasmid | Western blotting, PCR, sanger sequencing | Decreased clonogenic capacity, proliferation, cell viability, mitochondrial activity | [176] |
| RelB | In vitro, in vivo | RM-1 | Plasmid | Immunofluorescence, luciferase reporter assay | Decreased PD-L1 expression, improved susceptibility to T cell immunity | [177] |
| ASIC1 | In vitro, in vivo | 22Rv1 | Plasmid | Western blotting, real-time quantitative PCR | Reduced cell invasion, and decreased castration resistance | [178] |
| MAP4K4 | In vitro | PC3 | Lentiviral, plasmid | Western blotting, PCR, sanger sequencing, | Inhibition of metastatic PCa cells migration and clonogenic properties | [179] |
| CXCR2 | In vitro, in vivo | C4-2B/MDVR | PX458 plasmid | FACS | Suppressed tumor growth | [180] |
| CXCR7 | In vitro | LNCaP, C4-2B | Plasmid | RT-q-PCR, senescence assay, proximity ligation assay (PLA) | A complete stop in cell proliferation, disrupted EGFR signaling | [181] |
| In vitro, in vivo | C4-2B | Lentiviral, plasmid | Genotyping, PCR, flow cytometry | Inhibition of tumor growth | [182] | |
| LNCaP, C4-2B | Lentiviral, plasmid | Cell proliferation, colony formation, cell invasion assays, FACS | Demonstrating CXCR7-mediated MAPK activation as a mechanism of resistance to second-generation antiandrogen therapy | [182] |
In an attempt to find the mechanisms by which conversion of different FGFR isoforms participates in the progression prostate cancer, Wang et al. conducted a study. They reported that FGF promoted NF-κB signaling in prostate cancer cells and in association with FGFR1 expression. CRISPR/Casp-mediated of FGFR1 disruption retracted both FGF activity and NF-κB signals. Further experiments revealed that the role of FGFR1 in stimulation of NF-κB signaling is mediated by TGF β-activating kinase 1 (TAK1). In fact, FGFR1 promoted NF-κB signaling through decreasing TAK1 degradation and thus maintaining continued NF-κB activation. Collectively, this study revealed that FGFR1 promoted progression of prostate cancer through induction of inflammatory responses in the tumor microenvironment [75]. Figure 4 demonstrates selected targeted genes in prostate cancer participating to the immune responses.
Fig. 4.
Targeted genes by CRISPR/Cas9 in prostate cancer participating to the immune responses. Figure was depicted using BioRender
CRISPR-mediated modification of other genes and signaling pathways
A recent work by Kypta et al. explored the potential of using CRISPR to activate the DKK3 gene as a therapeutic modality for prostate cancer. Human DNA contains DKK3, a tumor-suppressor gene that suppresses prostate cancer progression and metastasis. Its expression is reduced by promoter methylation in prostate cancer. The researchers demonstrated that a DNA methyltransferase inhibitor had a hypomethylating effect on the DKK3 promoter, leading to elevated DKK3 level in prostate cancer cells. Moreover, by transcription from DKK3 using CRISPR-dCas9-VPR, the activity of TGF-β/Smad pathway was suppressed, thus proliferation and metastasis of prostate cancer cells were inhibited. Crucially, these findings open the door for the application of CRISPR-mediated DKK3 induction in prostate cancer treatment [76].
One notable endeavor focused on targeting lipocalin 2 (Lcn2/NGAL), a member of the lipocalin superfamily with various roles, to investigate its precise role in cancer development. This study utilized CRISPR/Cas9 technology to knockout Lcn2 expression in a metastatic and invasive prostate cancer cell line, PC3. This study aimed to evaluate the efficacy of combining Lcn2 knockdown with cisplatin, a widely used chemotherapeutic medication. The researchers co-transfected PC3 cells with the control CRISPR/Cas9 plasmid and the human Lcn2 CRISPR/Cas9-knockout plasmid or the HDR CRISPR/Cas9 plasmid. Stable cells were selected with puromycin. Then, the PC3 cells with Lcn2 knockout (Lcn2-KO) were treated with and without cisplatin, focusing on their proliferative ability, apoptosis rate, and migratory capabilities. Their study revealed that suppressing Lcn2 in PC3 cells repressed cell proliferation and enhanced the effectiveness of cisplatin. The significant decrease in expression of Lcn2 expression resulted in increased cisplatin induced apoptosis in PC3 cells. Moreover, cell migratory ability of PC3 cells decreased following Lcn2 knockout by CRISPR/Cas9 technology. The results demonstrated how Lcn2 can be both a reliable biomarker for prostate cancer diagnosis and prognosis in addition to a potential therapeutic target. The study also suggested that CRISPR-based technology to target Lcn2 may lead to improved disease outcomes for patients with extremely aggressive prostate cancer [77].
Based on recent advancements, researchers investigated the molecular biology of aberrant gene expression in prostate cancer cells. Yang et al. employed CRISPR interference (CRISPRi) and CRISPR activation (CRISPRa) techniques to control the transcription of ITGB5, TIMP1 and TMEM176B in prostate cancer cells. Various cellular experiments were conducted to define the involvement of these gens in prostate cancer, and it was discovered that their activation has an inhibitory effect on prostate cancer. Furthermore, these three genes were found to synergistically influence cancer cell proliferation, invasion and migratory capacity, highlighting their potential as therapeutic targets [78].
Another research team conducted a genome-wide CRISPR/Cas9 investigation on a mouse prostate cancer model to identify potential gene targets that might improve the effectiveness of docetaxel chemotherapy. Transcription elongation factor A-like 1 (TCEAL1) was identified as the most appropriate gene among the 17 candidate genes. Although the specific function of TCEAL1 is not yet completely clarified, it is supposed to regulate transcription in a promoter-dependent manner. Inhibition of TCEAL1 in several human prostate cancer cell lines increased effect of docetaxel, suggesting a potential target for combination therapy Investigators. Using gene culture analysis and flow cytometry, researchers further verified that loss of TCEAL1, in conjunction with docetaxel, alters the cell cycle profile. findings supported TCEAL1 as a potential option for enhancing the therapeutic effect of docetaxel [79].
Discussion
Prostate cancer, a prevalent and deadly disease with limited treatment options, requires innovative approaches to address its progression and overcome therapy resistance. Recent advancements in CRISPR technology have revolutionized research in this field, resulting in a significant progress in the detection and treatment of prostate cancer. Moreover, application of CRISPR-based techniques for gene regulation has offered opportunities to investigate gene function in cancer cells. In fact, it has demonstrated the role of interaction between classical tumor suppressors and epigenetic factors in the pathogenesis of this type of cancer [80].
The recent projects utilizing CRISPR technology in prostate cancer research have also provided new perceptions about the diagnostic and therapeutic strategies for this disease. Actually, the capacity of CRISPR/Cas system to target RNA has provided novel approaches to tumor diagnostics. However, most of applied research in this field has used mice models of cancer, thus making translation of the obtained data to clinical application challenging.
Most notably, mentioned experiments have shown that CRISPR/Cas9-mediated suppression of a number of genes can enhance therapeutic effects of conventional chemotherapeutic agents, suggesting novel combinatory regimens for treatment of prostate cancer. This technique has also facilitated identification of molecular events that contribute to each phase of prostate cancer development and progression. In fact, genome-wide CRISPR activation and inhibition screening has shown several drivers and inhibitors of metastasis cascades in prostate cancer [81]. Thus, several potential molecular targets for combating diverse aspects of carcinogenesis have been uncovered using this technique. In vivo application of CRISPR technology has unveiled the function of several commonly mutated genes in prostate cancer and their differential effects in the promotion of tumor growth and regulation of cell fate and dissemination.
As a novel therapeutic option, chimeric antigen receptor (CAR) T cell therapies were found to be safely tolerated in patients with prostate cancer. Moreover, this treatment led to TCR repertoire diversity and modulation of the tumor immune niche in a group of patients [82]. Meanwhile, CRISPR/Cas9 technique offered an effective way for enhancement of the proliferation ability and perseverance of CAR-T cells in the body. This tool was used in CAR-T cells to produce a memory phenotype, decrease exhaustion, and find novel targets to enhance the anti-tumor ability [83].
The main obstacle to bringing CRISPR technology into the clinic is the delivery of CRISPR/Cas to prostate tumors. An optimal targeted delivery system should have a safe vehicle protecting RNA from nuclease degradation in the circulation; and a targeting moiety/ligand that specifically recognizes the receptor and efficiently direct cargo into a specific tissue or cell [70]. In fact, this strategy requires a highly specific targeting ligand that has high affinity to a cellular receptor [84]. Thus, recognition of specific receptors on prostate cancer cells which are not expressed on normal cells can enhance the efficiency of this system. Among different delivery systems, the aptamer-liposome-CRISPR/Cas9 chimera has been proved to have a significant cell-type binding specificity, an extraordinary gene silencing impact in vitro, and a noticeable effect on in vivo regression of prostate tumors [70].
CRISPR therapy has experienced a truly extraordinary achievement, since it has been translated into the clinical application in just 11 years [85]. A number of clinical trials of CRISPR therapy are currently recruiting patients with hematological malignancies (NCT05885464) or solid tumors (NCT05795595). Thus, it is expected that this technology revolutionizes current therapy of cancer in near future. At this time, identification of appropriate targets for this system is a priority. In the context of prostate cancer research and therapy, this target should have an indispensible role in the carcinogenesis being dysregulated in a wide array of patients with different pathological features.
Author contributions
MT and FSM searched the literature and designed the figure. EM contributed in literature search. SG-F supervised the study and wrote the manuscript. All authors approved the final draft.
Funding
No funding was received.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Mobina Tabibian and Fahimeh Salasar Moghaddam contributed equally to this work.
Contributor Information
Elahe Motevaseli, Email: e_motevaseli@tums.ac.ir.
Soudeh Ghafouri-Fard, Email: s.ghafourifard@sbmu.ac.ir.
References
- 1.Mirza Z, Karim S, Advancements. in CRISPR/Cas9 technology—focusing on cancer therapeutics and beyond. In: Seminars in Cell & Developmental Biology, 2019. Elsevier, pp 13–21. [DOI] [PubMed]
- 2.Maeder ML, Gersbach CA. Genome-editing technologies for gene and cell therapy. Mol Ther. 2016;24(3):430–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ishino Y, Shinagawa H, Makino K, Amemura M, Nakata A. Nucleotide sequence of the iap gene, responsible for alkaline phosphatase isozyme conversion in Escherichia coli, and identification of the gene product. J Bacteriol. 1987;169(12):5429–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mojica FJ, Juez G, Rodriguez-Valera F. Transcription at different salinities of Haloferax mediterranei sequences adjacent to partially modified PstI sites. Mol Microbiol. 1993;9(3):613–21. [DOI] [PubMed] [Google Scholar]
- 5.Mojica FJ, Díez-Villaseñor Cs, García-Martínez J, Soria E. Intervening sequences of regularly spaced prokaryotic repeats derive from foreign genetic elements. J Mol Evol. 2005;60:174–82. [DOI] [PubMed] [Google Scholar]
- 6.Lau V, Davie JR. The discovery and development of the CRISPR system in applications in genome manipulation. Biochem Cell Biol. 2017;95(2):203–10. [DOI] [PubMed] [Google Scholar]
- 7.Barrangou R, Fremaux C, Deveau H, Richards M, Boyaval P, Moineau S, Romero DA, Horvath P. CRISPR provides acquired resistance against viruses in prokaryotes. Science. 2007;315(5819):1709–12. [DOI] [PubMed] [Google Scholar]
- 8.Ratan Z, Son Y, Haidere M, Mahtab Uddin B, Yusuf M, Zaman S. CRISPR-Cas9: a promising genetic engineering approach in cancer research. Ther Adv Med Oncol. 2018;10:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sapranauskas R, Gasiunas G, Fremaux C, Barrangou R, Horvath P, Siksnys V. The Streptococcus thermophilus CRISPR/Cas system provides immunity in Escherichia coli. Nucleic Acids Res. 2011;39(21):9275–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gasiunas G, Barrangou R, Horvath P, Siksnys V. (2012) Cas9–crRNA ribonucleoprotein complex mediates specific DNA cleavage for adaptive immunity in bacteria. Proceedings of the National Academy of Sciences 109 (39):E2579-E2586. [DOI] [PMC free article] [PubMed]
- 11.Deltcheva E, Chylinski K, Sharma CM, Gonzales K, Chao Y, Pirzada ZA, Eckert MR, Vogel J, Charpentier E. CRISPR RNA maturation by trans-encoded small RNA and host factor RNase III. Nature. 2011;471(7340):602–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jinek M, Chylinski K, Fonfara I, Hauer M, Doudna JA, Charpentier E. A programmable dual-RNA–guided DNA endonuclease in adaptive bacterial immunity. Science. 2012;337(6096):816–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cong L, Ran FA, Cox D, Lin S, Barretto R, Habib N, Hsu PD, Wu X, Jiang W, Marraffini LA. Multiplex genome engineering using CRISPR/Cas systems. Science. 2013;339(6121):819–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mali P, Yang L, Esvelt KM, Aach J, Guell M, DiCarlo JE, Norville JE, Church GM. RNA-guided human genome engineering via Cas9. Science. 2013;339(6121):823–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Qi LS, Larson MH, Gilbert LA, Doudna JA, Weissman JS, Arkin AP, Lim WA. Repurposing CRISPR as an RNA-guided platform for sequence-specific control of gene expression. Cell. 2013;152(5):1173–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sarkar E, Khan A. Erratic journey of CRISPR/Cas9 in oncology from bench-work to successful-clinical therapy. Cancer Treat Res Commun. 2021;27:100289. 10.1016/j.ctarc.2020.100289. [DOI] [PubMed] [Google Scholar]
- 17.Sinkunas T, Gasiunas G, Fremaux C, Barrangou R, Horvath P, Siksnys V. Cas3 is a single-stranded DNA nuclease and ATP‐dependent helicase in the CRISPR/Cas immune system. EMBO J. 2011;30(7):1335–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anantharaman V, Iyer LM, Aravind L. Presence of a classical RRM-fold palm domain in Thg1-type 3’-5’nucleic acid polymerases and the origin of the GGDEF and CRISPR polymerase domains. Biol Direct. 2010;5:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Makarova KS, Aravind L, Wolf YI, Koonin EV. Unification of Cas protein families and a simple scenario for the origin and evolution of CRISPR-Cas systems. Biol Direct. 2011;6:1–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nimkar S, Anand B. Cas3/I-C mediated target DNA recognition and cleavage during CRISPR interference are independent of the composition and architecture of Cascade surveillance complex. Nucleic Acids Res. 2020;48(5):2486–501. 10.1093/nar/gkz1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kolesnik MV, Fedorova I, Karneyeva KA, Artamonova DN, Severinov KV. Type III CRISPR-Cas systems: deciphering the most Complex Prokaryotic Immune System. Biochem Biokhimiia. 2021;86(10):1301–14. 10.1134/s0006297921100114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Biagioni A, Chillà A, Andreucci E, Laurenzana A, Margheri F, Peppicelli S, Del Rosso M, Fibbi G. Type II CRISPR/Cas9 approach in the oncological therapy. J Experimental Clin Cancer Res. 2017;36:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Makarova KS, Wolf YI, Iranzo J, Shmakov SA, Alkhnbashi OS, Brouns SJ, Charpentier E, Cheng D, Haft DH, Horvath P. Evolutionary classification of CRISPR–Cas systems: a burst of class 2 and derived variants. Nat Rev Microbiol. 2020;18(2):67–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sorek R, Kunin V, Hugenholtz P. CRISPR—a widespread system that provides acquired resistance against phages in bacteria and archaea. Nat Rev Microbiol. 2008;6(3):181–6. [DOI] [PubMed] [Google Scholar]
- 25.Bhaya D, Davison M, Barrangou R. CRISPR-Cas systems in bacteria and archaea: versatile small RNAs for adaptive defense and regulation. Annu Rev Genet. 2011;45:273–97. [DOI] [PubMed] [Google Scholar]
- 26.Shin U, Brondani V. Analysis of wild type LbCpf1 protein, and PAM recognition variants, in a cellular context. Front Genet. 2021;11:571591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Amitai G, Sorek R. CRISPR–Cas adaptation: insights into the mechanism of action. Nat Rev Microbiol. 2016;14(2):67–76. [DOI] [PubMed] [Google Scholar]
- 28.Jackson SA, McKenzie RE, Fagerlund RD, Kieper SN, Fineran PC, Brouns SJ. CRISPR-Cas: adapting to change. Science. 2017;356(6333):eaal5056. [DOI] [PubMed] [Google Scholar]
- 29.Chylinski K, Le Rhun A, Charpentier E. The tracrRNA and Cas9 families of type II CRISPR-Cas immunity systems. RNA Biol. 2013;10(5):726–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hille F, Richter H, Wong SP, Bratovič M, Ressel S, Charpentier E. The biology of CRISPR-Cas: backward and forward. Cell. 2018;172(6):1239–59. [DOI] [PubMed] [Google Scholar]
- 31.Chen H, Choi J, Bailey S. Cut site selection by the two nuclease domains of the Cas9 RNA-guided endonuclease. J Biol Chem. 2014;289(19):13284–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Levy A, Goren MG, Yosef I, Auster O, Manor M, Amitai G, Edgar R, Qimron U, Sorek R. CRISPR adaptation biases explain preference for acquisition of foreign DNA. Nature. 2015;520(7548):505–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mali P, Esvelt KM, Church GM. Cas9 as a versatile tool for engineering biology. Nat Methods. 2013;10(10):957–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ma Y, Zhang L, Huang X. Genome modification by CRISPR/Cas9. FEBS J. 2014;281(23):5186–93. [DOI] [PubMed] [Google Scholar]
- 35.Pellagatti A, Dolatshad H, Valletta S, Boultwood J. Application of CRISPR/Cas9 genome editing to the study and treatment of disease. Arch Toxicol. 2015;89:1023–34. [DOI] [PubMed] [Google Scholar]
- 36.Liang F, Han M, Romanienko PJ, Jasin M. Homology-directed repair is a major double-strand break repair pathway in mammalian cells. Proc Natl Acad Sci. 1998;95(9):5172–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ran FA, Hsu PD, Lin C-Y, Gootenberg JS, Konermann S, Trevino AE, Scott DA, Inoue A, Matoba S, Zhang Y. Double nicking by RNA-guided CRISPR Cas9 for enhanced genome editing specificity. Cell. 2013;154(6):1380–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Findlay GM, Boyle EA, Hause RJ, Klein JC, Shendure J. Saturation editing of genomic regions by multiplex homology-directed repair. Nature. 2014;513(7516):120–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu J, Sareddy GR, Zhou M, Viswanadhapalli S, Li X, Lai Z, Tekmal RR, Brenner A, Vadlamudi RK. Differential effects of estrogen receptor β isoforms on glioblastoma progression. Cancer Res. 2018;78(12):3176–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hegge B, Sjøttem E, Mikkola I. Generation of a PAX6 knockout glioblastoma cell line with changes in cell cycle distribution and sensitivity to oxidative stress. BMC Cancer. 2018;18:1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Walter DM, Venancio OS, Buza EL, Tobias JW, Deshpande C, Gudiel AA, Kim-Kiselak C, Cicchini M, Yates TJ, Feldser DM. Systematic in vivo inactivation of chromatin-regulating enzymes identifies Setd2 as a potent tumor suppressor in lung adenocarcinoma. Cancer Res. 2017;77(7):1719–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.He J, Jin Y, Zhou M, Li X, Chen W, Wang Y, Gu S, Cao Y, Chu C, Liu X. Solute carrier family 35 member F2 is indispensable for papillary thyroid carcinoma progression through activation of transforming growth factor-β type I receptor/apoptosis signal‐regulating kinase 1/mitogen‐activated protein kinase signaling axis. Cancer Sci. 2018;109(3):642–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Anelli V, Villefranc JA, Chhangawala S, Martinez-McFaline R, Riva E, Nguyen A, Verma A, Bareja R, Chen Z, Scognamiglio T. Oncogenic BRAF disrupts thyroid morphogenesis and function via twist expression. Elife. 2017;6:e20728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rabaan AA, AlSaihati H, Bukhamsin R, Bakhrebah MA, Nassar MS, Alsaleh AA, Alhashem YN, Bukhamseen AY, Al-Ruhimy K, Alotaibi M. Application of CRISPR/Cas9 technology in cancer treatment: a future direction. Curr Oncol. 2023;30(2):1954–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hazafa A, Mumtaz M, Farooq MF, Bilal S, Chaudhry SN, Firdous M, Naeem H, Ullah MO, Yameen M, Mukhtiar MS. CRISPR/Cas9: a powerful genome editing technique for the treatment of cancer cells with present challenges and future directions. Life Sci. 2020;263:118525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stefanoudakis D, Kathuria-Prakash N, Sun AW, Abel M, Drolen CE, Ashbaugh C, Zhang S, Hui G, Tabatabaei YA, Zektser Y, Lopez LP, Pantuck A, Drakaki A. The potential revolution of Cancer Treatment with CRISPR Technology. Cancers (Basel). 2023;15(6). 10.3390/cancers15061813. [DOI] [PMC free article] [PubMed]
- 47.Wen L, Zhao C, Song J, Ma L, Ruan J, Xia X, Chen YE, Zhang J, Ma PX, Xu J. CRISPR/Cas9-mediated TERT disruption in cancer cells. Int J Mol Sci. 2020;21(2):653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lu Y, Xue J, Deng T, Zhou X, Yu K, Deng L, Huang M, Yi X, Liang M, Wang Y, Shen H, Tong R, Wang W, Li L, Song J, Li J, Su X, Ding Z, Gong Y, Zhu J, Wang Y, Zou B, Zhang Y, Li Y, Zhou L, Liu Y, Yu M, Wang Y, Zhang X, Yin L, Xia X, Zeng Y, Zhou Q, Ying B, Chen C, Wei Y, Li W, Mok T. Safety and feasibility of CRISPR-edited T cells in patients with refractory non-small-cell lung cancer. Nat Med. 2020;26(5):732–40. 10.1038/s41591-020-0840-5. [DOI] [PubMed] [Google Scholar]
- 49.Hughes C, Murphy A, Martin C, Sheils O, O’leary J. Molecular pathology of prostate cancer. J Clin Pathol. 2005;58(7):673–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stefanoudakis D, Kathuria-Prakash N, Sun AW, Abel M, Drolen CE, Ashbaugh C, Zhang S, Hui G, Tabatabaei YA, Zektser Y. The potential revolution of cancer treatment with CRISPR technology. Cancers. 2023;15(6):1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hååg P, Bektic J, Bartsch G, Klocker H, Eder IE. Androgen receptor down regulation by small interference RNA induces cell growth inhibition in androgen sensitive as well as in androgen independent prostate cancer cells. J Steroid Biochem Mol Biol. 2005;96(3–4):251–8. 10.1016/j.jsbmb.2005.04.029. [DOI] [PubMed] [Google Scholar]
- 52.Yu Y, Papukashvili D, Ren R, Rcheulishvili N, Feng S, Bai W, Zhang H, Xi Y, Lu X, Xing N. siRNA-based approaches for castration-resistant prostate cancer therapy targeting the androgen receptor signaling pathway. Future Oncol. 2023;19(30):2055–73. 10.2217/fon-2023-0227. [DOI] [PubMed] [Google Scholar]
- 53.He Y, Xu W, Xiao Y-T, Huang H, Gu D, Ren S. Targeting signaling pathways in prostate cancer: mechanisms and clinical trials. Signal Transduct Target Therapy. 2022;7(1):198. 10.1038/s41392-022-01042-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wei C, Wang F, Liu W, Zhao W, Yang Y, Li K, Xiao L, Shen J. CRISPR/Cas9 targeting of the androgen receptor suppresses the growth of LNCaP human prostate cancer cells. Mol Med Rep. 2018;17(2):2901–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Obinata D, Takayama K, Inoue S, Takahashi S. Exploring androgen receptor signaling pathway in prostate cancer: a path to new discoveries. International Journal of Urology; 2024. [DOI] [PubMed]
- 56.Yang Y, Mei H, Han X, Zhang X, Cheng J, Zhang Z, Wang H, Xu H. Synthetic CRISPR/dCas9-KRAB system driven by specific PSA promoter suppresses malignant biological behavior of prostate cancer cells through negative feedback inhibition of PSA expression. Cell Mol Biol Lett. 2023;28(1):96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Akbaba H, Erel-Akbaba Gla S. (2023) Design of Liposome Formulations for CRISPR/Cas9 Enzyme Immobilization: Evaluation of 5-Alpha-Reductase Enzyme Knockout for Androgenic Disorders. ACS omega 8 (48):46101–46112. [DOI] [PMC free article] [PubMed]
- 58.Zhang M, Yang J, Li F. Transcriptional and post-transcriptional controls of survivin in cancer cells: novel approaches for cancer treatment. J Exp Clin Cancer Res. 2006;25(3):391–402. [PMC free article] [PubMed] [Google Scholar]
- 59.Farhadi L, Fakhari S, Soleimani F, Jalili A. (2021) Survivin Gene disruption via CRISPR/Cas9 induces apoptosis through down-regulation of FBXO5 and RRM2 in prostate Cancer cell line PC3. Crescent J Med Biol Sci 8 (3).
- 60.Jeter CR, Liu B, Lu Y, Chao H-P, Zhang D, Liu X, Chen X, Li Q, Rycaj K, Calhoun-Davis T, Yan L, Hu Q, Wang J, Shen J, Liu S, Tang DG. NANOG reprograms prostate cancer cells to castration resistance via dynamically repressing and engaging the AR/FOXA1 signaling axis. Cell Discovery. 2016;2(1):16041. 10.1038/celldisc.2016.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kawamura N, Nimura K, Nagano H, Yamaguchi S, Nonomura N, Kaneda Y. CRISPR/Cas9-mediated gene knockout of NANOG and NANOGP8 decreases the malignant potential of prostate cancer cells. Oncotarget. 2015;6(26):22361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Driehuis E, Clevers H. (2017) CRISPR-Induced TMPRSS2-ERG gene fusions in mouse prostate organoids. JSM Biotechnol Biomedical Eng 4 (1). [PMC free article] [PubMed]
- 63.Thomas MA, Preece DM, Bentel JM. Androgen regulation of the prostatic tumour suppressor NKX3.1 is mediated by its 3’ untranslated region. Biochem J. 2010;425(3):575–83. 10.1042/bj20091109. [DOI] [PubMed] [Google Scholar]
- 64.Bowen C, Shibata M, Zhang H, Bergren SK, Shen MM, Gelmann EP. CRISPR/Cas9-Mediated point mutation in Nkx3. 1 Prolongs protein half-life and reverses effects Nkx3. 1 allelic loss. Cancer Res. 2020;80(21):4805–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Taylor BS, Schultz N, Hieronymus H, Gopalan A, Xiao Y, Carver BS, Arora VK, Kaushik P, Cerami E, Reva B, Antipin Y, Mitsiades N, Landers T, Dolgalev I, Major JE, Wilson M, Socci ND, Lash AE, Heguy A, Eastham JA, Scher HI, Reuter VE, Scardino PT, Sander C, Sawyers CL, Gerald WL. Integrative genomic profiling of human prostate cancer. Cancer Cell. 2010;18(1):11–22. 10.1016/j.ccr.2010.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lee Y-R, Chen M, Pandolfi PP. The functions and regulation of the PTEN tumour suppressor: new modes and prospects. Nat Rev Mol Cell Biol. 2018;19(9):547–62. [DOI] [PubMed] [Google Scholar]
- 67.Laplante M, Sabatini DM. mTOR signaling in growth control and disease. Cell. 2012;149(2):274–93. 10.1016/j.cell.2012.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Peterson TR, Laplante M, Thoreen CC, Sancak Y, Kang SA, Kuehl WM, Gray NS, Sabatini DM. DEPTOR is an mTOR inhibitor frequently overexpressed in multiple myeloma cells and required for their survival. Cell. 2009;137(5):873–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chen X, Xiong X, Cui D, Yang F, Wei D, Li H, Shu J, Bi Y, Dai X, Gong L. DEPTOR is an in vivo tumor suppressor that inhibits prostate tumorigenesis via the inactivation of mTORC1/2 signals. Oncogene. 2020;39(7):1557–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhen S, Takahashi Y, Narita S, Yang Y-C, Li X. Targeted delivery of CRISPR/Cas9 to prostate cancer by modified gRNA using a flexible aptamer-cationic liposome. Oncotarget. 2017;8(6):9375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Riedel M, Cai H, Stoltze IC, Vendelbo MH, Wagner EF, Bakiri L, Thomsen MK. Targeting AP-1 transcription factors by CRISPR in the prostate. Oncotarget. 2021;12(19):1956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ye R, Pi M, Cox JV, Nishimoto SK, Quarles LD. CRISPR/Cas9 targeting of GPRC6A suppresses prostate cancer tumorigenesis in a human xenograft model. J Experimental Clin Cancer Res. 2017;36:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Park JJ, Kim JE, Jeon Y, Lee MR, Choi JY, Song BR, Park JW, Kang MJ, Choi HJ, Bae SJ. Deletion of NKX3. 1 via CRISPR/Cas9 induces prostatic intraepithelial neoplasia in C57BL/6 mice. Technol Cancer Res Treat. 2020;19:1533033820964425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gao S, Wang S, Zhao Z, Zhang C, Liu Z, Ye P, Xu Z, Yi B, Jiao K, Naik GA. TUBB4A interacts with MYH9 to protect the nucleus during cell migration and promotes prostate cancer via GSK3β/β-catenin signalling. Nat Commun. 2022;13(1):2792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wang C, Ke Y, Liu S, Pan S, Liu Z, Zhang H, Fan Z, Zhou C, Liu J, Wang F. Ectopic fibroblast growth factor receptor 1 promotes inflammation by promoting nuclear factor-κB signaling in prostate cancer cells. J Biol Chem. 2018;293(38):14839–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kardooni H, Gonzalez-Gualda E, Stylianakis E, Saffaran S, Waxman J, Kypta RM. CRISPR-mediated reactivation of DKK3 expression attenuates TGF-β signaling in prostate cancer. Cancers. 2018;10(6):165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rahimi S, Roushandeh AM, Ebrahimi A, Samadani AA, Kuwahara Y, Roudkenar MH. CRISPR/Cas9-mediated knockout of Lcn2 effectively enhanced CDDP-induced apoptosis and reduced cell migration capacity of PC3 cells. Life Sci. 2019;231:116586. [DOI] [PubMed] [Google Scholar]
- 78.Yang Y, Feng Q, Hu K, Cheng F. Using CRISPRa and CRISPRi technologies to study the biological functions of ITGB5, TIMP1, and TMEM176B in prostate cancer cells. Front Mol Biosci. 2021;8:676021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rushworth LK, Harle V, Repiscak P, Clark W, Shaw R, Hall H, Bushell M, Leung HY, Patel R. (2020) In vivo CRISPR/Cas9 knockout screen: TCEAL1 silencing enhances docetaxel efficacy in prostate cancer. Life Sci Alliance 3 (12). [DOI] [PMC free article] [PubMed]
- 80.Cai H, Zhang B, Ahrenfeldt J, Joseph JV, Riedel M, Gao Z, Thomsen SK, Christensen DS, Bak RO, Hager H, Vendelbo MH, Gao X, Birkbak N, Thomsen MK. CRISPR/Cas9 model of prostate cancer identifies Kmt2c deficiency as a metastatic driver by Odam/Cabs1 gene cluster expression. Nat Commun. 2024;15(1):2088. 10.1038/s41467-024-46370-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Arriaga JM, Ronaldson-Bouchard K, Picech F, Nunes de Almeida F, Afari S, Chhouri H, Vunjak-Novakovic G, Abate-Shen C. In vivo genome-wide CRISPR screening identifies CITED2 as a driver of prostate cancer bone metastasis. Oncogene. 2024;43(17):1303–15. 10.1038/s41388-024-02995-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Dorff TB, Blanchard MS, Adkins LN, Luebbert L, Leggett N, Shishido SN, Macias A, Del Real MM, Dhapola G, Egelston C, Murad JP, Rosa R, Paul J, Chaudhry A, Martirosyan H, Gerdts E, Wagner JR, Stiller T, Tilakawardane D, Pal S, Martinez C, Reiter RE, Budde LE, D’Apuzzo M, Kuhn P, Pachter L, Forman SJ, Priceman SJ. PSCA-CAR T cell therapy in metastatic castration-resistant prostate cancer: a phase 1 trial. Nat Med. 2024;30(6):1636–44. 10.1038/s41591-024-02979-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wei W, Chen ZN, Wang K. CRISPR/Cas9: a powerful strategy to improve CAR-T cell persistence. Int J Mol Sci. 2023;24(15). 10.3390/ijms241512317. [DOI] [PMC free article] [PubMed]
- 84.Zhou J, Bobbin ML, Burnett JC, Rossi JJ. Current progress of RNA aptamer-based therapeutics. Front Genet. 2012;3:234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sheridan C. The world’s first CRISPR therapy is approved: who will receive it? Nat Biotechnol. 2024;42(1):3–4. 10.1038/d41587-023-00016-6. [DOI] [PubMed] [Google Scholar]
- 86.Li Y, Yang R, Henzler CM, Ho Y, Passow C, Auch B, Carreira S, Nava Rodrigues D, Bertan C, Hwang TH. Diverse AR gene rearrangements mediate resistance to androgen receptor inhibitors in metastatic prostate cancer. Clin Cancer Res. 2020;26(8):1965–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bluemn EG, Coleman IM, Lucas JM, Coleman RT, Hernandez-Lopez S, Tharakan R, Bianchi-Frias D, Dumpit RF, Kaipainen A, Corella AN. Androgen receptor pathway-independent prostate cancer is sustained through FGF signaling. Cancer Cell. 2017;32(4):474–89. e476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Deng G, Wang R, Sun Y, Huang C-P, Yeh S, You B, Feng C, Li G, Ma S, Chang C. Targeting androgen receptor (AR) with antiandrogen Enzalutamide increases prostate cancer cell invasion yet decreases bladder cancer cell invasion via differentially altering the AR/circRNA-ARC1/miR-125b-2-3p or miR-4736/PPARγ/MMP-9 signals. Cell Death Differ. 2021;28(7):2145–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Brennen WN, Zhu Y, Coleman IM, Dalrymple SL, Antony L, Patel RA, Hanratty B, Chikarmane R, Meeker AK, Zheng SL. Resistance to androgen receptor signaling inhibition does not necessitate development of neuroendocrine prostate cancer. JCI Insight. 2021;6:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Li Q, Deng Q, Chao H-P, Liu X, Lu Y, Lin K, Liu B, Tang GW, Zhang D, Tracz A. Linking prostate cancer cell AR heterogeneity to distinct castration and enzalutamide responses. Nat Commun. 2018;9(1):3600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Giambartolomei C, Seo J-H, Schwarz T, Freund MK, Johnson RD, Spisak S, Baca SC, Gusev A, Mancuso N, Pasaniuc B. H3K27ac HiChIP in prostate cell lines identifies risk genes for prostate cancer susceptibility. Am J Hum Genet. 2021;108(12):2284–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Naeem AA, Abdulsamad SA, Zeng H, He G, Jin X, Zhang J, Alenezi BT, Ma H, Rudland PS, Ke Y. FABP5 can substitute for androgen receptor in malignant progression of prostate cancer cells. Int J Oncol. 2024;64(2):1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kounatidou E, Nakjang S, McCracken SRC, Dehm SM, Robson CN, Jones D, Gaughan L. A novel CRISPR-engineered prostate cancer cell line defines the AR-V transcriptome and identifies PARP inhibitor sensitivities. Nucleic Acids Res. 2019;47(11):5634–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Zhu Y, Dalrymple SL, Coleman I, Zheng SL, Xu J, Hooper JE, Antonarakis ES, De Marzo AM, Meeker AK, Nelson PS. Role of androgen receptor splice variant-7 (AR-V7) in prostate cancer resistance to 2nd-generation androgen receptor signaling inhibitors. Oncogene. 2020;39(45):6935–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Shah N, Kesten N, Font-Tello A, Chang ME, Vadhi R, Lim K, Flory MR, Cejas P, Mohammed H, Long HW. ERG-mediated coregulator complex formation maintains androgen receptor signaling in prostate cancer. Cancer Res. 2020;80(21):4612–9. [DOI] [PubMed] [Google Scholar]
- 96.Yang X, Zhang Q, Li S, Devarajan R, Luo B, Tan Z, Wang Z, Giannareas N, Wenta T, Ma W. GATA2 co-opts TGFβ1/SMAD4 oncogenic signaling and inherited variants at 6q22 to modulate prostate cancer progression. J Experimental Clin Cancer Res. 2023;42(1):198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lee E, Wongvipat J, Choi D, Wang P, Lee YS, Zheng D, Watson PA, Gopalan A, Sawyers CL. GREB1 amplifies androgen receptor output in human prostate cancer and contributes to antiandrogen resistance. Elife. 2019;8:e41913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Palit SA, Vis D, Stelloo S, Lieftink C, Prekovic S, Bekers E, Hofland I, Šuštić T, Wolters L, Beijersbergen R. TLE3 loss confers AR inhibitor resistance by facilitating GR-mediated human prostate cancer cell growth. Elife. 2019;8:e47430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Vatapalli R, Sagar V, Rodriguez Y, Zhao J, Unno K, Pamarthy S, Lysy B, Anker J, Han H, Yoo Y. Histone methyltransferase DOT1L coordinates AR and MYC stability in prostate cancer. Nat Commun. 2020;11(1):4153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kawamura N, Nimura K, Saga K, Ishibashi A, Kitamura K, Nagano H, Yoshikawa Y, Ishida K, Nonomura N, Arisawa M. SF3B2-mediated RNA splicing drives human prostate cancer progression. Cancer Res. 2019;79(20):5204–17. [DOI] [PubMed] [Google Scholar]
- 101.Atobatele AG, Tonoli E, Vadakekolathu J, Savoca MP, Barr M, Kataria Y, Rossanese M, Burhan I, McArdle S, Caccamo D. Canonical and truncated transglutaminase-2 regulate mucin-1 expression and androgen independency in prostate cancer cell lines. Cell Death Dis. 2023;14(5):317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Rasool Ru, O’Connor CM, Das CK, Alhusayan M, Verma BK, Islam S, Frohner IE, Deng Q, Mitchell-Velasquez E, Sangodkar J. Loss of LCMT1 and biased protein phosphatase 2A heterotrimerization drive prostate cancer progression and therapy resistance. Nat Commun. 2023;14(1):5253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Gui B, Gui F, Takai T, Feng C, Bai X, Fazli L, Dong X, Liu S, Zhang X, Zhang W. Selective targeting of PARP-2 inhibits androgen receptor signaling and prostate cancer growth through disruption of FOXA1 function. Proc Natl Acad Sci. 2019;116(29):14573–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Haldrup J, Weiss S, Schmidt L, Sørensen KD. Investigation of enzalutamide, docetaxel, and cabazitaxel resistance in the castration resistant prostate cancer cell line C4 using genome-wide CRISPR/Cas9 screening. Sci Rep. 2023;13(1):9043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Mahajan K, Malla P, Lawrence HR, Chen Z, Kumar-Sinha C, Malik R, Shukla S, Kim J, Coppola D, Lawrence NJ. ACK1/TNK2 regulates histone H4 Tyr88-phosphorylation and AR gene expression in castration-resistant prostate cancer. Cancer Cell. 2017;31(6):790–803. e798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Zhang Z, Zhou N, Huang J, Ho T-T, Zhu Z, Qiu Z, Zhou X, Bai C, Wu F, Xu M. Regulation of androgen receptor splice variant AR3 by PCGEM1. Oncotarget. 2016;7(13):15481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lin C, Blessing AM, Pulliam TL, Shi Y, Wilkenfeld SR, Han JJ, Murray MM, Pham AH, Duong K, Brun SN. Inhibition of CAMKK2 impairs autophagy and castration-resistant prostate cancer via suppression of AMPK-ULK1 signaling. Oncogene. 2021;40(9):1690–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Penfold L, Woods A, Muckett P, Nikitin AY, Kent TR, Zhang S, Graham R, Pollard A, Carling D. CAMKK2 promotes prostate cancer independently of AMPK via increased lipogenesis. Cancer Res. 2018;78(24):6747–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lin C, Blessing AM, Pulliam TL, Shi Y, Wilkenfeld SR, Han JJ, Murray MM, Pham AH, Duong K, Brun SN, Shaw RJ, Ittmann MM, Frigo DE. Inhibition of CAMKK2 impairs autophagy and castration-resistant prostate cancer via suppression of AMPK-ULK1 signaling. Oncogene. 2021;40(9):1690–705. 10.1038/s41388-021-01658-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Williams A, Gutgesell L, de Wet L, Selman P, Dey A, Avineni M, Kapoor I, Mendez M, Brown R, Lamperis S. SOX2 expression in prostate cancer drives resistance to nuclear hormone receptor signaling inhibition through the WEE1/CDK1 signaling axis. Cancer Lett. 2023;565:216209. [DOI] [PubMed] [Google Scholar]
- 111.Cinar B, Al-Mathkour MM, Khan SA, Moreno CS. Androgen attenuates the inactivating phospho–Ser-127 modification of yes-associated protein 1 (YAP1) and promotes YAP1 nuclear abundance and activity. J Biol Chem. 2020;295(25):8550–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Mukhopadhyay C, Yang C, Xu L, Liu D, Wang Y, Huang D, Deonarine LD, Cyrta J, Davicioni E, Sboner A. G3BP1 inhibits Cul3SPOP to amplify AR signaling and promote prostate cancer. Nat Commun. 2021;12(1):6662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Davies A, Nouruzi S, Ganguli D, Namekawa T, Thaper D, Linder S, Karaoğlanoğlu F, Omur ME, Kim S, Kobelev M. An androgen receptor switch underlies lineage infidelity in treatment-resistant prostate cancer. Nat Cell Biol. 2021;23(9):1023–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Zhang Q, Kuang G, He S, Liu S, Lu H, Li X, Zhou D, Huang Y. Chain-shattering pt (IV)-backboned polymeric nanoplatform for efficient CRISPR/Cas9 gene editing to enhance synergistic cancer therapy. Nano Res. 2021;14:601–10. [Google Scholar]
- 115.Yuan H, Han Y, Wang X, Li N, Liu Q, Yin Y, Wang H, Pan L, Li L, Song K, Qiu T, Pan Q, Chen Q, Zhang G, Zang Y, Tan M, Zhang J, Li Q, Wang X, Jiang J, Qin J. SETD2 restricts prostate Cancer metastasis by integrating EZH2 and AMPK Signaling pathways. Cancer Cell. 2020;38(3):350–e365357. 10.1016/j.ccell.2020.05.022. [DOI] [PubMed] [Google Scholar]
- 116.Burleson M, Deng JJ, Qin T, Duong TM, Yan Y, Gu X, Das D, Easley A, Liss MA, Yew PR. GLI3 is stabilized by SPOP mutations and promotes castration resistance via functional cooperation with androgen receptor in prostate cancer. Mol Cancer Res. 2022;20(1):62–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Wang X, Jin J, Wan F, Zhao L, Chu H, Chen C, Liao G, Liu J, Yu Y, Teng H. AMPK promotes SPOP-mediated NANOG degradation to regulate prostate cancer cell stemness. Dev Cell. 2019;48(3):345–60. e347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Shi Q, Zhu Y, Ma J, Chang K, Ding D, Bai Y, Gao K, Zhang P, Mo R, Feng K. Prostate Cancer-associated SPOP mutations enhance cancer cell survival and docetaxel resistance by upregulating Caprin1-dependent stress granule assembly. Mol Cancer. 2019;18:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Jin X, Qing S, Li Q, Zhuang H, Shen L, Li J, Qi H, Lin T, Lin Z, Wang J. Prostate cancer-associated SPOP mutations lead to genomic instability through disruption of the SPOP–HIPK2 axis. Nucleic Acids Res. 2021;49(12):6788–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Shi Q, Jin X, Zhang P, Li Q, Lv Z, Ding Y, He H, Wang Y, He Y, Zhao X. SPOP mutations promote p62/SQSTM1-dependent autophagy and Nrf2 activation in prostate cancer. Cell Death Differ. 2022;29(6):1228–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Albayrak G, Konac E, Ugras Dikmen A, Bilen CY. FOXA1 knock-out via CRISPR/Cas9 altered Casp-9, Bax, CCND1, CDK4, and fibronectin expressions in LNCaP cells. Experimental Biology Med. 2018;243(12):990–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zhou S, Hawley JR, Soares F, Grillo G, Teng M, Madani Tonekaboni SA, Hua JT, Kron KJ, Mazrooei P, Ahmed M. Noncoding mutations target cis-regulatory elements of the FOXA1 plexus in prostate cancer. Nat Commun. 2020;11(1):441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Parolia A, Cieslik M, Chu S-C, Xiao L, Ouchi T, Zhang Y, Wang X, Vats P, Cao X, Pitchiaya S. Distinct structural classes of activating FOXA1 alterations in advanced prostate cancer. Nature. 2019;571(7765):413–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Baca SC, Takeda DY, Seo J-H, Hwang J, Ku SY, Arafeh R, Arnoff T, Agarwal S, Bell C, O’connor E. Reprogramming of the FOXA1 cistrome in treatment-emergent neuroendocrine prostate cancer. Nat Commun. 2021;12(1):1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Song B, Park S-H, Zhao JC, Fong K-W, Li S, Lee Y, Yang YA, Sridhar S, Lu X, Abdulkadir SA. Targeting FOXA1-mediated repression of TGF-β signaling suppresses castration-resistant prostate cancer progression. J Clin Investig. 2019;129(2):569–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Adams EJ, Karthaus WR, Hoover E, Liu D, Gruet A, Zhang Z, Cho H, DiLoreto R, Chhangawala S, Liu Y. FOXA1 mutations alter pioneering activity, differentiation and prostate cancer phenotypes. Nature. 2019;571(7765):408–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Cai H, Agersnap SN, Sjøgren A, Simonsen MK, Blaavand MS, Jensen UV, Thomsen MK. In vivo application of CRISPR/Cas9 revealed implication of foxa1 and foxp1 in prostate cancer proliferation and epithelial plasticity. Cancers. 2022;14(18):4381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Boysen G, Rodrigues DN, Rescigno P, Seed G, Dolling D, Riisnaes R, Crespo M, Zafeiriou Z, Sumanasuriya S, Bianchini D. SPOP-mutated/CHD1-deleted lethal prostate cancer and abiraterone sensitivity. Clin Cancer Res. 2018;24(22):5585–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Shenoy T, Boysen G, Wang M, Xu Q, Guo W, Koh F, Wang C, Zhang L, Wang Y, Gil V. CHD1 loss sensitizes prostate cancer to DNA damaging therapy by promoting error-prone double-strand break repair. Ann Oncol. 2017;28(7):1495–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Chatterjee P, Schweizer MT, Lucas JM, Coleman I, Nyquist MD, Frank SB, Tharakan R, Mostaghel E, Luo J, Pritchard CC. Supraphysiological androgens suppress prostate cancer growth through androgen receptor–mediated DNA damage. J Clin Investig. 2019;129(10):4245–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Chakraborty G, Patail NK, Hirani R, Nandakumar S, Mazzu YZ, Yoshikawa Y, Atiq M, Jehane LE, Stopsack KH, Lee G-SM. Attenuation of SRC kinase activity augments parp inhibitor–mediated synthetic lethality in BRCA2-altered prostate tumors. Clin Cancer Res. 2021;27(6):1792–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Chakraborty G, Armenia J, Mazzu YZ, Nandakumar S, Stopsack KH, Atiq MO, Komura K, Jehane L, Hirani R, Chadalavada K. Significance of BRCA2 and RB1 co-loss in aggressive prostate cancer progression. Clin Cancer Res. 2020;26(8):2047–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Nyquist MD, Corella A, Coleman I, De Sarkar N, Kaipainen A, Ha G, Gulati R, Ang L, Chatterjee P, Lucas J, Pritchard C, Risbridger G, Isaacs J, Montgomery B, Morrissey C, Corey E, Nelson PS. Combined TP53 and RB1 loss promotes prostate Cancer Resistance to a spectrum of therapeutics and confers vulnerability to replication stress. Cell Rep. 2020;31(8):107669. 10.1016/j.celrep.2020.107669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Nerlakanti N, Yao J, Nguyen DT, Patel AK, Eroshkin AM, Lawrence HR, Ayaz M, Kuenzi BM, Agarwal N, Chen Y. Targeting the BRD4-HOXB13 coregulated transcriptional networks with bromodomain-kinase inhibitors to suppress metastatic castration-resistant prostate cancer. Mol Cancer Ther. 2018;17(12):2796–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.VanOpstall C, Perike S, Brechka H, Gillard M, Lamperis S, Zhu B, Brown R, Bhanvadia R, Vander Griend DJ. MEIS-mediated suppression of human prostate cancer growth and metastasis through HOXB13-dependent regulation of proteoglycans. Elife. 2020;9:e53600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Wei Z, Wang S, Xu Y, Wang W, Soares F, Ahmed M, Su P, Wang T, Orouji E, Xu X. MYC reshapes CTCF-mediated chromatin architecture in prostate cancer. Nat Commun. 2023;14(1):1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Siddique AB, Ebrahim HY, Tajmim A, King JA, Abdelwahed KS, Abd Elmageed ZY, El Sayed KA. Oleocanthal attenuates metastatic castration-resistant prostate cancer progression and recurrence by targeting SMYD2. Cancers. 2022;14(14):3542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Li X, Wang Y, Deng S, Zhu G, Wang C, Johnson NA, Zhang Z, Tirado CR, Xu Y, Metang LA. Loss of SYNCRIP unleashes APOBEC-driven mutagenesis, tumor heterogeneity, and AR-targeted therapy resistance in prostate cancer. Cancer Cell. 2023;41(8):1427–49. e1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Ho T-T, Huang J, Zhou N, Zhang Z, Koirala P, Zhou X, Wu F, Ding X, Mo Y-Y. Regulation of PCGEM1 by p54/nrb in prostate cancer. Sci Rep. 2016;6(1):34529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Linder S, Hoogstraat M, Stelloo S, Eickhoff N, Schuurman K, de Barros H, Alkemade M, Bekers EM, Severson TM, Sanders J. Drug-induced epigenomic plasticity reprograms circadian rhythm regulation to drive prostate cancer toward androgen independence. Cancer Discov. 2022;12(9):2074–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Wang T, Sarwar M, Whitchurch JB, Collins HM, Green T, Semenas J, Ali A, Roberts CJ, Morris RD, Hubert M. PIP5K1α is required for promoting tumor progression in castration-resistant prostate cancer. Front cell Dev Biology. 2022;10:798590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Chen K, Xu H, Zhao J. (2019) Bloom syndrome protein activates AKT and PRAS40 in prostate cancer cells. Oxidative Medicine and Cellular Longevity 2019 (1):3685817. [DOI] [PMC free article] [PubMed]
- 143.Xu H, Li S, Sun Y, Xu L, Hong X, Wang Z, Hu H. ELOVL5-mediated long chain fatty acid elongation contributes to enzalutamide resistance of prostate cancer. Cancers. 2021;13(16):3957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Choi SY, Jeon JM, Na AY, Kwon OK, Bang IH, Ha Y-S, Bae EJ, Park B-H, Lee EH, Kwon TG. SIRT5 directly inhibits the pi3k/akt pathway in prostate cancer cell lines. Cancer Genomics Proteomics. 2022;19(1):50–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Kwon OK, Bang IH, Choi SY, Jeon JM, Na A-Y, Gao Y, Cho SS, Ki SH, Choe Y, Lee JN. LDHA desuccinylase sirtuin 5 as a novel cancer metastatic stimulator in aggressive prostate cancer. Genom Proteom Bioinform. 2023;21(1):177–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Su B, Zhang L, Zhuang W, Zhang W, Chen X. Knockout of Akt1/2 suppresses the metastasis of human prostate cancer cells CWR22rv1 in vitro and in vivo. J Cell Mol Med. 2021;25(3):1546–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Wang Z, Gao S, Han D, Han W, Li M, Cai C. LSD1 activates PI3K/AKT signaling through regulating p85 expression in prostate cancer cells. Front Oncol. 2019;9:721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Wang Z, Xu D, Ding H-F, Kim J, Zhang J, Hai T, Yan C. Loss of ATF3 promotes akt activation and prostate cancer development in a pten knockout mouse model. Oncogene. 2015;34(38):4975–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Wang Z, Hulsurkar M, Zhuo L, Xu J, Yang H, Naderinezhad S, Wang L, Zhang G, Ai N, Li L. CKB inhibits epithelial-mesenchymal transition and prostate cancer progression by sequestering and inhibiting AKT activation. Neoplasia. 2021;23(11):1147–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Wu R-C, Young I-C, Chen Y-F, Chuang S-T, Toubaji A, Wu M-Y. Identification of the PTEN-ARID4B-PI3K pathway reveals the dependency on ARID4B by PTEN-deficient prostate cancer. Nat Commun. 2019;10(1):4332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Caromile LA, Dortche K, Rahman MM, Grant CL, Stoddard C, Ferrer FA, Shapiro LH. PSMA redirects cell survival signaling from the MAPK to the PI3K-AKT pathways to promote the progression of prostate cancer. Sci Signal. 2017;10(470):eaag3326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Galbraith LC, Mui E, Nixon C, Hedley A, Strachan D, MacKay G, Sumpton D, Sansom OJ, Leung HY, Ahmad I. PPAR-gamma induced AKT3 expression increases levels of mitochondrial biogenesis driving prostate cancer. Oncogene. 2021;40(13):2355–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Mao N, Zhang Z, Lee YS, Choi D, Rivera AA, Li D, Lee C, Haywood S, Chen X, Chang Q. Defining the therapeutic selective dependencies for distinct subtypes of PI3K pathway-altered prostate cancers. Nat Commun. 2021;12(1):5053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Takao A, Yoshikawa K, Karnan S, Ota A, Uemura H, De Velasco MA, Kura Y, Suzuki S, Ueda R, Nishino T. Generation of PTEN–knockout (–/–) murine prostate cancer cells using the CRISPR/Cas9 system and comprehensive gene expression profiling. Oncol Rep. 2018;40(5):2455–66. [DOI] [PubMed] [Google Scholar]
- 155.Riedel M, Berthelsen MF, Cai H, Haldrup J, Borre M, Paludan SR, Hager H, Vendelbo MH, Wagner EF, Bakiri L. In vivo CRISPR inactivation of Fos promotes prostate cancer progression by altering the associated AP-1 subunit Jun. Oncogene. 2021;40(13):2437–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Wenta T, Schmidt A, Zhang Q, Devarajan R, Singh P, Yang X, Ahtikoski A, Vaarala M, Wei G-H, Manninen A. Disassembly of α6β4-mediated hemidesmosomal adhesions promotes tumorigenesis in PTEN-negative prostate cancer by targeting plectin to focal adhesions. Oncogene. 2022;41(30):3804–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Li N, Xue W, Yuan H, Dong B, Ding Y, Liu Y, Jiang M, Kan S, Sun T, Ren J. AKT-mediated stabilization of histone methyltransferase WHSC1 promotes prostate cancer metastasis. J Clin Investig. 2017;127(4):1284–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Caggia S, Chunduri H, Millena AC, Perkins JN, Venugopal SV, Vo BT, Li C, Tu Y, Khan SA. Novel role of Giα2 in cell migration: downstream of PI3-kinase–AKT and Rac1 in prostate cancer cells. J Cell Physiol. 2019;234(1):802–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Li G, Kanagasabai T, Lu W, Zou MR, Zhang S-M, Celada SI, Izban MG, Liu Q, Lu T, Ballard BR. KDM5B is essential for the hyperactivation of PI3K/AKT signaling in prostate tumorigenesis. Cancer Res. 2020;80(21):4633–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Zhang L, Wang P, Feng Q, Wang N, Chen Z, Huang Y, Zheng W, Jiang X. Lipid nanoparticle-mediated efficient delivery of CRISPR/Cas9 for tumor therapy. NPG Asia Mater. 2017;9(10):e441–441. [Google Scholar]
- 161.Rafiei S, Fitzpatrick K, Liu D, Cai M-Y, Elmarakeby HA, Park J, Ricker C, Kochupurakkal BS, Choudhury AD, Hahn WC. ATM loss confers greater sensitivity to ATR inhibition than PARP inhibition in prostate cancer. Cancer Res. 2020;80(11):2094–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Yin Y, Xu L, Chang Y, Zeng T, Chen X, Wang A, Groth J, Foo W-C, Liang C, Hu H. N-Myc promotes therapeutic resistance development of neuroendocrine prostate cancer by differentially regulating miR-421/ATM pathway. Mol Cancer. 2019;18:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Neeb A, Herranz N, Arce-Gallego S, Miranda S, Buroni L, Yuan W, Athie A, Casals T, Carmichael J, Rodrigues DN. Advanced prostate cancer with ATM loss: PARP and ATR inhibitors. Eur Urol. 2021;79(2):200–11. [DOI] [PubMed] [Google Scholar]
- 164.Arai S, Jonas O, Whitman MA, Corey E, Balk SP, Chen S. Tyrosine kinase inhibitors increase MCL1 degradation and in combination with BCLXL/BCL2 inhibitors drive prostate cancer apoptosis. Clin Cancer Res. 2018;24(21):5458–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Sawada Y, Kikugawa T, Iio H, Sakakibara I, Yoshida S, Ikedo A, Yanagihara Y, Saeki N, Győrffy B, Kishida T. GPRC5A facilitates cell proliferation through cell cycle regulation and correlates with bone metastasis in prostate cancer. Int J Cancer. 2020;146(5):1369–82. [DOI] [PubMed] [Google Scholar]
- 166.Li N, Liu Q, Han Y, Pei S, Cheng B, Xu J, Miao X, Pan Q, Wang H, Guo J. ARID1A loss induces polymorphonuclear myeloid-derived suppressor cell chemotaxis and promotes prostate cancer progression. Nat Commun. 2022;13(1):7281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Brown NE, Paluch AM, Nashu MA, Komurov K, Waltz SE. Tumor cell autonomous RON receptor expression promotes prostate cancer growth under conditions of androgen deprivation. Neoplasia. 2018;20(9):917–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Brown NE, Jones A, Hunt BG, Waltz SE. Prostate tumor RON receptor signaling mediates macrophage recruitment to drive androgen deprivation therapy resistance through Gas6-mediated Axl and RON signaling. Prostate. 2022;82(15):1422–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Sorrentino C, D’Antonio L, Ciummo SL, Fieni C, Landuzzi L, Ruzzi F, Vespa S, Lanuti P, Lotti LV, Lollini PL. CRISPR/Cas9-mediated deletion of Interleukin-30 suppresses IGF1 and CXCL5 and boosts SOCS3 reducing prostate cancer growth and mortality. J Hematol Oncol. 2022;15(1):145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Sorrentino C, Ciummo SL, Cipollone G, Caputo S, Bellone M, Di Carlo E. Interleukin-30/IL27p28 shapes prostate cancer stem-like cell behavior and is critical for tumor onset and metastasization. Cancer Res. 2018;78(10):2654–68. [DOI] [PubMed] [Google Scholar]
- 171.Chang M, He Y, Liu C, Lin R, Huang X, Liang D, Zhang J, Lu Y. Downregulation of SEPTIN5 inhibits prostate cancer progression by increasing CD8 + T cell infiltration. Int J Biol Sci. 2022;18(16):6035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Muresan XM, Slabáková E, Procházková J, Drápela S, Fedr R, Pícková M, Vacek O, Víchová R, Suchánková T, Bouchal J. Toll-like receptor 3 overexpression induces invasion of prostate cancer cells, whereas its activation triggers apoptosis. Am J Pathol. 2022;192(9):1321–35. [DOI] [PubMed] [Google Scholar]
- 173.Lopez-Bujanda ZA, Haffner MC, Chaimowitz MG, Chowdhury N, Venturini NJ, Patel RA, Obradovic A, Hansen CS, Jacków J, Maynard JP. Castration-mediated IL-8 promotes myeloid infiltration and prostate cancer progression. Nat cancer. 2021;2(8):803–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Liedtke V, Rose L, Hiemann R, Nasser A, Rödiger S, Bonaventura A, Winkler L, Sowa M, Stöckle M, Schierack P. Over-expression of LEDGF/p75 in HEp-2 cells enhances autoimmune IgG response in patients with Benign Prostatic Hyperplasia—A Novel Diagnostic Approach with Therapeutic Consequence? Int J Mol Sci. 2023;24(7):6166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Pavan ICB, Basei FL, Severino MB, Rosa e Silva I, Issayama LK, Mancini MCS, Góis MM, da Silva LGS, Bezerra RMN, Simabuco FM. NEK6 regulates redox balance and DNA damage response in DU-145 prostate cancer cells. Cells. 2023;12(2):256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Zhang Y, Zhu S, Du Y, Xu F, Sun W, Xu Z, Wang X, Qian P, Zhang Q, Feng J. RelB upregulates PD-L1 and exacerbates prostate cancer immune evasion. J Experimental Clin Cancer Res. 2022;41(1):66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Chen B, Liu J, Ho T, Ding X, Mo Y. ERK-mediated NF-κB activation through ASIC1 in response to acidosis. Oncogenesis. 2016;5(12):e279–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Garcia-Garcia S, Rodrigo-Faus M, Fonseca N, Manzano S, Győrffy B, Ocaña A, Bragado P, Porras A, Gutierrez-Uzquiza A. HGK promotes metastatic dissemination in prostate cancer. Sci Rep. 2021;11(1):12287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Li Y, He Y, Butler W, Xu L, Chang Y, Lei K, Zhang H, Zhou Y, Gao AC, Zhang Q. Targeting cellular heterogeneity with CXCR2 blockade for the treatment of therapy-resistant prostate cancer. Sci Transl Med. 2019;11(521):eaax0428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Hoy JJ, Kallifatidis G, Smith DK, Lokeshwar BL. Inhibition of androgen receptor promotes CXC-chemokine receptor 7-mediated prostate cancer cell survival. Sci Rep. 2017;7(1):3058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Rafiei S, Gui B, Wu J, Liu XS, Kibel AS, Jia L. Targeting the MIF/CXCR7/AKT signaling pathway in castration-resistant prostate cancer. Mol Cancer Res. 2019;17(1):263–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Li S, Fong K-w, Gritsina G, Zhang A, Zhao JC, Kim J, Sharp A, Yuan W, Aversa C, Yang XJ. Activation of MAPK signaling by CXCR7 leads to enzalutamide resistance in prostate cancer. Cancer Res. 2019;79(10):2580–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.