Abstract
Background
Chlamydia trachomatis (CT) and Neisseria gonorrhoeae (NG) are widespread, treatable sexually transmitted infections (STIs) of global significance, affecting millions annually. Left untreated, they pose significant risks, including pelvic inflammatory disease (PID), infertility, and complications during pregnancy. The U.S. Centers for Disease Control recommends annual chlamydial screening for sexually active women to address these risks. Responding to this global challenge, the World Health Organization (WHO) has formulated a global health sector strategy on sexually transmitted infections, outlining priority actions to strengthen STI responses in countries. However, STI epidemiological studies encounter challenges in developing nations like Egypt due to socio-cultural factors, poverty, and limited diagnostic facilities. In Egypt, STI diagnosis primarily relies on clinical presentations, lacking structured screening programs for CT and NG. This study’s main objective is to estimate the prevalence of Chlamydial and gonorrheal infections, advocating for supportive STI strategies in Egypt. Additionally, the study aims to provide a foundation for national prevalence estimates of CT and NG infections.
Methods
A cross-sectional study encompassed five antenatal clinics in different regions of Egypt. A total of 1040 pregnant women attending these clinics were consecutively sampled. Data collection involved structured questionnaires, and urine samples were subjected to the GeneXpert CT/NG qualitative real-time PCR test.
Results
The prevalence of CT infections was 0.29% (95% CI, 0.10–0.86%), with no detected NG infections. The three CT-positive cases were distributed across different recruitment centers, with no statistically significant differences observed between infected and non-infected participants. Notably, 40.3% of recruited women reported gynecological symptoms, primarily discharge. Additionally, 9.6% had undergone previous testing for sexually transmitted infections, with 8.2% receiving positive results.
Conclusions
This study provides valuable data on the prevalence of CT and NG infections among pregnant women attending ANC clinics in Egypt. The findings underscore the importance of ongoing surveillance, routine screening, and targeted interventions to ensure the reproductive health and well-being of pregnant women and their infants. Further research is warranted to explore the broader implications of STIs in different populations and to inform evidence-based guidelines for screening and management in diverse settings. Trial registration: IRB no.: 17,400,017; WHO ERC Protocol Id. A66005.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-20239-9.
Keywords: Sexually transmitted infections (STIs), Chlamydia trachomatis, Neisseria gonorrhoeae, GeneXpert CT/NG
Background
Chlamydia trachomatis (CT) and Neisseria gonorrhoeae (NG) infections represent prevalent, curable sexually transmitted infections (STIs) globally [1, 2], infecting an estimated 129 million and 82 million people, respectively, in 2020 [3]. Both infections, often asymptomatic, can lead to serious reproductive health complications, including pelvic inflammatory disease (PID), which is a significant cause of infertility, ectopic pregnancy, and chronic pelvic pain in women [1]. As with other inflammatory STIs, CT and NG infections can facilitate the transmission of HIV infection [4]. Additionally, pregnant women with CT may transmit the infection to their infants during pregnancy, leading to premature birth and placental insufficiency. It may lead to ophthalmia neonatorum during delivery, leading to blindness and pneumonia [5]. Due to the significant health challenges and potential dangers linked with infection, the U.S. Centers for Disease Control (CDC) suggest annual screening for Chlamydia in sexually active women below the age of 25, as well as in women aged 25 and above who face an elevated risk of infection [1, 6].
To tackle this urgent worldwide challenge and empower nations to achieve the Sustainable Development Goals (SDGs), the World Health Organization (WHO) formulated the Global Health Sector Strategy on Sexually Transmitted Infections, spanning 2022 to 2030 (Global HIV, Hepatitis, and STIs Strategy). This comprehensive strategy outlines critical steps for countries to enhance their response to sexually transmitted infections (STIs), aiming to strengthen efforts, save numerous lives, and enhance the health of millions [7].
However, epidemiological studies of sexually transmitted infections (STIs) in developing countries face challenges, including socio-cultural factors (stigma), poverty, and inadequate diagnostic facilities [8]. In Egypt, the diagnosis of STIs predominantly relies on etiological and clinical presentations due to the absence of structured screening programs for CT and NG [9]. Complicating matters, both CT and NG can manifest asymptomatically, contributing to a significant underreporting of cases [4, 7].
Despite their asymptomatic nature, untreated CT and NG infections can lead to detrimental consequences such as damage to the female genital system and infertility [5, 10]. The persistence of CT averages around 1.4 years, while NG can linger for about six months without antimicrobial treatment. Notably, the longer the clearance time, the higher the prevalence of untreated infections, necessitating effective screening interventions [4, 8].
The Egyptian Family Health Survey 2021, a national survey focusing on women in their reproductive years, sheds light on the prevalence of STIs. Of the surveyed women, only 1% reported that they had acquired STIs in the past 12 months. Additionally, one-fourth of women reported abnormal genital discharge [11].
Challenges in screening for CT and NG lie in the fact that the gold standard for diagnosis in a culture is a method demanding genital swabs. Recent advancements in diagnostic techniques, such as the Xpert CT/NG assay on the GeneXpert system, offer a more accessible approach [12, 13]. This nucleic acid-based test aligns with WHO REASSURED criteria for STI diagnostic tests, offering rapid results within 90 min, real-time connectivity, ease of specimen collection, affordability, sensitivity, specificity, user-friendliness, rapidity, robustness, equipment simplicity, environmental friendliness, and deliverability to end-users [12, 14].
Previous studies in Egypt mainly targeted symptomatic individuals or those already diagnosed with STIs, aiming to understand the etiology of infections. Similarly, studies among infertile women aimed to discern the role of infections in infertility. Due to difficulties in reaching sexually active women for prevalence studies, pregnant women are often considered proxies [8].
The absence of comprehensive epidemiological data on these infections poses a significant challenge in evaluating the disease burden, impeding the development of effective prevention and therapy programs, proper resource allocation, and targeted advocacy plans. This gap becomes particularly noticeable when contrasted with the prioritization and exclusive resource allocation for HIV infections. It underscores the potential cost-effectiveness of integrating other STIs into comprehensive intervention strategies. Therefore, this study seeks to determine the prevalence of CT and NG, specifically among pregnant women in Egypt. This research aims to contribute valuable insights into the broader epidemiology of STIs in the country.
Methods
Study design and setting
This multicenter cross-sectional study was conducted at five antenatal clinics representing diverse regions across Egypt. The investigation aimed to assess the prevalence of Chlamydia trachomatis (CT) and Neisseria gonorrhoeae (NG) infections among pregnant women attending antenatal care (ANC) clinics.
Study population
The study included pregnant women attending ANC clinics at the following centers: Kafr Nasar Maternal and Child Health Centre in Giza (Greater Cairo), Mansoura University Hospital (Delta region), Assiut University Hospital (Upper Egypt), Zagazig University Hospital (Lower Egypt), and Beni-Suef University Hospital (Upper Egypt).
Inclusion criteria
The inclusion criteria included pregnant women attending the clinic for the first time during their current pregnancy, consenting to participate, and having the ability to provide urine samples for testing.
Exclusion criteria
Exclusion criteria were pregnant women who had previously visited the clinic during the survey period, those not providing informed consent, and women who had used antibiotics, douches, or vaginal creams within the last 24 h.
Sample size
To ensure a representative sample, the sample size was calculated using Epi-Info software version 3.5.1 [15]. , incorporating assumptions of an expected frequency of 10% [8], a margin of error of 2%, and a confidence interval of 95%. The initially estimated sample size was 864 pregnant women, with a 20% increase applied, resulting in a final sample size of 1040.
Study instruments
A structured questionnaire was developed to collect participant data and laboratory tests for urine samples.
Structured questionnaire
The questionnaire was specifically developed for this study following a comprehensive review of existing literature to effectively gather data from participants through interviews conducted by research investigators. It covered socio-demographic and reproductive data (residence, age, education, work status, parity, etc.), the presence or absence of symptoms of infection (discharge, pain during intercourse, etc.), previous STIs, and extrauterine pregnancy. The questionnaire is provided in supplementary file 1.
Urine sample collection and testing
Urine samples were collected following specific guidelines for GeneXpert kit analysis [16]. Each participant received a unique identifier number, written on a sterile cup provided by the lab to ensure traceability. Participants were instructed to avoid cleaning the genital area and to catch the first-void urine in the sterile cup. An appropriate transport medium (Xpert CT/NG urine transport reagent tube) was used to stabilize nucleic acid until examination. The samples were preserved in the refrigerator at the study site before weekly transportation to the MoHP TB laboratory. The urine samples underwent Xpert CT/NG qualitative real-time PCR test for the automated detection and differentiation of CT and NG, run through a GenExpert Platform (Kits provided by Cepheid Co.). Results were typically obtained after 90 min.
Pilot study
A pilot study was conducted to validate the questionnaire and refine data collection procedures, including the logistics of urine sample collection, transportation, and laboratory analysis.
Data collection
Data were collected from August 2022 to September 2023. At each study site, a research investigator (a physician providing care at the clinic), assisted by the clinic nurse, conducted interviews and collected urine samples. The samples were labeled, and the investigators followed the instructions for preserving and transporting them to the laboratory. All investigators received training on the questionnaire and procedures for collecting urine samples, transporting them to the lab, and collecting the results of the urine examination, linking them to each participant’s questionnaire.
Data management and analysis
Data management involved Excel and RStudio software. After immediate review for completeness and accuracy, forms were sent to Assiut University for data entry. Double data entry, validation, and cleaning were performed before statistical analysis.
Statistical analysis
Descriptive statistics were used to characterize the sample, including frequencies, percentages, mean ± standard deviation, and median (minimum-maximum).
The prevalence of infection was calculated, and the 95% confidence interval was determined using the Wilson score interval method, which is particularly suitable for low prevalence [17].
Ethical considerations
The study protocol was reviewed and approved by the Institutional Review Board of the Faculty of Medicine, Assiut University (IRB no.: 17400017) and the WHO Research Ethics Review Committee (WHO ERC) (Protocol Id. A66005).
Informed consent
was obtained from all participants prior to their involvement in the study. In cases where participants were illiterate, informed consent was obtained from appropriate representatives. The study adhered strictly to ethical guidelines, ensuring participant privacy and confidentiality throughout the research process.
Furthermore, individuals diagnosed with infections received free treatment following WHO guidelines, underscoring our commitment to ethical and equitable care for all participants.
Results
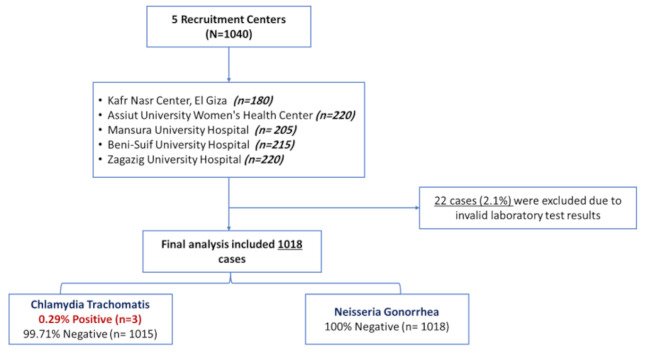
The study enrolled a diverse cohort of pregnant women across five antenatal care centers in Egypt: Assiut (21.2%), El-Giza (17.3%), Mansoura (19.7%), Beni-Suef (20.6%), and Zagazig (21.2%). However, 2.1% of the specimens were initially reported either as “error,” “invalid,” or “no result” by the Xpert test, so the results could not be reported as either positive or negative and have been excluded from the analysis. The flow of participants through the study is presented in Fig. 1.
Fig. 1.
Flow diagram of the study
The socio-demographic characteristics of the recruited women revealed a mean age of 27 years, with nearly 58.5% falling within the 20–29 age group. Most participants were married before age 30 (97.4%), and approximately one-third resided in urban areas (32.7%). Educational attainment varied, with 44.6% completing secondary school or vocational education. Housewives constituted the predominant occupation among participants (90%). Further details on socio-demographic characteristics are presented in Table 1.
Table 1.
Socio-demographic characteristics of recruited women
| Characteristics | Frequency | % |
|---|---|---|
| Age (years) | ||
| Mean ± SD | 27.2 ± 6.1 | |
| < 20 | 82 | 8.1 |
| 20–29 | 595 | 58.6 |
| 30–39 | 311 | 30.6 |
| ≥ 40 | 28 | 2.8 |
| Age at marriage (years) | ||
| Mean ± SD | 19.7 ± 3.8 | |
| ≤ 18 | 466 | 45.8 |
| 19–29 | 525 | 51.6 |
| ≥ 30 | 26 | 2.6 |
| Residency | ||
| Urban | 330 | 32.7 |
| Rural | 678 | 67.3 |
| Education | ||
| Illiterate/read and write | 177 | 17.4 |
| Completed primary/preparatory school | 249 | 24.5 |
| Completed secondary/Vocational education | 453 | 44.6 |
| University graduate or higher | 137 | 13.5 |
| Husband’s Education | ||
| Illiterate/read and write | 215 | 21.2 |
| Completed primary/preparatory school | 150 | 14.8 |
| Completed secondary/Vocational education | 481 | 47.4 |
| University graduate or higher | 165 | 16.3 |
| Do not Know | 4 | 0.39 |
| Work | ||
| Housewife | 920 | 90.4 |
| Paid work | 91 | 8.9 |
| Other | 7 | 0.69 |
| Husband’s Work | ||
| Not Working | 15 | 1.5 |
| Employee | 228 | 22.4 |
| Skilled/Unskilled worker | 563 | 55.4 |
| Private business | 207 | 20.4 |
| Others | 4 | 0.39 |
Reproductive characteristics of the participants revealed a mean pregnancy duration of 27 weeks, with the majority in the third trimester (56.1%). The median gravidity was 3, with 19.1% being primigravida. Most women reported no history of ectopic pregnancy (97.8%).
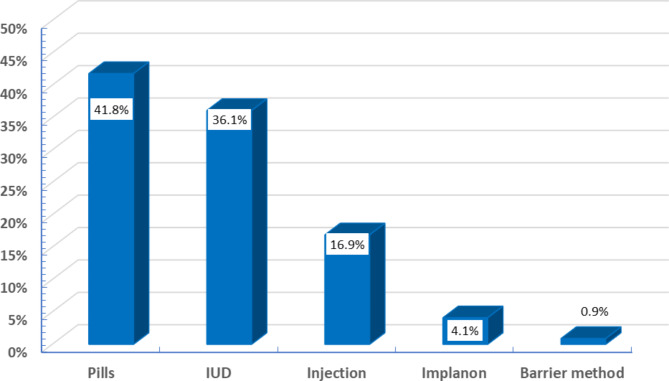
Concerning contraception practices, more than half of the participants (58%) reported using contraception before their current pregnancy. Pills and intrauterine devices (IUDs) were the prevalent choices, constituting 41.8% and 36.1%, respectively (Fig. 2).
Fig. 2.
Distribution of last used contraceptive method
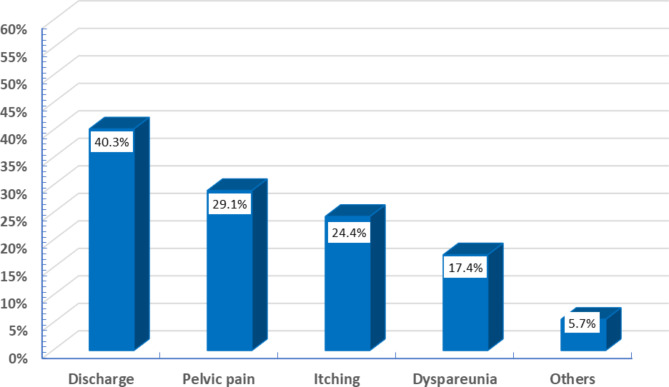
Participants exhibited various gynecological symptoms, with discharge being the most reported (40.3%). Other prevalent symptoms included pelvic pain (29.1%), itching (24.4%), and dyspareunia (17.4%) (Fig. 3).
Fig. 3.
Current presentation of gynecological symptoms
Previous testing for sexually transmitted infections (STIs) was reported by 9.6% of participants, with 8.2% receiving positive results, though the specific infection was not remembered. Among husbands who underwent STI testing, 3.1% had positive results. Notably, 76.8% of participants did not recall undergoing previous STI testing (Table 2).
Table 2.
Previous STIs test for women or her husband
| Characteristics | Frequency | % |
|---|---|---|
| Previous STIs test | ||
| Yes | 98 | 9.6 |
| No | 782 | 76.8 |
| Do not remember | 138 | 13.6 |
| Result of previous STIs test | ||
| Positive | 8 | 8.2 |
| Negative | 72 | 73.5 |
| Do not know | 18 | 18.4 |
| Husband’s previous STIs test results | ||
| Positive | 3 | 3.1 |
| Negative | 42 | 43.8 |
| Do not know | 51 | 53.1 |
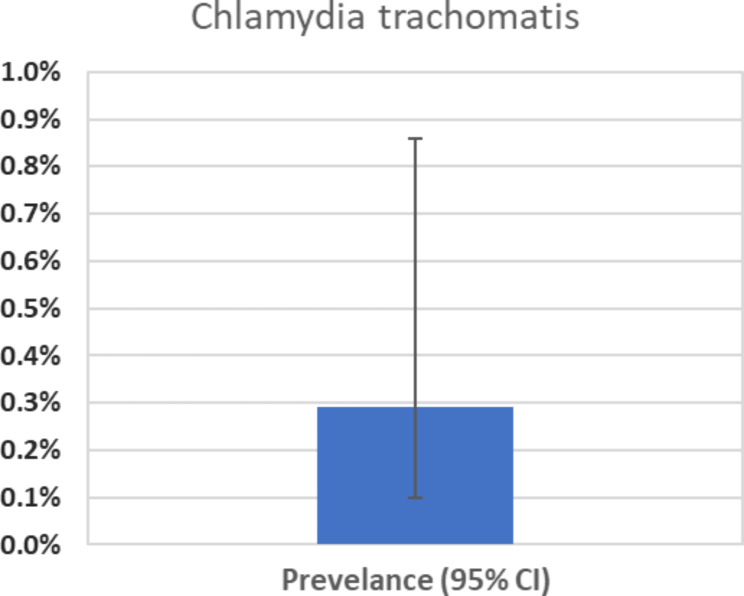
The prevalence of CT infections among the study participants was 0.29%, with confidence intervals ranging from 0.10 to 0.86% (Fig. 4). Notably, no NG infections were detected in the study.
Fig. 4.
CT prevalence with 95% CI
The three positive cases for CT were distributed across different recruitment centers, with one each in El-Giza, Mansoura, and Beni-Suef. In the third trimester of pregnancy, these cases were 29, 18, and 31 years old. Due to the low number of cases, no statistically significant differences were observed when comparing participants with STIs to the non-infected group.
Discussion
The present study aimed to investigate the prevalence of Chlamydia trachomatis (CT) and Neisseria gonorrhoeae (NG) infections among pregnant women attending antenatal care (ANC) clinics in various regions of Egypt. The findings offer essential insights into the epidemiology of these sexually transmitted infections (STIs) in a population vulnerable due to the potential consequences of maternal infections on both maternal and neonatal health.
To our knowledge, the current study is the first investigation in Egypt specifically focused on determining the prevalence of CT and NG among pregnant women, serving as a proxy for sexually active women. Previous research in the country predominantly targeted individuals with STI symptoms or those already diagnosed, with a focus on specific types of infections or cases related to infertility [9, 10, 18, 19]. The overall prevalence of CT infections among the study participants was 0.29%, and no cases of NG were detected.
In contrast, the 2021 Egyptian Family Health Survey inquired about STI history and genital discharge in the past year among women. The results indicated that only 1% of women reported having a sexually transmitted infection in the 12 months preceding the survey [11]. Regarding STI symptoms, 25% reported abnormal genital discharge, while the present study found that 40% reported having a discharge.
A study at Mansoura University Hospital aimed to detect C. trachomatis in Egyptian women with genital infection symptoms, revealing a positive CT cell culture in 22.8% of symptomatic cases [20]. Additionally, a study on Chlamydia trachomatis screening among Egyptian women with unexplained infertility showed a 6% prevalence of current Chlamydial infection [18]. Another investigation among infertile women at Suez Canal University Hospital found a 2.7% prevalence of CT and 2% of NG [10].
In 2020, a study in Assiut explored the prevalence of various STIs in married women, identifying common infections such as candidiasis, scabies, genital warts, and trichomoniasis. Neisseria gonorrhoeae was present in 5% of cases, though Chlamydia trachomatis was not investigated [9].
Despite variations in prevalence across studies, the low prevalence of CT and NG in Egypt aligns with rates in other Middle East and North Africa (MENA) region countries. A meta-analysis reported pooled prevalence rates: 3.0% in general populations such as antenatal clinic attendees, blood donors, and pregnant women; 2.8% in intermediate-risk populations, which include individuals who are presumed to have some sexual contact with groups engaging in high-risk sexual behavior; 13.2% in female sex workers; 11.3% in infertility clinic attendees; 12.4% in women with miscarriage; and 12.4% in symptomatic women [8].
Several factors may explain this. Firstly, the region lacks comprehensive screening for these infections, leading to diagnosed cases representing only the tip of the iceberg. In particular, silent infections, such as CT, may persist without symptoms for extended periods, contributing to underreporting [2, 6, 8].
A predominantly symptomatic diagnosis approach further influences the low prevalence. In cases where individuals complain of pelvic pain or discharge, antibiotics are often prescribed without thorough consideration of the specific infection causing the symptoms [4, 8]. Compounding this issue, the accessibility of antibiotics as over-the-counter drugs in our community contributes to their irrational use [2].
Additionally, seeking medical advice for sexually transmitted infections (STIs) may carry a stigma in our culture. Consequently, these infections are likely underreported in the Middle East due to a reluctance to disclose such information [8, 21].
The presence of symptoms like discharge, pelvic pain, and itching emphasizes the urgent need for comprehensive reproductive health services and education, particularly for pregnant women. Addressing these challenges requires a multifaceted approach, encompassing improved screening, judicious antibiotic use, and destigmatizing conversations surrounding STIs in the Middle East.
This study significantly contributes to the field by employing urine analysis to detect chlamydial and gonorrheal infections among pregnant women. The decision to utilize urine samples, as opposed to traditional genital swabs, is notable and provides practical advantages that enhance the feasibility and acceptability of screening in diverse healthcare settings. The non-invasive nature of urine sample collection streamlines the screening process and increases participation rates, making it an accessible and patient-friendly method. This approach aligns with recent advancements in non-invasive testing methods for sexually transmitted infections (STIs) and marks a positive step toward overcoming barriers to screening [12, 22].
The validity of the GeneXpert platform for STI detection has been established in prior studies. The qualitative real-time PCR test conducted through the GeneXpert system ensures automated and accurate detection and differentiation of CT and NG [13, 14]. The GeneXpert system is an automated molecular diagnostic method based on nucleic acid amplification testing developed by Cepheid in the USA. Its detection technology relies on a 90-minute real-time fluorescent qualitative polymerase chain reaction (FQ-PCR), exhibiting comparable performance to traditional nucleic acid amplification tests [12, 23]. The Xpert platform seamlessly integrates and automates various processes, including sample preparation, nucleic acid purification, gene amplification, and result reporting through qualitative PCR molecular detection. This enables the rapid detection of CT and NG pathogens on the same day [14].
The Xpert system offers numerous advantages, including the independent use of each machine module and the simultaneous screening of multiple samples. It is faster, simpler, accurate, and safer than traditional methods. A meta-analysis substantiates the high diagnostic accuracy of Xpert CT/NG for both CT and NG. Notably, the system demonstrated elevated sensitivity and specificity in detecting anorectal, urethral, and vaginal samples without significant differences based on gender. Consequently, Xpert CT/NG can potentially emerge as the primary method for detecting CT and NG, possibly evolving into the gold standard for diagnosis in the future [13].
The strengths of this multicenter study lie in its representative sample, which included various regions of Egypt. Significantly, the study enhances our understanding of chlamydial and gonorrheal infections among pregnant women as a proxy for sexually active women, emphasizing the necessity for a nuanced approach to STI research and prevention.
However, it is essential to acknowledge potential confounding factors, such as the widespread use of antibiotics, particularly azithromycin, during the peak of the COVID-19 epidemic. This prevalent usage, recommended by healthcare providers and available over-the-counter, may impact the observed low prevalence rates of the studied STIs, given their known sensitivity to this antibiotic.
Furthermore, the absence of comprehensive STI surveillance in Egypt underscores the imperative for an enhanced national system to monitor and effectively address STIs. This highlights the diversity of STIs in different populations and underscores the importance of tailored screening and management approaches. Future research should aim for a comprehensive understanding of STIs in diverse populations, informing targeted preventive measures and interventions.
Conclusions
In conclusion, this study contributes valuable data on the prevalence of CT and NG infections among pregnant women attending ANC clinics in Egypt. The findings underscore the importance of ongoing surveillance, routine screening, and targeted interventions to ensure the reproductive health and well-being of pregnant women and their infants. Further research is warranted to explore the broader implications of STIs in different populations and to inform evidence-based guidelines for screening and management in diverse settings.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors sincerely thank all study participants who contributed to successfully executing this research. Our gratitude is also extended to the study teams and site coordinators, whose commitment and professionalism significantly enhanced this scientific endeavor’s overall quality and success.
Author contributions
MW, OE, NG and MA contributed to concept and design of this study, the construction of the questionnaire and preparation of the manuscript. MN , AK, SM, MAW, WA, HE and SE collected the data. MA , NG, AH and OE analyzed and interpreted the data for this study. All authors provided substantial comments and approved the final version of the manuscript.
Funding
The study has received technical support and funding from the World Health Organization (WHO) headquarters. Moreover, Cepheid company has contributed by supplying kits and consumables and providing training for the laboratory personnel in implementing the GeneXpert assay.
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Data availability
The questionnaire and the datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
The study protocol was reviewed and approved by the Institutional Review Board of the Faculty of Medicine, Assiut University (IRB no.: 17400017) and the WHO Research Ethics Review Committee (WHO ERC) (Protocol Id. A66005).
Consent for publication
NA.
Competing interests
The authors declare no competing interests.
Informed consent
was obtained from all participants prior to their involvement in the study. In cases where participants were illiterate, informed consent was obtained from appropriate representatives. The study adhered strictly to ethical guidelines, ensuring participant privacy and confidentiality throughout the research process.
Furthermore, individuals diagnosed with infections received free treatment following WHO guidelines, underscoring our commitment to ethical and equitable care for all participants.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Smith LE. Sexually transmitted diseases. Princ. Pract. Surg. Colon, Rectum, Anus, Third Ed., 2007.
- 2.Carey AJ, Beagley KW. Chlamydia trachomatis, a hidden epidemic: effects on Female Reproduction and options for treatment. Am J Reprod Immunol. 2010;63:576–86. 10.1111/j.1600-0897.2010.00819.x. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Sexually transmitted infections (STIs) 2022. https://www.who.int/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis) (accessed August 14, 2024).
- 4.El-Kettani A, Mahiané G, Bennani A, Abu-Raddad L, Smolak A, Rowley J, et al. Trends in Adult Chlamydia and Gonorrhea Prevalence, incidence and urethral discharge case reporting in Morocco over 1995-2015-Estimates using the spectrum-sexually transmitted infection model. Sex Transm Dis. 2017;44:557–64. 10.1097/OLQ.0000000000000647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mullick S, Watson-Jones D, Beksinska M, Mabey D. Sexually transmitted infections in pregnancy: prevalence, impact on pregnancy outcomes, and approach to treatment in developing countries. Sex Transm Infect. 2005. 10.1136/sti.2002.004077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baraitser P, Alexander S, Sheringham J. Chlamydia trachomatis screening in young women. Curr Opin Obstet Gynecol. 2011. 10.1097/GCO.0b013e32834ac776. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. Geneva: World Health Organization; Global Health Sector Strategy on Sexually Transmitted Infections 2016–2021. Clin Colon Rectal Surg 2007;20:58–63.
- 8.Smolak A, Chemaitelly H, Hermez JG, Low N, Abu-Raddad LJ. Epidemiology of Chlamydia trachomatis in the Middle East and North Africa: a systematic review, meta-analysis, and meta-regression. Lancet Glob Heal. 2019;7:e1197–225. 10.1016/S2214-109X(19)30279-7. [DOI] [PubMed] [Google Scholar]
- 9.El-Moselhy E, Issa L, Mohamed M, Abdelati M, Eldhshan R, Mekky A, et al. Sexually transmitted infections: risk-factors among married female patients’ in Assiut, Egypt. Al-Azhar Int Med J. 2020;0:0–0. 10.21608/aimj.2020.38500.1295. [Google Scholar]
- 10.Elkayal NM, Mahmoud NF, Abdalla S. Detection of Chlamydia trachomatis and Neisseria gonorrhoeae in Egyptian women suffering from infertility. Adv Microbiol. 2015;05:769–79. 10.4236/aim.2015.512081. [Google Scholar]
- 11.Central Agency for. public mobilization and statistics (CAPMAS). Egypt Family Health Survey 2021. 2022.
- 12.Jacobsson S, Boiko I, Golparian D, Blondeel K, Kiarie J, Toskin I, et al. WHO laboratory validation of Xpert® CT/NG and Xpert® TV on the GeneXpert system verifies high performances. Apmis. 2018;126:907–12. 10.1111/apm.12902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Han Y, Shi MQ, Jiang QP, Le WJ, Qin XL, Xiong HZ, et al. Clinical performance of the Xpert® CT/NG Test for detection of Chlamydia trachomatis and Neisseria gonorrhoeae: a Multicenter evaluation in Chinese urban hospitals. Front Cell Infect Microbiol. 2022;11:1–7. 10.3389/fcimb.2021.784610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xie TA, Liu YL, Meng RC, Liu XS, Fang KY, Deng ST et al. Evaluation of the diagnostic efficacy of Xpert CT/NG for Chlamydia trachomatis and Neisseria gonorrhoeae. Biomed Res Int 2020;2020. 10.1155/2020/2892734 [DOI] [PMC free article] [PubMed]
- 15.Dean AG, Arner TG, Sunki GG, Friedman R, Lantinga M, Sangam S, Zubieta JC, Sullivan KM, BrendDean AG, Arner TG, Sunki GG, Friedman R, Lantinga M, Sangam S, Zubieta JC, Sullivan KM, Brendel KA, Gao Z, Fontaine N, Shu M, Fuller G, Smith DC, Nitschke DA. and and FR. Epi Info™, a database and statistics program for public health professionals. 2011.
- 16.Cepheid. Xpert® CT/NG Package Insert 2019.
- 17.Julious SA. Two-sided confidence intervals for the single proportion: comparison of seven methods. Stat Med. 2005;24:3383–4. 10.1002/sim.2164. [DOI] [PubMed] [Google Scholar]
- 18.Abdella RMA, Abdelmoaty HI, Elsherif RH, Sayed AM, Sherif NA, Gouda HM, et al. Screening for Chlamydia trachomatis in Egyptian women with unexplained infertility, comparing real-time PCR techniques to standard serology tests: case control study. BMC Womens Health. 2015;15:1–8. 10.1186/s12905-015-0202-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.El-Shourbagy M, Abd-El-Maeboud K, Diab KM, El-Ghannam A, Nabegh L, Ammar S. Genital Chlamydia trachomatis infection in Egyptian women: incidence among different clinical risk groups. J Obstet Gynaecol Res. 1996;22:467–72. 10.1111/j.1447-0756.1996.tb01059.x. [DOI] [PubMed] [Google Scholar]
- 20.Abd S, Agha E-F, El-Mashad N, Rakha SA, El A, Metwally G, El. Value of direct antigen detection methods in diagnosing women with suspected genital Chlamydia trachomatis infection. Afr J Microbiol Res. 2011;5:1215–9. 10.5897/AJMR11.178. [Google Scholar]
- 21.Haberland N, Winikoff B, Sloan N, Coggins C, Elias C. Case finding and case management of chlamydia and gonorrhea infections among women. What we do and do not know; 1999.
- 22.WHO. Sexually transmitted infections-Fact Sheet n.d. https://www.who.int/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis).
- 23.WHO. Standard protocol to assess prevalence of gonorrhoea and chlamydia among pregnant women in antenatal care clinics. 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The questionnaire and the datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.