Abstract
China has made substantial progress in healthcare delivery to reduce the burden of non-communicable diseases due to population ageing, although challenges and opportunities in long term care services have been under-recognised, argue Xiaoming Shi and colleagues
Despite a substantial improvement in understanding of the risk factors, no definitive solution for managing the care needs arising from the ageing population and the accompanying rise in non-communicable diseases yet exists, posing significant challenges to healthcare and long term care services in China over the past few decades.1 Although efforts have been made to enhance healthcare delivery and reduce inequalities, long term care services lag significantly behind, particularly as population ageing is progressing rapidly in China. This analysis provides an overview of the challenges in both healthcare delivery and long term care services, as well as current responses, and pinpoints significant gaps in actual care delivery that need urgent attention, aiming to offer insights for other nations facing similar demographic and societal shifts.
Population ageing in China
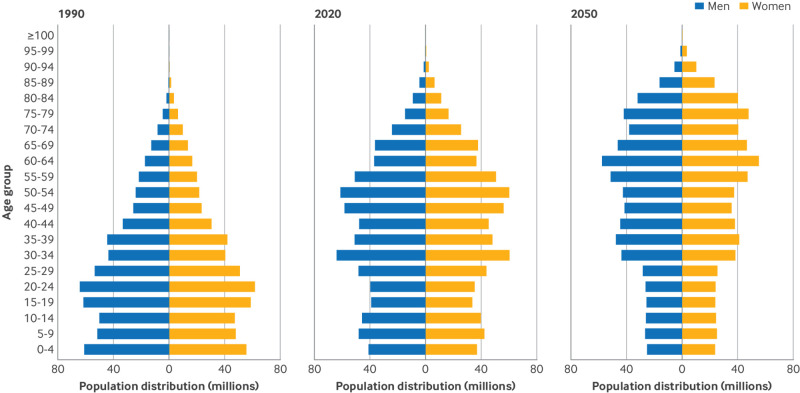
The number of older adults aged 65 years and over in China reached 191 million in 2020, accounting for 13.5% of the total population,2 and is predicted to reach 29.8% by 2050, almost twice the global level of 16.4%.3 China’s ageing population has several outstanding characteristics. Firstly, the number of older adults in China, especially the oldest people aged 80 years and over, is unparalleled in scale. The population aged 80 and over reached 35.8 million in 2020 and is projected to be 115 million in 2050, accounting for 13.6% and 31.5% of older adults, respectively,2 3 leading to a dramatic increase in the demand for healthcare in China. Secondly, with an unparalleled speed of ageing, the proportion of older adults has doubled in the past two decades. This situation is expected to worsen in the coming years, leading to a pagoda shaped population structure in 2050 (fig 1). The rapid ageing process and shortage of young people pose a great challenge to the unprepared long term care service system. Thirdly, regional inequalities have escalated. Recent decades of rapid social and economic change have widened regional gaps in access to healthcare, leaving underdeveloped areas with burgeoning older populations, posing broad challenges to the current insurance system.
Fig 1.
Population distribution by gender and age in 1990, 2020, and 2050 in China. Data source: The 4th and 7th National Census of China and the World Population Prospects of the UN
Burden of non-communicable diseases due to population ageing
Ageing of the population, emerging new risk factors, and more sensitive diagnostic methods contribute to the increase in the burden of non-communicable diseases. In 2019 deaths from non-communicable diseases reached 9.5 million in China, accounting for 90.1% of all deaths, higher than the global level of 74.3%, and this number is projected to double over the next 30 years.4 The major non-communicable diseases, including cardiovascular diseases, chronic obstructive pulmonary disease, and tracheal, bronchus, and lung cancer, have been the leading causes of death in China, corresponding to 43.1%, 9.7%, and 7.1% of mortality, respectively (estimated by Global Burden of Disease Compare).5
The burden of non-communicable diseases is closely associated with the age structure of the population. The ageing population and increasing age related diseases largely contribute to the increasing burden. In ageing countries, crude mortality rates of non-communicable diseases are higher than the corresponding rates adjusted for population structure. In China, a fast ageing population and growing health loss resulted in about 92.8 million increments in age specific, disability adjusted life years, although disability adjusted life years have been decreasing during the past three decades.6 In China, half of all disability adjusted life years can be attributed to 92 age related diseases (for example, stroke, chronic obstructive pulmonary disease, lung cancer, diabetes, and Alzheimer’s disease).7 Dementia, an age related disease, affected 15.1 million older adults in China,8 increasing by more than 50% in the past decade.8 The number of people with Parkinson’s disease is expected to increase from 3.3 million to 4.8 million in the next decade.9 Furthermore, the burden of non-communicable diseases will increase by more than two fifths in the coming decades owing to population ageing,10 posing a considerable challenge to China.
Challenges to healthcare delivery and long term care services
In response to the control and prevention of non-communicable diseases resulting from population ageing, healthcare delivery and long term care serve different purposes and target distinct populations. Healthcare services are medical services in hospitals, which are mainly aimed at the diagnosis, management, and treatment of non-communicable diseases. Long term care services are primarily provided by nursing homes or residential care facilities,10 aiming to meet people’s needs for assistance in daily activities, nursing care, functional rehabilitation, and so on (table 1). Facing the dual burden of the rising epidemic of non-communicable diseases and rapid population ageing, the demands for delivery of healthcare for the treatment and management of non-communicable diseases, as well as the need for long term care services for functional maintenance, have increased significantly. This also leads to increasing demand for funding and shortages in the long term care workforce and underscores the urgent need for innovative solutions such as age friendly environments.
Table 1.
Functional positioning and inadequate preparation for healthcare delivery and long term care services
| Category | Healthcare delivery | Long term care services |
|---|---|---|
| Institutions | ||
| Functional position | Healthcare system reform prioritises transforming hospital centred treatment to integrated and continued care through a three tier healthcare delivery system*: tier 3 includes county and city hospitals; tier 2 includes township health centres and community health centres/stations; tier 1 includes village and community clinics | Three main types include public social welfare facilities, nursing homes, and other residential care facilities (eg, senior apartments, assisted living facilities, and retirement communities) |
| Characteristic | Changing from treatment oriented to rehabilitation and prevention oriented | Growing residential (institutional) care sector, slow development of HCBS, and insufficient organised funding |
| Challenges | Ageing adds burdens on primary healthcare institutions (including tier 2 and tier 1). Primary healthcare institutions account for 94.8% of all three tier healthcare institutions, which account for only 53.2% of treatment visits and 16.1% of hospital admissions for all institutions† | New family structures, rapid urbanisation, and increased labour mobility, which increased the burden of care from relatives have weakened the family based long term care model of China‡ |
| Workers | ||
| Provider | Professional doctors or nurses | Nursing or social work staff |
| Challenges | Inadequate professional and technical skills, qualifications, and incentives of workers in primary healthcare institutions. The education level in primary healthcare institutions is much lower than in tier 3 healthcare institutions. Professional training in geriatrics and nursing provided by medical schools is limited. The incentive mechanism for primary healthcare institutions is relatively weak (eg, income is not linked with jobs) and relies more on the number of patients seen and medicine used | Shortage of long term care workers. Qualification certification, professional title evaluation, and promotion ladders. Challenges remain to improve working conditions and management systems and to increase the social values and reputation of the profession |
| Care and services | ||
| Services | Diagnosis and treatment of diseases, training and guidance. Tier 3 healthcare institutions: diagnosis and treatment of diseases, training and guidance to workers of primary medical institutions, public health, and emergency medical services. Primary medical institutions: basic public health services, diagnosis and treatment services for common diseases, rehabilitation and nursing services for some diseases, and transferring patients with critical and difficult cases beyond their own service capabilities to hospitals§ | Daily care, nursing care, risk prevention, and guide function maintenance. Daily care: cleaning, food/water assistance, etc. Nursing care: health guidance, blood glucose monitoring, etc. Risk prevention: prevention of pressure sores, choking, falls, burns, etc. Guide function maintenance: rolling training and guiding passive joint activities, etc |
| Challenges | Ageing has brought diverse overuse and overprovision of health services. Patients with NCDs bypass primary health facilities and seek perceived good quality of care in high level hospitals. For patients in the recovery period, community and home based rehabilitation services are more important but less used. For comorbidities, the use of traditional Chinese medicine could reduce the side effects of combined western medication | Professional long term care services are underdeveloped in China, and NCDs due to ageing put a higher demand on specialised and professional services. Long term care services are still not easily accessible or of high quality. Insufficient utilisation of beds in professional long term care institutions |
HCBS=home and community based services; NCD=non-communicable disease.
Meng Q, Mills A, Wang L, Han Q. What can we learn from China’s health system reform? BMJ 2019;365:l2349.
National Health Commission of the People’s Republic of China. Statistical Bulletin of China's Health Development in 2020. https://www.gov.cn/guoqing/2021-07/22/content_5626526.htm.
Fang EF, Scheibye-Knudsen M, Jahn HJ, et al. A research agenda for ageing in China in the 21st century. Ageing Res Rev 2015;24:197-205.
Office of the State Council. National healthcare policy announcement of strategic plan on national healthcare service system (2015–2020). 2015. https://www.gov.cn/zhengce/content/2015-03/30/content_9560.htm.
With the ageing of the population, the demand for long term care services in China will increase by 2.5 times between 2015 and 2050. However, the home and community based services system, which is supported by government subsidies to provide older adults with services such as living assistance, healthcare, and social support, offered ageing care services to only 5.35 million of the 264 million older adults in 2020.11 Regarding demand for financial support, the individual contribution to health expenditure increased from ¥68 CNY (£7.3; €8.7; $9.4) in 2012 to ¥274 in 2020 per capita, with its share of total insurance increasing from 22% in 2012 to 36% in 2020.12 Meanwhile, long term care insurance covers only 49 pilot cities in 2024, serving 2.4 of 40 million people with disabilities. Considering the limited provision and providers of ageing care, an estimated 10 million plus elderly caregivers will be needed by 2025, whereas fewer than 0.5 million certified caregivers were present in China at the end of 2020 (fig 2).13 Rapid urbanisation, socioeconomic shifts, and changes in family structures are weakening the traditional family based elder care model. Age friendly environments, designed to support older people to promote health and maximise their functional abilities when experiencing capacity loss, and smart aged care technology, are far from satisfying the growing demand with the transition from family support to a social services model. Specifically, in China, the proportion of high rise dwellings without elevators exceeds 60% in urban areas, and only 54 smart ageing care products such as wearable devices and health monitoring devices, as well as 25 smart ageing care services, have been screened to the national recommendation catalogue.14 Furthermore, fewer than 35% of older adults actually use a smartphone, although 77% had a smartphone in 2021, creating technological barriers to medical services for non-communicable diseases (for example, registration, checking examination results, remote medical consultation).
Fig 2.
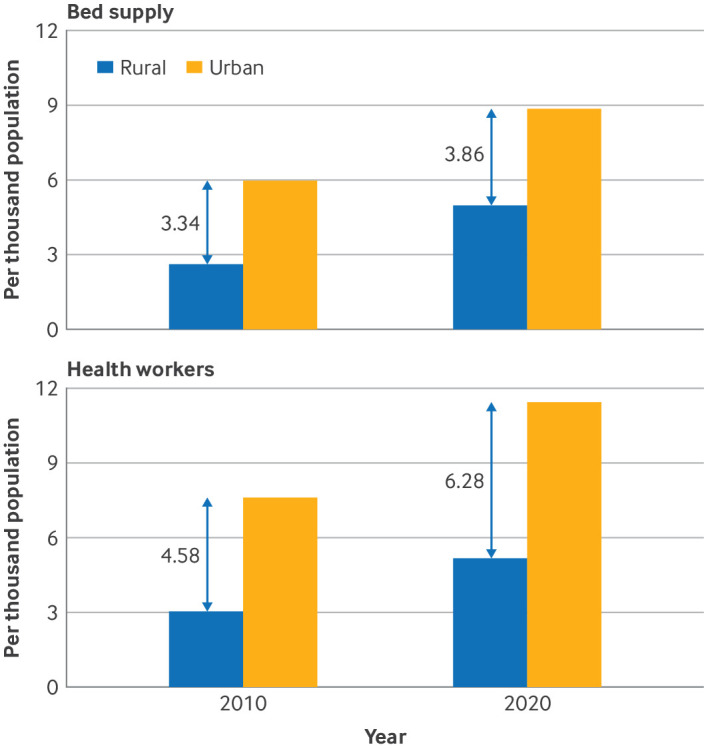
Inequalities in bed supply and health workers between urban and rural areas in China. Data source: Chinese Health Statistical Yearbook (2021)
China’s responses to the challenges
To alleviate the burden of non-communicable diseases attributed to factors such as population ageing, the Chinese government has implemented a series of proactive measures, which may offer insights for other developing countries facing similar challenges in combating population ageing. To overcome the challenges in growing services and their inequities, China has made great achievements in implementing the National Basic Public Health Service Program (NBPHSP) to mitigate healthcare inequalities, establishing the world’s most comprehensive healthcare insurance system to meet growing funding demands, and preliminarily applying the concept of whole life course approach to manage modifiable driving factors of non-communicable diseases.
Managing non-communicable diseases is a prioritised target in basic public health services policies
To tackle the dual burden of infectious diseases and non-communicable diseases, China launched the NBPHSP in 2009. The NBPHSP includes population based services for women, children, and older adults, as well as group specific services for patients with non-communicable diseases, including hypertension, hyperlipidaemia, diabetes, overweight or obesity, and fatty liver. In the past decade, the number of beds per thousand people has increased from 4.83 in 2014 to 6.92 in 2022. Health management services were provided to 127 million older adults aged 65 and above in 2022, constituting 14.9% of the total population, at primary healthcare institutions.15 The five year survival rate for cancer has increased from 40.5% in 2015 to 43.7% in 2022 with improving diagnosis and treatment. Significant improvements have been observed in the treatment of hypertension and diabetes between 2004 and 2018, with average annual percentage changes in patients treated of 3.3% and 3.9%, respectively.13 In the next few decades, the prevention and control of non-communicable diseases are among the most important national targets: “achieving hypertension and diabetes management rates up to 70% and 69% by 2050, respectively.” 16
Establishing the world’s largest social health insurance system
Owing to healthcare reform in 2009, China has become the country with the world’s largest social health insurance system, covering 95% of the population. The system includes the urban employee basic medical insurance programme, the urban-rural resident basic medical insurance programme, and medical assistance tailored to low income households.17 In addition, to ensure reasonable medical expenses, the government is involved in price determination and drug procurement supervision. These schemes collectively cover 37% of healthcare spending in China, and the coverage will continue to increase; the range of non-communicable diseases covered by medical insurance has also expanded, accompanied by an increase in the reimbursement ratio compared with total expenses.
Integrating the whole life course approach into the management of non-communicable diseases
China has proposed a whole life course approach to managing driving factors of non-communicable diseases from early stages to older adults, which aims to foster healthy ageing. Increasing attention is being paid to health management in children (under 6 years), maternal health care and free contraceptive provision for adults, and health management for older adults. Whole population management focusing on healthy lifestyles, environmental risk factors, health education, health literacy promotion, and vaccination has also been shown to be most effective when prevention and control of non-communicable diseases are tackled at the earliest stages.18 For instance, air quality management efforts from 2013 to 2020 resulted in a decrease in years of life lost due to exposure to PM2.5 (fine particulate matter), from 28.87 million to 22.62 million years of life lost.19
What is the way forward?
Although China has taken initiatives to prevent and control non-communicable diseases in light of the World Health Organization’s global targets, monitoring of indicators of progress shows that the improvement has been only partially achieved. To achieve sustainable development, China needs to more effectively overcome challenges to healthcare delivery and long term services arising from non-communicable diseases. Several critical recommendations exist to find a way out of the dilemma (box 1).
Box 1. Recommendations for healthcare delivery and long term care services for non-communicable diseases due to population ageing.
Developing differentiated functioning systems for integrated aged care
Developing clear functional positioning systems for providing integrated care for older adults
Further strengthening the integration of healthcare delivery and long term care services
Establishing differentiated, innovative, and collaborative healthcare and long term care systems
Establishing a sound and sustainable long term care insurance system
Integrating long term care insurance with existing health insurance
Encouraging commercial insurers
Developing the “silver economy” market
Strengthening the management of modifiable risk factors for non-communicable diseases
Improving education and economic equity in early life
Promoting healthy lifestyles across early life, midlife, and late life courses
Accelerating the development of age friendly products and environments
Accelerating technological progress and the application and construction of age friendly products and environments
Facilitating the translation of discoveries into practical healthcare tools
Enabling social participation, chance of volunteer work, or employment
Developing differentiated functioning systems for integrated aged care
To effectively tackle the diverse needs of healthcare and long term care services, China needs to develop tailored and collaborative healthcare systems, with a primary focus on medical services and robust long term care provision. Specialised long term care institutions can collaborate with hospitals to meet needs for functional rehabilitation, daily activities assistance, and social support while conducting comprehensive assessments of functional status and monitoring transitions in older adults with non-communicable diseases. This collaborative approach ensures timely and appropriate care delivery, especially for people with limited life expectancy or when treatment efficacy is constrained.
Establishing a sustainable long term care insurance system
Drawing from the experiences of countries such as the US, Japan, and Germany, integrating long term care insurance with existing health insurance is proposed to cover basic medical and long term care needs across different economic strata.20 To achieve sustainable solutions, insurance funds for long term care should not rely only on the surplus of medical insurance funds and government appropriations but also work with commercial insurance as a complementary option. Furthermore, leveraging the “silver economy” market can enhance the sustainability of long term care by offering diverse insurance options and financial products tailored to the needs of older people.
Strengthening the management of modifiable risk factors for non-communicable diseases
Non-communicable diseases are often characterised by interconnected cause and effect chains, so identifying a specific factor is very difficult and challenging. Four prioritised modifiable risk factors proposed by WHO—namely, tobacco use, alcohol use, physical inactivity (failure to meet ≥150 min/week of moderate activity, ≥75 min/week of vigorous activity, or a combination), and unhealthy diets—have not been fully controlled in China (for example, prevalence rates of tobacco use and physical inactivity are 49.7% (men) and 44.1%, respectively). Encouraging healthy lifestyles across all age groups is particularly important to eliminate the factors driving non-communicable diseases. Additionally, an air quality management effort was more pertinent and effective at specific stages of life, so ensuring its continued implementation is crucial.
Accelerating the development of age friendly products and environment
Development of new technologies is necessary to reduce the escalating burden of non-communicable diseases and connect recent research findings with clinical practice. Technologies such as robots and artificial intelligence have a promising future in medical research, aiding the translation of discoveries into practical tools in healthcare and long term care management. Moreover, enhancing opportunities for social participation among the ageing population (for example, through voluntary work, employment, digital access, and social media engagement) is essential to improve their overall well being.
Conclusion
Over the past few decades, China has faced a substantial rise in the burden of non-communicable diseases that is partly attributable to population ageing, which poses challenges not only in healthcare delivery but also in long term care services, such as inadequate system preparation, increasing demands for funding, shortages in the long term care workforce, and insufficient age friendly environmental support. With the establishment of the world’s largest healthcare insurance system and the implementation of basic public health services policies, China has made commendable strides in promoting equitable healthcare services and tackling the drivers of non-communicable diseases. Considering the challenges and gaps, we have made several critical recommendations to find a way out of the dilemma; China needs to develop tailored and collaborative healthcare systems, with a primary focus on medical services and robust long term care provisions.
Key messages.
Over the past few decades, although age specific, disability adjusted life years have been significantly reduced by the control of modifiable risk factors, the burden of non-communicable diseases is still increasing owing to the fast growing ageing population.
China’s burgeoning older demographic and the increasing prevalence of non-communicable diseases not only present a formidable challenge to the healthcare delivery system but also demand greater preparedness for the long term care sector.
With the establishment of the world’s largest healthcare insurance system and the implementation of basic public health services policies, China has made commendable strides in promoting equitable healthcare services and tackling the drivers of non-communicable diseases
To effectively fulfil the diverse needs of healthcare and long term care services, China needs to develop tailored and collaborative healthcare systems, with a primary focus on medical services and robust long term care provisions
Acknowledgments
We thank Yuan Wei, Yu Wang, Shilu Tong, John Ji, Peng Yin, and Zhaoxue Yin for their contribution to shaping the idea of the paper. The research was funded by National Natural Sciences Foundation of China (grant 82025030).
Contributors and sources: XS conceived and designed the paper. All authors contributed to drafting the manuscript, with YL taking the lead role in writing the manuscript and all authors providing intellectual input to improve it, as well as reading and approving the final version. XS is the guarantor.
Competing interests: We have read and understood BMJ policy on declaration of interests and have no interests to declare.
This article is part of a collection on chronic diseases in China funded by the Chinese Center for Disease Control and Prevention, Beijing Hospital, and the authors and their institutions. The BMJ commissioned, peer reviewed, edited, and made the decisions to publish these articles. The lead editors for The BMJ were Jin-Ling Tang and Di Wang.
References
- 1. Eaton S, Roberts S, Turner B. Delivering person centred care in long term conditions. BMJ 2015;350:h181. 10.1136/bmj.h181 [DOI] [PubMed] [Google Scholar]
- 2.State Council for the Seventh National Population Census. China population census yearbook 2020. https://www.stats.gov.cn/sj/ndsj/2020/indexch.htm.
- 3.United Nations Department of Economic and Social Affairs. World population prospects. https://population.un.org/wpp/Download/Standard/CSV/.
- 4. Liu J, Jiang B, Fu Y, et al. The future challenges of population health in China: a projection of the major health problems and life expectancy - China, 2015-2050. China CDC Wkly 2022;4:276-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Institute for Health Metrics and Evaluation. Global Burden of Disease Compare. https://vizhub.healthdata.org/gbd-compare/#.
- 6. Li R, Cheng X, Schwebel DC, et al. Disability-adjusted life years associated with population ageing in China, 1990-2017. BMC Geriatr 2021;21:369. 10.1186/s12877-021-02322-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chang AY, Skirbekk VF, Tyrovolas S, Kassebaum NJ, Dieleman JL. Measuring population ageing: an analysis of the Global Burden of Disease Study 2017. Lancet Public Health 2019;4:e159-67. 10.1016/S2468-2667(19)30019-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chan KY, Wang W, Wu JJ, et al. Global Health Epidemiology Reference Group (GHERG) . Epidemiology of Alzheimer’s disease and other forms of dementia in China, 1990-2010: a systematic review and analysis. Lancet 2013;381:2016-23. 10.1016/S0140-6736(13)60221-4 [DOI] [PubMed] [Google Scholar]
- 9. Chen F, Chen S, Si A, et al. The long-term trend of Parkinson’s disease incidence and mortality in China and a Bayesian projection from 2020 to 2030. Front Aging Neurosci 2022;14:973310. 10.3389/fnagi.2022.973310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. Long-term care Q&A. 2022. https://www.who.int/europe/news-room/questions-and-answers/item/long-term-care.
- 11. Meng Q, Mills A, Wang L, Han Q. What can we learn from China’s health system reform? BMJ 2019;365:l2349. 10.1136/bmj.l2349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zhong Y, Zhang J. China Medical Security Statistical Yearbook. China Statistics Press, 2021. [Google Scholar]
- 13. Zhou Y, Wu Q, Li C, Meng P, Ding L. Inequalities in non-communicable disease management in China and progress toward universal health coverage: an analysis of nationwide household survey data from 2004 to 2018. Lancet Reg Health West Pac 2023;44:100989. 10.1016/j.lanwpc.2023.100989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The Ministry of Industry and Information Technology of China. Catalogue of Smart Health and Elderly Care Products and Services Promotion (2022 Edition). 2023. https://wap.miit.gov.cn/zwgk/wjgs/art/2023/art_f6f7f2f5dd454afa81276687db9f5c44.html.
- 15.China National Health Commission. Statistical bulletin on the development of health care in 2022. 2023. https://www.gov.cn/lianbo/bumen/202310/content_6908686.
- 16.General Office of the State Council of China. China’s medium - and long term plan for the prevention and treatment of chronic non-communicable diseases (2017-2025). 2017. https://www.gov.cn/zhengce/content/2017-02/14/content_5167886.htm.
- 17. Yip W, Fu H, Chen AT, et al. 10 years of health-care reform in China: progress and gaps in Universal Health Coverage. Lancet 2019;394:1192-204. 10.1016/S0140-6736(19)32136-1 [DOI] [PubMed] [Google Scholar]
- 18. Mavrodaris A, Lafortune L, Brayne CE. The future longevity: designing a synergistic approach for healthy ageing, sustainability, and equity. Lancet Healthy Longev 2022;3:e584-6. 10.1016/S2666-7568(22)00145-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Xue T, Wang R, Wang M, et al. Health benefits from the rapid reduction in ambient exposure to air pollutants after China’s clean air actions: progress in efficacy and geographic equality. Natl Sci Rev 2023;11:nwad263. 10.1093/nsr/nwad263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ikegami N. Financing long-term care: lessons from Japan. Int J Health Policy Manag 2019;8:462-6. 10.15171/ijhpm.2019.35 [DOI] [PMC free article] [PubMed] [Google Scholar]