Abstract
Intimate partner violence (IPV) can increase a person’s risk of HIV and other sexually transmitted infections (STIs), and may affect access to sexual health services. We assessed the prevalence of HIV screening and IPV among heterosexually-active persons using data from the 2016 National HIV Behavioral Surveillance. Participants were eligible if they were 18–60 years old, could complete the interview in English or Spanish, and reported having sex with an opposite sex partner in the previous 12 months. People who reported neither injection drug use within the past 12 months nor prior HIV diagnosis, and persons with valid responses to questions regarding HIV screening and physical/sexual IPV within the past 12 months were included (N=7,777). Overall, 17% reported IPV in the previous 12 months and 19% had never had HIV screening. Abused persons were more likely to have been screened for HIV and to report high risk behaviors than non-abused persons. There was no difference in the proportion being offered HIV screening by their health care provider in the previous year. Findings suggest an integrated approach to violence prevention and sexual health may help increase awareness about clinical best practices and reduce risk for HIV/STIs among at-risk communities.
Keywords: intimate partner violence, HIV infection, sexual health, screening, testing
Introduction
In the U.S., nearly one in three persons will experience sexual violence, physical violence, or stalking by an intimate partner in their lifetime (Smith et al., 2018). Intimate partner violence (IPV) is a serious public health problem with an estimated total population cost of $3.6 trillion (Bonomi et al., 2009). In addition to physical injuries, IPV victims are at increased risk of chronic health conditions and mental health concerns, and risky sexual behaviors such as inconsistent or lack of condom use (Bacchus et al., 2018). A person’s ability to negotiate safe sexual practices can be compromised within the context of abusive relationships (Coker, 2007; Grace & Anderson, 2018; Park et al., 2016). In a recent meta-analysis, pooled results indicated physical IPV and sexual IPV were significantly associated with HIV infection among women (Li et al., 2014). Accordingly, other studies have explored the link between partner violence and risk of HIV and other sexually transmitted infections (STIs) though most have focused on violence perpetrated against women (Decker et al., 2009; Frye et al., 2011; Hess et al., 2012; Li et al., 2014; Raj et al., 2008).
In 2019, 23% of new HIV diagnoses were attributable to heterosexual contact in the U.S. (CDC, 2019a). Persons of lower socioeconomic status (SES), racial/ethnic minorities, and women are disproportionately affected by heterosexually acquired HIV (CDC, 2019a; DiNenno et al., 2012). HIV screening is essential for timely linkage to care and treatment after an HIV diagnosis, reducing transmission of infection, and improving health and quality of life. The US Preventive Services Task Force (USPSTF) recommends screening for HIV infection for all persons aged 15–65 years and repeat screening for those at increased risk (USPSTF et al., 2019). Yet, HIV screening in the general U.S. population is low (36–41%) (Brown et al., 2013; Nasrullah et al., 2013; Pitasi et al., 2018; Rountree et al., 2016), and one in seven (14%) of the 1.1 million people living with HIV have not received a diagnosis (CDC, 2019b). In 2019, the U.S. Department of Health and Human Services proposed a national initiative to end the HIV epidemic within 10 years, of which screening to diagnose individuals with HIV as early as possible after infection was listed as one of four key strategies towards achieving these goals (Fauci et al., 2019). Central to these efforts is ensuring equitable access to health care services and screening programs for populations at high risk of HIV infection, particularly those from socially and economically marginalized communities (Niyonsenga et al., 2013; Pellowski et al., 2013).
The role of IPV on health care utilization has been of growing interest (Bonomi et al., 2009; Dichter et al., 2018; Plichta, 2004). In a retrospective chart review of female patients enrolled in the Veterans Health Administration, women who reported IPV were 50% more likely to use outpatient care including psychosocial care, primary care, emergency department, or other specialty care than those who did not report IPV (Dichter et al., 2018). However, studies that assessed the association between violence victimization and HIV screening have shown conflicting results due to differences in sample characteristics (e.g., women only, low-risk population) (Brown et al., 2013; Gonzalez-Guarda et al., 2019; Mathew et al., 2013; McCall-Hosenfeld et al., 2013; Rountree et al., 2016) or limited sample size (Etudo et al., 2017; Washio et al., 2018). Moreover, some have focused broadly on general health care or preventive screenings (Cha & Masho, 2014; Dichter et al., 2018; Massetti et al., 2018), or did not consider the role of IPV on receipt of HIV screening (Diepstra et al., 2018; Pitasi et al., 2018). The paucity of studies assessing violence among men also warrants further investigation (Depraetere et al., 2020). Findings from extant literature demonstrate the importance of understanding the intersection and co-occurrence of multilevel risk factors (e.g., neighborhood poverty, low SES) contributing to HIV and violence among vulnerable populations (Brawner et al., 2021; Fox & Benson, 2006; Frew et al., 2016; Khalifeh et al., 2013; Peterman, Lindsey, & Selik, 2005).
The objectives of the current analysis were to determine the prevalence of partner violence victimization and HIV screening among heterosexually active women and men with low SES, evaluate the association between IPV and HIV screening, and assess factors associated with IPV and with HIV screening. Findings may help identify gaps in prevention and outreach among persons at risk of infection, and better elucidate the relationship between IPV and HIV screening to inform policies on violence prevention and sexual health.
Methods
Study population
For this cross-sectional study, data came from the CDC’s National HIV Behavioral Surveillance (NHBS) which collects behavioral information on HIV risk factors, HIV testing history, and receipt of health services, along with HIV test results, among populations at high risk for HIV infection. During 2016, heterosexually active persons of low SES were recruited from 17 U.S. urban cities using respondent-driven sampling (RDS) (Heckathorn, 2002). NHBS sampling methods are further described elsewhere (CDC, 2018b, 2018a). Participants were eligible if they were male or female (not transgender), 18–60 years old, resided in one of the participating cities, could complete the interview in English or Spanish, and reported having sex with an opposite sex partner in the previous 12 months. Additional inclusion criteria were low SES (defined as living in poverty or having completed no more than high school education) and no reported injection drug use in the previous 12 months. Men who reported ever having sex with men were excluded. Eligible participants completed an anonymous, standardized questionnaire administered by trained interviewers. Activities for NHBS were approved by the Centers for Disease Control and Prevention (CDC, 2018a) and applicable institutional review boards in each participating city.
Variables of interest
In the analytic sample, people who reported no prior HIV diagnosis, and those with valid responses to questions about ever being screened for HIV (outcome of interest) and experience with physical or sexual IPV victimization over the previous 12 months (exposure of interest) were included in the analyses (N=7,777). Experience with physical violence (i.e., slapped, punched, shoved, kicked, shaken or otherwise physically hurt) or sexual violence (i.e., forced or pressured to have vaginal, oral or anal sex) by a partner in the previous 12 months was combined into a single variable with dichotomized response (IPV; no IPV) given the co-occurrence of violence types and ease of interpretation.
Potential covariates included gender, age group, race/ethnicity, education, household income based on the 2015 federal poverty level (U.S. Department of Health and Human Services, 2015), and insurance status. Participants reported whether a health care provider had offered HIV screening in the past 12 months which differs from the outcome of interest defined as ever receiving HIV screening, and behavioral risk factors for HIV (e.g., ever injected drugs, exchanged sex for money or drugs with a casual partner in the past 12 months, condomless sex with an HIV positive partner in the past 12 months).
Statistical analysis
Descriptive statistics were used to assess the distribution of sample characteristics by HIV screening and IPV status. Crude and adjusted prevalence ratios (cPR, aPR) and 95% confidence intervals (CIs) were generated using modified Poisson regression models with generalized estimation equations (GEE) (Avery et al., 2019; Zou, 2004). To account for interdependence of observations, models accounted for clustering by RDS recruitment chains. P-values were based on Wald statistics for Type 3 GEE. Gender and race/ethnicity were assessed for interaction with IPV but were not found to be statistically significant (p>0.05); therefore, results were not stratified by gender or race/ethnicity. Multivariable models provided aPRs controlling for city and network size. Analyses were conducted using SAS statistical software version 9.4.
Results
Overall, 16.8% of participants reported IPV in the past 12 months. The majority of respondents were female (54.8%), were aged ≤39 years (54.2%), were of a minority racial/ethnic group (71.4% black, 20.0% Hispanic), lived at or below the federal poverty level (84%), and had health insurance (Table 1). Factors associated with IPV included age, race/ethnicity, education, income, and insurance (p<0.05). IPV prevalence was highest among persons aged 25–29 years, persons in poverty, and those with other or multiple types of health insurance or no insurance. There were no gender differences by IPV status (p=0.2014) and abused persons were not significantly more likely to be offered HIV screening than non-abused individuals (38.1% vs. 36.6%; p=0.4191). People who experienced IPV were more likely to report risk factors and adverse health behaviors than those with no IPV such as: ever engaging in injection drug use, having a last sex partner who ever injected drugs or who had sex with other people, receiving an STD diagnosis, exchanging sex for money or drugs, or having four or more sex partners in the past 12 months (Figure).
Table 1:
Distribution of characteristics by intimate partner violence victimization and prevalence of intimate partner violence victimization among heterosexually active persons – National HIV Behavioral Surveillance, 2016
| Total N = 7,777 | Intimate Partner Violence N = 1,303 | No Intimate Partner Violence N = 6,474 | Intimate Partner Violence N = 1,303 | No Intimate Partner Violence N = 6,474 | p-value | |
|---|---|---|---|---|---|---|
|
| ||||||
| Column % | Row % | |||||
| Gender | 0.2014 | |||||
| Male | 45.3 | 43.8 | 45.6 | 16.2 | 83.8 | |
| Female | 54.8 | 56.3 | 54.5 | 17.2 | 82.8 | |
| Age (years) | <.0001 | |||||
| 18–24 | 19.6 | 20.2 | 19.5 | 17.3 | 82.7 | |
| 25–29 | 13.9 | 16.7 | 13.3 | 20.1 | 79.9 | |
| 30–39 | 20.7 | 24.6 | 19.9 | 19.9 | 80.1 | |
| 40–49 | 20.2 | 19.7 | 20.3 | 16.4 | 83.7 | |
| 50–60 | 25.6 | 18.9 | 27.0 | 12.3 | 87.7 | |
| Race/Ethnicity | <.0001 | |||||
| Black | 71.4 | 69.8 | 71.8 | 16.4 | 83.7 | |
| Hispanic | 20.0 | 18.0 | 20.5 | 15.0 | 85.0 | |
| White | 3.6 | 4.9 | 3.3 | 22.7 | 77.3 | |
| Other | 4.9 | 7.4 | 4.4 | 25.1 | 74.9 | |
| Education | 0.0304 | |||||
| <High School | 29.2 | 28.9 | 29.2 | 16.6 | 83.4 | |
| High School | 53.6 | 51.3 | 54.1 | 16.0 | 84.0 | |
| >High School | 17.2 | 19.7 | 16.7 | 19.2 | 80.8 | |
| Household income | 0.0083 | |||||
| Above the Federal Poverty Level | 15.9 | 12.8 | 16.5 | 13.5 | 86.5 | |
| At or Below the Federal Poverty Level | 84.1 | 87.2 | 83.5 | 17.4 | 82.6 | |
| Insurance | 0.0108 | |||||
| Private | 6.8 | 4.6 | 7.2 | 11.2 | 88.8 | |
| Medicaid | 49.4 | 50.0 | 49.3 | 16.9 | 83.1 | |
| Medicare | 4.2 | 3.4 | 4.3 | 13.7 | 86.3 | |
| Other | 10.5 | 10.9 | 10.4 | 17.4 | 82.7 | |
| Multiple | 5.5 | 6.1 | 5.4 | 18.4 | 81.6 | |
| None | 23.7 | 25.1 | 23.5 | 17.6 | 82.4 | |
| HIV Screening Offered by Health Care Provider (in Past 12 months) | 0.4191 | |||||
| Offered | 36.6 | 38.1 | 36.4 | 17.4 | 82.6 | |
| Not Offered | 44.8 | 43.4 | 45.0 | 16.2 | 83.8 | |
| No Visit | 18.6 | 18.5 | 18.6 | 16.6 | 83.4 | |
Note: Race/ethnicity categories are mutually exclusive and Hispanics can be of any race; household income is based on the 2015 federal poverty level; p-value based on Wald statistics for Type 3 generalized estimating equations (GEE) clustered on recruitment chains and adjusted for city of interview and network size.
Figure:
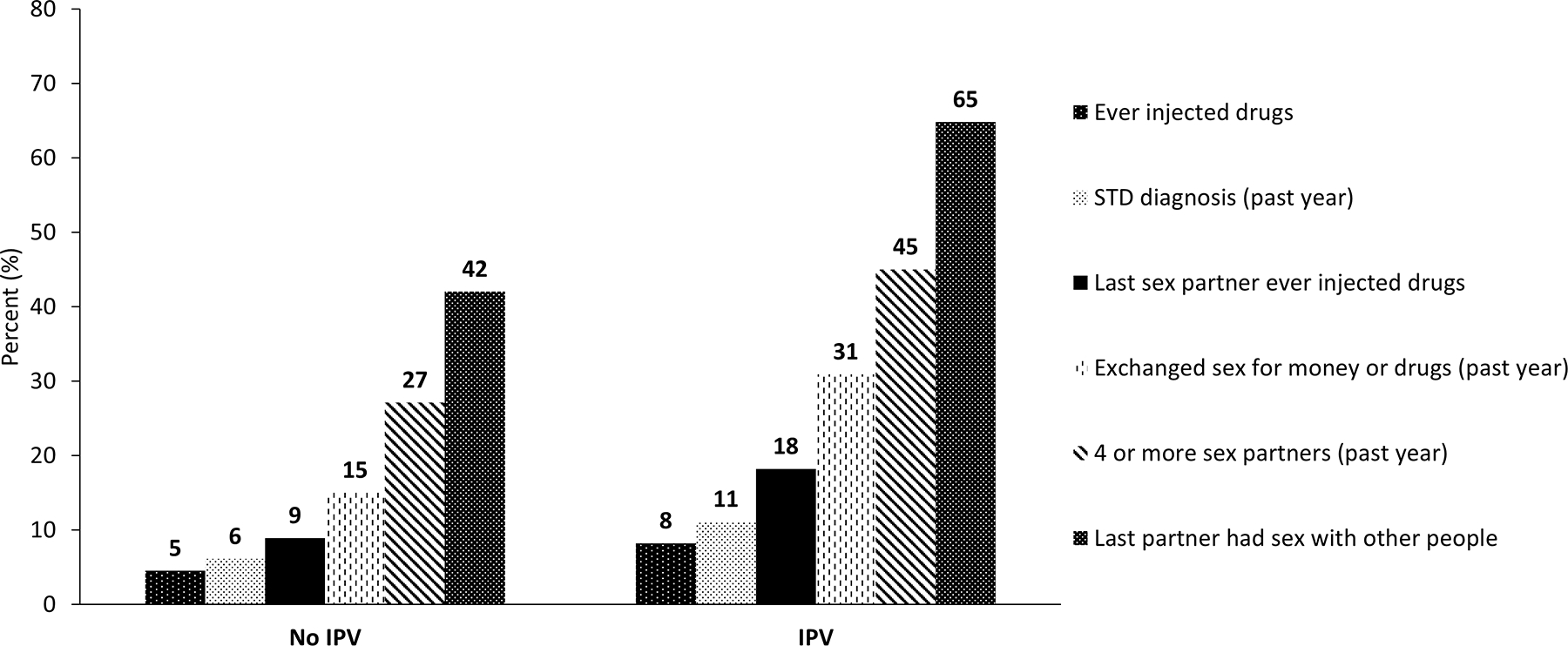
Prevalence of risk factors by intimate partner violence status among heterosexually active persons – National HIV Behavioral Surveillance, 2016. All factors were more common among persons experiencing IPV than no IPV (all p-values <.0001).
Table 2 shows the prevalence of HIV screening by IPV status and other characteristics. Most participants had been screened for HIV (81%). Thirty-seven percent of participants were offered HIV screening by their health care provider in the past 12 months, 45% were not offered HIV screening by their health care provider in the past 12 months, and 19% reported no visit to a health care provider. Among those who saw a health care provider in the past 12 months, only 10% of people who had never been screened were offered HIV screening (not in tables). Participants whose health care providers never offered screening had higher prevalence of no HIV screening (27%) than those who were offered screening (4%). HIV screening was more prevalent among persons who had ever injected drugs, persons who received an STD diagnosis within the past 12 months, and those who had a sexual partner who had sex with other people. Nearly one in five persons who reported exchanging sex for money or drugs, four or more sexual partners, or condomless sex with HIV-positive partner in the past 12 months were never screened for HIV.
Table 2:
Prevalence of HIV screening by characteristics among heterosexually active persons – National HIV Behavioral Surveillance, 2016
| Total N = 7,777 | Ever Screened N = 6,273 | Never Screened N = 1,504 | Crude PR (95% CI) | Adjusted PR (95% CI) | |
|---|---|---|---|---|---|
|
| |||||
| Row % | |||||
| IPV (in Past 12 months) | |||||
| Yes | 16.8 | 82.9 | 17.1 | 1.03 (1.01–1.06) | 1.03 (1.00–1.06) |
| No | 83.3 | 80.2 | 19.8 | 1.0 | 1.0 |
| Socio-demographic | |||||
| Gender | |||||
| Male | 45.3 | 77.8 | 22.3 | 0.94 (0.91–0.96) | 0.92 (0.90–0.95) |
| Female | 54.8 | 83.1 | 16.9 | 1.0 | 1.0 |
| Age (years) | |||||
| 18–24 | 19.6 | 66.0 | 34.0 | 0.81 (0.76–0.85) | 0.81 (0.77–0.86) |
| 25–29 | 13.9 | 82.0 | 18.0 | 1.0 | 1.0 |
| 30–39 | 20.7 | 88.5 | 11.6 | 1.08 (1.04–1.12) | 1.08 (1.04–1.12) |
| 40–49 | 20.2 | 85.8 | 14.3 | 1.05 (1.01–1.09) | 1.04 (1.01–1.08) |
| 50–60 | 25.6 | 80.8 | 19.2 | 0.99 (0.95–1.03) | 0.98 (0.94–1.01) |
| Race/Ethnicity | |||||
| Black | 71.4 | 83.9 | 16.1 | 1.15 (1.05–1.26) | 1.08 (1.01–1.15) |
| Hispanic | 20.0 | 70.4 | 29.6 | 0.96 (0.87–1.07) | 0.94 (0.87–1.03) |
| White | 3.6 | 73.0 | 27.0 | 1.0 | 1.0 |
| Other | 4.9 | 82.0 | 18.0 | 1.12 (1.02–1.22) | 1.09 (1.01–1.19) |
| Education | |||||
| <High School | 29.2 | 79.9 | 20.1 | 0.94 (0.90–0.98) | 0.92 (0.88–0.95) |
| High School | 53.6 | 79.6 | 20.4 | 0.93 (0.89–0.97) | 0.91 (0.88–0.95) |
| >High School | 17.2 | 85.3 | 14.7 | 1.0 | 1.0 |
| Household income | |||||
| Above the Federal Poverty Level | 15.9 | 76.2 | 23.8 | 1.0 | 1.0 |
| At or Below the Federal Poverty Level | 84.1 | 81.6 | 18.4 | 1.07 (1.02–1.12) | 1.06 (1.02–1.10) |
| Insurance | |||||
| Private | 6.8 | 73.0 | 27.1 | 1.0 | 1.0 |
| Medicaid | 49.4 | 83.6 | 16.4 | 1.15 (1.04–1.26) | 1.12 (1.03–1.22) |
| Medicare | 4.2 | 82.9 | 17.1 | 1.14 (1.03–1.25) | 1.11 (1.02–1.20) |
| Other | 10.5 | 78.3 | 21.7 | 1.07 (0.96–1.20) | 1.12 (1.03–1.22) |
| Multiple | 5.5 | 86.8 | 13.2 | 1.19 (1.08–1.32) | 1.15 (1.06–1.26) |
| None | 23.7 | 76.3 | 23.7 | 1.05 (0.96–1.14) | 1.02 (0.95–1.10) |
| HIV Screening Offered by Health Care Provider (in Past 12 months) | |||||
| Offered | 36.6 | 96.3 | 3.7 | 1.0 | 1.0 |
| Not Offered | 44.8 | 72.9 | 27.1 | 0.76 (0.72–0.79) | 0.78 (0.74–0.81) |
| No Visit | 18.6 | 68.7 | 31.3 | 0.71 (0.67–0.76) | 0.73 (0.69–0.77) |
| Risk Factors for HIV | |||||
| Ever Injected Drugs | |||||
| Yes | 5.1 | 85.6 | 14.4 | 1.06 (1.02–1.11) | 1.07 (1.02–1.11) |
| No | 94.9 | 80.4 | 19.6 | 1.0 | 1.0 |
| Last Sexual Partner Ever Injected Drugs | |||||
| Yes | 10.5 | 79.8 | 20.2 | 0.99 (0.95–1.03) | 1.00 (0.95–1.04) |
| No | 89.5 | 80.8 | 19.3 | 1.0 | 1.0 |
| Exchanged Sex for Money or Drugs With Casual Partner(s) (in Past 12 months) | |||||
| Yes | 17.7 | 82.9 | 17.1 | 1.03 (1.00–1.07) | 1.00 (0.98–1.03) |
| No | 82.3 | 80.2 | 19.8 | 1.0 | 1.0 |
| Condomless Sex With HIV Positive Partner (in Past 12 months) | |||||
| Yes | 1.1 | 81.8 | 18.2 | 1.01 (0.87–1.17) | 0.97 (0.83–1.14) |
| No | 98.9 | 81.0 | 19.1 | 1.0 | 1.0 |
| Number of Sexual Partners (in Past 12 months) | |||||
| 1 partner | 36.4 | 81.5 | 18.5 | 1.0 | 1.0 |
| 2 partners | 20.0 | 81.3 | 18.7 | 1.00 (0.97–1.03) | 1.00 (0.97–1.03) |
| 3 partners | 13.6 | 81.4 | 18.6 | 1.00 (0.95–1.05) | 0.99 (0.95–1.04) |
| ≥4 partners | 30.1 | 78.9 | 21.1 | 0.97 (0.93–1.00) | 0.96 (0.93–0.99) |
| Last Sexual Partner Had Sex With Other People (in Past 12 months) | |||||
| Yes | 45.8 | 81.9 | 18.1 | 1.03 (1.01–1.05) | 1.02 (1.00–1.04) |
| No | 54.2 | 79.5 | 20.5 | 1.0 | 1.0 |
| STD Diagnosis (in Past 12 months) | |||||
| Yes | 6.9 | 84.1 | 15.9 | 1.05 (1.01–1.09) | 1.04 (1.00–1.07) |
| No | 93.1 | 80.4 | 19.6 | 1.0 | 1.0 |
| Any Risk Behavior | |||||
| Yes | 66.3 | 81.6 | 18.4 | 1.03 (1.0–1.05) | 1.01 (0.99–1.04) |
| No | 33.7 | 79.5 | 20.5 | 1.0 | 1.0 |
PR, prevalence ratio; STD, sexually transmitted disease.
Note: Race/ethnicity categories are mutually exclusive and Hispanics can be of any race; household income is based on the 2015 federal poverty level; any risk behavior (i.e., ever injected drugs, last sexual partner ever injected drugs, exchanged sex for money or drugs with casual partner(s) in past 12 months, condomless sex with HIV positive partner in past 12 months, four or more sexual partners in past 12 months, last sexual partner had sex with other people in past 12 months, STD diagnosis in past 12 months); log-linked Poisson Regression was generated using generalized estimating equations (GEE) clustered on recruitment chains from seeds in respondent-driven sampling. Adjusted model controls for city of interview and network size. Bolded statistically significant results.
Persons who experienced IPV had greater prevalence of HIV screening than those with no IPV (aPR=1.03, 95% CI=1.00–1.06). Compared to heterosexually active persons who were offered HIV screening by their health care provider in the past 12 months, those who were not offered (aPR=0.78, 95% CI=0.74–0.81) and those who did not visit a provider (aPR=0.73, 95% CI=0.69–0.77) were significantly less likely to get screened. People who reported ever injecting drugs and people diagnosed with an STD in the prior 12 months were more likely to have HIV screening than their counterparts (aPR=1.07, 95% CI=1.02–1.11; aPR=1.04, 95% CI=1.00–1.07; respectively). However, persons with four or more sexual partners in the past 12 months were significantly less likely to be screened (79%) than those reporting one sexual partner (82%) (aPR=0.96, 95% CI=0.93–0.99).
Discussion
One in six heterosexually active persons of low SES (17%) experienced physical or sexual violence from an intimate partner in the previous 12 months. There were no gender differences in IPV prevalence, which is notable given the under-recognition of male victimization in scientific research (Depraetere et al., 2020; Miller & McCaw, 2019). IPV prevalence in the current analysis was higher than general population estimates from the 2015 National Intimate Partner and Sexual Violence Survey where 5.5% of women and 5.2% of men reported sexual violence, physical violence, and/or stalking by an intimate partner in the past 12 months (Smith et al., 2018). Differences could reflect a greater risk for violence victimization among NHBS participants who were all of low SES (Jewkes, 2002). Other studies conducted in multiple settings have reported past-year IPV prevalence ranging 2–18% among women (Brown et al., 2013; Dichter et al., 2018; Mathew et al., 13 C.E.; McCall-Hosenfeld et al., 2013; Washio et al., 2018), and lifetime IPV prevalence of 24% among women and 11% among men (Massetti et al., 2018).
Consistent with other studies, persons who experienced IPV were significantly more likely to have HIV screening than those who did not report IPV (Brown et al., 2013; McCall-Hosenfeld et al., 2013; Nasrullah et al., 2013). It is notable that abused persons, while more likely to screen, were not more likely to be offered testing by their health provider which suggests screenings could have been self-initiated rather than provider-driven. Seeking HIV screening may stem from patient concerns about contracting STIs from abusive partners or their lack of or reduced ability to control sexual decision-making such as negotiating consistent condom use (Bergmann & Stockman, 2015; Coker, 2007; Decker et al., 2009; Frye et al., 2011; Grace & Anderson, 2018; Park et al., 2016; Raj et al., 2008). A study that assessed HIV screening among persons seeking social services for IPV at a family justice center found clients who experienced greater severity in violence were more likely to request screening for HIV or other STIs (Gonzalez-Guarda et al., 2019).
Overall lifetime HIV screening in the general U.S. population ranges from 36–41% (Brown et al., 2013; Nasrullah et al., 2013; Pitasi et al., 2018; Rountree et al., 2016). Although screening among high risk individuals is more common (62–76%) (Diepstra et al., 2018; Etudo et al., 2017; Pitasi et al., 2018), as was observed in the current analysis (79–86%), it falls short of recommendations that everyone be screened. A recent analysis using data from the 2006–2016 General Social Survey of non-institutionalized U.S. adults reported 38% of persons with HIV-related risk behaviors (e.g., persons with multiple sex partners or who exchanged sex for money) in the previous 12 months were never tested for HIV (Pitasi et al., 2018). Similar findings were observed in the current analysis where one in five persons who reported high risk behaviors (e.g., exchanging sex for money or drugs, four or more sexual partners) were never screened for HIV. These results underscore important gaps in HIV prevention efforts despite the availability of low-cost and reliable tests, and potential added years of life with early diagnosis and treatment (Branson et al., 2006).
Extant literature has identified numerous patient barriers to HIV screening such as fear, stigma, financial burden, time constraints, and difficulties with accessing and navigating the health care system (Evangeli et al., 2016; Gwadz et al., 2018; Tokar et al., 2018; Wise et al., 2019). These barriers are facilitated or mitigated by complex, overlapping economic systems and social structures that shape the conditions in which people live, work, and access health care (CDC, 2010). Although individual level factors may influence a person’s decision to seek care and testing, missed opportunities by providers to discuss and offer HIV screening was noted in the current analysis. Among participants who saw a health care provider in the past 12 months, only 10% of those who were never screened were offered HIV screening. HIV screening is recommended for patients in all health-care settings and persons at high risk for HIV infection should be screened at least annually (Branson et al., 2006). These gaps demonstrate missed opportunities for HIV screening given the sample comprised of individuals from economically disadvantaged backgrounds who may already encounter difficulties with accessing or using health care and prevention services. The prevalence of no HIV screening was substantially higher among participants who were never offered HIV screening by their provider than those who were offered screening (27% vs. 4%). Health care workers who offer and provide HIV screening play a critical role in improving population health outcomes through early diagnosis, and linkages to care and prevention.
Screening is particularly germane in cases where persons experiencing violence seek medical services for care related to or secondary to their injuries. Indeed, those in the current analysis who reported IPV had higher prevalence of risk factors for HIV infection than persons reporting no IPV. Given the high prevalence of IPV, particularly among persons of low SES, routine IPV assessment should be incorporated in health care settings which provide the advantages of privacy and safety, opportunities for meaningful discussions about sexual health and healthy relationships, and support to community resources and additional services (Basile et al., 2007; Miller & McCaw, 2019). An integrated approach to violence prevention and sexual health can raise awareness that IPV is an important health issue and improve a clinician’s ability to provide patient-centered, appropriate care to abused individuals and linkages to social and medical services, e.g., HIV screening and treatment.
There were several limitations. The cross-sectional study design limits the ability to infer a causal relationship between the exposure and outcome of interest. IPV prevalence is likely underestimated in the population because we did not account for other forms of violence (e.g., emotional or psychological). Experiences with physical or sexual violence were combined rather than assessed separately. Self-reported data may be subject to socially desirable responses and recall bias. We did not assess other factors that could have affected HIV screening such as receipt of IPV screening which could have potentially affected some providers’ decision to offer HIV screening. Lastly, participants were recruited from 17 U.S. cities with high HIV prevalence and data are unweighted; thus, results may not be generalizable to individuals living in other cities or non-urban areas.
Overall, our findings indicate important gaps. Seventeen percent of participants reported physical or sexual IPV in the past 12 months and there were no significant gender differences in victimization. One in five heterosexually active persons were never screened for HIV. People who experienced IPV were more likely to get screened than those who did not report IPV; however, they were not more likely to be offered HIV screening by their health care provider. CDC’s Let’s Stop HIV Together communication campaign provides education materials for health providers on HIV screening, treatment, and prevention and risk reduction strategies (CDC, 2020). Clinicians should provide routine screening and counseling to everyone with no history of HIV screening or unknown HIV test result, with special considerations for those who may be in abusive relationships. A comprehensive approach that integrates violence prevention and sexual health services may help increase awareness about clinical best practices, improve access to care, and reduce risk for HIV and other STIs among at-risk communities (Prowse et al., 2014). Limited research among male IPV victims warrant further investigations to evaluate screening tools, interventions, and sexual health outcomes for men experiencing partner violence (USPSTF et al., 2018).
Acknowledgements
We thank all of the National HIV Behavioral Surveillance (NHBS) 2016 participants. We also thank members of the NHBS Study Group: Atlanta, Georgia: Pascale Wortley, Jeff Todd, David Melton; Boston, Massachusetts: Monina Klevens, Rose Doherty, Chris Wittke; Dallas, Texas: Jonathon Poe, Shane Sheu, Alicia Novoa; Denver, Colorado: Alia Al-Tayyib, Melanie Mattson; Los Angeles, California: Ekow Kwa Sey, Yingbo Ma; Memphis, Tennessee: Shanell McGoy, Samantha Mathieson, Ayesha Sarwar; Miami, Florida: Emma Spencer, John-Mark Schacht, David Forrest; Nassau-Suffolk, New York: Bridget Anderson, Ashley Tate, Anthony Romano; New Orleans, Louisiana: William T. Robinson, Narquis Barak, Jeremy M. Beckford; Newark, New Jersey: Barbara Bolden, Afework Wogayehu, Henry Godette; Philadelphia, Pennsylvania: Kathleen A. Brady, Chrysanthus Nnumolu, Jennifer Shinefeld; Portland, Oregon: Sean Schafer, E. Roberto Orellana, Amisha Bhattari; San Diego, California: Lynn Walton-Hayes, Anna Flynn, Elizabeth Lampley; San Francisco, California: H. Fisher Raymond, Theresa Ick; San Juan, Puerto Rico: Sandra Miranda De León, Yadira Rolón-Colón; Virginia Beach, Virginia: Celestine Buyu, Karen Diepstra, Toyah Reid; Washington, D.C.: Jenevieve Opoku, Irene Kuo; and the Centers for Disease Control and Prevention (CDC) Behavioral Surveillance Team.
Footnotes
Disclosure statement
The authors declare that they have no conflict of interest.
Disclaimer: The findings and conclusions in this paper are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. Use of trade names is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services, the Public Health Service, or the Centers for Disease Control and Prevention.
References
- Avery L, Rotondi N, McKnight C, Firestone M, Smylie J, & Rotondi M (2019). Unweighted regression models perform better than weighted regression techniques for respondent-driven sampling data: results from a simulation study. BMC Medical Research Methodology, 19(1), 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bacchus LJ, Ranganathan M, Watts C, & Devries K (2018). Recent intimate partner violence against women and health: A systematic review and meta-analysis of cohort studies. BMJ Open, 8(7), 1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basile KC, Hertz MF, & Back SE (2007). Intimate Partner Violence and Sexual Violence Victimization Assessment Instruments for Use in Healthcare Settings: Version 1. https://www.cdc.gov/violenceprevention/pdf/ipv/ipvandsvscreening.pdf
- Bergmann JN, & Stockman JK (2015). How Does Intimate Partner Violence Affect Condom and Oral Contraceptive Use in the United States?: A Systematic Review of the Literature. Contraception, 91(6), 438–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonomi AE, Anderson ML, Rivara FP, & Thompson RS (2009). Health Care Utilization and Costs Associated with Physical and Nonphysical-Only Intimate Partner Violence. Health Services Research, 44(3), 1052–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branson BM, Handsfield HH, Lampe MA, Janssen RS, Taylor AW, Lyss SB, Clark JE, & Centers for Disease Control and Prevention. (2006). Revised Recommendations for HIV Testing of Adults, Adolescents, and Pregnant Women in Health-Care Settings. MMWR Morbidity Mortality Weekly Report, 55(RR-14), 1–17. [PubMed] [Google Scholar]
- Brawner BM, Kerr J, Castle BF, Bannon JA, Bonett S, Stevens R, James R, & Bowleg L (2021). A systematic review of neighborhood-level influences on HIV vulnerability. AIDS and Behavior, 26, 874–934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown MJ, Weitzen S, & Lapane KL (2013). Association Between Intimate Partner Violence and Preventive Screening Among Women. Journal of Women’s Health, 22(11), 947–952. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2010). Establishing a holistic framework to reduce inequities in HIV, viral hepatitis, STDs, and tuberculosis in the United States. https://www.cdc.gov/nchhstp/socialdeterminants/docs/SDH-White-Paper-2010.pdf [Google Scholar]
- Centers for Disease Control and Prevention. (2018a). HIV Infection, Risk, Prevention, and Testing Behaviors Among Heterosexuals at Increased Risk for HIV Infection National HIV Behavioral Surveillance 17 U.S. Cities, 2016. https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-number-19.pdf
- Centers for Disease Control and Prevention. (2018b). National HIV Behavioral Surveillance System Round 5: Model Surveillance Protocol. https://www.cdc.gov/hiv/pdf/statistics/systems/nhbs/NHBS_Model_Protocol_Round5.pdf
- Centers for Disease Control and Prevention. (2019a). HIV Surveillance Report: Diagnoses of HIV Infection in the United States and Dependent Areas, 2019 (vol. 32). https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2018-updated-vol-32.pdf
- Centers for Disease Control and Prevention. (2019b). HIV Basic Statistics. https://www.cdc.gov/hiv/basics/statistics.html
- Centers for Disease Control and Prevention. (2020). Let’s Stop HIV Together. https://www.cdc.gov/stophivtogether/index.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Factagainstaids%2Findex.html
- Cha S, & Masho SW (2014). Intimate Partner Violence and Utilization of Prenatal Care in the United States. Journal of Interpersonal Violence, 29(5), 911–927. [DOI] [PubMed] [Google Scholar]
- Coker AL (2007). Does Physical Intimate Partner Violence Affect Sexual Health? A Systematic Review. Trauma Violence Abuse, 8(2), 149–177. [DOI] [PubMed] [Google Scholar]
- Decker MR, Seage GR, Hemenway D, Gupta J, Raj A, & Wilverman JG (2009). Intimate partner violence perpetration, standard and gendered STI/HIV risk behaviour, and STI/HIV diagnosis among a clinic-based sample of men. Sexually Transmitted Diseases, 85(7), 555–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Depraetere J, Vandeviver C, Vander Beken T, & Keygnaert I (2020). Big boys don’t cry: A critical interpretive synthesis of male sexual victimization. Trauma, Violence, & Abuse, 21(5), 991–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dichter ME, Sorrentino AE, Haywood TN, Bellamy SL, Medvedeva E, Roberts CB, & Iverson KM (2018). Women’s Healthcare Utilization Following Routine Screening for Past-Year Intimate Partner Violence in the Veterans Health Administration. Journal of General Internal Medicine, 33(6), 936–941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diepstra KL, Cunningham T, Rhodes AG, Yerkes LE, & Buyu CA (2018). Prevalence and Predictors of Provider-Initiated HIV Test Offers Among Heterosexual Persons at Increased Risk for Acquiring HIV Infection - Virginia, 2016. MMWR Morbidity Mortality Weekly Report, 67(25), 714–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiNenno EA, Oster AM, Sionean C, Denning P, & Lansky A (2012) Piloting a system for behavioral surveillance among heterosexuals at increased risk of HIV in the United States. The Open AIDS Journal, 6(1), 169–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etudo O, Metheny N, Stephenson R, & Kalokhe AS (2017). Intimate Partner Violence Is Linked to Less HIV Testing Uptake Among High-Risk, HIV-negative Women in Atlanta. AIDS Care, 29(8), 953–956. [DOI] [PubMed] [Google Scholar]
- Evangeli M, Pady K, & Wroe AL (2016). Which Psychological Factors Are Related to HIV Testing? A Quantitative Systematic Review of Global Studi. AIDS and Behavior, 20(4), 880–918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fauci AS, Redfield RR, Sigounas G, Weahkee MD, & Giroir BP (2019). Ending the HIV Epidemic: A Plan for the United States. JAMA - Journal of the American Medical Association, 321(9), 844–845. [DOI] [PubMed] [Google Scholar]
- Fox GL, & Benson ML (2006) Household and neighborhood contexts of intimate partner violence. Public Health Reports, 121, 419–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frew PM, Parker K, Vo L, Haley D, O’Leary A, Diallo DD, Golin CE, Kuo I, Soto-Torres L, Wang J, Adimora AA, Randall LA, del Rio C, Hodder S, and the HIV Prevention Trials Network 064 (HTPN) Study Team. (2016). Socioecological factors influencing women’s HIV risk in the United States: qualitative findings from the women’s HIV SeroIncidence study (HPTN 064). BMC Public Health, 16, 803–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frye V, Ompad D, Chan C, Koblin B, Galea S, & Vlahov D (2011). Intimate Partner Violence Perpetration and Condom Use-Related Factors: Associations With Heterosexual Men’s Consistent Condom Use. AIDS and Behavior, 15(1), 153–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Guarda RM, Williams JR, Williams W, Lorenzo D, & Carrington C (2019). Determinants of HIV and Sexually Transmitted Infection Testing and Acquisition Among Female Victims of Intimate Partner Violence. Journal of Interpersonal Violence, 1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grace KT, & Anderson JC (2018). Reproductive Coercion: A Systematic Review. Trauma Violence Abuse, 19(4), 371–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gwadz M, Leonard NR, Honig S, Freeman R, Kutnick A, & Ritchie AS (2018). Doing Battle With “The Monster:” How High-Risk Heterosexuals Experience and Successfully Manage HIV Stigma as a Barrier to HIV Testing. International Journal for Equity in Health, 17(1), 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckathorn DD (2002). Respondent-driven sampling II: Deriving valid population estimates from chain-referral samples of hidden populations. Social Problems, 49(1), 11–34. [Google Scholar]
- Hess KL, Javanbakht M, Brown JM, Weiss RE, Hsu P, & Gorbach PM (2012). Intimate partner violence and sexually transmitted infections among young adult women. Sexually Transmitted Diseases, 39(5), 366–371. https://pubmed.ncbi.nlm.nih.gov//22504601/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jewkes R (2002). Intimate Partner Violence: Causes and Prevention. Lancet, 359(9315), 1423–1429. [DOI] [PubMed] [Google Scholar]
- Khalifeh H, Hargreaves J, Howard LM, & Birdthistle I (2013). Intimate partner violence and socioeconomic deprivation in England: Findings form a national cross-sectional survey. American Journal of Public Health, 103, 462–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Marshall CM, Rees HC, Nunez A, Ezeanolue EE, & Ehiri JE (2014). Intimate Partner Violence and HIV Infection Among Women: A Systematic Review and Meta-Analysis. Journal of the International AIDS Society, 17(1), 18845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massetti GM, Townsend JS, Thomas CC, Basile KC, & Richardson LC (2018). Healthcare Access and Cancer Screening Among Victims of Intimate Partner Violence. Journal of Women’s Health, 27(4), 607–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathew A, Smith LS, Marsh B, & Houry D (13 C.E.). Relationship of Intimate Partner Violence to Health Status, Chronic Disease, and Screening Behaviors. Journal of Interpersonal Violence, 28(12), 2581–2592. [DOI] [PubMed] [Google Scholar]
- McCall-Hosenfeld JS, Chuang CH, & Weisman CS (2013). Prospective Association of Intimate Partner Violence With Receipt of Clinical Preventive Services in Women of Reproductive Age. Womens Health Issues, 23(2), e109–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller E, & McCaw B (2019). Intimate partner violence. New England Journal of Medicine, 380(9), 850–857. [DOI] [PubMed] [Google Scholar]
- Nasrullah M, Oraka E, Breiding MJ, & Chavez PR (2013). HIV Testing and Intimate Partner Violence Among Non-Pregnant Women in 15 US states/territories: Findings From Behavioral Risk Factor Surveillance System Survey Data. AIDS and Behavior, 17(7), 2521–2527. [DOI] [PubMed] [Google Scholar]
- Niyonsenga T, Trepka MJ, Lieb S, & Maddox LM (2013). Measuring socioeconomic inequality in the incidence of AIDS: rural-urban considerations. AIDS and Behaviors, 17(2), 700–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park J, Nordstrom SK, Weber KM, & Irwin T (2016). Reproductive Coercion: Uncloaking an Imbalance of Social Power. American Journal of Obstetrics and Gynecology, 214(1), 74–78. [DOI] [PubMed] [Google Scholar]
- Pellowski JA, Kalichman SC, Matthews KA, & Adler N (2013). A pandemic of the poor: social disadvantage and the U.S. HIV epidemic. American Psychologist, 68(4), 197–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterman TA, Lindsey CA, & Selik RM (2005) This place is killing me: a comparison of counties where the incidence rates of AIDS increased the most and the least. The Journal of Infectious Diseases, 191(Suppl 1), S123–S126. [DOI] [PubMed] [Google Scholar]
- Pitasi MA, Delaney KP, Oraka E, Bradley H, DiNenno EA, Brooks JT, & Prejean J (2018). Interval Since Last HIV Test for Men and Women With Recent Risk for HIV Infection - United States, 2006–2016. MMWR Morbidity Mortality Weekly Report, 67(24), 677–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plichta SB (2004). Intimate Partner Violence and Physical Health Consequences: Policy and Practice Implications. Journal of Interpersonal Violence, 19(11), 1296–1323. [DOI] [PubMed] [Google Scholar]
- Prowse KM, Logue CE, Fantasia HC, & Sutherland MA (2014). Intimate Partner Violence and the CDC’s Best-Evidence HIV Risk Reduction Interventions. Public Health Nursing, 31(3), 215–233. [DOI] [PubMed] [Google Scholar]
- Raj A, Reed E, Welles SL, Santana MC, & Silverman JG (2008). Intimate Partner Violence Perpetration, Risky Sexual Behavior, and STI/HIV Diagnosis Among Heterosexual African American Men. American Journal of Men’s Health, 2(3), 291–295. [DOI] [PubMed] [Google Scholar]
- Rountree MA, Chen L, & Bagwell M (2016). HIV-Testing Rates and Testing Locations Among Women Who Have Experienced Intimate Partner Violence: Data From the Centers for Disease Control Behavioral Risk Factor Surveillance System, 2006. Violence Against Women, 22(4), 399–414. [DOI] [PubMed] [Google Scholar]
- Smith SG, Zhang X, Basile KC, Merrick MT, Wang J, Kresnow M, & Chen J (2018). National Intimate Partner and Sexual Violence Survey: 2015 Data Brief -- Updated Release. https://www.cdc.gov/violenceprevention/pdf/2015data-brief508.pdf [DOI] [PMC free article] [PubMed]
- Tokar A, Broerse JEW, Blanchard J, & Roura M (2018). HIV Testing and Counseling Among Female Sex Workers: A Systematic Literature Review. AIDS and Behavior, 22(8), 2435–2457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. (2015). Annual update of the HHS poverty guidelines. Federal Register, 80(14), 3236–3237. [Google Scholar]
- U.S. Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, Davidson KW, Doubeni CA, Epling JW, Grossman DC, Kemper AR, Kubik M, Kurth A, Landefeld CS, Mangione CM, Silverstein M, Simon MA, Tseng C-W, & Wong JB (2018). Screening for Intimate Partner Violence, Elder Abuse, and Abuse of Vulnerable Adults: US Preventive Services Task Force Final Recommendation Statement. JAMA - Journal of the American Medical Association, 320(16), 1678–1687. [DOI] [PubMed] [Google Scholar]
- Preventive Services Taskforce US, Owens DK, Davidson KW, Krist AH, Barry MJ, Cabana M, Caughey AB, Curry SJ, Doubeni CA, Epling John W, Kubik M, Landefeld CS, Mangion CM, Pbert L, Silverstein M, Simon MA, Tseng C-W, & Wong JB (2019). Screening for HIV Infection: US Preventive Services Task Force Recommendation Statement. JAMA - Journal of the American Medical Association, 321(23), 2326–2336. [DOI] [PubMed] [Google Scholar]
- Washio Y, Wright EN, Davis-Vogel A, Chittams J, Anagnostopulos C, Kilby LM, & Teitelman AM (2018). Prior Exposure to Intimate Partner Violence Associated With Less HIV Testing Among Young Women. Journal of Interpersonal Violence, 886260518768564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wise JM, Ott C, Azuero A, Lanzi RG, Davies S, Gardner A, Vance DE, & Kempf M-C (2019). Barriers to HIV Testing: Patient and Provider Perspectives in the Deep South. AIDS and Behavior, 23(4), 1062–1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou G (2004). A modified poisson regression approach to prospective studies with binary data. American Journal of Epidemiology, 159(7), 702–706. [DOI] [PubMed] [Google Scholar]


