Abstract
INTRODUCTION
Alzheimer's disease (AD) disproportionately affects minoritized populations who remain underrepresented in AD trials.
METHODS
We partnered with local nursing community‐based organizations to implement a culturally tailored educational intervention and recruit Hispanic/Latino American, Filipino American, and Korean American adults aged 55 to 80 for the AHEAD study, a preclinical AD trial, at the University of California, Irvine.
RESULTS
We engaged 654 individuals across 21 events, leading to 71 prescreenings: 21.1% Filipino, 11.2% Hispanic/Latino, and 67.6% Korean adults. Ineligibility due to age and language barriers was common among Hispanic/Latino and Korean adults, respectively. Filipino adults often withdrew interest or were lost to follow‐up. Ultimately, 25 participants enrolled: eight Filipino, two Hispanic/Latino, and 15 Korean adults. Tailored, culturally relevant content significantly contributed to the engagement success.
DISCUSSION
This study demonstrates the value and impact of novel partnerships with health‐related provider organizations that provide trusted care and access to underrepresented communities.
Highlights
Six hundred and fifty four underrepresented individuals were reached, and 25 enrolled in the AHEAD 3‐45 trial.
Twenty‐one community events were held via partnerships with nursing and community organizations.
The study engaged 21% Filipino, 11% Hispanic/Latino, 68% Korean adults.
Community‐Based Participatory Research (CBPR) principles enhanced the recruitment process.
Transparent communication and joint planning were key.
Keywords: community, diversity, inclusion, minority, recruitment
1. BACKGROUND
Mild cognitive impairment (MCI) and dementia disproportionately impact minoritized populations within the United States. 1 , 2 Alzheimer's disease (AD) is the most common cause of these syndromes. However, minoritized groups are consistently underrepresented in AD clinical trials of pharmacological treatments. 3 This underrepresentation exacerbates health disparities and hinders equitable access to emergent therapies. 4 , 5 , 6 As underscored by the National Plan to address AD and the National Institute on Aging (NIA)’s National Strategy 7 for Clinical Research Recruitment, 8 diversifying AD clinical trial cohorts is not only essential but achievable.
Forging partnerships with community nurse leaders and community‐based organizations to recruit participants for clinical research is emerging as a novel approach, increasing the efficacy of outreach initiatives within minoritized communities. 9 , 10 Nurses have a strong foundation for understanding medical science and communicating effectively with patients and families, making them well positioned to implement educational interventions to improve research recruitment. This is particularly impactful when nurses share the cultural backgrounds of underrepresented communities, which strengthens trust building. 11 Emerging research increasingly recognizes the critical role of nurses as community gatekeepers, who are instrumental in navigating barriers and spearheading research activities in primary care settings. 12 Nonetheless, there remains a notable dearth of studies focused on examining the extensive capabilities of nurses in enhancing community recruitment to research, especially with regard to clinical trials in investigational treatments.
In the context of AD, this innovative approach of utilizing nurses in research recruitment becomes particularly relevant. The focus in AD research has shifted toward secondary prevention, enrolling individuals in the early stages of the disease before the onset of symptoms. These so‐called preclinical AD trials aim to enroll older individuals who are cognitively unimpaired but exhibit AD biomarkers and, thus, face a higher risk of cognitive impairment. 13 However, challenges persist in participant enrollment. Studies have shown a lower willingness among African American older adults to participate in preclinical AD trials 14 and a reduced inclination toward engaging in study procedures typical of these trials among Hispanics/Latino, Asian, and African American older adults compared to their non‐Hispanic White counterparts. 15
Among the few preclinical AD trials performed to date, representation of these groups has been suboptimal. 16 , 17 Limited available evidence on dementia incidence among Asian American communities suggests they have a lower dementia risk than White American individuals, 18 , 19 and incidence varies across subgroups. 20 However, representation in AD research participation is low among Asian American communities. Asian Americans and Hispanic/Latino communities include immigrants and their descendants from various countries, each with its own unique history, culture, traditions, and languages. Key barriers to participation include a lack of knowledge about AD and AD research, as well as a general mistrust in the healthcare system. 21 Nurses, particularly those sharing a similar cultural background with these communities, could play a pivotal role in overcoming these barriers.
In this study, guided by the principles of Community‐Based Participatory Research (CBPR) 22 and the PRECEDE‐PROCEED model, 23 , 24 we describe a novel intervention that leverages collaborations with nursing organizations to bolster the recruitment of Hispanic/Latino and Asian participants for the ongoing AHEAD Study. 25 This clinical trial is testing the efficacy of lecanemab, an anti‐amyloid monoclonal antibody treatment. 26 , 27 The study enrolls cognitively unimpaired individuals aged 55 to 80 years who, upon meeting eligibility criteria, undergo amyloid biomarker testing. Based on their amyloid levels (“not detected,” “intermediate,” or “elevated”), participants are allocated to one of two trials examining different dosing protocols of lecanemab.
A unique aspect of the AHEAD study but typical of every preclinical AD trial is the requirement for participants to enroll with a study partner. They must also commit to monthly or bimonthly intravenous administrations of lecanemab and participate in various study assessments, including multiple safety magnetic resonance imaging (MRI) scans at a designated study site over a period of 4 years. Here, we report on our experiences and insights gained from collaborating with three nursing organizations toward trial recruitment. These partnerships aimed to recruit Filipino, Hispanic/Latino, and Korean older adults from local communities of Southern California into the AHEAD study. We describe the recruitment outcomes and the valuable lessons learned from this innovative recruitment strategy.
2. METHODS
2.1. Study design
Through the Alzheimer's Clinical Trials Consortium (ACTC)/ Alzheimer's Association AHEAD diversity initiative project funding (July 2022 to June 2023), we aimed at enhancing the recruitment of underrepresented groups at our AHEAD study site, located at the University of California, Irvine Alzheimer's Disease Research Center (UCI ADRC). We identified three populations from our local communities (Filipino, Hispanic/Latino, and Korean adults) who are considered underrepresented for AHEAD and therefore appropriate for this funding. Our objective was to establish partnerships with community nurse leaders and three professional nursing organizations (described below) and utilize their broad community networks to recruit Filipino, Hispanic/Latino, and Korean older adults from Southern California into the AHEAD study.
This recruitment project was guided by CBPR principles and the PRECEDE‐PROCEED model. The PRECEDE‐PROCEED model helped us systematically assess the needs of the community, plan and implement the educational intervention, and evaluate its impact. The project was executed in two distinct phases. In the initial phase, we conducted in‐person stakeholder interviews with 20 nurses from each organization. These interviews were designed to yield insights into the perceived barriers and facilitators regarding biomarker testing and clinical trial participation within the interviewees’ communities. Findings from these interviews will be reported in a subsequent paper. The second phase involved the development and cultural adaptation of educational interventions. These interventions were integrated into community engagement events involving Hispanic/Latino, Filipino, and Korean communities within Southern California. Seven community events were planned by each nurse organization, and funds were allocated equally among the organizations toward this effort. Nurse and community leaders were the decision makers on the selection of event venues, coordination of events, and implementation of the customized materials to meet the needs of each community.
RESEARCH IN CONTEXT
Systematic review: Our literature review focused on recruitment strategies for preclinical Alzheimer's disease (AD) trials, particularly targeting historically underrepresented populations. We found limited articles on such strategies and no specific studies on recruiting racial and ethnic minoritized groups into preclinical AD trials.
Interpretation: Our study highlights the pivotal role of community partners in successfully recruiting underrepresented groups for preclinical AD trials. It emphasizes the importance of early engagement with these partners, advocating for equal power sharing in line with Community‐Based Participatory Research (CBPR) principles. Transparent communication and collaborative recruitment planning were essential and significantly enhanced participant diversity in AD preclinical trials.
Future directions: To advance recruitment science, further research should evaluate the efficacy of our community‐based strategy in broader contexts. Future studies should aim to extend this approach to increase the participation of diverse underrepresented groups in preclinical AD trials, addressing critical gaps in current recruitment practices.
2.2. Diversity, equity, and inclusion (DEI) statement
Our study is firmly grounded in the principles of DEI. We recognize the importance of diverse representation in preclinical AD trials to ensure that findings are generalizable and beneficial to all populations. To this end, we made concerted efforts to include underrepresented groups, specifically those of Hispanic/Latino, Filipino, and Korean racial and ethnic backgrounds.
2.3. Key partner organizations
During the pre‐award period (January to June 2022) we leveraged existing relationships with nurse leaders who had pre‐existing affiliations with their professional nurse organizations conducting community‐engaged work. This approach ensured that we would partner with organizations that were already trusted within their communities and had the capacity to support our study's recruitment and engagement activities. The principal investigators (PIs) of the study already had established connections with leaders of these organizations. Utilizing these pre‐existing collegial relationships, we aimed to both deepen these partnerships and enhance the likelihood of project success through strengthened collaborative efforts. The underrepresented populations under study were chosen based on the working relationship with these leaders. The nursing organizations we partnered with were as follows:
The Philippine Nurses Association of Southern California (PNASC) is an organization that unites 155 Filipino nurses and 15 nursing trainees in Southern California, championing the positive image and welfare of its members while promoting professional excellence. Through strategic collaborations with professional entities and agencies, PNASC actively develops and implements programs pertinent to nursing practice, education, and research, thereby contributing significantly to its constituents.
The National Association of Hispanic Nurses‐Orange County (NAHN‐OC), with 45 active nurses, three retired nurses, and six nursing trainees, is dedicated to enhancing the health of Hispanic/Latino communities. By leading, promoting, and advocating for educational, professional, and leadership opportunities, NAHN‐OC substantially contributes to the advancement of Hispanic/Latino nurses.
Somang Society/Korean American Nurses Association of Southern California (KANASC) is a partnership that was pivotal in providing reliable health information to the Korean American community in Southern California, particularly engaging it in aging and dementia research and education. Somang Society, founded in 2007, is a non‐profit organization dedicated to serving Korean American seniors in California and various other states across the United States. Its primary mission involves imparting knowledge and support in critical areas such as end‐of‐life matters, including advanced healthcare directives and dementia and dementia caregiving. The majority of Somang Society's dedicated volunteers comprise retired nurses who are members of KANASC. Somang Society closely collaborates with KANASC, an organization established in 1969 with approximately 1000 members. KANASC is committed to offering professional development opportunities to its members, advocating for their rights and interests, fostering professional camaraderie, and contributing significantly to the well‐being of communities and society at large.
2.4. Participant recruitment strategy
Utilizing established community networks, the three partner organizations (PNASC, NAHN‐OC, and Somang Society/KANASC) were tasked with the identification of appropriate venues for community engagement events in which members of the research team could perform partnered outreach and education related to the AHEAD study. Each organization was responsible for the selection of locations within their respective communities to host a series of seven events. Recruitment of participants from the communities proximal to these event locations was conducted through a multifaceted approach. This approach included the distribution of culturally appropriate informational flyers, person‐to‐person communication, and the leveraging of both social and professional networks to extend invitations to potential participants. The Institutional Review Board at UCI approved this study, and participants were provided with a study information sheet with basic elements of informed consent.
We adopted a culturally sensitive approach to our recruitment strategy. To facilitate this, we included bilingual/bicultural staff of Filipino, Korean, and Hispanic/Latino backgrounds to communicate in the participants' preferred languages. This created a comfortable environment for participants, allowing for effective communication and a better understanding of their questions and concerns. All recruitment events incorporated cultural elements such as food and activities to honor participants' heritage, fostering a welcoming atmosphere and demonstrating our respect for cultural diversity.
2.5. Educational intervention
Education was chosen as a key intervention based on formative research, including stakeholder interviews with nurses and assessment of community needs, which identified a significant gap in knowledge about AD and clinical trial participation among our underrepresented local communities. Moreover, previous studies showed that culturally and linguistically tailored educational interventions could effectively increase awareness and willingness to participate in clinical trials. 28 , 29 Our educational intervention was designed to address specific informational needs, dispel myths, and build trust within the community.
During the first 3 months of the study (July to September 2022), together with our nurse partners, we collaboratively and systematically developed an educational intervention. This structured program aimed to disseminate knowledge and improve awareness regarding the AHEAD study to our local communities. The educational component was delivered through a PowerPoint presentation by the co‐PIs (CRS, MT, HWS) and associated staff.
The PowerPoint slides, originally designed for community engagement by the AHEAD Recruitment and Retention Workgroup, 30 were adapted by our local site recruitment team to meet our specific needs as described below. The PowerPoint presentations included three slides describing dementia and AD, four slides articulating the spectrum of risk factors – both modifiable and non‐modifiable – and three slides on strategies for the reduction of risk through lifestyle modification. The core elements of the educational content also included a primer on clinical trials in five slides and an in‐depth exposition of the AHEAD study in eight slides, elucidating its scientific objectives, methodological framework, and participant eligibility criteria. The intervention also described community resources accessible to families affected by dementia.
To address the linguistic and cultural nuances of the three demographic cohorts, the presentations were culturally and linguistically adapted. The Filipino and Korean community presentations were initially developed in English; however, for the Korean audience, a bilingual presenter delivered the material in Korean to ensure linguistic congruence and cultural resonance. For the Hispanic/Latino community, the presentation materials and delivery were conducted entirely in Spanish to meet the audience's linguistic preferences. The translation and adaptation of all outreach materials and questionnaires/study instruments into Spanish followed a six‐stage standard process adapted from the World Health Organization's process of translation and adaptation of instruments 31 : forward translation (Stage 1), back‐translation (Stage 2), discussion to reach consensus on the translations (Stage 3), independent and consensus verification by members of our Hispanic Community Advisory Board, NAHN nurse partners, and recruitment staff (Stage 4), pilot testing (Stage 5), and development of the final version (Stage 6). This process ensured that the materials were conceptually and cross‐culturally appropriate rather than merely literal translations of the English versions.
Despite these cultural adjustments, the core educational content was consistent across the three cohorts in the information provided. This involved ensuring uniformity in describing dementia and AD, risk factors, risk reduction strategies, and the AHEAD study's objectives, methods, and eligibility criteria. Each educational session was structured to span 1.5 h and made accessible through both in‐person and virtual modalities, accommodating the diverse preferences and circumstances of the participants. Participant feedback was systematically collected through informal discussions during community events. This feedback was essential in refining the educational content to achieve cultural relevance and effectiveness.
Attendees who were interested in participating in the AHEAD study underwent a prescreening process. This involved a brief evaluation of their eligibility either in‐person or via telephone, capturing sociodemographic information including age and years of education, followed by a referral for comprehensive screening at the study site.
2.6. Measures
Structured questionnaires were collected before and after each educational intervention anonymously. Data collection was conducted either digitally via a quick‐response (QR) code displayed on a slide during an educational event, linked to a REDCap database, or through traditional paper and pencil methods. The vast majority of attendees (>95%) opted for paper and pencil. The pre‐intervention questionnaire gathered sociodemographic characteristics including age, sex at birth, gender identity, education, race, ethnicity, primary language, nativity status, duration of US residence, and marital status. To assess the factors that influenced attendees to join the community event, we inquired about their motivations for their attendance. Respondents could select any of the following seven responses: (1) because of a family history of AD, (2) because they are caring for someone with AD, (3) they received a recommendation to attend the event from a friend or family, (4) they received a recommendation to attend the event from a nurse, (5) they learned how they can contribute to science and/or medical research, (6) they had concerns about memory loss for themselves or family members, (7) they desire to gain new information from researchers/scientists.
To provide geographical context for the community event locations, we used the Area Deprivation Index (ADI) 32 to assess neighborhood deprivation. The ADI, which comprises 17 indicators from the US Census, ranks and describes the socioeconomic conditions of Census block groups. For neighborhood mapping, we utilized state decile ranks of the ADI, with higher scores denoting greater neighborhood disadvantage.
2.7. Outcome assessments
Success for the project was defined and operationalized through several metrics: (1) engagement, as measured by the number of community members attending the events; (2) knowledge increase and research attitude improvement, as measured by pre‐ and post‐intervention surveys assessing changes in knowledge about the AHEAD study and research attitudes (described in a subsequent publication); (3) willingness to participate, as measured by the proportion of attendees expressing willingness to prescreen for the trial; and (4) diversity of enrollment, as measured by the number of participants from underrepresented groups who enrolled in the trial.
3. RESULTS
3.1. Community‐engaged events
Of the 21 community events planned, three (14%) were conducted virtually via Zoom and 18 were held in‐person in various locales within Southern California as depicted in Figure 1. The venues of the in‐person events ranged from large community centers to events hosted by nurses in their homes (Table 1). The nurses leveraged their extensive social and professional networks to recruit individuals from their local communities to these events. A predominant portion of the events involving the Hispanic/Latino demographic were situated in neighborhoods experiencing higher levels of socioeconomic deprivation (higher ADI scores) and were notably closer to the medical center at UCI compared to events held for the other groups (Table 1).
FIGURE 1.
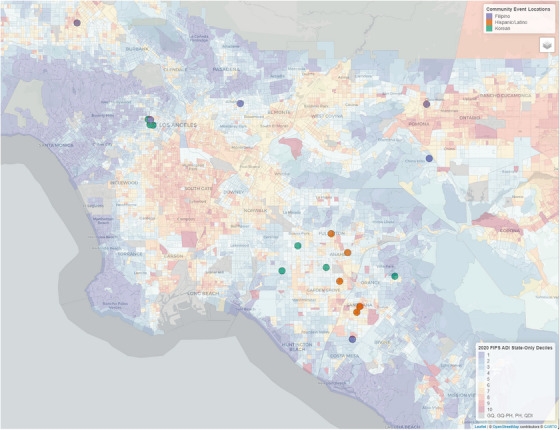
Geographical distribution of 18 community events and Area Deprivation Index (ADI) overlays in Southern California. Each dot represents the location of a community event involving various racial and ethnic groups. The ADI overlays are based on 2020 Census block data, categorized into state deciles. Higher deciles indicate greater neighborhood deprivation.
TABLE 1.
Characteristics of community events held by each nurse organization.
| Venue | No. attendees | Attendee description | Event type (in‐person or virtual) | Approximate distance from medical center a |
|---|---|---|---|---|
| ||||
|
90 | Active and retired Filipino/a nurses | In‐person | 69.2 km |
|
|
|
In‐person | 74.8 km |
|
30 | Community members (congregation) | In‐person | 56.5 km |
|
50 | Business owners and professional network | In‐person | 54.9 km |
|
25 | Community members (professional network) | In‐person | 62.9 km |
|
25 | Community members (professional network) | Virtual | N/A |
| National Association of Hispanic Nurses (NAHN) – Orange County chapter | ||||
|
30 | Active and retired Hispanic nurses | Virtual | N/A |
|
45 | Community members (families) | In‐person | 24.0 km |
|
60 | Community members (older adults) | In‐person | 15.1 km |
|
25 | Cancer survivor group attendees | In‐person | 29.3 km |
|
30 | Community members (professional network) | Virtual | N/A |
| Korean American Nurse Association (KANA)/Somang Society | ||||
|
31 |
|
In‐person | 55.5 km |
|
39 | Senior ministry members | In‐person | 24.3 km |
|
|
|
In‐person | 51.5 km |
|
59 | Community members (older adult) | In‐person | 74.7 km |
|
30 | Community members (professional network) | In‐person | 7.9 km |
Distance in miles to UCI Health Gottschalk Medical Plaza. Distances are averaged for multiple events.
3.2. Community event attendees
A total of 654 community members attended the educational events, as shown in Figure 2. Of these, 105 participants (16.1%) did not complete the pre‐intervention surveys and 39 (6.0%) had missing data regarding race or ethnicity. After the aforementioned exclusions, a total of 510 participants were grouped into four racial and ethnic categories: Hispanic/Latino (n = 187), Filipino (n = 149), Korean (n = 147), and other (n = 27). The “Other” category consisted of individuals who self‐identified as non‐Hispanic White (n = 10), non‐Hispanic Black (n = 1), Vietnamese (n = 4), Japanese (n = 2), Chinese (n = 2), and Asian not otherwise specified (n = 8).
FIGURE 2.
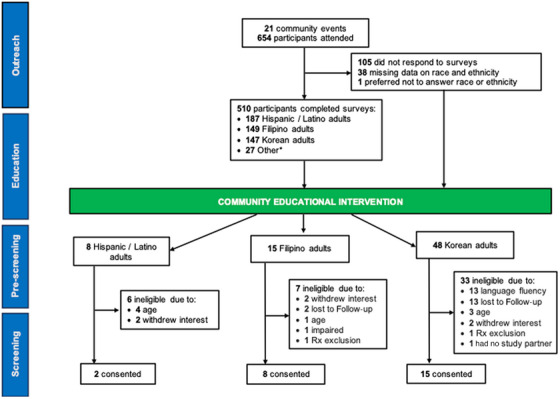
Flow schematic of participant recruitment to AHEAD 3‐45 trial. The “other” category encompasses adults who self‐identified under various race and ethnic groups: non‐Hispanic White (n = 10), non‐Hispanic Black (n = 1), Vietnamese (n = 4), Japanese (n = 2), Chinese (n = 2), and Asian not otherwise specified (n = 8).
The distribution of characteristics for the community attendees is depicted in Table 2. The average age of the overall sample was 59 years. Notably, Korean individuals had a higher average age, compared to the Filipino and Hispanic/Latino groups. The proportion of attendees aged 55 or older varied between groups, ranging from 33.7% among Hispanic/Latino adults to 81.6% among Korean adults. Sex and gender distributions revealed that 77.1% of the attendees were female; the sample included five transgender individuals. Among the Hispanic/Latino participants, a majority (82.4%) identified as Mexican American. Over 80% of attendees reported being born outside of the United States. For this immigrant population, the average duration of residence in the United States was 33 years, with an average age of immigration of 27 years. Differences in educational attainment were evident between the groups. Over a third of Hispanic/Latino attendees (37%) had an education level below high school, a contrast to other racial and ethnic groups, in which less than 3% reported having an education below the high school level. Additionally, 51% of Filipino attendees reported full‐time employment, a percentage higher than the other groups.
TABLE 2.
Distribution of participant characteristics according to racial and ethnic background.
| Overall sample | Hispanic/Latino a | Filipino | Korean | Other b | |
|---|---|---|---|---|---|
| Total N | 510 | 187 | 149 | 147 | 27 |
| Age, mean (SD) | 58.6 (16.1) | 52.8 (18.4) | 57.8 (13.4) | 67.4 (10.1) | 45.9 (20.2) |
| ≥ 55 years, n (%) | 278 (54.5%) | 63 (33.7%) | 88 (59.1%) | 120 (81.6%) | 7 (25.9%) |
| Prefer not to answer or missing | 74 (14.5%) | 56 (30.0%) | 3 (2.0%) | 13 (8.8%) | 2 (7.4%) |
| Sex at birth, n (%) | |||||
| Male | 113 (22.2%) | 24 (12.8%) | 42 (28.2%) | 36 (24.5%) | 11 (40.7%) |
| Female | 393 (77.1%) | 161 (86.1%) | 106 (71.1%) | 110 (74.8%) | 16 (59.3%) |
| Intersex | 1 (< 1%) | 1 (< 1%) | 0 | 0 | 0 |
| Prefer not to answer or missing | 3 (< 1%) | 1 (< 1%) | 1 (< 1%) | 1 (< 1%) | 0 |
| Gender identity, n (%) | |||||
| Man | 107 (21.0%) | 20 (10.7%) | 41 (27.5%) | 35 (23.8%) | 11 (40.7%) |
| Woman | 380 (74.5%) | 157 (84.0%) | 105 (70.5%) | 102 (69.4%) | 16 (59.3%) |
| Transgender man | 0 | 0 | 0 | 0 | 0 |
| Transgender woman | 5 (1.0%) | 3 (1.6%) | 1 (< 1%) | 1 (< 1%) | 0 |
| Gender queer | 0 | 0 | 0 | 0 | 0 |
| Gender non‐binary | 0 | 0 | 0 | 0 | 0 |
| Another gender | 0 | 0 | 0 | 0 | 0 |
| Prefer not to answer or missing | 18 (3.5%) | 7 (3.7%) | 2 (1.3%) | 9 (6.1%) | 0 |
| Primary language spoken, n (%) | |||||
| English | 147 (28.8%) | 40 (21.4%) | 68 (45.6%) | 15 (10.2%) | 24 (88.9%) |
| Spanish | 142 (27.8%) | 142 (75.9%) | 0 | 0 | 0 |
| Korean | 132 (25.9%) | 1 (< 1%) | 0 | 131 (89.1%) | 0 |
| Tagalog | 73 (14.3%) | 0 | 73 (49.0%) | 0 | 0 |
| Other | 11 (2.2%) | 0 | 7 (4.7%) | 1 (< 1%) | 3 (11.1%) |
| Prefer not to answer or missing | 5 (1.0%) | 4 (2.1%) | 1 (< 1%) | 0 | 0 |
| Hispanic/Latino heritage, n (%) | |||||
| Mexican | — | 154 (82.4%) | — | — | — |
| Central American | — | 13 (7.0%) | — | — | — |
| Cuban | — | 2 (1.1%) | — | — | — |
| Dominican | — | 1 (< 1%) | — | — | — |
| Puerto Rican | — | 3 (1.6%) | — | — | — |
| South American | — | 3 (1.6%) | — | — | — |
| More than one heritage | — | 3 (1.6%) | — | — | — |
| Other | — | 5 (2.7%) | — | — | — |
| Prefer not to answer or missing | — | 3 (1.6%) | |||
| Born outside of United States, n (%) | 409 (80.2%) | 134 (71.7%) | 129 (86.6%) | 137 (93.2%) | 9 (33.3%) |
| Prefer not to answer or missing | 23 (4.5%) | 11 (5.9%) | 5 (3.4%) | 7 (4.8%) | 0 |
| Years in the United States, mean (SD) | 33.3 (14.4) | 32.5 (13.9) | 32.2 (15.3) | 38.6 (11.7) | 11.0 (11.1) |
| Age at migration, mean (SD) | 26.9 (12.2) | 24.2 (13.4) | 27.1 (11.2) | 30.3 (12.5) | 25.7 (2.1) |
| Missing, n (%) | 180 (44.0%) | 45 (11.0%) | 38 (9.3%) | 91 (22.3%) | 6 (1.5%) |
| Educational attainment, n (%) | |||||
| Less than high school | 75 (14.7%) | 70 (37.4%) | 2 (1.3%) | 3 (2.0%) | 0 |
| High school | 19 (3.7%) | 17 (9.1%) | 0 | 2 (1.4%) | 0 |
| Some college | 81 (15.9%) | 29 (15.5%) | 23 (15.4%) | 22 (15.0%) | 7 (25.9%) |
| College/University | 179 (35.1%) | 21 (11.2%) | 67 (45.0%) | 78 (53.1%) | 13 (48.2%) |
| Postgraduate | 97 (19.0%) | 10 (5.4%) | 51 (34.2%) | 31 (21.1%) | 5 (18.5%) |
| Prefer not to answer or missing | 59 (11.6%) | 40 (21.4%) | 6 (4.0%) | 11 (7.5%) | 2 (7.4%) |
| Employment status, n (%) | |||||
| Full‐time | 149 (29.2%) | 40 (21.4%) | 77 (51.7%) | 21 (14.3%) | 11 (40.7%) |
| Part‐time | 78 (15.3%) | 36 (19.3%) | 18 (12.1%) | 15 (10.2%) | 9 (33.3%) |
| Retired | 230 (45.1%) | 65 (34.8%) | 52 (34.9%) | 107 (72.8%) | 6 (22.2%) |
| Prefer not to answer or missing | 53 (10.4%) | 46 (24.6%) | 2 (1.3%) | 4 (2.7%) | 1 (3.7%) |
Four percent of individuals with Hispanic/Latino heritage additionally self‐identified as Filipino (n = 6), Korean (n = 1), and Native Hawaiian (n = 1).
The “Other” category encompasses adults who self‐identified under various race and ethnic groups: non‐Hispanic White (n = 10), non‐Hispanic Black (n = 1), Vietnamese (n = 4), Japanese (n = 2), Chinese (n = 2), and Asian not otherwise specified (n = 8).
3.3. Reasons for attending the community events
Participants were surveyed regarding their motivations for attending the community events. Figure 3 presents the distribution of these motivations stratified by race and ethnicity. The predominant reasons across all groups were (1) concerns about memory loss, either personally or in family members, and (2) an interest in acquiring new information from researchers or scientists. Korean adults more frequently reported caregiving for an individual with AD as a reason for attendance (25.2%) compared to Filipino (10.1%) and Hispanic/Latino (4.3%) adults. No other major differences in reasons for attending were observed among these three main populations of interest.
FIGURE 3.
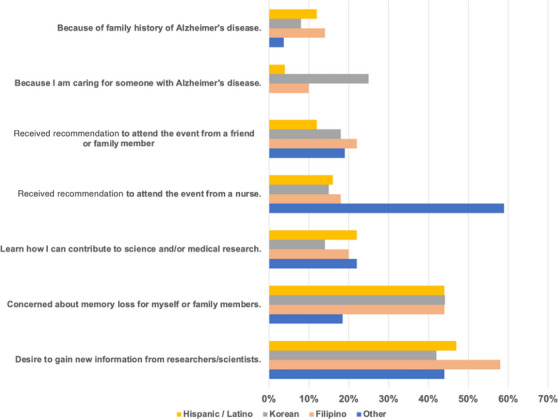
Reason for attending community events by race and ethnicity.
3.4. Recruitment outcomes
A total of 71 adults, representing 10.9% of those who received the education, were successfully recruited to prescreen for the AHEAD study. Of these, 11.2% were Hispanic/Latino adults, 21.1% were Filipino adults, and 67.6% were Korean adults. Among Hispanic/Latino adults who prescreened, 50% were deemed ineligible primarily due to age requirements. Approximately 47% of the Filipino adults who prescreened did not proceed to in‐person screening, with the primary reasons being withdrawn interest and loss to follow‐up. Of the Korean adults who prescreened, 69% were found ineligible, predominantly due to challenges with English fluency and loss to follow‐up.
In sensitivity analyses comparing age and education distributions between community event attendees who completed the pre‐intervention survey and those who prescreened for the AHEAD study (Supplementary Table), we observed significant differences. Filipino adults who prescreened were significantly older than those who completed the pre‐intervention survey (68.9 vs 57.8 years, p < 0.001). In addition, Hispanic/Latino adults who prescreened were significantly more likely to have higher levels of education than those who completed the survey.
Of the individuals reached through community engagement, 25 participants (3.8%) were successfully enrolled. The breakdown of enrollees included two Hispanic/Latino adults (1.1% of those reached within their demographic), eight Filipino adults (5.3% of their demographic reached), and 15 Korean adults (10.2% of their demographic reached). Notably, a single Filipino family contributed five of the eight Filipino participants. This recruitment was initiated by the elder sister, who learned of the trial through a friend that attended a community event hosted by a nurse.
3.5. Lessons learned
Key insights from our study implementation, as summarized in Table 3, include the following:
Partnership dynamics: A critical factor contributing to the success of the study was the existing trust and rapport established with leaders of the nursing and community‐based organizations. To maintain and grow the partnerships, study investigators developed methods and systems to ensure consistent opportunities for communication and troubleshooting (see Table 4 for a full description). These pre‐existing relationships facilitated effective collaboration, with the nurse leaders playing a pivotal role in operational decisions. They provided valuable insights into culturally appropriate activities, suitable food distribution, and forms of entertainment that resonated with the community members, thereby enhancing engagement. Moreover, their coordination with local venues, such as churches and senior and family facilities, was instrumental in the smooth execution of the events. Early involvement of these leaders in the recruitment strategy was vital, as it allowed for efficient problem‐solving and further strengthened the trust in these partnerships.
Feedback‐driven content refinement: Participant feedback was indispensable for achieving cultural relevance and effectiveness in educational content. For instance, in Hispanic/Latino community events, there was a preference for including more information on specific risk factors such as diabetes and cardiovascular risks, as well as on lifestyle and behavioral modifications. While the core elements of the intervention were maintained, these targeted adjustments resulted in a more pertinent and engaging educational program. This process demonstrated a responsive and community‐centric approach to health education.
Interest and eligibility in research participation: The disparity between community interest in research participation and the constraints imposed by eligibility criteria was a notable challenge. For example, younger Hispanic/Latino attendees often did not meet the age criterion for the AHEAD study despite their enthusiasm. Similarly, older Korean adults showed a keen interest in participation but faced language barriers that made them ineligible. These limitations highlighted the need for alternative research participation options to sustain community engagement and avoid potential disenfranchisement.
Navigational challenges with academic–community partnerships: Integrating nursing and community‐based partners into the study framework presented bureaucratic challenges. The onboarding process was encumbered by extensive paperwork, resulting in delayed reimbursements for their services. This complexity posed a risk to the trust established with our community partners. These experiences underscore the need for universities to develop policies attuned to the operational realities of community‐based organizations. Streamlining these processes and adopting more efficient financial practices for onboarding new partners are essential steps to ensure timely and effective collaboration.
Cultural considerations in recruitment: Our recruitment strategy required a culturally sensitive approach, or “recruitment etiquette,” 33 anchored in respect, compassion, and cultural awareness. Bilingual/bicultural staff from Filipino, Korean, and Hispanic/Latino backgrounds facilitated comfortable environments for participants, allowing effective communication and deeper understanding of their questions and concerns. Recruitment events also incorporated cultural elements, including food and activities, to celebrate and honor participants’ heritage, creating a welcoming atmosphere and demonstrating our commitment to cultural diversity.
Operational challenges in data collection: We encountered operational challenges related to data collection, with attendees for traditional methods like paper‐based surveys over digital means. This suggested a need for support mechanisms for individuals with limited digital literacy to avoid excluding certain population segments. Staffing constraints also affected our ability to manage the recruitment process, particularly from prescreening to screening stages, resulting in gaps in data collection on reasons for non‐continuation. Adequate staffing is critical to ensure thorough data collection and understanding of participant experiences and barriers in the recruitment process. , ,
TABLE 3.
Thematic summary of lessons learned from community recruitment.
| Theme | Key lessons learned | Implications/recommendations |
|---|---|---|
| Community partnership |
|
Foster and build on strong relationships with community partners |
| Participant feedback |
|
Continuously adapt educational content |
| Research inclusivity |
|
|
| Academic‐Community based organization collaboration |
|
Implement policies for effective collaborations |
| Cultural considerations |
|
Incorporate cultural elements in interventions |
| Operational challenges |
|
Improve recruitment systems and data collection |
TABLE 4.
Systems and methods used for sustaining partnerships.
| System/method | Description |
|---|---|
| Initial project training | Conducted with all three partner organizations to align goals, expectations, and protocols |
| Monthly Zoom meetings | Regular virtual meetings to discuss progress, address challenges, and ensure continuous engagement |
| Frequent emails and phone calls | Ongoing communication between principal investigators and partners to provide updates, troubleshoot issues, and maintain strong relationships |
| Feedback mechanisms | Established processes for nurse partners to provide feedback on study processes and suggest improvements |
| Collaborative planning sessions | Joint sessions with partner organizations to plan recruitment strategies and tailor interventions to community needs |
| Resource sharing | Providing partner organizations with necessary resources, such as educational materials and training sessions, to support their involvement in study |
4. DISCUSSION
Efforts to improve recruitment of underrepresented groups into AD trials have historically posed a challenge. In this study, we shared our experiences, outcomes, and lessons learned from recruiting local populations of Hispanic/Latino, Korean, and Filipino origin from Southern California into the AHEAD study through a novel initiative. We successfully engaged a large population of diverse community members through innovative partnerships with professional nursing and community‐based organizations, resulting in an additional 25 enrollees in a high‐burden interventional drug trial. Our findings indicate that while the support and partnership of key nursing community‐based organizations were vital for such engagement, more research is needed to understand how to translate engagement into actual enrollment, particularly among groups that may face additional barriers and challenges.
The total number of screens (n = 25) resulting from this study was relatively small compared to the overall AHEAD study, which screened more than 20,000 individuals to achieve a total sample size of 1400 randomized individuals. The yield of our efforts was high, however, compared to some previous recruitment efforts, 34 with 4% of those reached enrolling and 14% willing to prescreen for the trial. Moreover, the site‐level expectation in the AHEAD study was to randomize 20 participants, with at least 30% being from a racial, ethnic, or other underrepresented group. Therefore, these additional participants represented a meaningful increase in our overall site enrollment diversity. Extrapolating these findings to all sites would result in nearly 2000 additional screens from underrepresented backgrounds and an approximately 10% increase in the overall diversity of screening.
We observed differences in consent rates among ethnic and racial groups, with Hispanic/Latino participants constituting only two of the 25 consenting individuals. This low representation may be partially explained by the underrepresentation of Hispanic/Latino adults aged 55 to 80 at our community events, a key inclusion criterion for the AHEAD study. Enhancing the participation of age‐appropriate Hispanic/Latino populations could improve outcomes. However, adopting a more family‐centric approach to recruitment, which acknowledges the role of familism in decision‐making, may be particularly effective in AD and related dementias (ADRD) studies. 35 , 36 Our findings also highlighted a significant interest in participation among younger Hispanic/Latino attendees and older Korean adults, but many did not meet the eligibility criteria due to age and language barriers, respectively.
Our findings revealed a distinct preference for Spanish‐language materials among Hispanic/Latino participants. This preference, coupled with generally lower levels of educational attainment, may lead to challenges in health literacy. 37 , 38 , 39 Such challenges are often associated with increased medical mistrust, 40 , 41 which could be a contributing factor to the observed lower rates of prescreening and consent in this group. Indeed, our sensitivity analyses indicated that Hispanic/Latino adults with lower education levels were less likely to prescreen. Moreover, there was a notable discrepancy in data completeness, with a disproportionately higher amount of missing information, particularly regarding age, education, and employment status, from Hispanic/Latino attendees. This lack of comprehensive data presents a barrier to fully understanding the engagement and participation dynamics within the Hispanic/Latino community.
Another potential factor affecting the Hispanic/Latino community's enrollment in the AHEAD study is concern regarding undocumented status. 42 California has approximately two million undocumented immigrants. The fear of deportation, often underaddressed in research settings, may heighten mistrust and reluctance to engage in clinical trials. 43 Future recruitment strategies must thoughtfully incorporate these insights, 44 considering both cultural sensitivities and the unique challenges faced by the Hispanic/Latino community, to enhance their engagement in preclinical trials.
The Filipino community's participation in our community recruitment provided valuable cultural perspectives on trial decision‐making. We found that a significant number of AHEAD study consents were concentrated within a single family unit, reflecting the communal decision‐making practices ingrained in Filipino culture. Collective orientation and familial solidarity are Filipino cultural traits that underscore the emphasis on unity, deference to family hierarchy, and shared decision‐making in health‐related matters. 45 , 46 The proactive involvement of an entire family in the study highlights the role of familial endorsement and collective agreement in making informed choices about trial participation. These findings further advocate for the incorporation of family‐centered approaches in research recruitment strategies and underscore the need for further research to comprehensively understand the role of culture in clinical trial decision‐making. 47
Korean older adults represented the largest proportion of consents for the AHEAD study among the groups studied. This may be attributed to a higher proportion of individuals who met the study's age criterion, coupled with a greater likelihood of these individuals providing care for older adults with AD. The partnership with Somang Society, known for its dementia caregiving education, enabled retired Korean nurses to effectively reach a demographic with a significant proportion of AD caregivers. Nonetheless, English language proficiency emerged as a significant barrier to participation in the AHEAD study within the Korean community. This finding aligns with existing literature indicating that Asian immigrants with limited English proficiency face substantial obstacles in accessing healthcare services due to language barriers. 48 Further research is warranted to explore these challenges within the context of clinical trial participation.
Our recruitment strategy emphasized the importance of adhering to CBPR principles, 22 which promote collaborative partnerships with community members and leaders. These partnerships foster mutual learning, shared resources, and collective decision‐making, benefiting both academic researchers and community stakeholders. We engaged community partners in designing our intervention and recruiting participants for our educational events. Additionally, community members played a crucial role in both the initial design and subsequent refinement of our educational interventions, positioning them as essential contributors to the success and impact of our efforts. Community nursing organizations emerged as invaluable partners, offering unique insights and established connections to our diverse communities, thereby enhancing the effectiveness of our recruitment approach.
To further strengthen our approach and guide future efforts, we will continue to apply and expand upon CBPR principles. This includes maintaining regular communication with our nurse partners to ensure that interventions remain relevant and effective. We will emphasize capacity building by providing training to our nurse partners, empowering them to take on leadership roles in future recruitment efforts. Developing long‐term partnerships and securing funding will be essential to sustaining community engagement efforts beyond the initial study period. Furthermore, we will continuously evaluate the effectiveness of our strategies and make necessary adjustments based on community feedback and changing needs. By integrating these CBPR principles and actions into our framework, we aim to create a more inclusive and participatory research environment that can adapt to the evolving needs of our diverse communities.
While the study demonstrated notable strengths, there were also limitations. Our recruitment efforts were concentrated on three specific underrepresented groups – Filipino, Hispanic/Latino, and Korean – driven by convenience and pre‐existing connections with nurse leaders belonging to these ethnicities. This focus might not comprehensively reflect the vast diversity inherent in the Southern California region. In addition, the majority of attendees (77%) were female, which could affect the generalizability of the findings. Moreover, the applicability of these findings to other underrepresented communities remains uncertain.
To increase the inclusion of men, several strategies could be implemented. A recent systematic review identified key facilitators for male recruitment and retention in longitudinal studies, such as clear communication and tailoring recruitment methods to men's interests. 49 Leveraging health service provider referrals may enhance participation among underrepresented older adults. In addition, fostering positive relationships between staff and participants and providing ongoing health monitoring may further motivate male participation. More research into evidence‐based strategies is needed to address the gender imbalance in our recruitment efforts and improve overall diversity and representativeness in AD trials.
Another limitation of this study was the challenge of achieving sustained engagement throughout the recruitment process. In particular, the recruitment of underrepresented groups who encounter more structural barriers may need a continuous engagement approach. 50 , 51 Recognizing this, our future plans include investing additional effort to focus on training nurses to conduct community‐based educational interventions. Such training is anticipated to not only enhance their capacity to engage these communities effectively but also contribute to the long‐term sustainability of the project.
5. CONCLUSION
This study demonstrates the critical role of community partners, particularly nursing community organizations, in effectively recruiting underrepresented groups for preclinical AD trials. Our findings highlight the necessity of engaging these partners from the very beginning and ensuring equal power sharing in accordance with CBPR principles. A novel aspect of our approach was the involvement of nursing community organizations, which played a pivotal role in building trust and facilitating recruitment. Key to this collaborative approach is the establishment of transparent communication channels and the joint development of a recruitment plan. As demonstrated in our research, this strategy is instrumental in enhancing the diversity of participant representation in AD preclinical trials.
CONFLICT OF INTEREST STATEMENT
Christian R. Salazar received research funding from the National Institute on Aging and Alzheimer's Association. David L. Sultzer received research funding from Esai and participates on a data safety monitoring board or advisory board for Janssen, Otsuka, NovoNordisk, and Ono. Joshua D. Grill received research funding from the National Institute on Aging, Alzheimer's Association, BrightFocus Foundation, Eli Lilly, Genentech, Biogen, and Eisai. Hye‐Won Shin has been executive director of the Somang Society since 2023. All other authors have no disclosures to report. Author disclosures are available in the supporting information.
CONSENT STATEMENT
All participants were provided with a study information sheet with basic elements of informed consent. Event attendees who agreed to participate in the study completed the study questionnaires.
Supporting information
Supporting Information
Supporting Information
ACKNOWLEDGMENTS
The authors thank our partner organizations: NAHN‐Orange County, PNASC, Somang Society, and KANASC, as well as other community‐based organizations that hosted our events. The authors thank all of our community members who participated in our community events. This project was supported by a subcontract SG‐22‐877415‐AHEAD: ACTC AHEAD Alzheimer's Association Proposal: Diverse Recruitment Component. The ACTC is funded by U24AG057437. CRS is supported by NIA K01AG076811 and Alzheimer's Association AARFD‐20‐682432. The UC Irvine ADRC is supported by NIA P30AG066519.
Salazar CR, Tallakson M, Corona MG, et al. Community recruitment of underrepresented populations to the AHEAD 3‐45 preclinical AD trial using novel partnerships with nursing and community‐based organizations: Lessons and outcomes. Alzheimer's Dement. 2024;20:7160–7173. 10.1002/alz.14211
REFERENCES
- 1. 2023 Alzheimer's disease facts and figures. Alzheimers Dement. 2023;19(4):1598‐1695. [DOI] [PubMed] [Google Scholar]
- 2. Manly JJ, Jones RN, Langa KM, et al. Estimating the prevalence of dementia and mild cognitive impairment in the US: the 2016 Health and Retirement Study Harmonized Cognitive Assessment Protocol Project. JAMA Neurol. 2022;79:1242‐1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Franzen S, Smith JE, van den Berg E, et al. Diversity in Alzheimer's disease drug trials: the importance of eligibility criteria. Alzheimers Dement. 2022;18:810‐823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Babulal GM, Franzen S, Abner EL, et al. Diversity in Alzheimer's disease drug trials: reflections on reporting and social construction of race. Alzheimers Dement. 2022;18:867‐868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Schwartz AL, Alsan M, Morris AA, Halpern SD. Why diverse clinical trial participation matters. N Engl J Med. 2023;388:1252‐1254. [DOI] [PubMed] [Google Scholar]
- 6. Grill JD, Sperling RA, Raman R. What should the goals be for diverse recruitment in Alzheimer clinical trials? JAMA Neurol. 2022;79:1097‐1098. [DOI] [PubMed] [Google Scholar]
- 7. Watson JL, Ryan L, Silverberg N, Cahan V, Bernard MA. Obstacles and opportunities in Alzheimer's clinical trial recruitment. Health Aff (Millwood). 2014;33:574‐579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Elliott CL. Together we make the difference: national strategy for recruitment and participation in Alzheimer's and related dementias clinical research. Ethn Dis. 2020;30:705‐708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Vluggen S, Hoving C, Vonken L, Schaper NC, de Vries H. Exploring factors influencing recruitment results of nurses recruiting diabetes patients for a randomized controlled trial. Clin Trials. 2020;17:448‐458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Burnett C, Bullock L, Collins CA, Hauser L. Evaluation of a clinical cancer trial research training workshop: helping nurses build capacity in southwest Virginia. Public Health Nurs. 2016;33:565‐572. [DOI] [PubMed] [Google Scholar]
- 11. Beer K, Gentgall M, Templeton N, Whitehouse C, Straiton N. Who's included? The role of the Clinical Research Nurse in enabling research participation for under‐represented and under‐served groups. J Res Nurs. 2022;27:143‐154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ballintine A, Potter R. What are the experiences of nurses delivering research studies in primary care? Prim Health Care Res Dev. 2023;24:e46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sperling RA, Aisen PS, Beckett LA, et al. Toward defining the preclinical stages of Alzheimer's disease: recommendations from the National Institute on Aging‐Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7:280‐292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zhou Y, Elashoff D, Kremen S, Teng E, Karlawish J, Grill JD. African Americans are less likely to enroll in preclinical Alzheimer's disease clinical trials. Alzheimers Dement (N Y). 2017;3:57‐64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Salazar CR, Hoang D, Gillen DL, Grill JD. Racial and ethnic differences in older adults' willingness to be contacted about Alzheimer's disease research participation. Alzheimers Dement (N Y). 2020;6:e12023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sperling RA, Donohue MC, Raman R, et al. Trial of solanezumab in preclinical Alzheimer's disease. N Engl J Med. 2023;389:1096‐1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Raman R, Quiroz YT, Langford O, et al. Disparities by race and ethnicity among adults recruited for a preclinical Alzheimer disease trial. JAMA Netw Open. 2021;4:e2114364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mayeda ER, Glymour MM, Quesenberry CP, Whitmer RA. Inequalities in dementia incidence between six racial and ethnic groups over 14 years. Alzheimers Dement. 2016;12:216‐224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gilsanz P, Corrada MM, Kawas CH, et al. Incidence of dementia after age 90 in a multiracial cohort. Alzheimers Dement. 2019;15:497‐505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mayeda ER, Glymour MM, Quesenberry CP Jr, Whitmer RA. Heterogeneity in 14‐year dementia incidence between Asian American Subgroups. Alzheimer Dis Assoc Disord. 2017;31:181‐186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Savold J, Cole M. Barriers and solutions to Alzheimer's disease clinical trial participation for Black Americans. Alzheimers Dement (N Y). 2023;9:e12402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wallerstein N, Duran B. Community‐based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health. 2010;100(Suppl 1):S40‐S46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gielen AC, Green LW. The impact of policy, environmental, and educational interventions: a synthesis of the evidence from two public health success stories. Health Educ Behav. 2015;42:20S‐34S. [DOI] [PubMed] [Google Scholar]
- 24. Trifiletti LB, Gielen AC, Sleet DA, Hopkins K. Behavioral and social sciences theories and models: are they used in unintentional injury prevention research? Health Educ Res. 2005;20:298‐307. [DOI] [PubMed] [Google Scholar]
- 25. Rafii MS, Sperling RA, Donohue MC, et al. The AHEAD 3‐45 Study: design of a prevention trial for Alzheimer's disease. Alzheimers Dement. 2023;19:1227‐1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. van Dyck CH, Swanson CJ, Aisen P, et al. Lecanemab in early Alzheimer's Disease. N Engl J Med. 2023;388:9‐21. [DOI] [PubMed] [Google Scholar]
- 27. Swanson CJ, Zhang Y, Dhadda S, et al. A randomized, double‐blind, phase 2b proof‐of‐concept clinical trial in early Alzheimer's disease with lecanemab, an anti‐Abeta protofibril antibody. Alzheimers Res Ther. 2021;13:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ma GX, Tan Y, Blakeney NC, et al. The impact of a community‐based clinical trial educational intervention among underrepresented Chinese Americans. Cancer Epidemiol Biomarkers Prev. 2014;23:424‐432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cunningham‐Erves J, Mayo‐Gamble TL, Hull PC, et al. A pilot study of a culturally‐appropriate, educational intervention to increase participation in cancer clinical trials among African Americans and Latinos. Cancer Causes Control. 2021;32:953‐963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Molina‐Henry DP, Grill J, Sperling RA, et al. Strategies for diverse participant recruitment to a preclinical Alzheimer's Disease prevention trial: the AHEAD study. Alzheimer's & Dementia. 2022;18:e068222. [Google Scholar]
- 31. Process of translation and adaptation of instruments. World Health Organization. 2022. [Google Scholar]
- 32. Kind AJH, Buckingham WR. Making neighborhood‐disadvantage metrics accessible—The Neighborhood Atlas. N Engl J Med. 2018;378:2456‐2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Gyure ME, Quillin JM, Rodriguez VM, et al. Practical considerations for implementing research recruitment etiquette. IRB. 2014;36:7‐12. [PMC free article] [PubMed] [Google Scholar]
- 34. Fitzpatrick AL, Fried LP, Williamson J, et al. Recruitment of the elderly into a pharmacologic prevention trial: the Ginkgo Evaluation of Memory Study experience. Contemp Clin Trials. 2006;27:541‐553. [DOI] [PubMed] [Google Scholar]
- 35. Lamar M, Glover CM, Capuano AW, et al. Stability and change in acculturation‐related characteristics in older Latinos: implications for culturally compatible ADRD research. Alzheimers Dement (N Y). 2023;9:e12380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Glover CM, Shah RC, Bennett DA, Wilson RS, Barnes LL. Perceived impediments to completed brain autopsies among diverse older adults who have signed a uniform anatomical gift act for brain donation for clinical research. Ethn Dis. 2020;30:709‐718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Rikard RV, Thompson MS, McKinney J, Beauchamp A. Examining health literacy disparities in the United States: a third look at the National Assessment of Adult Literacy (NAAL). BMC Public Health. 2016;16:975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Soto Mas F, Jacobson HE. Advancing health literacy among Hispanic immigrants: the intersection between education and health. Health Promot Pract. 2019;20:251‐257. [DOI] [PubMed] [Google Scholar]
- 39. Cohen AK, Syme SL. Education: a missed opportunity for public health intervention. Am J Public Health. 2013;103:997‐1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Gonzalez HM, Vega WA, Tarraf W. Health care quality perceptions among foreign‐born Latinos and the importance of speaking the same language. J Am Board Fam Med. 2010;23:745‐752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Abraido‐Lanza AF, Cespedes A, Daya S, Florez KR, White K. Satisfaction with health care among Latinas. J Health Care Poor Underserved. 2011;22:491‐505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Rodriguez MA, Bustamante AV, Ang A. Perceived quality of care, receipt of preventive care, and usual source of health care among undocumented and other Latinos. J Gen Intern Med. 2009;24(Suppl 3):508‐513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Arevalo M, Heredia NI, Krasny S, et al. Mexican‐American perspectives on participation in clinical trials: a qualitative study. Contemp Clin Trials Commun. 2016;4:52‐57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Aranda MP, Marquez DX, Gallagher‐Thompson D, et al. A call to address structural barriers to Hispanic/Latino representation in clinical trials on Alzheimer's disease and related dementias: a micro‐meso‐macro perspective. Alzheimers Dement (N Y). 2023;9:e12389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Cura JD. Respecting autonomous decision making among Filipinos: a re‐emphasis in genetic counseling. J Genet Couns. 2015;24:213‐224. [DOI] [PubMed] [Google Scholar]
- 46. Pusey E, Tinker A, Lucivero F. The shared decision making of older adults in healthcare. Working with Older People. 2019;23:77‐86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Guss CD, Robinson B. Predicted causality in decision making: the role of culture. Front Psychol. 2014;5:479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Jang Y, Kim MT. Limited english proficiency and health service Use in Asian Americans. J Immigr Minor Health. 2019;21:264‐270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Borg DJ, Haritopoulou‐Sinanidou M, Gabrovska P, et al. Barriers and facilitators for recruiting and retaining male participants into longitudinal health research: a systematic review. BMC Med Res Methodol. 2024;24:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Gilmore‐Bykovskyi AL, Jin Y, Gleason C, et al. Recruitment and retention of underrepresented populations in Alzheimer's disease research: a systematic review. Alzheimers Dement (N Y). 2019;5:751‐770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Rabinowitz YG, Gallagher‐Thompson D. Recruitment and retention of ethnic minority elders into clinical research. Alzheimer Dis Assoc Disord. 2010(Suppl 24):S35‐S41. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information
Supporting Information


