ABSTRACT
Growing Up in New Zealand is this country’s largest contemporary longitudinal study of child development. The study has been designed to provide insight into the lives of children and young people growing up in the context of twenty-first century New Zealand. The Growing Up in New Zealand cohort recruited 6853 children representative of the current ethnic and socioeconomic diversity of births in Aotearoa, New Zealand in 2009 and 2010. The developmental wellbeing of the children has been tracked in detail over their first thousand days of life and every two to three years since. While the majority of the cohort are growing up healthy and happy, a significant proportion of children are growing up in families who have been persistently burdened with multiple stressors associated with economic, material and social hardship. This has created a disproportionate burden of poorer overall wellbeing outcomes and limited life course opportunities for these children from an early age. This paper will explore some of the evidence collected from the diverse cohort of New Zealand children and their families and whānau from before birth to middle childhood, highlighting the key findings and the utility of the evidence to improve wellbeing.
KEYWORDS: Cohort study, longitudinal, life course, child wellbeing, health inequalities, social determinants, resilience
Introduction
Longitudinal studies collect information from the same group of individuals over time and can provide insights into how the capacity of individuals, their parents and families, communities and wider social environments operate together to influence the health and wellbeing of the individuals being followed. Longitudinal information from birth cohorts can provide developmental information and evidence about how to support parents, families, communities, and society to optimise all children’s development and wellbeing from early life.
In New Zealand, a new longitudinal study of children and families was established in 2008 to provide evidence about what shapes contemporary children’s wellbeing and development. This study was deemed necessary because New Zealand children have continued to rank very poorly in terms of their wellbeing when compared to children growing up in other high-income countries (Adamson et al. 2007; Adamson 2010; NZ Child and Youth Epidemiology Service 2011; Baker et al. 2012; OECD 2014). These overall international comparisons hide unacceptable inequalities in child wellbeing outcomes for groups within the New Zealand population. Specifically, Māori and Pacific children and those growing up in the greatest socioeconomic adversity experience wellbeing outcomes below the population average. These wellbeing gaps have been persistent despite widespread acknowledgement that they exist. Consequently, it is important to understand the drivers of wellbeing for all children growing up in New Zealand today to ensure that effective support can be provided where it is needed most, and strategies can be developed based on lived realities of contemporary children and families to enable these inequalities not only to be repeatedly measured but also to be effectively reduced.
Growing Up in New Zealand
Growing Up in New Zealand is New Zealand’s largest contemporary longitudinal study of child development which began by recruiting mothers and their partners of the potential cohort in pregnancy from 2008. Participants were recruited from Auckland, Counties Manukau and Waikato District Health Boards if they had an estimated delivery date between April 25th, 2009 and March 25th 2010 (Morton et al. 2012b). A total of 6853 children were recruited and the cohort has subsequently been shown to be broadly generalisable to current Aotearoa, New Zealand births (Morton et al. 2015). Importantly, the study is of sufficient size to have adequate statistical power to examine what shapes child wellbeing outcomes across the diversity of current births with respect to the distribution of parental and child ethnicity and key socio-economic characteristics of contemporary New Zealand parents and families/whānau.
The study has collected extensive longitudinal information about parental, family and whānau wellbeing including family background, families and home environments, evolving socioeconomic status and connections to wider society that are important for intergenerational wellbeing from late pregnancy and across the cohort children’s early lives. Recognising the importance of the first 1000 days of a child’s life for shaping lifecourse wellbeing meant four detailed data collections were completed during this time.
To date, there have been five main face-to-face data collection waves (antenatal, 9 months, 2, 4.5 and 8 years) and at the time of writing the Growing Up team is in the field collecting information from the 12-year-old children and their caregivers. Interviews have primarily been conducted in the participants’ homes. Each of the main data collection waves consisted of parental reports, anthropometric assessments and child observations, with a child questionnaire also included at age 8 collecting the voices and views of the cohort children themselves for the first time. Telephone interviews and linkage to routine health datasets have also been conducted between the main data collection waves to collect additional information and assist with tracking and tracing.
The attrition rate of the cohort is low overall and is detailed in each of the cohort reports relating to the main data collection waves (Morton et al. 2012a, 2014b, 2017, 2020b), At the time of the last data collection (aged eight), 282 children had either been opted out of the study by their parents or had died, leaving 6571 of the original recruited sample of 6853 (96% of the birth cohort). Of the 6571 children eligible for the eight-year data collection 15% did not participate (1015 children). Many of these children ‘skipped’ the data collection wave and hence the proportion of the baseline cohort that has completely opted out is low (less than 10%) compared to other international contemporary cohort studies (Morton et al. 2020b). While there is some attrition bias (see Morton et al. 2020b) the ethnic identity of the children that participated in the eight-year data collection wave remains broadly generalisable to the ethnicity of the cohort of births continuing to allow for sub-group analysis.
Development during the first 1000 days
Evidence that the first thousand days of a child’s life (from conception until the end of their second year of life) are critical for setting life course wellbeing trajectories is now well accepted. Multiple studies have consistently demonstrated strong relationships between measures of child wellbeing over the first thousand days (including size at birth, early postnatal growth, early feeding and attachment, development of pro-social behaviours) and later life course opportunities for health, wealth, social and economic wellbeing (Phillips and Shonkoff 2000; Evans and English 2002; Walker et al. 2007). Importantly, trajectories that can be set into play in the first thousand days are not necessarily deterministic at an individual level but they can have long term implications at a population level (Morton et al. 2020a; Baldwin et al. 2021).
From conception, a developing fetus responds to changes in their environment, facilitated via the wellbeing experienced by their mother, including the influences of her own early life course wellbeing trajectory (Morton et al. 2014d). The mother’s wellbeing is dependent on her interactions and responses to stressors and cues in her proximal and distal family and wider social environments (Moore et al. 2017). Different theories have provided frameworks to link child wellbeing in the first thousand days of life with life course wellbeing, including the primarily biological Developmental Origins of Health and Adult Disease paradigm (Gluckman and Hanson 2006) and the Social Determinants of health framework, which acknowledges the importance of the social context experienced by individuals over time for shaping their health and wellbeing (Graham and Power 2004). The different research approaches have been integrated into a life course approach to health and wellbeing that posits that an individual develops as a result of the dynamic interactions between their own biologic potential (genomic and innate) and the proximal and distal environments around them (Ben-Shlomo and Kuh 2004).
A life course approach to wellbeing
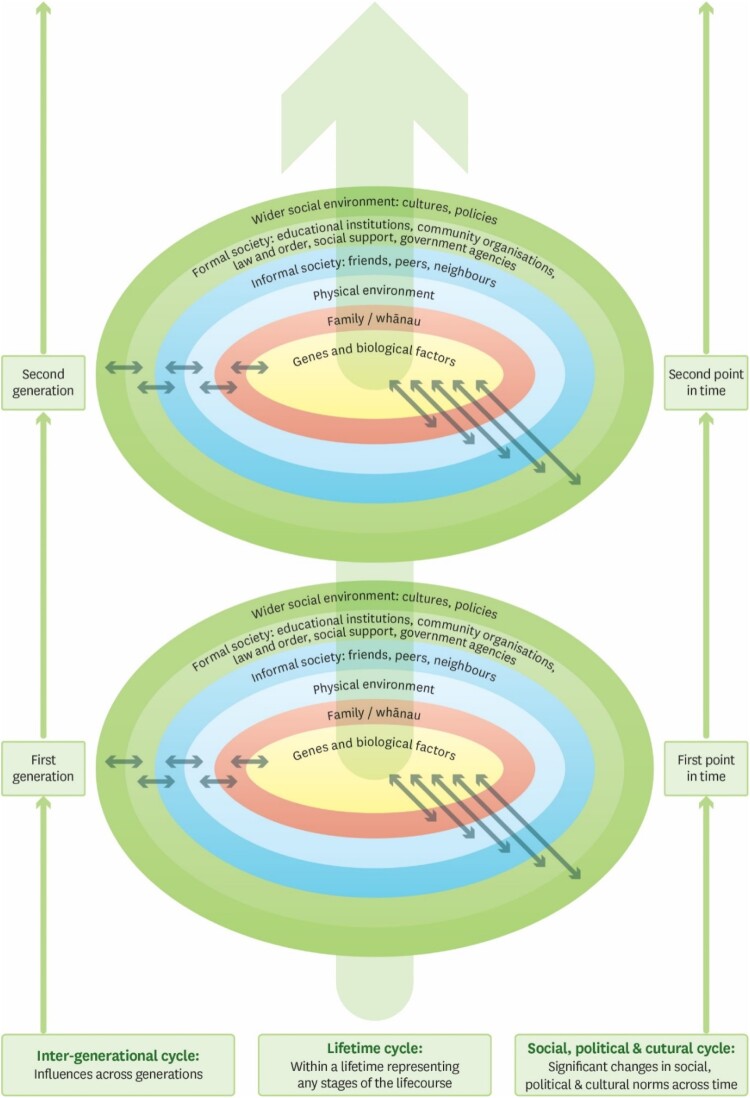
The conceptual framework for the Growing Up in New Zealand longitudinal study is grounded in life course epidemiology and takes a broad social determinants approach to child wellbeing (Figure 1).
Figure 1.
A life course and social determinants approach to wellbeing (Shulruf et al. 2007).
The framework acknowledges that children develop wellbeing and resilience in dynamic interaction with the people and environments they are exposed to over time. The environments range from the most proximal to more distal formal policy and global environments. During the first thousand days of life, the most important influences on child wellbeing are the psychosocial and physical environments provided by parents, families/whānau and households. Parental and family/whānau status is also dependent on relationships and interactions with proximal informal and formal structures within the wider societal environment that may either facilitate or hinder the ability of families to provide appropriate support to enable children to thrive.
Using the rich longitudinal evidence, collected directly from the Growing Up in New Zealand families and whānau (the cohort) over the first decade of the study, the evolution of early life wellbeing from the perinatal period and across the first thousand days into middle childhood has been tracked to understand how inequalities in wellbeing originate from birth onwards in the context of contemporary parental and family wellbeing. The longitudinal evidence has also been used to explore how to potentially support families to enhance children's wellbeing across the life course. These findings are summarised below.
Trajectories in early life
Perinatal wellbeing
Child wellbeing is shaped by the wellbeing and status of parents and their wider environments from before conception. Key known determinants of offspring wellbeing include completed level of maternal education, maternal age at the time of pregnancy and parental health-related behaviours (smoking, alcohol intake and use of illicit drugs). Further, offspring size at birth, an indicator of perinatal health, is patterned by a mother’s own life course growth and development from her own childhood (Morton et al. 2014d; Moore et al. 2017). Intergenerational continuities in wellbeing mean that not all children are born with the same opportunities for achieving optimal life course wellbeing.
Preparation for pregnancy can partially mitigate transmission of intergenerational disadvantage if pregnancy is intentionally planned (Davies et al. 2016). However, in the Growing Up in New Zealand, 40% of the 6822 pregnant mothers reported that their pregnancy was unplanned. Unplanned pregnancies were more prevalent in mothers already experiencing poorer physical, mental, psychosocial, and socioeconomic wellbeing. Mothers tended to be younger (mean age of 28 years compared to 32 years for planned pregnancies), without a current partner and with fewer completed educational qualifications (22% had completed post NCEA qualifications compared to almost half of all mothers where pregnancy was planned). Unplanned pregnancies were also reported as often for subsequent births (40%) as for first births (Morton et al. 2010).
An unplanned pregnancy limits the opportunities parents have to make choices and act on recommended behavioural changes either in the first trimester of pregnancy or before conception, including dietary changes. These changes can impact the nutritional environment a fetus experiences in its earliest days of development. Maternal nutrition has been associated with the in-utero growth trajectory as well as with postnatal growth and risk of childhood obesity, which in turn is associated with risks for chronic diseases such as diabetes, cancer and cardiovascular diseases (Harding 2001; Davies et al. 2016).
Whether a pregnancy was planned or not, the overall adherence to the current New Zealand Ministry of Health recommended nutritional guidelines by mothers of the Growing Up in New Zealand cohort was poor. The majority (97%) of all pregnant mothers did not meet all the NZ Ministry of Health guidelines relating to the recommended quantity and diversity of dietary intake in pregnancy (Morton et al. 2010). Adherence to guidelines was lowest in pregnancies that were unplanned, as well as in younger mothers and those experiencing the greatest economic hardship. Mothers with less family support were also less likely to be enabled to action the behavioural choices they wished to make during their pregnancy, despite usually having sufficient knowledge about why these changes were important for their child’s wellbeing (Morton et al. 2012a).
In terms of supplementation with folic acid, 90% of mothers did not take folic acid as recommended (starting prior to pregnancy and reducing after the first trimester), and one in six mothers did not take any folic acid before or during pregnancy. In an unplanned pregnancy there is little or no chance for a mother to begin supplementation prior to conception, hence recommendations to fortify basic foods, such as bread and flour, at a population level so that all potential parents might benefit. The Growing Up in New Zealand evidence showed that mothers who are most likely to experience an unplanned pregnancy do differentially consume greater quantities of the foods that are now planned to be supplemented following a recent (2021) government decision.
In terms of health-related behaviours known to impact perinatal wellbeing, 11% of all cohort mothers continued to smoke throughout their pregnancies after their first trimester (Law et al. 2003). In unplanned pregnancies, 21% continued to smoke tobacco beyond their first trimester, compared to only 4% of mothers where the pregnancy was planned (Morton et al. 2010). Mothers were also more likely to smoke throughout their pregnancies if they lived in the highest deprivation areas (17% compared to 5% in the least deprived areas) and if they had less completed maternal education (43% of mothers who had no formal secondary school qualifications smoked throughout pregnancy compared to 2% who had completed tertiary level education). Seven percent of mothers reported being regularly in the vicinity of other smokers (passive smoking), half of whom were smokers themselves, potentially creating a double burden in terms of the impact on child wellbeing from early life (Collaco et al. 2017).
Similarly, exposure to alcohol in pregnancy, especially during the first trimester, is a major cause of cognitive impairment and neurodevelopmental problems in children globally, with physical, learning and behavioural impacts, which collectively can result in fetal alcohol spectrum disorder (FASD) (Elliott et al. 2008). This spectrum of disorders remains quite poorly recognised in early childhood, and the effects may not be evident until middle childhood, when they can be indicative of lifelong cognitive and behavioural challenges (Elliott et al. 2008; Moore et al. 2017). Seventy percent of the cohort mothers regularly consumed alcohol prior to their pregnancy and more than 5% consumed alcohol at a level categorised as dangerous (more than 20 standard drinks per week) after their first trimester (Morton et al. 2010). Fewer mothers of unplanned pregnancies (69%) had stopped drinking alcohol after becoming aware they were pregnant compared to 83% of mothers of planned pregnancies who reported stopping drinking by their first trimester (Morton et al. 2010) Longitudinal research found that even when low levels of alcohol were consumed during early pregnancy, small associations with infant temperament were found (less positive affect, regulation and attention/orientation). Higher levels of antenatal alcohol consumption were associated with an increased likelihood of conduct problems and higher total difficulties scores when the child was 2 years of age. Mothers who stopped drinking after they became aware they were pregnant but had an unplanned pregnancy (and hence may have a baby exposed to alcohol for longer), also reported infants with lower attention/orientation, regulation, and higher fear, compared to those that did not drink (Schoeps et al. 2018). These findings were found after controlling for a range of maternal and child covariates (including socio demographics, maternal employment status, smoking, mental health, perceived stress, and child gestation, birth weight, gender).
Maternal mental health
Maternal wellbeing is a major determinant of the nature of the environments that infants experience from conception. When a mother is experiencing poor wellbeing (mental, physical or psychosocial) this can disrupt the quality and consistency of the proximal care-giving environment she is able to provide during a child’s first thousand days (Moore et al. 2017). The disruptive impact of poor maternal mental health has been shown to persist throughout the pre-school years with children born to mothers who were experiencing depressive symptoms during infancy having reduced cognitive scores and a greater prevalence of behavioural problems at age four, both of which can predispose individuals to life-long reductions in their human capital (Frank and Meara 2009).
Maternal depressive symptoms measured in Growing Up in New Zealand revealed 12% of mothers were experiencing symptoms characteristic of depression late in their pregnancies, and most (80%) were not receiving any concurrent pharmacological treatment (Svardal et al. 2021). Depressive symptoms were more common for younger mothers (less than 30 years of age at pregnancy) and those who identified as Pacific, Māori or Asian (compared to NZ European). Receiving pharmacological treatment in the presence of depressive symptoms was least common for Māori and Pacific mothers (Svardal et al. 2021).
During infancy, the overall proportion of mothers experiencing depressive symptoms dropped to 8%, but there was considerable flux at an individual level. Approximately half of the mothers experiencing postnatal symptoms were newly identified as having depressive symptoms postnatally, and half of the mothers who were experiencing depressive symptoms in late pregnancy did not have significant depressive symptoms postnatally. Depressive symptoms increased postnatally if the household financial situation had worsened, or if physical or psychological inter-partner conflict was reported by the mother after the birth of her child (Morton et al. 2012a). By contrast, mothers who had returned to work by the time their children were nine months old and those reporting higher levels of external family support (informal or formal) tended to have better mental wellbeing in the postnatal period compared to during pregnancy. These effects were found after controlling for a wide range of covariates including maternal demographics, mental health issues prior to pregnancy and health behaviours prior to and during pregnancy, specific physical health issues, and relationship conflict.
Findings from Growing Up in NZ looking at risk factors for early childhood cognition found that while a number of perinatal environmental factors (pre and antenatal smoking, lack of folate in the first semester, maternal stress, and anxiety) were found to be related to children’s cognitive abilities (executive control, motor ability and receptive language) at 4.5 years age, antenatal depression was not significantly related to any of the 4-year cognitive outcomes (Neumann et al. 2019). These findings highlight the need to take a broad view of maternal mental health, especially during the prenatal period, and consider the role of stress and anxiety which notably frequently coexist with other behaviours such as substance abuse.
Paternal mental health
The mental health of other adults in the family home also impacts on the quality of the proximal environment provided to support children’s wellbeing. Twice as many new fathers of the Growing Up in New Zealand cohort experienced depressive symptoms as age-matched males in the general population who were not experiencing the birth of a new baby, although the rates were lower for fathers than mothers (6% of new dads compared to 3% of males in the general population – postnatally). In contrast to mothers, depressive symptoms were more prevalent in fathers postnatally than antenatally. Poorer paternal mental wellbeing also increased the likelihood that a mother would experience poorer mental wellbeing postnatally (but not vice versa). Akin to passive smoking, this cumulative parental burden of poor mental health potentially exacerbates the impact of poor parental wellbeing on the child’s immediate and longer-term wellbeing (Kim-Cohen et al. 2005).
Psychosocial stress
Transition to parenthood is generally a time of increased stress for all parents, but higher levels of maternal stress have been linked to reduced size at birth, reduced maternal bonding in the immediate postnatal period and an increased risk of behavioural and emotional problems during childhood (Matvienko-Sikar et al. 2021). Stress is a multifaceted construct that covers psychological stress and physiological stress at an individual level as well as exposure to external stressors in the wider environment. Parental stress likely influences child wellbeing through multiple pathways. Current theories suggest maternal stress influences the epigenome of the developing infant and thus creates life-long changes in offspring stress responsiveness to their environments (Shonkoff and Garner 2012). Within Growing Up in New Zealand higher levels of maternal perceived psychosocial stress during pregnancy were associated with increased rates of childhood obesity (after adjusting for mother’s ethnicity, maternal education, household income, maternal BMI, and childbirth weight and gender) (Farewell et al. 2018) and depressive symptoms at aged 8 (after adjusting for rurality, neighbourhood deprivation, parity, child gender mother ethnicity, maternal age, planned pregnancy and education) (Theunissen et al. 2022) as well as poorer cognitive outcomes at aged 2 and 4 (Neumann et al. 2019).
The impacts of maternal mental, physical and psychosocial wellbeing on maternal and child health are often considered separately, but it is clear from the Growing Up in New Zealand cohort that these multiple stressors tend to cluster and are more common in mothers who are more socioeconomically disadvantaged, specifically those experiencing greater material hardship, financial stress and relationship conflict (Morton et al. 2012a).
Home environments
The nature of the inter-parental relationship is an important source of either support or stress for parents during pregnancy and thereafter. The quality of the interparental relationship impacts the wellbeing of both parents as well as the wellbeing of their children. Pregnancy has been recognised as a time when domestic violence tends to worsen in terms of physical and psychological violence, particularly towards mothers (Moore et al. 2017). Research also shows that abuse during pregnancy strongly predicts the likelihood of abuse continuing in the postnatal period. Children who have witnessed interparental violence in their earliest years have been shown to have poorer psychological wellbeing, manifesting in eating and sleep disturbances as well as slower development throughout early childhood when compared to their peers and lower levels of social competence in later life (Moore et al. 2017). Approximately one in ten children in the cohort have regularly witnessed interparental emotional, psychological and physical conflict throughout their early years (Morton et al. 2017, 2020b). Children inevitably learn behaviours from observing their parents’ behaviours and the way they engage with each other. It seems likely that the frequent exposure to interparental conflict may be related to the high rates of early child bullying reported across the cohort. Before entry to formal schooling, one in three of the children are reported by their mothers as being regularly bullied by their peers, and 10% of the cohort are reported as experiencing persistent bullying between 2 and 4 years of age (Morton et al. 2017).
Increasingly in New Zealand, children are being raised in extended family/whānau households, which are often multi-generational. The wellbeing of all those in the extended family household can impact children’s health and wellbeing in both positive and negative ways. One in four of the cohort children (25%) were born into an extended family household and one in five children were living in this type of household environment at the time they were preparing to start formal schooling, with change in household structures common throughout childhood (Morton et al. 2020b). The structure of households varies by parental ethnicity. It is more common for children whose mothers identify as Pacific or Asian to live in extended family households (54% and 30% respectively), and less common for NZ European children to do so (13%) around the time of a child’s birth.
Many extended households meet the criteria for living in overcrowded situations (defined as having two or more people per bedroom in a dwelling). Overcrowding has been associated with poorer child wellbeing outcomes including avoidable admissions to hospital with respiratory infections in early life and Streptococcal infections in later childhood that are associated with Rheumatic fever and its sequelae of chronic medical issues (cardiac and renal predominantly) throughout the life course (Oliver et al. 2017). Overcrowding in childhood has also been found to be a major contributing factor to a higher prevalence in adults of h. pylori infection and a key driver of an excess risk of later stomach cancer for Māori and Pasifika (McDonald 2014). However, overcrowded households can also create supportive environments to enable child wellbeing. For example, during the first NZ lockdown during the COVID pandemic in 2020 children living in households (bubbles) with more than six people were relatively protected from increased anxiety and depression compared to children in homes with fewer people (Walker et al. 2021).
Housing quality – safety and warmth
The physical environments that children experience in their early years also impacts their wellbeing. Whether a home environment has features that allow children to grow and explore in a safe way can mean the difference between experiencing preventable injuries or facilitating safe exploration that can enhance cognitive wellbeing. Stability of the physical home environment is also important for child wellbeing in their early years, as is the quality of the homes that children grow up in (especially in terms of ambient temperature and dampness) (Ingham et al. 2019).
Many of the houses families were living in during their children’s first thousand days did not adhere to current recommended safety guidelines. By the age of two almost one in three of the cohort had had a significant injury, most often in their homes, requiring medical treatment (Growing Up in New Zealand 2014). More than one in five (21%) of the children’s homes did not have working smoke alarms, almost 25% of homes did not have a safe fenced play area and 40% did not have a fully fenced driveway. These safety features were much less common for families living in rental properties and living in the highest deprivation areas (Morton et al. 2014b). Almost half of the cohort were living in rental accommodation (40% in private and 7% in public rentals) at birth, and almost half (45%) at two years.
Many of the homes the children were growing up in their earliest years were also regularly damp (20%) and cold (22%), including the bedrooms that the children slept in. Experiencing damp and cold environments has negative impacts on wellbeing for all age groups in a population, but children are particularly sensitive. Experiencing colder environments is associated with greater risks of childhood respiratory illnesses, including serious events requiring hospital admission (Ingham et al. 2019; Morton et al. 2020c). Experiencing cold and damp homes in addition to overcrowding is also associated with Rheumatic fever and its chronic sequelae which disproportionately impact Māori and Pacific New Zealand children (Oliver et al. 2017).
In infancy over one in five (22%) children were sleeping in bedrooms that were often or always cold and damp, increasing to 30% for children living in the highest deprivation areas. Almost one in five families (19%) also reported putting up with feeling cold to save on heating costs when their children were infants. By age eight, one in three children were living in homes that were regularly cold. For those living in the highest deprivation areas, this was the case for over half of children. Almost four in ten (37%) children, at age eight, also experienced exposure to dampness and mould. Exposure was highest for children who identified as Māori or Pacific (partly explained by area-level deprivation).
In 2018, the cohort children (aged eight) were provided with small hand-held temperature and humidity monitors to measure the temperatures and relative humidity in their bedrooms over two assigned days, including when they went to bed at night. Overall these direct measures demonstrated that 60% of the cohort children were regularly experiencing less than optimal temperatures in their bedrooms at night, and that this was associated with poorer physical and mental wellbeing, including higher rates of asthma, allergy and respiratory illness and higher depression and anxiety scores at age eight. Exposure to less than optimal indoor environments was more frequent for children in families experiencing greater financial stress and economic hardship (Morton et al. 2020c). These effects were found after controlling for neighbourhood and individual level deprivation as well as seasonality.
Residential mobility
Regular residential mobility, especially if necessitated because of changes in employment and economic circumstances, can impact on children’s development and life course trajectories of wellbeing (Jelleyman and Spencer 2008; Morton et al. 2014a). High rates of residential mobility during childhood have been associated with increases in behavioural problems in early childhood and more engagement in risk-taking behaviours in adolescence. Frequent mobility is also associated with discontinuity of engagement in health services (Jelleyman and Spencer 2008).
Residential mobility can mean children are moving to more stable and secure environments which can be positive for children’s wellbeing in the medium to longer term. However, overall greater family residential mobility tends to be associated with poorer child wellbeing at a population level because it tends to occur most often for families who are already burdened by financial hardship and instability in employment and relationships (Jelleyman and Spencer 2008).
This generation of families with young children appears to be highly mobile. Only one in three of all the Growing Up in New Zealand cohort children and their families had not moved house at least once during their pre-school years and a few families (less than 1% overall) had experienced more than ten moves in less than five years (Morton et al. 2017). By the time the children were eight years of age only one in four of all the Growing Up in New Zealand cohort children had not experienced any residential mobility at all during their short lives (Morton et al. 2020b).
The most important determinant of mobility in the children’s early years was tenure type, with the greatest mobility in infancy seen for children born into and growing up in private rentals (40% moved). Mobility was less common for children in public rentals (25% moved) and only 20% of families who owned their homes (with or without a mortgage) moved in the perinatal period. Parents who reported better neighbourhood integration and feeling safe and secure in their neighbourhoods in late pregnancy, regardless of tenure, were significantly less likely to move postnatally (Morton et al. 2014a). Higher residential mobility was seen for families at both extremes of financial wellbeing. Higher levels of financial stress were associated with an increased chance of mobility, as was moving to or maintaining a higher level of family or household income. Parents who reported higher levels of external family support were less likely to move, but the quality of the home environment (in terms of damp and mould) did not impact mobility after adjusting for other family and socio-demographic factors (Morton et al. 2014a).
Throughout childhood, up to and including age eight, the most important factor for predicting residential mobility across time was living in a rental property. In general, movement for renters was between private rental properties rather than into more secure home ownership. Given that rental properties are least likely to be safe, and more often cold and damp, this mobility adds to the burden of poor child wellbeing. By age eight, after controlling for a range of neighbourhood and family socio-demographic covariates, we found children who had experienced the greatest mobility were more likely to be overweight or obese, and have higher depression and anxiety scores than their peers who had experienced more residential stability (Morton et al. 2020b). We also found that high residential mobility and financial stress in the first 1000 days of life were related to increased odds of having two or more chronic health conditions by the age of 2 (e.g, asthma or eczema requiring medication, birth condition, obesity) (Russell et al. 2020). This highlights the potential impact that cumulative socioeconomic disadvantage can have on the chance of chronic health conditions developing in the early years over and above factors such as maternal health, depression, birth weight and smoking and alcohol consumption during pregnancy.
Ethnic identity
Having a strong sense of identity is important for parental wellbeing and important for intergenerational transfer of strong identities to enhance children’s wellbeing. During pregnancy, mothers of the cohort children and their partners expected one in four (24%) children to identify as Māori, one in five (21%) as a Pacific ethnicity, and one in six (16%) as Asian, with seven out of ten (73%) expected to identify as New Zealand European. Almost half the children were expected to identify with more than one ethnic group (48%).
For almost all wellbeing metrics in Aotearoa, New Zealand, we see inequalities by ethnicity. Māori and Pacific parents are over-represented in measures of poorer physical wellbeing in pregnancy (higher rates of unplanned pregnancies, higher proportions of maternal and paternal smoking, greater likelihood of parental obesity, less adherence to nutritional guidelines), and they are also over-represented in measures of poor maternal mental wellbeing (higher depression and anxiety scores). In the postnatal period children identified as Māori or Pacific are over-represented in poorer wellbeing statistics, including being at greater risk of respiratory infections and hospitalisations for severe infections during infancy, experiencing more frequent ear and throat infections in their first thousand days, and being more likely to be classified as overweight and obese in their pre-school years (Morton et al. 2014b).
Experiences of environmental adversities over the first thousand days are also unequally distributed by ethnicity, with more parents who identify as Māori, Pacific and to a lesser extent Asian, as well as those living in areas of high deprivation (with considerable overlap between ethnic identity and deprivation area), experiencing greater rates of unemployment, less total household income and more financial hardship and financial stress (Morton et al. 2014c). Poorer parental and child wellbeing, while being greater in those who identify with non-European ethnicities, does not result from ethnic background or cultural identity alone. The poorer intergenerational wellbeing is much more likely to be the result of exposure to, and the accumulation of, intergenerational stressors and hardships experienced over time, including exposure to systemic discrimination.
Exposure to systemic discrimination, for non-European New Zealanders and for many migrants, remains prevalent within New Zealand society. Feeling accepted and welcome within society is important for parents’ wellbeing as well as for intergenerational transfer of wellbeing to their children (Talamaivao et al. 2020). In the Growing Up in New Zealand cohort, Māori, Pacific, and Asian women that had experienced unfair treatment by a health professional were found to be 66% more likely to suffer from postnatal depression, compared to women who did not report these experiences. Further, a dose response association between lifetime experiences of ethnically-motivated personal attacks and poor maternal mental health was also found (Bécares and Atatoa-Carr 2016). Feeling accepted and welcome also matters for timely access to and utilisation of universal services designed to support wellbeing.
Parental and family socioeconomic status
A significant body of evidence supports strong and consistent relationships between exposure to what are collectively referred to as the social determinants of health and adverse health and wellbeing outcomes across the life course and across generations (Kramer et al. 2000; Moore et al. 2017). Measures of parental socio-economic status, including completed parental education, parental employment, parental and household incomes (total and relative), and collective measures such as the deprivation area that a family resides in, each show a graded association with wellbeing across the life course, starting from the first thousand days of life (Heckman 2007). While trajectories established in early life are not deterministic, it is theorised that it is easier to establish the foundations of good child wellbeing in the first thousand days of life than it is to remediate the impacts of disadvantage later in the life course (Center on the Developing Child 2010).
However, while singular measures of parental wellbeing and household socioeconomic status show strong graded relationships with early child wellbeing, their individual effects on later life outcomes have been found to be relatively modest (Fergusson and Horwood 2003). More recently exposures to multiple parental and family risk factors have been considered together, given that this is the lived reality for families with young children internationally as well as in NZ (Luthar 2003). Longitudinal studies such as Growing Up in New Zealand that can track the impact of the early family environment and multiple measures of parental wellbeing on children’s wellbeing over time are considered ideally placed to pursue this research (Sabates and Dex 2012).
Child wellbeing trajectories in the first thousand days of life have been shown to be highly sensitive to the combination of parental wellbeing and household socioeconomic factors measured around the time of birth in international longitudinal studies (Heckman 2007; Sabates and Dex 2012). Growing Up in New Zealand information collected over the first thousand days was used to consider clustering and the cumulative impact of exposure to social disadvantage during a child’s early life in NZ today. The risk factors chosen (Table 1) were based on international evidence regarding: existing literature demonstrating a relationship to unfavourable wellbeing outcomes for children; suitability to the age of the children and the lifecourse stage of the parents; risks that might be directly targeted by government policies; and the prevalence and reliability of the measures (Sabates and Dex 2012).
Table 1.
Parental and family/whānau risk factors for poor child wellbeing over first 1000 days.
| Proximity to child | Risk factors | Prevalence in GUiNZ (%)a | ||
|---|---|---|---|---|
| Pregnancy (antenatal) | 9 mth (infancy) | 2 yrs | ||
| Proximal family variables | Maternal depression (EPDS >12)b | 12.1% | 7.9% | – |
| Maternal physical wellbeing (poor/fair)b | 9.6% | 9.4% | – | |
| Maternal smoking | 10.2% | 13.6% | 13.5% | |
| Maternal age (teenage pregnancy)c | 4.4% | – | – | |
| Distal family variables | Relationship status (no partner/single) | 9.1% | 8.1% | 9.7% |
| Maternal education (no secondary qualification)c | 6.1% | – | – | |
| Financial stress (high) | 17.3% | 14.3% | 16.9% | |
| Home environment | Deprivation area (NZDep2006 decile 9 or 10) | 25.7% | 25.0% | 25.0% |
| Unemployment (mother not in work or on parental leave) | 8.1% | 6.1% | 6.9% | |
| Tenure (public rental) | 6.9% | 6.6% | 6.1% | |
| Income tested benefit | 14.3% | 16.9% | 16.0% | |
| Overcrowding (≥2 per bedroom) | 12.8% | 20.6% | 20.4% | |
Percentages are based on denominator of N = 5737 – participants with complete information on 12 risk factors and who participated in the 2 year Data Collection Wave.
Not measured again at 2 years given little expected proportional change.
Not measured again in first 2 years postnatally (no change).
The international analyses were extended in the NZ context to include perinatal measures and consider the persistence of exposure (clustering and accumulation) across the three-time points information was collected over the first thousand days of life (Morton et al. 2014c).
Exposure to the set of risk factors in Table 1 clustered across the cohort, albeit not uniformly (Morton et al. 2014c). Parental and family/whānau risks that clustered together (co-occurred) across the cohort included being a young (teenage) mother, maternal smoking, being on an income-tested benefit, living in a public rental home, having no partner and not having any formal secondary school qualifications. This was in contrast to financial stress, maternal depression and poor physical wellbeing (including maternal disability) that commonly occurred as single risk factors (Morton et al. 2015). Exposure to the type and number of these risks was also unequally distributed according to maternal ethnicity, with a greater absolute number of risks being experienced by children born to Māori and Pacific mothers.
The risk factors that clustered together were not always the same set of risks but the burden experienced appeared to be proportional to the absolute number experienced, rather than the specific factors (Sabates and Dex 2012). Experiencing any four or more of the risk factors at any time point identified families experiencing significant socioeconomic adversity in Growing Up in New Zealand (Center on the Developing Child 2010). At each timepoint across the first thousand days, around 13% of the cohort children were exposed to significant socioeconomic adversity.
While the absolute proportions of cohort parents and families experiencing significant adversity at each time point were similar at a population level, there was considerable flux in the individual children who were exposed to this persistent level of adversity (Morton et al. 2014c). Those children who were exposed to persistent significant adversity over their first thousand days were falling behind their peers in terms of multiple measures of their wellbeing during their preschool years. The co-morbidities experienced tended to cluster and accumulate and collectively diminish opportunities for achieving life course wellbeing (Russell et al. 2020). Impacts of persistent exposure included poorer physical wellbeing: less completed and timely immunisations; greater risks of being overweight or obese; more serious and repeated respiratory infections; more accidents and injuries, and poorer psychosocial wellbeing: greater risk of displaying abnormal behaviours, less self-regulation, and poorer cognitive development. There were also measurable impacts on early literacy and numeracy with children exposed to persistent adversity being less ready for school than their peers (The Southern Initiative and Auckland Co-Design Lab 2017; Wallander et al. 2019; Russell et al. 2020).
By the time the cohort children reached middle childhood (eight years old), the longitudinal picture that has emerged is one of a growing disproportionate burden of poorer overall child wellbeing outcomes across multiple domains of development (physical, mental and psychosocial) and more limited opportunities for the children exposed to persistent adversity across childhood (Morton et al. 2020b). The gaps that were emerging in terms of impact on child wellbeing during the first thousand days of life and before school entry have been further exacerbated by the cumulative experience of adversity for children growing up with parents and in families/whānau who have been chronically burdened by economic, physical and psychosocial external and internal stressors beyond the perinatal period (Morton et al. 2020b).
Using longitudinal information to co-create innovative solutions
While poorer wellbeing is much more likely for cohort children exposed to persistent adversity across their first thousand days, not all individual children who experienced this clustering of significant adversity had poorer early wellbeing relative to their cohort peers.
Growing Up in New Zealand longitudinal information gathered directly from the families was utilised to understand what parental and family/whānau behaviours and characteristics, and what external informal and formal supports, conferred resilience in terms of protecting the wellbeing of children who were exposed to persistent early life adversity.
This approach was recently utilised in a collaborative project with South Auckland co-design experts and with communities who experience the greatest burden of life course socioeconomic disadvantage (The Southern Initiative and Auckland Co-Design Lab 2017). The breadth of longitudinal information collected specifically from the 1252 children and their families/whānau in the cohort growing up in South Auckland was examined to understand what could enable resilience and promote child wellbeing in the face of persistent parental and family socioeconomic adversity.
In the collaborative project, resilience was considered as a multidimensional construct encompassing more than the absence of exposure to risk factors, although resilience should be enabled if exposure to risk factors is reduced. Resilience factors were defined as those in the wider environment that could support or enable wellbeing rather than being innate characteristics of a child or their family (National Scientific Council on the Developing Child 2015).
The information collected directly from the families and children growing up in South Auckland demonstrated that if families had: good informal networks and support systems; if they had safe places to gather to support each other outside their home environments; and if services designed to support child wellbeing could come to those safe spaces rather than families and parents needing to reach out to find and connect with services individually, then children in families and whānau who had that kind of informal and formal support wrapped around them in their first thousand days were much less likely to experience the same cumulative and multiple impacts on their wellbeing compared to the children in the cohort living in families and whānau experiencing the same significant adversity but without those informal and formal connections and supports (Morton et al. 2014c, 2015; The Southern Initiative Auckland Co-Design Lab 2017).
Discussion
The first thousand days of a child’s life are critical for establishing early wellbeing trajectories that are often starting points for later life opportunities and life course wellbeing. The collective findings from the contemporary New Zealand longitudinal study over the first decade provide evidence that prenatal and postnatal parental and family/whānau wellbeing influence the early life wellbeing of the current generation of New Zealand children in potentially important ways. From the time of conception, it is apparent that preparedness for pregnancy and readiness for the challenges that families and whānau will face once a child is born are not equitably distributed across all parents and families. The greatest challenges in terms of supporting children’s wellbeing will inevitably fall on those parents who are the youngest, with the least formal educational qualifications and with the least resources and opportunities to create a better life either for themselves or for their children in pregnancy or thereafter.
Exposure to material hardship and socio-economic disadvantage at any point in their lives can create a complex and challenging environment for individuals and families, and this is particularly the case when a new baby is born into a family. Giving every child the best start in life means enabling all parents to have the best wellbeing from before pregnancy and throughout the perinatal and postnatal periods. Of great concern in terms of supporting optimal perinatal wellbeing is that rates of maternal depressive symptoms measured in late pregnancy suggest that there is currently an opportunity gap in terms of ensuring all parents are optimally prepared for their child’s birth. Better screening for parental mental health issues at all points across the first thousand days with an increased awareness for mothers and families about how common and impactful mental ill health can be at this stressful time in their lives should become the norm. At a societal level, we require greater acknowledgement about how prevalent mental distress is in pregnancy and postnatally and how underlying socioeconomic disadvantage exacerbates poor wellbeing rather than poor maternal health being a reason for self-blame.
The wider family and home contexts and environments also matter for child wellbeing from pregnancy onwards. Currently, for example, too many families with young children do not have access to affordable, safe, warm and stable housing so they can provide the necessary environment to promote their child’s wellbeing. A significant proportion of this generation’s families are likely to be renting for most of their children’s early years, and rental properties (that almost half of the cohort spend their early years in) are the least safe, secure and stable environments for children to spend their early years in.
In the New Zealand context there continue to be unacceptable gaps in wellbeing by ethnic identity, with tamariki Māori and Pacific children experiencing a disproportionate burden of poor wellbeing throughout their lives. Taking a life course approach, it is apparent that families and whānau of Māori and Pacific children experience greater socioeconomic adversity at all time points during their children’s first thousand days, and across generations, which begins to explain, but not reduce, these disparities. In addition to a clear and ongoing need to address income inequality and socioeconomic adversity, evidence from the cohort suggests that these groups also have the greatest need for services to support their wellbeing, and that need is not being matched by service delivery. These groups also bear the burden of systemic discrimination.
When looking to services to help close the wellbeing gaps it is important that these are designed to support parents and family and that they are culturally acceptable and accessible. To ensure that service delivery is aligned to real need, more proportionate universal approaches (Marmot et al. 2011) should be considered, based on lived realities and co-design, to give all children an equally good start to life. Essentially this means providing disproportionately more support to those families and whānau who are already socially, physically and psychologically disadvantaged from before their children are born.
There is novel evidence from the Growing Up in New Zealand families about how we might support and work alongside contemporary families and whānau to enable them to provide an environment that is likely to give their children the best start in life and the best opportunities for life course wellbeing. Families who have good social networks, with their own extended families as well as with their wider communities, who feel safe and integrated into their neighbourhoods, who feel accepted and celebrated for their diverse backgrounds and cultural identities, and who can navigate the existing systems successfully to access what they need, appear to be able to mitigate the impacts that persistent economic adversity, poor housing and intergenerational disadvantage generally confer on their children’s wellbeing.
Applying approaches to support enabling resilience will not alleviate the clustering of adversity and poor wellbeing that too many parents, families and whānau in New Zealand are experiencing in the short term, and that Māori and Pacific tamariki experience disproportionately and unacceptably in Aotearoa today. However, it may mean that a further generation of New Zealand children are not left as far behind as we try to solve the wicked and entrenched, intergenerational continuities in poor wellbeing and social disadvantage that enable current international and NZ specific gaps in child wellbeing to persist.
Evidence collected directly from families and children themselves in longitudinal studies such as Growing Up in New Zealand can help build better opportunities for all families having children in New Zealand today and inform the design of appropriate multi-level supports to enable families and whānau to grow a healthier future for all our tamariki and for all of our futures.
Acknowledgements
Growing Up in New Zealand is indebted to the children and families who so generously share their time and information with the study team. It is only through the continued generosity of every one of the cohort members that these research outputs can be developed and the wider body of knowledge accumulated to enhance the lives and wellbeing of all New Zealand children.
Funding Statement
Growing Up in New Zealand is led by the University of Auckland with management of the contract through Auckland UniServices Limited. The study has been funded by the New Zealand Government and funding is managed through the Ministry for Social Development. Funding and support have also been received from the Ministries of Health and Education, as well as Oranga Tamariki, Te Puni Kōkiri, the Ministry of Justice, the Ministry of Business Innovation and Employment, the Ministry for Pacific Peoples, the Ministry for Women, and the Department of Corrections. Support has also been provided for the study from the Office of the Children’s Commissioner, Housing New Zealand (now Ministry of Housing and Urban Development), the Office of Ethnic Communities, Statistics New Zealand, the Department of Prime Minister and Cabinet and the Treasury.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Adamson P. 2010. The children left behind: a league table of inequality in child well-being in the world’s rich countries. Innocenti Report Card 9. Florence: UNICEF Innocenti Research Centre. [Google Scholar]
- Adamson P, Bradshaw J, Hoelscher P, Richardson D.. 2007. Child poverty in perspective: an overview of child well-being in rich countries. Innocenti Report Card 7. Florence: UNICEF Innocenti Research Centre. [Google Scholar]
- Baker MG, Barnard LT, Kvalsvig A, Verrall A, Zhang J, Keall M, Wilson N, Wall T, Howden-Chapman P.. 2012. Increasing incidence of serious infectious diseases and inequalities in New Zealand: a national epidemiological study. The Lancet. 379(9821):1112–1119. [DOI] [PubMed] [Google Scholar]
- Baldwin JR, Caspi A, Meehan AJ, Ambler A, Arseneault L, Fisher HL, Harrington H, Matthews T, Odgers CL, Poulton R, et al. 2021. Population vs individual prediction of poor health from results of adverse childhood experiences screening. JAMA Pediatrics. 175(4):385–393. doi: 10.1001/jamapediatrics.2020.5602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bécares L, Atatoa Carr P.. 2016. The Association between maternal and partner experienced racial discrimination and prenatal perceived stress, prenatal and postnatal depression: findings from the Growing up in New Zealand cohort study. International Journal of Equity in Health. 15(1):155. doi: 10.1186/s12939-016-0443-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Shlomo Y, Kuh D.. 2004. A life course approach to chronic disease epidemiology. Oxford: Oxford University Press. [PubMed] [Google Scholar]
- Center on the Developing Child . 2010. The foundations of lifelong health are built in early childhood. Harvard University. [accessed 25 November 21]. http://www.developingchild.harvard.edu.
- Collaco JM, Wilson KM, McGrath-Morrow SA.. 2017. More evidence linking smoke-free legislation and lower risk of prematurity and low birth weight. Pediatrics. 139(6):e20170795. doi: 10.1542/peds.2017-0795. [DOI] [PubMed] [Google Scholar]
- Davies PSW, Funder J, Palmer DJ, Sinn J, Vickers MH, Wall CR.. 2016. Early life nutrition and the opportunity to influence long-term health: an Australasian perspective. Journal of Developmental Origins of Health and Disease. 7(5):440–448. doi: 10.1017/S2040174415007989. [DOI] [PubMed] [Google Scholar]
- Elliott L, Coleman K, Suebwongpat A, Norris S.. 2008. Fetal alcohol spectrum disorders (FASD): systematic reviews of prevention, diagnosis and management. Christchurch: Health Services Assessment Collaboration (HSAC) Report 2008. [Google Scholar]
- Evans GW, English K.. 2002. The environment of poverty: multiple stressor exposure, psychophysiological stress, and socioemotional adjustment. Child Development. 73(4):1238–1248. [DOI] [PubMed] [Google Scholar]
- Farewell CV, Thayer ZM, Tracer DP, Morton S.. 2018. Prenatal stress exposure and early childhood: exploring associations in a New Zealand context. American Journal of Human Biology. 30(4):e23116. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ.. 2003. Resilience to childhood adversity: results of a 21-year study. In: Luthar SS, editor. Resilience and vulnerability: Adaptation in the context of childhood adversities. Cambridge: Cambridge University Press; p. 130–155. [Google Scholar]
- Frank RG, Meara E.. 2009. The effect of maternal depression and substance abuse on child human capital development. Cambridge: National Bureau of Economic Research. No 15314. [Google Scholar]
- Gluckman PD, Hanson MA.. 2006. The Developmental Origins of Health and Disease . Cambridge: Cambridge University Press. [Google Scholar]
- Graham H, Power C.. 2004. Childhood disadvantage and adult health: a lifecourse framework. Child Care & Health Development. 30(6):671–678. [DOI] [PubMed] [Google Scholar]
- Growing Up in New Zealand . 2014. Growing in New Zealand policy brief. Keeping our children injury-free: household safety evidence from Growing in New Zealand. Auckland: Growing Up in New Zealand. [Google Scholar]
- Harding J. 2001. The nutritional basis of the fetal origins of adult disease. International Journal of Epidemiology. 30(1):15–23. [DOI] [PubMed] [Google Scholar]
- Heckman JJ. 2007. The economics, technology, and neuroscience of human capability formation. Proceedings of the National Academy of Sciences. 104(33):13250–13255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingham T, Keall M, Jones B, Aldridge DRT, Dowell AC, Davies C, Crane J, Draper JB, Baily LO, Viggers H, et al. 2019. Damp mouldy housing and early childhood hospital admissions for acute respiratory infection: a case control study. Thorax. 74(9):849–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jelleyman T, Spencer N.. 2008. Residential mobility in childhood and health outcomes: a systematic review. Journal of Epidemiology and Community Health. 62(7):584–592. [DOI] [PubMed] [Google Scholar]
- Kim-Cohen J, Moffitt TE, Taylor A, Pawlby SJ, Caspi A.. 2005. Maternal depression and children’s antisocial behavior: nature and nurture effects. Archives of General Psychiatry. 62(2):173–181. [DOI] [PubMed] [Google Scholar]
- Kramer MS, Séguin L, Lydon J, Goulet L.. 2000. Socio-economic disparities in pregnancy outcome: why do the poor fare so poorly? Paediatric and Perinatal Epidemiology. 14(3):194–210. [DOI] [PubMed] [Google Scholar]
- Law KL, Stroud LR, LaGasse LL, Niaura R, Liu J, Lester BM.. 2003. Smoking during pregnancy and newborn neurobehavior. Pediatrics. 111(6):1318–1323. [DOI] [PubMed] [Google Scholar]
- Luthar SS. 2003. Resilience and vulnerability: adaptation in the context of childhood adversities. Cambridge: Cambridge University Press. [Google Scholar]
- Marmot M, Allen J, Goldblatt P, Boyce T, McNeish D, Grady M, Geddes I.. 2011. Fair society, healthy lives. London: Institute of Health Equity. [Google Scholar]
- Matvienko-Sikar K, Cooney J, Flannery C, Murphy J, Khashan A, Huizink A.. 2021. Maternal stress in the first 1000 days and risk of childhood obesity: a systematic review. Journal of Reproductive & Infant Psychology. 39(2):180–204. [DOI] [PubMed] [Google Scholar]
- McDonald AM. 2014. Casting a long shadow: the role of household crowding on Helicobacter pylori infection, and excess stomach cancer incidence among Māori and Pacific people (Thesis, Master of Public Health). University of Otago.
- Moore T, Arefadib N, Deery A, West S.. 2017. The first thousand days: an evidence paper. Parkville: Centre for Community Child Healh, Murdoch Children’s Research Institute. [Google Scholar]
- Morton S, Lai H, Walker C, Cha J, Smith A, Marks E, Pillai A.. 2020c. Keeping our children warm and dry: evidence from Growing Up in New Zealand. Porirua: Building Research Association of New Zealand. [Google Scholar]
- Morton SMB, Atatoa Carr PE, Bandara DK, Grant CC, Ivory VC, Kingi TR, Liang TR, Perese LM, Peterson E, Pryor JR, et al. 2010. Growing up in New Zealand: a longitudinal study of New Zealand children and their families. Report 1: Before We Are Born. Auckland: Growing Up in New Zealand.
- Morton SMB, Atatoa Carr PE, Berry SD, Grant CC, Bandara DK, Mohal J, Tricker PJ.. 2014a. Growing Up in New Zealand: a longitudinal study of New Zealand children and their families. Residential mobility report 1: moving house in the first 1000 days. Auckland: Growing Up in New Zealand. [Google Scholar]
- Morton SMB, Atatoa Carr PE, Grant CC, Berry SD, Bandara DK, Mohal J, Tricker PJ, Ivory VC, Kingi TR, Liang TR, et al. 2014b. Growing up in New Zealand: a longitudinal study of New Zealand children and their families. Now we are two: describing our first 1000 days. Auckland: Growing Up in New Zealand. [Google Scholar]
- Morton SMB, Atatoa Carr PE, Grant CC, Berry SD, Marks EJ, Chen XM-H, Lee AC.. 2014c. Growing up in New Zealand: a longitudinal study of New Zealand children and their families. Vulnerability report 1: exploring the definition of vulnerability for children in their first 1000 days. Auckland: Growing Up in New Zealand. [Google Scholar]
- Morton SMB, Atatoa Carr PE, Grant CC, Berry SD, Mohal J, Pillai A.. 2015. Growing up in New Zealand: a longitudinal study of New Zealand Children and their families. Vulnerability report 2: transitions in exposure to vulnerability in the first 1000 days of life. Auckland: Growing Up in New Zealand. [Google Scholar]
- Morton SMB, Atatoa Carr PE, Grant CC, Lee AC, Bandara DK, Mohal J, Kinloch JM, Schmidt JM, Hedges MR, Ivory VC, et al. 2012a. Growing up in New Zealand: a longitudinal study of New Zealand children and their families. Report 2: Now We Are Born. Auckland: Growing Up in New Zealand.
- Morton SMB, Atatoa Carr PE, Grant CC, Robinson EM, Bandara DK, Bird A, et al. 2012b. Cohort profile: growing Up in New Zealand. International Journal of Epidemiology. 42(1):65–75. [DOI] [PubMed] [Google Scholar]
- Morton SMB, De Stavola BL, Leon DA.. 2014d. Intergenerational determinants of offspring size at birth: a life course and graphical analysis using the Aberdeen children of the 1950s study (ACONF). International Journal of Epidemiology. 43(3):749–759. [DOI] [PubMed] [Google Scholar]
- Morton SMB, Grant CC, Berry SD, Walker CG, Corkin M, Ly K, de Castro TG, Atatoa Carr PE, Bandara DK, Mohal J.. 2017. Growing up in New Zealand: a longitudinal study of New Zealand children and their families. Now we are four: describing the preschool years. Auckland: Growing Up in New Zealand. [Google Scholar]
- Morton SMB, Peterson E, Buckley J, Murray S.. 2020a. Early self-control development: prevalence, persistence and change in a NZ cohort. Wellington: Ministry of Social Dewvelopment. [Google Scholar]
- Morton SMB, Walker CG, Gerritsen S, Smith A, Cha J, Atatoa Carr P, Chen R, Exeter DJ, Fa’alili-Fidow J, Fenaughty J, et al. 2020b. Growing up in New Zealand: a longitudinal study of New Zealand children and their families. Now we are eight. Auckland: Growing Up in New Zealand. [Google Scholar]
- National Scientific Council on the Developing Child . 2015. Supportive relationships and active-skill building strengthening the foundations of resilience: Working paper 13. Boston: Center on the Developing Child, Harvard University. [Google Scholar]
- Neumann D, Herbert SE, Peterson ER, Underwood L, Morton SM, Waldie KE.. 2019. A longitudinal study of antenatal and perinatal risk factors in early childhood cognition: evidence from Growing Up in New Zealand. Early Human Development. 132:45–51. [DOI] [PubMed] [Google Scholar]
- NZ Child and Youth Epidemiology Service . 2011. Youth epidemiology service, the children’s social health monitor 2011 update. [accessed 25 November 21]. http://www.nzchildren.co.nz/.
- OECD . 2014. OECD factbook 2014: economic, environmental and social statistics. Paris: OECD Publishing. [Google Scholar]
- Oliver JR, Pierse N, Stefanogiannis N, Jackson C, Baker MG.. 2017. Acute rheumatic fever and exposure to poor housing conditions in New Zealand: a descriptive study. Journal of Paediatrics and Child Health. 53(4):358–364. [DOI] [PubMed] [Google Scholar]
- Phillips DA, Shonkoff JP.. 2000. From neurons to neighborhoods: the science of early childhood development. Washington DC: National Academies Press. [PubMed] [Google Scholar]
- Russell J, Grant CC, Morton SMB.. 2020. Multimorbidity in early childhood and socioeconomic disadvantage: findings from a large New Zealand child cohort. Academic Pediatrics. 20(5):619–627. [DOI] [PubMed] [Google Scholar]
- Sabates R, Dex S.. 2012. Multiple risk factors in young children’s development. London: Centre for Longitudinal Studies, Institute of Education, University of London. [Google Scholar]
- Schoeps A, Peterson ER, Mia Y, Waldie KE, Underwood L, D’Souza S, Morton SM.. 2018. Prenatal alcohol consumption and infant and child behavior: evidence from the Growing Up in New Zealand cohort. Early Human Development. 123:22–29. [DOI] [PubMed] [Google Scholar]
- Shonkoff JP, Garner AS.. 2012. The committee on psychosocial aspects of child family health, committee on early childhood, adoption, and dependent care, section on developmental behavioral pediatrics. 2012. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 129(1):e232–e246. [DOI] [PubMed] [Google Scholar]
- Shulruf B, Morton S, Goodyear-Smith F, O’Loughlin C, Dixon R.. 2007. Designing multidisciplinary longitudinal studies of human development: analyzing past research to inform methodology. Evaluation & Health Professions. 30(3):207–228. [DOI] [PubMed] [Google Scholar]
- Svardal CA, Waldie K, Milne B, Morton SMB, D’Souza S.. 2021. Prevalence of antidepressant use and unmedicated depression in pregnant New Zealand women. Australian & New Zealand Journal of Psychiatry. doi: 10.1177/00048674211025699. [DOI] [PubMed] [Google Scholar]
- Talamaivao N, Harris R, Cormack D, Paine S-J, King P.. 2020. Racism and health in Aotearoa New Zealand: a systematic review of quantitative studies. The New Zealand Medical Journal. 133(1521):58–68. [PubMed] [Google Scholar]
- The Southern Initiative and the Auckland Co-Design Lab . 2017. Early years challenge: supporting parents to give Tamariki a great start in Life. Auckland: the southern initiative. [accessed 25 November 21]. https://static1.squarespace.com/static/5cf74c8f2829e20001db724f/t/5d0dc5ae247fa10001df4e30/1568803263111/Early+Years+Challenge.
- Theunissen G, D’Souza S, Peterson ER, Walker C, Morton SMB.. 2022. Prenatal determinants of depressive symptoms in childhood: evidence from Growing Up in New Zealand. Journal of Affective Disorders. 302:41–49. [DOI] [PubMed] [Google Scholar]
- Walker N, Dubey N, Bergquist M, Janicot S, Swinburn B, Napier C, Peterson E, Evans R, Gerritsen S, Langridge F, et al. 2021. The GUiNZ COVID-19 wellbeing survey: part 1: health and wellbeing. Auckland: Growing Up in New Zealand. [Google Scholar]
- Walker SP, Wachs TD, Gardner JM, Lozoff B, Wasserman GA, Pollitt E.. 2007. Child development: risk factors for adverse outcomes in developing countries. Lancet. 369(9556):145–157. [DOI] [PubMed] [Google Scholar]
- Wallander JL, Berry S, Atatoa Carr PE, Peterson ER, Waldie KE, Marks E, D’Souza S, Morton SMB.. 2019. Patterns of exposure to cumulative risk through age 2 and associations with problem behaviors at age 4.5: evidence from Growing Up in New Zealand. Journal of Abnormal Child Psychology. 47(8):1277–1288. [DOI] [PubMed] [Google Scholar]