Abstract
Craniopharyngiomas are tumors of the central nervous system, typically located in the sellar/parasellar region. Despite being benign, they behave aggressively due to their propensity to invade nearby important structures, making total resection challenging. Distant spread of craniopharyngioma is a rare but significant complication. Most cases result from spread along the surgical path, while others result from dissemination along the cerebrospinal fluid (CSF) pathways.
We report a case of a parasellar adamantinomatous craniopharyngioma with progressive visual loss. The patient was operated on through a right pterional craniotomy three times due to recurrence. After the last surgery, fractionated stereotactic radiotherapy was performed on the tumor residue. On follow-up brain MRI, a new extra-axial lesion was found in the left frontal region with solid and cystic components, with apparent dural implantation. Left frontal craniotomy was performed, and the lesion was excised with resection of its dural implant. Histological findings revealed it to be adamantinomatous craniopharyngioma, grade 1, according to the World Health Organization (WHO).
Despite being rare, craniopharyngioma ectopic recurrence is a possible surgical complication. Despite the poorly understood mechanism, the literature highlights the importance of paying attention to tumor spillage during surgery to prevent distant recurrences.
Keywords: adamantinomatous craniopharyngioma, craniopharyngioma, ectopic craniopharyngioma, ectopic recurrence, neoplasm metastasis, neoplasm seeding
Introduction
Craniopharyngiomas are benign (World Health Organization (WHO) grade 1) epithelial tumors arising from embryologic squamous remnants of the craniopharyngeal duct or Rathke's pouch. They represent 0.8% of all brain tumors, with an incidence of 0.19 per 100,000 [1]. They have a bimodal age distribution, with a childhood peak age between five and 15 and an adult peak age between 45 and 60 [2].
There are two histologic types: adamantinomatous and papillary. Although both tumors arise in the same region and display squamous lineage, recent consensus is that they are distinct tumors with differing epidemiology, radiology, histology, and molecular genetics [3]. Adamantinomatous craniopharyngiomas are usually lobulated and cystic sellar and suprasellar lesions. Calcification, ossification, fibrosis, and cholesterol deposits are frequently present. On the other hand, papillary craniopharyngiomas are less often cystic and rarely have calcifications [4]. They often demonstrate local brain invasion and may adhere to adjacent vessels and nerves, making it extremely hard to achieve a total resection with recurrence rates as high as 57% [5].
Common presentations include visual disturbances and endocrine dysfunction. Cognitive impairment, personality change, and symptoms of elevated intracranial pressure have also been described.
The treatment of craniopharyngiomas typically involves surgical resection, sometimes accompanied by radiation therapy. There is ongoing debate about whether to opt for complete surgical resection alone or to combine a more limited resection with radiation therapy. While local recurrence is frequently seen after surgical resection, ectopic recurrence is rare and scarcely reported in the literature. Two mechanisms of spread have been described: seeding along the surgical tract or through the cerebrospinal fluid (CSF) [6].
In this article, we report on a 77-year-old male with ectopic recurrent craniopharyngioma and a review of the literature.
Case presentation
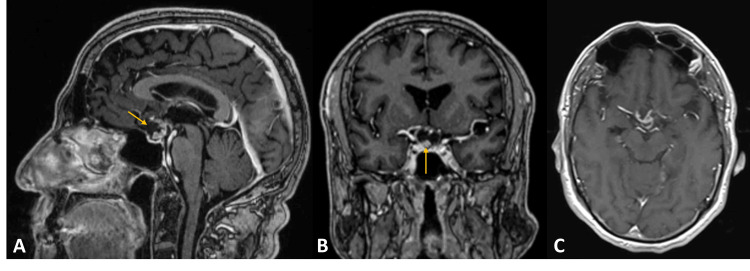
A 77-year-old male with complaints of progressive visual loss, diagnosed with bitemporal hemianopsia, was studied with a brain MRI. A sellar and suprasellar extra-axial lesion with 15.5×12 mm was identified, compressing the optic chiasma. It had mixed solid and cystic components. The solid component and the cystic wall enhanced heterogeneous with contrast (Figure 1).
Figure 1. Preoperative MRI .
Sellar/parasellar extra-axial lesion with solid and cystic components. Contrast enhancement of the solid element and cystic wall. Gadolinium-enhanced T1-weighted images: (A) sagittal, (B) coronal, and (C) axial. Yellow arrows indicating the lesion.
The patient underwent a right pterional approach and a gross total lesion resection. His vision improved after surgery. The histologic examination revealed epithelial tissue with sizeable cystic component, squamous epithelial trabeculae, basaloid cells, stellate reticulum, and nodules of wet keratin compatible with adamantinomatous craniopharyngioma, grade 1 (WHO 2021).
Three years later, and with a new bilateral visual deficit with an almost amaurotic right eye, he was investigated with a new MRI, which revealed a significant tumor recurrence. The pterional craniotomy was performed again, and the lesion was partially resected, decompressing the optic chiasm and the optic nerves. Despite that, the vision in his right eye did not improve.
One year later, he started to lose vision in his left eye. A new tumoral recurrence was diagnosed, and he underwent a third surgery through the previous right pterional craniotomy, resulting in new partial resection and decompression of the left optic nerve and optic chiasma, sparing the remaining vision of his left eye. After, he underwent radiotherapy for the suprasellar residual lesion.
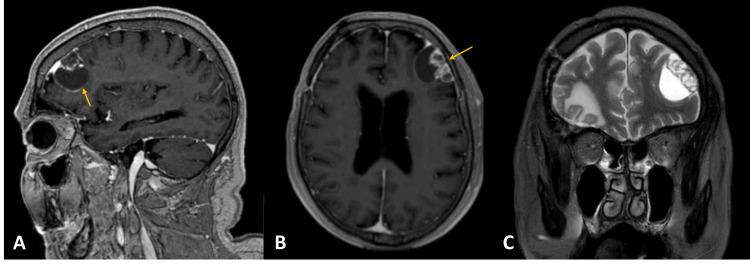
However, eight months after the last surgery, a routine brain MRI demonstrated a new multicystic left frontal lesion, apparently extra-axial (Figure 2).
Figure 2. Cranial MRI showing ectopic recurrence.
Left frontal lobe extra-axial lesion with a solid and cystic component, with heterogeneous contrast enhancement. (A) Gadolinium-enhanced sagittal T1-weighted image; (B) gadolinium-enhanced axial T1-weighted image; (C) T2-weighted coronal image. Yellow arrow indicating the lesion.
A left frontal craniotomy was made, and the extra-axial lesion was fully resected. Intraoperatively, the dura was involved by the lesion, which was also excised. The pathological staining confirmed adamantinomatous craniopharyngioma (Figure 3).
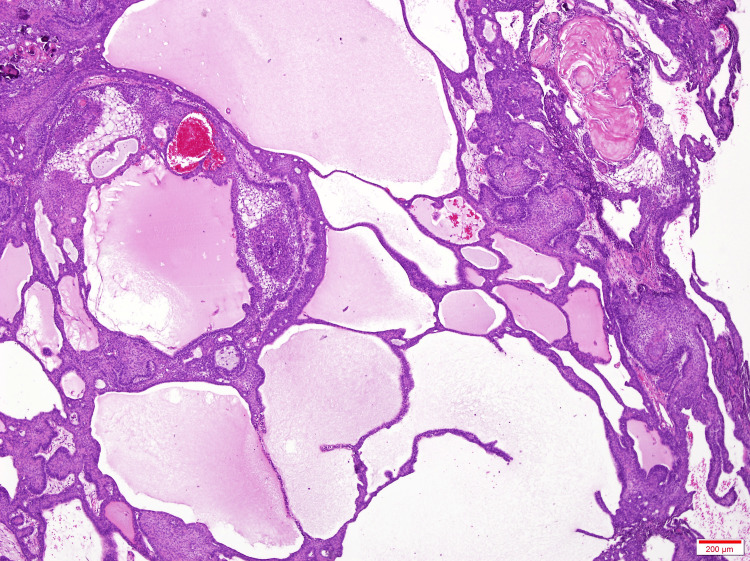
Figure 3. Histopathological results showing adamantinomatous craniopharyngioma.
H&E at 40×. Mixture of solid and cystic areas, with the cysts filled with a proteinaceous material that stains pink with H&E.
H&E: hematoxylin and eosin
The patient had no new deficits following surgery. A cerebral MRI conducted six months post-surgery showed no evidence of recurrence of the metastatic lesion and stability of the sellar craniopharyngioma.
Discussion
Ectopic or metastatic recurrent craniopharyngioma is extremely rare. Up to date, only 66 patients with 68 cases have been described, including ours (Table 1) [5-55].
Table 1. Review of cases of ectopic recurrent craniopharyngioma .
NM: not mentioned; STR: subtotal resection; GTR: gross total resection; PR: partial resection, gamma knife; M: male; F: female; RT: radiotherapy; CPA: cerebellopontine angle
| Author, year | Age (years), gender | Histology | Previous treatments | Ectopic recurrence location | Ectopic recurrence mechanism | Interval between the first surgery and ectopic recurrence (years) |
| Present | 77, M | ACP | Cranio GTR (first); cranio STR (second); cranio STR+RT (third) | Left frontal lobe | CSF | 4 |
| Carfagno et al. (2023) [7] | 17, M | NM | Cranio GTR | Right ventricle | CSF | 10 |
| Steed et al. (2023) [8] | 10, F | ACP | Cranio STR+RT (first); cranio STR (second) | Dorsal (T1) | CSF | 3.5 |
| Selfa et al. (2023) [9] | 7, M | ACP | Cranio STR (first); cranio STR+RT (second) | CPA | CSF | 20 |
| 36, M | ACP | Cranio GTR | Cerebellum | CSF | 18 | |
| Ji et al. (2023) [10] | 63, F | ACP | Cranio STR (first); TSS STR (second) | Right temporal lobe | CSF | 3 |
| 49, F | ACP | Right | Right frontal lobe | Surgical approach | 7 (first); 16 (second) | |
| Cai et al. (2019) [5] | 28, M | ACP | Cranio GTR | Right temporal lobe | CSF | 1 |
| Renfrow et al. (2018) [11] | 14, F | ACP | Cranio GTR (first); cranio GTR (second); RT (third) | Left lateral ventricle | CSF | 12 |
| Mahdi et al. (2018) [12] | 24, M | ACP | Cranio GTR | Right CPA | CSF | 1 |
| Jian et al. (2017) [13] | 42, M | PCP | Cranio GTR | Right frontal lobe | CSF | 0.3 |
| Carleton-Bland et al. (2017) [14] | 10, M | ACP | Cranio STR (first); cranio STR+RT (second) | Right lateral ventricle | CSF | 2 |
| Du et al. (2016) [15] | 6, F | ACP | Cranio GTR | Right frontal lobe | Surgical approach | 5 |
| 4, M | ACP | Cranio GTR | Fourth ventricle | CSF | 4 | |
| Clark et al. (2015) [16] | 33, F | ACP | Cranio GTR (first); cranio GTR (second) | Left Sylvian fissure | Surgical approach | 34 |
| Yang et al. (2015) [17] | 35, M | NM | Cranio GTR | Right frontal lobe | Surgical approach | 9 |
| 46, M | PCP | Cranio GTR | Interhemispheric | Surgical approach | 2 | |
| 42, M | ACP | Cranio GTR (first); cranio GTR (second) | Right frontal lobe | Surgical approach | 6 | |
| Gonçalves et al. (2014) [18] | 49, M | ACP | Cranio GTR | Right frontal lobe | Surgical approach | 5 |
| Jakobs and Orakcioglu (2012) [19] | 61, F | ACP | Cranio GTR (first); RT (second) | Right frontal bone | Surgical approach | 11 |
| Elfving et al. (2011) [20] | 4, F | ACP | Cranio GTR (first); cranio STR+RT (second) | Right frontal lobe | Surgical approach | 11 |
| Salunke et al. (2011) [21] | 5, F | NM | Cranio STR | Right Sylvian fissure | Surgical approach | 0.92 |
| de Blank and Minturn (2011) [22] | 5, F | NM | Cranio GTR (first); RT (second) | Left CPA | Surgical approach | 17 |
| Kordes et al. (2011) [23] | 7, M | ACP | Cranio PR+TSS+RT | Right parietal lobe | Surgical approach | 1.25 |
| Wang et al. (2010) [24] | 3, M | ACP | Cranio GTR+RT | Right frontal lobe | Surgical approach | 2 |
| Lermen et al. (2010) [25] | 45, M | ACP | Cranio STR (first); cranio GTR (second) | Lumbar space | CSF | 0.5 |
| Schmalisch et al. (2010) [26] | 11, M | ACP | Cranio GTR | Right Sylvian fissure | Surgical approach | 2 |
| 23, F | ACP | Cranio STR (first); TSS (second) | Right frontal lobe | Surgical approach | 4 | |
| 32, M | ACP | Cranio GTR | Right parietal lobe | CSF | 10 | |
| Romani et al. (2010) [27] | 18, F | ACP | Cranio GTR | Interhemispheric | Surgical approach | 4 |
| Frangou et al. (2009) [6] | 10, M | ACP | Cranio STR (first); cranio STR (second); cranio STR+RT (third) | Right parietal lobe | CSF | 4 |
| Elliott et al. (2009) [28] | 3, F | ACP | Cranio GTR | Prepontine cistern | CSF | 10 |
| 2, M | ACP | Cranio STR (first); cranio GTR (second); cranio GTR (third) | Left CPA | CSF | 3.5 | |
| 3, F | ACP | Cranio GTR | Right Sylvian fissure | Surgical approach | 1.67 | |
| 6, M | ACP | Cranio STR (first); cranio GTR (second) | Left frontal lobe | CSF | 7.08 | |
| Bikmaz et al. (2009) [29] | 37, F | NM | NM | Prepontine | CSF | 15 |
| 32, M | NM | GTR | Right frontal lobe | Surgical approach | 9 | |
| 12, M | NM | STR+RT | CPA | CSF | 12 | |
| Novák et al. (2008) [30] | 48, M | NM | NM | Posterior fossa | CSF | 19 |
| Jeong et al. (2006) [31] | 8, F | ACP | Cranio GTR | Right frontal lobe | Surgical approach | 4 |
| Yamada et al. (2006) [32] | 17, F | ACP | Cranio STR+RT | Left frontal lobe | CSF | 5 |
| Bianco et al. (2006) [33] | 27, F | ACP | Cranio STR (first); cranio GTR (second) | Left temporal lobe cortex | Surgical approach | 10 |
| Kawaguchi et al. (2005) [34] | 50, F | NM | NM (first); cranio GTR (second) | Left frontal lobe | Surgical approach | 2 |
| Ishii et al. (2004) [35] | 2, M | NM | Cranio STR (first); cranio GTR (second) | Right frontal lobe | Surgical approach | 0.17 |
| Liu et al. (2002) [36] | 65, F | NM | Cranio GTR | Right frontal lobe | Surgical approach | 3 |
| Nomura et al. (2002) [37] | 17, F | ACP | Cranio STR (first); cranio STR+RT (second) | Right frontal and temporal lobe | CSF | 3.92 |
| Fuentes et al. (2002) [38] | 32, M | ACP | GTR | Right frontal lobe | Surgical approach | 5 |
| 11, M | ACP | GTR | NM | Surgical approach | 3 | |
| 9, M | ACP | GTR | Right frontal lobe; right temporal lobe | Surgical approach | 10 | |
| Elmaci et al. (2002) [39] | 62, F | PCP | Cranio GTR | Left temporal lobe | CSF | 2 |
| Novegno et al. (2002) [40] | 6, M | ACP | Cranio GTR | First left frontal lobe; second left pontine R cerebral basal | 1st surgical approach; 2nd CSF | 3 (first); 4 (second) |
| Lee et al. (2001) [41] | 26, M | PCP | Cranio STR+GK | Lumbar space | CSF | 1.58 |
| Ito et al. (2001) [42] | 62, M | ACP | Cranio GTR | Right frontal lobe | CSF | 3 |
| Freitag et al. (2001) [43] | 61, F | NM | NM | Right frontal lobe | Surgical approach | 5 |
| Kim et al. (2001) [44] | Child, NM | NM | NM | Internal auditory canal | CSF | NM |
| Gupta et al. (1999) [45] | 73, M | ACP | Cranio GTR | Left parietal lobe and left frontal lobe | CSF | 7 |
| Lee et al. (1999) [46] | 31, M | NM | Cranio GTR | Right frontal lobe | Surgical approach | 5 |
| Israel and Pomeranz (1995) [47] | 12, M | NM | Cranio GTR | Right frontal lobe | Surgical approach | 2 |
| Keohane et al. (1994) [48] | 7, F | NM | Cranio STR+RT | Left CPA | CSF | 26 |
| Tomita and McLone (1993) [49] | Child, NM | NM | NM | Right frontal lobe | Surgical approach | NM |
| Malik et al. (1992) [50] | 6, M | ACP | Cranio PR+RT (first); 2nd cranio PR (second); cranio GTR (third) | Right frontal lobe | Surgical approach | 21 |
| Tomita et al. (1992) [51] | 23, F | NM | Cranio PR (first); RT (second) | Right CPA, interpeduncle, prepontine | CSF | 25 |
| Gökalp et al. (1991) [52] | 3, M | NM | Cranio GTR | Fourth ventricle | CSF | 20 |
| Ragoowansi and Piepgras (1991) [53] | 47, M | NM | Stereotactic biopsy (first); cranio GTR (second) | Right Sylvian fissure | Surgical approach | 1 |
| Barloon et al. (1988) [54] | 5, M | NM | Cranio STR RT (first); cyst aspiration+RT | Right frontal lobe | Surgical approach | 5 |
| Baba et al. (1978) [55] | 7, F | NM | Cranio STR | Prepontine C3 | CSF | 7 |
The literature describes two mechanisms of spread: seeding along the surgical tract, which is attributed to iatrogenic contamination of brain tissue with tumor cells during the process of removing parts of the tumor, and dissemination via CSF with metastasis that have no relationship with the surgical tract [5,6,25].
The majority of cases (35) were related to the surgical tract, and 33 were due to seeding through the CSF pathway. The most common site of ectopic recurrence is, by far, the frontal lobe (29 cases). This may be due to transcranial surgery for craniopharyngioma via the pterional approach being the most frequently used, with local cell dissemination during operation.
Despite our case being also a frontal ectopic craniopharyngioma, the proposed dissemination mechanism was most probably due to dissemination by CSF because it is on the contralateral side of the approach. Other locations (temporal, parietal cerebellopontine angle, etc.) were also associated with CSF dissemination. The lumbar spine was the most faraway location reported [10,15]. Most of these lesions were extra-axial. These suggest that the meninges may serve as a base for the implantation of craniopharyngioma cells. Also, as demonstrated in some cases, marked bony erosion may be seen [6].
Craniopharyngiomas have a bimodal age distribution. Thirty-four cases were found in children and 32 cases in adults. This distribution suggests that ectopic recurrences don't seem to be confined to a particular age group. The mean age in children was 7.44 (±4.14) and in adults 43.69 (±14.54). Our case, at 77 years old (81 at ectopic diagnosis), is the oldest reported. Male gender was more frequent, with 37 cases reported vs. 26 on women; in other cases, gender was not reported. This suggests potential gender-related factors in the occurrence of ectopic craniopharyngioma.
Only four metastatic craniopharyngiomas were papillary, which is no surprise since it is the less frequent type. Also, the papillary type usually has a more indolent course with lower recurrence rates after total resection [14]. In 21 cases, the pathology was unclear, especially in older reports.
Gross total resection does not seem to prevent metastatic disease. It may even be associated with more recurrence since more aggressive surgery and longer operative time allow more tumor tissue to be manipulated and exposed to either the surgical tract or CSF pathways [16]. This highlights the need for protection of the surgical field, cyst aspiration before lesional excision, careful manipulation of the tumor during surgery, and extensive irrigation with saline throughout the surgery to prevent contamination with tumor cells [33,42].
Postoperative radiotherapy remains controversial as a treatment option for craniopharyngiomas [3]. It is usually indicated in cases where total gross resection is not possible. As in this case report, another 18 patients received postoperative adjuvant radiotherapy and still had ectopic recurrence. It seems that radiotherapy is not protective against ectopic recurrence.
Conclusions
The treatment and recurrence of craniopharyngiomas present significant challenges. While surgical resection, sometimes combined with radiation therapy, remains the primary treatment approach, there is ongoing debate about the best strategy to minimize recurrence.
Local recurrence is common, but ectopic recurrence is rare and can occur through seeding along the surgical tract or dissemination via CSF. The frontal lobe is the most frequent site of ectopic recurrence, likely due to the common use of the pterional approach in surgery.
Ectopic recurrences are not confined to a specific age group, though they appear more frequently in males.
Despite aggressive surgical techniques and the use of postoperative radiotherapy, ectopic recurrences still occur, highlighting the need for meticulous surgical practices and further research into effective preventive measures.
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: João Nogueira, Miguel Afonso Filipe
Acquisition, analysis, or interpretation of data: João Nogueira, Cristiano Antunes, Joana Sobreiro Silva, Miguel Afonso Filipe, Renato Pereira, Renata Marques
Drafting of the manuscript: João Nogueira
Critical review of the manuscript for important intellectual content: João Nogueira, Cristiano Antunes, Joana Sobreiro Silva, Miguel Afonso Filipe, Renato Pereira, Renata Marques
References
- 1.CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2015-2019. Ostrom QT, Price M, Neff C, Cioffi G, Waite KA, Kruchko C, Barnholtz-Sloan JS. Neuro Oncol. 2022;24:0–95. doi: 10.1093/neuonc/noac202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The 2021 WHO classification of tumors of the central nervous system: a summary. Louis DN, Perry A, Wesseling P, et al. Neuro Oncol. 2021;23:1231–1251. doi: 10.1093/neuonc/noab106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Craniopharyngioma. Müller HL, Merchant TE, Warmuth-Metz M, Martinez-Barbera JP, Puget S. Nat Rev Dis Primers. 2019;5:75. doi: 10.1038/s41572-019-0125-9. [DOI] [PubMed] [Google Scholar]
- 4.Magnetic resonance imaging of craniopharyngioma. Johnson LN, Hepler RS, Yee RD, Frazee JG, Simons KB. Am J Ophthalmol. 1986;102:242–244. doi: 10.1016/0002-9394(86)90152-2. [DOI] [PubMed] [Google Scholar]
- 5.An ectopic recurrent craniopharyngioma of the temporal lobe: case report and review of the literature. Cai M, He H, Zhang B, et al. World Neurosurg. 2019;126:216–222. doi: 10.1016/j.wneu.2019.02.196. [DOI] [PubMed] [Google Scholar]
- 6.Metastatic craniopharyngioma: case report and literature review. Frangou EM, Tynan JR, Robinson CA, Ogieglo LM, Vitali AM. Childs Nerv Syst. 2009;25:1143–1147. doi: 10.1007/s00381-009-0917-4. [DOI] [PubMed] [Google Scholar]
- 7.Ectopic recurrence of a craniopharyngioma. Carfagno VF, Rouintan J, Ahmed I. Cureus. 2023;15:0. doi: 10.7759/cureus.35988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Spinal ectopic recurrence of craniopharyngioma in a pediatric patient. Steed T, Indelicato DJ, Souster J, van Landeghem FK, Mehta V, Patel S. Childs Nerv Syst. 2023;39:279–284. doi: 10.1007/s00381-022-05604-6. [DOI] [PubMed] [Google Scholar]
- 9.Ectopic recurrence of craniopharyngioma in the posterior fossa: case report and review of the literature. Selfa A, Arráez C, Ros Á, Linares J, Cerro L, Arráez MÁ. Neurocirugia (Astur: Engl Ed) 2023;34:32–39. doi: 10.1016/j.neucie.2022.11.001. [DOI] [PubMed] [Google Scholar]
- 10.Ectopic recurrence craniopharyngioma: series report and literature review. Ji C, Cheng H, Zhou X, et al. Chin Neurosurg J. 2023;9:13. doi: 10.1186/s41016-023-00326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Intraventricular recurrence of a craniopharyngioma: case report. Renfrow JJ, Greeneway GP, Carter L, Couture DE. J Neurosurg Pediatr. 2018;22:393–396. doi: 10.3171/2018.4.PEDS18112. [DOI] [PubMed] [Google Scholar]
- 12.Early ectopic recurrence of craniopharyngioma in the cerebellopontine angle. Mahdi MA, Krauss JK, Nakamura M, Brandis A, Hong B. Turk Neurosurg. 2018;28:313–316. doi: 10.5137/1019-5149.JTN.17215-16.1. [DOI] [PubMed] [Google Scholar]
- 13.Craniopharyngioma: a case report of ectopic recurrence. Jian XD, Shrestha D, Zhuang Z. Turk Neurosurg. 2017;27:160–162. doi: 10.5137/1019-5149.JTN.12386-14.2. [DOI] [PubMed] [Google Scholar]
- 14.Ventricular metastatic dissemination of a paediatric craniopharyngioma: case report and literature review. Carleton-Bland N, Kilday JP, Pathmanaban ON, Stivaros S, Kelsey A, Kamaly-Asl ID. Br J Neurosurg. 2017;31:474–477. doi: 10.3109/02688697.2016.1139050. [DOI] [PubMed] [Google Scholar]
- 15.Ectopic recurrence of pediatric craniopharyngiomas after gross total resection: a report of two cases and a review of the literature. Du C, Feng CY, Yuan J, Yuan X. Childs Nerv Syst. 2016;32:1523–1529. doi: 10.1007/s00381-016-3050-1. [DOI] [PubMed] [Google Scholar]
- 16.Recurrent ectopic craniopharyngioma in the Sylvian fissure thirty years after resection through a pterional approach: a case report and review of the literature. Clark SW, Kenning TJ, Evans JJ. https://pubmed.ncbi.nlm.nih.gov/25797995/ Nagoya J Med Sci. 2015;77:297–306. [PMC free article] [PubMed] [Google Scholar]
- 17.Ectopic recurrence of craniopharyngioma: reporting three new cases. Yang Y, Shrestha D, Shi XE, Zhou Z, Qi X, Qian H. Br J Neurosurg. 2015;29:295–297. doi: 10.3109/02688697.2014.967751. [DOI] [PubMed] [Google Scholar]
- 18.Subgaleal recurrence of craniopharyngioma of rapid growing pattern. Gonçalves CB, Lima GA, Nogueira J, do Souto AA, Chimelli L, Taboada GF. Pituitary. 2014;17:214–219. doi: 10.1007/s11102-013-0490-4. [DOI] [PubMed] [Google Scholar]
- 19.Ectopic recurrent craniopharyngioma of the frontal bone. Jakobs M, Orakcioglu B. J Neurosurg. 2012;117:490–497. doi: 10.3171/2012.6.JNS111885. [DOI] [PubMed] [Google Scholar]
- 20.Ectopic recurrence of a craniopharyngioma in a 15-year-old girl 9 years after surgery and conventional radiotherapy: case report. Elfving M, Lundgren J, Englund E, Strömblad LG, Erfurth EM. Childs Nerv Syst. 2011;27:845–851. doi: 10.1007/s00381-010-1375-8. [DOI] [PubMed] [Google Scholar]
- 21.Ectopic recurrence of craniopharyngioma along the surgical tract. Salunke P, Bhardwaj LK, Gupta K, Das K. Neurol India. 2011;59:137–139. doi: 10.4103/0028-3886.76881. [DOI] [PubMed] [Google Scholar]
- 22.A rare case of ectopic recurrence of a craniopharyngioma diagnosed 17 years after initial presentation. de Blank PM, Minturn JE. J Pediatr Hematol Oncol. 2011;33:392–397. doi: 10.1097/MPH.0b013e31820acfb2. [DOI] [PubMed] [Google Scholar]
- 23.Ectopic craniopharyngioma. Kordes U, Flitsch J, Hagel C, et al. Klin Padiatr. 2011;223:176–177. doi: 10.1055/s-0031-1273743. [DOI] [PubMed] [Google Scholar]
- 24.Post-operative implantation metastasis of craniopharyngioma: a case report. Wang XY, Xu SJ, Li XG. J Int Med Res. 2010;38:1876–1882. doi: 10.1177/147323001003800536. [DOI] [PubMed] [Google Scholar]
- 25.Postoperative spinal recurrence of craniopharyngioma. Lermen O, Frank S, Hassler W. Acta Neurochir (Wien) 2010;152:309–311. doi: 10.1007/s00701-009-0537-5. [DOI] [PubMed] [Google Scholar]
- 26.Postoperative intracranial seeding of craniopharyngiomas--report of three cases and review of the literature. Schmalisch K, Beschorner R, Psaras T, Honegger J. Acta Neurochir (Wien) 2010;152:313–319. doi: 10.1007/s00701-009-0538-4. [DOI] [PubMed] [Google Scholar]
- 27.Ectopic recurrence of craniopharyngioma along the surgical route: case report and literature review. Romani R, Niemelä M, Celik O, Isarakul P, Paetau A, Hernesniemi J. Acta Neurochir (Wien) 2010;152:297–302. doi: 10.1007/s00701-009-0415-1. [DOI] [PubMed] [Google Scholar]
- 28.Surgical treatment of ectopic recurrence of craniopharyngioma. Report of 4 cases. Elliott RE, Moshel YA, Wisoff JH. J Neurosurg Pediatr. 2009;4:105–112. doi: 10.3171/2009.3.PEDS0948. [DOI] [PubMed] [Google Scholar]
- 29.Ectopic recurrence of craniopharyngiomas: case report. Bikmaz K, Guerrero CA, Dammers R, Krisht AF, Husain MM. Neurosurgery. 2009;64:0–3. doi: 10.1227/01.NEU.0000337078.60998.98. [DOI] [PubMed] [Google Scholar]
- 30.Minimally invasive treatment of posterior fossa craniopharyngioma by means of navigated endoscopy. Novák Z, Chrastina J, Feitová V, Lzicarová E, Ríha I. Minim Invasive Neurosurg. 2008;51:165–168. doi: 10.1055/s-2008-1062743. [DOI] [PubMed] [Google Scholar]
- 31.Ectopic recurrence of craniopharyngioma: a case report and review of the literature. Jeong IH, Lee JK, Moon KS, et al. J Neurooncol. 2006;79:191–195. doi: 10.1007/s11060-006-9124-2. [DOI] [PubMed] [Google Scholar]
- 32.Ectopic recurrence of craniopharyngioma. Yamada Y, Haraoka J, Akimoto J. Neurol Med Chir (Tokyo) 2006;46:598–600. doi: 10.2176/nmc.46.598. [DOI] [PubMed] [Google Scholar]
- 33.Cortical seeding of a craniopharyngioma after craniotomy: case report. Bianco AM, Madeira LV, Rosemberg S, Shibata MK. Surg Neurol. 2006;66:437–440. doi: 10.1016/j.surneu.2005.12.027. [DOI] [PubMed] [Google Scholar]
- 34.Ectopic recurrence of craniopharyngioma. Kawaguchi T, Fujimura M, Shirane R, Shoji T, Watanabe M, Tominaga T. J Clin Neurosci. 2005;12:307–309. doi: 10.1016/j.jocn.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 35.Intracranial ectopic recurrence of craniopharyngioma after Ommaya reservoir implantation. Ishii K, Sugita K, Kobayashi H, Kamida T, Fujiki M, Izumi T, Mori T. Pediatr Neurosurg. 2004;40:230–233. doi: 10.1159/000082297. [DOI] [PubMed] [Google Scholar]
- 36.Ectopic recurrence of craniopharyngioma after an interhemispheric transcallosal approach: case report. Liu JM, Garonzik IM, Eberhart CG, Sampath P, Brem H. Neurosurgery. 2002;50:639–644. doi: 10.1097/00006123-200203000-00041. [DOI] [PubMed] [Google Scholar]
- 37.Multiple intracranial seeding of craniopharyngioma after repeated surgery--case report. Nomura H, Kurimoto M, Nagai S, Hayashi N, Hirashima Y, Tsukamoto E, Endo S. Neurol Med Chir (Tokyo) 2002;42:268–271. doi: 10.2176/nmc.42.268. [DOI] [PubMed] [Google Scholar]
- 38.Postoperative intracranial seeding of craniopharyngioma. Three case reports and a review of the literature [Article in French] Fuentes S, Metellus P, Dufour H, Do L, Grisoli F. https://pubmed.ncbi.nlm.nih.gov/12407320/ Neurochirurgie. 2002;48:345–350. [PubMed] [Google Scholar]
- 39.Metastatic papillary craniopharyngioma: case study and study of tumor angiogenesis. Elmaci L, Kurtkaya-Yapicier O, Ekinci G, et al. Neuro Oncol. 2002;4:123–128. doi: 10.1093/neuonc/4.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ectopic recurrences of craniopharyngioma. Novegno F, Di Rocco F, Colosimo C Jr, Lauriola L, Caldarelli M. Childs Nerv Syst. 2002;18:468–473. doi: 10.1007/s00381-002-0641-9. [DOI] [PubMed] [Google Scholar]
- 41.Postoperative spinal seeding of craniopharyngioma. Case report. Lee DK, Jung HW, Kim DG, Paek SH, Gwak HS, Choe G. J Neurosurg. 2001;94:617–620. doi: 10.3171/jns.2001.94.4.0617. [DOI] [PubMed] [Google Scholar]
- 42.Does craniopharyngioma metastasize? Case report and review of the literature. Ito M, Jamshidi J, Yamanaka K. Neurosurgery. 2001;48:933–935. doi: 10.1097/00006123-200104000-00050. [DOI] [PubMed] [Google Scholar]
- 43.Recurrent ectopic craniopharyngioma. Freitag SK, Miller NR, Brem H. Br J Neurosurg. 2001;15:511–513. doi: 10.1080/02688690120097723. [DOI] [PubMed] [Google Scholar]
- 44.Radical excision of pediatric craniopharyngioma: recurrence pattern and prognostic factors. Kim SK, Wang KC, Shin SH, Choe G, Chi JG, Cho BK. Childs Nerv Syst. 2001;17:531–536. doi: 10.1007/s003810100458. [DOI] [PubMed] [Google Scholar]
- 45.Metastatic craniopharyngioma. Gupta K, Kuhn MJ, Shevlin DW, Wacaser LE. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7056229/ AJNR Am J Neuroradiol. 1999;20:1059–1060. [PMC free article] [PubMed] [Google Scholar]
- 46.Postoperative ectopic seeding of craniopharyngioma. Case illustration. Lee JH, Kim CY, Kim DG, Jung HW. J Neurosurg. 1999;90:796. doi: 10.3171/jns.1999.90.4.0796. [DOI] [PubMed] [Google Scholar]
- 47.Intracranial craniopharyngioma seeding following radical resection. Israel ZH, Pomeranz S. Pediatr Neurosurg. 1995;22:210–213. doi: 10.1159/000120903. [DOI] [PubMed] [Google Scholar]
- 48.Late recurrence of craniopharyngioma in the cerebellopontine angle in a fertile woman. Keohane C, Hally M, Ryder DQ, Buckley TF. J Neurol Neurosurg Psychiatry. 1994;57:873–874. doi: 10.1136/jnnp.57.7.873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Radical resections of childhood craniopharyngiomas. Tomita T, McLone DG. Pediatr Neurosurg. 1993;19:6–14. doi: 10.1159/000120693. [DOI] [PubMed] [Google Scholar]
- 50.Remote recurrence of craniopharyngioma in the epidural space. Case report. Malik JM, Cosgrove GR, VandenBerg SR. J Neurosurg. 1992;77:804–807. doi: 10.3171/jns.1992.77.5.0804. [DOI] [PubMed] [Google Scholar]
- 51.Recurrent craniopharyngioma in the posterior fossa. Tomita S, Mendoza ND, Symon L. Br J Neurosurg. 1992;6:587–590. doi: 10.3109/02688699209002377. [DOI] [PubMed] [Google Scholar]
- 52.Craniopharyngioma of the posterior fossa. Gökalp HZ, Egemen N, Ildan F, Bacaci K. Neurosurgery. 1991;29:446–448. doi: 10.1097/00006123-199109000-00020. [DOI] [PubMed] [Google Scholar]
- 53.Postoperative ectopic craniopharyngioma. Case report. Ragoowansi AT, Piepgras DG. J Neurosurg. 1991;74:653–655. doi: 10.3171/jns.1991.74.4.0653. [DOI] [PubMed] [Google Scholar]
- 54.Frontal lobe implantation of craniopharyngioma by repeated needle aspirations. Barloon TJ, Yuh WT, Sato Y, Sickels WJ. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8334225/ AJNR Am J Neuroradiol. 1988;9:406–407. [PMC free article] [PubMed] [Google Scholar]
- 55.Cystic craniopharyngioma extending down into the upper cervical spinal canal (author's transl) [Article in Japanese] Baba M, Iwayama S, Jimbo M, Kitamura K. https://pubmed.ncbi.nlm.nih.gov/683451/ No Shinkei Geka. 1978;6:687–693. [PubMed] [Google Scholar]