Abstract
Background:
Migraine affects ~14–15% of the global population, contributing to nearly 5% of the world’s health burden. When drug treatments prove ineffective for intractable migraines, highly specific surgical interventions emerge as potential solutions. The authors aimed to analyze surgical approaches for these refractory or intractable migraines through a systematic review and meta-analysis.
Methods:
The authors conducted a literature search across databases such as PubMed, Scopus, Web of Science, and Embase, focusing on studies related to migraines and surgical outcomes. The authors considered clinical trials or observational studies that included any surgical intervention for refractory or intractable migraines, emphasizing key outcomes such as reductions in migraine intensity, Migraine Disability Assessment scores (MIDAS), and 50% Migraine Headache Index (MHI) reduction rates. Statistical analyses were performed using R version 4.3.
Results:
Eleven studies were included in the systematic review. A meta-analysis of four studies involving overall 95 patients showed a significant reduction in mean migraine intensity scores using ONS (−2.27, 95% CI: −3.92 to −0.63, P=0.021). Three studies with 85 patients showed an average MIDAS score reduction of −52.3, though this was not statistically significant (95% CI: −136.85 to 32.19, P=0.116). Two additional studies corroborated these reductions in MIDAS scores. Nerve decompression surgery showed a substantial decrease in the average migraine intensity (from 8.31 down to 4.06). Median MIDAS score dropped from 57 to 20. Two studies indicated a success rate of 40 and 82%, respectively, in achieving a 50% reduction in the migraine MHI through nerve decompression. Findings from two studies suggest that septorhinoplasty and sinus surgery effectively decrease migraine intensity scores.
Conclusion:
The existing evidence emphasizes the potential advantages of surgical interventions as a promising approach to managing intractable or refractory migraines. However, robust and comprehensive research is crucial to refine and solidify the efficacy of these surgical methods, aiming for widespread benefits for patients, considering cost-effectiveness factors.
Keywords: intractable, migraine, nerve decompression, occipital nerve stimulation, surgery
Introduction
Highlights
Surgical approaches, notably ONS, significantly reduced migraine intensity.
Observed reductions in MIDAS scores were notable but not statistically significant.
Nerve decompression yielded substantial decreases in migraine intensity and had varying success rates in reducing migraine MHI.
Both septorhinoplasty and sinus surgery were effective in mitigating migraine intensity.
The findings emphasize the potential of surgical interventions for intractable migraines, highlighting the need for further refinement and research.
A migraine is an episodic headache with specific traits like heightened sensitivity to light, sound, or motion. Moreover, it can appear as a recurring headache syndrome linked with a range of neurological symptoms1. This includes associated conditions like cyclic vomiting, somnambulism, abdominal migraine, benign paroxysmal torticollis, benign paroxysmal vertigo, and confusional migraine. These various syndromes have distinct clinical features, durations, and prevalence rates2. The nature of migraine follows a cyclic pattern involving multiple phases: the premonitory phase, fleeting neurological symptoms referred to as migraine aura, an intense headache episode, and the postdrome phase3. Beyond its physical toll, migraine substantially burdens different aspects of an individual’s life, encompassing financial status, family relationships, and participation in work or studies4. At present, the prevalence of migraine stands at ~14–15%. This condition contributes to around 4.9% of the overall burden of health issues experienced by the global population, as measured in years lived with disability (YLDs)5. Migraines can be categorized into two distinct groups: resistant migraines, characterized by a lack of response to at least three different classes of migraine preventatives, accompanied by a minimum of eight incapacitating headache days each month for a continuous period of 3 months without any improvement; and refractory migraines, where all available preventative treatments have proven ineffective, and individuals experience a minimum of eight debilitating headache days per month for a continuous duration of 6 months6. Ordinary migraine episodes can often be alleviated with interventions like triptan medications and pain relievers. However, in the case of intractable migraines, these treatments may not yield favorable responses.
For individuals who have not experienced positive outcomes from alternative treatments, surgical intervention becomes a viable option for addressing intractable migraines7. The peripheral theory of migraines finds support in the pain relief experienced by many patients through treatments like Botulinum toxins or local nerve blocks7. Surgical approaches for migraines could involve decompressing one or more nerves, akin to the treatment methodologies employed for conditions like cubital tunnel syndrome, carpal tunnel syndrome, or thoracic outlet syndrome8. Surgical approaches for managing migraines encompass a diverse range of methods, including procedures such as peripheral nerve decompression via myectomy or foraminotomy, nerve excision, artery resection, and others, reflecting their heterogeneous nature7. Occipital nerve Stimulation (ONS) is another procedure with help to alleviate migraine headache9. It involves implanting a small electrical device near the occipital nerve at the skull’s base. This device delivers continuous electrical impulses to the nerve, which is believed to modulate pain signals, thereby reducing the frequency and severity of migraine attacks9.
Numerous systematic reviews have explored the field of invasive, surgical treatments for migraines, reporting varying results for different types of surgical procedures10–13. Previous reviews have shown that nerve decompression surgery can be beneficial, yet not all patients have experienced significant reductions in migraine frequency or intensity. Notably, no previous systematic reviews have focused solely on intractable migraines. Understanding the efficacy of surgical techniques specifically for intractable migraine is crucial. Findings across studies have been mixed, revealing diverse degrees of evidence regarding the effectiveness of such treatments. Our study aims to address these gaps by conducting a comprehensive systematic review and meta-analysis on surgical interventions for intractable or refractory migraines. By focusing exclusively on this particularly challenging subset of migraine patients, who suffer from severe, debilitating pain and significant reductions in quality of life, we underscore the urgency and novelty of our research. The recent emergence of studies centered on surgical approaches for migraine treatment further underlines the need for our study to validate the effectiveness of these interventions in reducing migraine symptoms, specifically addressing the needs of patients who often struggle the most.
Methods
The systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines14,15, as detailed in Table S1 (Supplemental Digital Content 2, http://links.lww.com/JS9/C406). This study has been registered in PROSPERO.
Inclusion and exclusion criteria
This systematic review aimed to assess the efficacy of selected surgical procedures specifically for intractable migraines. We focused on migraines that are refractory or intractable, meaning they do not respond to drug therapy. Our analysis was limited to surgical interventions, such as nerve decompression or ONS. We excluded remote interventions without surgery. Both observational studies (cohort and case–control) and clinical trials were considered for inclusion. Key outcomes of interest included reductions in migraine intensity, changes in Migraine Headache Index (MHI) and Migraine Disability Assessment (MIDAS) scores, the proportion of participants experiencing at least a 50% reduction in symptoms, and reductions in migraine frequency.
We excluded narrative reviews, protocols, unpublished reports, editorials, clinical case reports, commentaries, and abstracts as they did not align with the focus of our study. Our review encompassed only preprints and articles published in English, with no limitations on geographical location or research setting. For more information on the inclusion criteria, refer to Table S2 (Supplemental Digital Content 2, http://links.lww.com/JS9/C406).
Search strategy and screening
We conducted a literature search across multiple databases, including PubMed, Web of Science, Scopus, and Embase, from inception until 05 August 2023. The search strategy combined keywords, MeSH terms, and synonyms pertinent to migraines, surgery, and associated outcomes. We specifically focused on publications in English, with no restrictions concerning the year of publication. Please refer to Table S3 (Supplemental Digital Content 2, http://links.lww.com/JS9/C406) for further details.
We utilized AutoLit, Nested Knowledge, a semi-automated software platform for removing duplicates, screening, and extraction processes. Upon retrieval of search results, an initial screening of the identified articles was undertaken by two independent researchers. Both researchers autonomously assessed the titles and abstracts to exclude articles not pertinent to the study’s objectives. After this preliminary screening, a detailed evaluation of the full-text articles was conducted to ascertain their relevance and eligibility for inclusion in this systematic review. In instances of discrepancies or divergences in opinion between the two primary researchers, a third senior researcher was consulted to arbitrate and provide a definitive inclusion decision.
Data extraction and quality assessment
Two investigators undertook the task of data extraction from the selected studies. The extracted data included the first author’s name, the country of the study’s origin, the year of publication, participants’ age, demographic specifics, population type, total sample size, type of the intervention, and each pertinent outcome such as reduction in intensity score, rate of patients who got 50% reduction in migraine headache and MIDAS scores.
We assessed the quality of included RCTs using the Cochrane Risk of Bias 2 (RoB 2) tool, which examines several bias domains to ensure study reliability16. This involves a detailed examination of five critical bias domains: bias arising from the randomization process, bias due to deviations from intended interventions, bias due to missing outcome data, bias in measurement of the outcome, and bias in selection of the reported result. Each domain is assessed to determine the risk of bias as ‘low’, ‘some concerns’, or ‘high’, based on specific criteria outlined by the RoB 2 tool. The overall risk of bias in a study is determined by the highest risk level found in any domain. If any domain is judged high, the study has a high risk of bias. If all domains are low, the study has a low risk of bias. If any domain has some concerns without any high risks, the study is considered to have some concerns overall. For observational studies, we applied the Newcastle–Ottawa Scale (NOS) to evaluate their quality based on three domains: selection, comparability, and outcome measurement. High-quality studies score 7–9, meeting most criteria across domains; moderate-quality studies score 4–6, meeting some criteria but with flaws; low-quality studies score 0–3, failing to meet several criteria.
Statistical analysis
We utilized a random-effects model to determine the combined effect sizes to address potential research discrepancies. DerSimonian–Laird (DL) estimator was used for the meta-anlaysis. This method acknowledges the natural differences in the studies and offers a more reliable estimate of the overall effect15. The variability in outcomes across studies, termed heterogeneity, was assessed using I 2 and tau-squared metrics17,18. I² values can range from 0 to 100%, with higher values indicating greater heterogeneity. Heterogeneity is classified as high (I²>50%), moderate (I²=26–50%), or low (I²<25%)19,20. We set a specific threshold in advance to gauge the statistical relevance of the detected heterogeneity. The 95% prediction interval is a statistical measure used to estimate the range within which future observations are expected to fall with a 95% confidence level21,22. Generally, a P-value of under 0.05 is deemed statistically relevant. The tau-squared value is derived from the maximum likelihood estimation technique23. All our statistical analyses were executed with the R software, version 4.3.024.
Certainty of evidence
We used the grading of Recommendations, Assessment, Development, and Evaluations (GRADE) approach for assessing the certainty of evidence25. The GRADE approach assesses the quality of evidence across studies in a systematic review, classifying it into four levels: high, moderate, low, or very low, based on the risk of bias, inconsistency, indirectness, imprecision, and publication bias. Each outcome for each intervention was assessed for certainty of evidence by using GRADEpro.
Results
Literature search
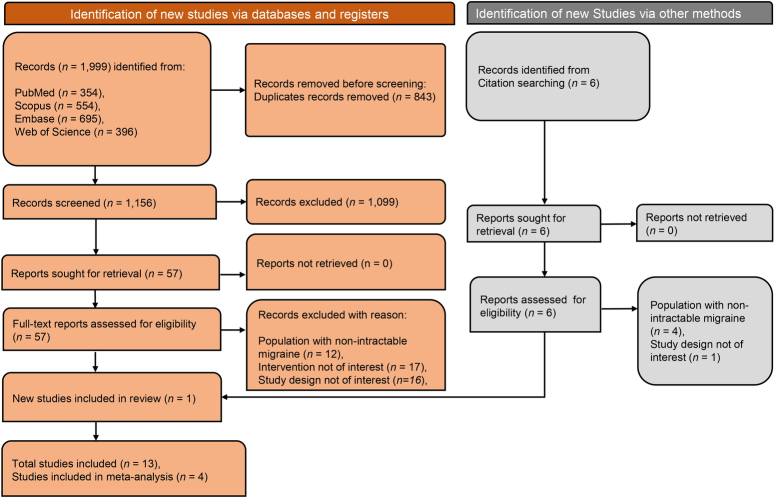
A comprehensive literature search was conducted across various databases to identify eligible studies. Figure 1 illustrates the process of identifying and selecting relevant studies. Initially, 1999 articles were retrieved from PubMed, Scopus, Embase, and Web of Science databases. Among these, 843 duplicates were eliminated, and the remaining articles underwent primary screening. During the primary screening, which involved assessing titles and abstracts, 1099 articles were excluded for various reasons, leaving 57 articles to proceed to the full-text screening phase. Following full-text screening, only ten studies satisfied the inclusion criteria. Additionally, a cross-reference search was performed to uncover additional studies, identifying six relevant articles, of which one met the inclusion criteria. A total of 13 were included in the study, of which 10 were observational studies, and the remaining three were randomized controlled trials (RCTs).
Figure 1.
PRISMA flow diagram depicting screening and selection of studies.
Characteristics of included studies
The characteristics of the included studies in the review are given in Table 1. A total of 519 subjects were involved in the studies. The studies were conducted in different regions globally. Specifically, eight were conducted in the USA9,26–32, two in Iran33,34, and one each in Spain35, UK36, and Italy37. Various types of surgeries/interventions were performed across studies for the treatment of intractable or refractory migraine. Nerve Depression in three studies26,27,33, Functional Endoscopic Sinus Surgery32, Septorhinoplasty34 in each study and seven studies performed ONS9,29–31,35–37. Most studies were conducted in the USA and focused specifically on Nerve Decompression surgery. Among the three RCTs, one showed a high risk of bias30, and the other two had some concerns regarding the risk of bias31,37. The observational studies were assessed to be of moderate quality overall (Table S4, Supplemental Digital Content 2, http://links.lww.com/JS9/C406).
Table 1.
Characteristics of included studies.
| Outcomes | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Migraine intensity | MIDAS | ||||||||||||
| Study | Country | Study design | Population | Age (mean) | Male % | Sample size | Type of surgery/intervention | Baseline mean (SD) | Final mean (SD) | Baseline mean (SD) | Final mean (SD) | 50% MHI reduction (%) | Follow-up duration |
| Albano et al., 202328 | USA | Prospective observational study | Chronic migraine patients failed drug therapy | 43 | 18 | 34 | Decompression or neurectomy | NA | NA | 57 (87) Median | 20 (59) Median | NA | 20.7 mo |
| Behin et al., 200532 | USA | Prospective observational study | Migraine patients failed at least three drugs | 45 | NA | 21 | Functional Endoscopic Sinus Surgery | 7.8 (1.5) | 3.6 (3.7) | NA | NA | NA | 62 mo |
| Dirnberger et al., 200427 | USA | Prospective observational study | Migraine patients not responding to drug therapy | NA | NA | 60 | Nerve Decompression | NA | NA | NA | NA | 40 | Six months |
| Gfrerer et al., 201926 | USA | Prospective observational study | Refractory migraine Patients | 45 | 14 | 85 | Nerve Decompression | NA | NA | NA | NA | 82 | 12 mo |
| Ghazisaidi et al., 201234 | Iran | Prospective observational study | Patients with a refractory migraine and deviated nose | NA | NA | 24 | Septorhinoplasty | 8.9 (8–10) | 0.72 (0–3) | NA | NA | NA | 31 mo |
| Hann et al., 201329 | USA | Prospective observational study | Polypharmacological therapy failed chronic migraine patients | 41.5 | 21 | 14 | Occipital nerve stimulation | 7.32 (2.4)a | 3.4 (2.3) | NA | NA | NA | 31 mo |
| Mekhail et al., 201638 | USA | Randomized, Double-blind, Controlled trial | Chronic migraine patients failed drug therapy | 44.6 | 25 | 13 | Occipital nerve stimulation | 7.29 (1.20) | 5.14 (2.25) | 168 (55.36) | 86.43 (73.58) | NA | 13 mo |
| Miller et al., 201739 | UK | Prospective cohort study | Intractable chronic migraine | 47.7 | 24 | 53 | Occipital nerve stimulation | 6 (1.71) | 4.66 (2.59) | 154.91 (84.03) | 134.28 (92.7) | NA | 42 mo |
| Omranifard et al., 200440 | Iran | Prospective, randomized, controlled trial | Migraine patients not controlled by drug treatment | 42.2 | 12 | 25 | Nerve Decompression | 8.31 (0.28) | 4.06 (0.18) | NA | NA | NA | 12 mo |
| Rodrigo et al., 201735 | Spain | Prospective observational study | Chronic migraine patients with poor response to drug | 46.9 | NA | 35 | Occipital nerve stimulation | 9.1 (0.64) | Decreased by 4.9 (2.0) | NA | NA | NA | 112.8 mo |
| Schwedt et al., 20079 | USA | Retrospective observational study | Medically intractable migraine | 39 | 20 | 15 | Occipital nerve stimulation | 7.1 (1.3) | 4.7 (2.2) | 178 (80) | 109 (92) | NA | 19 mo |
| Serra et al., 201237 | Italy | Randomized cross-over study | Chronic refractory migraine | 46 | 34 | 29 | Occipital nerve stimulation | NA | NA | 79 (30–135) | 10 (0–20) | NA | 12 mo |
| Silberstein et al., 201231 | USA | Prospective, randomized, controlled trial | Refractory chronic migraine Patients | 45 | 22.9 | 105 | Occipital nerve stimulation | 5.99 (1.68) | NA | 158.4 (76.8) | Reduced by 64.6 points | NA | 18.3 mo |
Calculated by adding mean follow-up score and mean reduction score.
NA, Not available.
Occipital nerve stimulation
Seven studies analyzed the efficacy of ONS for intractable or refractory migraine. The migraine intensity score (on a scale of 0–10) was reported in four studies for ONS surgery. The meta-analysis, which included 95 patients, showed a significant decrease in the mean migraine intensity score of −2.27 (95% CI: −3.92; −0.63) (P=0.021), with a prediction interval of −6.25 to 1.71. A heterogeneity with an I 2 value of 60% was observed (P=0.06). Figure 2 illustrates a forest plot of the meta-analysis. Rodrigo et al. also reported a decrease in mean migraine intensity scores by 4.9 points from 9.1 in 35 patients. The certainty of the evidence was found to be very low for reducing migraine intensity with ONS due to imprecision (Table S5, Supplemental Digital Content 2, http://links.lww.com/JS9/C406).
Figure 2.
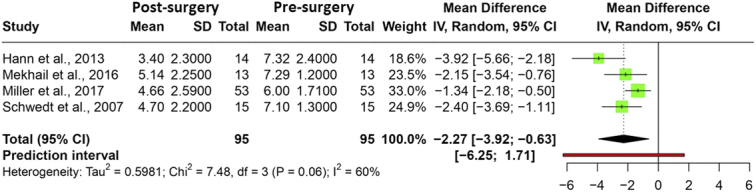
Forest plot depicting the mean difference in migraine intensity presurgery and postsurgery.
Five studies reported changes in MIDAS scores with ONS. Among these, three studies reported baseline and final MIDAS scores as mean and SD, including 81 patients. A reduction in the mean MIDAS score of −52.3 (95% CI: −136.85–32.19) (P=0.116) with a prediction interval of −488.7 to 384.1 was observed. A moderate heterogeneity with an I 2 value of 57% was observed (P=0.10). Figure 3 illustrates a forest plot of the meta-analysis. Serra et al. reported baseline and final MIDAS scores in mean and range for 34 patients who underwent ONS. The baseline mean MIDAS score was reduced from 79 (30–135) to 10 (0–20). Similarly, Silberstein et al. reported a reduction in MIDAS by 64.6 points post-ONS surgery in 105 patients. The certainty of the evidence was found to be moderate for the reduction in MIDAS with ONS due to imprecision (Table S5, Supplemental Digital Content 2, http://links.lww.com/JS9/C406).
Figure 3.
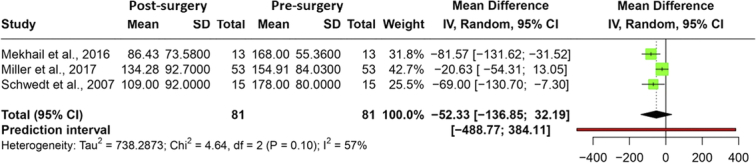
Forest plot depicting the mean difference in MIDAS score presurgery and postsurgery.
Nerve decompression surgery
Three studies were available for nerve decompression surgery for intractable migraine. Omranifard et al. found a reduction in the mean migraine intensity scale from 8.31 (0.28) to 4.06 (0.18) postsurgery by nerve decompression. The certainty of the evidence was found to be low for the reduction of migraine intensity with nerve decompression due to imprecision (Table S6, Supplemental Digital Content 2, http://links.lww.com/JS9/C406). Albano et al. found a median MIDAS reduction from 57 to 20 scores after surgery. The certainty of the evidence was very low for the reduction in MIDAS score with nerve decompression due to imprecision (Table S6, Supplemental Digital Content 2, http://links.lww.com/JS9/C406).
Two studies reported a 50% reduction in MHI with nerve decompression surgery. Dirnberger et al. reported that 40% of the participants experienced a 50% reduction in MHI with surgery. Similarly, Grefer et al. found that 82% of the participants who underwent surgery experienced a 50% reduction in MHI. The certainty of the evidence was found to be very low for the 50% reduction in MHI with nerve decompression due to imprecision (Table S6, Supplemental Digital Content 2, http://links.lww.com/JS9/C406).
Septorhinoplasty and functional endoscopic sinus surgery
Two studies were available which evaluated the efficacy of nose-related surgeries for migraine headaches. Behin et al. conducted a study on the efficacy of functional sinus surgery among 21 patients with intractable migraines and found a mean reduction in the Migraine Intensity Scale from 7.8 (1.5) to 3.6 (3.7). Septorhinoplasty was assessed by Ghazisaidi et al. among 24 patients, and they found a mean reduction in migraine intensity from 8.9 to 0.72. The certainty of evidence was very low for migraine intensity reduction due to imprecision (Table S7, Supplemental Digital Content 2, http://links.lww.com/JS9/C406).
Publication bias
Due to the limited number of studies in the meta-analysis, we could not perform the publication bias assessment statistically.
Discussion
This systematic review and meta-analysis showed a significant postsurgical decrease in migraine intensity MIDAS and the proportion of participants with 50% MHI. Nerve decompression and ONS, the most studied and clinically proven techniques, yielded promising results. The considerable mean difference postsurgery indicates potential therapeutic benefits for patients suffering from intractable migraines. These findings provide a substantial contribution to the field of migraine management, particularly in addressing the challenges of intractable or refractory migraines. The novelty of this research lies in its specific focus on the effectiveness of surgical interventions for this subset of migraines. This area has previously garnered skepticism within the medical community. A thorough meta-analysis provides empirical evidence supporting the efficacy of surgical approaches like nerve decompression and ONS, showcasing their potential to reduce migraine intensity and MIDAS scores significantly. This is particularly noteworthy as it offers a new direction for treatment where conventional methods have failed.
Although our study is the first meta-analysis to evaluate surgery for intractable migraine in specific, several other systematic reviews and meta-analyses have already addressed surgical interventions for certain types of migraines. To facilitate and quantify analysis, we established specific criteria for intractable or refractory migraine. For instance, the study by Elwahary et al.11 found that migraine surgery significantly reduced migraine outcomes (duration, intensity, and frequency) and led to an overall decrease in the MHI. Their meta-analysis showed enhanced results postmigraine surgery, albeit with some variability. This inconsistency arises from the inclusion of diverse surgical techniques, differences in study parameters, and the evolving landscape of migraine surgery. While past skepticism existed, the current literature supports the surgery’s efficacy. However, safety concerns persist, with the American Headache Society emphasizing the need for more evidence41. Their study analyzed complication rates and found that, although over a third of the 1645 patients experienced complications, most were minor. Similarly, another systematic review by Henriques et al.13 presented robust clinical data from high-impact journals supporting extracranial surgical treatment’s safety and efficacy for migraine headaches.
The predominance of US-based research in our systematic review and meta-analysis may reflect the advanced state of medical research and surgical innovation within the country, particularly in the field of migraine treatment. However, this concentration also suggests a need for caution when applying these results globally. The variability in healthcare systems, access to surgical interventions, and patient populations across different regions could influence the effectiveness and feasibility of these surgical treatments for intractable migraines. Therefore, while our findings indicate promising therapeutic benefits of surgical interventions such as nerve decompression and ONS, the potential impact of regional differences on treatment outcomes cannot be overlooked. Further research involving diverse geographical locations is crucial to validate the efficacy of these interventions in a broader context and to understand any variations in treatment response among different populations. This aspect underscores the importance of including studies from a wider range of countries in future research to ensure the findings are applicable and beneficial to migraine sufferers worldwide.
The findings from our meta-analysis indicate the potential therapeutic benefits of surgical interventions for intractable or refractory migraines. Clinicians may consider these surgical options viable alternatives for patients who have not responded to conventional treatment. The consistent outcomes across various surgical techniques suggest that there is not a one-size-fits-all approach, allowing for tailored interventions based on individual patient needs and identified triggers. As the field evolves, future research should further prioritize large-scale, multicenter randomized controlled trials to validate the efficacy and safety of these surgical interventions. Additionally, long-term follow-up studies are crucial to assessing surgical outcomes’ sustainability and potential complications. Given the skepticism in parts of the medical community, especially among neurologists, bridging the knowledge gap through interdisciplinary collaborations is imperative, ensuring that the benefits of migraine surgery reach a broader audience. Lastly, with the emerging understanding of peripheral nerve irritation’s role in migraines, research should progress deep into the mechanisms underlying surgical success, potentially paving the way for innovative, less invasive interventions.
Our study has some limitations that warrant consideration. Firstly, we restricted our inclusion criteria to articles published solely in English, which may have introduced a language bias. Secondly, the outcomes, such as migraine intensity, MHI, and MIDAS, were based on patient-reported outcomes. Such self-reported measures are inherently subjective and can vary based on individual perceptions, potentially introducing bias into research findings. Quantitative analysis was only possible for some of the studies due to the limited number of studies available and the need to stratify them by the type of surgery and the nature of the reported outcomes. We acknowledge a significant limitation in our study’s design, which is the reliance on preintervention and postintervention values without the comparison to a control group. This methodological choice restricts our ability to definitively attribute the observed changes solely to the surgical intervention, as other potential factors or confounding variables could also influence the outcomes. The absence of a direct statistical comparison between intervention and control groups limits the strength of our conclusions regarding the efficacy of the surgical treatments for intractable or refractory migraines. The limited number of trials included in our analysis, with only three clinical trials incorporated, underscores the need for more comprehensive and robust research.
Conclusion
This study indicates the clinical potential of surgical interventions as a promising avenue for managing intractable and/or refractory migraines. As the medical community continues to explore this therapeutic approach, interdisciplinary collaboration and extensive research remain vital for fine-tuning and substantiating the effectiveness of dedicated surgical procedures, ultimately leading to broader patient benefits.
Ethical approval
Not required.
Informed consent statement
Not applicable.
Source of funding
None.
Author contribution
B.K.P., T.A., A.M., A.A., H.F.A., and V.R.: concept; M.S., G.B., and B.K.P.: data acquisition; A.B., K.A., M.N.K., S.G., and Q.S.Z.: data analysis; B.K.P., T.A., A.M., A.A., H.F.A., V.R., A.B., K.A., M.N.K., and S.G.: drafting of manuscript; M.N.K., S.G., Q.S.Z., M.S., G.B., S.R., N.K., P.S., R.K.M., and A.D.: critical analysis and reviewing; B.K.P., T.A., A.M., A.A., H.F.A., V.R., A.B., K.A., M.N.K., S.G., Q.S.Z., M.S., G.B., S.R., N.K., P.S., R.K.M., and A.D.: approval for final version.
Conflicts of interest disclosure
The authors declare no conflicts of interest.
Research registration unique identifying number (UIN)
PROSPERO: CRD42023464281.
Guarantor
Bijaya Kumar Padhi.
Data availability statement
Documents containing all extracted data are available in the manuscript and the accompanying Supplementary Material (Supplemental Digital Content 1, http://links.lww.com/JS9/C407).
Data are available with authors and available on request. Some data are available in supplementary material file.
Provenance and peer review
Invited.
Institutional review board statement
Not applicable.
Supplementary Material
Acknowledgements
Assistance with the study: none.
Presentation: none.
The authors acknowledge the Nested-Knowledge, MN, USA for providing the access to the software.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Supplemental Digital Content is available for this article. Direct URL citations are provided in the HTML and PDF versions of this article on the journal’s website, www.lww.com/international-journal-of-surgery.
Published online 15 April 2024
Contributor Information
Tahani Alrahbeni, Email: ph.tahani@riyadh.edu.sa.
Ahmed Mahal, Email: ahmed.mahal@cihanuniversity.edu.iq.
Anas Alkhouri, Email: anas.alkhouri@cihanuniversity.edu.iq.
Hadil F. Alotaibi, Email: Hfalotaibi@pnu.edu.sa.
Vineet Rajagopal, Email: drvineethrajagopal@gmail.com.
Ashish Behera, Email: drashishbehera@gmail.com.
Khalid AL-Mugheed, Email: khaled.almugheed@riyadh.edu.sa.
Mahalaqua N. Khatib, Email: nazli.786@rediffmail.com.
Shilpa Gaidhane, Email: drshilpagaidhane@gmail.com.
Quazi S. Zahiruddin, Email: zahirquazi@gmail.com.
Muhammed Shabil, Email: mohdshabil99@gmail.com.
Ganesh Bushi, Email: ganyganesh313@gmail.com.
Sarvesh Rustagi, Email: sarveshrustagi@uumail.in.
Neelima Kukreti, Email: nkukreti@gehu.ac.in.
Prakasini Satapathy, Email: prakasini.satapathy@gmail.com.
Ranjan K. Mohapatra, Email: ranjank_mohapatra@yahoo.com.
Arkadiusz Dziedzic, Email: adziedzic@sum.edu.pl.
Bijaya K. Padhi, Email: padhi.bijaya@pgimer.edu.in;bkpadhi@gmail.com.
References
- 1. Amiri P, Kazeminasab S, Nejadghaderi SA, et al. Migraine: a review on its history, global epidemiology, risk factors, and comorbidities. Front Neurol 2022;12:800605; 2553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Straube A, Andreou A. Primary headaches during lifespan. J Headache Pain 2019;20:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Andreou AP, Edvinsson L. Mechanisms of migraine as a chronic evolutive condition. J Headache Pain 2019;20:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Matilde L, Raggi A. A narrative review on the burden of migraine: when the burden is the impact on people’s life. J Headache Pain 2019;20:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Steiner TJ, Stovner LJ. Global epidemiology of migraine and its implications for public health and health policy. Nat Rev Neurol 2023;19:109–117. [DOI] [PubMed] [Google Scholar]
- 6. Simona S, Braschinsky M, Ducros A, et al. European headache federation consensus on the definition of resistant and refractory migraine. J Headache Pain 2020;21:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bajaj J, Munakomi S. Migraine surgical interventions. 2018. [PubMed]
- 8. Guyuron B, Reed D, Kriegler JS, et al. A placebo-controlled surgical trial of the treatment of migraine headaches. Plast Reconstr Surg 2009;124:461–468. [DOI] [PubMed] [Google Scholar]
- 9. Schwedt T, Dodick D, Hentz J, et al. Occipital nerve stimulation for chronic headache—long-term safety and efficacy. Cephalalgia 2007;27:153–157. [DOI] [PubMed] [Google Scholar]
- 10. Nagori SA, Jose A, Roychoudhury A. Surgical management of migraine headaches: a systematic review and meta-analysis. Ann Plast Surg 2019;83:232–240. [DOI] [PubMed] [Google Scholar]
- 11. ElHawary H, Barone N, Baradaran A, et al. Efficacy and safety of migraine surgery: a systematic review and meta-analysis of outcomes and complication rates. Ann Surg 2022;275:e315–e323. [DOI] [PubMed] [Google Scholar]
- 12. Vincent AJ, Van Hoogstraten WS, Maassen Van Den Brink A, et al. Extracranial trigger site surgery for migraine: a systematic review with meta-analysis on elimination of headache symptoms. Front Neurol 2019;10:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Henriques S, Almeida A, Peres H, et al. Current evidence in migraine surgery: a systematic review. Ann Plast Surg 2022;89:113–120. [DOI] [PubMed] [Google Scholar]
- 14. Kabir R, Hayhoe R, Bai AC, et al. The systematic literature review process: a simple guide for public health and allied health students. 2023.
- 15. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg 2021;88:105906. [DOI] [PubMed] [Google Scholar]
- 16. Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
- 17. IntHout J, Ioannidis JP, Rovers MM, et al. Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open 2016;6:e010247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bushi G, Shabil M, Padhi BK, et al. Prevalence of acute kidney injury among dengue cases: a systematic review and meta-analysis. Trans R Soc Trop Med Hyg 2024;118:1–11. [DOI] [PubMed] [Google Scholar]
- 19. Gandhi AP, Shamim MA, Padhi BK. Steps in undertaking meta-analysis and addressing heterogeneity in meta-analysis. The Evidence 2023;1:44–59. [Google Scholar]
- 20. Shabil M, Bushi G, Beig MA, et al. Cardiovascular manifestation in tuberculosis cases: a systematic review and meta-analysis. Curr Probl Cardiol 2023;48:101666. [DOI] [PubMed] [Google Scholar]
- 21. Bushi G, Padhi BK, Shabil M, et al. Cardiovascular disease outcomes associated with obstructive sleep apnea in diabetics: a systematic review and meta-analysis. Diseases 2023;11:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Swarup SS, P AK, Padhi BK, et al. Cardiovascular consequences of financial stress: a systematic review and meta-analysis. Curr Probl Cardiol 2024;49:102153. [DOI] [PubMed] [Google Scholar]
- 23. Langan D, Higgins JP, Jackson D, et al. A comparison of heterogeneity variance estimators in simulated random‐effects meta‐analyses. Res Synth Methods 2019;10:83–98. [DOI] [PubMed] [Google Scholar]
- 24. Shamim MA, Gandhi AP, Dwivedi P, et al. How to perform meta-analysis in R: a simple yet comprehensive guide. The Evidence 2023;1:60–80. [Google Scholar]
- 25. Langendam MW, Akl EA, Dahm P, et al. Assessing and presenting summaries of evidence in cochrane reviews. Syst Rev 2013;2:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gfrerer L, Hulsen JH, McLeod MD, et al. Migraine surgery: an all or nothing phenomenon? Prospective evaluation of surgical outcomes. Ann Surg 2019;269:994–999. [DOI] [PubMed] [Google Scholar]
- 27. Dirnberger F, Becker K. Surgical treatment of migraine headaches by corrugator muscle resection. Plast Reconstr Surg 2004;114:652–657. [DOI] [PubMed] [Google Scholar]
- 28. Albano NJ, Israel JS, Carbullido MK, et al. Measuring success in headache surgery: a comparison of different outcomes measures. Plast Reconstr Surg 2023;151:469e–476e. [DOI] [PubMed] [Google Scholar]
- 29. Hann S, Sharan A. Dual occipital and supraorbital nerve stimulation for chronic migraine: a single-center experience, review of literature, and surgical considerations. Neurosurg Focus 2013;35:E9. [DOI] [PubMed] [Google Scholar]
- 30. Mekhail NA, Estemalik E, Azer G, et al. Safety and efficacy of occipital nerves stimulation for the treatment of chronic migraines: randomized, double‐blind, controlled single‐center experience. Pain Practice 2017;17:669–677. [DOI] [PubMed] [Google Scholar]
- 31. Silberstein SD, Dodick DW, Saper J, et al. Safety and efficacy of peripheral nerve stimulation of the occipital nerves for the management of chronic migraine: results from a randomized, multicenter, double-blinded, controlled study. Cephalalgia 2012;32:1165–1179. [DOI] [PubMed] [Google Scholar]
- 32. Behin F, Behin B, Bigal M, et al. Surgical treatment of patients with refractory migraine headaches and intranasal contact points. Cephalalgia 2005;25:439–443. [DOI] [PubMed] [Google Scholar]
- 33. Omranifard M, Abdali H, Ardakani MR, et al. A comparison of outcome of medical and surgical treatment of migraine headache: in 1 year follow-up. Adv Biomed Res 2016;5:121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ghazisaidi MR, Kalantar-Hormozi A, Mozaffari N, et al. Septorhinoplasty as a treatment modality in refractory migraine headaches. Eur J Plast Surg 2012;35:267–271. [Google Scholar]
- 35. Rodrigo D, Acín P, Bermejo P. Occipital nerve stimulation for refractory chronic migraine: results of a long-term prospective study. 2017. [PubMed]
- 36. Miller S, Watkins L, Matharu M. Long-term outcomes of occipital nerve stimulation for chronic migraine: a cohort of 53 patients. J Headache Pain 2016;17:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Serra G, Marchioretto F. Occipital nerve stimulation for chronic migraine: a randomized trial. Pain Physician 2012;15:245. [PubMed] [Google Scholar]
- 38. Mekhail NA, Estemalik E, Azer G, et al. Safety and efficacy of occipital nerves stimulation for the treatment of chronic migraines: randomized, double‐blind, controlled single‐center experience. Pain Practice. 2017;17:669–677. [DOI] [PubMed] [Google Scholar]
- 39. Omranifard M, Abdali H, Ardakani MR, et al. A comparison of outcome of medical and surgical treatment of migraine headache: In 1 year follow-up. Adv Biomed Res 2016;5:121. doi: 10.4103/2277-9175.186994. PMID: 27563631; PMCID: PMC4976529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Miller S, Watkins L, Matharu M. Long-term outcomes of occipital nerve stimulation for chronic migraine: a cohort of 53 patients. The journal of headache and pain 2016;17:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Loder E, Weizenbaum E, Frishberg B, et al. American Headache Society Choosing Wisely Task Force. Choosing wisely in headache medicine: the American Headache Society’s list of five things physicians and patients should questio. n Headache 2013;53:1651–1659. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Documents containing all extracted data are available in the manuscript and the accompanying Supplementary Material (Supplemental Digital Content 1, http://links.lww.com/JS9/C407).
Data are available with authors and available on request. Some data are available in supplementary material file.