Abstract
Background:
Skin of color clinics (SOCCs) are dermatology clinics that provide specialized care for patients with melanated skin. Little is known about patient perceptions and attitudes toward these clinics.
Objective:
We sought to perform a survey study to assess the opinions of patients of color previously seen in our dermatology department toward SOCC.
Methods:
A 14-question survey was sent by email to patients of color seen at our institution between January 1, 2015 and December 31, 2021.
Results:
Out of 264 participants who completed the survey, 176 (66.7%) indicated they would prefer to be seen in a SOCC and 88 (33.3%) preferred to be seen in a general dermatology clinic (GDC). Clinic choice varied significantly by ethnicity, with Black/African American participants being the most likely to prefer SOCC over GDC than other races/ethnicities. Those interested in SOCC were primarily motivated by a search for expertise in the skin of color (SOC) and did not have a preference for the skin color of the SOCC dermatologist. Those interested in GDC were happy with their current care.
Limitations:
This study was limited by the single-center design and sample bias.
Conclusion:
Our results overall provide positive patient feedback for the creation of SOCCs as centers for expertise in SOC. The preference for SOCC varied by race/ethnicity, highlighting that clinic choice is best left to the patient.
Keywords: health equity, healthcare disparities, patient-centered care, skin of color
What is known about this subject in regard to women and their families?
Little is known about what patients of color think about skin of color clinics (SOCC), and this includes women of color.
In 2019, Gorbatenko-Roth et al performed focus groups and administered surveys to 19 black patients, 18 of whom were women, who had been seen at their Center for Ethnic Skin. They reported uniformly positive experiences, suggesting that black women overall have interest in being seen in a SOCC.
These patients had already established care in a SOCC. We know relatively little about the opinions of patients (and women) of color toward SOCC who have not yet sought one out.
What is new from this article as messages for women and their families?
The majority (approximately 2/3) of our study participants, of whom the majority were women, were interested in being seen in an SOCC for their next visit. The primary motivation for this interest was in seeing a dermatologist with expertise in skin of color.
Interest in SOCC varied by race/ethnicity: black patients were more likely to want to be seen in an SOCC compared to other race/ethnic groups in our study.
Women of color should feel empowered to seek care in whatever setting they think best fits their needs. Some may seek expertise in SOC, while others may be content with care received in a general dermatology clinic.
Introduction
Across the United States, many academic centers offer specialty clinics dedicated to the needs of patients with pigmented skin.1 Known by various names, such as “skin of color clinic” (SOCC), “multicultural dermatology clinic,” or “ethnic skin clinic,” these clinics offer expertise in the diagnosis and management of skin of color (SOC). In addition to clinical care, many dermatologists in these clinics will serve as experts in SOC education and perform research on SOC topics.
The establishment of these clinics answers a call to address the unmet needs of patients with SOC, as well as a recognition of the expected diversification of the US population: by 2044, people of color are expected to make up more than half of the US population,2 further stressing the need for greater expertise in the care of SOC. The availability of SOCC appears to be welcomed by physicians, trainees, and patients alike. However, few studies have formally assessed patient perspectives toward SOCC. In this study, we performed a large survey study asking patients of color for their thoughts on SOCC, including interest in being seen in an SOCC, reasons for their choice, perceptions around the importance of skin color, and expectations toward the skin color of their dermatologist.
Methods
Survey
A 14-question survey was developed. The survey was designed with input from focus groups performed with patients of color previously seen at the Michigan Medicine Department of Dermatology and is available in the supplement. The survey was sent via email to patients who were 18 years or older at the time of a previous visit to general dermatology clinics (GDCs) between January 1, 2015 and December 31, 2021 and who self-identified as one or more of the following races and ethnicities: Black/African American, Asian, American Indian/Alaska Native, Native Hawaiian/Other Pacific Islander, and Hispanic/Latinx. Participants were offered a $10 Amazon gift card for completing the survey.
Data analysis
Survey results were analyzed for differences between participants that selected SOCC versus GDC using a 2-tailed student’s t test for continuous variables and χ2 test for categorical variables, P ≤ .05. Groups with fewer than 10 participants were excluded from statistical analyses. Racial and ethnic groups with fewer than 10 participants were grouped into an “other” category. This study was deemed exempt by our institutional review board.
Results
Demographic breakdown
In total 3,635 patients were eligible for our study. Of these, 3,148 (86.6%) had e-mails and received our recruitment e-mail. There were 264 completed surveys, yielding a response rate of 8.4%. Among these, 200 participants (75.8%) were female, 62 (23.5%) were male, 1 (0.4%) was nonbinary/nonconforming, and 1 (0.4%) preferred not to say (Table 1). Participants were distributed across all age groups: 22 (8.3%) were 18 to 24 years old, 73 (27.7%) were 25 to 34 years old, 59 (22.3%) were 35 to 44 years old, 46 (17.4%) were 45 to 54 years old, 41 (15.5%) were 55 to 64 years old, and 23 (8.7%) were 65 or older. Participants self-identified as the following races/ethnicities: 106 (40.2%) Black/African American, 73 (27.7%) East Asian, 35 (13.3%) South Asian, 35 (13.3%) selected multiple entries, and 15 (5.7%) were in the “other” category, which included those identifying as Hispanic/Latinx and Middle Eastern. By comparison, based on medical record data, the ethnic and racial breakdown of nonwhite patients seen at Michigan Medicine during the study period was as follows: 56.4% Black/African American, 40.9% Asian/Pacific Islander, 2.7% American Indian/Alaska Native, and 1.6% Hispanic/Latinx.
Table 1.
Demographic information
| Overall | SOCC | GDC | P value | |
|---|---|---|---|---|
| Total, n | 264 | 176 | 88 | |
| Age, n (%) | .044 | |||
| 18–24 y | 22 (8.3) | 17 (9.7) | 5 (5.7) | |
| 25–34 y | 73 (27.7) | 51 (29.0) | 22 (25.0) | |
| 35–44 y | 59 (22.3) | 44 (25.0) | 15 (17.0) | |
| 45–54 y | 46 (17.4) | 29 (16.5) | 17 (19.3) | |
| 55–64 y | 41 (15.5) | 26 (14.8) | 15 (17.0) | |
| 65+ y | 23 (8.7) | 9 (5.1) | 14 (15.9) | |
| Gender, n (%) | .259 | |||
| Male | 62 (23.5) | 38 (21.6) | 24 (27.3) | |
| Female | 200 (75.8) | 138 (78.4) | 62 (70.5) | |
| Nonbinary/nonconforminga | 1 (0.4) | 0 (0.0) | 1 (1.1) | |
| Prefer not to saya | 1 (0.4) | 0 (0.0) | 1 (1.1) | |
| Race/ethnicity, n (%) | <.001 | |||
| Black/African American | 106 (40.2) | 90 (51.1) | 16 (18.2) | |
| East Asian | 73 (27.7) | 31 (17.6) | 42 (47.7) | |
| South Asian | 35 (13.3) | 22 (12.5) | 13 (14.8) | |
| Multiple entries | 35 (13.3) | 23 (13.1) | 12 (13.6) | |
| Other ethnicityb | 15 (5.7) | 10 (5.7) | 5 (5.7) |
This table displays demographic information for study participants overall as well as for participants based on their interest in SOCC versus GDC.
GDC, general dermatology clinic; SOCC, Skin of color clinics; y, years.
Groups that were excluded from statistical analysis due to small sample size.
Includes Middle Eastern, Hispanic/Latinx, Native American, Southeast Asian, Native Hawaiian or Other Pacific Islander, Hmong, Unspecified Other, Prefer not to say.
Clinic preference
Of the 264 participants, 176 (66.7%) indicated they would prefer to be seen in a SOCC and 88 (33.3%) preferred to be seen in a GDC at their next visit (Table 1). The preference varied significantly by race/ethnicity. Among Black/African American participants, 90 (51.1%) preferred to be seen in SOCC. Among East Asian and South Asian participants, 31 (17.6%) and 22 (12.5%) preferred to be seen in SOCC, respectively. Clinic preference also varied significantly based on age, with younger age groups (18-44 years old) preferring to be seen in SOCC. There was no significant difference in clinic preference based on gender.
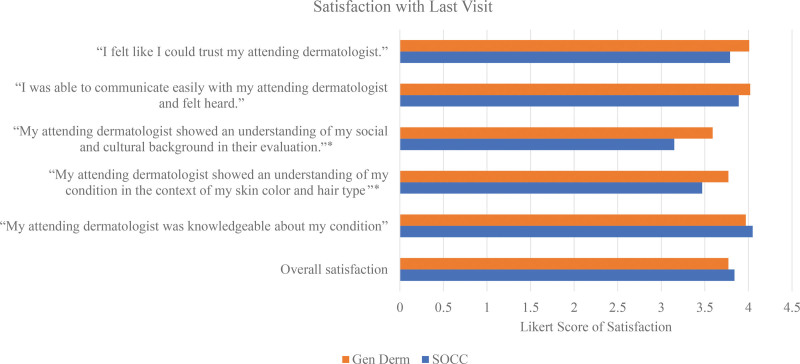
Conditions seen and satisfaction with last visit
Participants were last seen in the clinic for a variety of dermatologic complaints (Supplementary Table 1, http://links.lww.com/IJWD/A58). When asked to rate their last visit, there was no difference in overall satisfaction between those who selected SOCC versus GDC (3.84/5 for SOCC versus 3.77/5 for GDC, P = .670) (Fig. 1). Similarly, there was no difference when rating the dermatologist’s knowledge base (4.05/5 for SOCC versus 3.97/5 for GDC, P = .549), communication (3.89/5 for SOCC versus 4.02/5 for GDC, P = .338), and level of trust (3.79/5 for SOCC versus 4.01/5 for GDC, P = .121). However, those who preferred SOCC gave significantly lower scores for their dermatologist’s consideration of skin color/hair type (3.47/5 for SOCC versus 3.77/5 for GDC, P = .035) and sociocultural competency (3.15/5 for SOCC versus 3.59/5 for GDC, P = .002) when compared to those who preferred GDC.
Fig. 1.
Satisfaction with last visit. Participants were asked to rate each statement on a Likert scale from 1 (strongly disagree) to 5 (strongly agree). Average scores for those who were interested in SOCC vs GDC are shown. The asterisks denote a significant difference with P < .05. GDC, general dermatology clinic; SOCC, Skin of color clinics.
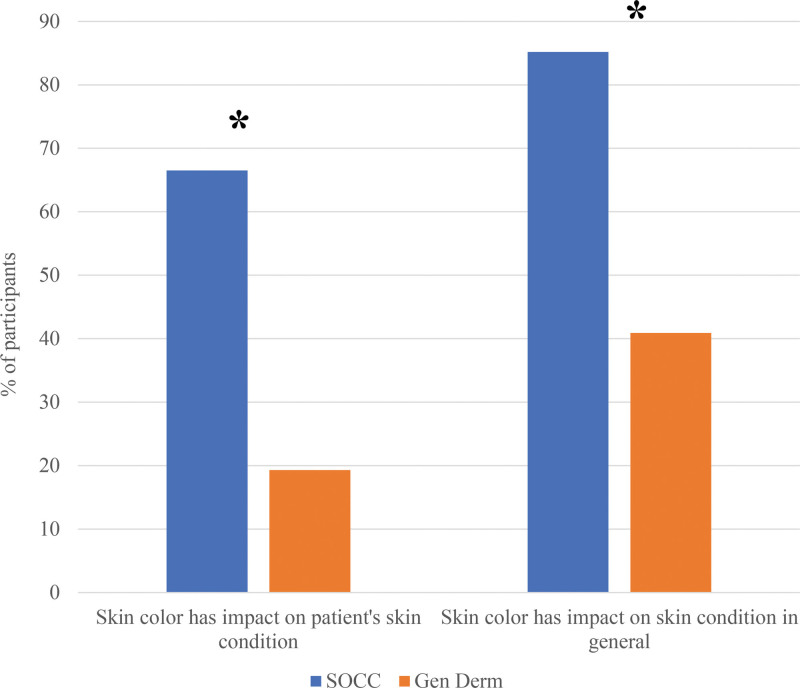
Impact of skin of color
When asked about the impact of skin color on skin disease, a significantly greater proportion of those who preferred SOCC felt that skin color impacted their skin disease compared to those who preferred GDC (117 [66.5%] for SOCC versus 17 [19.3%] for GDC, P < 0.001) (Fig. 2). Similarly, a significantly greater proportion of those who preferred SOCC felt that skin color could impact skin disease in general compared to those who preferred GDC (150 [85.2%] for SOCC versus n = 36 [40.9%] for GDC, P < 0.001).
Fig. 2.
Impact of skin color. Participants were asked whether or not skin color has an impact on their own skin condition or skin conditions in general. Those who answered yes are shown as a percent of total participants.
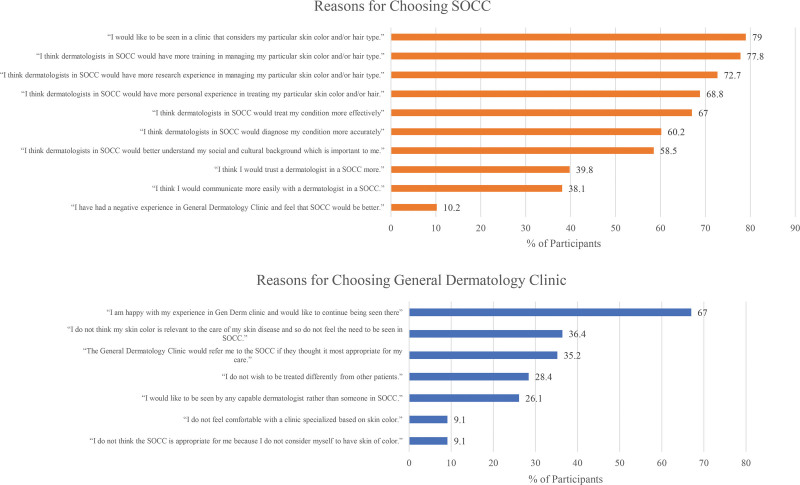
Reason(s) for clinic selection
The top 3 reasons for preferring SOCC were: wishing to be seen in a clinic that considers a patient’s skin color and/or hair type (n = 139, 79.0%), seeking a dermatologist with more training in managing their particular skin color and/or hair (n = 137, 77.8%), and seeking a dermatologist with more research experience in managing their particular skin color and/or hair type (n = 128, 72.7%) (Fig. 3). The top 3 reasons for preferring GDC were: satisfaction with the last experience in general dermatology and wishing to continue being seen there (n = 59, 67.0%), not feeling that skin color impacts their skin condition (n = 32, 36.4%), and deferring the decision to be seen in a SOCC to their general dermatologist (n = 31, 35.2%). A minority of patients in the GDC group expressed concern about being treated differently from others (n = 25, 28.4%) and establishing a clinic based on skin color (n = 8, 9.1%).
Fig. 3.
Reasons for clinic choice. Participants were asked to select any and all statements they agreed with in selecting their (top) SOCC or (bottom) GDC. Answers are summarized as the percentage of participants who selected each statement. GDC, general dermatology clinic; SOCC, Skin of color clinics.
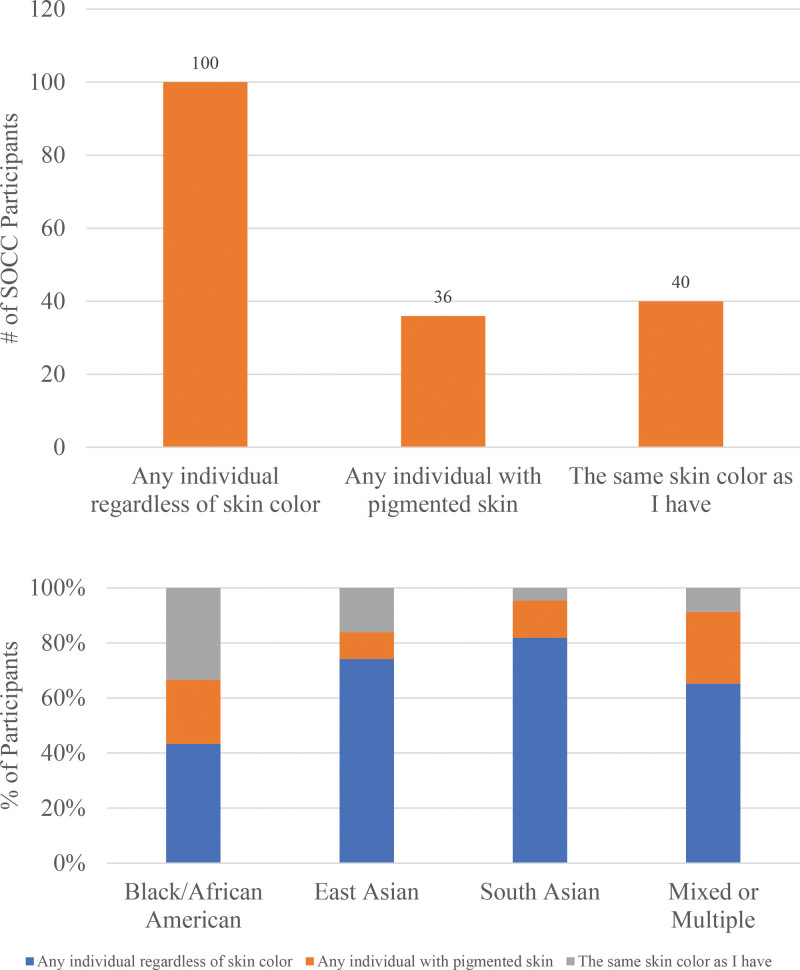
Skin color of dermatologist
Of the participants who preferred SOCC, 100 (56.8%) felt the SOCC dermatologist could be any individual, regardless of skin color, 36 (20.5%) felt the dermatologist should have SOC themselves, and 40 (22.7%) felt the dermatologist should have the same skin color as the patient. This preference varied significantly by race/ethnicity. Black/African American participants were more likely than other ethnic groups to prefer a dermatologist with the same skin color as their own (Fig. 4).
Fig. 4.
Expectations for skin color of dermatologist. (Top) Participants who were interested in SOCC were asked for expectations around the skin color of their provider. (Bottom) Answers are shown by participant’s race/ethnicity.
Research and referral
The majority of participants voiced an interest in participating in SOC research: 125 (47.3%) were willing to participate without additional specifications, 24 (9.1%) preferred to participate only through the SOCC, and 85 (32.2%) preferred to limit their involvement to research on their own condition (Supplementary Table 2, http://links.lww.com/IJWD/A59). About 30 (11.4%) declined participation in research. There was no clear preference for a method of referral to SOCC: 154 (58.3%) wished to be offered the option when they called, 123 (46.6%) preferred referrals from their primary care physician, and 112 (42.4%) preferred referrals from their dermatologist (Supplementary Table 3, http://links.lww.com/IJWD/A60).
Discussion
In the past 20 years, there have been a growing number of dermatology clinics specialized in the care of SOC in the United States. As of 2020, 15 academic centers had established SOC centers, many not only providing clinical care but also serving as hubs for SOC education and research.1
Among dermatologists and in the media, SOCCs are well-regarded and welcomed. However, little formal research has been done on patient perspectives toward SOCCs. In 2019, Gorbatenko-Roth et al.3 performed focus groups and administered surveys to Black patients seen at the Northwestern Center for Ethnic Skin. They found uniformly positive experiences, with patients reporting higher levels of satisfaction compared to prior experiences in non-SOCC. In a large survey study of people of color, Scott et al.4 also showed broad interest in SOCCs. To our knowledge, no previous studies have assessed the perspectives of dermatology patients toward SOCC before establishing care in a SOCC. Our study sought to address these gaps through a large survey study of patients of color seen in GDCs at our institution.
Our data support that the majority of patients of color prefer to be seen in a SOCC. Those wishing to be seen in a SOCC were previously seen in GDCs for a variety of skin conditions, and not just those conditions with increased prevalence among SOC patients. Interestingly, the preference for SOCC varied significantly based on race/ethnicity. Among ethnic groups, Black/African American participants were most likely to prefer SOCC, and East Asian patients were least likely. Similar findings were reported by Scott et al.4 The reason for the variation is likely multifactorial and tied to the complex sociocultural and historical fabric of the United States. We hypothesize that the variation may be at least in part explained by the degree to which participants identify as having SOC. Indeed, Black/African American participants were more likely than East Asian participants to think that their skin color impacted their skin condition or skin conditions generally, speaking to a differing perception toward the significance of one’s own skin pigmentation.
Those interested in SOCC were motivated by a desire to see a provider with expertise in SOC (ie, training and research experience), selecting these reasons more often than those relating to communication and trust. In line with these reasons, those who preferred SOCC gave significantly lower scores with regard to the sociocultural competency of the dermatologist at their last visit in GDC. Providers may therefore benefit from being explicit—and also sensitive—in their sociocultural considerations when relevant to the patient’s care. In addition, SOCC may consider exhibiting clear messaging around the expertise of their SOCC dermatologists.
These top-cited reasons for wanting to be seen in SOCC highlight the importance of dedicated training and research in SOC. The desire for improved training is shared by dermatology trainees, many of whom report deficiencies in their current comfort with SOC.5–10 In 1 study, 47% of dermatologists and dermatology residents felt that their medical training was inadequate in training them to treat conditions in SOC patients.5 These results emphasize the call for concerted efforts to diversify training curricula. A greater inclusion of SOC patients in research is also greatly needed,11,12 an opportunity that is recognized by patients. In our study, the majority of our patients expressed interest in participating in research. Importantly, some expressed interest only if offered through the SOCC and others only when pertaining to their skin condition, stressing the role of SOC centers as research hubs, and the need for sensitivity around approaching marginalized groups for research.
Those interested in GDC were primarily motivated by satisfaction with their prior experience, suggesting that not all patients of color desire a SOC expert. Many may regard their needs as being adequately addressed with a general dermatologist. Notably, approximately one-third of participants who preferred GDC stated they did not want to be treated differently from other patients or were not comfortable with a clinic specialized based on skin color. These responses reveal concerns people may have around the potential for discrimination with a SOCC, and stress the importance of thoughtful explanations around the purpose and optionality of a SOCC in patient-facing communications.
Among those who preferred to be seen in SOCC, we explored expectations around the skin color of the provider seen. The majority of participants felt they could be seen by any individual, regardless of skin color, again speaking to the priority for expertise in a SOCC. As with clinic choice, this preference varied significantly by race/ethnicity. One-third of Black/African American patients preferred to see a dermatologist with the same skin color as their own, compared to 16% of East Asians and 4.5% of South Asians. Our findings support those of Venkatesh et al.,13 who found that the preference for race concordance varies by race/ethnicity. In their survey study of dermatology patients, 42% of Black patients and 44% of Hispanic patients preferred to receive care from dermatologists of their own race/ethnicity, compared to 2% of White patients.13 As with clinic preference, we hypothesize that this finding may be at least in part explained by the degree to which patients feel their skin’s pigmentation will impact their care, and thus a desire to find a dermatologist who would identify with them on this basis. Many studies in the medical literature have pointed to a potential benefit of race-concordant visits in improving compliance and patient satisfaction.14–17 Overall, these data highlight the need to diversify our workforce and improve the cultural competency of all medical providers for patients to feel safe and understood.
There are several limitations to our study. Our study was performed at a single institution and therefore reflects the specific sociocultural environment at the University of Michigan and the communities we serve. Patient perspectives toward SOCC could understandably differ in urban versus rural settings and depending on the diversity of the provider population. Importantly, our results were subject to sampling bias, as suggested by our low response rate. Only patients with e-mails were included, which may explain the greater representation of younger patients in our study. Given these limitations, the generalizability of our results is limited. In our effort to survey patients of color, those identifying as White/Caucasian were excluded, which may have excluded certain races/ethnicities. We wonder if this impacted those who identify as Middle Eastern, for whom our sample size is small. All in all, our results should be followed up by multicenter studies that sample opinions across the United States to ensure we adequately capture the opinions of SOC patients. To this end, it would be important to query patients in different languages, as English may not be the primary language for certain SOC populations.
Our data shine a light on patient perspective toward SOCCs. Patients of color are interested in being seen in SOCCs for expertise in how their skin color may affect their care. Importantly, the interest was not held by all patients of color and varied by race/ethnicity, emphasizing that clinic choice should be a personal decision best left to the patient. In addition, our data suggest the benefit of SOCC as hubs for SOC training and research. With the existing healthcare disparities in our patient outcomes and the lagging diversity of our workforce, there is a need to accelerate our progress in SOC education and research. SOCC may serve this purpose as centers that concentrate our efforts in these areas.
Conflicts of interest
None.
Funding
Supported by the Garbose Family Resident Research Fund.
Study approval
N/A
Author contributions
SC, RT, GH, MPC-T, and ME contributed to survey development and data collection. SC, RT, MM, and JLR contributed to data analysis. The manuscript was written by SC and edited by all authors.
Acknowledgements
We acknowledge the Garbose Family Resident Research Fund, whose funding assisted with data collection in supplying gift cards to participants. Funding was not utilized for design and conduct of the study; management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Supplementary data
Supplementary material associated with this article can be found at http://links.lww.com/IJWD/A58, http://links.lww.com/IJWD/A59, and http://links.lww.com/IJWD/A60.
Supplementary Material
Footnotes
Published online 17 October 2024
References
- 1.Tull RZ, Kerby E, Subash JJ, McMichael AJ. Ethnic skin centers in the United States: where are we in 2020? J Am Acad Dermatol 2020;83:1757–9. [DOI] [PubMed] [Google Scholar]
- 2.Colby SL, Ortman JM. Projections of the Size and Composition of the U.S. population: 2014 to 2060. Current population reports, P25-1143. Washington, DC: U.S. Census Bureau; 2015. Available from: https://www.census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf. Accessed July 24, 2023. [Google Scholar]
- 3.Gorbatenko-Roth K, Prose N, Kundu RV, Patterson S. Assessment of black patients’ perception of their dermatology care. JAMA Dermatol 2019;155:1129–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scott K, Poondru S, Jackson KL, Kundu RV. The need for greater skin of color training: perspectives from communities of color. Arch Dermatol Res 2023;315:2441–4. [DOI] [PubMed] [Google Scholar]
- 5.Buster KJ, Stevens EI, Elmets CA. Dermatologic health disparities. Dermatol Clin 2012;30:53–9, viii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cline A, Winter RP, Kourosh S, et al. Multiethnic training in residency: a survey of dermatology residents. Cutis 2020;105:310–3. [PubMed] [Google Scholar]
- 7.Ibraheim MK, Gupta R, Dao H, Patel A, Koshelev M. Evaluating skin of color education in dermatology residency programs: data from a national survey: edited by Stephen P. Stone, MD. Clin Dermatol 2021;40:228–33. [DOI] [PubMed] [Google Scholar]
- 8.Okoro U, Chau TQ, Kawaoka J, Wong V, Qureshi AA. Skin of color in preclinical medical education: a cross-institutional comparison and a call to action. Cutis 2021;108:204–9. [DOI] [PubMed] [Google Scholar]
- 9.Nijhawan RI, Jacob SE, Woolery-Lloyd H. Skin of color education in dermatology residency programs: does residency training reflect the changing demographics of the United States? J Am Acad Dermatol 2008;59:615–8. [DOI] [PubMed] [Google Scholar]
- 10.Syder NC, McKenzie S, Omar D, Brown-Korsah JB, Taylor SC, Elbuluk N. Gaps in medical education curricula on skin of color in medical school, residency, and beyond: Part 1. J Am Acad Dermatol 2023;89:885–92. [DOI] [PubMed] [Google Scholar]
- 11.Omar D, Syder N, Brown-Korsah JB, McKenzie S, Elbuluk N, Taylor SC. Racial and ethnic disparities in clinical research and the dermatology workforce. J Am Acad Dermatol 2022;89:895–902. [DOI] [PubMed] [Google Scholar]
- 12.Sun M, Wilson BN, Zhou RZ, Murrell DF, Murase JE. Evaluation of skin of color content in skin research and technology. Skin Res Technol 2022;28:355–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Venkatesh KP, Nelson K, Friedman A. Sociocultural attitudes and perceptions of potential barriers to care for dermatology patients. J Am Acad Dermatol 2021;85:983–6. [DOI] [PubMed] [Google Scholar]
- 14.Adamson AS, Glass DA, 2nd, Suarez EA. Patient-provider race and sex concordance and the risk for medication primary nonadherence. J Am Acad Dermatol 2017;76:1193–5. [DOI] [PubMed] [Google Scholar]
- 15.Harvey VM, Ozoemena U, Paul J, Beydoun HA, Clemetson NN, Okoye GA. Patient-provider communication, concordance, and ratings of care in dermatology: results of a cross-sectional study. Dermatol Online J 2016;22:13030/qt06j6p7gh. [PubMed] [Google Scholar]
- 16.Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med 2003;139:907–15. [DOI] [PubMed] [Google Scholar]
- 17.Otte SV. Improved patient experience and outcomes: is patient-provider concordance the key? J Patient Exp 2022;9:23743735221103033. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.