Abstract
While hip arthroscopy (HA) has increased in recent years, limited data exists regarding utilization and outcomes among racial groups. The National Surgical Quality Improvement Program (NSQIP) database was queried for patients who underwent HA from 2006 to 2017. Patients were stratified into 6 self-reported racial/ethnic categories: White, African American, Hispanic, Asian and Pacific Islander, Native American, and Unknown. Major and minor complications in the 30-day post-operative period were identified. Data were available for 2230 patients who underwent HA. There were significant differences in the proportions of HA procedures when examining by race. White patients comprised 69% of the patient sample, African American patients 5.6%, Hispanic patients 3.9%, Asian patients 2.5%, Native American patients 0.7% and Unknown race/ethnicity patients 18.3% (P < .05). HA utilization increased significantly over time by all groups but remained low among ethnic minorities compared to the White cohort. Overall, major, and minor 30-day complication rates were 1.3%, 0.5%, and 0.9%, respectively. Although African American and Hispanic patients had higher overall complication rates than White patients, the differences were not statistically significant. Surgeons should be aware of the underutilization of HA among racial/ethnic minorities, and further studies evaluating insurance status and access to care are needed.
Keywords: hip arthroscopy, racial disparities, complications, healthcare utilization
What do we already know about this topic?
Hip arthroscopy utilization has increased in recent years, however limited data exists regarding utilization and outcomes among ethnic groups.
How does your research contribute to the field?
Our research increases awareness of the underutilization of hip arthroscopy among racial/ethnic minorities.
What are your research’s implications toward theory, practice, or policy?
By increasing awareness, our research may influence surgeons in their practice to increase utilization of hip arthroscopy when appropriate.
Introduction
The utilization of hip arthroscopy (HA) in the United States has been increasing over the past 2 decades. A study of insurance data from 2004 to 2009 demonstrated a 365% increase in HA utilization. 1 One of the largest HA utilization studies found that HA rates increased from 3.6 per 100 000 in 2005 to 16.7 per 100 000 in 2013 in privately insured and Medicare Advantage populations. 2 Given that this is a relatively new technique that is only recently being taught consistently across fellowships, some have attributed this rise in utilization to the increased number of new surgeons performing HA. A recent study showed an increase of nearly 600% in HA procedures being performed amongst American Board of Orthopaedic Surgical (ABOS) Part II Candidates from 2006 to 2010. 3
Several population-based studies of surgical outcomes after HA demonstrate low overall complications.2,4 -7 Independent risk factors for complications in the literature include regional/monitored anesthesia care, chronic corticosteroid use, and hypertension.5,8 Much less data exists pertaining to the impact of race/ethnicity on outcomes or utilization. Racial health disparities are vital to appreciate so that they may be addressed, giving access to high-quality care to all patients. Given that racial and ethnic minority patients have been shown to have both lower utilization and higher complication rates after orthopedic procedures compared to White patients, there is reason to suspect that HA may be similar.9 -14 The relationship between race/ethnicity and utilization or outcomes in healthcare is complex and involves multiple socio-economic determinants of health. Individual studies on racial health disparities can each only address a small component of this issue, with the broader goal being to address and alleviate these disparities.
The purpose of this study was to determine hip arthroscopy utilization and 30-day outcomes by race/ethnicity using the American College of Surgeons-National Surgical Quality Improvement Program (ACS-NSQIP) database from 2006 to 2017. The study hypotheses were that ethnic minority patients would (1) have lower utilization rates of HA and (2) have higher complication rates after hip arthroscopy.
Methods
Data Source and Study Population
NSQIP is a prospectively collected database from over 700 inpatient and outpatient facilities across the United States. Given that the database relies upon registered nurses specifically trained in NSQIP data collection, the data collection is likely more rigorous and accurate than that of administrative or claims-based databases.15 -17 More than 270 variables are tracked, including patient demographics, patient comorbidities, intraoperative variables, laboratory values, readmissions, and 30-day postoperative outcomes. 15
Patient Selection
Inclusion criteria included all patients who underwent HA from 2006 to 2017 in the ACS-NSQIP. HA patients were identified using the following Current Procedural Terminology codes: 29860, 29861, 29862, 29863, 29914, 29915, and 29916 (Table 1). Notably, CPT codes 29914, 29915, and 29916 were added in 2011. 18 To minimize outliers undergoing HA, we excluded patients who were more than 70 years of age, emergent surgery, pre-op wound infections, disseminated sepsis, disseminated cancer, ventilator dependency.
Table 1.
Hip Arthroscopy CPT Codes*.
| Code | Procedure listing |
|---|---|
| 29860 | Hip Arthroscopy, diagnostic, with or without synovial biopsy |
| 29861 | Hip Arthroscopy, removal of loose body or foreign body |
| 29862 | Hip Arthroscopy, chondroplasty, abrasion arthroplasty and/or resection of labrum |
| 29863 | Hip Arthroscopy, synovectomy |
| 29914 | Hip Arthroscopy, with femoroplasty |
| 29915 | Hip Arthroscopy, with acetabuloplasty |
| 29916 | Hip Arthroscopy, with labral repair |
CPT codes 29914, 29915, and 29916 were added in 2011. 19
Data Collection
Our primary independent variable of interest was race/ethnicity. Patients were stratified into 6 self-reported categories: White, African American, Hispanic, Asian or Pacific Islander, Native American, and Unknown. We recognize that the reporting of race and ethnicity is a complex endeavor and that patients may be of a particular race but may identify with a particular ethnicity (eg, African American patients of Hispanic ethnicity, White patients of Hispanic ethnicity). 20 To that extent, we decided to categorize patients into ethnicities rather than races per FDA definitions with the exception of Pacific Islanders who were grouped with Asians due to their small numbers included in the data sets and because they have been grouped together previously by the US Department of Labor.21,22 NSQIP also had a change in its “race” variable after the 2008 year in order to classify those patients who have a Hispanic ethnicity, but a different racial background. 23 We therefore categorized patients as “Hispanic” if they were classified as having a Hispanic ethnicity in the datasets regardless of race.
Peri-operative medical complications in the 30-day post-operative period after HA were categorized into minor and major complications in accordance with prior literature with minor adjustments.5,24 Organ space infections and reintubation were added to the major complication variable. The coma, graft failure, and peripheral injury complication variables were excluded from the analysis of NSQIP, as these variables are not accurate for any dataset after 2010 due to a change in coding structure. 15 Minor complications included renal insufficiency, pneumonia, bleeding requiring a blood transfusion, DVT, urinary tract infection, and superficial infection not requiring return to the operating room for operative debridement. Major complications included sepsis, septic shock, organ space infection, deep infection, wound dehiscence, return to the operating room, myocardial infarction, cardiac arrest, cerebrovascular accident, acute renal failure, pulmonary embolism, reintubation, being on a ventilator for more than 48 h, and death. Given the low complication rates, overall organ system complication variables were created to group similar complications as performed in prior studies.25,26 Pulmonary complications included pneumonia, reintubation, ventilator dependency greater than 48 h, and pulmonary embolism. Cardiac complications included myocardial infarction and cardiac arrest. Wound complications included superficial wound infection, deep wound infection, wound dehiscence, and organ space infection. Urinary complications included renal insufficiency, renal failure, and urinary tract infection. Septic complications included sepsis and septic shock. An overall complication variable was also created by combining all complication variables.
Patient demographics, clinical characteristics, process-of-care variables, and comorbidities were also obtained from the NSQIP database.
Statistical Analyses
HA utilization per year by ethnic group were calculated and graphed. A univariate analysis of the independent variable (ethnicity) by our outcomes of interest was performed by analysis of variance for continuous variables and by the χ2 or Fisher exact test for categorical variables. Data analysis was performed using SPSS version 26.0 (SPSS, Chicago, IL). All tests were two-sided, with statistical significance set at a probability value of .05 or less. Our institution granted an exemption from institutional review board approval for this study because NSQIP is a public, de-identified database.
Results
Patient Demographics
Over the study period, 2230 patients who underwent HA were included following application of the exclusion criteria. Of these, 1538 (69%) were White, 125 (5.6%) were African American, 87 (3.9%) were Hispanic, 56 (2.5%) were Asian/Pacific Islander, 15 (0.7%) were Native American, and 408 (18.3%) were Unknown. Differences in patient demographics/clinical characteristics are shown in Table 2. The White cohort had a relatively larger proportion of females compared to the other ethnicities (P < .05). Native Americans were older, had higher Body Mass Indices, and underwent surgery in an inpatient setting more frequently (all P < .05). African American patients had a larger proportion of patients (15.2%) with an American Society of Anesthesiologists (ASA) class of 3 to 4 compared to the other ethnic groups (P < .05).
Table 2.
Demographic/Clinical Characteristics and Process-of-Care Variables of Patients Undergoing Hip Arthroscopy by Ethnic Group (N = 2230). a
| Ethnicity | P | ||||||
|---|---|---|---|---|---|---|---|
| White | Black | Hispanic | Asian b | Native American | Unknown | ||
| (n = 1539) | (n = 125) | (n = 87) | (n = 56) | (n = 15) | (n = 408) | ||
| Demographic and Clinical Characteristics (%) | |||||||
| Sex | .002 | ||||||
| Female | 60.6% | 48.8% | 56.3% | 57.1% | 40.0% | 51.0% | |
| Male | 39.4% | 51.2% | 43.7% | 42.9% | 60.0% | 49.0% | |
| Age (years) | .012 | ||||||
| <29 | 24.8% | 21.6% | 28.7% | 28.6% | 13.3% | 30.6% | |
| 30-60 | 69.0% | 72.0% | 65.5% | 62.5% | 80.0% | 67.9% | |
| ≥61 | 6.2% | 6.4% | 5.7% | 8.9% | 6.7% | 1.5% | |
| BMI group (kg/m2) c | .014 | ||||||
| <18.5 | 2.0% | 1.6% | 1.1% | 5.4% | 0.0% | 1.0% | |
| 18.5-24.9 | 33.6% | 20.2% | 21.8% | 39.3% | 26.7% | 35.7% | |
| 25-29.9 | 35.4% | 42.7% | 43.7% | 39.3% | 20.0% | 37.9% | |
| 30-34.9 | 19.2% | 21.0% | 21.8% | 12.5% | 33.3% | 18.7% | |
| >35 | 9.7% | 14.5% | 11.5% | 3.6% | 20.0% | 6.7% | |
| Process of care variables (%) | |||||||
| ASA classification | <.001 | ||||||
| 1-2 | 89.1% | 84.8% | 89.7% | 92.9% | 86.7% | 95.8% | |
| 3-4 | 10.9% | 15.2% | 10.3% | 7.1% | 13.3% | 4.2% | |
| Procedure classification | |||||||
| Outpatient | 93.2% | 84.8% | 90.8% | 91.1% | 80.0% | 90.7% | .006 |
| Inpatient | 6.8% | 15.2% | 9.2% | 8.9% | 20.0% | 9.3% | |
Note. Items in boldface indicate significant differences (P < .05).
ASA = American Society of Anesthesiologists.
Percentages have been rounded and may not add to 100. bIncludes Pacific Islander.
BMI = weight. (kg)/height (m) 2 .
Differences in patient comorbidities are shown in Table 3. Overall, African American patients had a higher incidence of hypertension requiring medication and of having a pre-operative blood transfusion (both P < .05). Native Americans had a higher incidence of dyspnea and of diabetes (both P < .05). There were no other significant differences in comorbidities by ethnic group in our patient sample. The mean operative time was 99.51 min (mean standard deviation of 53.95 min); there were no significant differences in operative time among the ethnic groups.
Table 3.
Comorbidities of Patients Undergoing Hip Arthroscopy by Ethnic Group (N = 2230). a
| Demographic and clinical characteristics (%) | Ethnicity | P | |||||
|---|---|---|---|---|---|---|---|
| White | Black | Hispanic | Asian b | Native American | Unknown | ||
| (n = 1539) | (n = 125) | (n = 87) | (n = 56) | (n = 15) | (n = 408) | ||
| Cardiovascular | |||||||
| Congestive heart failure | 0.1% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | .994 |
| Hypertension requiring medication | 15.1% | 28.8% | 8.0% | 21.4% | 13.3% | 3.7% | .000 |
| Pulmonary | |||||||
| Current smoker | 20.0% | 20.8% | 14.9% | 16.1% | 40.0% | 15.7% | .085 |
| Dyspnea | 1.1% | 0.0% | 1.1% | 0.0% | 6.7% | 0.0% | .031 |
| COPD | 1.0% | 1.6% | 0.0% | 0.0% | 0.0% | 0.0% | .250 |
| Renal | |||||||
| Currently on dialysis | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | NA |
| Other | |||||||
| Weight loss (>10% in last 6 months) | 0.3% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | .814 |
| Diabetes | 4.0% | 7.2% | 4.6% | 3.6% | 20.0% | 1.7% | .002 |
| Alcohol use (>2 drinks/day) | 1.1% | 4.0% | 0.0% | 0.0% | 0.0% | 0.0% | .535 |
| Chronic corticosteroid use | 1.8% | 0.8% | 2.3% | 0.0% | 0.0% | 1.2% | .767 |
| Bleeding disorder | 0.6% | 1.6% | 0.0% | 0.0% | 0.0% | 0.2% | .538 |
| Pre-operative blood transfusion | 0.0% | 0.8% | 0.0% | 0.0% | 0.0% | 0.0% | .005 |
| Recent Surgery (within 30 days) | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | NA |
| Operative time | |||||||
| Mean (min) (total mean = 99.51 min) | 100.22 | 103.25 | 99.76 | 107.38 | 109.33 | 94.196 | .259 |
| SD ( total mean SD 53.95) | 56.28 | 59.68 | 48.51 | 50.70 | 56.81 | 43.45 | |
Note. Items in boldface indicate significant differences (P < .05).
NA = not applicable; SD = standard deviation.
Percentages have been rounded and may not add to 100.
Includes Pacific Islander.
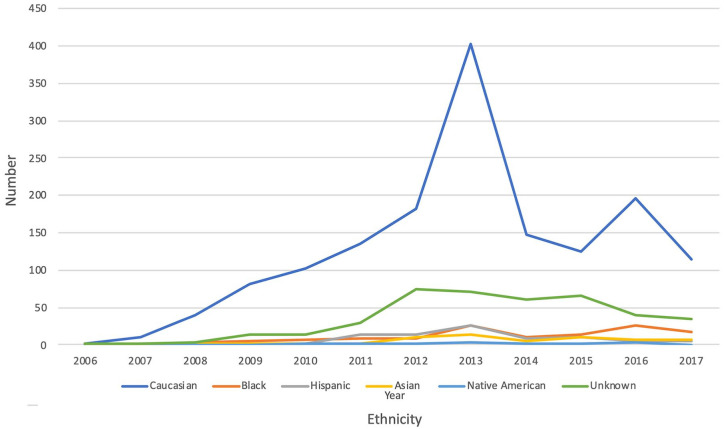
Utilization of Hip Arthroscopy by Race/Ethnicity
Regarding utilization rates, there was a significant increase in HA utilization over time in all ethnic groups from 2006 through 2013 (Figure 1). In the White cohort, there was a sharp decrease in the number of HA procedures starting in 2014 with a rise and then fall thereafter. Utilization of HA among ethnic minorities remained significantly lower throughout all years compared to its utilization in the White population. Utilization by ethnic minorities did not increase at the same rate as that of White patients (P < .05).
Figure 1.
Hip arthroscopy utilization by ethnicity from 2006 to 2017.
Complications of Hip Arthroscopy by Race/Ethnicity
The overall complication rate was 1.3%, with rates of major and minor complications of 0.5% and 0.9%, respectively (Table 4) The most common complications overall were return to the operating room (0.3%), bleeding requiring a blood transfusion (0.4%) and superficial wound infections (0.2%).
Table 4.
Univariate Analysis of Complications Undergoing Hip Arthroscopy by Ethnic Group (N = 2230).a
| Complications (n total, % total) | Ethnicity | P | |||||
|---|---|---|---|---|---|---|---|
| White | Black | Hispanic | Asian b | Native American | Unknown | ||
| (n = 1539) | (n = 125) | (n = 87) | (n = 56) | (n = 15) | (n = 408) | ||
| Major | |||||||
| Sepsis (n = 0, 0.0%) | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | NA |
| Septic shock (n = 1, 0.0%) | 0.1% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | .994 |
| Organ space infection (n = 1, ) | 0.1% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | NA |
| Deep infection (n = 2, 0.1%) | 0.1% | 0.8% | 0.0% | 0.0% | 0.0% | 0.0% | .177 |
| Wound dehiscence (n = 1, 0.0%) | 0.0% | 0.0% | 1.1% | 0.0% | 0.0% | 0.0% | .000 |
| Return to operating room (n = 6, 0.3%) | 0.3% | 0.8% | 0.0% | 0.0% | 0.0% | 0.2% | .882 |
| Myocardial infarction (n = 1, 0.0%) | 0.1% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | .994 |
| Cardiac arrest (n = 0, 0.0%) | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | NA |
| Cerebrovascular accident (n = 0, 0.0%) | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | NA |
| Acute renal failure (n = 0, 0.0%) | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | NA |
| Pulmonary embolism (n = 1, 0.0%) | 0.1% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | .994 |
| Reintubation (n = 1, 0.0%) | 0.1% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | .994 |
| Ventilator use >48 h (n = 0, 0.0%) | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | NA |
| Death (n = 1, 0.0%) | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.2% | .484 |
| Minor | |||||||
| Renal insufficiency (n = 0, 0.0%) | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | NA |
| Pneumonia (n = 2, 0.1%) | 0.0% | 0.0% | 1.1% | 0.0% | 0.0% | 0.0% | .970 |
| Bleeding requiring transfusion (n = 9, 0.4%) | 0.5% | 0.8% | 0.0% | 0.0% | 0.0% | 0.0% | .654 |
| Deep venous thrombosis (n = 3, 0.1%) | 0.2% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | .930 |
| Urinary tract infection (n = 3, 0.1%) | 0.1% | 0.8% | 0.0% | 0.0% | 0.0% | 0.0% | .430 |
| Superficial wound infection (n = 5, 0.2%) | 0.3% | 0.0% | 1.1% | 0.0% | 0.0% | 0.0% | .444 |
| Overall complications by organ system | |||||||
| Pulmonary complications (0 = 4, 0.2%) | 0.3% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | .876 |
| Cardiac complications (n = 1, 0.0%) | 0.1% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | .994 |
| Wound complications (n = 9, 0.4%) | 0.4% | 0.8% | 2.3% | 0.0% | 0.0% | 0.0% | .069 |
| Urinary complications (n = 3, 0.1%) | 0.1% | 0.8% | 0.0% | 0.0% | 0.0% | 0.0% | .430 |
| Septic complications (n = 1, 0.0%) | 0.1% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | .994 |
| Total major complications (n = 11, 0.5%) c | 0.4% | 1.6% | 1.1% | 0.0% | 0.0% | 0.5% | .471 |
| Total minor (n = 21, 0.9%) c | 1.2% | 1.6% | 1.1% | 0.0% | 0.0% | 0.0% | .303 |
| Any complication (n = 30, 1.3%) c | 1.4% | 3.2% | 2.3% | 0.0% | 0.0% | 0.5% | .211 |
Note. Items in boldface indicate significant differences (P < .05).
Pulmonary complications: pneumonia, reintubation, ventilator dependency >48 h, pulmonary embolism. Cardiac complications: myocardial infarction and cardiac arrest. Wound complications: superficial wound infection, deep wound infection, wound dehiscence, organ space infection. Urinary complications: renal insufficiency, renal failure, and urinary tract infection. Septic complications included sepsis and septic shock.
NA = not applicable.
Percentages have been rounded and may not add to 100.
Includes Pacific Islander.
Refers to number of patients having at least 1 complication. Thus if a patient had 2 complications, for example, the patient is only counted once in this total.
On univariate analyses (Table 4), there were no significant differences in pulmonary, cardiac, wound, urinary, septic, major, minor, and overall complication rates by ethnic group (all P > .05). There was no significant difference for the overall wound complication incidence by ethnic group as shown in Table 4 (P = .069).
Although not statistically significant, African American and Hispanic patients had a higher incidence of overall complications compared to the White cohort and the overall population average (Table 4). The incidence of major complications was 0.4% for Whites and 0.5% for the entire cohort, whereas it was 1.6% and 1.1% for African American and Hispanic patients, respectively (P = .471). Similarly, the overall complication incidence was 1.4% for Whites and 1.3% for the entire cohort, whereas it was 3.2% and 2.3% for African American and Hispanic patients, respectively (P = .211).
Discussion
Our study contributes to the current literature both by demonstrating that there are discrepancies in the rate of HA utilization by ethnic minority groups and by examining differences in post-operative complications by ethnic minority groups.
Over the last several years, HA utilization has increased significantly.1 -3,5,6 Our study is in concordance with these studies, as we demonstrated a substantial increase in HA utilization by all ethnic groups, particularly from 2006 to 2013 (Figure 1). A decrease in number of HAs for all ethnic groups after 2014 may reflect a shift in procedures being performed at ambulatory surgery centers, which NSQIP does not capture.15,23 However, overall utilization continues to rise. This is consistent with a prior study that showed an increase in HA surgeries being performed at ambulatory surgery centers (ASCs) around this time period (3.06% in 2007% vs 20.45% in 2015). 27 That study compared patients undergoing HA at ASCs versus hospital-based outpatient departments and showed no statistically significant differences for in complications, readmissions, visits to the emergency department, and re-operations. This suggests that HAs performed at ASCs may have similar surgical safety outcomes as those performed in the hospital setting.
The racial composition of the hip arthroscopy cohort in the present study may be compared to the racial composition of NSQIP to illustrate utilization rates overall. NSQIP is a large multi-institutional database that provides patient data from 708 hospitals across the United States, whose outcome measures have been shown to be generalizable to the United States population.15 -17,23 According to the United States Census Bureau, it is estimated that in 2019, 60.4% of the United States population was White, 13.4% African American, 18.3% Hispanic, 6.1% Asian/Pacific Islander, and 1.3% Native American. 28 This is in contrast to our patient sample in which 69% were White, 5.6% African American, 3.9% Hispanic, 2.5% Asian/Pacific Islander, 0.7% Native American, and 18.3% were Unknown. If the cohort were to be excluded from our analysis, the cohort would be even more unrepresentative of the current United States ethnic distributions with 84.5% White, 6.9% African American, 4.8% Hispanic, 3.1% Asian, and 0.8% Native American. To the best of our knowledge, only 2 prior large studies have investigated hip arthroscopy utilization by year.2,6 Although these studies collected demographic data including ethnicity/race, which demonstrated similar underutilization by ethnic minorities as our study, neither reported a comparison between postoperative complications and ethnicity.
Similar to prior studies using the NSQIP database, the overall complication rate after hip arthroscopy found in our study was low. 5 Our study did not show significant differences in complication rates by ethnic groups; however, African American and Hispanic patients did have a non-significantly higher rate of major complication than White patients as seen in Table 4. (1.6% and 1.1% vs 0.4%, P > .05). Part of this difference in complication rate for African American patients included in our study may be explained by the significantly higher prevalence of hypertension requiring medication, diabetes, and a higher ASA classification compared to the White cohort (Tables 2 and 3). However, it is difficult to analyze surgical outcomes in the context of race/ethnicity due to the multi-dimensional role that race/ethnicity plays in influencing socioeconomic status, access to educational opportunities, access to medical care, and the subsequent feedback effect that these forces can have on health. It is crucial to not assume that one race is genetically or culturally predisposed to worse outcomes or decreased utilization. Despite considerable prior investigation, evidence regarding ethnic differences in hip bone morphology and subsequent need for intervention does not have good consensus, and thus it is difficult to draw conclusions on how this may influence HA utilization by ethnicity.29 -32
Worse outcomes and decreased utilization seen in orthopedic patients likely reflect social determinants of health that are differentially experienced by patients of different races/ethnicities on average. In 2013, it is estimated that 40.5% of Hispanic patients and 25.8% of African American patients were uninsured compared to 14.8% of White patients.10,11,14,33,34 Although the implementation of the Affordable Care Act (ACA) reduced the number of uninsured patients in the United States, substantial ethnic disparities remain. 35 Among many studies on race, insurance status, and health care disparities seen in the literature, Schairer et al found that non-white race and public insurance were independently associated with lower rates of meniscus surgery. 36 Although the ACA has reduced the number of uninsured patients, discrepancies in access to orthopedic sports medicine care remain. A 2017 study by Wiznia et al demonstrated that patients with Medicaid were more likely to be denied appointments and experience longer wait times than privately insured patients at orthopedic sports medicine practices, even after implementation of the ACA. 37 Therefore, it is more likely that the underutilization of HA by ethnic minority populations is related to complex socio-economic factors in the United States including the high prevalence of uninsured and underinsured patients within these populations in the United States.
Of note, we elected not to perform multivariate logistic regression analyses as a study by Cvetanovich et al has previously reported on the independent risk factors for complications after hip arthroscopy using NSQIP files from 2006 to 2013. 5 Furthermore, a multivariate logistic regression analysis in our study would have shown that ethnicity was not a significant predictor of post-operative medical complications after HA, since our univariate analyses demonstrated no significant differences in medical complications based on ethnicity, with the exception of wound dehiscence (Table 4). Although the wound dehiscence complication was statistically significant, only one patient had a wound dehiscence complication, making the finding not of clinical relevance. Our paper adds to the work by Cvetanovich et al by specifically reporting on the utilization rates and surgical outcomes by ethnic group and by surveying an additional 4 years of data, making it one of the largest studies to date on HA outcomes by ethnicity. 5
This study is not without limitations. Though NSQIP is used extensively in the orthopedic literature, the database focuses primarily on general surgery outcomes, with less focus on orthopedic-specific outcome measures. 38 Therefore, certain orthopedic complications that are common to HA, such as neuropraxia or heterotopic ossification, are not available in the data sets. The data set also does not include patients at ambulatory surgery centers. In addition, NSQIP does not report on insurance status, socioeconomic status, surgeon volume, academic status of hospitals, costs, or outcomes beyond 30-days. This limited the authors’ ability to identify the underlying reasons behind racial disparities in utilization. There was a large proportion of patients (18.3%) whose ethnicity was not recorded.
In conclusion, hip arthroscopy utilization has increased significantly over the past 2 decades in the White population, but its utilization has remained low among racial and ethnic minorities. In our study, there were no statistically significant differences in complication rates based on race, despite African American and Hispanic patients having a non-significantly higher percentage of perioperative complications. Surgeons should be aware of the underutilization of hip arthroscopic procedures in the racial and ethnic minorities. Underutilization and disparities in access to specialized surgeries such as hip arthroscopy are likely due to multiple complex factors related to socioeconomic inequities and barriers to care. Future goals related to this topic include conducting larger studies that take into consideration insurance status, socioeconomic status, and orthopedic-specific complications of hip arthroscopy to further elucidate the etiology of disparate access to care. This will facilitate the most important goal—reducing racial health disparities in hip arthroscopy and orthopedic surgery.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Shaan Sadhwani  https://orcid.org/0000-0002-5635-943X
https://orcid.org/0000-0002-5635-943X
References
- 1. Montgomery SR, Ngo SS, Hobson T, et al. Trends and demographics in hip arthroscopy in the United States. Arthroscopy. 2013;29(4):661-665. [DOI] [PubMed] [Google Scholar]
- 2. Maradit Kremers H, Schilz SR, Van Houten HK, et al. Trends in utilization and outcomes of hip arthroscopy in the United States between 2005 and 2013. J Arthroplasty. 2017;32(3):750-755. [DOI] [PubMed] [Google Scholar]
- 3. Bozic KJ, Chan V, Valone FH, Feeley BT, Vail TP. Trends in hip arthroscopy utilization in the United States. J Arthroplasty. 2013;28(8 Suppl):140-143. [DOI] [PubMed] [Google Scholar]
- 4. Ashberg L, Walsh JP, Yuen LC, Perets I, Chaharbakhshi EO, Domb BG. Outcomes of hip arthroscopy in adolescents: A comparison of acute versus chronic presentation. Two-year minimum follow-up. J Pediatr Orthop. 2018;38(2):e50-e56. [DOI] [PubMed] [Google Scholar]
- 5. Cvetanovich GL, Chalmers PN, Levy DM, et al. Hip arthroscopy surgical volume trends and 30-day postoperative complications. Arthroscopy. 2016;32(7):1286-1292. [DOI] [PubMed] [Google Scholar]
- 6. Degen RM, Bernard JA, Pan TJ, et al. Hip arthroscopy utilization and associated complications: a population-based analysis. J Hip Preserv Surg. 2017;4(3):240-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Griffin DW, Kinnard MJ, Formby PM, McCabe MP, Anderson TD. Outcomes of hip arthroscopy in the older adult: a systematic review of the literature. Am J Sports Med. 2017;45(8):1928-1936. [DOI] [PubMed] [Google Scholar]
- 8. Hartwell MJ, Morgan AM, Johnson DJ, et al. Risk factors for 30-day readmission following hip arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2020;28(4):1290-1295. [DOI] [PubMed] [Google Scholar]
- 9. Clohisy JC, Nunley RM, Carlisle JC, Schoenecker PL. Incidence and characteristics of femoral deformities in the dysplastic hip. Clin Orthop Relat Res. 2009;467(1):128-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zhang W, Lyman S, Boutin-Foster C, et al. Racial and ethnic disparities in utilization rate, hospital volume, and pPerioperative outcomes after Total Knee Arthroplasty. J Bone Jt Surg. 2016;98(15):1243-1252. [DOI] [PubMed] [Google Scholar]
- 11. Dy CJ, Lane JM, Pan TJ, Parks ML, Lyman S. Racial and socioeconomic disparities in hip fracture care. J Bone Joint Surg Am. 2016;98(10):858-865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Elsharydah A, Embabi AS, Minhajuddin A, Joshi GP. Racial isparity in the erioperative are for atients ndergoing otal nee and ip arthroplasty: a retrospective propensity-matched cohort study. J Racial Ethn Health Disparities. 2018;5(3):632-637. [DOI] [PubMed] [Google Scholar]
- 13. Liu JH, Zingmond DS, McGory ML, et al. Disparities in the utilization of high-volume hospitals for complex surgery. JAMA. 2006;296(16):1973-1980. [DOI] [PubMed] [Google Scholar]
- 14. Nwachukwu BU, Kenny AD, Losina E, Chibnik LB, Katz JN. Complications for racial and ethnic minority groups after total hip and knee replacement. J Bone Jt Surg. 2010;92(2):338-345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. American College of Surgeons. ACS-NSQIP: User Guide for the 2017 Participant Use Data File. American College of Surgeons; 2018:1-20. [Google Scholar]
- 16. Cima RR, Lackore KA, Nehring SA, et al. How best to measure surgical quality? Comparison of the Agency for Healthcare Research and Quality Patient Safety Indicators (AHRQ-PSI) and the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) postoperative adverse events at a single institution. Surgery. 2011;150(5):943-949. [DOI] [PubMed] [Google Scholar]
- 17. Davenport DL, Holsapple CW, Conigliaro J. Assessing surgical quality using administrative and clinical data sets: a direct comparison of the University HealthSystem Consortium Clinical Database and the National Surgical Quality Improvement Program data set. Am J Med Qual. 2009;24(5):395-402. [DOI] [PubMed] [Google Scholar]
- 18. 2011 CPT code updates. Accessed March 10, 2024. https://www.aaos.org/aaosnow/2011/Feb/managing/managing1/.
- 19. Brand JC, Rossi MJ, Lubowitz JH. Hip arthroscopy complications are rare, but there is room for improvement. Arthroscopy. 2019;35(5):1297-1299. [DOI] [PubMed] [Google Scholar]
- 20. Leopold SS, Beadling L, Calabro AM, et al. Editorial: the Complexity of reporting race and ethnicity in orthopaedic research. Clin Orthop. 2018;476(5):917-920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. OFCCP. | U.S. Department of Labor. Accessed March 10, 2024. https://www.dol.gov/agencies/ofccp.
- 22. Center for Devices and Radiological Health. Evaluation and Reporting of Age-, Race-, and Ethnicity-Specific Data in Medical Device Clinical Studies. U.S. Food and Drug Administration; 2019. Accessed March 10, 2024. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/evaluation-and-reporting-age-race-and-ethnicity-specific-data-medical-device-clinical-studies [Google Scholar]
- 23. American College of Surgeons. ACS-NSQIP: User Guide for the 2008 Participant Use Data File. American College of Surgeons; 2009. [Google Scholar]
- 24. Martin CT, Pugely AJ, Gao Y, Wolf BR. Risk factors for thirty-day morbidity and mortality following knee arthroscopy: a review of 12,271 patients from the national surgical quality improvement program database. J Bone Joint Surg Am. 2013;95(14):e98 1-e9810. [DOI] [PubMed] [Google Scholar]
- 25. Buerba RA, Fu MC, Gruskay JA, Long WD, Grauer JN. Obese Class III patients at significantly greater risk of multiple complications after lumbar surgery: an analysis of 10,387 patients in the ACS NSQIP database. Spine J. 2014;14(9):2008-2018. [DOI] [PubMed] [Google Scholar]
- 26. Buerba RA, Giles E, Webb ML, Fu MC, Gvozdyev B, Grauer JN. Increased risk of complications after anterior cervical discectomy and fusion in the elderly: an analysis of 6253 patients in the American College of Surgeons National Surgical Quality Improvement Program database. Spine. 2014;39(25):2062-2069. [DOI] [PubMed] [Google Scholar]
- 27. Qin C, Lee C, Ho S, Koh J, Athiviraham A. Complication rates following hip arthroscopy in the ambulatory surgical center. J Orthop. 2020;20:28-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. U.S. Census Bureau QuickFacts: United States. Accessed March 10, 2024. https://www.census.gov/quickfacts/fact/table/US/PST045222.
- 29. Clohisy JC, Baca G, Beaulé PE, et al. Descriptive epidemiology of femoroacetabular impingement: a North American cohort of patients undergoing surgery. Am J Sports Med. 2013;41(6):1348-1356. [DOI] [PubMed] [Google Scholar]
- 30. Mosler AB, Crossley KM, Waarsing JH, et al. Ethnic differences in bony hip morphology in a cohort of 445 professional male soccer players. Am J Sports Med. 2016;44(11):2967-2974. [DOI] [PubMed] [Google Scholar]
- 31. Rhyu KH, Chun YS, Jung GY, Cho YJ. Age and sex-related distribution of alpha angles and the prevalence of the cam morphology of the hip in Asians do not differ from those of other ethnicities. Knee Surg Sports Traumatol Arthrosc. 2019;27(10):3125-3132. [DOI] [PubMed] [Google Scholar]
- 32. Tannenbaum E, Kopydlowski N, Smith M, Bedi A, Sekiya JK. Gender and racial differences in focal and global acetabular version. J Arthroplasty. 2014;29(2):373-376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Yin C, Sing DC, Curry EJ, et al. The effect of race on early perioperative outcomes after shoulder arthroplasty: a propensity score matched analysis. Orthopedics. 2019;42(2):95-102. [DOI] [PubMed] [Google Scholar]
- 34. Sanford Z, Taylor H, Fiorentino A, et al. Racial disparities in surgical outcomes after spine surgery: an ACS-NSQIP analysis. Glob Spine J. 2019;9(6):583-590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Buchmueller TC, Levinson ZM, Levy HG, Wolfe BL. Effect of the affordable care act on racial and ethnic disparities in health insurance coverage. Am J Public Health. 2016;106(8):1416-1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Schairer WW, Nwachukwu BU, Lyman S, Allen AA. Race and insurance status are associated with surgical management of isolated meniscus tears. Arthrosc J Arthrosc Relat Surg. 2018;34(9):2677-2682. [DOI] [PubMed] [Google Scholar]
- 37. Wiznia DH, Nwachuku E, Roth A, et al. The influence of medical insurance on patient access to orthopaedic surgery sports medicine appointments under the affordable care act. Orthop J Sports Med. 2017;5(7):2325967117714140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Schilling PL, Hallstrom BR, Birkmeyer JD, Carpenter JE. Prioritizing perioperative quality improvement in orthopaedic surgery. J Bone Joint Surg Am. 2010;92(9):1884-1889. [DOI] [PubMed] [Google Scholar]