Abstract
Background
Vaccine hesitancy and resistance pose significant threats to controlling pandemics and preventing infectious diseases. In a group of individuals unvaccinated against the disease caused by the SARS-CoV-2 coronavirus (COVID-19), we investigated how age, intolerance of uncertainty (IU), and their interaction affected the likelihood of having changed one’s vaccination decision a year later. We hypothesized that higher IU would increase the likelihood of becoming vaccinated, particularly among individuals of younger age. We predicted that this effect would remain significant, even after controlling for delay discounting and trust in science.
Purpose
The goal of this research was to understand the factors influencing changes in vaccination decisions among the vaccine hesitant.
Methods
In a larger longitudinal study, ~7,500 participants from Prolific.co completed demographic and vaccination status questions, a delay discounting task, and the Intolerance of Uncertainty Scale in June–August 2021. Approximately 3,200 participants completed a follow-up survey in July–August 2022, answering questions about vaccination status, reasons for vaccination decision, and trust in science. We analyzed data from 251 participants who initially had no intention of getting vaccinated and completed the follow-up survey; 38% reported becoming vaccinated in the intervening year.
Results
Data were analyzed using multilevel logistic regression. Over and above other factors related to vaccination decisions (delay discounting, trust in science), younger participants were more likely to change their decision and become vaccinated a year later, especially if they had higher IU, confirming our predictions. Primary reasons for becoming vaccinated were necessity and seeking protection against the virus.
Conclusions
These findings highlight the complex interplay between age, uncertainty, and vaccination decisions, and inform health policies by suggesting the need for tailoring interventions to specific concerns in different age groups.
Keywords: Intolerance of uncertainty, Public health measures, Vaccination, Vaccine hesitancy, COVID-19
Individuals who indicated that they had no intention of getting vaccinated against COVID-19 were more likely to change their mind if they were younger in age and had higher intolerance of uncertainty.
Introduction
Widespread vaccination has been critical to containing the COVID-19 pandemic [1] as well as other infectious diseases [2], but efforts have been threatened by vaccine hesitancy and resistance [3, 4]. Research on predictors of COVID-19 vaccination has considered effects of various factors, including environmental factors (e.g., government regulations and COVID-19 impact severity) [5], and at the level of the individual, both immutable variables (e.g., demographic and personality variables) [6–9], and potentially modifiable variables including psychological (e.g., anxiety and depression) [10] and cognitive mechanisms (e.g., trust in science and delay discounting) [11–13]. Although the intention-behavior relationship has not been empirically demonstrated for all of the public health measures recommended during the COVID-19 pandemic [14], research shows that most, but not all, individuals tend to follow through on their vaccination intentions [15]. From a public health perspective, as protective behaviors become increasingly optional and responsibility for long-term immunity maintenance shifts from official mandates to individual decision-making, it is necessary to identify the factors that contribute to change in people’s attitudes, intentions, and behaviors towards vaccines and boosters—particularly in those who are vaccine hesitant. The current longitudinal study investigated whether two factors known to influence health intentions and behaviors—intolerance of uncertainty (IU) and age—predicted decisions to be vaccinated in adults who were initially vaccine hesitant. Understanding the factors contributing to how working-aged adults change their minds about vaccination during a pandemic is crucial for supporting safe return to work (including essential occupations) and school as well as social activities.
The pandemic significantly increased uncertainty in many aspects of life. The sudden and widespread outbreak of COVID-19 caused global disruptions affecting healthcare, employment, education, and social interactions. The rapidly changing nature of the virus [16] and the subsequent implementation of various containment measures such as lockdowns and travel restrictions, created a sense of unpredictability and ambiguity [17–19]. Constantly evolving information, conflicting reports, and misinformation surrounding the effectiveness of preventive measures further contributed to the heightened sense of uncertainty experienced by individuals and communities worldwide [20]. IU, a cognitive bias marked by a fear of, and reduced ability to handle, the unknown [21], is an important factor in understanding the process of behavior change when it comes to overcoming vaccine hesitancy. The construct of IU has recently captured a lot of attention in clinical psychology [22, 23], as it is recognized as global trait that may serve as a transdiagnostic risk factor for emotional psychopathology [24] and emerging IU-focused interventions aim to increase people’s tolerance of uncertainty (e.g., through mindfulness and exposure therapy [25]). IU is composed of two factors: prospective anxiety that captures cognitive components related to uncertainty and inhibitory anxiety that captures certain safety behaviors associated with encountering uncertainty (e.g., avoidance). Interestingly, IU is associated with two potential behavioral outcomes with respect to vaccination. One is to reduce or eliminate the source of uncertainty. There is evidence that higher IU is associated with a higher likelihood of engaging in public health measures as a strategy to mitigate fears of the virus itself [20]. The tendency to engage in coping behaviors, such as checking, repeating, and excessively preparing, with the intention to enhance one’s perceived control over a given situation and reduce anxiety, is also well-documented in the literature [26, 27].
On the contrary, others have reported that, despite higher distress about COVID-19, those with higher IU are less likely to get vaccinated due to heightened fears and concerns about unknown risks and efficacy of the vaccine [28]. Gillman et al. [29] similarly report that lower tolerance of ambiguity is associated with vaccine hesitancy, again likely because of uncertainty around efficacy. This phenomenon, known as “uncertainty paralysis” [30], represents another type of coping behavior—avoidance—that has been well-researched in relation to worry and anxiety [31]. Such behavioral avoidance has been found to be predicted by cognitive inflexibility during times of increased uncertainty [32].
In the context of vaccination, two constructs related to IU are trust in science (i.e., the extent to which one trusts in scientists and scientific findings related to vaccines) [11] and delay discounting (i.e., a near-universal tendency to favor smaller immediate rewards over large later rewards) [12]. A previously established negative relationship between uncertainty and trust in health information about COVID-19 [29] suggests that increased IU may be associated with lower trust in science. IU was also found to be positively correlated with delay discounting [33]. It was reasoned that delayed rewards are uncertain, and therefore would require greater tolerance of uncertainty [33, 34].
The factors that determine whether someone with high IU is more likely to engage in behaviors such as vaccination in an effort to reduce feelings of uncertainty or instead become paralyzed and remain unvaccinated remain unclear. Age may be critical to understanding the relation of IU to vaccination decisions under these circumstances. Although younger adults generally show more resistance to vaccination than their older counterparts [35], and COVID-19 vaccination rates are lower amongst younger adults [36], there is also evidence that younger adults tend to be more open [37] and more encouraged [38] to change their health-related behaviors. Moreover, when faced with emotionally salient situations, younger age is associated with increased use of problem-solving strategies to regulate emotions by managing or eliminating the stressor itself [39]. Taken together, we hypothesize that unvaccinated individuals of younger age with higher IU would be more likely to change their mind and decide to get vaccinated as a means to reduce or eliminate their experience of COVID-related uncertainty.
When faced with emotionally salient situations, older age is associated with increased use of passive or avoidant-denial coping strategies [40]. Coupled with less flexibility in the selection of coping strategies [41], it is likely that, as one gets older, higher IU becomes increasingly associated with an avoidant response such as uncertainty paralysis. Therefore, even though age has been one of the most salient clinical indicators monitored in relation to the risk of SARS-CoV-2 exposure [42] and infection [43–45], severity of illness [46], and vaccine availability, we predict that with increasing age, unvaccinated individuals with higher IU would be less likely to decide to become vaccinated.
Given that IU is a trait-like variable and may not tell us about the specific source of uncertainty contributing to health-related decisions during the pandemic, it is important to also qualitatively assess reasons for vaccination decisions. There are several sources of uncertainty that may contribute to decisions to get vaccinated, including mandates (e.g., requirements for work or school), trust in science (e.g., skepticism about vaccine effectiveness), concerns about health, and possible side effects (of both vaccination and contracting the virus).
In the current study, we examined data from a subsample of a large longitudinal survey [13], focusing on an adult sample of individuals aged 18 to 69 years who reported being unvaccinated against SARS-CoV-2 in mid-2021. We investigated whether, a year later, they had changed their mind and were vaccinated, and whether IU and age measured at Time 1 interacted to predict change in vaccination status over time, after controlling for two variables related to vaccination decisions: delay discounting [12, 13, 47] and trust in science [11]. We hypothesized that higher IU would be associated with a higher likelihood of changing minds about vaccination with younger age, while the reverse association would be evident with older age.
Methods
Study methods and results are reported following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement for cross-sectional studies [48]. The study was not pre-registered.
Participants
Participants were recruited to participate in a larger study through an online platform (Prolific.co). At Time 1 (July–August, 2021), we aimed to recruit as many participants as possible to ensure a large enough sample of participants who might remain unvaccinated over time. The final Time 1 sample comprised 6,926 participants from 13 countries [12, 13]; n = 2,890 indicated that they were fully vaccinated, 1,465 that they were partially vaccinated, 2,012 that they were not vaccinated yet but were planning to get vaccinated in the future, and 559 that they were unvaccinated and did not intend to get vaccinated in the future.
At Time 2, approximately one year later (July–August, 2022), all participants in the final sample of the larger study were invited to complete a follow-up survey. Of the 3,185 who participated a year later, a subset of individuals (n = 251) had indicated at Time 1 that they had no intention to get vaccinated in the future. Of this sub-sample, 38% reported being vaccinated at Time 2.
Participants provided demographic information at Time 1. For the sub-sample reported here, mean age was 31.93 years old (SD = 10.60); 127 self-identified as female, 124 as male, and 0 as non-binary. Approximately 24% of the sample were residing in the USA, 15% in Poland, 9% in the UK, 8% in Italy, 7% in Canada, 7% in Australia, 6% in Spain, 5% in France, 5% in Mexico, 4% in Germany, 4% in New Zealand, 4% in Portugal, and 1% in the Netherlands. Given the internationality of our sample, we used a subjective measure of relative income where participants estimated their current income relative to others in their own country/region on a sliding scale (0 = low, 50 = average, 100 = high [49, 50]). Average subjective relative income was 37.88 (SD = 21.10). Approximately 20% of our sample self-identified as essential workers in occupations supplying critical services during the pandemic: government; health and safety (e.g., healthcare and emergency response); utilities (e.g., water, energy, sanitation, transport, and communications); food (e.g., supermarkets); and manufacturing. In terms of the highest level of education, 38% of the sample reported having a high school education, 47% a university degree (undergraduate degree or professional equivalent), and 15% a postgraduate degree.
We also examined the demographic characteristics of individuals who at Time 1 expressed no intention to get vaccinated and were invited to participate at Time 2 but chose not to (Supplementary Table S1). Individuals who returned to participate in the study at Time 2 (M = 31.93, SD = 10.60) were significantly older than individuals who did not return to participate at Time 2 (M = 28.50, SD = 9.50). No other significant differences in demographic variables were observed between those who returned to participate in Time 2 of the study and those who did not.
Measures
Intolerance of uncertainty scale-12 ([51])
The intolerance of uncertainty scale-12 (IUS-12) is a 12-item measure of one’s difficulties tolerating uncertainty (e.g., “I always want to know what the future has in store for me”). Participants provided responses to items on a six-point scale (0 = Not at all characteristic of me; 5 = Entirely characteristic of me). The IU score was the sum of participants’ responses to the 12 items, ranging from 0 to 60; the average score was 34.27 (SD = 9.61). The scale demonstrated acceptable internal consistency (omega hierarchical = 0.84; Supplementary Materials).
Vaccination status
Participants were asked to indicate their vaccination status at both Time 1 and Time 2. Participants chose between five options in response to the question about their vaccination status: 1 = yes, I have received all necessary doses, 2 = yes, although I require another dose, 3 = no, but I am planning to get vaccinated, 4 = no, I am not planning to get vaccinated, 5 = prefer not to say. As described earlier, only participants with a Time 1 response of 4 (“no, I am not planning to get vaccinated”) were included in this study. From their responses to this question at Time 2, a binary vaccination status variable was created as the primary outcome variable, distinguishing between those who were vaccinated (fully or partially) or not (including both those who were planning and not planning to get vaccinated in the future).
Reasons for vaccination
At Time 2, participants had the opportunity to explain their reason(s) for their decision to be vaccinated or not. We first examined the full corpus of responses in the larger study to identify the main reasons mentioned by participants. Reasons for getting vaccinated (or not) were: (i) ending the pandemic (e.g., “it will stop the virus”), (ii) protecting oneself or others from COVID-19 (e.g., “to protect myself and my family”), (iii) (non-) necessity (e.g., “I had to in order to continue being enrolled in college”), (iv) trust (in science, government, or vaccines; e.g., “don’t trust the vaccine”), (v) vaccine availability, (vi) health reasons (e.g., “medical complications,” “side effects”), or (vii) other (e.g., “afraid of needles”). These categories were then used to classify each participant response provided by the current sub-sample; if multiple reasons were mentioned, the most prominent reason was scored. To establish the inter-rater reliability of this classification, the lead rater (S.F.C) and two additional raters (R.T. and W.F.) independently classified 100 responses randomly selected from the larger study. Raters had 84–86% agreement on their categorizations of responses, and acceptable inter-rater reliability (Cohen’s Kappa ranged from = 0.79–0.81). S.F.C. then scored all of the responses from the participants reported on in this paper.
Trust in science
We used two items designed to measure trust in scientific institutions by asking participants to indicate their confidence in science and in scientists on a scale from 0 = “no confidence at all” to 10 = “a lot of confidence” [52]. Ratings on the two items were added together into a single composite Trust in Science variable.
Delay discounting
In this intertemporal choice procedure [12, 13, 53, 54], participants viewed pairs of monetary amounts and were asked to choose between smaller, immediate rewards which varied between trials, and a larger, delayed reward of $2,000. Participants were asked to make six choices at each of seven delays for the larger reward (waiting 1 week, 1 month, 3 months, 6 months, 1 year, 3 years, and 10 years before receiving the $2,000 reward). An iterative, adjusting-amount procedure was used in which the amount of the immediate reward was increased or decreased based on the participant’s previous choice at that delay, converging on the amount of the immediate reward equivalent in subjective value to the delayed reward. Degree of discounting was measured by examining the subjective values of reward across the seven delays and computing Area-under-the-Curve (AuC), a single, theoretically-neutral measure of discounting [55]. The scores range from 0 to 1, with lower AuC representing a greater discounting rate (i.e., greater tendency to choose smaller immediate rewards over larger later rewards).
Attention checks
To identify random responders, three items from the Conscientious Responder Scale [56] were included at select points within the survey at Time 1 (e.g., “To answer this question, please choose option three, neither agree nor disagree”). At Time 2, only one item was used given that the survey was much shorter. None of the participants in the current subsample failed the attention check.
Procedure
Data were collected longitudinally using two online Qualtrics surveys as part of a larger study. At Time 1, participants provided informed consent and, among other measures (see Halilova et al., [12, 13]), provided demographic information (including age and country of residence), completed the IUS-12 [51] and the delay discounting task, and answered questions about their COVID-19 vaccination status. At Time 2, participants completed a series of COVID-related questions, including vaccination status and their reasons for their vaccination decision, as well as questions regarding their trust in science.
Statistical Analysis
We computed Pearson’s product moment correlations between the variables of interest. Multilevel logistic regression models were constructed using R packages lme4 [57] and lmerTest [58]. First, we constructed the model with vaccination status at Time 2 (unvaccinated vs. vaccinated) as the outcome variable, and age (Time 1), IUS-12 (Time 1), and age × IUS-12 interaction as predictors. Each participant’s vaccination status at Time 2 (Level 1) was nested within country (Level 2) to account for possible systematic differences across countries. A likelihood ratio test showed that the model including age × IUS-12 interaction accounted for significantly more variance in the data compared to an intercept-only model, χ2(3)= 16.91, p < .001. The model was then expanded to include AuC (Time 1) and Trust in Science (Time 2) as covariates to test whether the age × IUS-12 interaction remains significant after controlling for these variables.
Results
Descriptive Statistics
Of those who completed Time 2 (n = 251), 38% reported that they were now vaccinated. Descriptive statistics for the key variables of interest are presented in Table 1, broken down by vaccination status. Supplementary Figure S1 shows the distribution of age across the sample. The correlations between the variables are reported in Table 2.
Table 1.
Descriptive Statistics for Variables of Interest
| Vaccinated | Unvaccinated | |
|---|---|---|
| n | 95 | 156 |
| Mean age (years) | 29.52 (9.79) | 33.40 (10.83) |
| Age range (years) | 18–69 | 18–64 |
| Mean IUS-12 score | 35.89 (9.21) | 33.28 (9.75) |
| IUS-12 range | 15–59 | 12–58 |
| Mean AuC | 0.36 (0.27) | 0.40 (0.25) |
| AuC range | 0.01–0.99 | 0.01–0.99 |
| Mean Trust in Science score | 13.79 (4.07) | 11.03 (4.97) |
| Trust in Science range | 0–20 | 0–20 |
Standard deviation is shown in parentheses. AuC = Area-under-the-Curve; and IUS-12 = Intolerance of Uncertainty Scale-12.
Table 2.
Correlations Between Variables of Interest
| IUS-12 | Age | AuC | |
|---|---|---|---|
| IUS-12 | – | ||
| Age | −0.17 | – | |
| AuC | −0.06 | −0.11 | – |
| Trust in Science | 0.04 | −0.28 | −0.06 |
AuC = Area-under-the-curve; and IUS-12 = Intolerance of Uncertainty Scale-12.
Vaccination Status
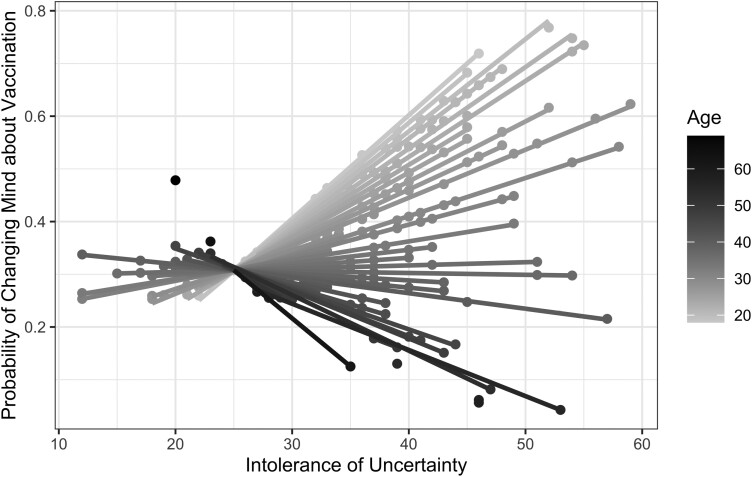
The logistic multilevel model without AuC and Trust in Science as covariates showed a significant age × IUS-12 interaction on the likelihood of change in vaccination status a year after expressing no intention of getting vaccinated, b = −0.06, SE = 0.02, z = −3.00, OR = 0.95, 95% CI [0.91, 0.98], p = .003. This interaction remained significant even after controlling for the effects of AuC and Trust in Science (Table 3; Fig. 1). Specifically, the younger the age of the participant, the higher the odds of change in vaccination status a year later with higher IU, OR = 1.05, p = .006. Controlling for age, AuC and Trust in Science, higher IU was associated with increased odds of being vaccinated, OR = 6.60, p < .001. Similarly, controlling for IU, AuC, and Trust in Science younger age was a significant predictor of higher odds of being vaccinated a year after reporting no intention to get vaccinated, OR = 1.05, p = .006.
Table 3.
Results of the Logistic Multilevel Model Predicting the Likelihood of Change in Vaccination Status a Year After Initially Expressing No Intention to Get Vaccinated
| Fixed effects | b | SE | z | p | OR | 95% CI |
|---|---|---|---|---|---|---|
| Intercept | −0.27 | 0.92 | −0.29 | .774 | 0.77 | [0.13, 4.68] |
| Trust in Science | 0.13 | 0.04 | 3.30 | <.001 | 1.14 | [1.05, 1.22] |
| AuC | −0.26 | 0.63 | −0.41 | .683 | 0.77 | [0.23, 2.65] |
| Age | −0.05 | 0.02 | −2.72 | .006 | 0.95 | [0.92, 0.99] |
| IUS-12 | 1.89 | 0.63 | 3.01 | .003 | 6.60 | [1.93, 22.57] |
| Age × IUS-12 | −0.05 | 0.02 | −2.73 | .006 | 0.95 | [0.91, 0.99] |
| Random effects | Estimate | SD | ||||
| Intercept error variance (country) | 0.75 | 0.87 |
Age, IUS, and AuC were measured at Time 1. Trust in Science and vaccination status (the outcome variable) were measured at Time 2. Age is measured in years. IUS-12 = Intolerance of Uncertainty-12 total score; AuC = Area-under-the-Curve CI = Confidence interval; OR = odds ratio; SD = standard deviation; and SE = standard error of the mean.
Fig. 1.
The likelihood of being vaccinated (0 = unvaccinated and 1 = vaccinated) at Time 2, a year after reporting no intention to get vaccinated, plotted by age and total score on the Intolerance of Uncertainty Scale at Time 1. The plot indicates that younger age (shown in lighter shades) is associated with greater likelihood of change in vaccination status a year later in individuals with higher intolerance of uncertainty.
Also of interest were the effects of the predictors that were not a primary focus of our hypotheses: Trust in Science and delay discounting (AuC). After controlling for the effects of IUS, age, and AuC, greater Trust in Science predicted an increased likelihood of getting vaccinated, OR = 1.14, p < .001. After controlling for the effects of IU, age, and Trust in Science, AuC was not a significant predictor of vaccination, OR = 0.77, p = .683.
Vaccination reasons
At Time 2, participants could provide reasons for their decision to become vaccinated or not. Approximately 94% of participants who provided qualitative responses identified a single reason for their decision. Of the 95 participants who changed their mind about vaccination one year later, n = 49 provided reasons for their decision: 45% felt it necessary to get vaccinated (8% for social reasons, 18% for work, and 18% for other reasons), of which 95% explicitly mentioned the influence of government mandates; 29% sought protection against the virus (16% for themselves, 10% for their family, and 2% for others), of which 21% specifically mentioned preventing severe illness or death; 8% based their decision on trust in vaccines and 2% trust in science; 2% were influenced by vaccine availability; 2% had a desire to contribute to ending the pandemic; and 12% were scored as other (e.g., peer pressure). Out of 157 participants who did not change their mind and remained unvaccinated a year later, n = 109 provided reasons for their decision: 43% based their decision on mistrust (24% in vaccines, 10% in government, 5% in science, and 5% other); 31% said vaccination was not necessary for them; and 16% said they were protecting themselves from experiencing other health complications or side effects; and 10% mentioned “other” reasons for remaining unvaccinated, referring primarily to personal circumstances (e.g., “afraid of needles”) or personal opinions (e.g., “don’t like vaccines”).
Discussion
This longitudinal investigation assessed the contributions of age and IU to the process of changing one’s mind about getting vaccinated a year after reporting no intention to get vaccinated, over and above well-established predictors of vaccination, such as delay discounting and trust in science. We found that IU significantly interacted with age in predicting the likelihood of changing one’s mind about vaccination: with younger age, those who were more intolerant of uncertainty in 2021 were more likely to be vaccinated in 2022. Thus, while younger adults may have shown greater resistance to vaccination throughout the pandemic [59], our findings suggest that younger adults with higher IU were more likely to change their minds about vaccination over the course of a year.
These findings build on extant literature emphasizing the role of IU in health behaviors, such as vaccination. IU is commonly associated with behavioral avoidance of situations that are uncertain. In the context of COVID-19, however, exposure to uncertainty was unavoidable, given the rapidly changing situation in terms of the threat of SARS-CoV-2 (e.g., waves of infection and new variants) as well as the changing policies and mandates designed to contain its impact. In those who experience higher levels of anxiety when encountering uncertainty (i.e., individuals who are highly intolerant of uncertainty), younger age was associated with an increased likelihood of changing one’s mind. This finding is broadly consistent with previous work showing that younger adults have more flexible coping styles [40, 41] and are more likely to take action—in this case, getting vaccinated—as a means to eliminate stressors [39]. The findings are also consistent with previous research indicating a functional role of anxiety in health-related behaviors, showing that decisions to not get vaccinated are associated with a decrease in fear of COVID-19 [60].
Among those participants who changed their vaccination status a year after stating no intention to get vaccinated, the most commonly provided reason for doing so (approximately 45%) was because of government mandates related to work and social activities; the second most common reason (29%) was related to prevention of serious illness. Even though all of these participants were vaccinated at Time 2, these different catalysts may reflect different forms of behavior change. On the one hand, individuals who described getting vaccinated because they were mandated to do so might have changed their behavior (i.e., became vaccinated) without changing their mind about vaccination (e.g., “I was planning to travel abroad so needed to be fully vaccinated. Otherwise I wouldn’t have gotten the vaccines”). It can be reasoned that these individuals may be less likely to engage in these efforts voluntarily—an important observation now that the pandemic has been declared over and responsibility for maintaining long-term immunity via booster vaccine doses has gradually shifted from government mandates to individual decision-making. On the other hand, individuals who stated that they got vaccinated to protect themselves against severe illness may be more likely to receive future doses for long-term immunity maintenance because of the apparent change in their belief about vaccination. Future research should focus on investigating the long-term maintenance of behavior change and how to combine short- and long-term interventions to influence both rapid and sustained uptake of protective health behaviors.
Older age was associated with a lower likelihood of changing one’s mind about vaccination, particularly among those who endorsed higher IU. This finding is consistent with research on uncertainty paralysis (i.e., inaction in the face of uncertainty about the outcome), both in relation to COVID-19 protective behaviors [28] and when faced with other health-related issues [61, 62]. Our results suggest that uncertainty paralysis may be a more prevalent response among individuals of older age when coping with uncertain situations, and may reflect the adoption of more avoidant coping strategies [40]. The findings are also consistent with previous research showing that as adults age, they tend to become less flexible, are more resistant to change, and display an increased preference for stability and familiarity [63]. This highlights the importance of targeted communication strategies, suggesting that approaching individuals of older age with messages that instill certainty (e.g., clear and easy-to-understand content from a trusted source, like a family doctor) [64] may be more effective in changing their mind about vaccination. Other intervention approaches may also involve psychoeducation and behavioral approaches (e.g., exposure) [65] focused on introducing strategies to reduce IU.
Another explanation for the moderating effect of age on the relationship between IU and changing one’s mind about vaccination is the age differences in beliefs about uncertainty and worry. IU diminishes as people transition from young adulthood to middle and advanced age, as they learn that excessive worrying about the unknown is counterproductive and as their belief in the functional value of worry weakens [66]. It is possible that, compared to their older counterparts, younger individuals were more motivated to get vaccinated and reduce feelings of uncertainty because they experienced more worries about potential consequences of not getting vaccinated. This possibility is consistent with research showing that age moderates the relationship between COVID-19 worries and anxiety: among individuals aged 50+ years, anxiety was unrelated to perceived likelihood of contracting COVID-19, whereas among younger ages (18–49 years), these variables were positively correlated [67].
It is notable that the interaction between IU and age accounted for a significant amount of variance in likelihood of change in vaccination status, over and above other well-established cognitive predictors of vaccination, such as trust in science [11] and delay discounting [12, 13, 47]. These findings are supported by participants’ qualitative reasons for their decisions, which revealed evidence of mistrust in science (e.g., “COVID vaccine is ineffective”), delay discounting (e.g., “I don’t think the benefits outweighed the long-term unknown and known short-term risks”), as well as uncertainty (e.g., “I’m just worried about how my body will handle it. I mostly trust the vaccine, just not for myself.”; “I needed it to travel, but I’m not sure about it so I won’t get the third dose.”).
Interestingly, we did not find a significant association between delay discounting, a well-established predictor of vaccination [12, 13, 15], and the likelihood of changing mind about vaccination among vaccine-hesitant individuals. The finding suggests that the process of changing mind about vaccination in this population likely relies on a different set of predictors compared to the initial decision to get vaccinated in the general population. The range of qualitative responses confirm the complexity of the decision-making process when it comes to getting vaccinated. It is possible that more effective interventions for encouraging people to engage in protective behaviors would have to carefully assess their stage of readiness for change [68]. For example, individuals in the preparation stage (i.e., have decided to change and are planning to take the first steps) may benefit from interventions involving individual nudges [69, 70]. In our sample, one participant stated “I’ve been too busy” as their reason for not getting vaccinated. It is possible that someone who is generally not opposed to vaccines but is struggling to find time to follow through on their intentions may respond well to nudges to get vaccinated through personal messages. However, the same intervention may not be effective for individuals in the precontemplative stage (i.e., not yet considering change), as was evident from a study showing ineffectiveness of nudges in a vaccine-hesitant population [71]. A number of participants in our sample who expressed concerns about vaccines (e.g., “I don’t trust that it will not adversely affect me”) may not be as receptive to the nudge messages. Incorporating alternative interventions (e.g., motivational interviewing) [72] for the individuals in the precontemplative stage may be necessary to facilitate change.
The choice of intervention should also consider the context. When a rapid change in behavior is required for short-term virus containment, government mandates seem to be the most effective, as suggested by participants’ qualitative responses (e.g., “I needed the vaccine for employment”) and supported by prior research [73, 74]. The pervasive uncertainty associated with the pandemic, reflected in government policies (e.g., lack of a clear timeline for easing restrictions, ambiguity about future travel, and social activity constraints), may motivate individuals to take action and get vaccinated. Conversely, if the objective is to promote long-term immunity maintenance (e.g., increasing willingness to receive vaccine booster doses), it will be essential to concentrate on programs aimed at changing people’s attitudes in the long run, rather than immediately altering their behavior.
Limitations and Future Directions
The study has a number of limitations. First, our sample at Time 2 was significantly older compared to those Time 1 participants who were eligible for Time 2 but lost to attrition (Supplementary Table S1). Although this finding may suggest that the Time 2 sub-sample was not representative of Time 1 participants who expressed no indication to get vaccinated, it should be noted that this age difference was small (mean ages of 29 vs. 32 years). Second, the majority of the participants in the current study were aged under 50 years old. Given the purpose of this research was to investigate the effect of age as a continuous variable (i.e., not to compare younger vs. older adults), it should be noted that the age range of our sample was sufficiently wide to investigate the effect of age (18–69 years; Supplementary Fig. S1). Nevertheless, additional studies replicating the effect and extending it into older-aged participants would help consolidate the findings reported here. Third, it is important to note that although the participants in this study are from 13 countries, the relatively small sample size (N = 251) meant we were unable to explore country-related differences. Lastly, the cross-sectional nature of this study does not allow for causal inferences about the effect of IU on individuals’ decisions to get vaccinated. The field would benefit from further work testing the effect of uncertainty interventions on the process of changing mind about vaccination in vaccine-hesitant individuals. Moreover, future research in this area can benefit from studies focused exclusively on vaccine-hesitant individuals, allowing for a more nuanced investigation of the decision-making process in this population.
Conclusion
Overall, this study showed a significant interaction between age and IU on the decision to get vaccinated a year after initially expressing no intention to do so, over and above the effects of delay discounting and trust in science. In the context of this research, we also explored participants’ own reasoning about their vaccination decisions. Future research could further examine various factors of people’s uncertainty regarding vaccination. Unlike studies investigating predictors of vaccination during COVID-19 at a single time point, this longitudinal investigation of the process of changing one’s mind about vaccination in vaccine-hesitant populations allows for a better understanding of the dynamic nature of vaccine hesitancy and when it might shift into vaccine willingness. By recognizing the influence of age and IU on changes in vaccine decisions, public health campaigns can tailor their messages to address specific concerns and uncertainties (e.g., trust in science vs. uncertainty about future mandates) in different age groups. Additionally, future longitudinal research will inform development of targeted interventions aimed at reducing vaccine hesitancy over time, emphasizing the importance of building trust in vaccines and healthcare systems. Recognizing the complex interplay between age, uncertainty, and vaccination decisions can contribute to more effective strategies to promote vaccine uptake and ultimately inform public health measures in preparation for future pandemics or other health crises.
Supplementary Material
Supplementary material is available at Annals of Behavioral Medicine online.
Acknowledgements
We thank Geneviève Quintin and Caitlin Terao for helpful discussion. We thank Riya Trikha and William Fisher for assistance with scoring. Research reported in this manuscript was funded by the Canadian Institutes of Health Research (CIHR) Canadian 2019 Novel Coronavirus (COVID-19) Rapid Research Funding Opportunity Operating Grant (grant 172681) and the York University-Beneva Anxiety Research Fund to R.S.R. and D.R.A. D.R.A is supported by the Canada 150 Research Chairs Program. R.S.R. is supported by a York Research Chair in Cognitive Neuroscience of Memory. The funding agencies had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Contributor Information
Julia G Halilova, Department of Psychology and Centre for Integrative and Applied Neuroscience, York University, 4700 Keele St., Toronto, Ontario, M3J 1P3, Canada.
Samuel Fynes-Clinton, Baycrest Health Sciences, Rotman Research Institute, 3560 Bathurst St, North York, ON M6A 2E1, Canada.
Donna Rose Addis, Baycrest Health Sciences, Rotman Research Institute, 3560 Bathurst St, North York, ON M6A 2E1, Canada; Department of Psychology, University of Toronto, 27 King’s College Cir, Toronto, ON M5S 1A1, Canada; Department of Psychology, The University of Auckland, 34 Princes Street, Auckland CBD, Auckland 1010, New Zealand.
R Shayna Rosenbaum, Department of Psychology and Centre for Integrative and Applied Neuroscience, York University, 4700 Keele St., Toronto, Ontario, M3J 1P3, Canada; Baycrest Health Sciences, Rotman Research Institute, 3560 Bathurst St, North York, ON M6A 2E1, Canada.
Compliance with Ethical Standards
Conflict of Interest The authors declare no conflict of interest (individual DOI forms were signed and submitted by every author).
Authors’ Contributions Julia G. Halilova ( Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Visualization, Writing—original draft, Writing—review & editing), Samuel Fynes-Clinton (Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Writing—review & editing), Donna Rose Addis (Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Writing—original draft, Writing—review & editing), and R. Shayna Rosenbaum (Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Writing—original draft, Writing—review & editing)
Statement on the Welfare of Animals This article does not contain any studies with animals performed by any of the authors.
Statement of Human Rights and Ethics Approval The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The research was approved by the York University and Baycrest Research Ethics Boards REB# 19-07.
Informed Consent Informed consent was obtained from all individual participants included in the study.
Transparency Statement
(1) This study was not formally registered. (2) The analysis plan was not formally pre-registered. (3, 4) De-identified data from this study and analytic code used to conduct the analyses presented in this study are available in a public archive Open Science Framework https://osf.io/8g5ue/?view_only=f6480e76660046f7aa87b1d20528fbb3. (5) All materials used to conduct the study are publicly available.
References
- 1. Lopez Bernal J, Andrews N, Gower C, et al. Effectiveness of Covid-19 vaccines against the B.1.617.2 (Delta) variant. N Engl J Med. 2021; 385(7):585–594. doi: 10.1056/NEJMoa2108891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization. Vaccines and immunization. Available at https://www.who.int/health-topics/vaccines-and-immunization. Accessed September 2, 2022. [Google Scholar]
- 3. Campos-Mercade P, Meier AN, Schneider FH, Meier S, Pope D, Wengström E.. Monetary incentives increase COVID-19 vaccinations. Science. 2021; 374(6569):879–882. doi: 10.1126/science.abm0475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Szilagyi PG, Thomas K, Shah MD, et al. The role of trust in the likelihood of receiving a COVID-19 vaccine: Results from a national survey. Prev Med. 2021; 153:106727. doi: 10.1016/j.ypmed.2021.106727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Levitt EE, Gohari MR, Syan SK, et al. Public health guideline compliance and perceived government effectiveness during the COVID-19 pandemic in Canada: Findings from a longitudinal cohort study. Lancet Reg Health Am. 2022; 9:100185. doi: 10.1016/j.lana.2022.100185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jantzen R, Maltais M, Broët P.. Socio-demographic factors associated with COVID-19 vaccine hesitancy among middle-aged adults during the Quebec’s vaccination campaign. Front Public Health. 2022; 10:756037. doi: 10.3389/fpubh.2022.756037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Li H. To vaccinate or not: the relationship between conscientiousness and individual attitudes toward vaccination in real-life contexts. Scand J Psychol. 2022; 63:376–382. doi: 10.1111/sjop.12816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Choi SL, Martin P, Cho J, Ryou YJ, Heinz M.. Personality and compliance with COVID-19 protective measures among older Americans: Moderating effects of age, gender, and race/ethnicity. Pers Individ Differ. 2022; 189:111499. doi: 10.1016/j.paid.2022.111499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Steinmetz L. Sociodemographic predictors of and main reasons for COVID-19 vaccine hesitancy in eastern Oslo: A cross-sectional study. BMC Public Health. 2022; 22:1878. doi: 10.1186/s12889-022-14261-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pandolfo G, Genovese G, Iannuzzo F, Bruno A, Pioggia G, Gangemi S.. COVID-19 vaccination and mental disorders, what has been accomplished and future direction. Brain Sci. 2022; 12:292. doi: 10.3390/brainsci12020292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Carrieri V, Guthmuller S, Wübker A.. Trust and COVID-19 vaccine hesitancy. Sci Rep. 2023; 13:9245. doi: 10.1038/s41598-023-35974-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Halilova JG, Fynes-Clinton S, Green L, et al. Short-sighted decision-making by those not vaccinated against COVID-19. Sci Rep. 2022; 12:11906. doi: 10.1038/s41598-022-15276-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Halilova JG, Fynes-Clinton S, Addis DR, Rosenbaum RS.. Assessing the relationship between delay discounting and decisions to engage in various protective behaviors during COVID-19. Cogn Res Princ Implic. 2024;9(1):38. doi: 10.1186/s41235-024-00566-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Liang W, Duan Y, Li F, et al. Psychosocial determinants of hand hygiene, facemask wearing, and physical distancing during the COVID-19 pandemic: A systematic review and meta-analysis. Ann Behav Med. 2022; 56:1174–1187. doi: 10.1093/abm/kaac049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Strickland JC, Reed DD, Dayton L, et al. Behavioral economic methods predict future COVID-19 vaccination. Transl. Behav. Med. 2022; 12(1004-8):1004–1008. doi: 10.1093/tbm/ibac057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. El-Shabasy RM, Nayel MA, Taher MM, Abdelmonem R, Shoueir KR, Kenawy ER.. Three waves changes, new variant strains, and vaccination effect against COVID-19 pandemic. Int J Biol Macromol. 2022; 204:161–168. doi: 10.1016/j.ijbiomac.2022.01.118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zhao S, Ye B, Wang W, Zeng YT. The intolerance of uncertainty and “untact” buying behavior: The mediating role of the perceived risk of COVID-19 variants and protection motivation. Front Psychol. 2022; 13:807331. doi: 10.3389/fpsyg.2022.807331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Koffman J, Gross J, Etkind SN, Selman L.. Uncertainty and COVID-19: How are we to respond? J R Soc Med. 2020; 113:211–216. doi: 10.1177/0141076820930665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Capurro G, Jardine CG, Tustin J, Driedger M.. Communicating scientific uncertainty in a rapidly evolving situation: A framing analysis of Canadian coverage in early days of COVID-19. BMC Public Health. 2021; 21:2181. doi: 10.1186/s12889-021-12246-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Baerg L, Bruchmann K.. COVID-19 information overload: Intolerance of uncertainty moderates the relationship between frequency of internet searching and fear of COVID-19. Acta Psychol (Amst). 2022; 224:103534. doi: 10.1016/j.actpsy.2022.103534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Carleton RN. Into the unknown: A review and synthesis of contemporary models involving uncertainty. J Anxiety Disord. 2016; 39:30–43. doi: 10.1016/j.janxdis.2016.02.007 [DOI] [PubMed] [Google Scholar]
- 22. Talkovsky AM, Norton PJ.. Intolerance of uncertainty and transdiagnostic group cognitive behavioral therapy for anxiety. J Anxiety Disord. 2016; 41:108–114. doi: 10.1016/j.janxdis.2016.05.002 [DOI] [PubMed] [Google Scholar]
- 23. Rosser BA. Intolerance of uncertainty as a transdiagnostic mechanism of psychological difficulties: A systematic review of evidence pertaining to causality and temporal precedence. Cogn Ther Res 2019; 43:438–463. doi: 10.1007/s10608-018-9964-z [DOI] [Google Scholar]
- 24. Hunt C, Exline JJ, Fletcher TL, Teng EJ.. Intolerance of uncertainty prospectively predicts the transdiagnostic severity of emotional psychopathology: Evidence from a Veteran sample. J Anxiety Disord. 2022; 86:102530. doi: 10.1016/j.janxdis.2022.102530 [DOI] [PubMed] [Google Scholar]
- 25. Miller ML, McGuire JF.. Targeting intolerance of uncertainty in treatment: A meta-analysis of therapeutic effects, treatment moderators, and underlying mechanisms. J Affect Disord. 2023; 341:283–295. doi: 10.1016/j.jad.2023.08.132 [DOI] [PubMed] [Google Scholar]
- 26. Boswell JF, Thompson-Hollands J, Farchione TJ, Barlow DH.. Intolerance of uncertainty: A common factor in the treatment of emotional disorders. J Clin Psychol. 2013; 69:630–645. doi: 10.1002/jclp.21965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Jessup SC, Knowles KA, Olatunji BO.. Linking the estimation of threat and COVID-19 fear and safety behavior use: Does intolerance of uncertainty matter? Int J Cogn Ther. 2022; 15:479–491. doi: 10.1007/s41811-022-00148-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Fitzgerald HE, Parsons EM, Indriolo T, et al. Worrying but not acting: The role of intolerance of uncertainty in explaining the discrepancy in COVID-19-related responses. Cognit Ther Res. 2022; 46:1150–1156. doi: 10.1007/s10608-022-10321-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gillman AS, Scharnetzki L, Boyd P, Ferrer RA, Klein WMP, Han PKJ.. Perceptions and tolerance of uncertainty: Relationship to trust in COVID-19 health information and vaccine hesitancy. J Behav Med. 2023; 46:40–53. doi: 10.1007/s10865-022-00302-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Horenstein A, Rogers AH, Bakhshaie J, Zvolensky MJ, Heimberg RG.. Examining the role of anxiety sensitivity and intolerance of uncertainty in the relationship between health anxiety and likelihood of medical care utilization. Cognit Ther Res. 2019; 43:55–65. doi: 10.1007/s10608-018-9980-z [DOI] [Google Scholar]
- 31. Ball TM, Gunaydin LA.. Measuring maladaptive avoidance: From animal models to clinical anxiety. Neuropsychopharmacology. 2022; 47:978–986. doi: 10.1038/s41386-021-01263-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Godara M, Everaert J, Sanchez-Lopez A, Joormann J, De Raedt R.. Interplay between uncertainty intolerance, emotion regulation, cognitive flexibility, and psychopathology during the COVID-19 pandemic: A multi-wave study. Sci Rep. 2023; 13:9854. doi: 10.1038/s41598-023-36211-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Luhmann CC, Ishida K, Hajcak G.. Intolerance of uncertainty and decisions about delayed, probabilistic rewards. Behav Ther. 2011; 42(3):378–386. doi: 10.1016/j.beth.2010.09.002 [DOI] [PubMed] [Google Scholar]
- 34. Amlung M, Marsden E, Holshausen K, et al. Delay discounting as a transdiagnostic process in psychiatric disorders: A meta-analysis. JAMA Psychiatry. 2019; 76(11):1176–1186. doi: 10.1001/jamapsychiatry.2019.2102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Robertson E, Reeve KS, Niedzwiedz CL, et al. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav Immun. 2021; 94:41–50. doi: 10.1016/j.bbi.2021.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Guay M, Maquiling A, Chen R, et al. Measuring inequalities in COVID-19 vaccination uptake and intent: Results from the Canadian Community Health Survey 2021. BMC Public Health. 2022; 22:1708. doi: 10.1186/s12889-022-14090-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ferrini R, Edelstein S, Barrett-Connor E.. The association between health beliefs and health behavior change in older adults. Prev Med. 1994; 23:1–5. doi: 10.1006/pmed.1994.1001 [DOI] [PubMed] [Google Scholar]
- 38. Tucker JS, Klein DJ, Elliott MN.. Social control of health behaviors: A comparison of young, middle-aged, and older adults. J Gerontol B Psychol Sci Soc Sci 2004; 59:147–150. doi: 10.1093/geronb/59.4.p147 [DOI] [PubMed] [Google Scholar]
- 39. Chen Y, Peng Y, Xu H, O’Brien WH.. Age differences in stress and coping: Problem-focused strategies mediate the relationship between age and positive affect. Int J Aging Hum Dev. 2018; 86:347–363. doi: 10.1177/0091415017720890 [DOI] [PubMed] [Google Scholar]
- 40. Blanchard-Fields F, Jahnke HC, Camp C.. Age differences in problem-solving style: The role of emotional salience. Psychol Aging. 1995; 10:173–180. doi: 10.1037//0882-7974.10.2.173 [DOI] [PubMed] [Google Scholar]
- 41. Eldesouky, L, English, T.. Another year older, another year wiser? Emotion regulation strategy selection and flexibility across adulthood. Psychol Aging. 2018; 33:572–585. doi: 10.1037/pag0000251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Amore S, Puppo E, Melara J, Terracciano E, Gentili S, Liotta G.. Impact of COVID-19 on older adults and role of long-term care facilities during early stages of epidemic in Italy. Sci Rep. 2021; 11:12530. doi: 10.1038/s41598-021-91992-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Levin AT, Hanage WP, Owusu-Boaitey N, Cochran KB, Walsh SP, Meyerowitz-Katz G.. Assessing the age specificity of infection fatality rates for COVID-19: Systematic review, meta-analysis, and public policy implications. Eur J Epidemiol. 2020; 35:1123–1138. doi: 10.1007/s10654-020-00698-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mueller AL, McNamara MS, Sinclair DA.. Why does COVID-19 disproportionately affect older people? Aging (Milano). 2020; 12:9959–9981. doi: 10.18632/aging.103344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Shahid Z, Kalayanamitra R, McClafferty B, et al. COVID-19 and older adults: What we know. J Am Geriatr Soc. 2020; 68:926–929. doi: 10.1111/jgs.16472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Romero Starke K, Reissig D, Petereit-Haack G, Schmauder S, Nienhaus A, Seidler A.. The isolated effect of age on the risk of COVID-19 severe outcomes: A systematic review with meta-analysis. BMJ Global Health. 2021; 6:e006434. doi: 10.1136/bmjgh-2021-006434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hudson A, Hall PA, Hitchman SC, Meng G, Fong GT.. Cognitive predictors of COVID-19 mitigation behaviors in vaccinated and unvaccinated general population members. Vaccine. 2022; 41:4019–4026. doi: 10.1016/j.vaccine.2022.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Ann Int Med. 2007; 147:573–577. doi: 10.7326/0003-4819-147-8-200710160-00010 [DOI] [PubMed] [Google Scholar]
- 49. Adler NE, Epel ES, Castellazzo G, Ickovics JR.. Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy white women. Health Psychol. 2000; 19:586–592. doi: 10.1037//0278-6133.19.6.586 [DOI] [PubMed] [Google Scholar]
- 50. Smith ML, Kakuhikire B, Baguma C, et al. Relative wealth, subjective social status, and their associations with depression: Cross-sectional, population-based study in rural Uganda. SSM Popul Health. 2019; 8:100448. doi: 10.1016/j.ssmph.2019.100448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Carleton RN, Norton MA, Asmundson GJ.. Fearing the unknown: A short version of the intolerance of uncertainty scale. J Anxiety Disord. 2007; 21:105–117. doi: 10.1016/j.janxdis.2006.03.014 [DOI] [PubMed] [Google Scholar]
- 52. Achterberg P, de Koster W, van der Waal J.. A science confidence gap: Education, trust in scientific methods, and trust in scientific institutions in the United States, 2014. Public Underst Sci. 2017; 26:704–720. doi: 10.1177/0963662515617367 [DOI] [PubMed] [Google Scholar]
- 53. Ciaramelli E, De Luca F, Kwan D, et al. The role of ventromedial prefrontal cortex in reward valuation and future thinking during intertemporal choice. eLife. 2021; 10:e67387. doi: 10.7554/eLife.67387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Mok JNY, Kwan D, Green L, Myerson J, Craver CF, Rosenbaum RS.. Is it time? Episodic imagining and the discounting of delayed and probabilistic rewards in young and older adults. Cognition. 2020; 199:104222. doi: 10.1016/j.cognition.2020.104222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Myerson J, Green L, Warusawitharana M.. Area under the curve as a measure of discounting. J Exp Anal Behav. 2001; 76:235–243. doi: 10.1901/jeab.2001.76-235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Marjanovic Z, Holden R, Struthers W, Cribbie R, Greenglass E.. The inter-item standard deviation (ISD): An index that discriminates between conscientious and random responders. Pers Individ Differ. 2015; 84:79–83. doi: 10.1016/j.paid.2014.08.021 [DOI] [Google Scholar]
- 57. Bates, D., Maechler, M., Bolker, B, Walker, S.. Fitting Linear Mixed-Effects Models Using lme4. J Stat Soft. 67(1):1–48. [Google Scholar]
- 58. Kuznetsova A, Brockhoff PB, Christensen RHB.. lmerTest package: Tests in linear mixed effects models. J Stat Softw. 2017; 82(13):1–26. doi: 10.18637/jss.v082.i13 [DOI] [Google Scholar]
- 59. Pires C. Global predictors of COVID-19 vaccine hesitancy: A systematic review. Vaccines. 2022; 10:1349. doi: 10.3390/vaccines10081349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Mertens G, Lodder P, Smeets T, Duijndam S.. Pandemic panic? Results of a 14-month longitudinal study on fear of COVID-19. J Affect Disord. 2023; 322:15–23. doi: 10.1016/j.jad.2022.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Piccolo M, Milos GF, Bluemel S, et al. Behavioral responses to uncertainty in weight-restored anorexia nervosa—preliminary results. Front Psychol. 2019; 10:2492. doi: 10.3389/fpsyg.2019.02492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Berenbaum H, Bredemeier K, Thompson RJ.. Intolerance of uncertainty: Exploring its dimensionality and associations with need for cognitive closure, psychopathology, and personality. J Anxiety Disord. 2008; 22:117–125. doi: 10.1016/j.janxdis.2007.01.004 [DOI] [PubMed] [Google Scholar]
- 63. Matamales M, Skrbis Z, Hatch RJ, Balleine BW, Götz J, Bertran-Gonzalez J.. Aging-related dysfunction of striatal cholinergic interneurons produces conflict in action selection. Neuron. 2016; 90:362–373. doi: 10.1016/j.neuron.2016.03.006 [DOI] [PubMed] [Google Scholar]
- 64. Salali G, Uysal M.. Effective incentives for increasing COVID-19 vaccine uptake. Psychol Med. 2023; 53:3242–3244. doi: 10.1017/s0033291721004013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Freeman D, Lambe S, Yu LM, et al. Injection fears and COVID-19 vaccine hesitancy. Psychol Med. 2023; 53:1185–1195. doi: 10.1017/S0033291721002609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Basevitz P, Pushkar D, Chaikelson J, Conway M, Dalton C.. Age-related differences in worry and related processes. Int J Aging Hum Dev. 2008; 66:283–305. doi: 10.2190/AG.66.4.b [DOI] [PubMed] [Google Scholar]
- 67. Wilson JM, Lee J, Shook NJ.. COVID-19 worries and mental health: The moderating effect of age. Aging Ment Health. 2021; 25:1289–1296. doi: 10.1080/13607863.2020.1856778 [DOI] [PubMed] [Google Scholar]
- 68. Prochaska JO, DiClemente CC.. Stages and processes of self-change of smoking: Toward an integrative model of change. J Consult Clin Psychol. 1983; 51:390–395. doi: 10.1037//0022-006x.51.3.390 [DOI] [PubMed] [Google Scholar]
- 69. Dai H, Saccardo S, Han MA, et al. Behavioural nudges increase COVID-19 vaccinations. Nature. 2021; 597(7876):404–409. doi: 10.1038/s41586-021-03843-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Milkman KL, Gandhi L, Patel MS, et al. A 680,000-person megastudy of nudges to encourage vaccination in pharmacies. Proc Natl Acad Sci U S A. 2022; 119:e2115126119. doi: 10.1073/pnas.2115126119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. de Ridder D, Adriaanse M, van Gestel L, Wachner J.. How does nudging the COVID-19 vaccine play out in people who are in doubt about vaccination? Health Policy. 2023; 134:104858. doi: 10.1016/j.healthpol.2023.104858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Miller WR, Rollnick S,. Motivational Interviewing: Helping People Change. 3rd ed. NY: Guilford Press. 2013. [Google Scholar]
- 73. Brewer NT, Chapman GB, Rothman AJ, Leask J, Kempe A.. Increasing vaccination: Putting psychological science into action. Psychol Sci Public Interest. 2017; 18(3):149–207. doi: 10.1177/1529100618760521 [DOI] [PubMed] [Google Scholar]
- 74. Broomell SB, Chapman GB.. Looking beyond cognition for risky decision making: COVID-19. J Appl Res Mem Cogn 2021; 10:512–516. doi: 10.1016/j.jarmac.2021.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.