Abstract
Diaphragmatic ultrasound, valued for its portability and safety, assesses both structural and functional aspects of the diaphragm. While some studies support its predictive value, others conflict. This meta-analysis aims to clarify diaphragmatic ultrasound’s role in predicting successful liberation from mechanical ventilation in intensive care settings. A systematic search was performed on Web of Science, Scopus, and PubMed up to March, 2024. The search strategy included a combination of relevant medical subject heading (MeSH) terms and relevant keywords. We defined our eligibility criteria based on the PICO framework. Two authors performed the data extraction using a standardized sheet. The pooled mean difference was calculated using random effects model and Hedges’ g along with SD estimation. R and RStudio were used for the statistical analysis and creating forest and funnel plots. The pooled mean difference was 7.25 (95% CI: 4.20, 10.21) for DE among the two groups. We found a statistically significant difference between the two groups indicating that those with successful weaning from intubation had higher means of DE compared to those with failed weaning attempt (p-value<0.01). The mean difference of DTF was also higher among those with successful weaning from intubation compared to those with failed weaning attempt with the pooled mean difference of 14.52 (95% CI: 10.51, 18.54, p-value<0.01). The mean difference of RSBI was lower among those with successful weaning from intubation compared to those with failed weaning attempt with the pooled mean difference of -28.86 (95% CI: -41.82, -15.91, p-value<0.01). Our results suggest that evaluating diaphragmatic excursion and thickening fraction can reliably anticipate successful liberation from mechanical ventilation. However, significant heterogeneity was present among the included studies. High-quality research, particularly randomized clinical trials, is required to further elucidate the role of diaphragmatic ultrasound in predicting weaning from mechanical ventilation.
Key Words: ultrasound, ultrasonography, diaphragm, thickening fraction, excursion
Weaning patients off mechanical ventilation in the ICU poses a significant challenge. It’s crucial for the multidisciplinary team to determine the ideal timing for this process. Premature weaning can result in weaning failure, leading to higher risks of hospital-acquired infections, increased healthcare costs, prolonged ICU and hospital stays, and potential diaphragmatic dysfunction.1,2 Existing guidelines suggest using various bedside indices to anticipate successful weaning from mechanical ventilation.
However, these indices have not demonstrated absolute effectiveness, likely because critically ill patients exhibit diverse characteristics, which can impede the predictive accuracy of these indices across different patient groups. While a Spontaneous Breathing Trial (SBT) is a suitable method to ready the patient for extubation, failure rates and the need for subsequent reintubation can surpass 20% in patients at the highest risk.3-5
Patients undergoing mechanical ventilation may experience a complex decline in diaphragmatic function, which can contribute to weaning difficulties and prolonged dependence on invasive mechanical ventilation. Therefore, evaluating diaphragmatic function could aid in predicting the patient’s capacity to sustain spontaneous breathing over an extended period.6-8 The application of diaphragmatic ultrasound in the intensive care setting has garnered increasing interest due to its portability, rapidity, and safety. This technique enables assessment of both the structural and functional aspects of the diaphragm, offering insights into the likelihood of successful weaning from mechanical ventilation. While certain studies have highlighted the utility of ultrasound in predicting weaning success, others have presented conflicting findings, prompting ongoing investigation into its efficacy.6-11 This systematic review and meta-analysis aim to assess the role of diaphragmatic ultrasound in predicting successful liberation from mechanical ventilation.
Methods and Materials
The present study was conducted based on the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guideline 2020.12
Search strategy
A systematic search was performed on electronic databases such as Web of Science, Scopus, and PubMed from the beginning until March, 2024. The search strategy included a combination of relevant medical subject heading (MeSH) terms and relevant keywords for (“ultrasonography” OR “ultrasound” OR “US”) AND (“diaphragm excursion” OR “diaphragm thickening fraction” OR “rapid shallow breathing index”) AND (“extubating” OR “weaning” OR “extubation”).
Eligibility criteria
We defined our eligibility criteria based on the PICO framework: (P) Population: critically ill patients. (I) Intervention: mechanical ventilation. (C) Comparison: diaphragm parameters. (O) Outcome: weaning success. The exclusion criteria were defined as: absence of diaphragm parameters, not reporting weaning outcome, lack of individual data, and non-English language.
Data extraction and outcome measures
Two independent authors performed the data extraction using a standardized sheet. Any disagreement was resolved through a discussion with a third party. The standardized sheet included: authors’ name, year of publication, total number of participants, male to female ratio, mean and SD of diaphragm excursion, mean and SD of diaphragm thickening fraction, mean and SD of rapid shallow breathing index. The aforementioned variables were extracted in two groups: the weaning success and weaning failure.
Statistical analysis and data synthesis
The pooled mean difference was calculated using random effects model and Hedges’ g along with SD estimation. For assessing the heterogeneity of the included studies, the I2 (I square) test was used. The Mantel-Haenszel method and random effects model was used for pooling the effect sizes and SD was consequently calculated. For testing the overall significance of the random model, z-test was performed Potential publication bias was graphically assessed by creating funnel plots for each of the aforementioned groups. R (R Foundation for Statistical Computing, Vienna, Austria) and RStudio (RStudio, Inc., Boston, MA) were used for the statistical analysis and creating forest and funnel plots.
Results
Our initial search retrieved 2444 articles from PubMed, Scopus, and Web of Science, from which 942 duplicates were removed. After screening the title and abstract of 1502 records, 91 full texts were retrieved, among which 1610,11,13-26 studies were included based on our eligibility criteria (Figure 1). More detail regarding the study characteristics of the included studies is summarized in Table 1.
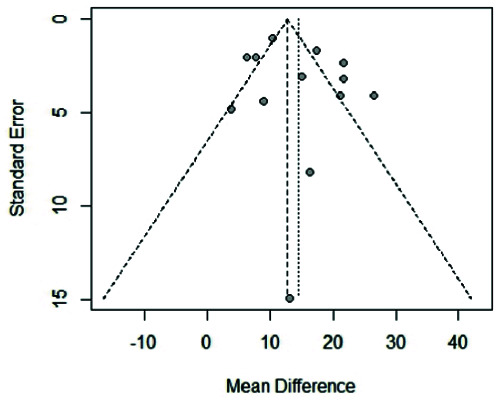
Based on the random effects model for pooling the mean difference of DE among those with/without successful weaning from intubation, the pooled mean difference was 7.25 (95% CI: 4.20, 10.21). We found a statistically significant difference between the two groups indicating that those with successful weaning from intubation had higher means of DE compared to those with failed weaning attempt (p-value<0.01). Figure 2 and 3 show the forest and funnel plots for the pooled mean difference of DE among the two groups. Table 1 summarizes the characteristics of the included studies for DE.
The mean difference of DTF was also higher among those with successful weaning from intubation compared to those with failed weaning attempt with the pooled mean difference of 14.52 (95% CI: 10.51, 18.54) based on the random effects model (p-value<0.01). Figure 4 and 5 show the funnel and forest plots for pooled DTF among the two groups. Table 2 summarizes the characteristics of the included studies for DTF.
The mean difference of RSBI was lower among those with successful weaning from intubation compared to those with failed weaning attempt with the pooled mean difference of -28.86 (95% CI: -41.82, -15.91) based on the random effects model (p-value<0.01). Table 3 summarizes the characteristics of the included studies for RSBI.
Discussion
Based on the results of our systematic review and meta-analysis, DE and DTF showed significant difference among those with successful weaning from intubation and those with failed attempt of weaning. These results can indicate that DE and DTF be used as non-invasive methods for prediction of the outcome of weaning from mechanical ventilation among critically ill patients.
In recent years, several systematic reviews and meta-analyses have examined the utility of diaphragmatic ultrasound in predicting weaning success or failure in mechanically ventilated patients.27-34 Our findings align with the conclusions drawn in most of these previously published studies. For instance, one study reported satisfactory diagnostic accuracy in predicting extubation outcomes, while another concluded that diaphragmatic thickening fraction alone modestly predicts weaning outcomes.35-37 Additionally, recent research has linked ultrasound-detected diaphragm dysfunction with an elevated risk of extubation failure. Moreover, findings from another study indicate that reduced diaphragmatic excursion and thickening fraction values are associated with a heightened risk of extubation failure, exhibiting moderate to high specificity.20,38,39
In clinical practice, patients experiencing respiratory failure often rely on mechanical ventilation for assistance in breathing. This form of respiratory support is widely utilized and effectively facilitates the transition from shallow, rapid breathing to normal breathing, without imposing additional strain on the respiratory system.40,42 This improves overall alveolar ventilation. However, the mechanical stimulation associated with mechanical ventilation can trigger a heightened inflammatory response in the patient’s body. Prolonged use of mechanical ventilation may also contribute to progressive organ damage and subsequent multi-organ failure, thereby increasing the risk of mortality. As such, it is crucial to withdraw mechanical ventilation promptly once the underlying causes of respiratory distress have been adequately addressed. While weaning from mechanical ventilation is typically successful, there are cases where patients fail spontaneous breathing trials or require reintubation shortly after extubation. Thus, successfully weaning patients from mechanical ventilation remains a significant clinical challenge in the management of respiratory failure.19,34,43,44
Figure 1.
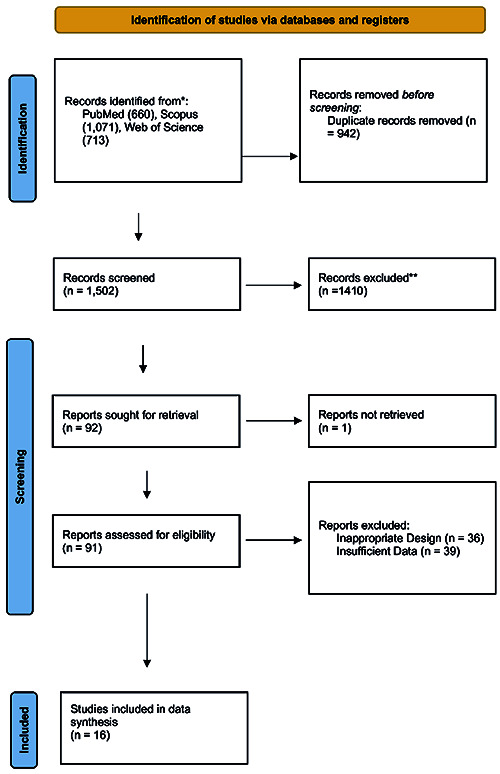
The PRISMA flow chart of the included studies.
Table 1.
Characteristics of the included studies for DE.
| Author | Year | Country | Population | M/F | DE | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Success | Failure | |||||||||
| Mean | SD | N | Mean | SD | N | |||||
| Alam et al. (14) | 2022 | Bangladesh | 31 | 19/12 | 12.41 | 2.38 | 18 | 9.2 | 1.87 | 13 |
| Elshazly et al. (15) | 2020 | Egypt | 62 | NR | 21.81 | 7.04 | 34 | 9.28 | 3.9 | 28 |
| Eltrabili et al. (16) | 2019 | Egypt | 35 | 16/19 | 18.37 | 7.27 | 17 | 7.78 | 4.15 | 13 |
| Farghaly et al. (17) | 2017 | Egypt | 54 | 31/23 | 15.07 | 5.07 | 40 | 10.23 | 2.63 | 14 |
| Fossat et al. (19) | 2022 | France | 100 | NR | 23.8 | 9.2 | 91 | 25.9 | 10.5 | 9 |
| Kaur et al. (20) | 2022 | India | 50 | NR | 37.5 | 9 | 31 | 21.2 | 6.7 | 19 |
| Li et al. (21) | 2021 | China | 101 | 42/59 | 15.93 | 5.14 | 69 | 8.03 | 4.57 | 32 |
| Osman et al. (23) | 2017 | Egypt | 68 | NR | 24.17 | 4.23 | 50 | 9.29 | 5.48 | 18 |
| Palker et al. (24) | 2018 | USA | 73 | 37/36 | 22 | 9 | 53 | 16.6 | 8 | 20 |
| Sabetian et al. (25) | 2024 | Iran | 50 | 39/11 | 12.50 | 4.78 | 26 | 10.22 | 3.15 | 24 |
| Theerawit et al. (10) | 2018 | Thailand | 52 | 38/14 | 13.5 | 5.3 | 51 | 12.8 | 9.6 | 11 |
| Yoo et al. (26) | 2018 | Korea | 60 | 42/18 | 15.93 | 5.20 | 47 | 8.03 | 4.90 | 13 |
Figure 2.
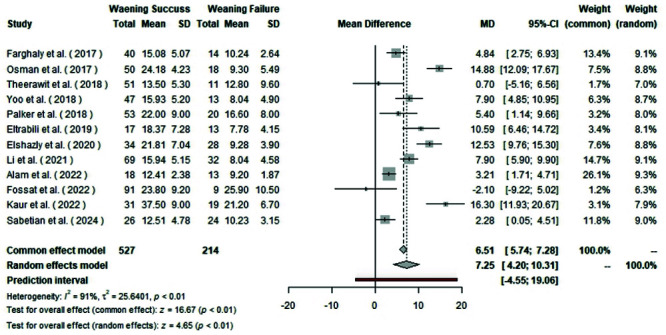
Forest plot of pooled mean difference of DE among the two groups.
Figure 3.
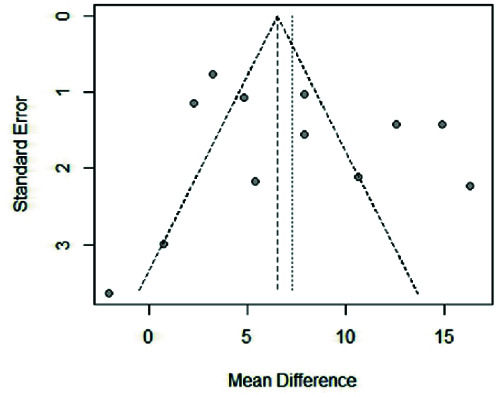
Funnel plot of mean difference of DE among the included studies.
Bedside ultrasound technology has gained widespread acceptance and is often referred to as a visual "stethoscope" due to its rapid, non-invasive, reproducible, and intuitive nature. In the context of weaning from invasive mechanical ventilation, bedside ultrasound plays a crucial role by facilitating diaphragm function monitoring, lung ultrasound, volume responsiveness assessment, and cardiac ultrasound indicators.45-47 Its utility extends to assessing the pathophysiological status of patients and identifying the underlying causes of weaning failure. One key parameter used to evaluate diaphragm function is the diaphragm thickening fraction.15,48-50
Figure 4.
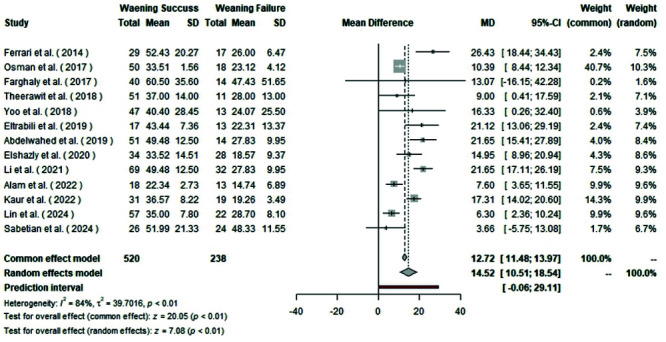
Forest plot of pooled mean difference of DTF among the two groups.
Figure 5.
Funnel plot of mean difference of DTE among the included studies.
Several limitations should be acknowledged in this study. First, potential biases may exist in each of the included studies as randomized trials were not incorporated. Additionally, the absence of a standardized reference value for diaphragmatic thickening and excursion fraction could introduce measurement inaccuracies. Furthermore, subgroup analysis based on sex and the duration of mechanical ventilation prior to the spontaneous breathing trial and ultrasound assessment was not conducted, which could potentially influence the ultrasound outcomes.
Table 2.
Characteristics of the included studies for DTF.
| Author | Year | Country | Population | M/F | DTF | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Success | Failure | |||||||||
| Mean | SD | N | Mean | SD | N | |||||
| Abdelwahed et al. (13) | 2019 | Egypt | 65 | 40/25 | 49.48 | 12.5 | 51 | 27.83 | 9.95 | 14 |
| Alam et al. (14) | 2022 | Bangladesh | 31 | 19/12 | 22.34 | 2.73 | 18 | 14.74 | 6.89 | 13 |
| Elshazly et al. (15) | 2020 | Egypt | 62 | NR | 33.52 | 14.51 | 34 | 18.57 | 9.37 | 28 |
| Eltrabili et al. (16) | 2019 | Egypt | 35 | 16/19 | 43.43 | 7.35 | 17 | 22.31 | 13.37 | 13 |
| Farghaly et al. (17) | 2017 | Egypt | 54 | 31/23 | 60.49 | 35.60 | 40 | 47.43 | 51.64 | 14 |
| Ferrari et al. (18) | 2014 | Italy | 46 | 34/12 | 52.43 | 20.27 | 29 | 26 | 6.46 | 17 |
| Kaur et al. (20) | 2022 | India | 50 | NR | 36.57 | 8.22 | 31 | 19.26 | 3.49 | 19 |
| Li et al. (21) | 2021 | China | 101 | 42/59 | 49.48 | 12.5 | 69 | 27.83 | 9.95 | 32 |
| Lin et al. (22) | 2024 | China | 79 | 69/10 | 35 | 7.8 | 57 | 28.7 | 8.1 | 22 |
| Osman et al. (23) | 2017 | Egypt | 68 | NR | 33.50 | 1.56 | 50 | 23.11 | 4.11 | 18 |
| Sabetian et al. (25) | 2024 | Iran | 50 | 39/11 | 51.99 | 21.33 | 26 | 48.33 | 11.55 | 24 |
| Theerawit et al. (10) | 2018 | Thailand | 52 | 38/14 | 37 | 14 | 51 | 28 | 13 | 11 |
| Yoo et al. (26) | 2018 | Korea | 60 | 42/18 | 40.40 | 28.44 | 47 | 24.06 | 25.49 | 13 |
Table 3.
Characteristics of the included studies for RSBI.
| Author | Year | Country | Population | M/F | RSBI | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Success | Failure | |||||||||
| Mean | SD | N | Mean | SD | N | |||||
| Abdelwahed et al. (13) | 2019 | Egypt | 65 | 40/25 | 79.58 | 20 | 51 | 102 | 17.07 | 14 |
| Alam et al. (14) | 2022 | Bangladesh | 31 | 19/12 | 100.46 | 2.84 | 18 | 99 | 3.71 | 13 |
| Elshazly et al. (15) | 2020 | Egypt | 62 | NR | 43.95 | 14 | 34 | 54 | 25.48 | 28 |
| Eltrabili et al. (16) | 2019 | Egypt | 35 | 16/19 | 39 | 18 | 17 | 77 | 30 | 13 |
| Farghaly et al. (17) | 2017 | Egypt | 54 | 31/23 | 58.59 | 26 | 40 | 51 | 20.59 | 14 |
| Ferrari et al. (18) | 2014 | Italy | 46 | 34/12 | 70 | 20 | 29 | 126 | 30.71 | 17 |
| Fossat et al. (19) | 2022 | France | 100 | NR | 56 | 26 | 91 | 56 | 28.3 | 9 |
| Kaur et al. (20) | 2022 | India | 50 | NR | 46.61 | 18. | 31 | 105 | 7.93 | 19 |
| Li et al. (21) | 2021 | China | 101 | 42/59 | 75.68 | 18. | 69 | 105 | 16.07 | 32 |
| Lin et al. (22) | 2024 | China | 79 | 69/10 | 44.57 | 6. | 57 | 73 | 16.85 | 22 |
| Osman et al. (23) | 2017 | Egypt | 68 | NR | 72.18 | 10 | 50 | 114 | 5.48 | 18 |
| Palker et al. (24) | 2018 | USA | 73 | 37/36 | 45.9 | 19 | 53 | 75.5 | 57.4 | 20 |
| Sabetian et al. (25) | 2024 | Iran | 50 | 39/11 | 38.24 | 7 | 26 | 120 | 16.86 | 24 |
| Tenza-Lozano et al. (11) | 2018 | Spain | 69 | 43/26 | 31.35 | 17 | 44 | 40 | 18.86 | 25 |
| Theerawit et al. (10) | 2018 | Thailand | 52 | 38/14 | 55.11 | 25 | 51 | 83 | 53.11 | 11 |
Contrary to the outcomes of this meta-analysis, two referenced studies did not discover any correlation between diaphragmatic excursion and thickening fraction values below the designated cutoff point measured via ultrasound and the outcome of weaning from mechanical ventilation. A recent study characterized extubation failure as the necessity for intubation within 72 hours post-extubation, while another study defined it as the requirement for intubation or death within seven days postextubation.27,34 This contrasts with our investigation, as the studies included in this meta-analysis assessed extubation success within 48 hours following mechanical ventilator weaning.51,54
Even minor differences in measurement among observers could impact the results and introduce heterogeneity; indeed, it is a technique dependent on the observer. Nevertheless, several studies have determined that diaphragmatic ultrasound measurements are replicable. The findings of this study hold significance for clinical application, indicating that diaphragmatic ultrasound is a viable tool in the intensive care unit during spontaneous breathing trials to objectively anticipate successful weaning from mechanical ventilation. It is a convenient, swift, noninvasive, straightforward, and safe technique that does not expose healthcare workers to ionizing radiation.27-34 However, given the observed high heterogeneity, which is common in diagnostic test meta-analyses, the aggregated measurements should be cautiously interpreted, especially across various subgroups of critically ill patients, to ensure personalized determination of the optimal outcome.13,55-59
Conclusions
The findings of this systematic review and meta-analysis indicate that assessing diaphragmatic excursion and diaphragmatic thickening fraction can effectively predict the likelihood of successful weaning from mechanical ventilation. However, notable heterogeneity was observed across the various studies included in the analysis. There is a need for high-quality studies with robust methodologies, particularly randomized clinical trials, to further assess the utility of diaphragmatic ultrasound as a predictor of weaning from mechanical ventilation.
List of acronyms
- MeSH
Medical Subject Heading.
- ICU
Intensive Care Unit.
- PRISMA
Preferred Reporting Items for Systematic reviews and Meta-Analyses.
- SBT
Spontaneous Breathing Trial.
- DE
Diaphragmatic Excursion.
- DTF
Diaphragm Thickening Fraction.
- RSBI
Rapid Shallow Breathing Index.
Funding Statement
Funding: None.
Footnotes
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Zhou P, Zhang Z, Hong Y, et al. The predictive value of serial changes in diaphragm function during the spontaneous breathing trial for weaning outcome: a study protocol. BMJ Open 2017;7:e015043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang L, Chen G, Wang H, Yu W. [Predictive value of combined assessment of diaphragmatic and pulmonary ultrasound for weaning outcomes in mechanical ventilated patients with acute respiratory failure]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 2022;34:941-6. [DOI] [PubMed] [Google Scholar]
- 3.Yin K, Xu Q, Wang J, et al. The predictive value of lung ultrasound combined with central venous oxygen saturation variations in the outcome of ventilator weaning in patients after thoracic surgery. Am J Transl Res 2022;14:8621-31. [PMC free article] [PubMed] [Google Scholar]
- 4.Yao Y, He L, Chen W, et al. Predictive Value of diaphragmatic ultrasonography for the weaning outcome in mechanically ventilated children aged 1-3 years. Front Pediatr 2022;10:840444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xue Y, Zhang Z, Sheng CQ, et al. The predictive value of diaphragm ultrasound for weaning outcomes in critically ill children. BMC Pulm Med 2019;19:270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang L, Muhetaer Y, Zhu L, et al. Is it reasonable to predict weaning by measuring diaphragm activity under ultrasound especially its reduction of excursion? Crit Care 2023;27:309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang J, Duan FJ, Du Y, et al. [The application value of diaphragm ultrasound in the weaning of ventilator for patients undergoing heart valve replacement]. Zhonghua Yi Xue Za Zhi 2021;101:3814-8. [DOI] [PubMed] [Google Scholar]
- 8.Vetrugno L, Orso D, Corradi F, et al. Diaphragm ultrasound evaluation during weaning from mechanical ventilation in COVID-19 patients: a pragmatic, cross-section, multicenter study. Respir Res 2022;23:210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Turton P, S AL, Welters I. A narrative review of diaphragm ultrasound to predict weaning from mechanical ventilation: where are we and where are we heading? Ultrasound J 2019;11:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Theerawit P, Eksombatchai D, Sutherasan Y, et al. Diaphragmatic parameters by ultrasonography for predicting weaning outcomes. BMC Pulm Med 2018;18:175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tenza-Lozano E, Llamas-Alvarez A, Jaimez-Navarro E, Fernández-Sánchez J. Lung and diaphragm ultrasound as predictors of success in weaning from mechanical ventilation. Crit Ultrasound J 2018;10:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abdelwahed WM, Abd Elghafar MS, Amr YM, et al. Prospective study: Diaphragmatic thickness as a predictor index for weaning from mechanical ventilation. J Crit Care 2019;52:10-5. [DOI] [PubMed] [Google Scholar]
- 14.Alam MJ, Roy S, Iktidar MA, et al. Diaphragm ultrasound as a better predictor of successful extubation from mechanical ventilation than rapid shallow breathing index. Acute Crit Care 2022;37:94-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Elshazly MI, Kamel KM, Elkorashy RI, et al. Role of bedside ultrasonography in assessment of diaphragm function as a predictor of success of weaning in mechanically ventilated patients. Tuberc Respir Dis (Seoul) 2020;83:295-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eltrabili HH, Hasanin AM, Soliman MS, et al. Evaluation of diaphragmatic ultrasound indices as predictors of successful liberation from mechanical ventilation in subjects with abdominal sepsis. Respir Care 2019;64:564-9. [DOI] [PubMed] [Google Scholar]
- 17.Farghaly S, Hasan AA. Diaphragm ultrasound as a new method to predict extubation outcome in mechanically ventilated patients. Aust Crit Care 2017;30:37-43. [DOI] [PubMed] [Google Scholar]
- 18.Ferrari G, De Filippi G, Elia F, et al. Diaphragm ultrasound as a new index of discontinuation from mechanical ventilation. Crit Ultrasound J 2014;6:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fossat G, Daillet B, Desmalles E, Boulain T. Does diaphragm ultrasound improve the rapid shallow breathing index accuracy for predicting the success of weaning from mechanical ventilation? Aust Crit Care 2022;35:233-40. [DOI] [PubMed] [Google Scholar]
- 20.Kaur A, Sharma S, Singh VP, et al. Sonographic assessment of diaphragmatic thickening and excursion as predictors of weaning success in the intensive care unit: A prospective observational study. Indian J Anaesth 2022;66:776-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li S, Chen Z, Yan W. Application of bedside ultrasound in predicting the outcome of weaning from mechanical ventilation in elderly patients. BMC Pulm Med 2021;21:217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lin H, Yao M, Qin Z, et al. Predictive values of ultrasonic diaphragm thickening fraction combined with integrative weaning index in weaning patients with mechanical ventilation: a retrospective study. J Cardiothorac Surg 2024;19:66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Osman AM, Hashim RM. Diaphragmatic and lung ultrasound application as new predictive indices for the weaning process in ICU patients. Egyptian J Radiol Nuclear Med 2017;48:61-6. [Google Scholar]
- 24.Palkar A, Narasimhan M, Greenberg H, et al. Diaphragm excursion-time index: a new parameter using ultrasonography to predict extubation outcome. Chest 2018;153:1213-20. [DOI] [PubMed] [Google Scholar]
- 25.Sabetian G, Mackie M, Asmarian N, et al. Ultrasonographic evaluation of diaphragm thickness and excursion: correlation with weaning success in trauma patients: prospective cohort study. J Anesth 2024;38: 354-63. [DOI] [PubMed] [Google Scholar]
- 26.Yoo JW, Lee SJ, Lee JD, Kim HC. Comparison of clinical utility between diaphragm excursion and thickening change using ultrasonography to predict extubation success. Korean J Intern Med 2018;33:331-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parada-Gereda HM, Tibaduiza AL, Rico-Mendoza A, et al. Effectiveness of diaphragmatic ultrasound as a predictor of successful weaning from mechanical ventilation: a systematic review and meta-analysis. Crit Care 2023;27:174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mahmoodpoor A, Fouladi S, Ramouz A, et al. Diaphragm ultrasound to predict weaning outcome: systematic review and meta-analysis. Anaesthesiol Intensive Ther 2022;54:164-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Llamas-Álvarez AM, Tenza-Lozano EM, Latour-Pérez J. Diaphragm and lung ultrasound to predict weaning outcome: systematic review and meta-analysis. Chest 2017;152:1140-50. [DOI] [PubMed] [Google Scholar]
- 30.Li C, Li X, Han H, et al. Diaphragmatic ultrasonography for predicting ventilator weaning: A meta-analysis. Medicine (Baltimore) 2018;97:e10968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Le Neindre A, Philippart F, Luperto M, et al. Diagnostic accuracy of diaphragm ultrasound to predict weaning outcome: A systematic review and meta-analysis. Int J Nurs Stud 2021;117:103890. [DOI] [PubMed] [Google Scholar]
- 32.Ji X, Shi K, Li J, et al. The value of ultrasound in diagnosing metastatic internal mammary lymph nodes in preoperative breast cancer. Gland Surg 2020;9: 1478-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hua-Rong Z, Liang C, Rong L, et al. Ultrasonographic evaluation of diaphragm function in patients with chronic obstructive pulmonary disease: A systematic review and meta-analysis. Medicine (Baltimore) 2022;101:e32560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gao Y, Yin H, Wang MH, Gao YH. Accuracy of lung and diaphragm ultrasound in predicting infant weaning outcomes: a systematic review and meta-analysis. Front Pediatr 2023;11:1211306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lalwani LK, Govindagoudar MB, Singh PK, et al. The role of diaphragmatic thickness measurement in weaning prediction and its comparison with rapid shallow breathing index: a single-center experience. Acute Crit Care 2022;37:347-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kundu R, Baidya D, Anand R, et al. Integrated ultrasound protocol in predicting weaning success and extubation failure: a prospective observational study. Anaesthesiol Intensive Ther 2022;54:156-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kim WY, Suh HJ, Hong SB, et al. Diaphragm dysfunction assessed by ultrasonography: influence on weaning from mechanical ventilation. Crit Care Med 2011;39:2627-30. [DOI] [PubMed] [Google Scholar]
- 38.Khan MT, Munawar K, Hussain SW, et al. Comparing Ultrasound-based Diaphragmatic Excursion with Rapid Shallow Breathing Index as a Weaning Predictor. Cureus 2018;10:e3710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Huang D, Song F, Luo B, et al. Using automatic speckle tracking imaging to measure diaphragm excursion and predict the outcome of mechanical ventilation weaning. Crit Care 2023;27:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Huang D, Ma H, Zhong W, et al. Using M-mode ultra-sonography to assess diaphragm dysfunction and predict the success of mechanical ventilation weaning in elderly patients. J Thorac Dis 2017;9:3177-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.He G, Han Y, Zhan Y, et al. The combined use of parasternal intercostal muscle thickening fraction and P0.1 for prediction of weaning outcomes. Heart Lung 2023;62:122-8. [DOI] [PubMed] [Google Scholar]
- 42.Gok F, Mercan A, Kilicaslan A, et al. Diaphragm and lung ultrasonography during weaning from mechanical ventilation in critically ill patients. Cureus 2021;13:e15057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Garrido-Aguirre E, Ñamendys-Silva SA, Del Moral OR, et al. Diaphragmatic Ultrasonography, a Novel Approach in Critical Care: A Proposal for a New Weaning Index. Ultrasound Q 2020;36:54-8. [DOI] [PubMed] [Google Scholar]
- 44.Fan M, Luo J, Wen H, et al. [Value of the diaphragm movement index tested by ultrosonography for ventilation weaning]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 2018;30:1041-5. [DOI] [PubMed] [Google Scholar]
- 45.Evans D, Shure D, Clark L, et al. Temporary transvenous diaphragm pacing vs. standard of care for weaning from mechanical ventilation: study protocol for a randomized trial. Trials 2019;20:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Er B, Simsek M, Yildirim M, et al. Association of baseline diaphragm, rectus femoris and vastus intermedius muscle thickness with weaning from mechanical ventilation. Respir Med 2021;185:106503. [DOI] [PubMed] [Google Scholar]
- 47.Er B, Mızrak B, Aydemir A, et al. Is diaphragm ultrasound better than rapid shallow breathing index for predicting weaning in critically ill elderly patients? Tuberk Toraks 2023;71:197-202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.El Gharib K, Assaad M, Chalhoub M. Diaphragmatic ultrasound in weaning ventilated patients: a reliable predictor? Expert Rev Respir Med 2022;16:853-5. [DOI] [PubMed] [Google Scholar]
- 49.Dres M, Goligher EC, Dubé BP, et al. Diaphragm function and weaning from mechanical ventilation: an ultrasound and phrenic nerve stimulation clinical study. Ann Intensive Care 2018;8:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dres M, Dubé BP, Goligher E, et al. Usefulness of Parasternal Intercostal Muscle Ultrasound during Weaning from Mechanical Ventilation. Anesthesiology 2020;132: 1114-25. [DOI] [PubMed] [Google Scholar]
- 51.Costanzo DD, Mazza M, Esquinas A. Diaphragm ultrasound in weaning from mechanical ventilation: a last step to predict successful extubation? Acute Crit Care 2022;37:681-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chang JE, Park SH, Do SH, Song IA. Successful weaning from mechanical ventilation in the quadriplegia patient with C2 spinal cord injury undergoing C2-4 spine laminoplasty -A case report. Korean J Anesthesiol 2013;64:545-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Boscolo A, Sella N, Pettenuzzo T, et al. Diaphragm dysfunction predicts weaning outcome after bilateral lung transplant. Anesthesiology 2024;140:126-36. [DOI] [PubMed] [Google Scholar]
- 54.Blanco JB, Esquinas A. Diaphragm evaluation and lung ultrasound score during weaning. Indian J Crit Care Med 2022;26:1054-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bao Q, Zhou M, Liao W, et al. [Impact of hypophosphatemia on weaning from mechanical ventilation]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 2021;33: 821-5. [DOI] [PubMed] [Google Scholar]
- 56.Banerjee A, Mehrotra G. Comparison of lung ultrasound-based weaning indices with rapid shallow breathing index: are they helpful? Indian J Crit Care Med 2018;22:435-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Amara V, Chaudhuri S. Author’s response to diaphragm evaluation and lung ultrasound score during weaning. Indian J Crit Care Med 2022;26:1056-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Al-Husinat L, Jouryyeh B, Rawashdeh A, et al. The role of ultrasonography in the process of weaning from mechanical ventilation in critically ill patients. Diagnostics (Basel) 2024;14:398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Abdel Rahman DA, Saber S, El-Maghraby A. Diaphragm and lung ultrasound indices in prediction of outcome of weaning from mechanical ventilation in pediatric intensive care unit. Indian J Pediatr 2020;87: 413-20. [DOI] [PMC free article] [PubMed] [Google Scholar]


