Summary
Background
Violence against healthcare workers is an escalating public health concern, affecting the quality of care, and causing significant psychological and physical effects on healthcare professionals. This study analysed the trend in aggressions in healthcare settings in the pre-pandemic, pandemic, and post-pandemic periods.
Methods
An observational descriptive study was conducted to analyse reports of violence against healthcare workers from January 2018 to June 2023 at a Local Health Authority “ASL3” in the Liguria region of Italy. The study considered variables such as the severity of aggression, professional category involved, and location of incident. Episodes of violence were classified according to severity by means of a colour-coded system. We used multinomial logistic regression to examine any associations between the pandemic phase and the various factors, while controlling for relevant variables.
Results
The number of reported aggressions rose from 48 in 2018 to 90 in 2022, with a partial count of 35 in the first half of 2023. The pandemic phase saw a rise in incidents classified as Green codes, which accounted for 58.3%, and a significant involvement of District Services. The post-pandemic phase showed a reversion to pre-pandemic levels but with an increase in Yellow codes (5.6%). Nurses were the most frequent victims, with figures ranging from 50.8% to 95.6% over the years. The Emergency Department and Psychiatric Services emerged as the most critical settings of aggressions, with incidents recorded in these areas constituting over half of the total number. However, an increase in violence was also recorded in district healthcare settings during the post-pandemic phase.
Conclusions
There is an urgent need for comprehensive strategies for the prevention of violence in healthcare settings. The increasing trend in violence, especially during the pandemic, necessitates integrated approaches that encompass training, psychological support, security policies, and a strong organizational culture to promote safety and respect. Protecting healthcare workers is crucial to their wellbeing and the quality of healthcare delivery.
Keywords: Healthcare workers, Violence, COVID-19, Pandemic, Aggression
Introduction
Violence against healthcare workers has adverse effects on the quality of their work, causing psychological stress and sleep disturbances, and negatively impacting healthcare provider-patient relationships. Indeed, it significantly affects healthcare settings and the overall quality of care [1-5]. The European Observatory on Risks of the European Agency for Safety and Health at Work (EU-OSHA) has identified violence and harassment as emerging psychosocial risks in terms of safety and health, especially in the healthcare sector, where staff are often exposed to threats and aggressions. In EU member States, workplace violence often goes unrecognised [6]. However, systematic reviews indicate that 60-70% of healthcare workers encounter violence, either physical or psychological, with approximately one-third suffering physical violence [7, 8]. These data underscore the urgent need to address this issue.
Interestingly, the frequency and the reporting of episodes of violence in healthcare settings vary markedly from one country to another. Anglo countries, such as Australia, Canada, England, Ireland, New Zealand, Scotland, and the United States show higher reporting rates; this may be due to greater awareness, and lower tolerance of the phenomenon [7]. In Europe, by contrast, reporting rates are lower, which may reflect a different culture or lower awareness of workplace violence. In this regard, a systematic review conducted in Spain has confirmed that, despite an increasing trend in recent years, episodes of violence are rarely reported and recorded [1-5, 7, 9]. In the United States, violence against healthcare workers is particularly problematic in Emergency Departments, with about one-quarter of physicians experiencing physical violence, and 78% of emergency room physicians reporting some form of violence in the past year [10-13]. In Italy, according to the Ministry of Health’s data, reports of violent acts have dramatically increased in the last 15 years, suggesting that the phenomenon is growing. The occurrence of a single case of violence is sufficient to trigger an audit, as it indicates organizational deficiencies and insufficient awareness of the potential danger of violence within healthcare facilities [14].
A crucial aspect is the widespread underreporting of incidents [15]. According to previous literature, only a small fraction of incidents is reported to the authorities [16]. Underreporting may be due to the perception that the risk of violence is a normal part of healthcare work [17-22], to the lack of organizational support [10, 23-25], and to the fear of consequences of reporting. Some healthcare workers may also feel too ashamed or afraid of the judgment of others to report being victims of violence [18, 26-28]. A study conducted in Istanbul revealed that about 80% of nurses did not report episodes of violence and felt more supported by their colleagues than by the healthcare authorities [29]. Additionally, healthcare staff may be unaware of reporting policies and procedures [30, 31].
To effectively address these issues, an integrated approach is necessary; this must include awareness-raising, training, and the promotion of a culture of safety. Moreover, it is essential to ensure the availability of accessible and confidential reporting procedures nationwide. In response to these needs, in 2007, the Italian Ministry of Health drafted the document “Recommendation for Preventing Acts of Violence against Healthcare Workers” [32]. During the COVID-19 pandemic, healthcare professionals played a central role in safeguarding public health, especially in emergency situations. Paradoxically, this increased the risk of aggression and violence [33, 34].
This observational study investigated trends in violence against healthcare workers in a Local Health Authority in the Liguria region from 2018 to 2023, focusing on pandemic-related changes.
Materials and methods
STUDY DESIGN
We conducted an observational descriptive study on violent episodes against healthcare workers in a Local Health Authority in Liguria, Italy, from 2018 to 2023, and compared the data collected before, during and after the COVID-19 pandemic. The study used data that were completely anonymised and routinely collected by the healthcare organisation for administrative and reporting purposes. The research adhered to robust research practices, and was aligned with the principles of the Declaration of Helsinki.
COLLECTION OF REPORTS
In Local Health Authority 3 (ASL3) - Liguria Region Healthcare System, a specific procedure for reporting and managing acts of aggression against healthcare workers has been implemented, as outlined in the resolution “Recommendations for Preventing Acts of Violence Against Healthcare Workers” (“Raccomandazioni per prevenire atti di violenza nei confronti degli operatori”; third revision published on December 24, 2019).
The reporting procedure involves filling in a form, which is available on the corporate intranet. In cases of violence, affected healthcare workers complete this form, and send it to several key individuals within the organization, including the Director/Manager of their own Operational Unit, the Director of the Department concerned, the Manager of the Prevention and Protection Service, and the secretariats of the various Departments involved, depending on the location of the incident.
Upon receiving the report, the Director/Manager of the Operational Unit where the incident occurred is responsible for organizing an internal audit. This audit involves all relevant personnel and the safety representative. It is aimed at analysing the incident and identifying preventive and corrective strategies. The Prevention and Protection Service, upon receiving the report, plans, and activates corrective actions, which may include meetings at the location of the incident. Furthermore, in the presence of a “sentinel event”, the Service sends a formal communication to the Clinical Risk Management Department. The Clinical Risk Management Department, in response to a sentinel event, activates the procedures outlined in the Ministerial Recommendation “Reporting and Management of Sentinel Events” [14].
STUDY VARIABLES
The study analysed reports collected by ASL3 from January 1, 2018, to June 30, 2023. From these reports, we extracted data on the number of individuals assaulted in cases of aggression involving more than one healthcare worker in a single incident. The data collected from the reporting form included details such as the context of the event (location, date, time), the roles and qualifications of the healthcare workers involved, whether the aggressor was previously known to the service, and the types of aggression experienced. Roles and qualifications are listed as: Medical Doctors, Nurses, Health Care Assistants, and Other Health Staff, such as prevention technicians, pharmacists, psychologists, radiology technicians, social workers, security guards, and administrative staff.
Within the Local Health Authority’s jurisdiction, there are 6 Health Districts, each with outpatient services and facilities. The area is served by 4 hospitals, which include a variety of wards; one of these hospitals has an emergency department. Psychiatric services are available in all 6 districts: in 2 of the hospitals, and in various care centres throughout the territory [35].
In Italy, COVID-19 was declared an emergency on January 31, 2020 [36], signalling the beginning of the pandemic phase; the state of emergency was revoked on March 31, 2022 [37]. To ensure a coherent analytical framework and facilitate a consistent annual comparative analysis, considering that access to healthcare services can vary with the change in seasons and annual period, we divided the study period into three phases; the first phase (2018 and 2019) was defined as pre-pandemic, i.e. before the pandemic’s extensive socio-economic and public health ramifications; the second phase (2020 and 2021) was defined as the pandemic phase, i.e. when stringent emergency measures were in force, notably social distancing and mobility restrictions; the third, or post-pandemic phase, encompassed the years 2022 and 2023, when restrictions were substantially relaxed and large-scale vaccination had significantly mitigated the pandemic’s public health impact.
CLASSIFICATION OF VIOLENT EPISODES
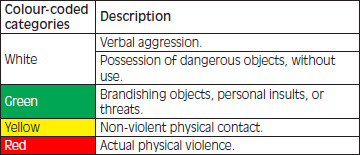
Violent episodes were classified according to severity by means of a colour-coded system: White code (for verbal aggression, possession of dangerous objects, without use), Green code (brandishing objects, personal insults or threats), Yellow code (non-violent physical contact), and Red code (actual physical violence), in addition to any other damage caused by the aggressor within the facility (Tab. I).
Tab. I.
Colour-coded classification of aggression against healthcare workers.
|
STATISTICAL METHODS
To analyse the data collected, we adopted a descriptive approach in order to provide a clear and detailed overview of violent episodes, and their characteristics. To investigate the relationship between the phase of the pandemic and profession, place, and colour code, we conducted a multinomial logistic regression analysis. We controlled for month of the year, time of day, and whether the aggressor was known to the healthcare staff. Additionally, we controlled for profession, place, and colour code, but only when these were not the specific outcome variable under investigation. Results are presented as regression coefficients (Coeff.), and 95% confidence intervals (95% CI). Analyses were performed by means of Stata 15.0 MP.
Results
The characteristics of aggressions are presented in Table II.
Tab. II.
Characteristics of reported aggressions.
| Total | 2018 | 2019 | 2020 | 2021 | 2022 | 2023 | Pre-pandemic | Pandemic | Post-pandemic | χ2 test | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | 396 | 48 | 107 | 63 | 52 | 90 | 36 | 155 | 115 | 126 | |
| Colour Code | |||||||||||
| White | 76 | 10 | 24 | 12 | 5 | 12 | 13 | 34 | 17 | 25 | 0.003 |
| % | 19.2 | 20.8 | 22.4 | 19.1 | 9.6 | 13.3 | 36.1 | 21.9 | 14.8 | 19.8 | |
| Green | 193 | 19 | 41 | 30 | 37 | 49 | 17 | 60 | 67 | 66 | |
| % | 48.7 | 39.6 | 38.3 | 47.6 | 71.2 | 54.4 | 47.2 | 38.7 | 58.3 | 52.4 | |
| Yellow | 43 | 9 | 19 | 5 | 3 | 5 | 2 | 28 | 8 | 7 | |
| % | 10.9 | 18.8 | 17.8 | 7.9 | 5.8 | 5.6 | 5.6 | 18.1 | 7.0 | 5.6 | |
| Red | 84 | 10 | 23 | 16 | 7 | 24 | 4 | 33 | 23 | 28 | |
| % | 21.2 | 20.8 | 21.5 | 25.4 | 13.5 | 26.7 | 11.1 | 21.3 | 20.0 | 22.2 | |
| Professional | |||||||||||
| Doctor | 77 | 4 | 20 | 22 | 16 | 4 | 11 | 24 | 38 | 15 | < 0.001 |
| % | 19.4 | 8.3 | 18.7 | 34.9 | 30.8 | 4.4 | 30.6 | 15.5 | 33.0 | 11.9 | |
| Nurse | 276 | 42 | 69 | 32 | 26 | 86 | 21 | 111 | 58 | 107 | |
| % | 69.7 | 87.5 | 64.5 | 50.8 | 50.0 | 95.6 | 58.3 | 71.6 | 50.4 | 84.9 | |
| Care Assistant | 28 | 1 | 12 | 8 | 5 | 0 | 2 | 13 | 13 | 2 | |
| % | 7.1 | 2.1 | 11.2 | 12.7 | 9.6 | 0.0 | 5.6 | 8.4 | 11.3 | 1.6 | |
| Other Health Staff | 15 | 1 | 6 | 1 | 5 | 0 | 2 | 7 | 6 | 2 | |
| % | 3.8 | 2.1 | 5.6 | 1.6 | 9.6 | 0.0 | 5.6 | 4.5 | 5.2 | 1.6 | |
| Place | |||||||||||
| District Service | 71 | 2 | 9 | 8 | 20 | 22 | 10 | 11 | 28 | 32 | < 0.001 |
| % | 17.9 | 4.2 | 8.4 | 12.7 | 38.5 | 24.4 | 27.8 | 7.1 | 24.4 | 25.4 | |
| Hospital Ward | 63 | 0 | 24 | 1 | 10 | 20 | 8 | 24 | 11 | 28 | |
| % | 15.9 | 0.0 | 22.4 | 1.6 | 19.2 | 22.2 | 22.2 | 15.5 | 9.6 | 22.2 | |
| Emergency Department | 101 | 28 | 20 | 9 | 6 | 28 | 10 | 48 | 15 | 38 | |
| % | 25.5 | 58.3 | 18.7 | 14.3 | 11.5 | 31.1 | 27.8 | 31.0 | 13.0 | 30.2 | |
| Psychiatric Service | 161 | 18 | 54 | 45 | 16 | 20 | 8 | 72 | 61 | 28 | |
| % | 40.7 | 37.5 | 50.5 | 71.4 | 30.8 | 22.2 | 22.2 | 46.5 | 53.0 | 22.2 | |
| Aggressor Identity | |||||||||||
| Unknown | 115 | 19 | 25 | 11 | 12 | 33 | 15 | 44 | 23 | 48 | 0.008 |
| % | 29.0 | 39.6 | 23.4 | 17.5 | 23.1 | 36.7 | 41.7 | 28.4 | 20.0 | 38.1 | |
| Known | 281 | 29 | 82 | 52 | 40 | 57 | 21 | 111 | 92 | 78 | |
| % | 71.0 | 60.4 | 76.6 | 82.5 | 76.9 | 63.3 | 58.3 | 71.6 | 80.0 | 61.9 | |
DESCRIPTION OF INCIDENTS OVER THE YEARS
In 2018, 48 incidents of aggression were reported. These incidents were classified by severity codes: White codes (20.8%), Green codes (39.6%), Yellow codes (18.8%), and Red codes (20.8%). The majority of the personnel involved were Nurses (87.5%), followed by Medical Doctors (8.3%), Health Care Assistants (2.1%), and Other Healthcare Staff (2.1%). A significant portion of these incidents (58.3%) occurred in the Emergency Department, with others happening in Psychiatric Services (37.5%) and District Services (4.2%). Notably, in approximately 60.4% of cases, the aggressor was already known to the healthcare service.
In 2019, 107 incidents of aggression were recorded: White codes (22.4%), Green codes (38.3%), Yellow codes (17.8%), and Red codes (21.5%). The personnel involved varied, with 64.5% being Nurses, 18.7% Medical Doctors, 5.6% other health staff, and 11.2% Health Care Assistants. These incidents occurred in various healthcare settings, including the Emergency Department (18.7%), Psychiatric Services (50.5%), District Services (8.4%), and Hospital Wards (22.4%). In 76.6% of cases, the aggressor was known to the healthcare service.
In 2020, 63 incidents of aggression were registered: White codes (19.1%), Green codes (47.6%), Yellow codes (7.9%), and Red codes (25.4%). The majority of personnel affected were Nurses (50.8%), followed by Medical Doctors (34.9%), Health Care Assistants (12.7%), and Other Healthcare Staff (1.6%). Incidents occurred in various healthcare settings, including the Emergency Department (14.3%), Psychiatric Services (71.4%), District Services (12.7%), and Hospital Wards (1.6%). In 82.5% of cases, the aggressor was known to the healthcare service.
In 2021, 52 incidents of aggression were reported: White codes (9.6%), Green codes (71.2%), Yellow codes (5.8%), and Red codes (13.5%). The personnel involved were: Nurses (50.0%), Medical Doctors (30.8%), Health Care Assistants (9.6%), and Other Healthcare Staff (9.6%). The majority of these incidents occurred in District Services (38.5%), followed by Psychiatric Services (30.8%), the Emergency Department (11.5%), and Hospital Wards (19.2%). In 2021, 76.9% of aggressors was known to the healthcare service.
In 2022, there were 90 documented incidents of aggression: White codes (13.3%), Green codes (54.4%), Yellow codes (5.6%), and Red codes (26.7%). Nearly all the personnel involved were Nurses (95.6%), with a smaller percentage of Medical Doctors (4.4%). Incidents occurred in various healthcare settings: the Emergency Department (31.1%), Psychiatric Services (22.2%), District Services (24.4%), and Hospital Wards (22.2%). In 63.3% of cases, the aggressor was known to the healthcare service.
In the first half of 2023, there were reports of 36 incidents of aggression: White codes (36.1%), Green codes (47.2%), Yellow codes (5.6%), and Red codes (11.1%). The personnel involved were Nurses (58.3%), Medical Doctors (30.6%), Health Care Assistants (5.6%), and Other Healthcare Staff (5.6%). These incidents took place in various locations: District Services (27.8%), the Emergency Department (27.8%), Psychiatric Services (22.2%), and Hospital Wards (22.2%). In 58.3% of cases, the aggressor was known to the healthcare service.
DESCRIPTION OF AGGRESSIONS DURING THE PANDEMIC PHASES
Trends in the characteristics of aggressions during the various phases of the pandemic are illustrated in Figure 1.
Fig. 1.
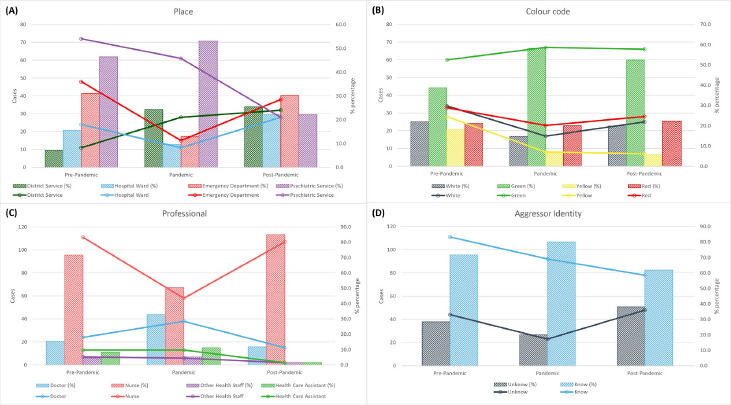
Description of aggressions by pandemic phases.
In the pre-pandemic phase, 155 incidents of aggression were reported; these were classified as White codes (21.9%), Green codes (38.7%), Yellow codes (18.1%), and Red codes (21.3%). Nurses were the most frequently involved professionals (71.6%), followed by Doctors (15.5%), Health Care Assistants (8.4%), and Other Healthcare Staff (4.5%). The majority of incidents occurred in Psychiatric Services (46.5%) and the Emergency Department (31.0%), with District Services (7.1%) and Hospital Wards (15.5%) accounting for the remainder. Known aggressors were involved in the majority of cases (71.6%).
During the pandemic phase, 115 incidents were recorded: White codes (14.8%), Green codes (58.3%), Yellow codes (7.0%), and Red codes (20.0%). Most victims were Nurses (50.4%) or Doctors (33.0%), though other health staff (5.2%), and Health Care Assistants (11.3%) were also involved. Psychiatric Services saw the majority of incidents (53.0%), followed by District Services (24.4%), the Emergency Department (13.0%), and Hospital Wards (9.6%). The proportion of known aggressors was the highest (80.0%).
In the post-pandemic phase, 126 incidents were documented: White codes (19.8%), Green codes (52.4%), Yellow codes (5.6%), and Red codes (22.2%). Incidents involving Nurses (84.9%), Doctors (11.9%), Other Healthcare Staff (1.6%), and Health Care Assistants (1.6%) were recorded. Increases were observed in the Emergency Department (30.2%) and District Services (25.4%), with Hospital Wards (22.2%) also reported, while aggressions in Psychiatric Services decreased (22.2%). Known aggressors showed a decline from the pandemic phase (61.9%).
The χ² test revealed significant differences across the pandemic phases, in terms of the colour codes of the incidents, the professional groups involved and the locations of the aggression. Additionally, the ratio of known to unknown aggressors differed significantly, with the number of known aggressors increasing during the pandemic phase.
STATISTICAL ANALYSES
We observed that, during the pandemic phase, the probability of having a Green code was higher than that of having a White code (Coef. 0.836, p-value 0.029, 95% CI 0.084 to 1.59). Conversely, in the post-pandemic phase, the probability of having a Yellow code was lower than that of having a White code (Coef. -1.174, p-value 0.034, 95% CI -2.260 to -0.087) (Fig. 2).
Fig. 2.
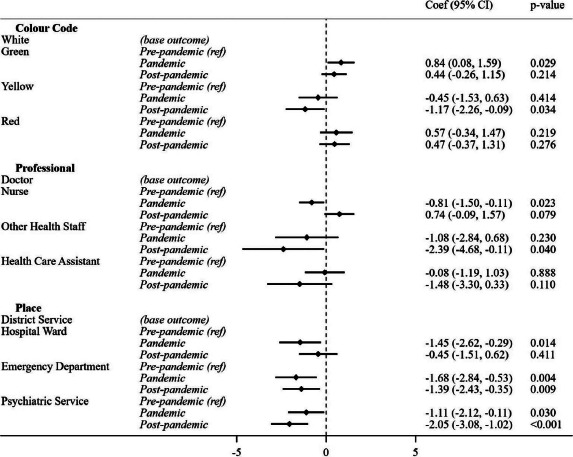
Association of Pandemic Phase with Colour Code, Professional Category, and Place of Aggression.
Regarding professions, when comparing trends with those concerning assaults on doctors, nurses were less likely to be involved during the pandemic phase (Coef. -0.807, p-value 0.023, 95% CI -1.504 to -0.110). Moreover, Other Health Staff were less involved during the post-pandemic phase (Coef. -2.394, p-value 0.040, 95% CI -4.677 to -0.112) (Fig. 2).
Regarding the place of aggression, the probability of aggression occurring in a Hospital Ward was lower than in District Services during the pandemic phase (Coef. -1.452, p-value 0.014, 95% CI -2.616 to -0.289). In the Emergency Department, a decrease was observed both during (Coef. -1.684, p-value 0.004, 95% CI -2.839 to -0.528) and after the pandemic (Coef. -1.387, p-value 0.009, 95% CI -2.426 to -0.347). Additionally, in Psychiatric Services, the probability was lower during (Coef. -1.113, p-value 0.030, 95% CI -2.117 to -0.110) and after the pandemic (Coef. -2.050, p-value < 0.001, 95% CI -3.081 to -1.019) (Fig. 2).
Multinomial logistic regression analysis was conducted to assess the association between the Pandemic Phase and Colour Code, Profession, or Place of aggression. This analysis was controlled for the month of the year, the time of day when the event occurred, aggressor identity, and for professional category, place, and colour code, if these were not the outcome. Results are presented as regression coefficients (Coef.) and 95% confidence intervals (95% CI).
Discussion
The data on reported aggressions against healthcare workers in Genoa’s ASL3 from January 2018 to June 2023 show a significant increase: from 48 in 2018 to 90 in 2022, with a partial count of 35 in the first half of 2023. This local pattern also reflects a global trend, where verbal violence is more prevalent than physical violence [38]. The classification of aggressions into colour-coded categories of severity provides further insight into the nature of the violence, underscoring the higher frequency of verbal incidents [34]. During the pandemic phase, Green codes increased, while in the post-pandemic phase, the types of aggressions reverted to a pattern similar to that observed in the pre-pandemic phase, but with a significant increase in Yellow codes.
The predominant incidence of aggressions against nursing staff – ranging from 50.8% to 95.6% in the years under review – highlights the particular vulnerability of these healthcare workers. This finding aligns with global trends and calls for specific attention to the safety of this professional category. Indeed, targeted prevention strategies are needed in order to ensure a safe working environment. This pattern, which has been observed in various settings, healthcare systems and countries [9, 25, 39-45], suggests that the greater exposure of Nurses to violence may be due to their closer contact with patients and their families. In our analysis, nurses consistently emerged as the group most frequently targeted throughout the study period. During the pandemic phase, however, we observed a marked decrease in both the absolute numbers, and the percentages of nurses involved in aggressive incidents. This was probably because of the reduced patient and family interactions due to pandemic-related restrictions [46]. In the post-pandemic phase, the frequency of aggressions involving healthcare workers returned to pre-pandemic levels, with nurses again constituting the majority of victims, albeit in a slightly higher proportion than during the pre-pandemic phase. Remarkably, the incidence of aggression towards physicians significantly increased during the pandemic but reverted to lower levels in the subsequent post-pandemic phase. It is also noteworthy that non-medical and non-nursing HCWs, including administrative, and support staff, consistently accounted for only a small fraction of cases of aggression, a trend that further declined over time.
Of particular interest are the data regarding the locations of aggression. The majority of violent episodes were recorded in the Emergency Department and Psychiatric Services, a trend consistent with the previous literature [8]. During the pandemic phase, however, District Services saw a significant increase in aggressive behaviour, while other healthcare settings, particularly emergency services, registered a decrease. This could be attributed to the reduced use of emergency services during the pandemic, and patients’ preference to avoid the Emergency Department and the hospital setting whenever possible [47]. In the post-pandemic phase, the picture that emerged was significantly different from that seen during the pre-pandemic phase, in that the hospital setting and territorial services were more frequently involved. Clearly, there is a need for specific preventive and safety measures in these areas, so as to reduce the risk of aggression, and improve staff safety. Future trends will also need to be monitored in order to understand how to adapt measures to counteract emerging phenomena in new healthcare settings, especially in light of the changes that will be implemented by the National Recovery and Resilience Plan [48].
The high percentage of aggressors already known to healthcare services, which increased from 60.4% to 76.9%, indicates the need for a proactive approach to managing relationships, and preventing conflictual situations. In this regard, the early identification of individuals at risk of committing violence can significantly contribute to prevention and staff protection [45]. These data are particularly interesting, as they show that aggressive behaviour is enacted even when the perpetrator is not protected by anonymity, and deliberately risks legal repercussions. The peak of known aggressors was recorded during the pandemic phase; this could have been due to entry screening, and greater control of patient flows [36, 46].
When analysing the phenomena associated with the various pandemic phases, we observed a greater involvement of nursing staff during the post-pandemic phase, along with an increase in Green and Red codes during the pandemic phase. The increased involvement of nurses during the post-pandemic phase aligns with previous literature [9, 25, 39-45], but further investigation is needed in order to explain this significant increase. Also interesting is the increase in Green and Red codes, compared with White codes, during the pandemic [33]. Despite the reduction in non-urgent services provided during the pandemic, the level of reporting remained largely unchanged, and the severity seemed to increase [47].
There are several areas that require further research. Indeed, it would be useful to explore regional or national differences in experiences of violence, and to assess the effectiveness of specific prevention and intervention strategies. Research should also investigate the long-term impact of violence on healthcare staff, including effects on staff turnover and the quality of care.
STRENGTHS AND LIMITATIONS
The primary limitation of this study is its reliance on self-reported data on incidents of aggression, which may have resulted in underreporting. Indeed, voluntary reporting may be prone to errors and inaccuracies [49]. Secondly, although the study focused on the specific context of ASL3, the findings seem to be applicable to similar settings, given the substantial number of healthcare workers and patients involved and the diversity of facilities and services provided. Moreover, this study did not explore the extent of underreporting, nor did it examine the reasons behind the decision to report or not report incidents. Additionally, the study did not analyse the frequency of reports or estimate the overall prevalence of incidents of aggression. Lastly, regarding 2023, only data from the first semester were available, and we did not conduct analyses of prevalence or incidence; however, on comparing the first and second semesters of each year, the proportions of events were consistent. Despite this, the study is based on the most complete and credible official data available for the healthcare setting considered.
POLICY
The systematic collection and analysis of incidents of aggression against healthcare workers are crucial to comprehending the risks faced by these people and highlight significant ethical and social concerns. Establishing a secure and respectful working environment for healthcare professionals is imperative and tackling the underlying causes of violence in healthcare settings, including societal, economic, and cultural factors, is a collective responsibility. Training staff to recognise, manage and de-escalate potentially violent situations is pivotal, and implementing specific training programmes can empower staff with effective conflict management skills, thereby mitigating the risk of escalation and augmenting overall safety. However, an efficacious approach to managing violence in healthcare settings demands a collaborative, interdisciplinary strategy that incorporates the expertise of psychologists, social workers, and other specialists. The present research underscores the need for healthcare policies that address violence against healthcare workers by integrating preventive strategies into policy planning and ensuring that sufficient resources are allocated for staff safety and welfare. The overarching aims are to raise collective awareness of this issue, and to enact effective strategies prevention, in order to guarantee a safe working environment for individuals who are dedicated to the care of others.
Conclusions
The data collected from January 2018 to June 2023 reveal an escalating trend of violence against healthcare workers, particularly in new healthcare settings, such as District Services, which have been enhanced due to the COVID-19 pandemic. While no significant difference emerged between the post-pandemic and the pre-pandemic phases, in terms of the type of aggression or personnel involved, the pandemic phase saw a shift in aggressions in terms of severity, healthcare settings, and staff involved.
This analysis underscores the urgent need for effective prevention policies and strategies to safeguard healthcare workers. Its findings offer a robust foundation for developing targeted interventions and emphasize the importance of an integrated approach that includes not just physical security but also organisational improvement and staff training. Ensuring that healthcare workers operate in a safe and protected environment is paramount in order to deliver high-quality healthcare and guarantee patient safety.
Acknowledgements
We thank the ASL3 Healthcare System of the Liguria Region for allowing us to use the data for this study.
Conflict of interest statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Data availability statement
The anonymised data presented in the study can be provided upon request and authorisation from the data-holding authority.
Authors’ contributions
GS, SR, and BR: conceived and supervised the study, and devised its methodology. NC and AG: contributed to the acquisition of data. MM and GS: analysed the data. GS, MM, AMLDM, and EC: wrote the first draft of the manuscript. BR and GS: had final responsibility for the decision to submit for publication. All authors reviewed, and edited the manuscript, contributed to the article, and approved the submitted version.
History
Received on December 10, 2023. Accepted on May 9, 2024.
Figures and tables
References
- [1].Ielapi N, Andreucci M, Bracale UM, Costa D, Bevacqua E, Giannotta N, Mellace S, Buffone G, Cerabona V, Arturi F, Provenzano M, Serra R. Workplace violence towards healthcare workers: an Italian cross-sectional survey. Nurs Rep 2021;11:758-64. https://doi.org/10.3390/nursrep11040072. 10.3390/nursrep11040072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Hamdan M, Abu Hamra A. Workplace violence towards workers in the emergency departments of Palestinian hospitals: a cross-sectional study. Hum Resour Health 2015;13:28. https://doi.org/10.1186/s12960-015-0018-2. 10.1186/s12960-015-0018-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Tucker JD, Cheng Y, Wong B, Gong N, Nie JB, Zhu W, McLaughlin MM, Xie R, Deng Y, Huang M, Wong WC, Lan P, Liu H, Miao W, Kleinman A, Patient-Physician Trust Project Team . Patient-physician mistrust and violence against physicians in Guangdong Province, China: a qualitative study. BMJ Open 2015;5:e008221. https://doi.org/10.1136/bmjopen-2015-008221. 10.1136/bmjopen-2015-008221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Sun T, Gao L, Li F, Shi Y, Xie F, Wang J, Wang S, Zhang S, Liu W, Duan X, Liu X, Zhang Z, Li L, Fan L. Workplace violence, psychological stress, sleep quality and subjective health in Chinese doctors: a large cross-sectional study. BMJ Open 2017;7:e017182. https://doi.org/10.1136/bmjopen-2017-017182. 10.1136/bmjopen-2017-017182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Davey K, Ravishankar V, Mehta N, Ahluwalia T, Blanchard J, Smith J, Douglass K. A qualitative study of workplace violence among healthcare providers in emergency departments in India. Int J Emerg Med 2020;13:33. https://doi.org/10.1186/s12245-020-00290-0. 10.1186/s12245-020-00290-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Workplace Violence and Harassment: a European Picture. [cited 2023 Dec 5]; Available at: https://osha.europa.eu/en/publications/workplace-violence-and-harassment-european-picture (Accessed on: 5/12/2023).
- [7].Spector PE, Zhou ZE, Che XX. Nurse exposure to physical and nonphysical violence, bullying, and sexual harassment: a quantitative review. Int J Nurs Stud 2014;51:72-84. https://doi.org/10.1016/j.ijnurstu.2013.01.010. 10.1016/j.ijnurstu.2013.01.010 [DOI] [PubMed] [Google Scholar]
- [8].Liu J, Gan Y, Jiang H, Li L, Dwyer R, Lu K, Yan S, Sampson O, Xu H, Wang C, Zhu Y, Chang Y, Yang Y, Yang T, Chen Y, Song F, Lu Z. Prevalence of workplace violence against healthcare workers: a systematic review and meta-analysis. Occup Environ Med 2019;76:927-37. https://doi.org/10.1136/oemed-2019-105849. 10.1136/oemed-2019-105849 [DOI] [PubMed] [Google Scholar]
- [9].Serrano Vicente MI, Fernández Rodrigo MT, Satústegui Dordá PJ, Urcola Pardo F. Agresiones a profesionales del sector sanitario en España, revisión sistemática. Rev Esp Salud Pública 2019;93:e201910097. [PubMed] [Google Scholar]
- [10].Kowalenko T, Gates D, Gillespie GL, Succop P, Mentzel TK. Prospective study of violence against ED workers. Am J Emerg Med 2013;31:197-205. https://doi.org/10.1016/j.ajem.2012.07.010. 10.1016/j.ajem.2012.07.010 [DOI] [PubMed] [Google Scholar]
- [11].Kowalenko T, Cunningham R, Sachs CJ, Gore R, Barata IA, Gates D, Hargarten SW, Josephson EB, Kamat S, Kerr HD, McClain A. Workplace violence in emergency medicine: current knowledge and future directions. J Emerg Med 2012;43:523-31. https://doi.org/10.1016/j.jemermed.2012.02.056. 10.1016/j.jemermed.2012.02.056 [DOI] [PubMed] [Google Scholar]
- [12].Pompeii LA, Schoenfisch AL, Lipscomb HJ, Dement JM, Smith CD, Upadhyaya M. Physical assault, physical threat, and verbal abuse perpetrated against hospital workers by patients or visitors in six U.S. hospitals. Am J Ind Med 2015;58:1194-204. https://doi.org/10.1002/ajim.22489. 10.1002/ajim.22489 [DOI] [PubMed] [Google Scholar]
- [13].Behnam M, Tillotson RD, Davis SM, Hobbs GR. Violence in the emergency department: a national survey of emergency medicine residents and attending physicians. J Emerg Med 2011;40:565-79. https://doi.org/10.1016/j.jemermed.2009.11.007. 10.1016/j.jemermed.2009.11.007 [DOI] [PubMed] [Google Scholar]
- [14].Monitoraggio eventi sentinella. Available at: https://www.salute.gov.it/portale/sicurezzaCure/dettaglioContenutiSicurezzaCure.jsp?lingua=italiano&id=238&area=qualita&menu=vuoto (Accessed on: 05/12/2023).
- [15].Brunetti L, Bambi S. Le aggressioni nei confronti degli infermieri dei dipartimenti di emergenza: revisione della letteratura internazionale. Prof Inferm 2013;66:109-16. https://doi.org/10.7429/pi.2013.662109. 10.7429/pi.2013.662109 [DOI] [PubMed] [Google Scholar]
- [16].Lyneham J. Violence in New South Wales emergency departments. Aust J Adv Nurs 2000;18:8-17. [PubMed] [Google Scholar]
- [17].Civilotti C, Berlanda S, Iozzino L. Hospital-based healthcare workers victims of workplace violence in Italy: a scoping review. Int J Environ Res Public Health 2021;18:5860. https://doi.org/10.3390/ijerph18115860. 10.3390/ijerph18115860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Crilly J, Chaboyer W, Creedy D. Violence towards emergency department nurses by patients. Accid Emerg Nurs 2004;12:67-73. https://doi.org/10.1016/j.aaen.2003.11.003. 10.1016/j.aaen.2003.11.003 [DOI] [PubMed] [Google Scholar]
- [19].Pich J, Hazelton M, Sundin D, Kable A. Patient-related violence at triage: A qualitative descriptive study. Int Emerg Nurs 2011;19:12-9. https://doi.org/10.1016/j.ienj.2009.11.007. 10.1016/j.ienj.2009.11.007 [DOI] [PubMed] [Google Scholar]
- [20].Ayasreh IR, Hayajneh FA. Workplace violence against emergency nurses: a literature review. Crit Care Nurs Q 2021;44:187-202. https://doi.org/10.1097/CNQ.0000000000000353. 10.1097/CNQ.0000000000000353 [DOI] [PubMed] [Google Scholar]
- [21].Pich JV, Kable A, Hazelton M. Antecedents and precipitants of patient-related violence in the emergency department: Results from the Australian VENT Study (Violence in Emergency Nursing and Triage). Australas Emerg Nurs J 2017;20:107-13. https://doi.org/10.1016/j.aenj.2017.05.005. 10.1016/j.aenj.2017.05.005 [DOI] [PubMed] [Google Scholar]
- [22].Hesketh KL, Duncan SM, Estabrooks CA, Reimer MA, Giovannetti P, Hyndman K, Acorn S. Workplace violence in Alberta and British Columbia hospitals. Health Policy 2003;63:311-21. https://doi.org/10.1016/s0168-8510(02)00142-2. 10.1016/s0168-8510(02)00142-2 [DOI] [PubMed] [Google Scholar]
- [23].Zafar W, Siddiqui E, Ejaz K, Shehzad MU, Khan UR, Jamali S, Razzak JA. Health care personnel and workplace violence in the emergency departments of a volatile metropolis: results from Karachi, Pakistan. J Emerg Med 2013;45:761-72. https://doi.org/10.1016/j.jemermed.2013.04.049. 10.1016/j.jemermed.2013.04.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].AbuAlRub RF, Al Khawaldeh AT. Workplace physical violence among hospital nurses and physicians in underserved areas in Jordan. J Clin Nurs 2014;23:1937-47. https://doi.org/10.1111/jocn.12473. 10.1111/jocn.12473 [DOI] [PubMed] [Google Scholar]
- [25].Algwaiz WM, Alghanim SA. Violence exposure among health care professionals in Saudi public hospitals. A preliminary investigation. Saudi Med J 2012;33:76-82. [PubMed] [Google Scholar]
- [26].Rose M. A survey of violence toward nursing staff in one large Irish Accident and Emergency Department. J Emerg Nurs 1997;23:214-9. https://doi.org/10.1016/s0099-1767(97)90010-6. 10.1016/s0099-1767(97)90010-6 [DOI] [PubMed] [Google Scholar]
- [27].Eslamian J, Fard SH, Tavakol K, Yazdani M. The effect of anger management by nursing staff on violence rate against them in the emergency unit. Iran J Nurs Midwifery Res 2010;15(Suppl 1):337-42. [PMC free article] [PubMed] [Google Scholar]
- [28].Luck L, Jackson D, Usher K. Innocent or culpable? Meanings that emergency department nurses ascribe to individual acts of violence. J Clin Nurs 2008;17:1071-8. https://doi.org/10.1111/j.1365-2702.2006.01870.x. 10.1111/j.1365-2702.2006.01870.x [DOI] [PubMed] [Google Scholar]
- [29].Pinar R, Ucmak F. Verbal and physical violence in emergency departments: a survey of nurses in Istanbul, Turkey. J Clin Nurs 2011;20:510-7. https://doi.org/10.1111/j.1365-2702.2010.03520.x. 10.1111/j.1365-2702.2010.03520.x [DOI] [PubMed] [Google Scholar]
- [30].Kitaneh M, Hamdan M. Workplace violence against physicians and nurses in Palestinian public hospitals: a cross-sectional study. BMC Health Serv Res 2012;12:469. https://doi.org/10.1186/1472-6963-12-469. 10.1186/1472-6963-12-469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Rafeea F, Al Ansari A, Abbas EM, Elmusharaf K, Abu Zeid MS. Violence toward health workers in Bahrain Defense Force Royal Medical Services’ emergency department. Open Access Emerg Med 2017;9:113-21. https://doi.org/10.2147/OAEM.S147982. 10.2147/OAEM.S147982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Ministero della Salute, Dipartimento della Qualità Direzione Generale della Programmazione Sanitaria dei Livelli di Assistenza e dei Principi Etici di Sistema Ufficio III Raccomandazione per prevenire gli atti di violenza a danno degli operatori sanitari. 2007. Available at: https://www.salute.gov.it/imgs/C_17_pubblicazioni_721_allegato.pdf (Accessed on: 23/03/2024).
- [33].Zhang S, Zhao Z, Zhang H, Zhu Y, Xi Z, Xiang K. Workplace violence against healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Environ Sci Pollut Res Int 2023;30:74838-52. https://doi.org/10.1007/s11356-023-27317-2. 10.1007/s11356-023-27317-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Ministero della salute. Osservatorio Nazionale sulla Sicurezza degli Esercenti le Professioni Sanitarie e socio-sanitarie Relazione attività anno 2022. Available at: https://www.salute.gov.it/portale/documentazione/p6_2_2_1.jsp?lingua=italiano&id=3302 (Accessed on: 23/03/2024).
- [35].Sistema Sanitario Regione Ligure. Asl3 - Azienda Sanitaria Ligure 3. Available at: https://www.asl3.liguria.it/ (Accessed on: 23/03/2024).
- [36].Consiglio dei Ministri - Italy. Delibera del Consiglio dei Ministri 31 gennaio 2020. GU Serie Generale n. 26. 2020. Available at: https://www.gazzettaufficiale.it/eli/id/2020/02/01/20A00737/sg (Accessed on: 23/03/2024).
- [37].Presidente della Repubblica - Italy. Decreto-Legge 24 marzo 2022, n. 24. GU Serie Generale n. 70. 2022. Available at: https://www.gazzettaufficiale.it/eli/id/2022/03/24/22G00034/sg (Accessed on: 23/03/2024).
- [38].Rosenthal LJ, Byerly A, Taylor AD, Martinovich Z. Impact and Prevalence of Physical and Verbal Violence Toward Healthcare Workers. Psychosomatics 2018;59:584-90. https://doi.org/10.1016/j.psym.2018.04.007. 10.1016/j.psym.2018.04.007 [DOI] [PubMed] [Google Scholar]
- [39].Park M, Cho SH, Hong HJ. Prevalence and perpetrators of workplace violence by nursing unit and the relationship between violence and the perceived work environment. J Nurs Scholarsh 2015;47:87-95. https://doi.org/10.1111/jnu.12112. 10.1111/jnu.12112 [DOI] [PubMed] [Google Scholar]
- [40].Abed M, Morris E, Sobers-Grannum N. Workplace violence against medical staff in healthcare facilities in Barbados. Occup Med (Lond) 2016;66:580-3. https://doi.org/10.1093/occmed/kqw073. 10.1093/occmed/kqw073 [DOI] [PubMed] [Google Scholar]
- [41].Ferri P, Silvestri M, Artoni C, Di Lorenzo R. Workplace violence in different settings and among various health professionals in an Italian general hospital: a cross-sectional study. Psychol Res Behav Manag 2016;9:263-75. https://doi.org/10.2147/PRBM.S114870. 10.2147/PRBM.S114870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Alsaleem SA, Alsabaani A, Alamri RS, Hadi RA, Alkhayri MH, Badawi KK, Badawi AG, Alshehri AA, Al-Bishi AM. Violence towards healthcare workers: A study conducted in Abha City, Saudi Arabia. J Family Community Med 2018;25:188-93. https://doi.org/10.4103/jfcm.JFCM_170_17. 10.4103/jfcm.JFCM_170_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Honarvar B, Ghazanfari N, Raeisi Shahraki H, Rostami S, Lankarani KB. Violence against Nurses: A Neglected and Health-threatening Epidemic in the University Affiliated Public Hospitals in Shiraz, Iran. Int J Occup Environ Med 2019;10:111-23. https://doi.org/10.15171/ijoem.2019.1556. 10.15171/ijoem.2019.1556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Demirci Ş, Uğurluoğlu Ö. An evaluation of verbal, physical, and sexual violence against healthcare workers in Ankara, Turkey. J Forensic Nurs 2020;16:E33-41. https://doi.org/10.1097/JFN.0000000000000286. 10.1097/JFN.0000000000000286 [DOI] [PubMed] [Google Scholar]
- [45].Relazione sulle attività dell’Osservatorio Nazionale sulla sicurezza degli esercenti le professioni sanitarie e socio-sanitarie, anno 2022. Available at: https://www.salute.gov.it/portale/documentazione/p6_2_2_1.jsp?lingua=italiano&id=3302 (Accessed on: 23/03/2024).
- [46].Decreto del Presidente del Consiglio dei Ministri, 1 marzo 2020. Available at: https://www.gazzettaufficiale.it/atto/stampa/serie_generale/originario (Accessed on: 10/12/2023).
- [47].Mahmassani D, El Helou C, El Remlawi A, Mghames A, Mneimne O, Hitti E. Factors associated with emergency department avoidance during the COVID-19 pandemic and alternatives sought: a cross-sectional, telephone-based survey of frequent emergency department users in Beirut, Lebanon. BMJ Open 2023;13:e072117. https://doi.org/10.1136/bmjopen-2023-072117. 10.1136/bmjopen-2023-072117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Piano nazionale di ripresa e resilienza. Cos’è la Missione Salute. Available at: https://www.pnrr.salute.gov.it/portale/pnrrsalute/dettaglioContenutiPNRRSalute.jsp?lingua=italiano&id=5833&area=PNRR-Salute&menu=missionesalute (Accessed on: 10/12/2023).
- [49].Veronesi G, Ferrario MM, Giusti EM, Borchini R, Cimmino L, Ghelli M, Banfi A, Luoni A, Persechino B, Di Tecco C, Ronchetti M, Gianfagna F, De Matteis S, Castelnuovo G, Iacoviello L. Systematic Violence Monitoring to Reduce Underreporting and to Better Inform Workplace Violence Prevention Among Health Care Workers: Before-and-After Prospective Study. JMIR Public Health Surveill 2023;9:e47377. https://doi.org/10.2196/47377. 10.2196/47377 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The anonymised data presented in the study can be provided upon request and authorisation from the data-holding authority.


