Summary
Introduction
Osteoarthritis (OA) is one of the most common degenerative joint diseases which involved all joints. It is very important to choose a treatment method with high efficiency to reduce the pain and disability of patients and also to improve their quality of life. The current study aimed to investigate the therapeutic effects of intra-articular injection of PRP and hyaluronic acid (HA) in the knee of people with knee osteoarthritis (KOA).
Methods
In this randomized clinical trial study, 90 patients with KOA were randomly divided into two groups of intra-articular HA and PRP. The patients of the two groups were followed up for five months and different outcomes were recorded. The McMaster index (WOMAC) evaluated all patients at rest and during movements. Measurements were taken at the beginning and after the third month of follow-up.
Results
Three month after the last injection (5th month) and after adjusting of baseline value using analysis of covariance, the mean of knee pain, stiffness, physical function and finally total score in the PRP group, was significantly lower than the HA group. Regarding the Osteoarthritis grade, the mean of knee pain, Stiffness, Physical function and finally total score in the PRP group was significantly lower than the HA group in all Osteoarthritis grades. Also, there were no complications in the studied groups.
Conclusions
The results of the current study showed that pain and stiffness reduction as well as physical function of the knee joint in the PRP group was better than in the HA group.
Keywords: Intra-Articular, Hyaluronic Acid, Platelet-Rich Plasma, Knee Osteoarthritis
Introduction
Osteoarthritis (OA) is one of the most common degenerative joint diseases, involving all joints [1]. The nature of this disease is the progressive destruction of the joint, characterized by the progressive degeneration of articular cartilage and subchondral bone involvement [2]. While knee osteoarthritis (KOA) is one of the main causes of disability in the knee joint, this manifests itself with symptoms such as knee pain and stiffness, joint inflammation and degeneration, also has a major impact on disability and reduces quality of life [3]. The risk factors of this disease, include increasing age, obesity, female sex, and inflammation of the knee joint [4,5]. The knee is the most common joint affected by arthritis among the Iranian population. The prevalence of this disorder in Iran is estimated at 15.5% [6]. According to a study, knee osteoarthritis in Iran ranks ninth in terms of disease burden after accidents, natural disasters, cardiovascular diseases, etc. [7].
So far, many studies have been presented on the treatment methods of osteoarthritis such drug treatments, interventional methods, and auxiliary treatment regimens [8, 9]. Non-surgical measures are the first step to control patients’ knee pain, which includes weight loss, specific exercise regimens, lifestyle changes, physical therapy, use of non-steroidal anti-inflammatory drugs, painkillers, and intra-articular injections of corticosteroids, gels, etc. [10, 11]. Meanwhile, acetaminophen, non-steroidal anti-inflammatory drugs, and corticosteroids have analgesic and sometimes anti-inflammatory effects. However, the occurrence of common side effects in the use of such drugs limits their use in many patients. Gastrointestinal complications, aggravation of heart failure, increased blood pressure [12], liver disorders [13], kidney problems [14], exacerbation of asthma [15], and the risk of osteoporosis [16] in long-term use are common side effects of anti-inflammatory drugs.
The ability of cartilage to regenerate itself is unfortunately limited due to the lack of blood vessels and innervation, as well as its isolation from the body’s systemic circulation, so the intra-articular injection of a drug or drug combination with the property of regeneration and repair of cartilage tissue has always been of interest to researchers [17]. In recent years, intra-articular injection of platelet-rich plasma (PRP) in knee osteoarthritis has attracted the attention of researchers [18, 19]. This injection contains PRP, which has a higher concentration of platelets than normal blood. PRP is an environment rich in high concentrations of cytokines and various growth factors that are obtained through blood centrifugation and can be considered a new solution to stimulate mesenchymal cells to replicate and regenerate damaged tissues [20]. Samples from patients with knee osteoarthritis show that the number of mesenchymal cells in the synovial fluid of these people has significantly decreased compared to healthy individuals, as a result of PRP injection as a stimulating factor for the regeneration and replication of this cell can be effective in the treatment of arthritis [21]. Increasing the presence of mesenchymal cells in the synovial fluid of sick people can play a modulating role in the responses of the immune system, which accelerates the healing process [22]. The current study aimed to investigate the therapeutic effects of intra-articular injections of PRP and hyaluronic acid (HA) in patients with knee osteoarthritis.
Methods
In the current randomized clinical trial study, 90 patients with painful knee arthritis with radiological grades one to three of the Kellgren and Lawrence radiological criteria were included. More details were shown in figure1.
INCLUSION CRITERIA
Patients aged 40 to 65 years, history of knee pain for at least three months, knee osteoarthritis grade 1 to 3 based on the Kellgren and Lawrence criteria (based on knee osteoarthritis criteria of the American College of Rheumatology) were included.
EXCLUSION CRITERIA
Patients suffering from diseases such as diabetes, rheumatoid arthritis, hemophilia, dysfunction of blood platelets, any infection or active wound at the injection site, taking antiplatelet or anticoagulant drugs in the last ten days before injection, taking non-steroidal anti-inflammatory drugs, having history of intra-articular corticosteroid injection in the previous three weeks or systemic corticosteroid use in the last two weeks, peripheral blood platelet count less than 150,000 per microliter, patients with drug or alcohol addiction and abnormal ESR or CRP levels were excluded.
After selection of the cases, their basic information including age, sex, height, weight, and body mass index was recorded and patients were divided into the PRP and HA groups using simple random allocation methods.
INTERVENTIONS: PRP GROUP
After taking the patients’ history, examining them, and performing routine monitoring such as blood pressure, heart rate, and electrocardiogram (if necessary), 30-35 ml of the patient’s venous blood was taken from the upper limb with an 18G needle under sterile conditions and placed in special centrifuge kits (produced by Royagen, Iran) containing 5 ml of acid citrate dextrose solution-A to prepare platelet-rich plasma. This solution was placed in a centrifuge for 15 minutes with a rotation speed of 1600 rpm. The Buffy coat and plasma layer of the solution inside the test tube was separated and centrifuged again for 7 minutes with a rotation speed of 2800 rpm. Finally, 5 ml PRP was prepared for intra-articular injection. Anesthetic injections may also affect platelet activation by changing the PH of the environment, so no local anesthetic was injected. Instead, patients were given a single dose of acetaminophen and codeine two hours before injection. Under sterile conditions, a 22-gauge, 50 mm needle was inserted from the upper external area of the knee patella (suprapatellar) and the outside to the inside of the knee joint and the prepared plasma was injected inside the knee joint. In our study, the frequency of intra-articular injection of PRP was three times at one-month intervals.
HYALURONIC ACID GROUP
In this group, HA (Hyalgan®) was injected. Hyalgan produced by Fidia Farmaceutici S.p.A., Abano Terme, Italy, is a viscous solution consisting of a high molecular weight (500,000-730,000 Da) fraction of purified natural sodium hyaluronate in buffered physiological sodium chloride, having a PH of 6.8-7.5. The sodium hyaluronate is extracted from rooster combs. Hyalgan was supplied as a sterile, non-pyogenic solution in 2 mL pre-filled syringes containing 20 mg of sodium hyaluronate, 17 mg of sodium chloride, 0.1 mg of monobasic sodium phosphate, 1.2 mg of dibasic sodium phosphate, and up to 2 cc water for injection. After resting for 15-20 minutes, the patients were asked to flex and extend their knees to ensure even distribution of the HA in the joint space. The patients were monitored in the clinic for one hour after the injection and were discharged with written instructions regarding the following issues if no side effects occurred. Hyaluronic acid injections were administered three times at one-week intervals.
STUDY OUTCOMES
The intensity of pain, dryness, and knee function of the patients before the first injection and three months after the last injection were evaluated using the Western Ontario and McMaster Universities Arthritis Index (WOMAC) scores. The WOMAC criterion consists of three parts: pain level, joint stiffness level, and knee function level. Scoring in each case is from 0 to 4 and the total score of this scale is from 0 to 96.
STATISTICAL ANALYSIS
Descriptive statistics including mean ± standard and frequency (percentage) was used to present quantitative and qualitative findings. Data were analyzed using the independent sample t-test, paired sample t-test, Chi-square, or Fisher exact test and Analysis of covariance (ANCOVA) test. The statistical significance level was considered at: 0.05. All data were analyzed using SPSS, version 22.0, Armonk, NY, USA: IBM Corp. Released 2015.
Results
BASELINE CHARACTERISTICS
Regarding the gender, 26(63.4%) and 26(59.1%) of cases in the PRP and Hyaluronic Acid groups were females respectively (P: 0.682). Mean of age in the PRP and Hyaluronic Acid groups were 60.24 ± 1.97 and 61.90 ± 2.06 and the difference between two groups was statistically significant (P: 0.001). The mean of BMI in the PRP and Hyaluronic Acid groups were 29.47 ± 1.52 and 28.78 ± 1.39 and the difference between two groups was statistically significant (P: 0.032) (Tab. I).
Tab. I.
Descriptive characteristics of understudied cases.
| Variables | PRP (n: 41) | Hyaluronic Acid (n: 44) | p |
|---|---|---|---|
| Gender | |||
| Females | 26(63.4%) | 26(59.1%) | 0.682 |
| Osteoarthritis grade | |||
| 1 | 14(34.1%) | 15(34.1%) | |
| 2 | 14(34.1%) | 14(31.8%) | |
| 3 | 13(31.7%) | 15(34.1%) | 0.961 |
| Age | Mean ± SD | Mean ± SD | |
| 60.24 ± 1.97 | 61.90 ± 2.06 | 0.014 | |
| BMI | |||
| 29.47 ± 1.52 | 28.78 ± 1.39 | 0.032 | |
MAIN OUTCOMES: WITHIN GROUPS COMPARISON: PRP GROUP
In this group, the knee pain score three months after intervention decreased significantly from 13.66 ± 3.60 to 6.44 ± 1.42(P: 0.001), also the knee stiffness score decreased from 3.10 ± 0.80 to 1.80 ± 0.93 (P: 0.001). Regarding the knee physical function score, this score decreased significantly from 36.07 ± 6.71 to 18.85 ± 6.70 (P: 0.001), and finally the total score decreased significantly from 52.37 ± 9.19 to 27.10 ± 8.46 (P: 0.001) (Tab. II, Fig. 1).
Tab. II.
Comparison of different outcome scores within groups over the time.
| Group | N | Outcome | Baseline | Three months after the intervention | |
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | p | |||
| PRP | 41.00 | Pain | 13.66 ± 3.60 | 6.44 ± 1.42 | 0.001 |
| 41.00 | Stiffness | 3.10 ± 0.80 | 1.80 ± 0.93 | 0.001 | |
| 41.00 | Physical function | 36.07 ± 6.71 | 18.85 ± 6.70 | 0.001 | |
| 41.00 | Total | 52.37 ± 9.19 | 27.10 ± 8.46 | 0.001 | |
| Hyaluronic acid | 44.00 | Pain | 11.93 ± 1.59 | 10.61 ± 1.17 | 0.001 |
| 44.00 | Stiffness | 2.91 ± 0.86 | 2.52 ± 0.73 | 0.001 | |
| 44.00 | Physical function | 35.36 ± 6.42 | 33.05 ± 6.41 | 0.001 | |
| 44.00 | Total | 50.20 ± 8.41 | 46.18 ± 7.90 | 0.001 |
Fig. 1.
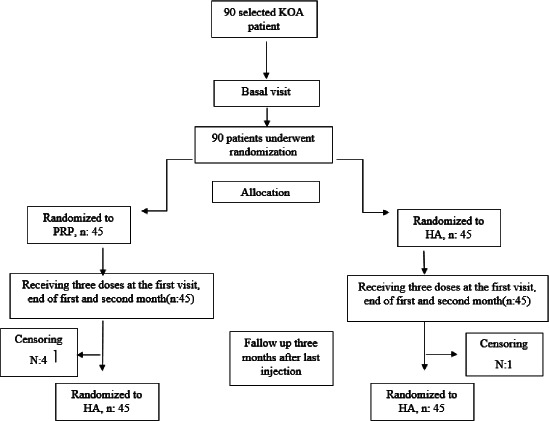
Flow diagram of the study. N: number of patients, KOA: Knee osteoarthritis; PRP: platelet-rich plasma; HA: hyaluronic acid.
HYALURONIC ACID
In this group, the knee pain score decreased significantly from 11.93 ± 1.59 to 10.61 ± 1.17 (P: 0.001) in three months after the intervention compared to baseline.
Also the knee stiffness score decreased significantly from 2.91 ± 0.86 to 2.52 ± 0.73 (P: 0.001). Regarding the knee physical function score, this score decreased from 35.36 ± 6.42 to 33.05 ± 6.41 (P: 0.001), and finally the total score decreased from 50.20 ± 8.41 to 46.18 ± 7.90 (P:0.001) (Tab. II, Fig. 2).
Fig. 2.

The trend of changes in different outcome scores in studied interventions.
BETWEEN GROUPS COMPARISON
Three months after the intervention, the mean of knee pain, stiffness, physical function and finally total score in the PRP group, was significantly lower than the Hyaluronic Acid group. More details were shown in the Table III. Regarding the Osteoarthritis grade, the mean of knee pain, Stiffness, Physical function and finally total score in the PRP group was significantly lower than the Hyaluronic Acid group in all Osteoarthritis grades (Tab. IV). Also, there were no complications in the studied groups.
Tab. III.
Comparison of different outcome scores between groups three month after the intervention.
| Outcome | PRP (n: 41) | Hyaluronic acid (n: 44) | Partial eta squared | P |
|---|---|---|---|---|
| Mean ±SD | Mean ± SD | |||
| Pain | 6.44 ± 1.42 | 10.61 ± 1.17 | 0.82 | 0.001 |
| Stiffness | 1.80 ± 0.93 | 2.52 ± 0.73 | 0.41 | 0.001 |
| Physical function | 18.85 ± 6.70 | 33.05 ± 6.41 | 0.95 | 0.001 |
| Total | 27.10 ± 8.46 | 46.18 ± 7.90 | 0.98 | 0.001 |
Tab. IV.
Comparison of different outcome scores between groups three month after the intervention by Osteoarthritis grades.
| Outcome | PRP (n: 41) | Hyaluronic acid (n: 44) | Partial eta squared | P |
|---|---|---|---|---|
| Pain | ||||
| Osteoarthritis grade | Mean ± SD | Mean ± SD | ||
| 1.00 | 4.93 ± 0.73 | 9.73 ± 0.80 | 0.96 | 0.001 |
| 2.00 | 6.86 ± 1.10 | 10.71 ± 0.73 | 0.81 | 0.001 |
| 3.00 | 7.62 ± 0.65 | 11.40 ± 1.24 | 0.96 | 0.001 |
| Stiffness | ||||
| 1.00 | 1.07 ± 0.73 | 1.93 ± 0.26 | 0.60 | 0.001 |
| 2.00 | 1.71 ± 0.61 | 2.29 ± 0.47 | 0.33 | 0.001 |
| 3.00 | 2.69 ± 0.63 | 3.33 ± 0.49 | 0.17 | 0.03 |
| Physical function | ||||
| 1.00 | 13.21 ± 1.97 | 27.60 ± 1.80 | 0.39 | 0.001 |
| 2.00 | 16.79 ± 1.63 | 31.36 ± 2.98 | 0.50 | 0.001 |
| 3.00 | 27.15 ± 5.08 | 40.07 ± 5.23 | 0.98 | 0.001 |
| Total | ||||
| 1.00 | 19.21 ± 1.97 | 39.27 ± 2.43 | 0.98 | 0.001 |
| 2.00 | 25.36 ± 2.71 | 44.36 ± 3.59 | 0.75 | 0.001 |
| 3.00 | 37.46 ± 5.84 | 54.80 ± 6.29 | 0.99 | 0.001 |
Discussion
One of the effective factors in the development and progression of knee arthritis is inflammation, which aggravates the symptoms. Therefore, the use of treatments that have an anti-inflammatory effect can have an effective role in reducing the symptoms of the disease as well as the side effects of osteoarthritis of the joints. One of these treatments is the use of blood derivatives such as PRP, which can play an important role in reducing symptoms. PRP.as an anti-inflammatory factor can affect various cells, including mesenchymal stem cells, and as a result, it can modulate various cellular activities [23-25]. Another property of PRP is the absorption of other cells effective in treatment [23]. This multifaceted property of PRP has made this drug play an important role in reducing joint inflammation and play an important role in improving function and reducing pain in people with osteoarthritis [26, 27]. It is believed that intra-articular injection of PRP and HA can reduce pain and improve quality of life in patients with OA [28-30]. Due to the importance of the issue the current study aimed to assess the short-term effect of intra-articular hyaluronic acid and platelet-rich plasma injections in knee osteoarthritis in a randomized clinical trial study.
Our results showed that the knee pain, knee stiffness, physical function and total WOMAC scores decreased significantly from baseline to three months after the intervention in both PRP and HA groups. Also, three months after the intervention the mean of knee pain, stiffness, physical function and finally total WOMAC scores in the PRP group, was significantly lower than the HA group. Regarding the osteoarthritis grade, the mean of knee pain, stiffness, physical function and finally total score in the PRP group, was significantly lower than the hyaluronic acid group in all osteoarthritis grades. This finding indicates that the PRP as well as HA improved OA indices, but the amount of changes in the PRP group was significantly more than HA group.
Several studies have been conducted comparing the effectiveness of PRP, and HA in the treatment of osteoarthritis [31-33]. In the study of Lana et al., they concluded that PRP has a greater effect on reducing patients’ pain scores compared to HA at different times after treatment [34]. The results of Sampson et al.’s study indicated a significant reduction in pain within one year after PRP injection in patients with OA [35]. The study by Sanchez et al showed a reduction in knee pain intensity for 5 weeks after PRP [36].
The findings of the meta-analyses conducted in this field also indicate the superiority of PRP over HA, and in reducing pain [27, 37, 38]. The results of the meta-analysis showed that the greatest effectiveness of PRP in reducing WOMAC pain and VAS pain outcomes was observed 6 months after treatment [32]. The results of other studies in this field indicate that the effectiveness of drug injection is not stable and usually decreases over times [37].
The results of our study indicated that PRP is more effective in reducing the stiffness and function of patients. Also, there were no significant complications among patients, and most of the patients only experienced brief pain at the injection site, which improved within a short time after the intervention. Other studies also support this finding. The meta-analysis results showed that pain, stiffness, and WOMAC performance in the PRP group improved the most in the 12 months after injection [32]. These results have been confirmed in other studies that have shown that after PRP injection, a drug effect lasts up to 12 and even 24 months [27, 39]. Another study showed improvement in patients’ quality of life in 12 months after injection of PRP and HA [30]. Tucker et al.’s study results showed that the pain stiffness and functional scores, improved significantly in the PRP group compared to the control group [40]. Therefore, as mentioned, the findings of various studies indicate that PRP is more effective in reducing knee joint pain than HA. In justification of these findings, it can be said that PRP has anti-inflammatory properties. Indeed, PRP reduces inflammation by inducing a more targeted and controlled anti-inflammatory response, modulating the immune response, and increasing angiogenesis and re-epithelialization [41]. Also, PRP can potentially reduce the impact of other underlying knee joint diseases [42-44]. In fact, by promoting tissue repair and regeneration, PRP can reduce the impact of these diseases on the progression of osteoarthritis [32].
LIMITATIONS OF THE STUDY
The present study had limitations, including the small sample size and the short follow-up period of the patients.
Conclusions
The results of the study indicate a significant improvement in pain, stiffness, and physical function of the knee joint in patients with arthritis especially in the PRP group. Due to its positive effect, safety, and availability, PRP has attracted the interest of Physician in the treatment of knee arthritis and it can be concluded that PRP injection can be considered a more effective treatment than HA in patients with knee osteoarthritis.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. This research approved by the ethical committee of Shahed University with approval id IR.SHAHED.REC.1399.028. The written informed consent was obtained from all participants.
Conflict of interest statement
The authors declare no conflict of interest.
Authors’ contributions
All authors contributed to the study conception and design. OG, DB: participated in the design of the study; OG, PYT: performed data collection, wrote the manuscript, and helped with statistical analysis; OG, DB: edited the manuscript. All authors read and approved the final manuscript.
History
Received on May 1, 2024. Accepted on June 19, 2024.
Figures and tables
References
- [1].Allen KD, Thoma LM, Golightly YM. Epidemiology of osteoarthritis. Osteoarthritis Cartilage 2022;30:184-95. https://doi.org/10.1016/j.joca.2021.04.020 10.1016/j.joca.2021.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Martel-Pelletier J, Barr AJ, Cicuttini FM, Conaghan PG, Cooper C, Goldring MB, Goldring SR, Jones G, Teichtahl AJ, Pelletier JP. Osteoarthritis. Nat Rev Dis Primers 2016;2:16072. https://doi.org/10.1038/nrdp.2016.72 10.1038/nrdp.2016.72. [DOI] [PubMed] [Google Scholar]
- [3].Lespasio MJ, Piuzzi NS, Husni ME, Muschler GF, Guarino A, Mont MA. Knee osteoarthritis: a primer. Perm J 2017;21:16-183. https://doi.org/10.7812/TPP/16-183 10.7812/TPP/16-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Cui A, Li H, Wang D, Zhong J, Chen Y, Lu H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine 2020;29-30:100587. https://doi.org/10.1016/j.eclinm.2020 10.1016/j.eclinm.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Peshkova M, Lychagin A, Lipina M, Di Matteo B, Anzillotti G, Ronzoni F, Kosheleva N, Shpichka A, Royuk V, Fomin V, Kalinsky E, Timashev P, Kon E. Gender-related aspects in osteoarthritis development and progression: a review. Int J Mol Sci 2022;23:2767. https://doi.org/10.3390/ijms23052767 10.3390/ijms23052767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Davatchi F, Sandoughi M, Moghimi N, Jamshidi AR, Tehrani Banihashemi A, Zakeri Z, Sadeghi Abdollahi B. Epidemiology of rheumatic diseases in Iran from analysis of four COPCORD studies. Int J Rheum Dis 2016;19:1056-62. https://doi.org/10.1111/1756-185X.12809 10.1111/1756-185X.12809. [DOI] [PubMed] [Google Scholar]
- [7].Naghavi M, Abolhassani F, Pourmalek F, Lakeh M, Jafari N, Vaseghi S, Mahdavi Hezaveh N, Kazemeini H. The burden of disease and injury in Iran 2003. Popul Health Metr 2009;7:9. https://doi.org/10.1186/1478-7954-7-9 10.1186/1478-7954-7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Zhu B, Ba H, Kong L, Fu Y, Ren J, Zhu Q, Fang M. The effects of manual therapy in pain and safety of patients with knee osteoarthritis: a systematic review and meta-analysis. Syst Rev 2024;13:91. https://doi.org/10.1186/s13643-024-02467-7 10.1186/s13643-024-02467-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Song X, Liu Y, Chen S, Zhang L, Zhang H, Shen X, Du H, Sun R. Knee osteoarthritis: a review of animal models and intervention of traditional Chinese medicine. Animal Model Exp Med 2024;7:114-26. https://doi.org/10.1002/ame2.12389 10.1002/ame2.12389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Allison K, Jones S, Hinman RS, Pardo J, Li P, DeSilva A, Quicke JG, Sumithran P, Prendergast J, George E, Holden MA, Foster NE, Bennell KL. Alternative models to support weight loss in chronic musculoskeletal conditions: effectiveness of a physiotherapist-delivered intensive diet programme for knee osteoarthritis, the POWER randomised controlled trial. Br J Sports Med 2024;58:538-47. https://doi.org/10.1136/bjsports-2023-107793 10.1136/bjsports-2023-107793. [DOI] [PubMed] [Google Scholar]
- [11].Dantas LO, Salvini TF, McAlindon TE. Knee osteoarthritis: key treatments and implications for physical therapy. Braz J Phys Ther 2021;25:135-46. https://doi.org/10.1016/j.bjpt.2020.08.004 10.1016/j.bjpt.2020.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Snowden S, Nelson R. The effects of nonsteroidal anti-inflammatory drugs on blood pressure in hypertensive patients. Cardiol Rev 2011;19:184-91. https://doi.org/10.1097/CRD.0b013e31821ddcf4 10.1097/CRD.0b013e31821ddcf4. [DOI] [PubMed] [Google Scholar]
- [13].García Rodríguez LA, Williams R, Derby LE, Dean AD, Jick H. Acute liver injury associated with nonsteroidal anti-inflammatory drugs and the role of risk factors. Arch Intern Med 1994;154:311-6. https://doi.org/10.1001/archinte.1994.00420030117012 10.1001/archinte.1994.00420030117012. [DOI] [PubMed] [Google Scholar]
- [14].Winkelmayer WC, Waikar SS, Mogun H, Solomon DH. Nonselective and cyclooxygenase-2-selective NSAIDs and acute kidney injury. Am J Med 2008;121:1092-8. https://doi.org/10.1016/j.amjmed.2008.06.035 10.1016/j.amjmed.2008.06.035. [DOI] [PubMed] [Google Scholar]
- [15].Day RO, Graham GG. Non-steroidal anti-inflammatory drugs (NSAIDs). BMJ 2013;346:f3195. https://doi.org/10.1136/bmj.f3195 10.1136/bmj.f3195. [DOI] [PubMed] [Google Scholar]
- [16].van Esch RW, Kool MM, van As S. NSAIDs can have adverse effects on bone healing. Med Hypotheses 2013;81:343-6. https://doi.org/10.1016/j.mehy.2013.03.042 10.1016/j.mehy.2013.03.042. [DOI] [PubMed] [Google Scholar]
- [17].Kon E, Filardo G, Drobnic M, Madry H, Jelic M, van Dijk N, Della Villa S. Non-surgical management of early knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc 2012;20:436-49. https://doi.org/10.1007/s00167-011-1713-8 10.1007/s00167-011-1713-8. [DOI] [PubMed] [Google Scholar]
- [18].Garcia-Motta H, Carvalho C, Guilherme EM, de Oliveira MPB, Rossi KNZP. Effects of intra-articular injection of platelet-rich plasma on the inflammatory process and histopathological characteristics of cartilage and synovium in animals with osteoarthritis: a systematic review with meta-analysis. Adv Rheumatol 2024;64:24. https://doi.org/10.1186/s42358-024-00364-0 10.1186/s42358-024-00364-0. [DOI] [PubMed] [Google Scholar]
- [19].Patel S, Gahlaut S, Thami T, Chouhan DK, Jain A, Dhillon MS. Comparison of conventional dose versus superdose platelet-rich plasma for knee osteoarthritis: a prospective, triple-blind, randomized clinical trial. Orthop J Sports Med 2024;12:23259671241227863. https://doi.org/10.1177/23259671241227863 10.1177/23259671241227863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Werner S, Grose R. Regulation of wound healing by growth factors and cytokines. Physiol Rev 2003;83:835-70. https://doi.org/10.1152/physrev.2003.83.3.835 10.1152/physrev.2003.83.3.835. [DOI] [PubMed] [Google Scholar]
- [21].Kohno Y, Mizuno M, Ozeki N, Katano H, Otabe K, Koga H, Matsumoto M, Kaneko H, Takazawa Y, Sekiya I. Comparison of mesenchymal stem cells obtained by suspended culture of synovium from patients with rheumatoid arthritis and osteoarthritis. BMC Musculoskelet Disord 2018;19:78. https://doi.org/10.1186/s12891-018-1998-6 10.1186/s12891-018-1998-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Mohanraj B, Huang AH, Yeger-McKeever MJ, Schmidt MJ, Dodge GR, Mauck RL. Chondrocyte and mesenchymal stem cell derived engineered cartilage exhibits differential sensitivity to pro-inflammatory cytokines. J Orthop Res 2018;36:2901-10. https://doi.org/10.1002/jor.24061 10.1002/jor.24061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Ishida K, Kuroda R, Miwa M, Tabata Y, Hokugo A, Kawamoto T, Sasaki K, Doita M, Kurosaka M. The regenerative effects of platelet-rich plasma on meniscal cells in vitro and its in vivo application with biodegradable gelatin hydrogel. Tissue Eng 2007;13:1103-1112. https://doi.org/10.1089/ten.2006.0193 10.1089/ten.2006.0193. [DOI] [PubMed] [Google Scholar]
- [24].Jeyakumar V, Niculescu-Morzsa E, Bauer C, Lacza Z, Nehrer S. Platelet-rich plasma supports proliferation and redifferentiation of chondrocytes during in vitro expansion. Front Bioeng Biotechnol 2017;5:75. https://doi.org/10.3389/fbioe.2017.00075 10.3389/fbioe.2017.00075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Olivotto E, Merli G, Assirelli E, Cavallo C, Belluzzi E, Ramonda R, Favero M, Filardo G, Roffi A, Kon E: Cultures of a human synovial cell line to evaluate platelet-rich plasma and hyaluronic acid effects. J Tissue Engin Regen Med 2018;12:1835-42. https://doi.org/10.1002/term.2704 10.1002/term.2704. [DOI] [PubMed] [Google Scholar]
- [26].Huang G, Hua S, Yang T, Ma J, Yu W, Chen X. Platelet-rich plasma shows beneficial effects for patients with knee osteoarthritis by suppressing inflammatory factors. Exp Ther Med 2018;15:3096-102. https://doi.org/10.3892/etm.2018.5794 10.3892/etm.2018.5794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Filardo G, Previtali D, Napoli F, Candrian C, Zaffagnini S, Grassi A. PRP injections for the treatment of knee osteoarthritis: a meta-analysis of randomized controlled trials. Cartilage 2021;13(Suppl 1):364S-75. https://doi.org/10.1177/1947603520931170 10.1177/1947603520931170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Yoga R, Mukaram M. Intra-articular sodium hyaluronate for the treatment of osteoarthritis of the knee. A retrospective review of 45 patients. Malaysian Orthop J 2009;3:4-7. https://doi.org/10.5704/MOJ.0911.001 10.5704/MOJ.0911.001. [DOI] [Google Scholar]
- [29].Haque Bhuyan MZ, Tamura Y, Sone E, Yoshinari Y, Maeda C, Takahashi M, Tabata Y, Murali R, Waki Y, Aoki K. The intra-articular injection of RANKL-binding peptides inhibits cartilage degeneration in a murine model of osteoarthritis. J Pharmacol Sci 2017;134:124-30. https://doi.org/10.1016/j.jphs.2017.05.008 10.1016/j.jphs.2017.05.008. [DOI] [PubMed] [Google Scholar]
- [30].Filardo G, Kon E, Buda R, Timoncini A, Di Martino A, Cenacchi A, Fornasari PM, Giannini S, Marcacci M. Platelet-rich plasma intra-articular knee injections for the treatment of degenerative cartilage lesions and osteoarthritis. Knee Surg Sports Traumatol Arthrosc 2011;19:528-35. https://doi.org/10.1007/s00167-010-1238-6 10.1007/s00167-010-1238-6. [DOI] [PubMed] [Google Scholar]
- [31].Konana VS, Yallapura HS, Bettaswamy S, Sivaram SP, Thimmegowda DG: Comparing the Effectiveness of Intra-articular injection with autologous platelet-rich plasma vs hyaluronic acid vs platelet-derived growth factors in early osteoarthritis of knee joint. J Orthop Joint Surg 2024;6:27-34. https://doi.org/10.5005/jojs-10079-1134 10.5005/jojs-10079-1134. [DOI] [Google Scholar]
- [32].Khalid S, Ali A, Deepak F, Zulfiqar MS, Malik LU, Fouzan Z, Nasr RA, Qamar M, Bhattarai P. Comparative effectiveness of intra-articular therapies in knee osteoarthritis: a meta-analysis comparing platelet-rich plasma (PRP) with other treatment modalities. Ann Med Surg 2024;86:361-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Abdulwahab D, Lateef S, Farïs W, Al Radhwany Y. Single shot of knee intraarticular injection of platelets rich plasma versus hyaluronic acid injections for symptomatic knee osteoarthritis. an observational prospective study. Int J Disab Sports Health Sci 2004;7:342-50. [Google Scholar]
- [34].Lana JF, Weglein A, Sampson SE, Vicente EF, Huber SC, Souza CV, Ambach MA, Vincent H, Urban-Paffaro A, Onodera CM, Annichino-Bizzacchi JM, Santana MH, Belangero WD. Randomized controlled trial comparing hyaluronic acid, platelet-rich plasma and the combination of both in the treatment of mild and moderate osteoarthritis of the knee. J Stem Cells Regen Med 2016;12:69-78. https://doi.org/10.46582/jsrm.1202011 10.46582/jsrm.1202011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Sampson S, Reed M, Silvers H, Meng M, Mandelbaum B. Injection of platelet-rich plasma in patients with primary and secondary knee osteoarthritis: a pilot study. Am J Phys Med Rehabil 2010;89:961-9. https://doi.org/10.1097/PHM.0b013e3181fc7edf 10.1097/PHM.0b013e3181fc7edf. [DOI] [PubMed] [Google Scholar]
- [36].Sánchez M, Anitua E, Azofra J, Aguirre JJ, Andia I. Intra-articular injection of an autologous preparation rich in growth factors for the treatment of knee OA: a retrospective cohort study. Clin Exp Rheumatol 2008;26:910-3. [PubMed] [Google Scholar]
- [37].McLarnon M, Heron N. Intra-articular platelet-rich plasma injections versus intra-articular corticosteroid injections for symptomatic management of knee osteoarthritis: systematic review and meta-analysis. BMC Musculoskelet Disord 2021;22:550. https://doi.org/10.1186/s12891-021-04308-3 10.1186/s12891-021-04308-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Nie LY, Zhao K, Ruan J, Xue J. Effectiveness of platelet-rich plasma in the treatment of knee osteoarthritis: a meta-analysis of randomized controlled clinical trials. Orthop J Sports Med 2021;9:2325967120973284. https://doi.org/10.1177/2325967120973284 10.1177/2325967120973284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Shen L, Yuan T, Chen S, Xie X, Zhang C. The temporal effect of platelet-rich plasma on pain and physical function in the treatment of knee osteoarthritis: systematic review and meta-analysis of randomized controlled trials. J Orthop Surg Res 2017;12:16. https://doi.org/10.1186/s13018-017-0521-3 10.1186/s13018-017-0521-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Tucker JD, Goetz LL, Duncan MB, Gilman JB, Elmore LW, Sell SA, McClure MJ, Quagliano PV, Martin CC. Randomized, placebo-controlled analysis of the knee synovial environment following platelet-rich plasma treatment for knee osteoarthritis. Randomized Controlled Trial 2021;13:707-19. https://doi.org/10.1002/pmrj.12561 10.1002/pmrj.12561. [DOI] [PubMed] [Google Scholar]
- [41].Xu P, Wu Y, Zhou L, Yang Z, Zhang X, Hu X, Yang J, Wang M, Wang B, Luo G, He W, Cheng B. Platelet-rich plasma accelerates skin wound healing by promoting re-epithelialization. Burns Trauma 2020;8:tkaa028. https://doi.org/10.1093/burnst/tkaa028 10.1093/burnst/tkaa028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Jawanda H, Khan ZA, Warrier AA, Acuña AJ, Allahabadi S, Kaplan DJ, Ritz E, Jackson GR, Mameri ES, Batra A, Dornan G, Westrick J, Verma NN, Chahla J. Platelet-rich plasma, bone marrow aspirate concentrate, and hyaluronic acid injections outperform corticosteroids in pain and function scores at a minimum of 6 months as intra-articular injections for knee osteoarthritis: a systematic review and network meta-analysis. Arthroscopy 2024;40:1623-36.e1. https://doi.org/10.1016/j.arthro.2024.01.037 10.1016/j.arthro.2024.01.037. [DOI] [PubMed] [Google Scholar]
- [43].Mouneshwaran R, Vijayaragavan R: A comparative study of functional outcome of single dose intra-lesional platelet rich plasma injection versus single dose corticosteroid injection for plantar fasciitis. Int J Orthop 2024;10:177-81. https://doi.org/10.22271/ortho.2024.v10.i1c.3516 10.22271/ortho.2024.v10.i1c.3516. [DOI] [Google Scholar]
- [44].Kavia A, Singh J, Raina S, Sahni G, Singh M. A comparative study of single intra-articular platelet-rich plasma versus corticosteroid injection in the treatment of adhesive capsulitis of the shoulder. Nat J Physiol Pharm Pharmacol 2024;14:10-10. https://doi.org/10.5455/njppp.2023.13.03153202331052023 10.5455/njppp.2023.13.03153202331052023. [DOI] [Google Scholar]


