Summary
Introduction
Hand hygiene in nurses is the most effective factor in controlling nosocomial infections. The objective of this study was to assess the effectiveness of motivational interviews and teach-back on the rate of hand hygiene compliance in Intensive Care Unit nurses.
Methods
A quasi-experimental study with pre-test and post-test design was performed. Three Intensive Care Units with 88 nurses were randomly divided into three study groups. The control group received only the usual hospital teaching in hand hygiene, the experimental groups 1 and 2, in addition to the usual teaching, they received motivational interview and teach back in five weekly sessions, respectively. The rate of hand hygiene compliance in nurses was measured by Hand Hygiene Practices Inventory.
Results
There was a statistically significant difference for the rate of hand hygiene compliance before and after the intervention in the study groups with p < 0.001. In comparison before and after, in experimental group 1, the rate of hand rub increased from 8% to 18.5% and the rate of hand wash from 1.5% to 22%; and in the experimental group 2, these values increased from 4% to 19.5% in hand rub and from 3.5% to 17% in hand wash, respectively. However, in the control group, the rate of hand hygiene compliance before and after the test did not show a statistically significant difference with p > 0.05.
Conclusions
Motivational interview and teach back methods were effective in promoting hand hygiene compliance in nurses and thus improve the control of nosocomial infections.
Keywords: Hand Hygiene, Motivational Interview, Teach back, Nurses, Intensive Care Unit
Introduction
Nurses are at the forefront of patient care. In this regard, hand hygiene in nurses is the most effective factor in controlling nosocomial infections, reducing costs, complications and mortality rate [1-3]. There is some evidence that the rate of hand hygiene compliance in nurses is not satisfactory and 70% of health care workers do not routinely observe hand hygiene [4, 5]. A review of 61 studies showed that the hand hygiene rate, with an average of 59.6% in the Intensive Care Unit, was significantly lower than the desired international targets. It is also around 64.5% in high-income countries, compared to 9.1% in low-income countries. This rate is 43.4% for nurses, 32.6% for physicians and 53.8% for other medical staff [6]. Chang et al. found that nurses observed less hand hygiene before intensive care than after that. In other words, nurses protect themselves more than patients, and do not follow methods in providing care that reduce the rate of infection transmission to patients. These conditions increase the risk of nosocomial infections in patients [7]. Evidence in health centers in Iran is somewhat similar to the statistics of other countries; in a study, the rate of hand hygiene by physicians was reported by 32% and nurses by 48% [8]. Nouri et al. reported that the average hand hygiene rate of Iranian nurses was 40.5% [9]. Ziasheikholeslami reported that the average hand hygiene in Intensive Care Unit nurses was 44.5% [10]. Mohanty et al. in a study on 171 medical and nursing students and faculty members at several teaching hospitals in India showed that although 66.4% of the participants had sufficient knowledge of hand hygiene, only 32% observed hand hygiene in the situations required [11]. Evidence at the international rate shows that despite the improvement of employees’ knowledge to observe hand hygiene, the rate of hand hygiene compliance is not optimal yet. In other words, the main challenge is not lack of awareness, but the lack of commitment and adherence to hand hygiene in the treatment staff [12]. The study of Neda Khairkhah showed that while education using film screening has increased awareness and belief change in nursing students, but has not changed the performance of hand hygiene in them [13]. Farias also showed that despite sufficient knowledge of nurses, they are not committed to hand hygiene in clinical situations. There is a need for interventions that turn nurses’ knowledge into positive behavior [14]. Numerous studies in the investigation of the causes of hand hygiene non-compliance showed that barriers such as lack of positive attitude, negligence and underestimation of hand hygiene, lack of motivation, internal commitment or professional commitment, poor understanding of the negative consequences of non-compliance with hand hygiene, high workload, disproportion of the number of nurses to the patient, the type of organizational culture, the facilities of each ward as well as common skin problems are effective in adhering to hand hygiene in nurses [15-17]. Some researchers divided the unfavorable situation in hand hygiene into several areas of knowledge, attitude, motivation and practice and believe that promoting hand hygiene in nurses is a complex and multifaceted behavior change process that requires the combination of educational and motivational interventions and change in systems structure [18]. Interventions in this area should lead to behavior change by increasing nurses’ motivation and professional commitment along with a supportive and empathetic environment [3, 19]. So far, various educational interventions are implemented to improve nurses’ adherence to the principles of hand hygiene, but the impact of these teachings on increasing nurses’ adherence is still disputed, so that some report the effectiveness of teaching and some report its ineffectiveness [20]. One of the most common educational methods is the transfer of information by lecturing method, the results of scientific research indicate that in this method, 40 to 80% of information is forgotten almost immediately after hearing it, plus half of the information that nurses remember, is incorrect, so appropriate teaching methods should be selected that lead to behavior change [21]. Some researchers consider the use of motivational approaches in this area to be more effective and some others the use of educational approaches, and less study has compared the effect of two educational and motivational approaches in promoting hand hygiene [22]. Various researches show that behavior change depend on the analysis and removal of internal contradictions, doubts in individuals, and changing these conditions is not possible with advice and education, but appropriate motivational interventions should be used [17, 23]. In contrast, experts in the field of education believe that education leads to behavior change when it is properly understood and internalized and a person is able to self-assess and transfer their knowledge to others [24-26]. Two famous interventions are based on theories of behavioral change, motivational interview, and teach back [27-29]. Motivational interview is one of the most effective behavioral change approaches developed in 1983 by William Miller and Stephen Rolnick. And was quickly used in various areas of behavior change [29, 30]. Motivational interview helps to strengthen the intrinsic motivation to change behavior in individuals by discovering, identifying and resolving doubts and ambivalence. A significant advantage of motivational interview is its flexibility and applicability in different areas of behavior [30, 31]. Several studies have confirmed the effectiveness of motivational interviewing in changing behavior [32-34]. A study by Östlund et al. on the effectiveness of motivational interview on patients’ lifestyle changes showed that nurses who use motivational interview in the patient education process had more positive effects on patients’ lifestyle changes [35]. Teach back is a well-known educational and interactive intervention to acquire health-promoting behaviors that combines three aspects of learning, teaching and evaluation, in which a person while mastering his/her perceptual problems, has reached a degree of mastery in skills and performance that teaches behavior in practice to others [36]. Pawase et al. studied the effectiveness of teach back method on the knowledge and performance of students in schools regarding hand hygiene. Their results have shown the positive effects of this method on the improvement of students’ knowledge and performance in hand hygiene techniques [37]. Considering the sensitivity of Intensive Care Units and the inevitable need to improve hand hygiene behavior in nurses with effective motivational and educational approaches, this study is designed and implemented to assess the effectiveness of motivational interviews and teach-back on the rate of hand hygiene compliance in Intensive Care Unit nurses.
Methods
A three-group quasi-experimental study with pre-test and post-test design was performed from May to September 2020 in a selected hospital in Tehran. Out of 9 Intensive Care Units of the hospital, 3 Intensive Care Units were randomly selected. Then the nurses working in selected ICUs were measured and statistically analyzed in terms of variables affecting the outcomes of the interventions such as age, gender, education level, work experience in ICU, marital status, and there was no statistically significant difference between all groups in terms of the mentioned variables with p < 0.05 (Tab. I). So the selected wards were randomly assigned to 3 study groups including: control group, experimental group 1 with motivational interview intervention and experimental group 2 with teach back intervention. The control group received only the usual hospital teaching in hand hygiene, but in the experimental groups 1 and 2, in addition to the usual teaching, they received motivational interview intervention and teach back in five weekly sessions, respectively. Inclusion criteria were having a bachelor’s degree or higher in nursing and at least 1 year of experience in the Intensive Care Unit, and exclusion criteria included not attending more than 20% of sessions.
Tab. I.
Comparison of Demographic Variables among Nurses in the study groups.
| Group → |
Experimental 1 (Motivational Interview) | Experimental 2 (Teach back) | Control | Total | Statistic tests | |
|---|---|---|---|---|---|---|
| Variable | Number (percent) | Number (percent) | Number (percent) | Number (percent) | ||
| Gender | Male | 19 (61.3%) | 23 (79.3%) | 19 (67.9%) | 61 (69.3%) | Chi-square = 3.75 P Value = 0.440 |
| Female | 12 (38.7%) | 6 (20.7%) | 9 (32.1%) | 27 (29.5%) | ||
| Marital status | Married | 28 (90.3%) | 29 (100%) | 26 (92.9%) | 83 (94.3%) | Chi-square = 2.78 P Value = 0.249 |
| Single | 3 (9.7%) | 0 (0%) | 7 (7.1%) | 5 (5.7%) | ||
| Educational attainment* | BS | 24 (77.4%) | 20 (69%) | 27 (96.4%) | 71 (80.7%) | Chi-square = 7.43 P value = 0.110 |
| MS | 6 (19.4%) | 7 (24.1%) | 1 (3.6%) | 14 (15.9%) | ||
| PhD | 1 (3.2%) | 2 (6.9%) | 0 (0%) | 3 (3.4%) | ||
| Employment history | < 7 years | 16 (51.6%) | 13 (44.8%) | 19 (67.9%) | 48 (54.5%) | Chi-square = 3.213 P Value = 0.217 |
| >7 years | 15 (48.4%) | 16 (55.2%) | 9 (32.1%) | 40 (45.5%) | ||
| Age | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | ANOVA F = 1.88 P value = 0.159 |
|
| 43.12 ± 8.99 | 41.68 ± 11.45 | 37.82 ± 11.86 | 40.96 ± 10.88 | |||
| Educational attainment* including: BS (Bachelor of Science), MS (Master of Science), PhD (Doctor of Philosophy). | ||||||
The study instrument consisted of two parts, the first part of the demographic information questionnaire including age, sex, degree of education, work experience and the second part, standard checklist (Hand Hygiene Practices Inventory (HHPI)) approved by the Ministry of Health and Medical Education to assess hand hygiene behaviors which is used equally for all medical centers across the country. According to the checklist, each nurse was examined in an open and direct observation with a time interval of 20 ± 10 minutes in terms of hand hygiene compliance in 5 defined positions including: (before contact with the patient, before aseptic procedures, after contact with the patient’s secretions, after physical contact with the patient and after contact with the patient’s environment) and in terms of hand hygiene including three types of performance: hand washing with soap and water (Hand Wash), rubbing with an alcohol-based solution (Hand Rub) and hand hygiene non-compliance or acting in an incorrect way. All observations were performed equally by a trained and experienced nurse in measuring hand hygiene behaviors in the morning and evening work shifts. The presence of the observer in the study sections was informed by the nurses. Based on the above checklist, the rate of hand hygiene compliance in the nurses under study was presented with the number and percentage based on the type of action taken in each observed position. Pre-test was performed within two weeks before the intervention and post-test was performed 4 weeks (follow-up stage) after the intervention. Data were analyzed using SPSS 24 software. For the nominal variables, we conducted descriptive analysis by using frequencies and percentages as well as inferential analysis was carried out using the Chi-square test. The normally distributed continuous variables (e.g., age) were analyzed by using mean (M) and standard deviations (±) also ANOVA test.
METHOD OF INTERVENTION
The executive model of motivational interview sessions is based on the relevant literatures [38, 39] and the outline of teach back sessions is based on the model proposed by Bodenheimer and Anderson [36, 40]. and was performed after obtaining the experiences of previous researchers and expert approval (consisting of 6 people with specialties of PhD in Health Education, Nursing Faculty, Infection Control Supervisor). To perform the interventions, a nurse participated in a special teaching course and was trained and the interventions were performed by a qualified nurse (certified) and under the supervision of the research team. Sessions in both types of interventions included 5 sessions in 5 consecutive weeks, which were held in accordance with the conditions and needs of nurses in different shifts in the morning and evening. The content of motivational interview sessions is: Session 1: Familiarity and agreement between nurses and the interviewer, Session 2: Identifying emotions and its effect on behavior, Session 3: Determining healthy and unhealthy behaviors and the need to change behavior, Session 4: Explaining personal values and goals, Session 5: Discovering doubts and ambiguities and being ready to change and determine the perspective. The duration of the sessions is between 20 to 45 minutes and in each session, special worksheets are provided to the samples to record their feelings, attitudes, thoughts, ambiguities and doubts, personal and professional values. After completing the next session, the necessary feedback was given to the samples. 5 teach back sessions included 3 individual sessions and 2 group sessions and the duration of the sessions was between 20-30 minutes. In individual sessions, educational concepts were presented and incorrect perceptions were corrected by receiving frequent feedback from the nurse. In the group meetings, in addition to the exchange of concepts between the instructor and the nurses, among the members of the group, an exchange took place so that each nurse repeated the correct concept to his colleague and created an atmosphere of participation, collective acceptance, empathy, emotional support, self-evaluation and mutual evaluation.
After the interventions, 4 weeks of follow-up and continuous exchange of information between the instructor and the samples in a WhatsApp group for both experimental groups continued, and after 4 weeks of follow-up, the post-test phase was measured.
Results
All 88 nurses of the mentioned wards met the inclusion criteria and were fully present until the end of the intervention. The number of samples was 31 in the motivational interview group, 29 in the teach back group and 28 in the control group (Fig. 1). The age range of nurses participating in the study was between 25 and 61 years. There was no Statistically significant difference between the groups in terms of demographic variables such as age (p = 0.159), gender (p = 0.440), marital status (p = 0.24 9), educational attainment (p = 0.110), employment history (p = 0.217) (Tab. I).
Fig. 1.
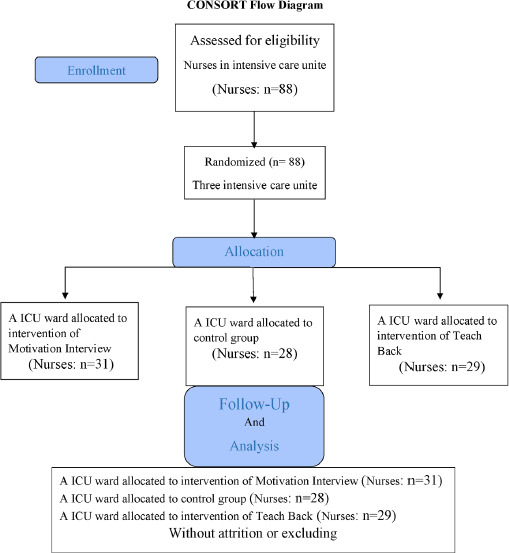
CONSORT Flow Diagram for the study.
In the pre-test stage, 200 positions in each study group were observed for hand hygiene compliance and in the post-test, 200 positions were observed, so a total of 600 positions were observed in the pre-test and 600 positions after the test. The rate of hand hygiene compliance in both stages of the assessment and in all three study groups was lower than the standard rate set by the Ministry of Health and Medical Sciences, i.e. 50%. In the pre-test stage, there was no statistically significant difference with p = 0.158 in all 3 groups in terms of hand hygiene. However, after the intervention, in the experimental group 1, the rate of hand hygiene compliance in the use of alcohol-based solution (hand rub) raised from 8% in the pre-test to 18.5% in the post-test and the rate of hand washing with soap and water (hand wash) increased from 1.5% to 22% and these values in experimental group 2, increased from 4% to 19.5% in hand rub and from 3.5% to 17% in hand wash, respectively. Chi-square test showed that the rate of hand rub and hand wash before and after the intervention in the experimental groups was statistically significant with p < 0.001. But in the control group, the rate of hand hygiene with two methods of hand rub and hand wash in the pre-intervention stage was 5.5% and 5%, respectively, which after the intervention was 1% and 2.5%, respectively. There was not a statistically significant difference in the rate of hand hygiene before and after the intervention in the control group (Tab. II).
Tab. II.
Comparison of Nurses performance in the study groups in 200 position of hand hygiene compliance in each stage of measurement.
| Group → |
Experimental 1 (Motivational Interview) | Experimental 2 (Teach back) | Control | Chi-square test | |
|---|---|---|---|---|---|
| Stage | Variable | Number (percent) | Number (percent) | Number (percent) | |
| Pre Test | Correct HW* | 3 (1.5%) | 7 (3.5%) | 10 (5%) | Chi-square = 6.603 P value = 0.158 |
| Correct HR* | 16 (8%) | 8 (4%) | 11 (5.5%) | ||
| Non/incorrect* | 181 (90.5%) | 185 (92.5%) | 179 (89.5%) | ||
| Total | 200 (100%) | 200 (100%) | 200 (100%) | ||
| Post Test | Correct HW | 44 (22%) | 34 (17%) | 5 (2.5%) | Chi-square = 85.512 P value < 0.001 |
| Correct HR | 37 (18.5%) | 39 (19.5%) | 2 (1%) | ||
| Non/incorrect | 119 (59.5%) | 127 (63.5%) | 193 (96.5%) | ||
| 200 (100%) | 200 (100%) | 200 (100%) | Total | ||
| Correct HW*: correct hand washing with soap and water (Hand Wash); Correct HR*: correct rubbing with an alcohol-based solution (Hand Rub); Non/ incorrect*: hand hygiene non-compliance or acting in an incorrect way. | |||||
Discussion
The present study was conducted with the aim of investigating the effectiveness of motivational interviews and teach-back on the rate of hand hygiene compliance in Intensive Care Unit nurses. The average age of the nurses participating in this study was 40.96 ± 10.88 years. The majority of them were male (69.3%), married (94.3%) with a bachelor’s degree in nursing (80.7%) and (54.5%) had less than 7 years of work experience in the ICU. In the wards under our study, due to the need for greater physical strength and endurance as well as sufficient knowledge and skills, the majority of nurses are men with a bachelor’s degree or higher. In a similar study, Salamati et al. showed the effectiveness of the motivational interviews following lecture teaching on hand hygiene behaviors in 128 nurses working in a pediatric hospital. The mean age of the nurses was 35.83 ± 7.184 years, also the majority of them were married (82.8%) and (76.6%) had a bachelor’s degree or higher. But unlike our study, (90.6%) were female [41]. This could be due to the fact that the research environment was a pediatric hospital. However, despite the different gender distribution in both studies, the results were similar and consistent.
Results of this study showed that both motivational interview and teach back were effective in promoting health compliance, but motivational interview was more effective that teach back on hand hygiene in Intensive Care Unit nurses. Numerous studies examined the positive effects of motivational interview [42-44] or teach back [26, 37, 45, 46] on behavior change separately, but the comparative study of the effect of both in one study was very small. Despite the need to promote behaviors related to hand hygiene in health workers, less of these two methods are used.
So, we had to use similar studies in other fields for comparison. Zabolipour et al. in comparing the effect of two methods of motivational interview and teach back on adherence of patients with hypertension to the treatment regimen showed that both methods are effective in increasing patients’ adherence to the treatment regimen but the rate of adherence to the treatment regimen in the motivational interview group was higher than the teach back group [47]. In their study, Najjar Nasab et al. showed the positive effect of motivational interviews on behavior change and lifestyle in women with eating disorders [48]. These findings indicate the facilitative effect of motivational interview on changing health-promoting behaviors.
In fact, no one is 100% unmotivated to change, but to motivate the individual to change requires internal conflicts to be resolved in an empathetic and supportive environment which is provided by a motivational interview. Real motivation is also enhanced by the successful experience that a person freely acquires in the right course of action [49]. It is noteworthy that although most studies emphasize the positive effect of motivational interview on behavior change, its persistence is still questionable. Dorstyn et al. investigated the effects of motivational interviewing on 987 patients with multiple sclerosis for their health care management. They found that motivational interview may improve rehabilitation care for these patients. However, evidence for persisting benefits to health outcomes and behavior is currently limited [50]. A meta-analysis study examining the effect of motivational interview on treatment adherence in 962 patients with chronic pain showed that the effect of motivational interview is limited and short-term and more studies are needed for long-term effect and change in patient self-management behavior [51]. In other words, the time and follow-up in an effective motivational interview, increases it. Numerous studies showed that most of the effects of motivational interview are mostly high in the first few months, but decrease over time, and this decrease is not due to a decrease in the effect of motivational interview, but to the fact that behavior changes requires appropriate contexts and other co-treatments in addition to motivational interview [52, 53]. Therefore, combining different methods of behavior change, such as teach back, motivational interview and follow-up care can be effective in perpetuating behavior change.
Numerous studies emphasized the effectiveness of teach back in changing health-promoting behaviors and the need to use it in various therapies. However, in the field of behavior, hand hygiene received less attention [54, 55]. Some studies showed that, when more information is provided, less information is remembered and almost half of the information remembered is incorrect. The use of teach back method has a great effect on strengthening and consolidating educational content and their application [21]. In one project, using teach back, 300 members of a multidisciplinary team (including intensive care nurses, emergency, surgical nurses, nutritionists, respiratory care practitioners, and occupational and physical therapists) were shown that the teach back method was able to enhance the quality and safety of the care provided by the team members [56]. Despite the effectiveness of teach back, the lasting effects cannot be definitively stated. In their study, Rahmani et al. showed that teach back was effective on knowledge, practice, reducing readmission and quality of life in patients with chronic hepatitis in the short term after the intervention, but its effect was reduced in the long term [57]. Although both teach back and motivational interview methods improved the rate of hand hygiene compliance in nurses in the present study, but the persistence of its desired effects still needs further investigation. On the other hand, context factors and working conditions such as the high volume of tasks assigned, non-observance of the standard ratio of nurse to patient, lack of attention of officials to the proper performance of a nurse, weakness of incentive systems play a significant role in reducing nurses’ motivation to maintain and adhere to the correct behavior and adherence to it; as well as failure in performing continuous visits in the field of measuring the rate of hand hygiene compliance, lack of nurses’ knowledge about the prevalence of nosocomial infections in the workplace and inappropriate access to facilities required for hand hygiene, including (low quality of solutions with an alcohol base, unsuitable wash basin and poor quality soap for washing hands) can significantly reduce the effects of these educational methods. Therefore, in order to study the durability and greater effectiveness of these methods, in addition to solving the problems raised, long-term studies and foresight are needed. Lack of follow-up and lack of understanding of support can reduce the effectiveness of interventions over time. One of the limitations of the present study is the lack of long-term follow-up and measuring the duration of the effect of motivational interview variables and teach back on the rate of hand hygiene compliance in nurses and also the limitation of the research environment to Intensive Care Units. Another limitation of the study was that nurses’ awareness of observing and measuring hand hygiene behaviors could have an effect on their performance and interfere with the results.
Conclusions
Findings showed that although both teach back and motivational interview methods are effective in promoting hand hygiene in nurses, the effect of motivational interview is more than teach back. Findings can help health policy makers in educational planning to improve nurses’ health behavior. Utilizing motivational interviews and teach back in medical centers can be a step in improving the performance of nurses in the field of hand hygiene and reduce nosocomial infections, treatment costs and length of hospital stay and death of patients.
Acknowledgments
This study was conducted in collaboration with the School of Nursing and the Health Management Research Center of Baqiyatallah University of Medical Sciences in Tehran, Iran. The officials of the selected hospital and the nurses participating in the study are appreciated. We also express our gratitude towards Clinical Research Center of Baqiyatallah Educational and Medical Hospital. The authors would like to acknowledge the School of Nursing of Baqiyatallah University of Medical Sciences in Tehran for their financial support in this study.
Funding
This study was supported by Baqiyatallah University of Medical Sciences in Tehran, Iran.
Etical consideration
Include observance of honesty and trustworthiness for the collection of information, consideration of the principle of usefulness for samples and obtaining written informed consent and the right to withdraw at any stage, and anonymity and confidentiality of information. This research project is registered and approved by National Ethics System in Biomedical Research under the supervision of the Ministry of Health and Medical Education of Iran with ID: (IR.BMSU.BAQ.REC.1398.019).
Informed consent statement
Informed consent was obtained from all participants (nurses).
Conflict of interest statement
The authors are responsible for the content of this article and state that there is no conflict of interest.
Authors’ contributions
ZA: contributed to design, implementation and data collection and writing of the manuscript. MM: contributed to the data collection, analysis and report the results. FK, MM: contributed to the conception, design, implementation of the study. ZV: contributed to the conception, design, implementation, data collection, analysis, and writing of the manuscript.
History
Received on January 25, 2022. Accepted on January 18, 2024.
Figures and tables
References
- [1].Anwar MM, Elareed HR. Improvement of hand hygiene compliance among health care workers in intensive care units. J Prev Med Hyg 2019;60:E31-5. https://doi.org/10.15167/2421-4248/jpmh2019.60.1.918. 10.15167/2421-4248/jpmh2019.60.1.918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Boyce JM. Current issues in hand hygiene. Am J Infect Control 2019;47S:A46-52. https://doi.org/10.1016/j.ajic.2019.03.024. 10.1016/j.ajic.2019.03.024 [DOI] [PubMed] [Google Scholar]
- [3].Sands M, Aunger R. Process evaluation of an acute-care nurse-centred hand hygiene intervention in US hospitals. Eval Rev 2020;41:29 https://doi.org/10.1186/s40985-020-00141-6. 10.1186/s40985-020-00141-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Longtin Y, Sax H, Allegranzi B, Schneider F, Pittet D. Videos in clinical medicine. Hand hygiene. N Engl J Med 2011;364:e24. https://doi.org/10.1056/NEJMvcm0903599. 10.1056/NEJMvcm0903599 [DOI] [PubMed] [Google Scholar]
- [5].Seferi A, Parginos K, Jean W, Calero C, Fogel J, Modeste S, Scott BA, Daly-Walsh M, Yap W, Kaur M, Brady T, Madaline T. Hand hygiene behavior change: a review and pilot study of an automated hand hygiene reminder system implementation in a public hospital. Antimicrob Steward Healthc Epidemiol 2023;3:e122. https://doi.org/10.1017/ash.2023.195. 10.1017/ash.2023.195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Lambe KA, Lydon S, Madden C, Vellinga A, Hehir A, Walsh M, O’Connor P. Hand hygiene compliance in the ICU: a systematic review. Crit Care Med 2019;47:1251-7. https://doi.org/10.1097/CCM.0000000000003868. 10.1097/CCM.0000000000003868 [DOI] [PubMed] [Google Scholar]
- [7].Chang NC, Jones M, Reisinger HS, Schweizer ML, Chrischilles E, Chorazy M, Huskins WC, Herwaldt L. Hand hygiene and the sequence of patient care. Infect Control Hosp Epidemiol 2022;43:218-23. https://doi.org/10.1017/ice.2021.82. 10.1017/ice.2021.82 [DOI] [PubMed] [Google Scholar]
- [8].Najafi Ghezeljeh T, Abbas Nejhad Z, Rafii F. A literature review of hand hygiene in Iran. Iran Journal of Nursing (IJN) 2013;25:1-13. [Google Scholar]
- [9].Nouri B, Hajizadeh M, Bahmanpour K, Sadafi M, Rezaei S, Valiee S. Hand hygiene adherence among Iranian nurses: a systematic review and meta-analysis. Nurs Pract Today 2021;8:11-24. https://doi.org/10.18502/npt.v8i1.4488. 10.18502/npt.v8i1.4488 [DOI] [Google Scholar]
- [10].Ziasheikholeslami N, Razavian F, Vafaei K, Esmkhani S. Evaluation of the Level of Hand Hygiene in Intensive Care Unit personnel of Kamkar Education, Research and Treatment Center of Qom in 2014, Iran. Qom University of Medical Sciences Journal 2016;10:64-9. [Google Scholar]
- [11].Mohanty A, Gupta PK, Gupta P, Kaistha N, Gupta P, Shankar R, Kumar P. Baseline assessment of hand hygiene knowledge perception: an observational study at a newly set up teaching hospital. J Family Med Prim Care 2020;9:2460-4. https://doi.org/10.4103/jfmpc.jfmpc_20_20. 10.4103/jfmpc.jfmpc_20_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Santy-Tomlinson J. We need to talk about hand hygiene: a time to reflect on compliance. Int J Orthop Trauma Nurs 2020;39:100819. https://doi.org/10.1016/j.ijotn.2020.100819. 10.1016/j.ijotn.2020.100819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Kobra P, Sima L, Fariborz R, Rasouli AS, Neda K. The comparison of the effectiveness of two education methods video and lecture on knowledge, belief and practice of hand hygiene in nursing students: clinical trial. Int J Med Res Health Sci 2016;5:240-8. [Google Scholar]
- [14].De Farias MEL, da Silva Gonçalves J, de Jesus IS. Adesão à higiene das mãos antes e após intervenções educativas do dia mundial para higienização das mãos em um hospital universitário. Revista Eletrônica Acervo Saúde 2019;11:e1354-e. https://doi.org/10.25248/reas.e1354.2019. 10.25248/reas.e1354.2019 [DOI] [Google Scholar]
- [15].Martos-Cabrera MB, Mota-Romero E, Martos-García R, Gómez-Urquiza JL, Suleiman-Martos N, Albendín-García L, Cañadas-De la Fuente GA. Hand hygiene teaching strategies among nursing staff: a systematic review. Int J Environ Res Public Health 2019;16:3039. https://doi.org/10.3390/ijerph16173039. 10.3390/ijerph16173039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Zandiyeh M, Borzo SR. The level of hand hygiene compliance by operating room personnel of Educational Hospitals in Hamadan University of Medical Science. JHNM 2012;22:23-9. [Google Scholar]
- [17].Sands M, Aunger R. Development of a behaviour change intervention using a theory-based approach, Behaviour Centred Design, to increase nurses’ hand hygiene compliance in the US hospitals. Implement Sci Commun 2021;2:1-18. https://doi.org/10.1186/s43058-021-00124-x. 10.1186/s43058-021-00124-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Nour-Eldein H, Eldahshan NA. The effectiveness of hand hygiene education intervention for medical students in primary care settings, Ismailia city, Egypt. Middle East J Fam Med 2015;13:32-40. https://doi.org/10.5742/MEWFM.2015.92667. 10.5742/MEWFM.2015.92667 [DOI] [Google Scholar]
- [19].Ghaffari M, Rakhshanderou S, Safari-Moradabadi A, Barkati H. Exploring determinants of hand hygiene among hospital nurses: a qualitative study. BMC Nurs 2020;19:109. https://doi.org/10.1186/s12912-020-00505-y. 10.1186/s12912-020-00505-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Bikmoradi A, Mardani D, Soltanian A, Khatiban M. The impact of educational evidence-based hand washing program on knowledge, attitude, and adherence of intensive care units nurses. Avicenna J Nurs Midwifery Care 2013;21:5-13. [Google Scholar]
- [21].Yen PH, Leasure AR. Use and effectiveness of the teach-back method in patient education and health outcomes. Fed Pract 2019;36:284-9. [PMC free article] [PubMed] [Google Scholar]
- [22].Graveto JM, Santos C, Costa PS, Fernandes E, Alarico S, Osório N, Albano H, Oliveira V. Hand hygiene management among nurses: collective health challenges. Rev Bras Enferm 2018;71(Suppl 1):562-7. https://doi.org/10.1590/0034-7167-2017-053. 10.1590/0034-7167-2017-053 [DOI] [PubMed] [Google Scholar]
- [23].Naar S, Suarez M. Motivational interviewing with adolescents and young adults. Guilford Publications; 2021. [Google Scholar]
- [24].Choi S, Choi J. Effects of the teach-back method among cancer patients: a systematic review of the literature. Support Care Cancer 2021;29:7259-68. https://doi.org/10.1007/s00520-021-06445-w. 10.1007/s00520-021-06445-w [DOI] [PubMed] [Google Scholar]
- [25].Shersher V, Haines TP, Sturgiss L, Weller C, Williams C. Definitions and use of the teach-back method in healthcare consultations with patients: A systematic review and thematic synthesis. Patient Educ Couns 2021;104:118-29. https://doi.org/10.1016/j.pec.2020.07.026. 10.1016/j.pec.2020.07.026 [DOI] [PubMed] [Google Scholar]
- [26].Oh EG, Lee HJ, Yang YL, Lee S, Kim YM. Development of a discharge education program using the teach-back method for heart failure patients. BMC Nurs 2021;20:109. https://doi.org/10.1186/s12912-021-00622-2. 10.1186/s12912-021-00622-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Barikani A, Negarandeh R, Moin M, Fazlollahi MR. The impact of motivational interview on self-efficacy, beliefs about medicines and medication adherence among adolescents with asthma: a randomized controlled trial. J Pediatr Nurs 2021;60:116-22. https://doi.org/10.1016/j.pedn.2021.04.020. 10.1016/j.pedn.2021.04.020 [DOI] [PubMed] [Google Scholar]
- [28].Eloi H. Implementing teach-back during patient discharge education. Nurs Forum 2021;56:766-71. https://doi.org/10.1111/nuf.12585. 10.1111/nuf.12585 [DOI] [PubMed] [Google Scholar]
- [29].McKay D. Motivational interviewing: accelerating readiness to change. J Cogn Psychother 2021. Apr 8:JCPSY-D-21-00005. https://doi.org/10.1891/JCPSY-D-21-00005. 10.1891/JCPSY-D-21-00005 [DOI] [PubMed] [Google Scholar]
- [30].Miller W.R, Rollnick S. Motivational interviewing: helping people change and grow. Guilford Publications; 2023. [Google Scholar]
- [31].Bischof G, Bischof A, Rumpf HJ. Motivational interviewing: an evidence-based approach for use in medical practice. Dtsch Arztebl Int 2021;118:109-15. https://doi.org/10.3238/arztebl.m2021.0014. 10.3238/arztebl.m2021.0014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Sokalski T, Hayden KA, Raffin Bouchal S, Singh P, King-Shier K. Motivational interviewing and self-care practices in adult patients with heart failure: a systematic review and narrative synthesis. J Cardiovasc Nurs 2020;35:107-15. https://doi.org/10.1097/JCN.0000000000000627. 10.1097/JCN.0000000000000627 [DOI] [PubMed] [Google Scholar]
- [33].Suire KB, Kavookjian J, Wadsworth DD. Motivational interviewing for overweight children: a systematic review. Pediatrics 2020;146:e20200193. https://doi.org/10.1542/peds.2020-0193. 10.1542/peds.2020-0193 [DOI] [PubMed] [Google Scholar]
- [34].Oveisi S, Stein LAR, Babaeepour E, Araban M. The impact of motivational interviewing on relapse to substance use among women in Iran: a randomized clinical trial. BMC Psychiatry 2020;20:157. https://doi.org/10.1186/s12888-020-02561-9. 10.1186/s12888-020-02561-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Östlund AS, Wadensten B, Kristofferzon ML, Häggström E. Motivational interviewing: experiences of primary care nurses trained in the method. Nurse Educ Pract 2015;15:111-8. https://doi.org/10.1016/j.nepr.2014.11.005. 10.1016/j.nepr.2014.11.005 [DOI] [PubMed] [Google Scholar]
- [36].Anderson KM, Leister S, De Rego R. The 5Ts for Teach Back: An Operational Definition for Teach-Back Training. Health Lit Res Pract 2020;4:e94-e103. https://doi.org/10.3928/24748307-20200318-01. 10.3928/24748307-20200318-01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Pawase MA, Tomy S, Gaikwad VS, Naik P, Gunjal VR, Kadam SB. Effectiveness of teach back method on knowledge and practice regarding hand washing among students of selected school. International Journal of Nursing Education and Research 2023;11:137-42. https://doi.org/10.52711/2454-2660.2023.00030. 10.52711/2454-2660.2023.00030 [DOI] [Google Scholar]
- [38].Widder R. Learning to use motivational interviewing effectively: modules. J Contin Educ Nurs 2017;48:312-9. https://doi.org/10.3928/00220124-20170616-08. 10.3928/00220124-20170616-08 [DOI] [PubMed] [Google Scholar]
- [39].Miller WR, Rollnick S. Motivational interviewing: helping people change and grow. Guilford press; 2012. [Google Scholar]
- [40].Bodenheimer T. Teach-back: a simple technique to enhance patients’ understanding. Fam Pract Manag 2018;25:20-2. [PubMed] [Google Scholar]
- [41].Salamati P, Poursharifi H, Rahbarimanesh AA, Koochak HE, Najafi Z. Effectiveness of motivational interviewing in promoting hand hygiene of nursing personnel. Int J Prev Med 2013;4:441-7. [PMC free article] [PubMed] [Google Scholar]
- [42].Gönderen Çakmak HS, Kapucu S. The effect of educational follow-up with the motivational interview technique on self-efficacy and drug adherence in cancer patients using oral chemotherapy treatment: a randomized controlled trial. Semin Oncol Nurs 2021;37:151140. https://doi.org/10.1016/j.soncn.2021.151140. 10.1016/j.soncn.2021.151140 [DOI] [PubMed] [Google Scholar]
- [43].Huang X, Xu N, Wang Y, Sun Y, Guo A. The effects of motivational interviewing on hypertension management: a systematic review and meta-analysis. Patient Educ Couns 2023;112:107760. https://doi.org/10.1016/j.pec.2023.107760. 10.1016/j.pec.2023.107760 [DOI] [PubMed] [Google Scholar]
- [44].Pas ET, Bradshaw CP. Introduction to the special issue on optimizing the implementation and effectiveness of preventive interventions through motivational interviewing. Prev Sci 2021;22:683-8. https://doi.org/10.1007/s11121-021-01278-9. 10.1007/s11121-021-01278-9 [DOI] [PubMed] [Google Scholar]
- [45].Mohammadi F, Jahromi MS, Bijani M, Karimi S, Dehghan A. Investigating the effect of multimedia education in combination with teach-back method on quality of life and cardiac anxiety in patients with heart failure: a randomized clinical trial. BMC Cardiovasc Disord 2021;21:535. https://doi.org/10.1186/s12872-021-02357-z. 10.1186/s12872-021-02357-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Oh EG, Lee HJ, Yang YL, Kim YM. Effectiveness of discharge education with the teach-back method on 30-day readmission: a systematic review. J Patient Saf 2021;17:305-310. https://doi.org/10.1097/PTS.0000000000000596. 10.1097/PTS.0000000000000596 [DOI] [PubMed] [Google Scholar]
- [47].Zabolypour S, Alishapour M, Behnammoghadam M, Abbasi Larki R, Zoladl M. A comparison of the effects of teach-back and motivational interviewing on the adherence to medical regimen in patients with hypertension. Patient Prefer Adherence 2020;14:401-10. https://doi.org/10.2147/PPA.S23171. 10.2147/PPA.S23171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Najjarnasab S, Dashbozorg Z. The effect of motivational interviewing on health promoting lifestyles and blood pressure of women with eating disorders. Health Psychology 2019;8:103-18. https://doi.org/10.30473/hpj.2019.40367.4005. 10.30473/hpj.2019.40367.4005 [DOI] [Google Scholar]
- [49].Dehghani F S, Ghasemi H, Safari S, Ebrahimi AA, Etemadi O. The effectiveness of group motivational interviewing sessions on enhancing of addicted women’s self-esteem and self efficacy. J Res Addict 2013;7:145-58. [Google Scholar]
- [50].Dorstyn DS, Mathias JL, Bombardier CH, Osborn AJ. Motivational interviewing to promote health outcomes and behaviour change in multiple sclerosis: a systematic review. Clin Rehabil 2020;34:299-309. https://doi.org/10.1177/0269215519895790. 10.1177/0269215519895790 [DOI] [PubMed] [Google Scholar]
- [51].Alperstein D, Sharpe L. The efficacy of motivational interviewing in adults with chronic pain: a meta-analysis and systematic review. J Pain 2016;17:393-403. https://doi.org/10.1016/j.jpain.2015.10.021. 10.1016/j.jpain.2015.10.021 [DOI] [PubMed] [Google Scholar]
- [52].Vafadar Z, Reazei R, Navidian A. Effectiveness of motivational interviewing on the weight self-efficacy life style in overweight and obese teenager boys. International Journal of Behavioral Sciences 2014;8:185-93. [Google Scholar]
- [53].Arkowitz H, Westra HA. Introduction to the special series on motivational interviewing and psychotherapy. J Clin Psychol 2009;65:1149-55. https://doi.org/10.1002/jclp.20640. 10.1002/jclp.20640 [DOI] [PubMed] [Google Scholar]
- [54].Feinberg I, Hendry T, Tighe E, Ogrodnick M, Czarnonycz C. Teach-Back Training for Nursing Students: Knowledge and Beliefs After Training for Health Literate Communication. Nurs Educ Perspect 2021;42:177-8. https://doi.org/10.1097/01.NEP.0000000000000670. 10.1097/01.NEP.0000000000000670 [DOI] [PubMed] [Google Scholar]
- [55].Masror Roudsari D, Feizi S, Maghsudlu M. Nurses’ hemovigilance knowledge and performance after teach-back, concept map, and lecture: a quasi-experimental study. Heliyon 2021;7:e05982. https://doi.org/10.1016/j.heliyon.2021.e05982. 10.1016/j.heliyon.2021.e05982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Klingbeil C, Gibson C. The Teach Back Project: a system-wide evidence based practice implementation. J Pediatr Nurs 2018;42:81-5. https://doi.org/10.1016/j.pedn.2018.06.002. 10.1016/j.pedn.2018.06.002 [DOI] [PubMed] [Google Scholar]
- [57].Rahmani A, Vahedian-Azimi A, Sirati-Nir M, Norouzadeh R, Rozdar H, Sahebkar A. The effect of the teach-back method on knowledge, performance, readmission, and quality of life in heart failure patients. Cardiol Res Pract 2020;2020:8897881. https://doi.org/10.1155/2020/8897881. 10.1155/2020/8897881 [DOI] [PMC free article] [PubMed] [Google Scholar]


