Abstract
Abstract
Objectives
To evaluate the effectiveness of lower limb robotic rehabilitation (LLRR) on cardiovascular health among individuals with stroke undergoing rehabilitation.
Design
Systematic reviews and meta-analysis.
Data sources
PubMed, Web of Science, Science Direct, Embase, China National Knowledge Infrastructure, Wangfang and VIP databases were searched from inception to 9 October 2023.
Eligibility criteria
Randomised controlled trials (RCTs) involving LLRR among individuals with stroke were included. We considered the potential impact of LLRR on the resting heart rate (HRrest), peak of oxygen uptake (VO2peak), peak of systolic blood pressure (SBPpeak) and peak of diastolic blood pressure (DBPpeak). Only studies published in Chinese or English were included.
Data extraction and synthesis
Two reviewers independently extracted data and assessed the risk of bias. Results were reported as Hedges’ g with 95% CIs. Meta-analyses were performed using a random effects model in STATA v17.0. The study was reported in compliance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement.
Results
Five RCTs with 179 patients were included in the meta-analysis. According to the Guideline Development Tool results, half of the evidence grades were moderate. The results of the meta-analysis showed that there were significant differences among robotic rehabilitation group than the control group in VO2peak (standard mean difference (SMD): 0.71, 95% CI: (0.28, 1.13), p<0.001, I2=45.61%), but insignificant difference found in HRrest (SMD: 0.30, 95% CI: (−0.12, 0.73), p=0.16, I2=34.25%), SBPpeak (SMD: 0.04, 95% CI: (−0.44, 0.52), p=0.86, I2=28.75%) and DBPpeak (SMD: 0.46, 95% CI: (−3.82, 4.73), p=0.83, I2=0.00%). No significant heterogeneity was found among articles. The risk of bias assessment revealed that two studies showed low bias in most domains.
Conclusion
Individuals undergoing stroke rehabilitation may benefit from LLRR with improved VO2peak but insignificantly impacted HRrest, SBPpeak and DBPpeak.
PROSPERO registration number
CRD42022382259.
Keywords: Systematic Review, Meta-Analysis, Stroke, REHABILITATION MEDICINE, Cardiovascular Disease
Strengths and limitations of this study.
The studies included in this systematic review and meta-analysis are randomised controlled trials (RCTs).
This study will be the first meta-analysis to evaluate the effectiveness of lower limb robotic rehabilitation on cardiopulmonary function among people with stroke.
Only five RCTs are included in this meta-analysis, all with a relatively small sample size.
Introduction
Stroke causes high morbidity, mortality, disability and heavy disease burden worldwide.1 According to the Global Burden of Disease report, there are an estimated 12.2 million patients with stroke all over the world, resulting in 143 million disability-adjusted life years and 6.55 million deaths.2 Stroke is one of the leading causes of motor dysfunction,3 especially lower limb dyskinesia. Lower limb dyskinesia is a common dysfunction in patients with stroke, which seriously affects their physical and mental health.4 Traditional rehabilitation approaches, such as occupational therapy, physical therapy and other rehabilitation approaches, are well-known in the field of stroke rehabilitation.5 Although traditional rehabilitation mostly depends on the clinical skill of a therapist. However, lower limb robotic rehabilitation (LLRR) opens up a new era in the field of post-stroke rehabilitation due to its wide application methods and success rate.6 7
The LLRR mainly focuses on improving post-stroke gait,8 balance9 and motor function.10 Studies showed that patients with stroke who received early robot-assisted gait training got better at achieving independent walking than those who received only conventional gait training.11 In addition to hemiplegia, patients with stroke are prone to decreased cardiovascular health and poor endurance. Based on the serious motor dysfunction of patients with stroke, how to improve the level of cardiovascular in patients is one of the urgent problems to be solved in clinical rehabilitation. Previous studies found that peak of oxygen uptake (VO2peak) was lower in patients with stroke compared with age-matched healthy people.12 13 However, peak exercise cardiac power output, cardiac output and the pressure-generating capacity of the heart are similar between stroke and healthy people.14 15 A recent study has shown that robot training may have an effect on cardiopulmonary function in stroke patients.16
Although several studies focused on post-stroke robotic rehabilitation on cardiovascular health, no consistent conclusions have yet been drawn. For instance, Lee et al17 suggested that robotic locomotor training was effective for improving cardiopulmonary function among patients with stroke, while another study showed that lower limb robot-assisted training just kept cardiopulmonary status stable without improving from pre-exercise states.18 Furthermore, to our knowledge, no systematic review has been conducted to evaluate the effects of LLRR on cardiopulmonary function among people with stroke.
Therefore, the objective of this study is to evaluate the effectiveness of LLRR on cardiovascular parameters such as resting heart rate, peak oxygen uptake and blood pressure among patients with stroke.
Methods
This systematic review was reported following the Preferred Reporting Items for the Systematic Reviews and Meta-Analyses statement 2020.19 This study was registered with the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42022382259).
Search strategy
We searched PubMed, Web of Science, Science Direct, Embase, China National Knowledge Infrastructure, Wanfang and VIP databases from inception to 9 October 2023 using the keywords ‘stroke’, ‘robot’ and ‘randomised controlled trial’. Search terms were combined in each database using the Boolean operators ‘AND’ or ‘OR’. In addition, the references list of the included studies was also hand-searched for inclusion. The search strategy is available in online supplemental material.
Inclusion and exclusion criteria
The following inclusion selection criteria were used: (a) population: patients with stroke; (b) intervention: patients were treated by LLRR; (c) comparison: patients were treated by conventional rehabilitation therapy or other therapies except for the LLRR; (d) outcomes: the resting heart rate (HRrest, beats per minute), peak of oxygen uptake (VO2peak, mL/kg/min), peak of systolic blood pressure (SBPpeak, mm Hg) and peak of diastolic blood pressure (DBPpeak, mm Hg); and (e) study design: randomised controlled trials (RCTs) to explore the effect of LLRR on cardiopulmonary function after stroke. The exclusion criteria were as follows: (a) letter, review, case report or comments; (b) studies with incomplete data that cannot be obtained from the authors; and (c) the language is not English or Chinese.
Quality evaluation
Two reviewers independently assessed the methodological quality of the included RCTs20 using the Cochrane Risk of Bias (RoB) Tool. Disagreements were resolved by discussion with a third reviewer. The RoB tool included seven aspects which were random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting and other bias. Each of aspects was rated as having a low risk of bias, an unclear/some concern and high risk of bias. Additionally, the Grading of Recommendations, Assessment, Development and Evaluation Profile (GRADEpro) Guideline Development Tool (GDT) was used to assess the evidence grade.21 This tool included five aspects: risk of bias, inconsistency, indirectness, imprecision and other considerations. The categories of recommendation level of evidence were as follows: (a) high: which means that further research is very unlikely to change our confidence in the effect estimate; (b) moderate: which means that further research is likely to play an important role in our confidence in the effect estimate and may change the estimate; (c) low: which means that further research is very likely to play an important role in our confidence in the effect estimate and to change the estimate; and (d) very low: which means that it is uncertain about any effect estimate. We used the online version of GRADEpro GDT21 to complete evidence synthesis.
Literature screening and data extraction
Two reviewers independently screened all of titles and abstracts and deleted duplicate and irrelevant studies. Two reviewers scanned the full text to determine whether the studies met the inclusion criteria. Two reviewers resolved disagreements about article inclusion through discussion with a third reviewer to reach a final consensus. Two reviewers completed the data extraction for the following characteristics of each study: author, publication year, sample size of patients in each group, mean age, intervention of each group and follow-up duration. The clinical outcomes included HRrest, SBPpeak, DBPpeak and VO2peak. The effect size measure selected in this meta-analysis was the standard mean difference (Hedges’ g).
Statistical analysis
We used STATA v17.0 to perform meta-analysis using the random effect model. We calculated the Hedges’ g and 95% CIs for continuous outcomes. The statistically significant value was a p value less than 0.05. If the I2 value was more than 50%, the heterogeneity was large. It was necessary to perform sensitivity tests using residual monadic analysis to estimate the impact of the study results. A small T2 value meant a small heterogeneity. Due to lack of required data and a small sample size, we did not analyse publication bias. Considering the non-uniform sample size, the effects were pooled using a random effects model.
Patient and public involvement
None.
Results
Study characteristics
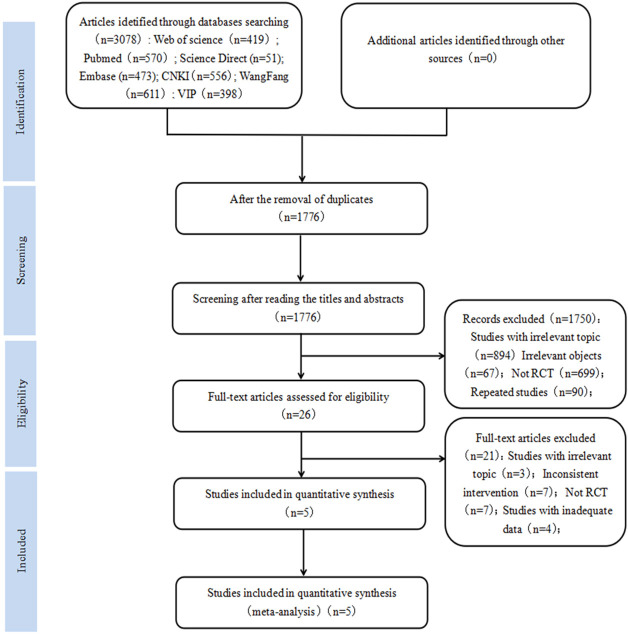
Of 3078 studies, five studies22,26 met all inclusion criteria and were included in this systematic review (figure 1). Online supplemental table 1 summarises the main characteristics of all included studies. We calculated data from a total of 179 patients with stroke with mean age of 60.76, 111 (62.01%) male. The most common treatment programme was routine rehabilitation therapy in the conventional treatment group and routine rehabilitation therapy plus robot therapy in the intervention group. The conventional treatment group included sit-stand balance training, active transfer, sit-stand training, reinforcement exercises and so on. Lokomat,25 26 GaitMotus,22 Flexbot24 and Walkbot23 were used in the intervention group. Of five articles, four articles23,26 compared the effectiveness of LLRR with conventional rehabilitation training, only one article22 combined LLRR with respiratory training and conventional therapy and compared it with respiratory training alone as a control group. Four articles were reported on HRrest, four on VO2Peak and two on blood pressure, with a follow-up period of 2 to 8 weeks.
Figure 1. Search results and the selection procedure.
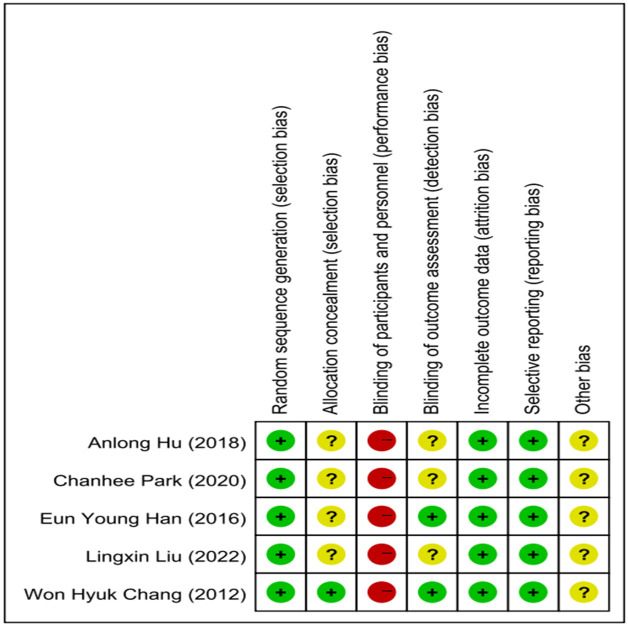
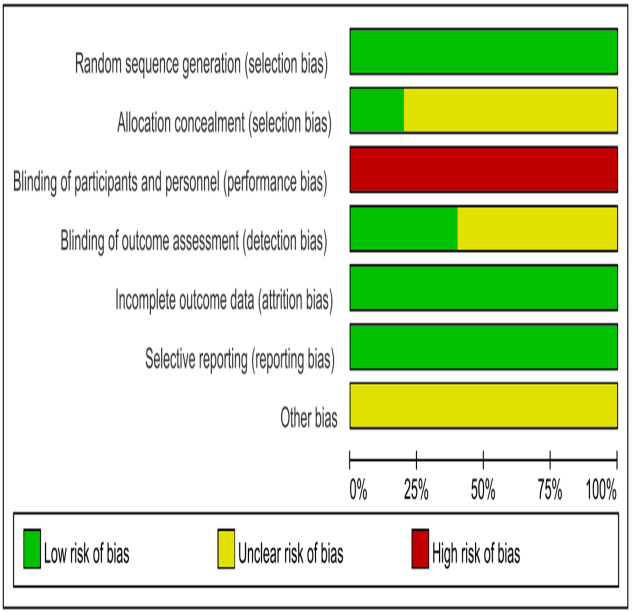
Risk of bias assessment
We assessed the quality of included RCTs according to the Cochrane RoB Tool (figure 2). According to RoB tools, five articles had a high risk of bias due to lacking blinding of patients and personnel, four articles had some concerns because of allocation concealment and blinding of outcome assessment, and five articles had a low risk in terms of random selection, incomplete outcome data and selection reporting (figure 3).
Figure 2. Methodological quality of the randomised controlled trials.
Figure 3. Risk of bias.
Effect of LLRR on cardiovascular parameters in patients with stroke
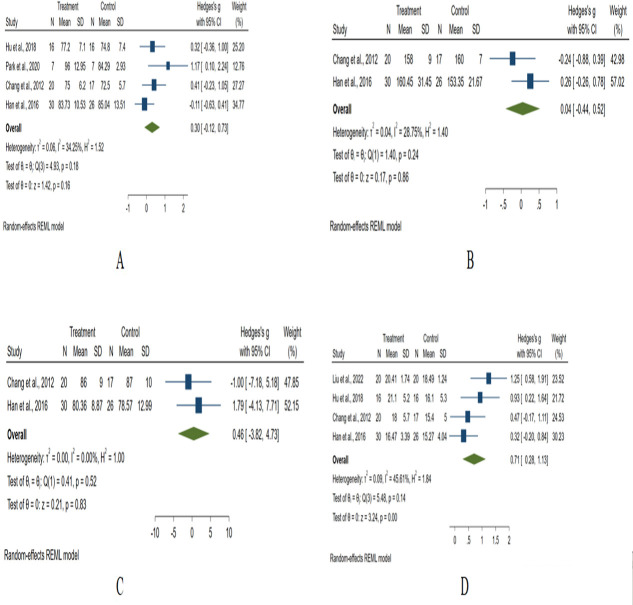
From 139 patients with four RCTs,23,26 we found that LLRR had no significant effect on HRrest improvement among patients with stroke (standard mean difference, SMD=0.30, 95% CI: −0.12 to 0.73, p=0.16, figure 4A. No significant heterogeneity was found among articles (T2=0.06, I2=34.25%, p=0.18).
Figure 4. Forest plot diagram showing HRrest (A), SBPpeak (B), DBPpeak (C) and VO2peak (D). DBPpeak, peak of diastolic blood pressure; HRrest, resting heart rate; SBPpeak, peak of systolic blood pressure; VO2peak, peak of oxygen uptake.
Regarding SBPpeak of 93 patients from two articles,25 26 we found that LLRR had no significant impact on the improvement of SBPpeak than the conventional treatment group (SMD=0.04, 95% CI: −0.44 to 0.52, p=0.86, figure 4B). No statistical heterogeneity was found among pooled studies (T2=0.04, I2=28.75%, p=0.24).
Two articles25 26 investigating DBPpeak of 93 patients, among the LLRR group, there was not significant improvement in the control group (SMD=0.46, 95% CI: −3.82 to 4.73, p=0.83, figure 4C). There was no significant statistical heterogeneity (T2=0.00, I2=0.00%, p=0.52).
From 165 patients with four articles,23,26 we found that LLRR significantly increased VO2peak compared with the control group (SMD=0.71, 95% CI: 0.28 to 1.13, p<0.001, figure 4D), but no significant heterogeneity was found (T2=0.09, I2=45.61%, p=0.14) among studies.
Evidence level and recommendation strengths
We evaluated the quality of evidence using GRADEpro GDT.21 Considering the different LLRR used in the studies, the inconsistency of HRrest and VO2peak was assessed as ‘serious’. The results of the GDT showed that half of evidence grades were moderate due to the fact that the certainty assessment was not serious in terms of indirectness and imprecision. LLRR may have no significant effect on HRrest (SMD=0.30, 95% CI: −0.12 to 0.73), SBPpeak (SMD=0.04, 95% CI: −0.44 to 0.52) and DBPpeak (SMD=0.46, 95% CI: −3.82 to 4.73). The effect of LLRR on VO2peak (SMD=0.71, 95% CI: 0.28 to 1.13) may be better than that of the conventional treatment group. Overall, the low or moderate level of evidence indicated that confidence in the effect estimate is likely to be changed by further research. Therefore, the result should be interpreted in clinical practice after a proper investigation of the patients’ cardiovascular status and other vitals (online supplemental table 2).
Discussion
Regarding cardiopulmonary function after LLRR, insufficient evidence is a concern in clinical practice. Our study focused on some prime variables to assess cardiopulmonary function after LLRR, and we found that VO2peak improved significantly, but HRrest, SBPpeak and DBPpeak remained unchanged. According to Pinna et al,27 a change of more than 30% of between-subject standard deviation (SD-change) was considered the minimal clinically important difference. However, the results of this study found no minimal clinically important differences in VO2peak (SD-change: 1.79% to 12.36%), HRrest (SD-change: 6.36% to 26.19%), SBPpeak (SD-change: 4.04% to 10.00%) and DBPpeak (SD-change: 0.11% to 18.18%) in the LLRR group. The I2 of the pooled meta-analysis results of HRrest, SBPpeak, DBPpeak and VO2peak in this study was less than 50% and T2 was small, indicating that the results of this meta-analysis were reliable.
LLRR had no significant effect on HRrest in patients with stroke (p>0.05), which was similar to the results of Qian Zhen et al.28 LLRR improved patients’ exercise endurance to a certain extent.29 The improvement of exercise ability is conducive to the prognosis of stroke patients. Study has shown that HRrest (80~85 beats per minute) was associated with an increased risk of stroke and could also accelerate the progression of atherosclerosis by increasing vascular oxidative stress.30 In future studies, it is recommended that the effect of LLRR in terms of HRrest be explored through high-quality RCTs in different stages of post-stroke patients.
The intervention of LLRR showed no significant effect in improving the SBPpeak (p>0.05) and DBPpeak (p>0.05). Another study31 also showed similar results. One reason of our results could be that our study included two studies on SBPpeak and DBPpeak, and the number of studies was too small. It is suggested that a large sample and multicentre RCT study be carried out in the future to verify the effect of blood pressure further. Exercise makes the heart and vascular system work more efficiently, promoting blood circulation and increasing the tolerance and elasticity of the heart muscle, thereby improving blood pressure. We suspect that the reason the results are not significant may be that LLRR training is usually low to moderate intensity and is designed to gradually improve blood circulation32 rather than drastically change blood pressure.
In this review, the intervention of LLRR increased VO2peak in patients with stroke compared with controls (p<0.05). This finding supported the basic principle of conventional rehabilitation supplemented with LLRR training on cardiovascular and exercise endurance in patients with stroke.22 The main reason is that LLRR promoted cardiomyocyte remodelling, which enhances diastolic function and improves blood pumping function in patients with stroke.33 Another reason is that LLRR increases oxygen intake and lactate threshold,34 which can improve the aerobic metabolism capacity of the body and increase the exercise endurance of patients with stroke. Hence, the LLRR is more likely to help patients with stroke to achieve better functional outcomes. Moreover, we found no minimal clinically important difference in VO2peak, which may be related to the fact that the sample size was too small to find clinical significance. It is suggested that a large sample study should be conducted in the future to explore the minimal clinical important difference of VO2peak.
Limitations
Several study limitations need to be noted. First, only five RCTs were included in this meta-analysis, all with a relatively small sample size. Second, only English and Chinese studies were included, which may lead to possible publication bias. Third, this study did not include studies with enough information, which may have an impact on the results of the meta-analysis. Therefore, more and better studies are needed in the field to validate the conclusions further.
Implications for future research
To the best of our knowledge, this is the first meta-analysis to explore the efficacy of LLRR on cardiovascular in patients with stroke. This study contributes to current knowledge by obtaining conclusions about the effectiveness of LLRR on VO2peak in patients with stroke. In addition, this study recommends more and more research to pay attention to the influence of LLRR on cardiovascular, which is conducive to further improving cardiovascular health for patients with stroke.
Conclusion
Individuals undergoing stroke rehabilitation may benefit from LLRR with improved VO2peak but insignificantly impacted HRrest, SBPpeak and DBPpeak.
supplementary material
Footnotes
Funding: This study was possible through funding from National Key R&D Program of China (No. 2023YFC3605203) and National Key R&D Program of China (No. 2022YFC3600300, No. 2022YFC3600305). The funding sources had no involvement in the study design, extraction, analysis, and interpretation of data, writing, or the decision to submit the article for publication.
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2023-082985).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Ethics approval: Not applicable.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Contributor Information
Yu Wu, Email: wy1059382020@163.com.
Jian Liu, Email: liujian0547@163.com.
Moneruzzaman Md, Email: mmshihab.pt@yahoo.com.
Jun Zhao, Email: zaojun@sohu.com.
Shicai Wu, Email: wscai66@163.com.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1.Geng H, Li M, Tang J, et al. Early Rehabilitation Exercise after Stroke Improves Neurological Recovery through Enhancing Angiogenesis in Patients and Cerebral Ischemia Rat Model. Int J Mol Sci. 2022;23:10508. doi: 10.3390/ijms231810508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2019 Stroke Collaborators Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20:795–820. doi: 10.1016/S1474-4422(21)00252-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang T, Zhao J, Li X, et al. Chinese Stroke Association guidelines for clinical management of cerebrovascular disorders: executive summary and 2019 update of clinical management of stroke rehabilitation. Stroke Vasc Neurol. 2020;5:250–9. doi: 10.1136/svn-2019-000321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bao Y, Duo Q, Zhang YR, et al. Effect of lower limb rehabilitation robot on walking function of ischemic stroke patients in convalescent stage. Chin J Rehabil Med. 2019;37:1079–83. doi: 10.3969/j.issn.1001-1242.2022.08.012. [DOI] [Google Scholar]
- 5.Hu J, Zou J, Wan Y, et al. Rehabilitation of motor function after stroke: A bibliometric analysis of global research from 2004 to 2022. Front Aging Neurosci. 2022;14:1024163. doi: 10.3389/fnagi.2022.1024163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Calafiore D, Negrini F, Tottoli N, et al. Efficacy of robotic exoskeleton for gait rehabilitation in patients with subacute stroke: a systematic review. Eur J Phys Rehabil Med. 2022;58:1–8. doi: 10.23736/S1973-9087.21.06846-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Terranova TT, Simis M, Santos ACA, et al. Robot-Assisted Therapy and Constraint-Induced Movement Therapy for Motor Recovery in Stroke: Results From a Randomized Clinical Trial. Front Neurorobot. 2021;15:684019. doi: 10.3389/fnbot.2021.684019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin Y-N, Huang S-W, Kuan Y-C, et al. Hybrid robot-assisted gait training for motor function in subacute stroke: a single-blind randomized controlled trial. J Neuroeng Rehabil. 2022;19:99. doi: 10.1186/s12984-022-01076-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Inoue S, Otaka Y, Kumagai M, et al. Effects of Balance Exercise Assist Robot training for patients with hemiparetic stroke: a randomized controlled trial. J Neuroeng Rehabil. 2022;19:12. doi: 10.1186/s12984-022-00989-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen Y-W, Chiang W-C, Chang C-L, et al. Comparative effects of EMG-driven robot-assisted therapy versus task-oriented training on motor and daily function in patients with stroke: a randomized cross-over trial. J NeuroEngineering Rehabil. 2022;19:6. doi: 10.1186/s12984-021-00961-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mayr A, Quirbach E, Picelli A, et al. Early robot-assisted gait retraining in non-ambulatory patients with stroke: a single blind randomized controlled trial. Eur J Phys Rehabil Med. 2018;54:819–26. doi: 10.23736/S1973-9087.18.04832-3. [DOI] [PubMed] [Google Scholar]
- 12.Dunn A, Marsden DL, Van Vliet P, et al. Independently ambulant, community-dwelling stroke survivors have reduced cardiorespiratory fitness, mobility and knee strength compared to an age- and gender-matched cohort. Top Stroke Rehabil. 2017;24:163–9. doi: 10.1080/10749357.2016.1236482. [DOI] [PubMed] [Google Scholar]
- 13.Ivey FM, Macko RF, Ryan AS, et al. Cardiovascular Health and Fitness After Stroke. Top Stroke Rehabil. 2005;12:1–16. doi: 10.1310/GEEU-YRUY-VJ72-LEAR. [DOI] [PubMed] [Google Scholar]
- 14.Jakovljevic DG, Moore SA, Tan L-B, et al. Discrepancy Between Cardiac and Physical Functional Reserves in Stroke. Stroke. 2012;43:1422–5. doi: 10.1161/STROKEAHA.111.649434. [DOI] [PubMed] [Google Scholar]
- 15.Araki S, Kamijo Y-I, Sato C, et al. Total Hemoglobin Mass Correlates with Peak Oxygen Consumption in Patients with Chronic Stroke. Cerebrovasc Dis. 2023;52:75–80. doi: 10.1159/000525597. [DOI] [PubMed] [Google Scholar]
- 16.Chen X, Yin L, Hou Y, et al. Effect of robot-assisted gait training on improving cardiopulmonary function in stroke patients: a meta-analysis. J Neuroeng Rehabil. 2024;21:92. doi: 10.1186/s12984-024-01388-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee H-J, Lee S-H, Seo K, et al. Training for Walking Efficiency With a Wearable Hip-Assist Robot in Patients With Stroke: A Pilot Randomized Controlled Trial. Stroke. 2019;50:3545–52. doi: 10.1161/STROKEAHA.119.025950. [DOI] [PubMed] [Google Scholar]
- 18.Ancona E, Quarenghi A, Simonini M, et al. Effect of verticalization with Erigo® in the acute rehabilitation of severe acquired brain injury. Neurol Sci. 2019;40:2073–80. doi: 10.1007/s10072-019-03917-0. [DOI] [PubMed] [Google Scholar]
- 19.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 21.GRADEpro GDT | Cochrane Community [EB/OL] 2023. https://community.cochrane.org/help/tools-and-software/gradepro-gdt Available.
- 22.Liu LX, Chen P, Yang S, et al. Effect of Lower limb robot training combined with breathing training on lung function and exercise endurance of stroke patients. Chin J Rehabil Med. 2022;37:1063–7. doi: 10.3969/j.issn.1001-1242.2022.08.009. [DOI] [Google Scholar]
- 23.Park C, Oh-Park M, Dohle C, et al. Effects of innovative hip-knee-ankle interlimb coordinated robot training on ambulation, cardiopulmonary function, depression, and fall confidence in acute hemiplegia. NeuroRehabilitation. 2020;46:577–87. doi: 10.3233/NRE-203086. [DOI] [PubMed] [Google Scholar]
- 24.Hu AL, Gu XD, Wu H, et al. Effect of Lower limb Rehabilitation robot training on cardiopulmonary function of stroke patients. Chin J Phys Med Rehabil. 2014;40:179–82. doi: 10.3760/cma.j.issn.0254-1424.2018.03.004. [DOI] [Google Scholar]
- 25.Han EY, Im SH, Kim BR, et al. Robot-assisted gait training improves brachial–ankle pulse wave velocity and peak aerobic capacity in subacute stroke patients with totally dependent ambulation. Medicine (Abingdon) 2016;95:e5078. doi: 10.1097/MD.0000000000005078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chang WH, Kim MS, Huh JP, et al. Effects of Robot-Assisted Gait Training on Cardiopulmonary Fitness in Subacute Stroke Patients. Neurorehabil Neural Repair. 2012;26:318–24. doi: 10.1177/1545968311408916. [DOI] [PubMed] [Google Scholar]
- 27.Pinna GD, Maestri R, Torunski A, et al. Heart rate variability measures: a fresh look at reliability. Clin Sci (Lond) 2007;113:131–40. doi: 10.1042/CS20070055. [DOI] [PubMed] [Google Scholar]
- 28.Qian Z, Lu LB, He J, et al. Effect of precise exercise prescription on cardiopulmonary fitness and sleep quality of stroke patients. Chin J Gen Pract. 2022;25:2468–74. doi: 10.12114/j.issn.1007-9572.2022.0030. [DOI] [Google Scholar]
- 29.Pak YJ, Koike A, Watanabe H, et al. Effects of a cyborg-type robot suit HAL on cardiopulmonary burden during exercise in normal subjects. Eur J Appl Physiol. 2019;119:487–93. doi: 10.1007/s00421-018-4040-7. [DOI] [PubMed] [Google Scholar]
- 30.Li XF, Sun K, Chen JZ, et al. Clinical characteristics of hypertensive patients with rapid resting heart rate. Chin J Circul. 2017;32:665–8. doi: 10.3969/j.issn.1000-3614.2017.07.010. [DOI] [Google Scholar]
- 31.Batacan RB, Jr, Duncan MJ, Dalbo VJ, et al. Effects of high-intensity interval training on cardiometabolic health: a systematic review and meta-analysis of intervention studies. Br J Sports Med. 2017;51:494–503. doi: 10.1136/bjsports-2015-095841. [DOI] [PubMed] [Google Scholar]
- 32.ADM Júnior F, Gomes SG, da Silva FF, et al. The effects of aquatic and land exercise on resting blood pressure and post-exercise hypotension response in elderly hypertensives. CVJA. 2020;31:8–14. doi: 10.5830/CVJA-2019-051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jin H, Jiang Y, Wei Q, et al. Effects of aerobic cycling training on cardiovascular fitness and heart rate recovery in patients with chronic stroke. NeuroRehabilitation. 2013;32:327–35. doi: 10.3233/NRE-130852. [DOI] [PubMed] [Google Scholar]
- 34.Jack LP, Purcell M, Allan DB, et al. Comparison of peak cardiopulmonary performance parameters during robotics-assisted treadmill exercise and arm crank ergometry in incomplete spinal cord injury. Technol Health Care. 2010;18:285–96. doi: 10.3233/THC-2010-0591. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.