Abstract
Background
Due to its deep position and complex surrounding anatomy, the scapular glenoid fracture was relatively difficult to deal with especially in cases of severe fracture displacement. Improper treatment may lead to failure of internal fixation and poor fracture reduction, severely affecting the function of the shoulder joint. Inferior scapular glenoid fracture was Ideberg type II fracture, and posterior approach was commonly used to deal with inferior scapular glenoid fracture. However, there are shortcomings of above surgical approach for inferior scapular glenoid fracture, such as insufficient exposure of the operative field, significant trauma, and limited screw fixation direction. This study adopts the axillary approach for surgery, which has certain advantages.
Methods
The clinical data of 13 patients with Ideberg type II scapular glenoid fractures treated from December 2018 to January 2024 were retrospectively analyzed. There were 8 males and 5 females, with an age range of 19 to 58 years and an average age of 38 years. The causes of injury were falls from heights in 7 cases and car accidents in 6 cases. There were 5 cases on the left side and 8 cases on the right side. The time from injury to surgery was 2 to 11 days, with an average of 5.5 days. All cases underwent open reduction and internal fixation through the axillary approach. Postoperative X-ray and CT three-dimensional reconstruction were performed on the next day to evaluate the fracture reduction and the position of internal fixation. During the follow-up period, follow-up examinations were performed every two months in the first half of the year and every three months in the second half. CT scans were performed during the examinations to assess the glenohumeral joint congruence, fracture healing, and position of internal fixation. The shoulder joint function was evaluated at 6 months postoperatively according to the Constant-Murley value score.
Results
The patients all achieved primary wound healing after surgery, without any complications such as infection or nerve injury. Re-examination on the second day after operation, all fractures obtained excellent reduction, and the internal fixation was in excellent position, and no screw was found to enter the joint cavity. All patients in this group were followed up for 6 to 25 months, with an average follow-up time of 11.7 months. All fractures were bony unioned, and the healing time ranged from 4 to 6 months, with an average healing time of 4.8 months. At 6-month follow-up, according to the Constant-Murley score, 11 cases were excellent and 2 case was good.
Conclusion
Open reduction and internal fixation through the axillary approach is an feasible and safe surgical method for the treatment in scapular Ideberg type II glenoid fractures with less stripping of soft tissue, minimal surgical trauma, and the incision is concealed and beautiful. It can provide a strong internal fixation for fractures, so patients can perform functional exercise early after operation, and the clinical results is satisfactory.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12893-024-02623-9.
Keywords: Surgical approach, Scapular glenoid, Fracture, Shoulder joint, Fracture fixation, Internal
Background
Scapular glenoid fractures are relatively rare clinically, accounting for about 10-15% of scapular fractures [1]. It is more common in young patients around 35 years old [2]. Most of them are caused by high-violence injuries such as car accident injuries and high-fall injuries [3]. Due to its deep position and complex surrounding anatomy, the scapular glenoid fracture was relatively difficult to deal with especially in cases of severe fracture displacement. Improper treatment may lead to failure of internal fixation and poor fracture reduction, severely affecting the function of the shoulder joint. According to the Ideberg classification [4], scapular glenoid fractures can be divided into six types, of which type I and type V can be divided into two and three subtypes respectively, while inferior edge fracture of the scapular glenoid belongs to Ideberg type II fracture.
With regard to the surgical indications for glenoid fractures, it is generally believed that articular surface collapse or fracture displacement greater than 5 mm, poor joint involution relationship of the glenohumeral joint, and glenohumeral joint instability are all recommended for surgical treatment [5]. For Ideberg type II scapular glenoid fracture, some studies recommend a posterior approach for surgery. After the fracture was reduced, 1 ∼ 2 hollow screws are used to fix the fracture fragments from the inferior edge of the glenoid to the basement of the coracoid process. The fixation of distal portion of the bone fragment is augmented with a plate [6]. However, It is difficult to screw the bone fragment in a direction which is vertical to the fracture line through posterior approach, and the mechanical strength of such fixation is decrease [7]. Xing Yong et al. [8] reported that the axillary approach was used to the treatment for type II scapular glenoid fracture, and achieved good clinical efficacy. This approach can expose the anterior and inferior margin of the glenoid. Therefore, we combine their experience and perform this approach for surgery. At the same time, the combination of screws and NICE knots was used to treat patients with Ideberg II glenoid fractures, and a good clinical effect was achieved, as reported as follows.
Patients and methods
Patient selection criteria
① Adult patients with ages older than 8 years; ② The fracture should classified type II according to Ideberg classification; ③ Patients with articular surface collapse or fracture displacement > 5 mm, poor humeral glenoid congruence, and instability of glenohumeral joint; ④ Patients who underwent surgery via axillary approach; ⑤ The time from injury to surgery ≤ 3 weeks; ⑥ Intact follow-up data.
Patient exclusion criteria
① Open fractures; ② Combined vascular or nerve injuries; ③ Old fractures; ④ Patients who underwent surgery via other approaches.
From December 2018 to January 2024, a total of 13 patients met the selection criteria and were included in the study. There were 8 males and 5 females, with an mean age of 38 years ranging from 19 to 58 years. The causes of injury included 7 cases of falling from height and 6 cases of car accidents. There were 5 cases on the left side and 8 cases on the right side, all of which were Ideberg type II glenoid fractures. The time from injury to surgery ranged from 2 to 11 days, with a mean of 5.5 days. Detailed patient information can be found in Table 1.
Table 1.
General information of patients in this group
| NO. | Cause of injury | Injury side | Time from injury to surgery(days) | Follow-up time(months) | Fracture healing time(months) | Constant-Murley score grade 6 months after surgery | Complications occurred |
|---|---|---|---|---|---|---|---|
| 1 | Fall from height | Left | 3 | 6 | 4 | Excellent | Not |
| 2 | Fall from height | Left | 5 | 8 | 6 | Excellent | Not |
| 3 | Car accident | Right | 11 | 20 | 5 | Good | Not |
| 4 | Fall from height | Right | 3 | 12 | 4 | Excellent | Not |
| 5 | Car accident | Left | 4 | 9 | 5 | Excellent | Not |
| 6 | Fall from height | Right | 6 | 10 | 6 | Excellent | Not |
| 7 | Fall from height | Left | 2 | 25 | 4 | Excellent | Not |
| 8 | Fall from height | Right | 5 | 12 | 5 | Excellent | Not |
| 9 | Car accident | Right | 10 | 8 | 4 | Excellent | Not |
| 10 | Fall from height | Right | 6 | 9 | 4 | Good | Not |
| 11 | Car accident | Left | 5 | 10 | 4 | Excellent | Not |
| 12 | Car accident | Right | 3 | 12 | 5 | Excellent | Not |
| 13 | Car accident | Right | 8 | 11 | 6 | Excellent | Not |
Surgical procedure
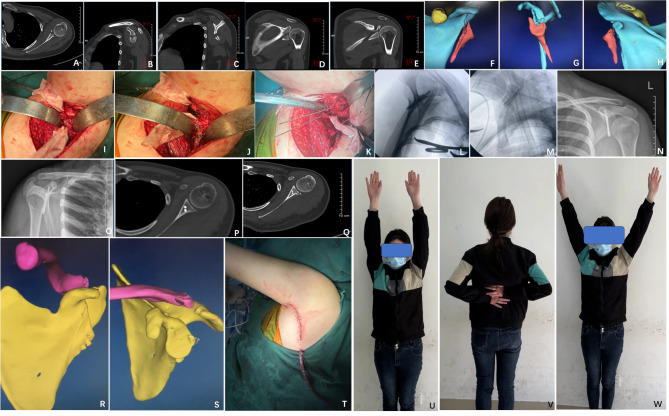
All patients in this study were placed under general anesthesia and operated on the lateral position. The surgical field and upper extremity are thoroughly disinfected for intraoperative control and adjustment of position. The affected limb is externally rotated, exposing the axilla. The incision extends from the top of the axilla along the anterior border of the latissimus dorsi muscle to the middle level of the outer border of the scapula [8], approximately 10 cm in length. The skin, subcutaneous tissue, and deep fascial layer are successively incised, exposing the latissimus dorsi muscle. Blunt dissection is performed to separate the anterior edge of the latissimus dorsi muscle, carefully exposing the axillary nerve, posterior circumflex humeral artery-vein-nerve bundle, and distal circumflex scapular artery. Rubber bands are used to protect these structures. The soft tissues overlying the bone surface are dissected, exposing the inferior border of the scapular glenoid. If the bone fragments at the inferior border of the scapular fossa are small and do not involve the distal end, it is not necessary to expose the distal circumflex scapular artery. However, if the fracture involves a larger range beyond the distal circumflex scapular artery, the distal end of the artery needs to be exposed for reduction and fixation of the distal fragment. After exposure, the assistant is instructed to pull the upper limb to avoid the humeral head impeding reduction of the fracture. Forceps or bone elevators are used to reduce the fracture fragments, and if necessary, Kirschner wires are inserted into the bone fragments as manipulative levers. It is important to note that after reduction, the articular surface and distal fracture ends need to be well-aligned. Otherwise, good reduction of one side may result in increased gap of other side. After confirming excellent reduction, temporary fixation is achieved using Kirschner wires. Fluoroscopy is performed to ensure good reduction and internal fixation, especially to confirm that the screws have not entered the joint space. The surgical cavity is irrigated with saline, and a drainage tube is left in place. The incision is closed layer by layer. (Figures 1 and 2)
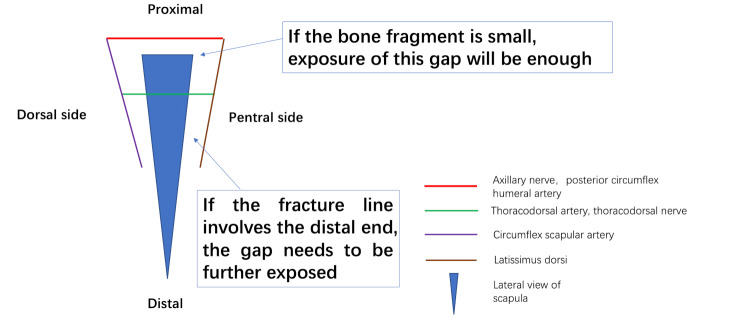
Fig. 1.
Exposure of the axillary approach in surgery. The yellow arrow indicates the anterior margin of the latissimus dorsi muscle, the blue arrow indicates the thoracodorsal artery, and the white arrow indicates the axillary nerve and posterior circumflex humeral artery
Fig. 2.
Illustration of the exposure in the axillary approach
Postoperative management and evaluation criteria for efficacy
The affected limb is suspended and immobilized for three weeks after surgery. Passive functional exercises, including elevation, extension, internal and external rotation, and adduction and abduction, are initiated on the first day after surgery. Active functional exercises are started one week later, and weight-bearing and daily activities are determined based on the follow-up condition. X-ray and CT three-dimensional reconstruction are conducted on the second day after surgery to evaluate fracture reduction and the position of internal fixation. During the follow-up period, patients receive a follow-up examination every two months in the first six months, and then once every three months. CT scans are performed during the follow-up to assess the congruency of the glenohumeral joint, fracture healing, and the position of internal fixation. After 6 months postoperatively, the Constant-Murley absolute value score is used to evaluate shoulder joint function, which includes pain (15 points), daily activities (20 points), range of motion (40 points), and muscle strength (25 points). Scores of 90–100 are considered excellent, 80–89 good, 70–79 fair, and < 70 poor [9].
Result
All incisions in this group of patients achieved phase I healing without complications such as infection or nerve injury. Follow-up X-ray examinations on the second day after surgery showed good fracture alignment and proper positioning of internal fixation. No screws were found in the joint space. All patients were up for an average duration of 11.7 months (ranging from 6 to 25 months). The fractures achieved bony union with a healing time ranging from 4 to 6 months with an average of 4.8 months. At the 6-month follow-up, according to the Constant-Murley grading system, 11 cases achieved excellent results, and 2 case achieved a good result. Among them, the two patients who achieved good results were 56 and 58 years old and both had preexisting shoulder osteoarthritis with limited range of motion and chronic shoulder pain. After fracture healing, the range of motion and pain symptoms did not worsen compared to before the injury. (Fig. 3)
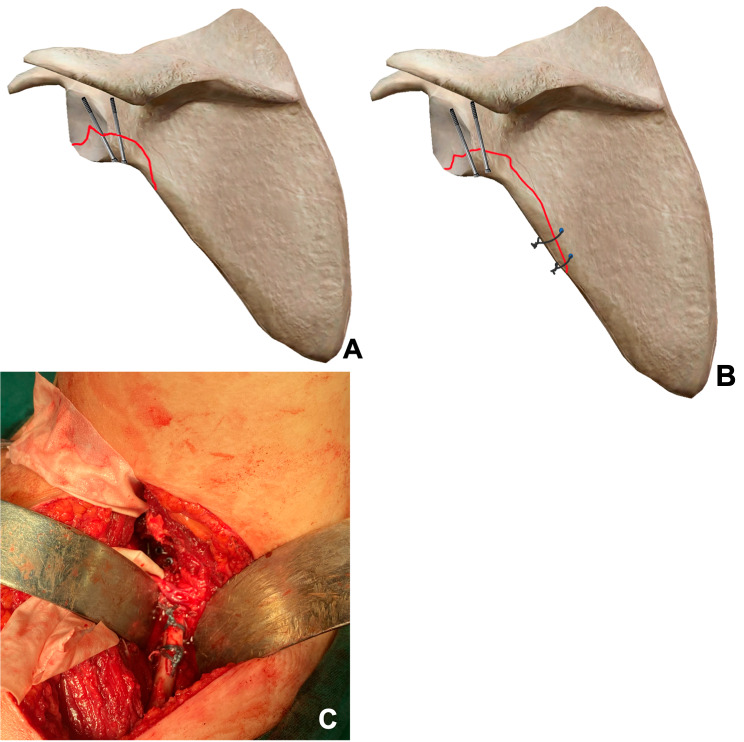
Fig. 3.
A 32-year-old female patient with left scapular glenoid fracture due to a vehicle accident, classified as Ideberg Type II. A ∼ H Preoperative CT scan showed scapular glenoid fracture(L)with fracture extending to the distal region; I The proximal fragment of the fracture was fixed with screws during surgery; J The distal fragment of the fracture was fixed using a Nice-Knot technique; K Surgical exposure through the axillary approach; L ∼ M intraoperative fluoroscopy showed excellent fracture reduction and proper screw placement; N ∼ S postoperative X-ray and CT scan showed excellent fracture reduction, satisfactory screw fixation without entering the joint cavity; T appearance of the incision site through the axillary approach, concealed and aesthetically pleasing; U ∼ W The patient’s shoulder joint function recovered well at the 6-month follow-up after surgery
Discussion
Scapular glenoid fractures are intra-articular fractures. It is generally believed that surgical treatment is recommended when the articular surface collapses or the fracture displacement is greater than 5 mm, the match between the glenoid and humerus is poor, and the glenohumeral joint is unstable [5]. For Ideberg II-type glenoid fractures, displacement usually occurs due to the traction of the triceps brachii muscle, so most of them require surgical treatment. Currently, the main surgical approaches for glenoid fractures include the deltoid-pectoralis major approach, the Judet and modified Judet approaches from the posterior, and surgical procedures assisted by arthroscopy. For Ideberg II-type glenoid fractures, since the fragments are located at the lower edge of the glenoid, good exposure and reduction cannot be achieved through either the anterior or posterior approaches, and both approaches require the disruption of muscle tissue, resulting in greater trauma and affecting the stability of the shoulder joint. In addition, the optimal fixation method for fractures is vertical fixation along the fracture line. However, for Ideberg II-type glenoid fractures, which have fragments located at the lower edge of the glenoid, neither anterior nor posterior approach can achieve optimal vertical fixation. Currently, there are also many studies recommending surgical procedures assisted by arthroscopy to minimize soft tissue trauma [10–13]. However, arthroscopic surgery is mainly suitable for patients with Ideberg Ia and III-type glenoid fractures [14], and it is difficult to achieve effective fixation for patients with type II fractures, especially for those with larger fragments and fractures extending beyond the joint capsule, resulting in risks of axillary nerve and posterior circumflex humeral artery injury [15].
Due to the rarity of Ideberg II glenoid fractures, there are few reports on the related approaches. There is a report [16] of a case applied the Brodsky approach (a modified posterior approach to the shoulder joint, entering through the gap between the infraspinatus and teres minor muscles) for the surgical treatment of Ideberg II glenoid fractures with shoulder joint subluxation. In the surgery, a screw and “H” plate were used to fix the fracture fragments, and good clinical results were achieved postoperatively. But this report is based on a single case with a small sample size. Park JK et al. [14] reported 7 cases treated using this approach, without opening the joint capsule for reduction and fixation during surgery. Two postoperative patients had minor complications, and the average Constant-Murley score was 89.1 ± 10.6. Tian Yun et al. [8, 17]first designed and invented the axillary approach through anatomical studies and applied it clinically. They used this approach to treat 13 cases of Ideberg type Ia glenoid fractures and 2 cases of type II fractures, all of which achieved good clinical efficacy. The average Constant-Murley score of the patients at 6 months after surgery was 84.54 ± 8.95, and no complications occurred. Ding H et al. [18] applied the same approach to treat 11 cases of Ideberg type I fractures and 2 cases of type II fractures. The shoulder joint range of motion at the last follow-up was 160.5°±9.3° in forward flexion, 155.6°±12.5° in abduction, 40.7°±5.8° in external rotation (neutral position), and 65.4°±12.1° in internal rotation (neutral position). The Constant-Murley score was (92.3 ± 6.5) points, and there were no complications in all patients. This study treated 13 cases of Ideberg type II glenoid fractures using this approach, and no complications occurred in all patients. At a 6-month follow-up, the Constant-Murley score was (93.1 ± 3.3), which was comparable to the aforementioned relevant reports.
Therefore, based on this study and relevant research, it is confirmed that the axillary approach has unique advantages in the treatment of Ideberg type I and type II glenoid fractures, including the following aspects: (1) This approach enters through the muscular and vascular/nerve gaps, without the need to disrupt muscle tissue, resulting in minimally invasive and less damage to shoulder joint stability, allowing for good postoperative shoulder joint function recovery; (2) For patients with Ideberg type II glenoid fractures, surgery can completely achieve reduction and fixation of the fracture under direct visualization through this approach. The direction of screw placement will not be hindered by the incision, allowing for vertical alignment with the fracture line and providing optimal biomechanical fixation strength; (3) The incision is located in the axilla, which is relatively concealed and aesthetically pleasing; (4) The incidence of vascular and nerve injuries is low.
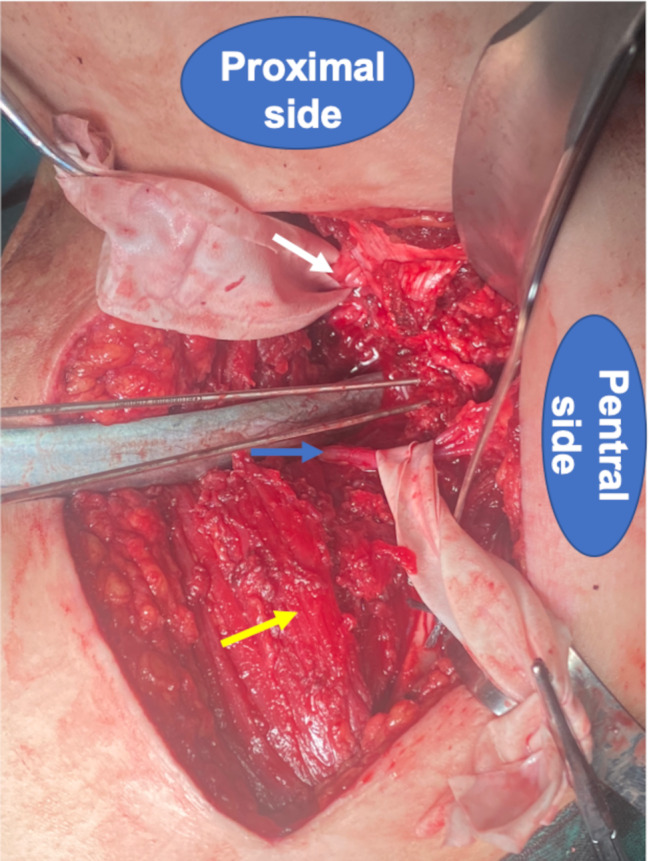
For patients with Ideberg type II glenoid fractures, current research tends to favor screw fixation or screw augmented plate fixation. For fractures with a smaller affected area, simple fixation with 1–2 hollow screws can be performed (Fig. 4a), which is relatively easy to perform. The main concern is the direction of screw placement to avoid entering the joint cavity. However, for fractures involving a more distal fracture line, isolated screw fixation alone cannot provide sufficient biomechanical strength. In most cases, it is necessary to combine the use of plates for fixation. However, we have found certain difficulties in plate fixation during clinical surgery. First, extensive stripping and exposure are required, at least beyond the range of two screw holes beyond the fracture line, in order to place the plate and fix it with screws at the distal end of the plate. Secondly, because the plate needs to be placed on the ridge of the scapula in the lateral aspect, and the distal end of the scapula is thin, a study [19] has found that the thickness of the scapula at distances of 1 cm and 2 cm from the articular surface are 17.8 ± 3.5 mm and 13.4 ± 10.5 mm, respectively. The thickness of the scapula at 1/4, 1/2, and 3/4 distances from the articular surface are 13.5 ± 5.8 mm, 11.5 ± 4.0 mm, and 8.6 ± 5.0 mm, respectively. Due to this anatomical feature, it poses some difficulties in placing the plate and inserting the screws. Therefore, considering these factors, we adjusted the fixation method during surgery and used a combination of screws and Nice knots to fix the fracture ends, effectively reducing muscle and soft tissue detachment (muscle detachment is only required to the distal end of the fracture line, without further detachment), and greatly reducing the difficulty of fixation, as well as reducing the surgical time and blood loss. The Nice knot is a double-wire self-locking knot which can provide sliding compression during the tightening process. It has good structural stability and is not easily to loosen. It has been widely used in fracture fixation [20–22] and can meet the needs of fixing distal fracture ends. The specific procedure is as follows: ① Reduce and confirm the excellent position of the fracture, and temporarily fix it with Kirschner wires; ② Place two 3.0 mm ∼ 3.5 mm hollow screws in the proximal end of the bone block (near the glenoid cavity); ③ Use a 2.0 mm Kirschner wire to drill two holes near the main bone block of the scapula, close to the fracture line, for preparation of passing the thread. First, pass one end of a 2# Ethibond suture through the bone hole, making it a double-strand, and wrap it around the far end of the fracture block. Then, use the Nice knot tying method to fix the main bone block and the distal end of the fracture block. Repeat this method for another set, increasing the stability of the fracture fixation (Fig. 4b and c). With this method of fixation, both the proximal and distal ends of the bone block are effectively fixed, resulting in good stability and minimal soft tissue detachment, thereby reducing the surgical trauma. This fixation method was used in all 4 patients in this group, and no cases of internal fixation failure or fracture displacement occurred.
Fig. 4.
Hollow screws combined with nice knot for the treatment of Ideberg type II glenoid fossa fractures A, For fractures with a smaller affected area, simple fixation with 1–2 hollow screws can be performed; B ∼ C, A combination of hollow screws and Nice knots was used to fix the Ideberg Type II fracture
For the axillary region has complex anatomical structures, including blood vessels, nerves, and lymph nodes, the surgeon needs to have a proficient understanding of these anatomical structures and perform gentle maneuvers during the operation. ① During the anatomical exposure in the surgery, it is necessary to first identify the anterior edge of the latissimus dorsi muscle, which is a key landmark for the surgical approach. After entering through this gap and pushing aside the muscle tissue, the proximal axillary nerve, posterior circumanal artery, and distal circumflex scapular artery should be identified. The anterior side is the thoracodorsal artery nerve, and the posterior side is the latissimus dorsi muscle. Operating within this range ensures a relatively safer surgery. In this group of patients, there were a total of 6 cases without any complications such as vascular or nerve injuries. ② When searching for the axillary nerve and circumflex humeral artery, the shoulder joint can be externally rotated by 90° to palpate the humeral head. The axillary nerve and its accompanying circumflex humeral artery are generally palpable as cord-like structures on the articular surface of the humeral head. ③ During reduction, it is not recommended to open the joint capsule to expose the articular surface. The assessment of whether the articular surface fracture is well reduced or not can be based on the reduction of the distal fracture ends. In most cases, a good reduction of the articular surface fracture can be achieved when the fracture is well reduced in a non-articular area. There may be a situation where the distal fracture end is well closed, but the articular surface fracture separates and opens. However, during the process of inserting a hollow screw, the separation of the articular surface fracture can gradually be compressed and closed by the sliding and compressive effects of the screw. ④ During the reduction process, if it is difficult to reduce, especially when the fracture involves a wider range, due to the deep location of the scapula, there are fewer options for reduction tools. One or two Kirschner wires can be inserted into the fracture fragments to assist the reduction operation, control rotation displacement, and combine with the pushing effect of the bone stripping. In general, the fracture can be well reduced in such cases. It should be noted that during the reduction process, the assistant can assist in traction of the upper limb to prevent the humeral head from pressing against the articular surface, which may make it difficult to reduce the fracture. ⑤ After the screw insertion, attention should be paid to the oblique radiographic view of the glenoid cavity to determine whether the screw has entered the joint cavity. Our experience with fluoroscopy is to have the patient lying on their side with the torso naturally leaning forward and the upper limb naturally hanging down, so that the direction of the fluoroscopy beam is perpendicular to the ground, which can obtain a relatively standard oblique view of the glenoid cavity.
Limitations of this study. Due to the rarity of Ideberg II-type glenoid fractures in clinical, the number of cases included in this study is relatively small. Therefore, further enlargement of the sample size and follow-up time is needed to further confirm the long-term efficacy and potential late complications of this approach.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
None.
Author contributions
Hai Wang and Jia-run Lin designed the study and drafted the manuscript. Hai Wang and Gui Wu collected and analyzed the data. Yun Xie and Yao-yu Qiu participated in critically read and revised the manuscript, performed the operation surgery. Yao-yu Qiu and Guo-zhen Wei performed the assessments and statistical analysis. All authors reviewed, read and approved the final manuscript. Availability of data and materials.
Funding
Joint Funds for the Innovation of Science and Technology, Fujian Province(NO. 2021Y9091).
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The ethics committee of the First Affiliated Hospital of Fujian Medical University approved the study protocol (approval number: MTCA, ECFAH of FMU[2015]084 − 1). Informed consent was obtained from all the study subject. The study was done in accordance with the principles outlined in the Declaration of Helsinki.
Consent for publication
All subjects and/or their legal guardians have informed consent to publish identification information/images in online public content.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Hai Wang and Jia-run Lin made equal contributions to this study and should serve as the co-first authors.
References
- 1.Südkamp NP, Jaeger N, Bornebusch L, Maier D, Izadpanah K. Fractures of the scapula. Acta Chir Orthop Traumatol Cech. 2011;78(4):297–304. [PubMed] [Google Scholar]
- 2.Lantry JM, Roberts CS, Giannoudis PV. Operative treatment of scapular fractures: a systematic review. Injury. 2008;39(3):271–83. [DOI] [PubMed] [Google Scholar]
- 3.ter Meulen DP, Janssen SJ, Hageman MG, Ring DC. Quantitative three-dimensional computed tomography analysis of glenoid fracture patterns according to the AO/OTA classification. J Shoulder Elb Surg. 2016;25(2):269–75. [DOI] [PubMed] [Google Scholar]
- 4.Ideberg R, Grevsten S, Larsson S. Epidemiology of scapular fractures. Incidence and classification of 338 fractures. Acta Orthop Scand. 1995;66(5):395–7. [DOI] [PubMed] [Google Scholar]
- 5.Kavanagh BF, Bradway JK, Cofield RH. Open reduction and internal fixation of displaced intra-articular fractures of the glenoid fossa. J Bone Joint Surgery-american Volume. 1993;75(4):479–84. [DOI] [PubMed] [Google Scholar]
- 6.Meng M, Dongning H, Kaixing Y, Jinming Z, Qiang H, Xieyuan J. Treatment of scapular glenoid fractures via the modified Judet approach. Chin J Orthop Trauma. 2021;23(11):4. [Google Scholar]
- 7.Jehan S, Baig NMA, Tavitian JD. Treatment of shoulder dislocation with greater tuberosity and glenoid fractures. J Coll Physicians Surg Pak. 2016;26:997. [PubMed] [Google Scholar]
- 8.Yong X, Yan ZZG, Guojin H, Jian D, Dankai W, Yun T. An axillary approach for open reduction and internal fixation to treat anterior glenoid fracture: an anatomical and clinical study. Chin J Orthop. 2022;42(1):8. [Google Scholar]
- 9.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 1987(214):160–4. [PubMed]
- 10.Goss DA Jr, Persinger F, Triplet JJ, Taylor BC, Long N. Arthroscopically assisted reduction and internal fixation of a displaced posterior glenoid fracture: a case report. JBJS Case Connect. 2017;7(4):e84. [DOI] [PubMed] [Google Scholar]
- 11.Papadonikolakis A. Arthroscopic reduction and fixation of transverse intra-articular glenoid fractures with scapular extension. Arthrosc Techniques. 2017;6(3):e879–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Voleti PB, Camp CL, Sinatro AL, Dines JS. Arthroscopic fixation of glenoid rim fractures after reduction by labral repair. Arthrosc Techniques. 2016;5(2):e379–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tucker A, Donnelly K, Murphy L, Ferguson G, Sloan S, Charlwood P. Percutaneous arthroscopic-assisted glenoid fixation: a novel surgical technique. J Orthop Case Rep. 2018;8(4):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Park JK, Jeong HS. Clinical and radiologic outcomes of Open reduction and internal fixation without capsular incision for Inferior Glenoid Fossa fractures. Clin Orthop Surg. 2023;15(2):175–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jehan S, Akhi Baig NM, Tavitian J. Treatment of shoulder dislocation with Greater Tuberosity and Glenoid fractures. J Coll Physicians Surg Pak. 2016;26(12):997–9. [PubMed] [Google Scholar]
- 16.Uzel AP, Laflamme GY. [Fracture of the glenoid cavity Goss-Ideberg type II with inferior dislocation of the shoulder]. Chir Main. 2009;28(4):260–4. [DOI] [PubMed] [Google Scholar]
- 17.Ziyan Z, Yong X, Jian D, Hua C, Yan G, Baichuan H, Chuangang P, Guangkai R, Dankai W, Yun T. Posterior axillary approach for treatment of some scapular fractures. Chin J Orthop Trauma. 2022;24(5):7. [Google Scholar]
- 18.Ding H, Bao YG, Yin B, Chang QH, Zai QS, Shi Q, Hu HJ, Wang HB, Zhao YF, Song FQ, et al. Efficacy analysis of axillary approach in the treatment of Ideberg type I and II scapular glenoid fractures: Case series. Med (Baltim). 2023;102(28):e34333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ye L, Huang H, Zhou F, Wan W, Jiang G, Y G, Zhang K. Applied anatomy of the scapula for internal fixation. Chin J Clin Anat. 2004;22(5):3. [Google Scholar]
- 20.Lee HJ, Kim BK, Ryu HS, Dan J. Vertical Interfragmentary doubled suture for displaced Patella fractures: sequential compressive tightening with nice knot. Clin Orthop Surg. 2020;12(3):413–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu G, Chen YQ, Chen CY, Lin ZX, Xie QY, Ye JJ, Xie Y. Clinical outcomes of doubled-suture nice knot augmented plate fixation in the treatment of comminuted midshaft clavicle fracture. BMC Surg. 2021;21(1):270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fan XL, Wang J, Zhang DH, Mao F, Liao Y. The Use of Nice knots Cerclage to Aid reduction and fixation of Metacarpal fractures. Plast Reconstr Surg. 2021;148(2):e338–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.