Abstract
There are no nationwide surveys on antihypertensive drugs in China. In order to assess the current status of antihypertensive drug therapy in patients with hypertension and analyzed factors that may affect combination therapy, using convenience sampling, we recruited 305,624 patients with hypertension from the Chinese Cardiovascular Association Database‐Hypertension Center between January 2019 and December 2021. Chi‐squared test was performed to analyze the administered antihypertensive drug types and their combinations in different hospital settings. Logistic regression was used to assess the factors influencing combination therapy. We found around 33.1% of the participants had stage 2 and above hypertension, of which 67.9% were treated with combination therapy. In community or general hospitals, the most common monotherapy was calcium channel blockers (CCB), angiotensin‐converting enzyme inhibitor/angiotensin II receptor inhibitor (ACEI/ARB) and diuretic were the main single‐pill combinations (SPCs), and ACEI/ARB and CCB were the main free combination. From 2019 to 2021, the rates of combination therapy increased (58.8%–64.1%) with SPCs from 25.9% to 31.0% and free combination from 31.9% to 32.6%. Patients aged < 60 years, with stage 2 and above hypertension, with an education level of high school and above, visiting general hospitals, living in the eastern region of China, with hypertension risk factors and comorbidities, and without anxiety or depression were more likely to receive combination therapy (all P < .05). The combination therapy use rate increased yearly and the rate of SPCs rose obviously. Individual, hospital, and regional differences in patients with hypertension influenced combination therapy.
Keywords: free combination, hypertension, monotherapy, single‐pill combinations
1. INTRODUCTION
Hypertension is associated with the occurrence and development of various cardiovascular diseases. 1 Studies have shown that for every 20 mmHg increase in systolic blood pressure (SBP) or 10 mmHg increase in diastolic blood pressure (DBP) the risk of cardiovascular and cerebrovascular diseases doubles. 2 , 3 Hypertension is a prevalent condition, with an incidence of 27.9% in China between 2012 and 2015. It is associated with high disability and mortality rates. However, a national survey in China revealed low awareness levels of hypertension, a treatment rate of less than 50%, and a control rate of less than 17%. 1
The timely administration of appropriate treatment can prevent or delay the occurrence of hypertension‐related complications. Some studies have suggested that monotherapy effectively lowers blood pressure (BP) in only a subset of patients with hypertension, with the remainder requiring combination therapy. 4 , 5 , 6 However, combination therapy is not routinely administered in China, resulting in a low control rate of hypertension. 7 To standardize the diagnosis, treatment, and management of hypertension and improve the BP control rate in patients, the Chinese Cardiovascular Association (CCA) Database‐Hypertension Center collected data from multiple centers regarding the administration of antihypertensives and personal characteristics of patients with hypertension. This study aimed to analyze the choice of antihypertensive drug therapy, particularly combination therapy to provide suggestions for the selection of antihypertensive drugs for patients with hypertension in China.
2. METHODS
2.1. Data source and study population
The aim of establishing the CCA Databases–Hypertension Center was to bridge the gap between general hospitals and community hospitals. General hospitals are usually the lead hospitals and need to establish cooperation systems with at least three community hospitals (also known as satellite hospitals), including joint consultation and referral systems for patients with hypertension. To be identified as a lead hospital, a hospital needs to meet the following conditions: (1) cardiovascular internal medicine is a dominant discipline in the region, and it can provide other medical institutions in the region with diagnosis and treatment of complex cases and continuing education; (2) the hospital establish an information sharing platform with three or more surrounding satellite hospitals; (3) the hospital is equipped with at least one intelligent sphygmomanometer that can transmit BP data in real‐time; (4) the hospital has basic laboratory and imaging examination conditions; (5) the hospital has an available hypertension clinic and ward; (6) the hospital has available educational facilities. To be identified as a satellite hospital, a hospital needs to meet the following conditions: (1) the team of internal medicine physicians has the ability to diagnose and treat mild hypertension; (2) the hospital is equipped with at least one intelligent sphygmomanometer that can transmit BP data in real‐time; (3) the hospital has available educational facilities. According to the CCA requirements, a lead hospital and all satellite hospitals that associated with the lead hospital have a combined population of not less than 500, and the number of patients in a satellite hospital must not be less than 100.
Data were collected from the CCA Database‐Hypertension Center by staff having a medical background. Using convenience sampling, patients with hypertension included in the database between January 1, 2019 and December 31, 2021, were selected as the study population. Data on patient demographics (age, sex, height, weight, body mass index [BMI], ethnic group, education level, and place of residence) and clinical characteristics (hospital attended, BP at clinical visit, clinical visit date, risk factors, hypertension course, comorbidities, psychological status, and antihypertensive medication) were collected.
2.2. BP measurements, diagnostic criteria, and definitions
The automatic sphygmomanometer validated according to standardized conditions and protocols was preferred. BP was measured sequentially in both upper arms, using an appropriate cuff size for the arm circumference by a trained physician or nurse, after the patient had sat still for five min in the hospital outpatient room. The upper arm with the highest BP was defined as the measurement arm and BP was measured three times in that arm. The average of the last two measurements was calculated every day. However, if the difference between the two SBP or DBP measurements was over 10 mmHg, another measurement was made, and the average of the last two was calculated. 6 , 8 On three consecutive days, the same doctor or nurse repeat above steps of BP measurement, and only the last 2 days of BP values were recorded.
The types and names of antihypertensive drugs were consistent with those of the Joint National Committee and Chinese definitions. 7 , 9 Hypertension was diagnosed in patients with an SBP of at least 140 mmHg or a DBP of at least 90 mmHg in the absence of antihypertensive medications, and in patients with a history of hypertension and receiving antihypertensive medications, regardless of their BP measurements. 8 Clinical visit date was defined as the first visit day to the current lead or satellite hospital. Patients with hypertension were classified according to their office BP at the clinical visit: below stage 2 hypertension (SBP < 160 mmHg and/or DBP < 100 mmHg) and; stage 2 and above hypertension (SBP ≥160 mmHg and/or DBP ≥100 mmHg). Controlled hypertension was defined as an average SBP of < 140 mmHg and an average DBP of < 90 mmHg in people with hypertension; patients not meeting these criteria were considered as uncontrolled hypertension.
Monotherapy was defined as the use of only one type of antihypertensive drug, whereas combination therapy was defined as the use of two or more antihypertensive pills (free combination) or any type of single‐pill combination (SPC), which includes only a SPC and SPC with other antihypertensive drugs. BMI was calculated as weight (kg) divided by the squared value of height (m2); a BMI ≥28.0 was considered to indicate obesity. 10 Participants who smoked > 400 cigarettes previously and smoked at the time of the examination were classified as current smoking. 11 People who drank three or more drinks per day and drank at the time of the examination were defined as current drinking. 12 Diabetes was diagnosed as glycosylated hemoglobin A1c≥6.5%, previous diagnosis of diabetes and/or chronic hypoglycemic drug usage. 13 Coronary lumen diameter stenosis ≥50% in the main artery or its major branches confirmed by angiography, computed tomography angiography or magnetic resonance imaging was diagnosed as coronary heart disease (CHD). 14 Patients filled out questionnaires of Patient Health Questionnaire‐9 (PHQ‐9) and 7‐item generalized anxiety disorder score (GAD‐7). Depression was diagnosed when PHQ‐9≥5 scores and anxiety was diagnosed when GAD‐7≥5 scores. 15 , 16 Grading details are provided in Supplemental Digital Content 1.
2.3. Statistical analyses
SPSS software (version 26.0; IBM Corporation, Armonk, NY) was used for database management and statistical analyses. Categorical variables are expressed as constituent ratios or rates, and continuous variables are expressed as mean ± standard deviation. We compared the characteristics of the patients in the controlled hypertension group and uncontrolled hypertension group using the Chi‐squared test for categorical variables and Student's t‐test for continuous variables. Chi‐squared test to was used analyze monotherapy and combination therapy in community and general hospitals. Multiple comparative analyses of the monotherapy, free combination, and SPC group were made using Bonferroni's correction. Multivariate logistic regression analysis was used to analyze the factors influencing combination therapy. The significance level α was equal to 0.05, and two‐sided P‐value < .05 was considered as statistically significant.
3. RESULTS
3.1. Patient characteristics
In this study, a total of 1409 hospitals participated in the accreditation between January 2019 and December 2021 from 34 provinces in China, including 310 lead hospitals and 1099 satellite hospitals. An average of 217 patients were enrolled in each hospital (least number in Deqing County Wukang town community hospital, n = 100, and highest number in Lanzhou First People's Hospital, n = 3,967).
A total of 356,783 patients with hypertension were included in the database between January 2019 and December 2021 along with the required information. The exclusion criteria were patients: (1) aged < 18 years, > 100 years, or no age provided (n = 733); (2) height < 140 cm, > 200 cm, or no height provided (n = 494); (3) weight < 40 kg, > 120 kg, or no weight provided (n = 795); (4) education information missing (n = 609); (5) geographical region information missing (n = 803); (6) SBP ≤60 mmHg, ≥250 mmHg, or information missing (n = 330); (7) DBP ≤40 mmHg, ≥180 mmHg, or information missing (n = 250); and (8) no antihypertensive drug treatment (about 47,145 cases in total, including 40,116 patients who refused to administer antihypertensive drugs, and 7,029 patients who were reluctant to answer). A total of 305,624 patients were included in the study, which involved 1,409 hospitals in 34 provinces in China. The Ethics Committee of the National Center for Institute of Geriatric Medicine, Chinese Academy of Medical Sciences/Beijing Hospital approved our study protocol.
The characteristics of the 305,624 study participants are summarized in Table 1. The participants had an average age of 64.7 ± 12.5 years and an average office BP of 147/86 mmHg. Among the participants, 52.7% (n = 161,177) were males, 28.4% (n = 86,658) attended community hospitals, 50.2% (n = 153,434) lived in the east of China, 61.9% (n = 189,137) had uncontrolled hypertension and 33.1% (n = 101,219) had stage 2 and above hypertension.
TABLE 1.
Characteristics of patients with hypertension.
| Analyzed parameter | Controlled hypertension (n = 116,487) | Uncontrolled hypertension (n = 189,137) | Total (n = 305,624) | P‐value |
|---|---|---|---|---|
| Age, years (mean ± SD) | 65.6 ± 11.6 | 64.1 ± 13.0 | 64.7 ± 12.5 | <.001 |
| Sex | <.001 | |||
| Male | 61,072 (52.4) | 100,105 (52.9) | 161,177 (52.7) | |
| Female | 55,415 (47.6) | 89,032 (47.1) | 144,447 (47.3) | |
| Duration of hypertension (years) | <0.001 | |||
| 1−10 | 44,124 (37.9) | 69,673 (36.8) | 113,797 (37.2) | |
| 11−20 | 43,025 (36.9) | 58,145 (30.8) | 101,170 (33.1) | |
| >20 | 12,873 (11.1) | 20,089 (10.6) | 32,962 (10.8) | |
| Unknown a | 16,465 (14.1) | 41,230 (21.8) | 57,695 (18.9) | |
| Level of hospital at clinical diagnosis | <.001 | |||
| Community | 43,495 (37.3) | 43,163 (22.8) | 86,658 (28.4) | |
| General | 72,992 (62.7) | 145,974 (77.2) | 218,966 (71.6) | |
| Geographical region of China | <0.001 | |||
| Eastern | 64,211 (55.2) | 89,223 (47.2) | 153,434 (50.2) | |
| Central | 27,896 (23.9) | 57,773 (30.5) | 85,669 (28.0) | |
| Western | 24,380 (20.9) | 42,141 (22.3) | 66,521 (21.8) | |
| Ethnicity | <.001 | |||
| Han | 112,276 (96.4) | 180,101 (95.2) | 292,377 (95.7) | |
| Non‐Han | 4,211 (3.6) | 9,036 (4.8) | 13,247 (4.3) | |
| Education | <.001 | |||
| Primary school and below | 55,033 (47.2) | 98,638 (52.1) | 153,671 (50.3) | |
| Middle school | 29,953 (25.7) | 45,246 (23.9) | 75,199 (24.6) | |
| High school | 19,663 (16.9) | 27,355 (14.5) | 47,018 (15.4) | |
| College and above | 11,838 (10.2) | 17,898 (9.5) | 29,736 (9.7) | |
| Risk factors | ||||
| Current smoking | 16,935 (14.5) | 28,730 (15.2) | 45,665 (14.9) | <.001 |
| Current drinking | 17,172 (14.7) | 31,059 (16.4) | 48,231 (15.8) | <.001 |
| Obesity | 17,237 (14.8) | 32,141 (17.0) | 49,378 (16.2) | <.001 |
| Comorbidities | ||||
| Diabetes | 22,436 (19.3) | 32,485 (17.2) | 54,921 (18.0) | <.001 |
| CHD | 29,590 (25.4) | 43,095 (22.8) | 72,685 (23.8) | <.001 |
| Stroke | 11,141 (9.6) | 20,952 (11.1) | 32,093 (10.5) | <.001 |
| Drug therapy | <.001 | |||
| Monotherapy | 49,039 (42.1) | 70,348 (37.2) | 119,387 (39.1) | |
| Free combination | 36,312 (31.2) | 63,635 (33.6) | 99,947 (32.7) | |
| Single‐pill combinations | 31,136 (26.7) | 55,154 (29.2) | 86,290 (28.2) | |
| Antihypertensive medication history | <.001 | |||
| Previously used | 85,512 (73.4) | 118,913 (62.9) | 204,425 (66.9) | |
| Have not used before a | 16,081 (13.8) | 31,419 (16.6) | 47,500 (15.5) | |
| Unknown b | 14,894 (12.8) | 38,805 (20.5) | 53,699 (17.6) | |
| Psychological factors c | <.001 | |||
| Health | 100,839 (86.6) | 158,156 (83.6) | 258,995 (84.7) | |
| Anxiety | 13,939 (12.0) | 27,897 (14.7) | 41,836 (13.7) | |
| Depression | 995 (0.9) | 2,025 (1.1) | 3,020 (1.0) | |
| Anxiety and depression | 714 (0.5) | 1,059 (0.6) | 1,773 (0.6) |
Unless stated otherwise, data are presented as number (percentage).
Abbreviations: SD, standard deviation; CHD, coronary heart disease.
“haven't used before” refers to patients with hypertension who never used antihypertensive drugs before but started to take such drugs at this clinical visit.
Patients did not know or did not wish to answer.
The psychological rating scale is described in supplemental digital content 1.
Compared to the participants with controlled hypertension, participants with uncontrolled hypertension were more likely to visit general hospitals, live in the central and western regions of China, have lower educational status, current smoking, current drinking, receive combination therapy, have not used antihypertensive drugs before and have a history of obesity, stroke, anxiety, and depression. Participants with controlled hypertension were more likely to be older, have a longer duration of hypertension, and have a history of diabetes and CHD, compared with participants with uncontrolled hypertension.
3.2. Antihypertensive drugs
Of the 305,624 patients with hypertension, 119,387 (39.1%) received monotherapy with a percentage decrease from 41.2% in 2019–35.9% in 2021, and 186,237 (60.9%) received combination therapy with a percentage increase from 58.8% in 2019–64.1% in 2021 (P < .001). About 40.4%∼44.4% of the patients with controlled hypertension received monotherapy and 30.9%∼31.6% of patients were treated with free combination during 2019–2021 as shown in Figure 1A. The percentage of SPCs jumped from 24.7% in 2019–27.3% in 2021 (P < .001). Monotherapy and combination therapy in uncontrolled hypertension patients over the 3 years of this study are shown in Figure 1B. The percentage of SPCs had gone up the most, which increased from 26.6% in 2019–33.1% in 2021. However, the decline in the percentage of monotherapy from 38.6% to 33.4% over 3 years for patients with uncontrolled hypertension more obviously than that for the patients with controlled hypertension (from 44.4% to 41.8%) over the same period (P < .001).
FIGURE 1.
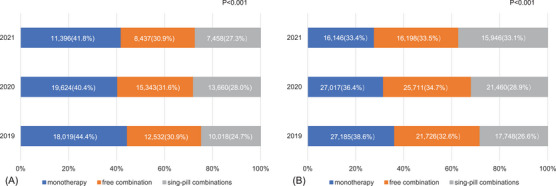
Percentage of monotherapy, free combination and single‐pill combinations in patients with controlled hypertension (A) and uncontrolled hypertension (B) in 2019−2021. Multiple comparative analyses of the monotherapy, free combination, and single‐pill combination groups were performed in (A) and (B), and the P‐value of Bonferroni's correction was .0167. For patients with controlled hypertension, the pairwise comparison of 3 years in the monotherapy group was statistically significant (P < .0167); the comparisons between 2020 and 2019, and 2021 and 2019 in single‐pill combinations group were statistically significant (all P < .0167), but the comparison between 2020 and 2019 was not significant (P > .0167). The pairwise comparison of 3 years in the free combination group was not statistically significant (P > .0167). The P‐values were all less than .0167 after pairwise comparisons among the three groups in (B).
The specific antihypertensive drugs used are shown in Table 2. Calcium channel blocker (CCB), administered to 53.8% (n = 64,226) of the patients receiving monotherapy, was the most commonly used monotherapy, followed by angiotensin II receptor blocker (ARB) and angiotensin‐converting enzyme inhibitor (ACEI), which was given to 24.8% (n = 29,559) and 10.1% (n = 12,082) of the patients, respectively.
TABLE 2.
Types of antihypertensive drugs used in patients with hypertension in different hospitals.
| Drug therapy | Community hospitals | General hospitals | Total | P‐value |
|---|---|---|---|---|
| Monotherapy | <.001 | |||
| CCB | 26,500 (58.6) | 37,726 (50.9) | 64,226 (53.8) | |
| ARB | 11,769 (26.0) | 17,790 (24.0) | 29,559 (24.8) | |
| ACEI | 3,783 (8.4) | 8,299 (11.2) | 12,082 (10.1) | |
| BB | 1,614 (3.6) | 8,594 (11.6) | 10,208 (8.6) | |
| Diuretic | 1,588 (3.4) | 1,724 (2.3) | 3,312 (2.7) | |
| Total | 45,254 (37.9) | 74,133 (62.1) | 119,387 (100.0) | |
| Combination therapy | <.001 | |||
| Free combination | ||||
| A+C | 10,718 (25.9) | 25,692 (17.7) | 36,410 (19.6) | |
| A+B | 1,690 (4.1) | 13,887 (9.6) | 15,577 (8.4) | |
| B+C | 2,656 (6.4) | 11,032 (7.6) | 13,688 (7.3) | |
| C+D | 725 (1.8) | 1,685 (1.2) | 2,410 (1.3) | |
| A+D | 642 (1.6) | 1,690 (1.2) | 2,332 (1.3) | |
| B+D | 143 (0.4) | 1,432 (1.0) | 1,575 (0.8) | |
| Other two | 540 (1.3) | 2,358 (1.6) | 2,898 (1.6) | |
| A+B+C | 1,336 (3.2) | 10,890 (7.5) | 12,226 (6.6) | |
| A+C+D | 508 (1.2) | 2,477 (1.7) | 2,985 (1.6) | |
| A+B+D | 121 (0.3) | 1,852 (1.3) | 1,973 (1.1) | |
| B+C+D | 102 (0.2) | 1,000 (0.7) | 1,102 (0.6) | |
| Other three | 153 (0.4) | 2,580 (1.8) | 2,733 (1.5) | |
| A+B+C+D | 83 (0.2) | 1,706 (1.2) | 1,789 (1.0) | |
| Other four | 97 (0.2) | 2,250 (1.6) | 2,347 (1.3) | |
| Five and above | 12 (0.1) | 654 (0.5) | 666 (0.4) | |
| SPCs | ||||
| A+D a | 15,130 (36.6) | 39,491 (27.3) | 54,621 (29.3) | |
| A+C b | 3,319 (8.0) | 23,004 (15.9) | 26,323 (14.1) | |
| Other SPCs | 3,429 (8.1) | 1,153 (0.6) | 4,582 (2.2) | |
| Total | 41,404 (22.2) | 144,833 (77.8) | 186,237 (100.0) |
Abbreviations: A, ACEI/ARB; B, BB; C, CCB; D, diuretic. A+D; ACEI, angiotensin‐converting enzyme inhibitor; ARB, angiotensin II receptor inhibitor; BB, beta‐blocker; CCB, calcium channel blockers; SPC, single‐pill combination.
Represents the SPC composed of ACEIs/ARBs and diuretics, and A+C.
Indicates the SPC composed of ACEIs/ARBs and CCB.
Beta‐blocker (BB) were used in 8.6% (n = 10,208) of the patients with hypertension receiving monotherapy, 41.7% (n = 4,259) of them had CHD. BB was administered to 3.6% (n = 1,614) and 11.6% (n = 8,594) of the patients with hypertension in community and general hospitals, respectively. Of the patients receiving BB in community and general hospitals, 19.3% (n = 312) and 45.9% (n = 3,947), respectively, had CHD.
A total of 186,237 patients were treated with combinations of antihypertensive drugs, of whom 54.1% (100,711) used free combinations and 45.9% (85,526) used SPCs. Of 85,526 patients using SPCs, 52.3% (44,740) were on SPC and also on other types of antihypertensive drugs. The most common free combination was ACEI/ARB (A)+CCB (C), which was taken by 35.7% (n = 36,410) of the patients receiving this drug therapy, followed by A+BB (B) (15.6%, n = 15,577) and B+C (13.7%, n = 13,688). The most frequently used SPC was A+diuretic (D), which was taken by 63.3% (n = 54,621) of patients receiving this therapy, followed by A+C (30.5%, n = 26,323). In most compositions of free combination and SPCs, ARB accounted for a larger proportion than ACEI. The usage rates of SPCs in community and general hospitals were 25.7%(n = 22,259) and 29.2%(n = 64,031), respectively.
CCB was the most commonly used monotherapy in patients with diabetes (n = 54,921), CHD (n = 72,685) and stroke (n = 32,093), followed by ARB. In patients with CHD, A+B and A+D were the most commonly used free combination and SPCs, respectively. In patients with diabetes and stroke, A+C was the most commonly used free combination and A+D was the most commonly used SPCs.
3.3. Factors associated with combination therapy
Forward binary logistic regression analysis was used to analyze 15 variables: age, sex, region, education level, hospital types, hypertension stage, risk factors for hypertension, comorbidities, and psychological factors.
The male patients aged < 60 years with stage 2 and above hypertension, an education level of high school and above, and visiting general hospitals were more likely to receive combination therapy (Figure 2). Patients with hypertension in the eastern region of China were more likely to receive combination therapy than those in the central and western regions. Patients with risk factors for hypertension, CHD, diabetes, and no anxiety or depression were more likely to receive combination therapy.
FIGURE 2.
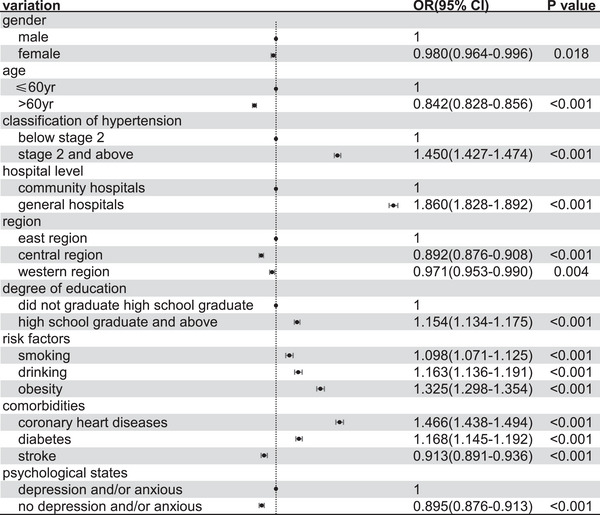
Factors that may influence the combination therapy. CI, confidence interval; OR, odds ratio.
4. DISCUSSION
A total of 305,624 patients with hypertension from more than 1,400 hospitals in China were included in this study. About 60.9% of these patients were treated with a combination of antihypertensive drugs. CCB was the most common monotherapy, A+C was the most common free combination, and A+D was the most common SPC. Among these, the use of SPCs has significantly increased over the 3 years.
The pathogenesis of hypertension is complex. Patients with significantly elevated BP, target organ damage, and clinical comorbidities require combination therapy. Previous studies have shown that more than 70% of patients with hypertension require combination therapy to effectively control BP. 17 , 18 In this study, similar proportions of patients received free combination and SPCs. A+C was the main type of free combination administered in community and general hospitals, which is consistent with the 2020 International Society of Hypertension guidelines. 19 A+D was the predominant SPCs used in community and general hospitals, which may be related to the drug availability in China. SPCs are recommended for combination therapy in the hypertension guidelines worldwide because of their efficacy and notable high compliance rates. 4 , 5 , 6 , 7 Thiazide diuretics, which are components of most SPCs, are recommended as first‐line antihypertensive drugs by the international guidelines. 20 , 21 The selection of A+C or A+D should be determined on a case‐by‐case basis after considering the clinical characteristics of each patient.
CCB, the most commonly used monotherapy in two hospital classes, is suitable for use in Asian populations because of its wide indications, good antihypertensive effects, and lack of absolute contraindications. 22 In this study, ARB was the second most popular monotherapy. ARB is related to target organ protection in patients with hypertension, thus, it is typically the first choice for patients with diabetes and CHD. 23 BB can inhibit sympathetic nerve activity and slow the heart rate, and is therefore suitable for patients with sympathetic nerve excitation. Due to a lack of evidence and the influence of international guidelines, only 6.4% of patients without comorbidities received BB monotherapy. The proportion of BB use in general hospitals was significantly higher than that in community hospitals, which may be related to the higher proportion of patients with CHD in general hospitals. Previous randomized controlled trials revealed that the low heart rate was associated with the occurrence of adverse cardiovascular events in older patients with hypertension, 24 which limits the use of BB in this population.
In our study, approximately 80% of the patients with hypertension, diabetes, and CHD were being treated with antihypertensive drugs at the time of the clinical consultation, and therefore had normal BP at that time. The hospital grade was related to the choice of antihypertensive drugs. The higher the hospital, the higher the proportion of combination treatment, which was related to hypertension severity and drug resource allocation. It is more challenging to control BP in patients who smoke, drink alcohol, and are obese. 25 , 26 , 27 Therefore, the proportion of combination therapy was higher in these patients. In addition, patients with comorbidities were more likely to choose combination therapy than others, which might be related to the difficulty in controlling BP in these patients and the lower BP target blood set. 28 , 29 Although a high proportion of patients with stroke had uncontrolled hypertension, the target BP was higher in these patients than that of the general population, which may explain the small proportion of these patients receiving combination therapy. 30 Patients with higher education levels were more likely to accept combination drug therapy, indicating that educational background could affect the choice of antihypertensive drugs. 31 , 32
Overall, the selection of antihypertensive drugs in this study was consistent with the recommendations of national and international guidelines. 4 , 5 , 6 , 7 However, certain matters require further investigation. First, the use of ACEIs was much lower than that of ARBs. Many studies have suggested that ACEI and ARB have similar antihypertensive effects, 33 , 34 , 35 but evidence suggests that ACEI can significantly reduce the risk of adverse cardiovascular events. 36 Accordingly, ACEI should be the first choice of treatment for patients with hypertension who can tolerate these drugs. Second, most patients with hypertension and diabetes received CCB monotherapy, which differed slightly from the recommendations of the guidelines. This may be related to the good tolerance of CCB and their widespread use in primary medical institutions. Third, the application of SPCs in community hospitals remains insufficient, which may be related to drug availability, regional differences, and economic conditions. Therefore, the use of SPCs requires further promotion in these settings. Fourth, SPCs were mainly limited to A+D and A+C, which are indicated for patients with comorbidities, suggesting that the variety of SPCs available in China is insufficient. Thus, there is scope for improvement in terms of selection of the appropriate antihypertensive drug in China.
This study has few limitations. First, factors that may affect the choice of antihypertensive drugs, such as income, occupation, and patient medication compliance, were not analyzed. Second, lifestyle interventions are important aspects of antihypertensive treatment; the effects of this factor on BP were not considered in this study. Although none of the enrolled patients were infected with the novel coronavirus, but quarantine, low physical activity, poor diet, and psychological stress may raise the incidence of hypertension. Some patients with well‐controlled BP may need intensive antihypertensive therapy. 37 Third, less commonly used antihypertensive medications, such as alpha‐blockers and angiotensin receptor neprilysin inhibitors, were not included in this study, which may have resulted in selection bias. Fourth, although convenience samples are easy and economical to acquire, the extent to which one can generalize the results from the patients in a convenience sample to others in the population is limited. 38
The novelty of this study is that it is the first to analyze the use of antihypertensive drugs in community and general hospitals in China. The proportions of patients treated with monotherapy, free combination, and SPCs were compared in detail and the rationality of antihypertensive drug use was analyzed. This study findings suggest that improvements are needed to conform to the current guidelines and optimize patient care.
5. CONCLUSIONS
In conclusion, the rate of combination therapy increased every year, and the rate of SPCs rose obviously in China from 2019 to 2021, especially for uncontrolled hypertension patients. For patients with or without comorbidities, the selection of antihypertensive drugs was roughly consistent with the recommendations of international guidelines. However, SPCs in community hospitals were still relatively insufficient, and for some patients with hypertension combined with diabetes, the first choice of antihypertensive drug was inconsistent with the guidelines. Finally, the individual, hospital and regional differences in patients with hypertension might influence combination therapy.
AUTHOR CONTRIBUTIONS
Wei Liu and Ningling Sun were the coordinators of the project and were responsible for the study implement and design. Material preparation, data collection was performed by Xiaoyang Luo, Peili Bo, Yuanyuan Chen, Qinghua Han, Nanfang Li, Xinzheng Lu, Jianjun Mou, Gang Sun and Yuqing Zhang. Data analysis was performed by Wei Liu and Xiaoyang Luo. The first draft of the manuscript was written by Xiaoyang Luo; Wei Liu, Ningling Sun and Xiaoyang Luo were all responsible for the revision of the manuscript. All authors contributed intellectually to this manuscript and approved the content of the manuscript.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
PATIENT CONSENT STATEMENT
Written informed consent was obtained from all participants before enrollment.
Supporting information
Supporting Information
Luo X, Liu W, Sun N, et al. The prevalence of monotherapy and combination therapy in hypertension in China from 2019 to 2021: A nationwide population‐based cross‐sectional study. J Clin Hypertens. 2024;26:1054–1062. 10.1111/jch.14870
Contributor Information
Wei Liu, Email: tgyliuw@163.com, Email: liuweibjyy@163.com.
Ningling Sun, Email: sunnl@263.net.
DATA AVAILABILITY STATEMENT
As the study materials were obtained from the CCA database in China, the data were confidential and not allowed to be opened in public. If there are any needs for clarification, the readers can contact the corresponding author for sharing the data.
REFERENCES
- 1. Wang Z, Chen Z, Zhang L, et al. Status of hypertension in china: results from the china hypertension survey, 2012–2015. Circulation. 2018;137(22):2344‐2356. [DOI] [PubMed] [Google Scholar]
- 2. Lewington S, Clarke R, Qizilbash N, et al. Age‐specific relevance of usual blood pressure to vascular mortality: a meta‐analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903‐1913. [DOI] [PubMed] [Google Scholar]
- 3. Fuchs FD, Whelton PK. High blood pressure and cardiovascular disease. Hypertension. 2020;75(2):285‐292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. WHO Guidelines Approved by the Guidelines Review Committee. Guideline for the pharmacological treatment of hypertension in adults; 2021. p. [Google Scholar]
- 5. Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021‐3104. [DOI] [PubMed] [Google Scholar]
- 6. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):e13‐e115. [DOI] [PubMed] [Google Scholar]
- 7. 2018 Chinese Guidelines for Prevention and Treatment of Hypertension‐A report of the revision committee of chinese guidelines for prevention and treatment of hypertension. J Geriatr Cardiol. 2019; 16(3): 182‐241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mancia G, Kreutz R, Brunström M, et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J Hypertens. 2023;41(12):1874‐2071. [DOI] [PubMed] [Google Scholar]
- 9. Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. Jama. 2003;289(19):2560‐2572. [DOI] [PubMed] [Google Scholar]
- 10. Pan XF, Wang L, Pan A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 2021;9(6):373‐392. [DOI] [PubMed] [Google Scholar]
- 11. Kamimura D, Cain LR, Mentz RJ, et al. Cigarette smoking and incident heart failure: insights from the Jackson heart study. Circulation. 2018;137(24):2572‐2582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mukamal KJ. The effects of smoking and drinking on cardiovascular disease and risk factors. Alcohol Res Health. 2006;29(3):199‐202. [PMC free article] [PubMed] [Google Scholar]
- 13. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014; 37(Suppl 1):S81‐90. [DOI] [PubMed] [Google Scholar]
- 14. Pyxaras SA, Wijns W, Reiber JHC, et al. Invasive assessment of coronary artery disease. J Nucl Cardiol. 2018;25(3):860‐871. [DOI] [PubMed] [Google Scholar]
- 15. Levis B, Benedetti A, Thombs BD. Accuracy of Patient Health Questionnaire‐9 (PHQ‐9) for screening to detect major depression: individual participant data meta‐analysis. Bmj. 2019;365(l):1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Toussaint A, Hüsing P, Gumz A, et al. Sensitivity to change and minimal clinically important difference of the 7‐item Generalized Anxiety Disorder Questionnaire (GAD‐7). J Affect Disord. 2020;265:395‐401. [DOI] [PubMed] [Google Scholar]
- 17. Egan BM, Bandyopadhyay D, Shaftman SR, et al. Initial monotherapy and combination therapy and hypertension control the first year. Hypertension. 2012;59(6):1124‐1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Brook RD, Kaciroti N, Bakris G, et al. Prior medications and the cardiovascular benefits from combination angiotensin‐converting enzyme inhibition plus calcium channel blockade among high‐risk hypertensive patients. J Am Heart Assoc. 2018;7(1):6‐19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension. 2020;75(6):1334‐1357. [DOI] [PubMed] [Google Scholar]
- 20. Blowey DL. Diuretics in the treatment of hypertension. Pediatr Nephrol. 2016;31(12):2223‐2233. [DOI] [PubMed] [Google Scholar]
- 21. Burnier M, Bakris G, Williams B. Redefining diuretics use in hypertension: why select a thiazide‐like diuretic? J Hypertens. 2019;37(8):1574‐1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Elliott WJ, Ram CV. Calcium channel blockers. J Clin Hypertens (Greenwich). 2011;13(9):687‐689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Li XC, Zhang J, Zhuo JL. The vasoprotective axes of the renin‐angiotensin system: physiological relevance and therapeutic implications in cardiovascular, hypertensive and kidney diseases. Pharmacol Res. 2017;125(Pt A):21‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Blood pressure‐lowering treatment based on cardiovascular risk: a meta‐analysis of individual patient data. Lancet. 2014; 384(9943): 591‐598. [DOI] [PubMed] [Google Scholar]
- 25. Roerecke M, Kaczorowski J, Tobe SW, et al. The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta‐analysis. Lancet Public Health. 2017;2(2):e108‐e120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dauchet L, Kesse‐Guyot E, Czernichow S, et al. Dietary patterns and blood pressure change over 5‐y follow‐up in the SU.VI.MAX cohort. Am J Clin Nutr. 2007;85(6):1650‐1656. [DOI] [PubMed] [Google Scholar]
- 27. van Oort S, Beulens JWJ, van Ballegooijen AJ, et al. Association of cardiovascular risk factors and lifestyle behaviors with hypertension: a Mendelian randomization study. Hypertension. 2020;76(6):1971‐1979. [DOI] [PubMed] [Google Scholar]
- 28. Rea F, Corrao G, Merlino L, et al. Initial antihypertensive treatment strategies and therapeutic inertia. Hypertension. 2018;72(4):846‐853. [DOI] [PubMed] [Google Scholar]
- 29. Karmali KN, Lloyd‐Jones DM, van der Leeuw J, et al. Blood pressure‐lowering treatment strategies based on cardiovascular risk versus blood pressure: a meta‐analysis of individual participant data. PLoS Med. 2018;15(3):e1002538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: a Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344‐e418. [DOI] [PubMed] [Google Scholar]
- 31. Iqbal A, Ahsan KZ, Jamil K, et al. Demographic, socioeconomic, and biological correlates of hypertension in an adult population: evidence from the Bangladesh demographic and health survey 2017–18. BMC Public Health. 2021;21(1):1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wang W, Zhang M, Xu CD, et al. Hypertension prevalence, awareness, treatment, and control and their associated socioeconomic factors in China: a spatial analysis of a national representative survey. Biomed Environ Sci. 2021;34(12):937‐951. [DOI] [PubMed] [Google Scholar]
- 33. Verdecchia P, Dagenais G, Healey J, et al. Blood pressure and other determinants of new‐onset atrial fibrillation in patients at high cardiovascular risk in the Ongoing Telmisartan Alone and in Combination With Ramipril Global Endpoint Trial/Telmisartan Randomized Assessment Study in ACE iNtolerant subjects with cardiovascular Disease studies. J Hypertens. 2012;30(5):1004‐1014. [DOI] [PubMed] [Google Scholar]
- 34. Suchard MA, Schuemie MJ, Krumholz HM, et al. Comprehensive comparative effectiveness and safety of first‐line antihypertensive drug classes: a systematic, multinational, large‐scale analysis. Lancet. 2019;394(10211):1816‐1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Abbasi J. Choose ARBs over ACE inhibitors for first‐line hypertension treatment, large new analysis suggests. Jama. 2021;326(13):1244‐1245. [DOI] [PubMed] [Google Scholar]
- 36. Li EC, Heran BS, Wright JM. Angiotensin converting enzyme (ACE) inhibitors versus angiotensin receptor blockers for primary hypertension. Cochrane Database Syst Rev. 2014;2014(8):Cd009096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Zhang V, Fisher M, Hou W, et al. Incidence of new‐onset hypertension post‐COVID‐19: comparison with influenza. Hypertension. 2023;80(10):2135‐2148. [DOI] [PubMed] [Google Scholar]
- 38. Gudmund R, Iversen MG. Statistics: The Conceptual Approach. Observational data: Problems and possibilities; 1997:36. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information
Data Availability Statement
As the study materials were obtained from the CCA database in China, the data were confidential and not allowed to be opened in public. If there are any needs for clarification, the readers can contact the corresponding author for sharing the data.


