Abstract
BACKGROUND
Spinal arachnoid cysts are cerebrospinal fluid–filled sacs that are frequently located within the thoracic spine and can lead to symptoms due to direct compression of the thoracic spinal cord. These lesions are typically treated with laminectomy and fenestration of the cyst, with or without shunting. However, with recurrence, treatment is often more complex and sometimes requires re-exposure and fenestration or shunting.
OBSERVATIONS
Here, the authors describe a 57-year-old female with a thoracic intradural arachnoid cyst that recurred despite extensive and initially successful fenestration. Given the failure of fenestration, the authors instead attempted to place a cystoperitoneal shunt. Given how extensive her laminectomy was, the authors elected to perform the procedure under ultrasonic guidance to avoid the large incision required for open shunt placement. The procedure was successful, with gradual improvement in the size of the arachnoid cyst as well as symptomatic improvement.
LESSONS
Here, the authors present a unique minimally invasive technique to treat recurrent spinal arachnoid cysts. They successfully demonstrated the feasibility and safety of this approach in shunting the cyst while avoiding the extensive re-exposure often required in such complex cases.
Keywords: arachnoid cyst, cystoperitoneal shunt, recurrent arachnoid cyst, ultrasound guidance
ABBREVIATIONS: MRI = magnetic resonance imaging, SAC = spinal arachnoid cyst.
Spinal arachnoid cysts (SACs) are cerebrospinal fluid–filled sacs found anywhere around the spine in the extradural, intradural, or intramedullary space.1–3 Although the pathophysiology is not well understood, they classically fall into either congenital or acquired lesions, with the latter typically occurring due to trauma, hemorrhage, infection, or past surgical procedures.1–3 Although they can be found anywhere along the spine, most are located in the thoracic region, with patients coming to medical attention due to back pain, radicular pain, or symptoms of spinal cord compression.1–3 Management of SACs can be challenging and often requires surgical intervention to decompress the spinal cord. This typically includes a laminectomy (or laminoplasty) followed by cyst fenestration or resection, with some surgeons also opting to shunt the cyst.4–9 Even with appropriate treatment, these lesions can potentially recur, which often requires careful repeat exposure of the previous durotomy and potential extension of the laminectomy.1, 9, 10 Another potential option after cyst recurrence is to shunt the cyst instead.1, 2 Shunt placement for SACs can involve placement under direct visualization, with shunting to the adjacent subarachnoid space or to other spaces in the form of a cystoperitoneal shunt or a cystopleural shunt.2, 10 Shunt insertion can also involve blind catheter placement, much like in a classic lumboperitoneal shunt.11 Other groups have also successfully treated a recurrence with a ventriculoperitoneal shunt.12 Here, we present the case of a 57-year-old female with a recurrent thoracic SAC that failed to respond to treatment via multilevel laminectomy and cyst fenestration.9 We decided to perform a cystoperitoneal shunting procedure. To avoid re-exposure of the previous laminectomy site, we chose a minimally invasive ultrasound-guided percutaneous approach for accessing the cyst, followed by the placement of a traditional cystoperitoneal shunt. To the best of our knowledge, there are no documented surgical descriptions on accessing SACs through a percutaneous ultrasound-guided approach in the literature. In this technical note, we aim to highlight the safety and feasibility of this minimally invasive technique for accessing SACs.
Illustrative Case
A 57-year-old female presented with a past medical history significant for incomplete paraplegia due to a previously treated intradural SAC after a T6–11 laminectomy with operative lysis of adhesions secondary to spontaneous spinal subarachnoid hemorrhage.9 At baseline, she used a wheelchair, with bilateral lower-extremity strength of 3–4/5 proximally and 1–3/5 distally. She presented to our clinic with concerns for worsening urinary incontinence, weakness, paresthesias, and increased mid-back pain with a new radicular component. Despite previous fenestration, a dorsal thoracic arachnoid cyst had re-developed (Fig. 1). Options were discussed with the patient, including continued observation and surgical interventions such as repeat open fenestration or cystoperitoneal shunting. Given her continued worsening symptoms, she was interested in operative intervention. In particular, she was interested in pursuing shunting via a cytoperitoneal shunt.
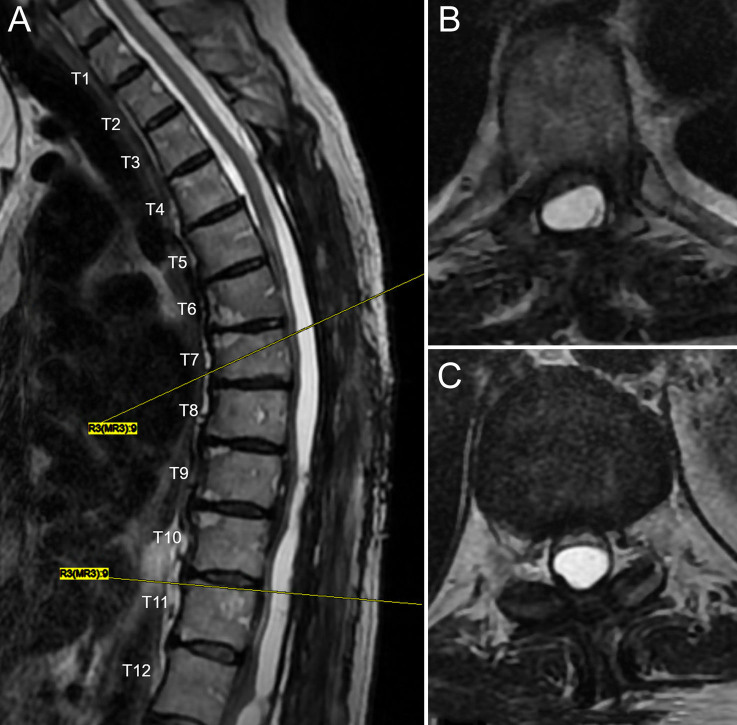
FIG. 1.
Preoperative T2-weighed MRI demonstrating a large dorsal arachnoid cyst causing ventral displacement of the spinal cord in the sagittal (A) and axial (B) planes at T6–7 and the axial plane (C) at T10–11.
The patient was placed prone on a Jackson table, and ultrasound was utilized to ensure the arachnoid cyst could be fully visualized. Her entire thoracolumbar spine was then prepped and draped in the typical fashion, including laterally to accommodate a passing incision. An ultrasound unit was draped in a typical sterile fashion and brought into the field. The dorsal arachnoid cyst could clearly be seen using ultrasound (Fig. 2A and B). Given how the arachnoid cyst could be clearly identified, we planned to place a catheter within the cyst using ultrasonic guidance. Using a 14-gauge Touhy needle, we entered the arachnoid cyst (Fig. 2C). There was a small amount of spontaneous flow of clear fluid under relatively low pressure. Further fluid was aspirated to confirm location, with minimal resistance to aspiration. A 4-Fr catheter was then threaded through the Touhy needle approximately 15 cm without resistance. The Touhy needle was then withdrawn, and spontaneous flow was observed from the catheter. Further localization was confirmed with ultrasound. A small incision was made around the catheter, and it was secured to the fascia. We then tunneled the catheter as far laterally as possible in the prone position and closed the midline incision and passing incision after temporarily tying off the catheter.
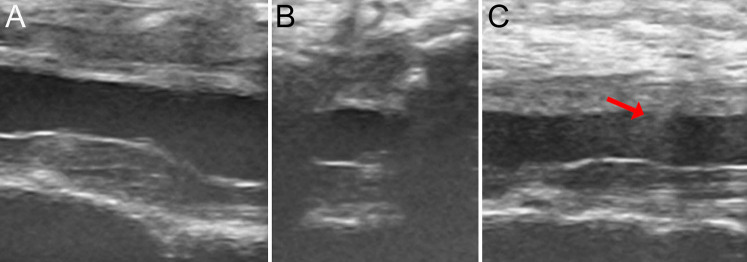
FIG. 2.
Intraoperative ultrasound images obtained during the procedure, demonstrating the enlarged dorsal arachnoid cyst from sagittal (A) and axial (B) views. The shadow from the needle entering the thecal sac is visible (C, red arrow) from a sagittal orientation.
The patient was then flipped supine, and her abdomen was prepped and draped in the typical fashion. The tunneling incision was reopened and enlarged to allow placement of a programmable shunt valve with siphon control (shunt valve set to 3, Codman Certas, Integra LifeSciences). A distal catheter was then tunneled, and the intra-abdominal component was placed under laparoscopic guidance. The patient awoke from anesthesia without complications with a stable neurological examination. Postoperative radiographs demonstrated the expected shunt position (Fig. 3), and the patient was discharged home on postoperative day 3.
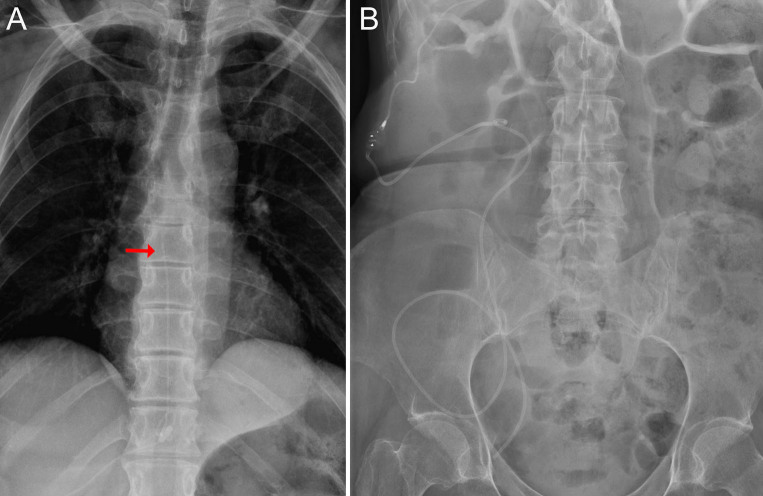
FIG. 3.
Postoperative radiographs confirming expected placement of the SAC to the peritoneal shunt. A: Anteroposterior thoracic spine radiograph demonstrating the proximal catheter within the thoracic spinal canal (red arrow). B: Kidney, ureter, and bladder radiograph demonstrating proximal catheter connection to the programmable shunt valve, followed by appropriate distal catheter placement within the peritoneum.
The patient was seen in the clinic approximately 1 month postoperatively with improvement in the size of the arachnoid cyst (Fig. 4). She has had subjective improvement in her symptoms and objective improvement when working with physical therapy. We plan to maintain the shunt at its current setting as she continues to work with therapy, with repeat imaging in the future to monitor the size of the arachnoid cyst.
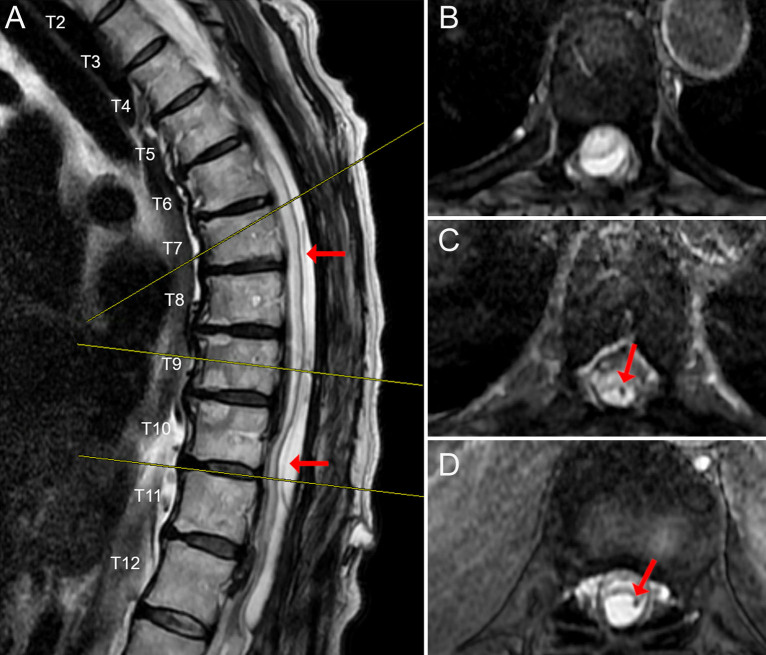
FIG. 4.
Postoperative T2-weighted MRI performed about 1 month postoperatively, demonstrating a decrease in the SAC as seen in the sagittal (A) and axial (B) planes at T6–7, T9 (C), and T10–11 (D). Red arrows highlight the catheter within the arachnoid cyst.
Informed Consent
The necessary informed consent was obtained in this study.
Discussion
Observations
Here, we present a 57-year-old female with a complex medical history, including spontaneous spinal subarachnoid hemorrhage complicated by a previously fenestrated thoracic arachnoid cyst,9 in whom an SAC recurred. She had significant neurological symptoms from thoracic spinal cord compression. Given the failure of the previous fenestration, we decided to attempt a different technique and performed cystoperitoneal shunting. Due to her previous surgery, we elected to perform a unique approach for shunt placement under ultrasonic guidance to avoid the potential complications of reopening her incision.
Traditional management of SACs often involves extensive surgical interventions, including multilevel laminectomies and cyst fenestration, which carry significant risks of morbidity and recurrence.1–3 Although recurrent SACs can be treated with reoperation,1, 9, 10 shunting could provide another option.1, 2 This case illustrates the successful use of a transcutaneous catheter for cyst drainage, a novel approach that potentially offers another option for the treatment of recurrent SACs in a less invasive manner.
A key aspect of this case is the careful preoperative planning and the use of advanced imaging techniques to accurately localize the cyst and guide the catheter placement. This precision is crucial in avoiding unnecessary tissue damage and ensuring effective cyst drainage. Comparatively, this case highlights several novel elements that add to the literature on SAC management. The use of ultrasound guidance for catheter placement into the arachnoid cyst is relatively uncommon but proved to be highly effective in this scenario. Although ultrasound is a well-established technique for lumbar puncture13 and cystoperitoneal shunting is an established technique for SACs,1, 2 the feasibility and safety of using ultrasound guidance for catheter placement in SAC have not been documented in the literature to date.
Although the technique of utilizing ultrasound to place a cystoperitoneal shunt works well in select patients, there are some potential limitations of this technique. If a patient does not already have a sufficiently wide laminectomy or if the laminectomies do not encompass enough levels, it may be difficult to visualize the needle tip and catheter entering the cyst. If the depth between the skin and the SAC is too long, it may also become difficult to safely visualize the needle entering the SAC. Another potential limitation would be a smaller SAC, which could be difficult to localize with ultrasound and difficult to get a sufficient catheter length into the SAC to ensure appropriate drainage. Lastly, intramedullary SACs would likely not be appropriate targets for this technique, as it would be difficult to ensure the passage of the needle through a safe corridor within the spinal cord.
Lessons
This case demonstrates a less invasive approach to the management of recurrent SACs. The primary takeaway is that with careful planning and the integration of advanced imaging and surgical techniques, it is possible to achieve effective cyst drainage with less invasive approaches. This approach mitigates the potential complications associated with reoperating via a previous spine and dural incision, including wound complications, infection, persistent cerebrospinal fluid leaks, and prolonged recovery time. We believe that this technique can serve as a viable alternative to more invasive surgeries for patients with recurrent SACs in which laminectomy and fenestration of the cyst have already failed.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: Treffy, DeGroot, Bakhaidar. Acquisition of data: Treffy, DeGroot, Bakhaidar, Rahman, Shabani. Analysis and interpretation of data: Treffy, DeGroot, Rahman. Drafting the article: Treffy, DeGroot, Palmer, Rahman, Shabani. Critically revising the article: Treffy, DeGroot, Bakhaidar, Palmer, Rahman. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript on behalf of all authors: Treffy. Administrative/technical/material support: DeGroot, Bakhaidar. Study supervision: DeGroot.
Correspondence
Randall W. Treffy: Medical College of Wisconsin, Milwaukee, WI. rtreffy@mcw.edu.
References
- 1.Wang YB, Wang DH, Deng SL. Symptomatic secondary spinal arachnoid cysts: a systematic review. Spine J. 2023;23(8):1199-1211. [DOI] [PubMed] [Google Scholar]
- 2.Kalsi P, Hejrati N, Charalampidis A, et al. Spinal arachnoid cysts: a case series & systematic review of the literature. Brain Spine. 2022;2:100904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garg K, Borkar SA, Kale SS, Sharma BS. Spinal arachnoid cysts—our experience and review of literature. Br J Neurosurg. 2017;31(2):172-178. [DOI] [PubMed] [Google Scholar]
- 4.Wang MY, Levi AD, Green BA. Intradural spinal arachnoid cysts in adults. Surg Neurol. 2003;60(1):49-56. [DOI] [PubMed] [Google Scholar]
- 5.Mohindra S, Gupta R, Bal A. Intra-dural spinal arachnoid cysts: a short series of 10 patients. Br J Neurosurg. 2010;24(6):679-683. [DOI] [PubMed] [Google Scholar]
- 6.Viswanathan VK, Manoharan SR, Do H, et al. Clinical and radiologic outcomes after fenestration and partial wall excision of idiopathic intradural spinal arachnoid cysts presenting with myelopathy. World Neurosurg. 2017;105:213-222. [DOI] [PubMed] [Google Scholar]
- 7.French H, Somasundaram A, Biggs M, et al. Idiopathic intradural dorsal thoracic arachnoid cysts: a case series and review of the literature. J Clin Neurosci. 2017;40:147-152. [DOI] [PubMed] [Google Scholar]
- 8.Moses ZB, Friedman GN, Penn DL, Solomon IH, Chi JH. Intradural spinal arachnoid cyst resection: implications of duraplasty in a large case series. J Neurosurg Spine. 2018;28(5):548-554. [DOI] [PubMed] [Google Scholar]
- 9.Hussain O, Treffy R, Reecher HM, et al. Management of a recurrent spinal arachnoid cyst presenting as arachnoiditis in the setting of spontaneous spinal subarachnoid hemorrhage: illustrative case. J Neurosurg Case Lessons. 2024;7(6):CASE23660.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Velz J, Fierstra J, Regli L, Germans MR. Spontaneous spinal subarachnoid hemorrhage with development of an arachnoid cyst—a case report and review of the literature. World Neurosurg. 2018;119:374-380. [DOI] [PubMed] [Google Scholar]
- 11.James HE, Postlethwait R. Spinal peritoneal shunts for conditions other than hydrocephalus and pseudotumor cerebri: a clinical report. Pediatr Neurosurg. 2007;43(6):456-460. [DOI] [PubMed] [Google Scholar]
- 12.Werner C, Mathkour M, Scullen T, Dallapiazza RF, Dumont AS, Maulucci CM. Recurrent arachnoid cysts secondary to spinal adhesive arachnoiditis successfully treated with a ventriculoperitoneal shunt. Clin Neurol Neurosurg. 2020;194:105835. [DOI] [PubMed] [Google Scholar]
- 13.Mofidi M, Mohammadi M, Saidi H, et al. Ultrasound guided lumbar puncture in emergency department: time saving and less complications. J Res Med Sci. 2013;18(4):303-307. [PMC free article] [PubMed] [Google Scholar]