Abstract
BACKGROUND
The Woven EndoBridge (WEB) is an effective embolization device. A few cases of WEB migration have been reported as adverse events, and most occurred during the procedure. A case of internal carotid artery (ICA) occlusion due to a trapped WEB, which occurred 12 days after the implantation procedure, is reported.
OBSERVATIONS
A woman in her 70s was referred for an enlarged left ICA aneurysm during follow-up. A WEB SL 5 × 3 was chosen as the embolic device, and the implantation procedure was completed uneventfully. The patient’s postoperative course was good, and she was discharged from the hospital. However, 12 days later, she was brought to the authors’ hospital because the WEB device was trapped and occluded in the left ICA. The trapped WEB could not be retrieved using a gooseneck snare or stent retriever, but suction from a Sofia catheter released the trapped device, allowing it to be repositioned within the aneurysm.
LESSONS
Most cases of WEB migration occur during surgery. In the present case, migration occurred 12 days after surgery, and to the best of the authors’ knowledge, no similar cases have been reported. It is important to keep in mind that there are cases similar to the current case.
Keywords: Woven EndoBridge, dislodging, aneurysm embolization
ABBREVIATIONS: AComA = anterior communicating artery, BA = basilar artery, FD = flow diverter, FRED = flow redirection endoluminal device, ICA = internal carotid artery, MCA = middle cerebral artery, MRI = magnetic resonance imaging, NBS = neck bridge stent, PComA = posterior communicating artery, WEB = Woven EndoBridge.
The Woven EndoBridge (WEB; Microvention-Terumo) is an effective embolization device with high technical success rates reported.1–4 In addition, good results have been reported,2–7 and medium-term and long-term data have also been published.4, 7 Unlike regular neck bridge stents (NBSs) and flow diverter (FD) stents, the WEB can be used even in the acute stage of ruptured aneurysms.2 Although a WEB device is often used for middle cerebral artery (MCA) aneurysms, anterior communicating artery (AComA) aneurysms, and basilar artery (BA) tip aneurysms,1, 2, 4, 5 good results have also been reported when used for sidewall types, such as internal carotid artery (ICA) and posterior communicating artery (PComA) bifurcation aneurysms and ICA paraclinoid aneurysms.8 There are also reports of its use for dissected aneurysms.9
Due to the characteristics of the system, there have been reports of perforation,2, 5, 7, 8 deformation,10 and dislocation.6, 11–13 Most of these cases were encountered during the procedure, and one case of WEB migration occurred the day after the procedure.13 However, in this case, because the WEB device had moved within the aneurysm during surgery, it was followed up the next day. It could be considered common to see some signs of an adverse event during the procedure in almost all cases.
A case of ICA occlusion caused by dislodgment of the WEB device 12 days after the implantation procedure is reported herein.
Illustrative Case
A woman in her 70s came to our hospital after a local doctor noted a tendency for her left ICA aneurysm to increase in size. The depth of the aneurysm was 5.5 mm, and its widths were 3.9 mm and 3.6 mm. A bleb-like structure on the lateral wall was observed on radiological examination, and preventive treatment was conducted. Regarding this sidewall aneurysm, we considered coil embolization combined with an NBS; however, we thought that the embolization procedure could be completed in a shorter time with the WEB device and that there was enough space inside the aneurysm to place the WEB. In addition, it would allow the use of antiplatelet agents for a much shorter period than would otherwise be possible, which was also the patient’s preference. Furthermore, we consulted with an experienced doctor in advance, and after being told that treatment with the WEB device was possible, we explained the procedure to the patient.
She was prescribed 100 mg of aspirin and 75 mg of clopidogrel from 10 days before the treatment, and after confirming suppression of platelet aggregation, she underwent surgery under general anesthesia. A Scepter C balloon catheter (Microvention-Terumo) was used in conjunction with a sidewall-type catheter to compensate for instability during WEB placement. The guiding catheter was a 9-Fr OPTIMO (Tokai Medical), and a 6-Fr Sofia catheter (Microvention-Terumo) was guided proximal to the aneurysm. A VIA21 microcatheter (Microvention-Terumo) was configured into a J shape and guided into the aneurysm using a CHIKAI black soft tip (Asahi Intecc). The WEB SL 5 × 3 was carefully detached, and while detaching, the balloon was half-inflated to prevent unexpected movement of the WEB. The images after WEB deployment were acceptable, and we judged that there was no problem (Fig. 1). In addition, since the literature confirmed that most adverse events with the WEB occur during the procedure, we had conducted an observation for a while after the WEB was placed, and we had confirmed that there were no unstable findings with the WEB, we completed the procedure. There was no problem in awakening the patient after the surgery, and magnetic resonance imaging (MRI) the next day demonstrated no high signal intensity on diffusion-weighted imaging and the left ICA signal on postoperative magnetic resonance angiography. The patient’s clinical course was good, and she was discharged 8 days after the procedure.
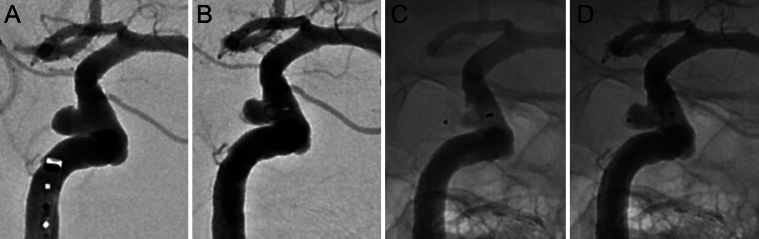
FIG. 1.
Intraoperative findings of the first procedure. Intraoperative working angle (A). Digital subtraction angiography after WEB placement (B). Fluorograms after WEB placement (C and D) showing no signs of instability.
Early in the morning 4 days after discharge, she complained of blurred vision in her left eye and called for an ambulance. On arrival at the hospital, she was conscious and had no obvious motor paralysis, but her left visual acuity was impaired. Head MRI was performed and showed left ICA occlusion. A thrombotic occlusion caused by the WEB device was initially considered, and angiography was performed, which showed that the WEB device had fallen out of the aneurysm and was trapped just proximal to the PComA. To attempt retrieval of the WEB device, a 9-Fr OPTIMO guiding catheter was placed at the origin of her left ICA, and retrieval was performed while maintaining the proximal occlusion. A 6-Fr Sofia catheter was navigated proximal to the occlusion site, and a Scepter C catheter was used to sandwich the device with the Sofia catheter to try to retrieve it, but this was not possible. A Goose Neck snare (Medtronic Neurovascular) of 4 or 7 mm was of no use, and a Solitaire device (6 mm × 40 mm, Medtronic Neurovascular) was used, but the WEB could not be retrieved. While retrieving the Solitaire device, suctioning from the Sofia catheter was tried, and the WEB moved slightly proximally due to the negative pressure, so the Scepter balloon catheter was carefully guided distally and pulled with the Sofia catheter under balloon inflation, and the WEB was reintroduced into the aneurysm (Fig. 2). The ICA was recanalized, and 3 days later, embolization was performed using a flow redirection endoluminal device (FRED; Microvention-Terumo) and coils (Fig. 3). After recanalization treatment, cerebral hemorrhage in the left occipital lobe was observed, which was thought to be due to hyperperfusion, but it was treated conservatively, leaving mild lower right quadrant blindness. The patient was discharged home with a modified Rankin Scale score of 1.
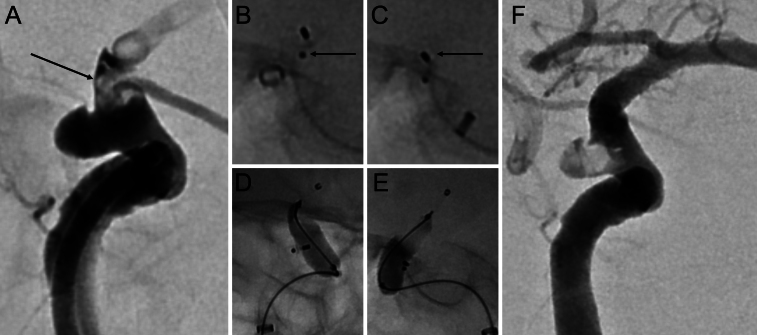
FIG. 2.
Cerebral angiography 12 days after initial treatment. The WEB that fell from within the aneurysm was trapped within the ICA (arrow, A). When suctioned with a Sofia catheter, the trapped WEB device moved proximally (arrows, B and C). Confirmation under balloon inflation that the WEB device was repositioned within the aneurysm and not prolapsed into the ICA (D and E). Final digital subtraction angiography (F).
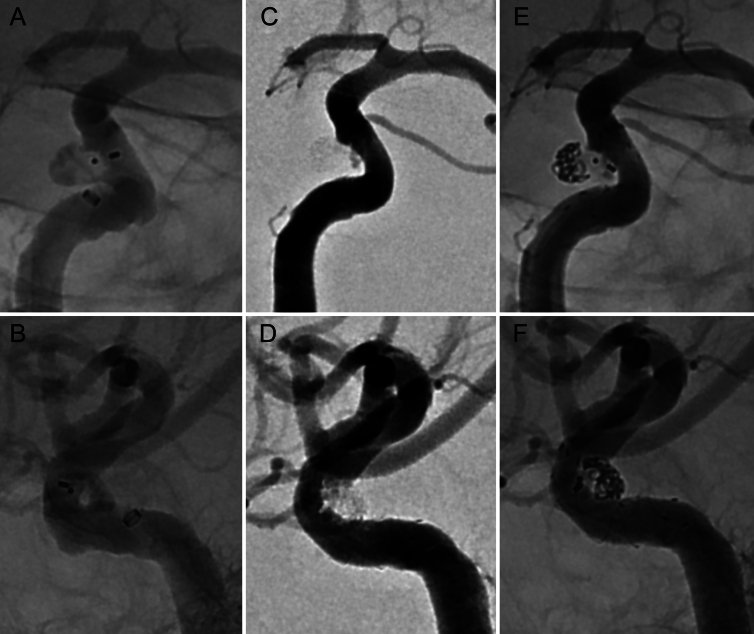
FIG. 3.
Images obtained during radical treatment. Preoperative fluorograms (A and B). Postoperative digital subtraction angiograms (C and D). Postoperative fluorograms (E and F).
Patient Informed Consent
The necessary patient informed consent was obtained in this study.
Discussion
The WEB consists of a self-expanding mesh structure, and when placed inside the aneurysm, it causes flow disruption to the aneurysm and promotes intra-aneurysmal thrombosis. Therefore, if implantation is successfully completed, antithrombotic drugs can be used for a very short period, unlike with NBSs and FD stents.6 Another feature is its utility for ruptured aneurysms.2 Lv et al. reported 967 aneurysms, with a technical success rate of 97%, an adequate occlusion rate of 81%, and a mortality rate of 2%;1 Zheng et al. reported a mortality rate of 1%.5 Mouchtouris et al. reported an adequate occlusion rate of 96.6%, and Pierot reported 81.1%.3, 6 Furthermore, Essibayi et al. reported an occlusion rate of 87.3% and Goertz et al., 90%.4, 13 In their review, Crinnion et al. reported an adequate occlusion rate of 71%–96% and mortality of 1.8%.2 Rodriguez-Calienes et al., who investigated the sidewall type of aneurysm, also reported that the adequate occlusion rate was 89%, and the technical success rate was 99%.8
Cherian et al. reported a comparison with clipping and noted that the complete occlusion rate was only 49%, which was a disappointing result.14 However, Chacón-Quesada et al. reported that there was no difference in morbidity or mortality between WEB cases and clipping cases,15 and Goertz et al. compared 103 clipping cases with 63 WEB cases and found that the therapeutic effect was equivalent to that of regular coiling and that indications should be determined on a case-by-case basis.13 Overall, WEB’s performance is not bad, and there is no doubt that it will be an option for aneurysm treatment. According to the literature, the MCA, AComA, and BA tip are typical sites for its use, and size selection is considered important since there are fewer size variations than for coils. In fact, Cherian et al. reported that 1.2 WEBs were used per surgery.14
Though a high technical success rate has been reported, there are also reports of technical failure. One was intraoperative perforation, which Zheng et al. reported in 4 cases (1%),5 Mouchtouris et al. in 1 case (0.9%),6 and Pierot in 2 cases (1.2%);3 Rodriguez-Calienes et al. reported it occurring in 1% of their patients.8 These adverse events occur when the WEB is deployed from the microcatheter or when resheathed, suggesting the importance of paying close attention to the movement and position of the microcatheter tip.
Another important issue is the unexpected movement of the WEB after detachment and its shedding into the parent vessel. Bañez and Chong reported a case in which the WEB became displaced during withdrawal from a BA tip aneurysm and was recovered using a Solitaire device.10 This is thought to be caused by an electrical detachment failure. Santhumayor et al. reported the case of a BA tip aneurysm in which the WEB became displaced and was recovered with a 4-mm gooseneck snare, as well as the case of an AComA aneurysm in which the WEB strayed into A2 and was recovered with a 2-mm gooseneck snare.11 In the reports of such recovery using gooseneck snares, the proximal markers of the WEB are captured by the snare. Di Caterino et al. reported the case of an M1–M2 aneurysm in which the WEB tilted within the aneurysm immediately after the WEB detached, and the next day it deviated to M2, so it was possible to rescue it using an NBS.12 The authors suggested that the apposition of the WEB to the aneurysm lateral wall was insufficient.13 In these reported cases, what is noteworthy is that a large WEB was unsuitable and that failure happened after the size was reduced.11, 12 This is because the second WEB becomes unstable after the downsizing of the first WEB to deviate from the neck, suggesting that there are some size variations that the WEB cannot accommodate. However, except for the case reported by Di Caterino et al.,12 all cases occurred during the procedure, and their reports confirmed that the situation was already unstable during the surgery. So, if there is a dangerous situation during the surgery, operators should not hesitate to change to another WEB.17 In addition, all reports of recovery involved a gooseneck snare, and this device captured the proximal WEB markers.10, 12 There is also a report that a Solitaire device was able to retrieve the WEB,11 and Simgen et al. stated that, in an animal experiment, WEB retrieval using a Solitaire was 100% effective.18 In their report, the Solitaire was fully deployed distal to the WEB and then entangled and retrieved at the proximal side of the stent.
Observations
Unlike previous reports, in the current case, the WEB became displaced 12 days after treatment, and because the WEB was anchored at the siphon, the proximal marker could not be captured at all with the snare, and the Solitaire device became flat due to the bending of the siphon, making WEB capture impossible. When suction was applied from a Sofia catheter in an attempt to retrieve the Solitaire device, the WEB moved slightly, and the anchor was released. By carrying the Scepter balloon catheter distally and sandwiching it with the Sofia catheter, it was possible to reposition the WEB within the aneurysm, allowing treatment to be performed 3 days later. During the first procedure, there were no signs of the WEB being displaced, and the event 12 days later was completely unexpected. However, when viewed retrospectively, it is possible that the WEB was slightly oversized, and the radial force of the slightly expanded portion within the parent vessel acted negatively, causing the WEB to deviate outside the aneurysm.
Lessons
To the best of our knowledge, there have been no reports of WEB migration 12 days after treatment. When selecting an undersized WEB or an inappropriate one without proper radial force to the aneurysm wall, poor apposition or compaction can occur,3 and oversizing can cause deviation to the parent vessel.12, 13 In most cases, there are some signs during the surgery, but considering that there are cases like the current one, we believe that it could be a good idea to confirm the position of the WEB by radiography in cases of broad-neck aneurysms. A case in which a WEB became displaced 12 days after surgery and became trapped in the ICA was reported herein. Size selection of the WEB is important; a small one can cause instability, and a large one can lead to deviation into the parent vessel. Although most technical failure events occur during surgery, it is important to keep in mind that there are cases similar to our present case and to perform follow-up.
Acknowledgments
We thank the radiologists at our hospital for their dedicated assistance during the procedures and Forte Science Communications for English-language editing.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: Kanazawa. Acquisition of data: Kanazawa, Kono, Ebise. Analysis and interpretation of data: Kanazawa. Drafting the article: Kanazawa. Critically revising the article: Kanazawa. Reviewed submitted version of manuscript: Kanazawa, Higashida. Approved the final version of the manuscript on behalf of all authors: Kanazawa. Administrative/technical/material support: Uchida. Study supervision: Kuniyoshi.
Correspondence
Ryuzaburo Kanazawa: Nagareyama Central Hospital, Nagareyama, Chiba, Japan. ryu.kan.jp.2412@gmail.com.
References
- 1.Lv X, Zhang Y, Jiang W. Systematic review of Woven EndoBridge for wide-necked bifurcation aneurysms: complications, adequate occlusion rate, morbidity, and mortality. World Neurosurg. 2018;110:20-25. [DOI] [PubMed] [Google Scholar]
- 2.Crinnion W, Bhogal P, Makalanda HLD, et al. The Woven EndoBridge as a treatment for acutely ruptured aneurysms: a review of the literature. Interv Neuroradiol. 2021;27(5):602-608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pierot L. Ten years of clinical evaluation of the Woven EndoBridge: a safe and effective treatment for wide-neck bifurcation aneurysms. NeuroIntervention. 2021;16(3):211-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Essibayi MA, Lanzino G, Brinjikji W. Safety and efficacy of the Woven EndoBridge device for treatment of ruptured intracranial aneurysms: a systematic review and meta-analysis. AJNR Am J Neuroradiol. 2021;42(9):1627-1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zheng H, Zhao Y, Zhou H, Tang Y, Xie Z, Liu CJ. Mid-to-long term safety and efficacy of Woven EndoBridge device for treatment of intracranial wide neck aneurysms: a systematic review and meta-analysis. Clin Neurol Neurosurg. 2023;232:107861. [DOI] [PubMed] [Google Scholar]
- 6.Mouchtouris N, Hasan D, Samaniego EA, et al. The Woven EndoBridge (WEB) device: feasibility, techniques, and outcomes after FDA approval. J Neurosurg. 2022;136(5):1266-1272. [DOI] [PubMed] [Google Scholar]
- 7.Stanca C, Carriero S, Negroni D, et al. Woven EndoBridge in wide-neck bifurcation aneurysms: digital subtraction angiography at 3-year follow-up. J Clin Med. 2022;11(10):2879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rodriguez-Calienes A, Vivanco-Suarez J, Galecio-Castillo M, et al. Use of the Woven EndoBridge device for sidewall aneurysms: systematic review and meta-analysis. AJNR Am J Neuroradiol. 2023;44(2):165-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khattar NK, White AC, Cruz AS, et al. Woven Endobridge device for treatment of dissection-related PICA aneurysm. Interv Neuroradiol. 2021;27(3):388-390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bañez RMF, Chong W. Retrieval of displaced Woven EndoBridge intrasaccular flow disruptor using Solitaire platinum revascularization device. NeuroIntervention. 2022;17(2):106-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Santhumayor BA, White TG, Werner C, Shah K, Woo HH. Woven EndoBridge device migration and microsnare retrieval strategy: single institutional case reports with technical video demonstration. NeuroIntervention. 2023;18(2):129-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Di Caterino F, Primikiris P, Vitale G, Biondi A. Woven EndoBridge device immediate post-detachment tilt with later displacement: case report, rescue techniques, and review of the literature. Interv Neuroradiol. 2020;26(4):483-487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goertz L, Liebig T, Siebert E, et al. Woven EndoBridge embolization versus microsurgical clipping for unruptured anterior circulation aneurysms: a propensity score analysis. Neurosurgery. 2021;88(4):779-784. [DOI] [PubMed] [Google Scholar]
- 14.Cherian J, Chen SR, Puri A, et al. Postmarket American experience with Woven EndoBridge device: adjudicated multicenter case series. Neurosurgery. 2021;89(2):275-282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chacón-Quesada T, Mielke D, Rohde V, Hernández-Durán S. Microsurgical clipping vs Woven EndoBridge (WEB) device for the management of unruptured wide-neck bifurcation aneurysms. Neurosurg Rev. 2022;45(4):2717-2722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goyal N, Hoit D, DiNitto J, et al. How to WEB: a practical review of methodology for the use of the Woven EndoBridge. J Neurointerv Surg. 2020;12(5):512-520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Amuluru K, Al-Mufti F, Sahlein DH, Scott J, Denardo A. Adjustment of malpositioned Woven EndoBridge device using gooseneck snare: complication management technique. NeuroIntervention. 2021;16(3):275-279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Simgen A, Yilmaz U, Dietrich P, et al. Rescue of migrated Woven Endobridge devices using a stent-retriever-technique in a porcine model. Interv Neuroradiol. 2020;26(6):772-778. [DOI] [PMC free article] [PubMed] [Google Scholar]