Introduction
Tick bite alopecia was described in the early 1900s1; however, few cases have been reported in the literature. Of the reported cases, alopecia following a tick bite on the scalp has been localized to the attachment site and the immediate surrounding area.1, 2, 3, 4, 5, 6, 7 Herein, we describe a unique case of tick bite alopecia in which the patient experienced diffuse alopecia areata-like hair loss in addition to hair loss in a similar distribution to prior cases.
Case report
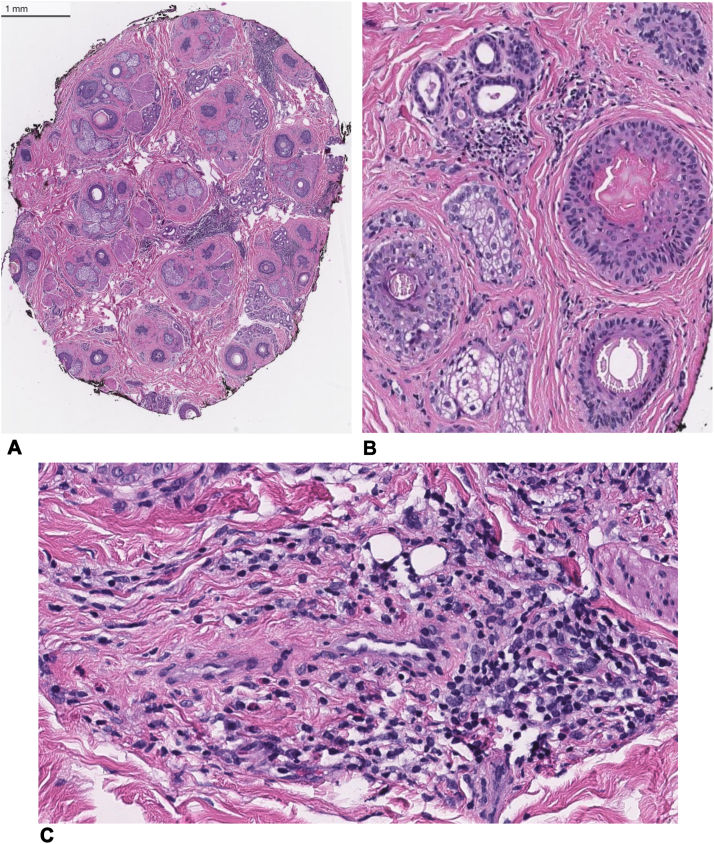
A 28-year-old woman with well-controlled polycystic ovary syndrome presented with a 7-month history of hair loss after being bitten by a tick on her vertex scalp. Initially, she developed alopecia around the tick attachment site; however, 1 month after the tick bite, the hair loss rapidly spread beyond the attachment site to involve the entire scalp (Fig 1, A). Therapies prior to presentation included over-the-counter vitamins and intralesional corticosteroids at an outside clinic, neither of which promoted hair regrowth. Upon presentation, her exam revealed diffuse patchy hair loss with a Severity of Alopecia Tool score of 52, with yellow and black dots and exclamation point hairs throughout the entire scalp, and postinflammatory hyperpigmentation and scar-like alopecia at the site of attachment. A hair pull test was not performed. Notably, she did not have any eyebrow, eyelash, or body hair loss. A 4 mm punch biopsy was performed, which captured both the attachment site and the adjacent area. The biopsy revealed a predominance of vellus hair follicles (terminal/vellus ratio = 0.7), with 42% of the follicles in catagen/telogen. There were also mildly atrophic sebaceous glands, mild to moderate superficial and deep perivascular, interstitial, and focally perifollicular lymphohistiocytic infiltrate with scattered eosinophils, and mild perifollicular fibrosis (Fig 2). The patient was started on a prednisone 1 mg/kg taper as a bridge to baricitinib 4 mg daily; however, she stopped after 5 days when she started baricitinib. Clinical improvement after baricitinib initiation was noted after 1 month, and she remained on 4 mg of baricitinib for 4 months before self-tapering off the medication. Upon discontinuation, the patient had significant regrowth in all prior alopecic sites apart from the tick attachment site and the immediate surrounding area (Fig 1, B).
Fig 1.
Clinical photos. A, Initial clinical presentation including site of attachment and biopsy site (Severity of Alopecia Tool score of 52). B, Regrowth 1 month after treatment of baricitinib therapy with residual alopecia at attachment site.
Fig 2.
Histopathologic findings of a transverse section at the level of the isthmus. A, Low-power (10×) magnification (H&E) demonstrating increased number of catagen/telogen and vellus hair follicles with a moderate perivascular and interstitial inflammatory infiltrate. B, Medium power (40×) magnification (H&E) showing cycling and miniaturized hair follicles adjacent to the area of inflammation with mild perifollicular fibrosis. C, High-power (100×) magnification (H&E) demonstrating perivascular and interstitial lympho-histiocytic infiltrate with scattered eosinophils. H&E, Hematoxylin and eosin.
Discussion
Tick bite alopecia, although rare, has maintained a relatively predictable clinical course involving a scalp eschar at the attachment site with surrounding nonscarring or cicatricial alopecia.7,8 Hard tick scalp attachment typically induces tissue necrosis and formation of an eschar that ultimately progresses to a patch of moth-eaten-appearing cicatricial alopecia.4, 5, 6,9 Surrounding hair loss can occur around the attachment site as tick saliva induces an abnormal telogen response via the interactions between the host’s tissues and tick saliva, which contains anticoagulant, anti-inflammatory, and immunomodulatory chemicals.2,3 While clinical response to tick bites on the scalp is variable with respect to time course, it typically presents with a similar type of hair loss pattern. Hair loss has been reported to resolve as early as 3 months; however, it has also been reported to remain for over 5 years. The scalp eschar at the attachment site has been demonstrated to persist in reported cases.4,8 Reports of hair loss aside from this pattern have not been made until recently when a case was reported involving localized alopecia areata-like changes surrounding the tick attachment site.10 Thus, this case represents a unique diffuse alopecia areata-like response to a tick bite on the scalp in addition to previously reported clinical features of tick bite alopecia. Biopsy findings are in line with previous reports including hair follicle miniaturization, increased number of catagen and telogen hairs, and perivascular and interstitial lymphocytic infiltrates with eosinophils.3,4 The markedly increased number of cycling and miniaturized hairs seen in tick bite alopecia are also seen in alopecia areata. Thus, this case represents a classic patchy alopecia areata-like pattern surrounding the bite site and an unusually more diffuse alopecia areata pattern throughout the scalp. While the differential diagnosis of the diffuse hair loss could also include telogen effluvium and only one biopsy was performed, which limits histologic comparison between the different alopecic patterns seen in this patient, the presence of diffuse yellow dots, black dots, exclamation point hairs, and rapid response to baricitinib favor a diagnosis of diffuse alopecia areata over telogen effluvium. This case represents a novel presentation of an uncommon entity, provides insight to other possible patterns of hair loss after tick bite, and demonstrates benefit with Janus kinase inhibitor therapy, traditionally reserved for treating classic severe alopecia areata.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
Patient consent: The authors have obtained written patient consent to use their photos and medical information to be published online with the understanding that this information may be publicly available and discoverable via search engines.
IRB approval status: Not applicable.
References
- 1.Gold L.S., Bagel J., Allenby K., Sidgiddi S. What's eating you? tick bite alopecia. Cutis. 2020;105(2):251–254. [Google Scholar]
- 2.Heyl T. Tick bite alopecia. Clin Exp Dermatol. 1982;5:537–542. doi: 10.1111/j.1365-2230.1982.tb02472.x. [DOI] [PubMed] [Google Scholar]
- 3.Castelli E., Caputo V., Morello V., Tomasino R.M. Local reactions to tick bites. Am J Dermatopathol. 2008;30(3):241–248. doi: 10.1097/DAD.0b013e3181676b60. [DOI] [PubMed] [Google Scholar]
- 4.Lynch M.C., Milchak M.A., Parnes H., Ioffreda M.D. Tick bite alopecia: a report and review. Am J Dermatopathol. 2016;38(11):e150–e153. doi: 10.1097/DAD.0000000000000598. [DOI] [PubMed] [Google Scholar]
- 5.Ross M.S., Friede H. Alopecia due to tick bite. AMA Arch Derm. 1955;71(4):524–525. doi: 10.1001/archderm.1955.01540280100026. [DOI] [PubMed] [Google Scholar]
- 6.Marshall J. Alopecia after tick bite. South African Med J. 1966;40(24):555–556. [PubMed] [Google Scholar]
- 7.Schaefer N., Agha R. Tick bite alopecia in an adult female patient. J Clin Aesthet Dermatol. 2024;17(3):S21–S22. [PMC free article] [PubMed] [Google Scholar]
- 8.Barbiero A., Manciulli T., Spinicci M., et al. Scalp eschar and neck lymph adenopathy after a tick bite (SENLAT) in Tuscany, Italy (2015–2022) Infection. 2023;51(6):1847–1854. doi: 10.1007/s15010-023-02079-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McGinley-Smith D.E., Tsao S.S. Dermatoses from ticks. J Am Acad Dermatol. 2003;49(3):363–392. doi: 10.1067/s0190-9622(03)01868-1. [DOI] [PubMed] [Google Scholar]
- 10.Peñuelas Leal R., Grau Echevarría A., Labrandero Hoyos C., Magdaleno Tapial J., Esteve Martínez A. Tick bite-induced alopecia areata-like effluvium. Australas J Dermatol. 2024;65(3):e79–e80. doi: 10.1111/ajd.14215. [DOI] [PubMed] [Google Scholar]