Abstract
OBJECTIVES
Colchicine, an anti-inflammatory agent, has been reported to improve myocardial infarction prognosis by inhibiting neutrophil extracellular traps (NETs) release. However, its role in cardiac surgery and the mechanisms behind NETs suppression remain unclear. This study aimed to explore colchicine’s cardioprotective effects against perioperative myocardial injury in cardiac surgery, focusing on NETs inhibition as a novel therapeutic strategy.
METHODS
Male Sprague-Dawley rats were pre-treated with colchicine (0.1 mg/kg/day) or CI-amidine (10 mg/kg/day) for 7 days before undergoing cardiopulmonary bypass and myocardial ischaemia/reperfusion injury. The model was created by subjecting the rats to cardiopulmonary bypass and myocardial ischaemia/reperfusion injury. Under 4.0% sevoflurane anaesthesia, cardiopulmonary bypass was initiated by cannulating the tail artery and right atrium, and perfusion was maintained for 4 h. Immunofluorescence detected NETs, and haematoxylin and eosin staining assessed inflammatory cell.
RESULTS
We found colchicine treatment significantly reduced perioperative myocardial injury in rats. Furthermore, we observed a notable elevation of NETs in the myocardial tissue of animal models. Moreover, suppressing peptidylarginine deiminase 4 was found to markedly diminish perioperative myocardial injury in rats. Additionally, colchicine can mitigate the release of NETs by inhibiting peptidylarginine deiminase 4.
CONCLUSIONS
NETs were significantly elevated during the perioperative period of cardiac surgery. Colchicine significantly mitigated myocardial injury in cardiac surgery by inhibiting NETs formation, with peptidylarginine deiminase 4 inhibition being one of its mechanisms.
Keywords: Cardiopulmonary bypass, Myocardial injury, Neutrophil extracellular traps, Colchicine
Cardiac surgery frequently results in perioperative complications like reperfusion arrhythmias and myocardial stunning, primarily due to ischaemia–reperfusion (I/R) injury [1].
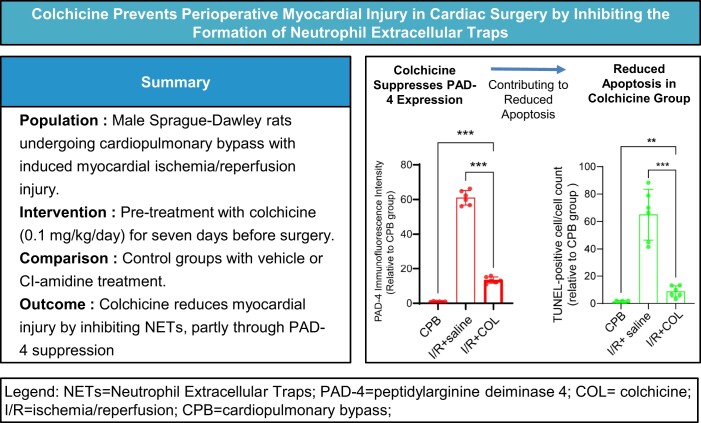
Graphical Abstract
INTRODUCTION
Cardiac surgery frequently results in perioperative complications like reperfusion arrhythmias and myocardial stunning, primarily due to ischaemia–reperfusion (I/R) injury [1]. This injury adversely impacts postoperative outcomes through inflammation, oxidative stress and cardiomyocyte apoptosis [2]. Inflammation, particularly driven by neutrophils, is central to this process [3]. Neutrophils, as the initial responders to I/R injury, release detrimental agents such as interleukins, tumour necrosis factors and reactive oxygen species (ROS) [3–5]. Previous researches underscored the importance of attenuating neutrophil activation to mitigate myocardial I/R injury and improve clinical outcomes [6–8].
Neutrophil extracellular traps (NETs), consisting of myeloperoxidase (MPO), neutrophil elastase (NE) and neutrophil-derived DNA, and regulated by the key enzyme peptidylarginine deiminase 4 (PAD-4), are critical mediators of neutrophil-driven cardiovascular inflammation. [3, 9–11]. NETs facilitate microthrombosis, intracellular calcium overload and amplify interleukins, tumour necrosis factors and radical production, which exacerbates myocardial I/R injury through the intensification of inflammation, endothelial damage and vascular permeability [12, 13]. Additionally, employing CI-amidine (CI-am), a specific inhibitor of PAD-4, can effectively reduce NETs synthesis, thereby diminishing their detrimental effects on the myocardium [10, 14]. However, existing studies predominantly address myocardial infarction or myocardial infarction-related I/R injuries [3, 5, 9], with limited focus on cardiac surgery models. Given that aortic cross-clamping and de-clamping during cardiopulmonary bypass (CPB) naturally induce myocardial I/R injury, it remains uncertain whether CPB-induced myocardial I/R also promotes NETs formation, exacerbating myocardial damage.
Colchicine (COL) has recently shown promise in reducing inflammation, improving cardiac function and mitigating cardiac remodelling in acute myocardial infarction by inhibiting NETs formation [9]. However, its effects in cardiac surgery and the mechanisms underlying COL’s inhibition of NETs remain unexplored. This study investigates COL’s potential to reduce I/R injury during the perioperative phase of cardiac surgery through NETs inhibition.
MATERIALS AND METHODS
Animals
Based on previous studies that utilized young adult rats to study myocardial inflammation [15] and to minimize the influence of age-related comorbidities, we selected 8-week-old male Sprague-Dawley rats for our model. The rats were obtained from Beijing Weitong Lihua Laboratory Animal Co. Ltd, housed under a 12-h light/12-h dark cycle and fed rodent chow at 25°C. All operators were blinded to group assignments throughout the experiment.
Ethical statement
Ethical approval was obtained from the Ethics Committee of Shanghai Children’s Medical Center (No. SCMC-LAWE-2023-006). All experimental procedures complied with the NIH guidelines for the Management and Use of Laboratory Animals (NIH publication no. 85-23, revised 1996) and were approved by the Ethics Committee.
Animal groups and drugs treatment
For the pharmacological intervention, rats in the I/R + CI-am group received CI-am (10 mg/kg/day; 0.5 ml; 506282, Sigma-Aldrich, USA) intraperitoneally for 7 days before surgery as an alternative to PAD-4 gene knockdown. Rats in the sham + COL, CPB + COL and I/R + COL groups were administered COL (0.1 mg/kg/day; 0.5 ml) intraperitoneally for 7 days before surgery (C3915, Sigma-Aldrich, USA). Control groups (sham + saline, CPB + saline and I/R+saline) received an equivalent volume (0.5 ml) of 0.9% saline. For non-pharmacological interventions, rats were assigned to sham, CPB or I/R groups based on the surgical procedure.
The I/R + COL, I/R + saline and I/R + CI-am groups underwent the same procedures as the I/R group; the CPB + COL and CPB + saline groups followed the CPB procedures; and the sham + COL and sham + saline groups followed the sham procedures.
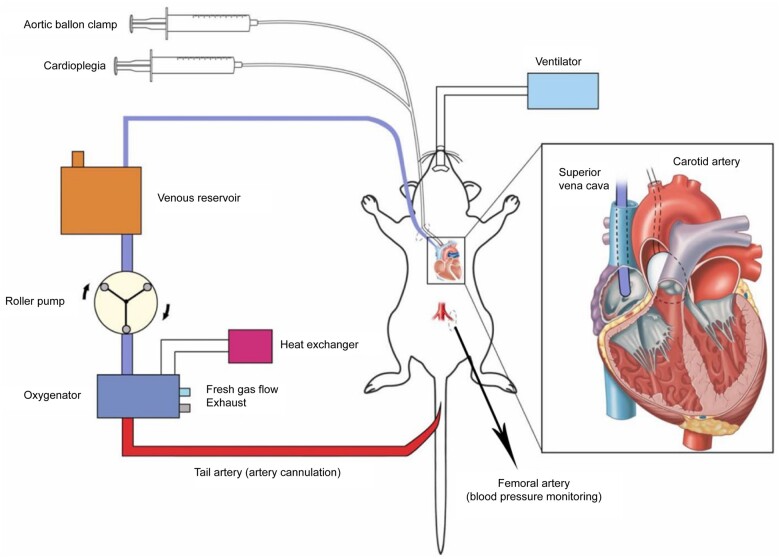
Establishment of animal models
The establishment of animal models is depicted in Fig. 1. Rats were anaesthetized with 4.0% sevoflurane, intubated and mechanically ventilated at 1.5% sevoflurane. The myocardial I/R injury model was created as follows: cannulation of the tail arteries and right atrium via the common jugular vein for CPB perfusion was performed. Cannulation of the ascending aorta via the arteria carotis communis for a balloon catheter insertion was conducted. The CPB circuit was prefilled with 12 ml of 6% hydroxyethyl starch, 1 ml heparin (250 IU/kg), 5% sodium bicarbonate and 1 ml of 20% mannitol. Upon reaching a rectal temperature of 32°C, the aorta was occluded using an inflatable balloon catheter, and then 0.9 ml of HTK (Histidine-tryptophan-ketoglutarate) solution was administered via the balloon catheter for cardioplegia. The aorta was reopened using a deflatable balloon catheter after the heart had been arrested for 40 min, followed by extubation of the balloon catheter. CPB was continuously reperfused via the right atrium and tail arteries for 4 h. Meanwhile, after the deflation of the balloon catheter, the temperature was rapidly raised to 36.5°C, and ventilation resumed for 4 h, with anaesthesia maintained at 1.0% sevoflurane. Subsequently, the rats were euthanized, myocardium harvested and rinsed with PBS (Phosphate Buffered Saline). The samples were then stored in 4% paraformaldehyde or liquid nitrogen. The CPB rats followed the same protocol without balloon inflation. The sham rats underwent the same procedures for cannulation and balloon catheter insertion and they did not undergo either CPB perfusion or balloon inflation.
Figure 1:
Diagram of CPB in rats. CPB: cardiopulmonary bypass.
Enzyme-linked immunosorbent assay
Complete methodology is provided in the Supplementary Material, Methods M1.
Haematoxylin and eosin staining
Complete methodology is provided in the Supplementary Material, Methods M2.
Immunofluorescence
Primary antibodies used were MPO (22225-1-AP, Proteintech, USA), NE (27642-1-AP, Proteintech, USA), cardiac troponin T (cTnT; 15513-1-AP, Proteintech, USA), CD11c (81853-1-RR, Proteintech, USA), citrullinated histone H3 (13754-1-AP, Proteintech, USA) and PAD-4 (17373-1-AP, Proteintech, USA). Secondary antibodies included CY3-conjugated antibody (SA00009-2, Proteintech, USA) and Alexa Fluor 488-conjugated antibody (RGAR002, Proteintech, USA). Nuclear staining was performed with DAPI (D1306, Thermo Fisher Scientific, USA). Detailed methodology is provided in Supplementary Material, Methods M3.
TUNEL (Terminal Deoxynucleotidyl Transferase dUTP Nick End Labeling) staining
Complete methodology is provided in the Supplementary Material, Methods M4.
Western blot
Primary antibodies used were MPO (ab208670, Abcam, USA), NE (ab310335, Abcam, USA), citrullinated histone H3 (CitH3; ab5103, Abcam, USA), cTnT (ab209813, Abcam, USA) and PAD-4 (ab214810, Abcam, USA). Detection employed a horseradish peroxidase-conjugated secondary antibody (ab6721, Abcam, USA), and protein bands were visualized using an ECL kit (#6883, Cell Signaling Technology, USA). Detailed methodology is provided in Supplementary Material, Methods M5.
Statistical analysis
Statistical analyses were conducted using SPSS version 24.0, with graphical representations generated in GraphPad Prism version 9.5. Normality of the data was assessed using the Shapiro–Wilk test. For normally distributed data, Student’s t-test was employed to compare 2 groups. For non-normally distributed data, the Mann–Whitney U-test was used. Comparisons between the experimental group and the 2 control groups were conducted twice, using separate t-tests or Mann–Whitney U-tests, as appropriate. Data are presented as mean (standard deviation), and statistical significance was set at P < 0.05. The power analysis process is detailed in Supplementary Material, Methods M6.
RESULTS
Complete analysis images (Supplementary Material, Figs S2–S13) and results data (Supplementary Material, Tables S1–S6) are provided in the Supplementary Material.
Generation of the perioperative myocardial injury animal models in cardiac surgery
Each group comprised 6 rats. Baseline characteristics of the successfully established models are detailed in Supplementary Material, Table S1. A total of 67 rats were utilized for model establishment, with 60 successfully developing myocardial injury models and 7 excluded due to failure to establish the model.
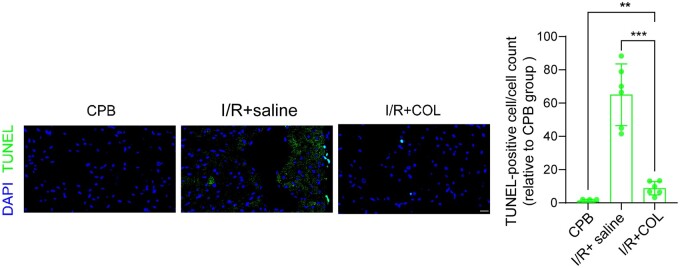
Colchicine reduced perioperative myocardial injury in cardiac surgery
We assessed the impact of COL on cardiomyocyte apoptosis by comparing the I/R + COL group with the I/R + saline group, which served as a control for I/R injury, and the CPB group, which controlled for CPB-induced apoptosis. Colchicine treatment resulted in a significant reduction in cardiomyocyte apoptosis, as demonstrated by TUNEL staining [TUNEL-positive cells/cell count (TUNEL ratio): I/R + COL 8.79(4.03) vs I/R + saline 65.02 (18.53), P < 0.001; vs CPB 1.00 (1.10), P < 0.01; Fig. 2; Supplementary Material, Fig. S1a and b; Supplementary Material, Table S3].
Figure 2:
Colchicine reduced perioperative myocardial injury in cardiac surgery. Rats in the I/R + colchicine group received colchicine for 7 days before model establishment. TUNEL staining (scale bars, 20 μm) was used to assess myocardial apoptosis (n = 6). Results are presented as the ratio of TUNEL-positive cells to total cell count. **P < 0.01, ***P < 0.001. Data are expressed as mean (SD). COL: colchicine; CPB: cardiopulmonary bypass; I/R: ischaemia–reperfusion; SD: standard deviation.
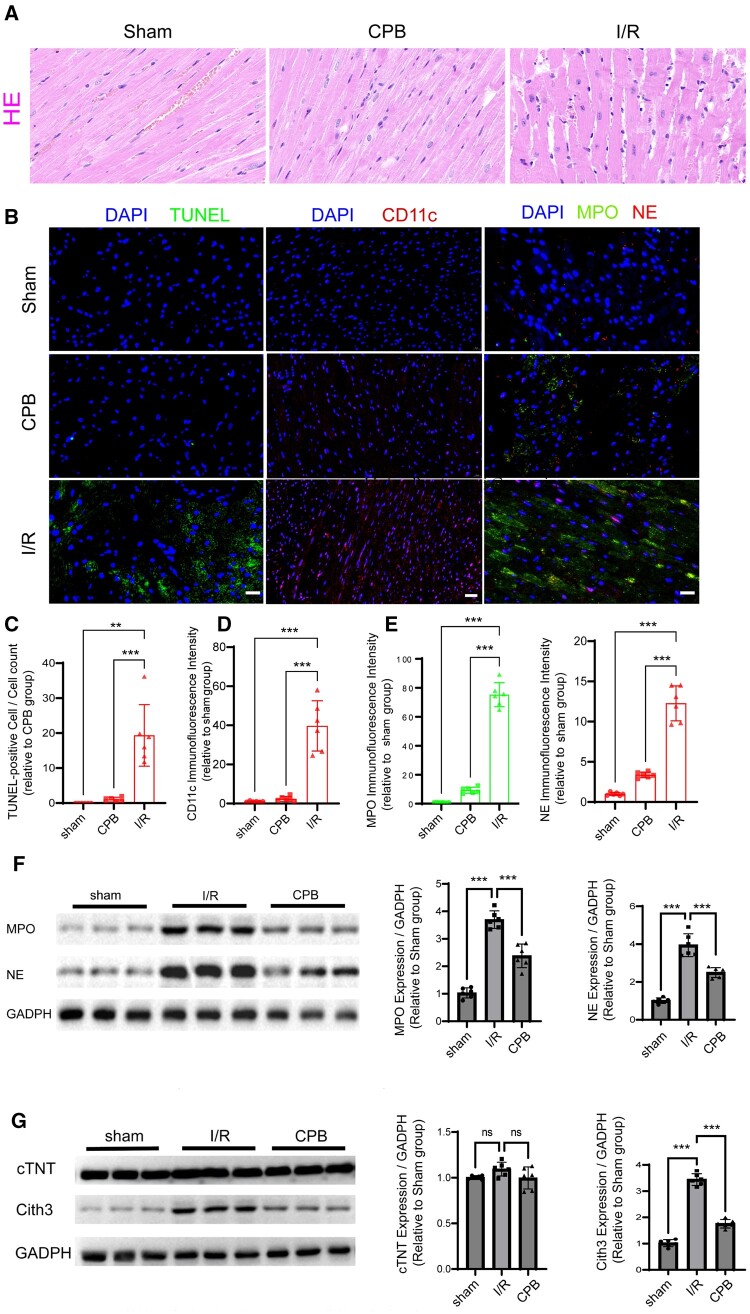
Neutrophil extracellular traps release increased in the perioperative period of heart surgery
To elucidate COL’s mechanisms in mitigating myocardial injury, we analysed NETs release in the I/R group, with CPB and sham groups as controls. Haematoxylin and eosin (HE) staining (Fig. 3A) revealed enhanced inflammatory cell infiltration in the I/R group compared to CPB and sham groups. TUNEL staining (Fig. 3B and C; Supplementary Material, Fig. S2b; Supplementary Material, Table S2) showed more pronounced injury in the I/R group [TUNEL ratio: I/R 19.35 (8.80) vs CPB 1.00 (0.69), P < 0.001; vs sham 0 (0), P < 0.01]. CD11c, a neutrophil marker, was significantly elevated in the I/R group [relative immunofluorescence intensity (RIFI): I/R 39.68 (12.87) vs CPB 2.36 (1.26), P < 0.001; vs sham 1.00 (0.28), P < 0.001; Fig. 3B and D; Supplementary Material, Fig. S2c; Supplementary Material, Table S2].
Figure 3:
NETs release increased in the perioperative period of heart surgery. (A) HE staining assessed inflammatory cell infiltration in myocardial tissues from sham, CPB and I/R rats. (B) TUNEL staining (scale bars, 20 µm) and immunofluorescence for CD11c, MPO and NE (scale bars, 20 µm) evaluated apoptosis and protein expression levels. (C) Apoptosis is represented as the ratio of TUNEL-positive cells to total cells (n = 6). (D and E) Fluorescence intensity of CD11c, MPO and NE was semi-quantitatively analysed (n = 6). (F and G) Western blot quantified MPO, NE, cTNT and CitH3 levels in myocardial tissues (n = 6). ‘ns’ denotes no significant difference. **P < 0.01, ***P < 0.001. Data are expressed as mean (SD). CitH3: citrullinated histone H3; CPB: cardiopulmonary bypass; cTNT: cardiac troponin T; HE: haematoxylin and eosin; I/R: ischaemia–reperfusion; MPO: myeloperoxidase; NE: neutrophil elastase; NETs: neutrophil extracellular traps; SD: standard deviation.
Given that neutrophil extracellular effects are primarily mediated by NETs, we investigated MPO and NE, key components of NETs. Immunofluorescence (Fig. 3B and E; Supplementary Material, Fig. S3a; Supplementary Material, Table S2) and western blot (WB) analysis (Fig. 3F; Supplementary Material, Fig. S3b; Supplementary Material, Table S2) revealed elevated MPO and NE levels in the I/R group. Additionally, CitH3, another NET marker, was significantly increased in the I/R group [RIFI: I/R 25.08 (1.93) vs CPB 6.92 (1.37), P < 0.001; vs sham 1.00 (0.17), P < 0.001; normalized protein expression-CitH3: I/R 3.44 (0.23) vs CPB 1.75 (0.16), P < 0.001; vs sham 1.00 (0.15), P < 0.001; Fig. 3G; Supplementary Material, Fig. S4a and b]. cTnT levels did not differ significantly among the groups (Fig. 3G; Supplementary Material, Fig. S4a and b; Supplementary Material, Table S2). Peripheral blood enzyme-linked immunosorbent assay further indicated significant increases in cTnT, IL (Interleukin)-6, IL-1β and procalcitonin in the I/R group (Supplementary Material, Fig. S4c–f; Supplementary Material, Table S2).
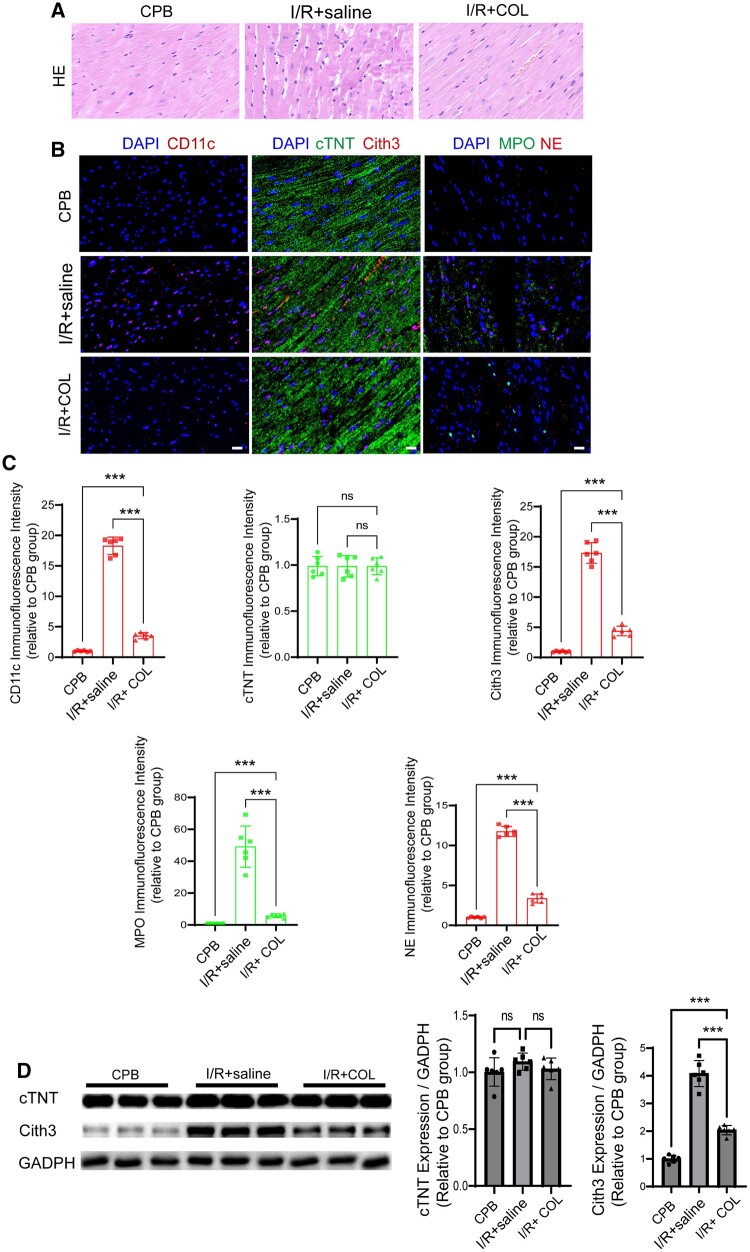
Colchicine reduced neutrophil extracellular traps release in heart surgery perioperative period
Our investigation then shifted to evaluating COL’s efficacy in reducing NETs release. HE staining (Fig. 4A) showed decreased inflammatory cell infiltration in the I/R + COL group compared to the I/R + saline group, indicating a potential reduction in NETs release. The CD11c was significantly reduced in the I/R + COL group [RIFI: I/R + COL 3.58 (0.54) vs I/R + saline 18.26 (1.47), P < 0.001; vs CPB 1.00 (0.11), P < 0.001; Fig. 4B and C, Supplementary Material, Fig. S5b; Supplementary Material, Table S3], corroborating the HE staining results.
Figure 4:
Colchicine reduced NETs release in the perioperative period of heart surgery. (A) HE staining evaluated inflammatory cell infiltration in colchicine-treated and control rats. (B) Immunofluorescence for CD11c, cTNT, CitH3, MPO and NE (scale bars, 20 μm) analysed protein expression levels. (C) Fluorescence intensity of these markers was semi-quantitatively assessed (n = 6). (D) Western blot quantified cTNT and CitH3 levels (n=6). ‘ns’ denotes no significant difference. ***P < 0.001. Data are expressed as mean (SD). CitH3: citrullinated Histone H3; COL: colchicine; CPB: cardiopulmonary bypass; cTNT: cardiac troponin T; I/R: ischaemia–reperfusion; MPO: myeloperoxidase; NE: neutrophil elastase; NETs: neutrophil extracellular traps; SD: standard deviation.
CitH3 expression was markedly diminished in the I/R + COL group, as evidenced by immunofluorescence [RIFI: I/R + COL 4.38 (0.80) vs I/R + saline 17.32 (1.69), P < 0.001; vs CPB 1.00 (0.12), P < 0.001; Fig. 4B and C; Supplementary Material, Fig. S5c; Supplementary Material, Table S3] and WB [normalized protein expression-CitH3: I/R + COL 2.24 (0.27) vs I/R + saline 3.23 (0.34), P < 0.001; vs CPB 1.00 (0.17), P < 0.001; Fig. 4D; Supplementary Material, Table S3]. Moreover, MPO and NE levels were also significantly reduced in the I/R + COL group (Fig. 4B and C; Supplementary Material, Fig. S6a and b; Supplementary Material, Table S3].
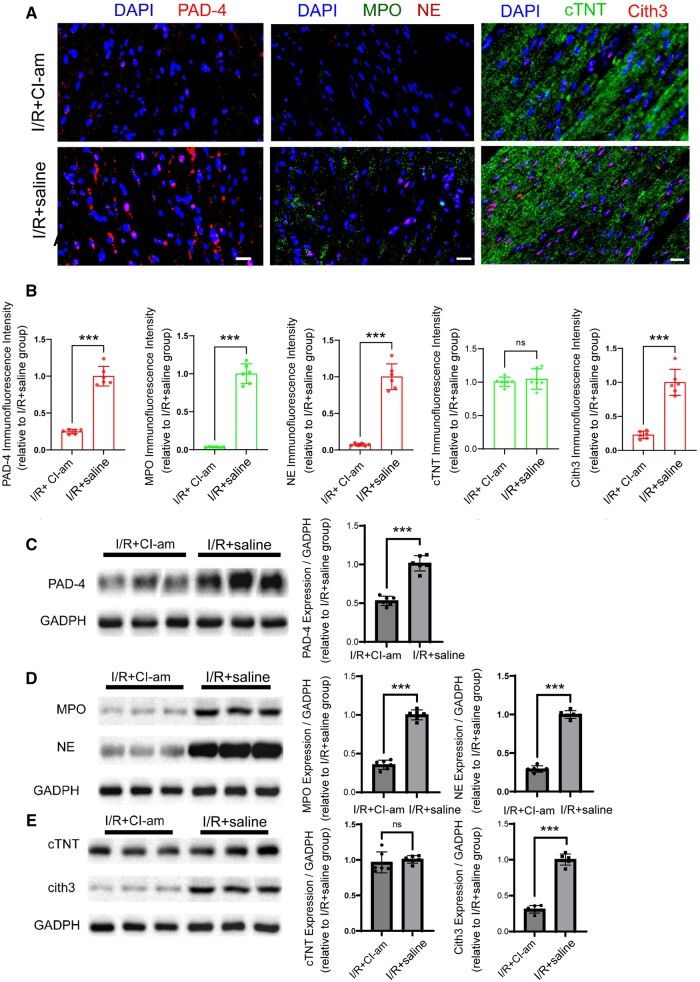
Suppressing peptidylarginine deiminase 4 protein reduced neutrophil extracellular traps release in heart surgery perioperative period
PAD-4 also plays a significant role in I/R injury during cardiac surgery. Immunofluorescence and WB analysis (Supplementary Material, Fig. S7a–d; Supplementary Material, Table S2) confirmed upregulation of PAD-4 expression in the I/R group compared to CPB and sham groups, highlighting its involvement. To explore whether PAD-4 inhibition could reduce myocardial injury during the perioperative period, rats were treated with CI-am for 7 days.
Immunofluorescence (Fig. 5A and B, Supplementary Material, Fig. S7e and f; Supplementary Material, Table S4) and WB (Fig. 5C, Supplementary Material, Fig. S7g and h; Supplementary Material, Table S4) demonstrated a marked reduction in PAD-4 expression in the I/R + CI-am group relative to the I/R + saline group [RIFI: I/R + CI-am 0.25 (0.03) vs I/R + saline 1.00 (0.13), P < 0.001; NEP-PAD-4: I/R + CI-am 0.53 (0.06) vs I/R + saline 1.00 (0.10), P < 0.001]. Additionally, PAD-4 inhibition led to a decrease in MPO and NE levels. Despite no significant variation in cTnT levels between the I/R + CI-am and I/R + saline groups, CitH3 levels were markedly reduced in the I/R + CI-am group [RIFI: I/R + CI-am 0.23 (0.06) vs I/R + saline 1.00 (0.19), P < 0.001; NEP-CitH3: I/R + CI-am 0.31 (0.08) vs I/R + saline 1.00 (0.12), P < 0.001; Fig. 5A, B and E, Supplementary Material, Fig. S9a–f; Supplementary Material, Table S4).
Figure 5:
Suppressing PAD-4 protein significantly reduced NETs release. (A) Immunofluorescence (scale bars, 20 μm) analysed PAD-4, MPO, NE, cTNT and CitH3 levels in I/R + CI-am and I/R + saline groups. (B) Fluorescence intensity of CD11c, cTNT, CitH3, MPO and NE was semi-quantitatively analysed (n = 6). (C–E) Western blot quantified PAD-4, MPO, NE, cTNT and CitH3 levels (n = 6). ‘ns’ denotes no significant difference. ***P < 0.001. Data are expressed as mean (SD). CI-am: CI-amidine; CitH3: citrullinated histone H3; cTNT: cardiac troponin T; I/R: ischaemia–reperfusion; MPO: myeloperoxidase; NE: neutrophil elastase; NETs: neutrophil extracellular traps; PAD-4: peptidylarginine deiminase 4; SD: standard deviation.
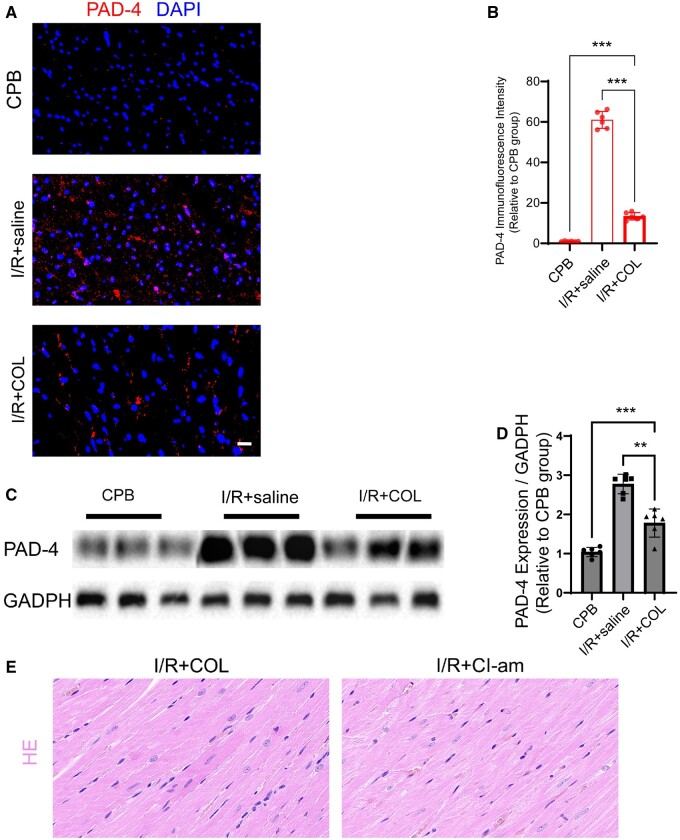
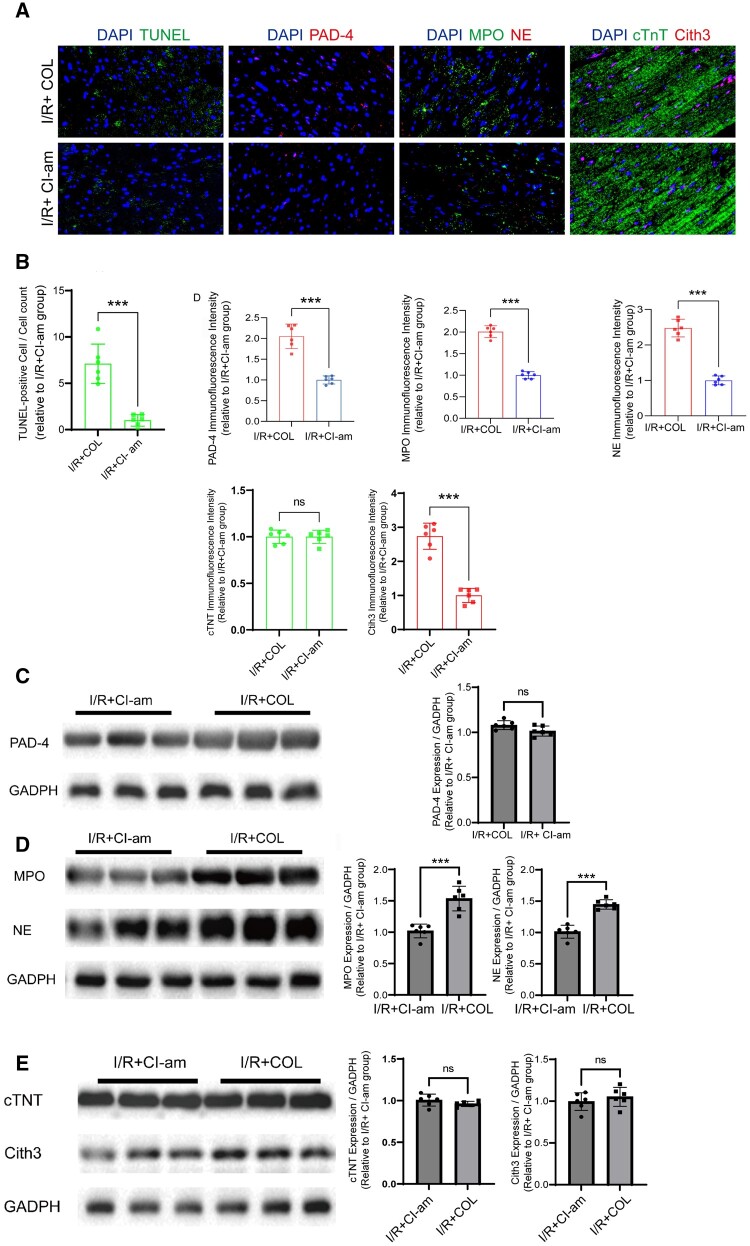
Colchicine can reduce neutrophil extracellular traps release by suppressing peptidylarginine deiminase 4
In our comparative analysis between the I/R + saline and I/R + COL groups, COL markedly reduced PAD-4 expression [RIFI: I/R + COL 13.39 (1.85) vs I/R + saline 61.00 (4.15), P < 0.001; vs CPB 1.00 (0.19), P < 0.001; NEP-PAD-4: I/R + COL 1.90 (0.45) vs I/R + saline 2.77 (0.25), P < 0.01; vs CPB 1.00 (0.12), P < 0.001; Fig. 6A–D, Supplementary Material, Fig. S10a and b; Supplementary Material, Table S3], indicating COL may inhibit NETs release by downregulating PAD-4. To evaluate whether COL alleviates myocardial I/R injury similarly to CI-am through PAD-4 inhibition, we compared the I/R + COL and I/R + CI-am groups. HE staining showed greater inflammatory cell infiltration and increased apoptosis in the I/R + COL group compared to the I/R + CI-am group [TUNEL ratio: I/R + COL 7.11 (0.87) vs I/R + CI-am 1.00 (0.26), P < 0.001; Fig. 7A and B, Supplementary Material, Fig. S10d; Supplementary Material, Table S5]. Additionally, MPO and NE levels were elevated in the I/R + COL group (Fig. 7A, B and D; Supplementary Material, Fig. S11e–j; Supplementary Material, Table S5). While significant differences in PAD-4 [RIFI: I/R + COL 42.91 (7.72) vs I/R + CI-am 1.00 (0.24), P < 0.001; Fig. 7A–C, Supplementary Material, Fig. S12a–d; Supplementary Material, Table S5] and CitH3 [RIFI: I/R + COL 2.74 (0.38) vs I/R + CI-am 1.00 (0.21), P < 0.001; Fig. 7A, B and E, Supplementary Material, Fig. S12a–d and f; Supplementary Material, Table S5] were observed, WB analysis showed that reductions in CitH3 [NEP-CitH3: I/R + COL 1.06 (0.11) vs I/R + CI-am 1.00 (0.10), P = 0.40) and PAD-4 [NEP-PAD-4: I/R + COL 1.06 (0.05) vs I/R + CI-am 1.00 (0.06), P = 0.58] were less pronounced. cTnT levels remained unchanged (Supplementary Material, Fig. S12a–e; Supplementary Material, Table S5).
Figure 6:
Colchicine reduced NETs release by suppressing PAD-4. (A) Immunofluorescence (scale bars, 20 μm) assessed PAD-4 levels in CPB, I/R + saline and I/R + COL groups (n = 6). (B) Fluorescence intensity of PAD-4 was semi-quantitatively analysed. (C and D) Western blot measured PAD-4 expression in CPB, I/R + saline and I/R + COL groups. (E) HE staining assessed inflammatory cell infiltration in I/R + COL and I/R + CI-am groups. **P < 0.01, ***P < 0.001. Data are expressed as mean (SD). CI-am: CI-amidine; COL: colchicine; CPB: cardiopulmonary bypass; HE: haematoxylin and eosin; I/R: ischaemia–reperfusion; PAD-4: peptidylarginine deiminase 4; SD: standard deviation.
Figure 7:
Colchicine reduced NETs release by suppressing PAD-4. (A) TUNEL staining (scale bars, 20 μm) assessed myocardial apoptosis in I/R + COL and I/R + CI-am groups. Immunofluorescence (scale bars, 20 μm) evaluated PAD-4, MPO, NE, cTNT and CitH3 levels. (B) Apoptosis and protein levels were semi-quantitatively analysed (n = 6). (C) Western blot quantified PAD-4, MPO, NE, cTNT and CitH3 levels. ‘ns’ denotes no significant difference. ***P<0.001. Data are expressed as mean (SD). CI-am: CI-amidine; Cith3: citrullinated histone H3; COL: colchicine; cTNT: cardiac troponin T; I/R: ischaemia–reperfusion; MPO: myeloperoxidase; NE: neutrophil elastase; PAD-4: peptidylarginine deiminase 4; SD: standard deviation.
Reflecting on our earlier comparisons, PAD-4 expression showed a sequential decline from the I/R group to the I/R + COL, I/R + CI-am and CPB groups. Peripheral blood enzyme-linked immunosorbent assay results supported this, revealing a stepwise reduction in inflammatory markers (Supplementary Material, Fig. S12g–j; Supplementary Material, Table S5) across these groups.
Low-dose colchicine showed no observed side effects on myocardial tissue
To investigate potential side effects of low-dose COL on myocardial tissue without I/R injury, we established sham + COL and CPB + COL groups, comparing them with respective non-drug intervention groups. Colchicine did not induce additional myocardial cell apoptosis and no differences in CD11c or NETs-related proteins (MPO, NE, Cith3) were observed between sham and sham + COL groups, and these indicators decreased post-COL intervention in the CPB group (Supplementary Material, Fig. S13; Supplementary Material, Table S6).
DISCUSSION
This animal study evaluates COL’s effectiveness in reducing perioperative myocardial injury during cardiac surgery. Our findings showed that COL significantly decreased cardiomyocyte apoptosis, evidenced by a lower TUNEL ratio in the I/R + COL group compared to the I/R + saline group. We also observed increased NETs release in the I/R group, with elevated levels of MPO, NE and CitH3. Colchicine treatment effectively reduced NETs release, as indicated by lower levels of these markers. Additionally, suppression of PAD-4 protein with CI-am significantly reduced NETs release, and COL produced similar effects by inhibiting PAD-4 expression. These results suggest that COL alleviates myocardial injury, at least in part, through PAD-4 inhibition, highlighting its potential as a therapeutic agent for myocardial protection in surgical contexts.
Our research concentrated on NETs, acknowledging PAD-4 as a critical enzyme in their regulation. It is also important to consider that PAD-4’s role extends beyond NETs formation; it is involved in gene expression, apoptosis and immune responses [16]. Recent studies have shown that NETs are implicated not only in inflammation but also in thrombosis, particularly in myocardial I/R injury, where NET-mediated microthrombosis may contribute to the ‘no-reflow’ phenomenon [17]. This study preliminarily substantiates the hypothesis that COL may alleviate myocardial injury by modulating the release of PAD-4-mediated NETs, positioning it as a potential alternative therapeutic agent. Colchicine reduces NETs, leading to decreased myocardial cell damage, which subsequently lowers cTnT release into peripheral blood [18]. However, due to CPB-induced I/R uniform damage and the inherently high expression of cTnT in myocardial tissue, immunofluorescence and WB might have no difference.
Colchicine, known for inhibiting leucocyte microtubule synthesis, was administered to rats at a dose of 0.1 mg/kg for 7 days, as per protocols from previous studies [20]. However, no leucocyte suppression was observed, consistent with the dose-dependent effects reported in the literature [20]. Therefore, it is reasonable to conclude that low-dose COL is safe for extended use and offers significant potential for myocardial protection. Major cardiovascular trials have shown that a continuous 30–90 days regimen of 0.5 mg COL significantly reduces serious adverse and cardiovascular events [7]. Additionally, COL has emerged as a novel therapy for chronic coronary syndrome [21]. In cardiac surgery, it significantly reduces postoperative atrial fibrillation [22]. Studies suggest that NETs and myocardial secretion after ischaemia contribute to AF and fibrosis, while COL’s anti-inflammatory effects help reduce calcium overload and ROS, key factors in postoperative atrial fibrillation [10, 15]. Our previous research showed that COL improves cardiac surgery outcomes [8], and this study further supports its foundation by demonstrating that COL also reduces myocardial injury from I/R through NETs inhibition. However, potential side effects, such as gastrointestinal disturbances and increased non-cardiovascular mortality, should be considered [23].
Thus, while COL shows great potential for application in the perioperative period of cardiac surgery, it is important to recognize its broader effects on PAD-4 and inflammation, as well as the associated risks. Further clinical trials are required to validate its safety profile.
Limitations
This study presents several limitations. First, while we concentrated on the role of NETs, we did not explore how COL modulates ROS levels and calcium influx by inhibiting NETosis, a critical process linked to myocardial injury via excessive ROS release and intracellular calcium overload [10, 12, 14]. This omission obscures the full mechanistic linkage between NETs and myocardial damage. Second, although preliminary evidence suggests that PAD-4 inhibition mitigates NETs release and myocardial injury, the absence of PAD-4 knockout models precludes definitive validation of this mechanism. Additionally, the use of 8-week-old rats deviates from the typical age of cardiac surgery patients, potentially impacting the applicability of our findings.
CONCLUSION
In conclusion, NETs were significantly elevated during the perioperative period of cardiac surgery. Colchicine reduces myocardial injury in cardiac surgery, and one of its mechanisms is through the inhibition of NETs formation, specifically targeting PAD-4.
Supplementary Material
Glossary
ABBREVIATIONS
- CI-am
CI-amidne
- CitH3
Citrullinated histone H3
- COL
Colchine
- CPB
Cardiopulmonary bypass
- cTNT
Cardiac troponin T
- HE
Haematoxylin and eosin
- I/R
Ischaemia–reperfusion
- MPO
myeloperoxidase
- NE
Neutrophil elastase
- NETs
Neutrophil extracellular traps
- PAD-4
Peptidylarginine deiminase 4
- RIFI
Relative immunofluorescence intensity
- ROS
Reactive oxygen species
- TUNEL ratio
TUNEL-positive cell/cell count
Contributor Information
Hao-Dong Pan, Department of cardiac surgery, Nanjing Drum Tower Hospital Clinical College of Nanjing University of Chinese Medicine, Number 321 Zhong shan Road, Nanjing 210008, Jiangsu, China; Department of Clinical Medicine, Norman Bethune Health Science Center of Jilin University, Changchun, China.
You-Ru Kong, Department of cardiac surgery, Nanjing Drum Tower Hospital Clinical College of Nanjing University of Chinese Medicine, Number 321 Zhong shan Road, Nanjing 210008, Jiangsu, China.
Li Xu, Clinical Trial Institution, Nanjing Drum Tower Hospital, The Affiliated Hospital of Nanjing University Medical School, Nanjing, Jiangsu, China.
Ming-Yue Liu, Department of Cardiac Surgery, Zhongshan Hospital of Fudan University, Shanghai, China.
Zhi-Kang Lv, Department of Cardiac Surgery, Nanjing Drum Tower Hospital, Affiliated Hospital of Medical School, Nanjing University, Nanjing, China.
Yusanjan Matniyaz, Department of Cardiac Surgery, Nanjing Drum Tower Hospital, Affiliated Hospital of Medical School, Nanjing University, Nanjing, China.
Hai-Tao Zhang, Department of Cardiac Surgery, Nanjing Drum Tower Hospital, Peking Union Medical College & Chinese Academy of Medical Sciences, Graduate School of Peking Union Medical College, Nanjing, China.
Yu-Xian Tang, Department of cardiac surgery, Nanjing Drum Tower Hospital Clinical College of Nanjing University of Chinese Medicine, Number 321 Zhong shan Road, Nanjing 210008, Jiangsu, China.
Wen-Xin Su, Department of cardiac surgery, Nanjing Drum Tower Hospital Clinical College of Nanjing University of Chinese Medicine, Number 321 Zhong shan Road, Nanjing 210008, Jiangsu, China.
Chen-Yu Jiang, Department of Cardio-Thoracic Surgery, Shanghai Children’s Medical Center, School of Medicine, Shanghai Jiao Tong University, Shanghai, China.
Yi-Fan Zhu, Department of Cardio-Thoracic Surgery, Shanghai Children’s Medical Center, School of Medicine, Shanghai Jiao Tong University, Shanghai, China.
Dong-Jin Wang, Department of cardiac surgery, Nanjing Drum Tower Hospital Clinical College of Nanjing University of Chinese Medicine, Number 321 Zhong shan Road, Nanjing 210008, Jiangsu, China; Department of Cardiac Surgery, Nanjing Drum Tower Hospital, Affiliated Hospital of Medical School, Nanjing University, Nanjing, China; Department of Cardiac Surgery, Nanjing Drum Tower Hospital, Peking Union Medical College & Chinese Academy of Medical Sciences, Graduate School of Peking Union Medical College, Nanjing, China.
Xiao-Lu Jiao, Department of Cardiology, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, Hangzhou, China.
Tuo Pan, Department of Cardiac Surgery, Nanjing Drum Tower Hospital, Affiliated Hospital of Medical School, Nanjing University, Nanjing, China; Department of Cardiac Surgery, Nanjing Drum Tower Hospital, Peking Union Medical College & Chinese Academy of Medical Sciences, Graduate School of Peking Union Medical College, Nanjing, China.
SUPPLEMENTARY MATERIAL
Supplementary material is available at EJCTS online.
FUNDING
This work was supported by grants from the National Natural Science Foundation of China (No. 82300459) and funding for Clinical Trials from the Affiliated Drum Tower Hospital, Medical School of Nanjing University: 2023-LCYJ-ZD-03.
Conflict of interest: none declared.
DATA AVAILABILITY
The data used to support the findings of this study are available from the corresponding author upon request. The data are not publicly available due to privacy or ethical restrictions.
Author contributions
Hao-Dong Pan: Conceptualization; Writing—original draft; Writing—review & editing. You-Ru Kong: Writing—original draft; Writing—review & editing. Li Xu: Conceptualization; Writing—review & editing. Ming-Yue Liu: Software; Validation. Zhi-Kang Lv: Software; Validation. Yusanjan Matniyaz: Software; Validation. Hai-Tao Zhang: Software; Validation. Yu-Xian Tang: Software; Validation. Wen-Xin Su: Software; Validation. Chen-Yu Jiang: Software; Validation. Yi-Fan Zhu: Software; Validation. Dong-Jin Wang: Conceptualization; Methodology; Writing—review & editing. Xiao-Lu Jiao: Methodology; Writing—review & editing. Tuo Pan: Funding acquisition; Methodology; Writing—review & editing.
Reviewer information
European Journal of Cardio-Thoracic Surgery thanks Claudia Heilmann, Samuel Heuts, and Philippe Grieshaber for their contribution to the peer review process of this article.
REFERENCES
- 1. Hausenloy DJ, Yellon DM.. Myocardial ischemia-reperfusion injury: a neglected therapeutic target. J Clin Invest 2013;123:92–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ali M, Pham A, Wang X, Wolfram J, Pham S.. Extracellular vesicles for treatment of solid organ ischemia-reperfusion injury. Am J Transplant 2020;20:3294–307. [DOI] [PubMed] [Google Scholar]
- 3. Stakos DA, Kambas K, Konstantinidis T, Mitroulis I, Apostolidou E, Arelaki S. et al. Expression of functional tissue factor by neutrophil extracellular traps in culprit artery of acute myocardial infarction. Eur Heart J 2015;36:1405–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ong SB, Hernández-Reséndiz S, Crespo-Avilan GE, Mukhametshina RT, Kwek XY, Cabrera-Fuentes HA. et al. Inflammation following acute myocardial infarction: multiple players, dynamic roles, and novel therapeutic opportunities. Pharmacol Ther 2018;186:73–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Döring Y, Libby P, Soehnlein O.. Neutrophil extracellular traps participate in cardiovascular diseases: recent experimental and clinical insights. Circ Res 2020;126:1228–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. García-Prieto J, Villena-Gutiérrez R, Gómez M, Bernardo E, Pun-García A, García-Lunar I. et al. Neutrophil stunning by metoprolol reduces infarct size. Nat Commun 2017;8:14780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tardif JC, Kouz S, Waters DD, Bertrand OF, Diaz R, Maggioni AP. et al. Efficacy and safety of low-dose colchicine after myocardial infarction. N Engl J Med 2019;381:2497–505. [DOI] [PubMed] [Google Scholar]
- 8. Pan T, Jiang CY, Zhang H, Han XK, Zhang HT, Jiang XY. et al. The low-dose colchicine in patients after non-CABG cardiac surgery: a randomized controlled trial. Crit Care 2023;27:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bonaventura A, Vecchié A, Abbate A, Montecucco F.. Neutrophil Extracellular Traps and Cardiovascular Diseases: An Update. Cells 2020;9:231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Li YW, Chen SX, Yang Y, Zhang ZH, Zhou WB, Huang YN. et al. Colchicine inhibits NETs and alleviates cardiac remodeling after acute myocardial infarction. Cardiovasc Drugs Ther 2024;38:31–41. [DOI] [PubMed] [Google Scholar]
- 11. Lee TL, Lai TC, Lin SR, Lin SW, Chen YC, Pu CM. et al. Conditioned medium from adipose-derived stem cells attenuates ischemia/reperfusion-induced cardiac injury through the microRNA-221/222/PUMA/ETS-1 pathway. Theranostics 2021;11:3131–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Saffarzadeh M, Juenemann C, Queisser MA, Lochnit G, Barreto G, Galuska SP. et al. Neutrophil extracellular traps directly induce epithelial and endothelial cell death: a predominant role of histones. PLoS One 2012;7:e32366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fuchs TA, Brill A, Duerschmied D, Schatzberg D, Monestier M, Myers DDJ. et al. Extracellular DNA traps promote thrombosis. Proc Natl Acad Sci U S A 2010;107:15880–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kusunoki Y, Nakazawa D, Shida H, Hattanda F, Miyoshi A, Masuda S et al Peptidylarginine deiminase inhibitor suppresses neutrophil extracellular trap formation and MPO-ANCA production. Front Immunol 2016;7:227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. He L, Liu R, Yue H, Zhang X, Pan X, Sun Y. et al. Interaction between neutrophil extracellular traps and cardiomyocytes contributes to atrial fibrillation progression. Signal Transduct Target Ther 2023;8:279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Koushik S, Joshi N, Nagaraju S, Mahmood S, Mudeenahally K, Padmavathy R. et al. PAD4: pathophysiology, current therapeutics and future perspective in rheumatoid arthritis. Expert Opin Ther Targets 2017;21:433–47. [DOI] [PubMed] [Google Scholar]
- 17. Ge L, Zhou X, Ji WJ, Lu RY, Zhang Y, Zhang YD. et al. Neutrophil extracellular traps in ischemia-reperfusion injury-induced myocardial no-reflow: therapeutic potential of DNase-based reperfusion strategy. Am J Physiol Heart Circ Physiol 2015;308:H500–H9. [DOI] [PubMed] [Google Scholar]
- 18. Shen L, Zhu Y, Chen Z, Shen F, Yu W, Zhang L.. Isoliquiritigenin attenuates myocardial ischemia reperfusion through autophagy activation mediated by AMPK/mTOR/ULK1 signaling. BMC Cardiovasc Disord 2024;24:415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zhang D, Li L, Li J, Wei Y, Tang J, Man X. et al. Colchicine improves severe acute pancreatitis-induced acute lung injury by suppressing inflammation, apoptosis and oxidative stress in rats. Biomed Pharmacother 2022;153:113461. [DOI] [PubMed] [Google Scholar]
- 20. Weng JH, Koch PD, Luan HH, Tu HC, Shimada K, Ngan I. et al. Colchicine acts selectively in the liver to induce hepatokines that inhibit myeloid cell activation. Nat Metab 2021;3:513–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Manolis AA, Manolis TA, Manolis AS.. Managing chronic coronary syndrome: how do we achieve optimal patient outcomes? Expert Rev Cardiovasc Ther 2024;22:243–63. [DOI] [PubMed] [Google Scholar]
- 22. Agarwal S, Beard CW, Khosla J, Clifton S, Anwaar MF, Ghani A. et al. Safety and efficacy of colchicine for the prevention of post-operative atrial fibrillation in patients undergoing cardiac surgery: a meta-analysis of randomized controlled trials. Europace 2023. Jul 4;25(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chen T, Liu G, Yu B.. A meta-analysis evaluating efficacy and safety of colchicine for prevention of major cardiovascular events in patients with coronary artery disease. Clin Res Cardiol 2023;112:1487–505. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request. The data are not publicly available due to privacy or ethical restrictions.