Abstract
Understanding the role of aberrant salience (AS) in psychosis is crucial for comprehending schizophrenia spectrum disorders (SSDs). Researchers emphasize the importance of salience attribution in schizophrenia, acknowledging its interaction with environmental stressors and multiple neurotransmitter systems. Childhood trauma and adversities (CTA) play a significant role in SSDs, potentially contributing to prodromal symptoms characterized by AS. While empirical evidence supports the relationship between AS and SSD, the interplay between different AS patterns, CTA, and psychotic symptoms remains unclear. Clinical diagnosis followed DSM-5 criteria, and participants completed assessments including the Aberrant Salience Inventory (ASI), Childhood Trauma Questionnaire – Short form (CTQ-SF), and Positive and Negative Symptom Scale (PANSS). Latent profile analysis (LPA) was employed to identify distinct AS profiles within the sample, with subsequent analyses examining differences in psychopathological variables among these profiles. Among 262 participants, four distinct AS profiles emerged from LPA: low AS, high AS with severe symptoms and CTA, intermediate AS with sexual abuse correlation, and chronic AS with specific childhood trauma associations. Profile distinctions included differences in age, hospitalizations, psychotic symptoms, and CTA. Logistic regression analyses showed significant associations between the four profiles and emotional and sexual abuse, physical neglect and clinical variables. Subtyping individuals with SSD based on AS revealed four distinct profiles, each with unique clinical characteristics and associations with CTA. Future studies should investigate whether these profiles correspond to diverse treatment outcomes. These findings highlight the complexity of schizophrenia presentation and underscore the importance of considering individualized diagnostic and therapeutic approaches.
Subject terms: Schizophrenia, Psychosis
Introduction
The construct of aberrant salience (AS) is intimately connected to the psychopathology of psychosis, characterized by the attribution of undue importance to normally insignificant stimuli1,2. This cognitive mechanism is linked to dysregulated dopaminergic neurons and significantly contributes to the onset and continuation of psychotic disorders by promoting delusional ideation3. Kapur suggests that dysregulated mesolimbic dopaminergic signaling aligns with the abnormal attribution of salience observed in psychosis4. Consequently, there have been suggestions to recognize the importance of salience attribution in diagnostic classifications of schizophrenia5. However, the dopamine hypothesis has also faced numerous criticisms, outlining significant limitations6,7, since it is more accurately described as addressing the pathophysiology rather than the etiology of schizophrenia. Its limitations in explaining symptoms beyond psychosis, along with evidence of the involvement of other neurotransmitters such as glutamate and adenosine, point to a broader view of the disease8. Therefore, researchers and clinicians have attempted to update the Kapur’s hypothesis, grounding its neurobiological basis in subsequent empirical discoveries. They particularly focus on the Salience Network and its interaction with other functional networks9,10, which are modulated by environmental stressors11. In this regard, psychosocial stressors, such as childhood trauma and adversities (CTA), migration, and urban living, have been linked to various psychiatric disorders, including schizophrenia, and might mediate the association between the salience network and aberrant functional networks associated with disruptions in corticostriatal connectivity and abnormalities in salience processing. Consequently, dysfunction in these mechanisms due to prolonged exposure to stress may offer insights into how common environmental factors contribute to a wide array of psychotic symptoms12. In doing so, they avoid oversimplifying the etiology of psychosis to the action of a single neurotransmitter. This approach aligns with research demonstrating abnormalities in multiple neurotransmitter systems in psychosis, including glutamate, GABA, and serotonin13.
Among environmental stressors, CTA seem to play a key role in the onset, development and maintenance of schizophrenia spectrum disorders (SSDs)14,15. Indeed, the duration and severity of psychotic episodes, as well as the emerging psychopathological dimensions, could also be related to specific features of CTA16. In this context, CTA can be seen as a distal risk factor contributing to the prodromal stage characterized by AS.
While some empirical evidence supports the relationship between AS and SSD17–20, it remains unclear whether different patterns of AS are linked to CTA and psychotic symptoms in patients with SSD. Specifically, a deeper understanding of the heterogeneity in their presentations is needed. In this framework, latent profile analysis (LPA) emerges as a fitting method for more accurately profile and characterize individuals displaying distinct patterns of AS21,22. LPA serves as a valuable tool for conducting person-centered analyses, which stand apart from variable-centered methodologies. Essentially, LPA is a statistical procedure that employs continuous variables (i.e. indicators) to reveal hidden subgroups within a given population (i.e. latent profiles) based on specific variables of interest. This methodology operates under the premise that individuals can be assigned to different profiles or groups with different probabilities23.
Currently, there are no studies in the literature that have investigated the relationship between AS, CTA, and psychotic symptoms in SSD patients using LPA. Hence, it would be very useful, from a clinical point of view, to shed light on the relationship between these dimensions by investigating different subgroups characterized by specific AS symptoms in order to structure more targeted interventions in the clinical practice.
Based on the above, the present study seeks to investigate the heterogeneity of AS symptoms within a group of patients with SSD using LPA. The first aim is to use LPA to identify potential hidden profiles with different AS symptoms. Next, we analyze distinctions between individuals within each profile regarding psychopathological variables, including CTA, psychotic symptoms, and clinical data such as age of onset of the disorder and number of hospitalizations. Finally, logistic regression models are used to explore relationships between profile memberships and the variables of interest. Even though this study is exploratory, we formulate several hypotheses about aberrant salience profiles based on the existing literature. We hypothesize that one profile would be characterized by high levels of AS associated with severe positive psychotic symptoms. Another profile was expected to feature low levels of AS, associated with milder positive psychotic symptoms. Additionally, we predict a third profile characterized by moderate levels of AS, with a mix of both positive and negative psychotic symptoms.
Methods
Participants
Partakers eligible to participate were chosen from individuals who sought treatment at the Psychiatry Unit of the University Hospital “Renato Dulbecco” of Catanzaro (Italy), and at the outpatient unit of the Centro di Salute Mentale of Lamezia Terme (Catanzaro), between July 2020 and February 2024. Inclusion criteria required that participants: 1) be between 18 and 65 years old and able of providing valid informed consent; 2) have been diagnosed with schizophrenia or schizoaffective disorder by a senior psychiatrist following the DSM-5 diagnostic criteria24; and 3) have been under the unit’s care for a minimum of 12 consecutive months.
Clinical diagnosis was made using the Structured Clinical Interview for DSM-5 (SCID-5-CV)25, in accordance with DSM-5 criteria24, by a psychiatrist experienced in performing neuropsychiatric assessments.
Participants were excluded if they met any of the following criteria: 1) diagnosis of dementia, intellectual disability, or other severe medical conditions associated with secondary psychiatric symptoms that could potentially skew the assessment; 2) diagnosed with a substance use disorder in the past six months; 3) inability to complete the assessment due to conditions such as language disorders or a lack of proficiency in the Italian language; and 4) failure to provide valid informed consent for participation in the study procedures.
This study adhered to the ethical principles outlined in the updated Declaration of Helsinki26 and received approval from the Ethical Committee of the “Regione Calabria, Sezione Area Centro” (identifier: Prot. 66/15.03.2018). Before completing the questionnaires, participants provided written informed consent.
Measures
Clinical and sociodemographic characteristics
An ad hoc form was completed to assess demographic and clinical characteristics of participants. Information collected included psychiatric history, age at first onset of symptoms, duration of untreated psychosis (DUP), previous admissions to psychiatric hospitals, and treatment with antipsychotic medications. The prescribed daily dosage of antipsychotics was standardized to the equivalent daily dose of chlorpromazine, following international consensus27.
Assessment
Participants completed the following set of questionnaires:
The Aberrant Salience Inventory (ASI)28, a self-administered assessment comprising 29 items with binary (yes/no) responses, designed to gauge individual tendencies towards aberrant salience and susceptibility to psychosis. This scale explores five dimensions: feelings of increased significance (FIS, 7 items), sense sharpening (SS, 5 items), impending understanding (IU, 5 items), heightened emotionality (HE, 6 items), and heightened cognition (HC, 6 items). The overall severity of aberrant salience is derived from the total score across all factors (ranging from 0 to 29) used for analysis. The Italian adaptation of the ASI29 utilized in this study demonstrated satisfactory psychometric properties. The Kuder-Richardson 20 coefficient, which is analogous to Cronbach’s alpha for dichotomous data, was 0.92 in this study.
The Childhood Trauma Questionnaire Short-Form (CTQ-SF)30 is a self-administered assessment comprising 28 items, utilizing a Likert-type response scale ranging from 1 (never) to 5 (very often). This questionnaire describes five subscales: emotional abuse, physical abuse, sexual abuse, emotional neglect, and physical neglect. In this study, internal consistency was evaluated using McDonald’s omega, yielding the following values: physical abuse (0.84), emotional abuse (0.88), sexual abuse (0.84), emotional neglect (0.91), and physical neglect (0.85).
The Positive and Negative Symptom Scale (PANSS)31 is a standardized clinical interview utilized to assess the severity and occurrence of positive and negative symptoms, alongside general psychopathology, among patients with schizophrenia in the preceding week. This instrument consists of 30 items using a Likert-type response scale ranging from 1 (absent) to 7 (extreme). Specifically, the positive and negative symptom subscales each contain seven items (score range: 7–49), while the general psychopathology subscale encompasses 16 items (score range: 16–122). The McDonald’s’ omega were: 0.85, 0.88, 0.89 for PANSS positive, negative and general respectively.
All measures were administered in a single session by the same trained practitioner, following this order: socio-demographic data collection, PANSS, ASI, and CTQ. The entire assessment took approximately 60 min to complete.
Statistical analyses
The analyses were conducted using SPSS Version 26.0 and R Version 4.3.1, with the tidyLPA package32. To determine the number of profiles within the sample, models ranging from one to five profiles were assessed using information statistical criteria, including Consistent Akaike’s Information Criteria (cAIC), Bayesian Information Criteria (BIC), sample size-adjusted BIC (saBIC), and approximate weight of evidence criterion (AWE). Lower values of these indices indicate higher predictive accuracy. Participant classification accuracy was assessed utilizing standardized entropy, with values ranging from 0 to 1. Values surpassing .80 indicate robust group differentiation33. Regarding sample size, there is no definitive recommendation for the minimum sample size in LPA34.
To empirically distinguish profiles linked to aberrant salience impairments in individuals with SSDs, we conducted an LPA based on their scores across the five subscales of the ASI.
Following the identification of an LPA solution, individuals were assigned to a class based on their most likely class membership. In case of departure from the homoscedasticity assumption, Welch ANOVA, followed by Dunnet T3 post hoc tests, was employed to identify differences among the empirically derived profiles in the self-reported measures.
Finally, logistic regression models were employed to explore relationships between profile memberships and the variables of interest (i.e. clinical characteristics, CTA, PANSS symptomatology).
Statistical significance was defined at p < 0.05.
Results
Description of the sample
Of the 281 patients initially contacted for the study, 22 were excluded during the screening or enrollment phase for the following reasons: nine patients (3.2%) were deemed ineligible due to an active substance use disorder; seven (2.5%) withdrew before completing the assessment and were consequently excluded; and six (2.1%) met the exclusion criteria for intellectual disability. Thus, a total of 262 patients (N = 221 schizophrenia, N = 41 schizoaffective disorder) met,inclusion criteria and were enrolled with a dropout rate of 7.8%.
In the final sample, 165 (63.0%) individuals identified themselves as males and 97 (37.0%) as female. The mean age of participants was 42.9 ± 13.3 years and the mean years of education was 11.3 ± 3.8. Most participants (71%) reported no familial history of SSD. Finally, the majority of the sample was single (80.6%) and unemployed (51.1%). All enrolled patients were taking antipsychotic therapy at the time of enrollment. Table 1 presents the socio-demographic characteristics of the sample.
Table 1.
Socio-demographic and clinical characteristics of the whole sample.
| N = 262 | |||
|---|---|---|---|
| Fr | % | ||
| Mean age (years)a | 42.9 | (13.3) | |
| Sex | Male | 165 | (63.0) |
| Female | 97 | (37.0) | |
| Civil status | Married | 37 | (14.1) |
| Divorced | 14 | (5.3) | |
| Single | 211 | (80.6) | |
| Education (years)a | 11.3 | (3.8) | |
| Employment | Employed | 40 | (15.3) |
| Unemployed | 134 | (51.1) | |
| On pension | 22 | (8.4) | |
| Unpaid activity | 46 | (17.6) | |
| Invalid/Retired | 20 | (7.6) | |
| Diagnosis | Schizophrenia | 221 | (84.4) |
| Schizoaffective Disorder | 41 | (15.6) | |
| Familiarity for psychosis | Yes | 76 | (29.0) |
| No | 186 | (71.0) | |
aData are expressed as means and (standard deviation).
Latent profile analysis
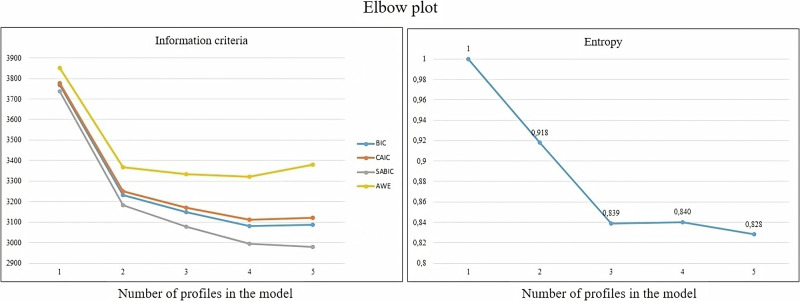
Among the statistics evaluated to compare model fit, the 4-class solution emerged as the most balanced option. Notably, the elbow plot showed a more pronounced shift in information criteria between the 3- and 4-profile models (Fig. 1). overall, the four-class model appeared to offer the best fit to the data. This model demonstrated the lowest values for AIC, cAIC, BIC, saBIC, and AWE. Additionally, the four-class model showed the highest entropy (.84), indicating a clear distinction between profiles33.
Fig. 1. Fit indices for the latent profile analysis of the ASI.
Information criteria values are shown on the left, and entropy values are shown on the right.
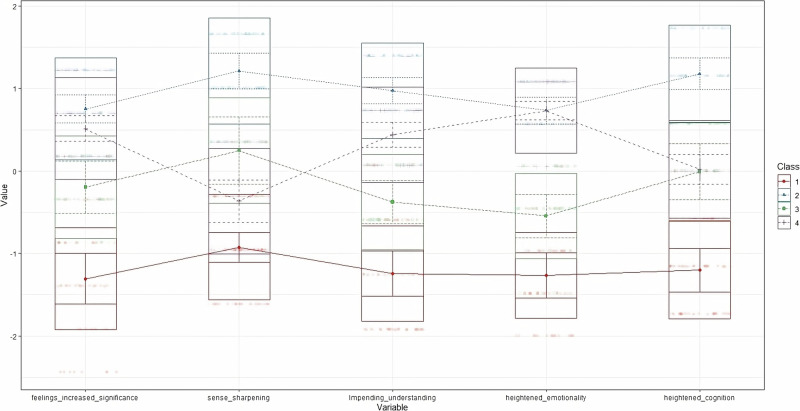
This solution revealed a baseline profile with low ASI scores in all domains, comprising 61 (23.3%) participants (Profile 1). In contrast, a second class consisting of 56 (21.4%) participants exhibited high aberrant salience impairment in all ASI domains (Profile 2). Interestingly, a third (N = 56, 21.4%; Profile 3) and a fourth (N = 89, 34%; Profile 4) profiles showed a mirrored trend across ASI score domains. Specifically, members of Profile 4 reported high scores on feelings of increased significance, impending understanding, and heightened emotionality, whereas those in Profile 3 showed high scores on sense sharpening, and vice versa. Both profiles showed similar scores in heightened cognition (Table 2).
Table 2.
Comparisons of latent profiles in socio-demographic and clinical features.
| Profile 1 | Profile 2 | Profile 3 | Profile 4 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n = 61 | n = 56 | n = 56 | n = 89 | |||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | F | p | Post-hoc | ||
| Demographic and clinical variables | Age | 39.9 | 13.5 | 44.4 | 12.2 | 39.1 | 12.5 | 46.3 | 13.5 | 4.843 | 0.003 | 4 > 1,3 |
| Age of onset | 27.1 | 10.2 | 24.0 | 8.2 | 24.5 | 8.6 | 26.6 | 11.0 | 1.603 | 0.191 | ||
| Hospitalizations | 1.1 | 1.4 | 2.4 | 2.9 | 1.6 | 2.4 | 0.8 | 1.7 | 5.372 | 0.002 | 2 > 1,4 | |
| Duration of untreated psychosis | 1.5 | 1.8 | 2.2 | 2.0 | 1.6 | 2.1 | 1.8 | 1.9 | 1.246 | 0.296 | ||
| Daily equivalent dose of chlorpromazine (mg) | 406.7 | 150.0 | 521.1 | 203.6 | 455.1 | 190.1 | 419.6 | 174.5 | 3.494 | .027 | 2 > 1 | |
| PANSS | Positive (7–49) | 17.1 | 7.8 | 20.2 | 6.8 | 18.1 | 7.1 | 17.9 | 7.6 | 2.073 | 0.107 | |
| Negative (7–49) | 21.1 | 7.3 | 22.4 | 6.3 | 21.6 | 6.5 | 24.0 | 7.7 | 2.235 | 0.087 | ||
| General (16–122) | 42.4 | 14.4 | 44.9 | 10.1 | 42.3 | 10.1 | 45.2 | 12.7 | 1.185 | 0.318 | ||
| CTQ-SF | Emotional Abuse (5–25) | 7.7 | 4.2 | 12.7 | 4.8 | 9.1 | 4.6 | 12.1 | 4.0 | 19.559 | <0.001 | 2,4 > 1,3 |
| Physical Abuse (5–25) | 6.5 | 2.9 | 8.7 | 4.0 | 7.2 | 3.2 | 8.3 | 2.7 | 6.467 | <0.001 | 2,4 > 1 | |
| Sexual Abuse (5–25) | 5.7 | 2.1 | 7.7 | 4.1 | 7.3 | 4.1 | 5.8 | 1.7 | 5.656 | 0.001 | 2,3 > 1,4 | |
| Emotional Neglect (5–25) | 11.5 | 5.4 | 16.1 | 5.4 | 12.4 | 5.8 | 16.5 | 5.6 | 14.001 | <0.001 | 2,4 > 1,3 | |
| Physical Neglect (5–25) | 7.6 | 3.3 | 11.0 | 3.8 | 8.4 | 3.4 | 11.7 | 3.5 | 22.106 | <0.001 | 2,4 > 1,3 | |
| Total (25–125) | 40.0 | 14.4 | 56.6 | 14.9 | 45.1 | 15.8 | 54.6 | 14.4 | 18.302 | <0.001 | 2,4 > 1,3 | |
| ASI | Feelings increased significance (0–7) | 2.1 | 1.5 | 6.1 | 0.9 | 4.4 | 1.2 | 5.7 | 1.1 | 118.984 | <0.001 | 2,4 > 1,3;3 > 1 |
| Sense sharpening (0–5) | 1.0 | 0.8 | 4.4 | 0.7 | 2.9 | 1.1 | 1.9 | 1.1 | 200.472 | <0.001 | 2>All; 3,4 > 1; 3 > 4 | |
| Impending understanding (0–5) | 1.0 | 1.0 | 4.4 | 0.7 | 2.3 | 0.9 | 3.6 | 0.8 | 173.949 | <0.001 | 2>All; 4 > 1,3; 3 > 1 | |
| Heightened emotionality (0–6) | 1.4 | 1.1 | 5.3 | 1.0 | 2.8 | 1.1 | 5.4 | 0.8 | 246.475 | <0.001 | 2,4 > 1,3 | |
| Heightened cognition (0–6) | 1.0 | 1.1 | 5.1 | 0.7 | 3.0 | 1.1 | 3.0 | 1.1 | 210.687 | <0.001 | 2>All; 3,4 > 1 | |
| Total (0–29) | 6.6 | 3.2 | 25.4 | 2.3 | 15.4 | 2.6 | 19.6 | 2.6 | 466.294 | <0.001 | 2>All;3,4 > 1; 4 > 3 |
Results in bold are statistically significant.
PANSS Positive and negative symptom scale, CTQ Childhood trauma questionnaire – Short form, ASI Aberrant salience inventory.
Figure 2 illustrates the standardized group means across ASI dimensions for the four-profile solution.
Fig. 2. Graphic representation of mean‐centered parameter estimates for ASI Profiles.
Standardized group averages on ASI subscales for a four-profile solution.
Comparison of psychopathological variables between the four profiles
Differences were found in age and hospital admissions, with members of profile 4 reporting a higher mean age than those in the Profiles 1 and 3; conversely, Profile 2 showed a higher number of hospital admissions than Profiles 1 and 4. No differences were found in DUP and age of onset among the four profiles.
Regarding the average dose of chlorpromazine equivalents, the only difference was that Profile 2 reported the highest average dose compared to Profile 1.
In terms of the mean scores for the variables of interest, no significant differences were found across the three PANSS dimensions.
Finally, with respect to CTA, both Profile 2 and Profile 4 reported higher scores on all CTQ subscales than Profiles 1 and 3, except for sexual abuse, where members of Profiles 2 and 3 reported higher scores than Profiles 1 and 4.
Association between group membership and psychopathological variables
A sequence of univariate logistic regressions with multinomial outcomes was conducted to assess the relationships between group membership and the variables of interest (Table 3), with adjustments made for their common variance. A high age of onset, low levels of emotional abuse, and low levels of physical neglect were associated with Profile 1. Furthermore, individuals with a higher number of hospital admissions had higher odds of belonging to Profile 2, whereas those with high scores for sexual abuse were more likely to be classified in Profile 3. Finally, individuals with high levels of emotional abuse and physical neglect and a low number of hospital admissions were more likely to be in Profile 4.
Table 3.
Associations between group membership and psychopathological variables.
| Profile 1 | Profile 2 | Profile 3 | Profile 4 | ||
|---|---|---|---|---|---|
| n = 61 | n = 56 | n = 56 | n = 89 | ||
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | ||
| Demographic and clinical variables | Age | 0.977 (0.943–1.012) | 1.019 (0.988–1.052) | 0.982 (0.949–1.015) | 1.014 (0.984–1.044) |
| Age of onset | 1.048 (1.003–1.095)* | 0.965 (0.925–1.007) | 1.004 (0.960–1.050) | 0.989 (0.952–1.027) | |
| Hospitalizations | 0.994 (0.836–1.182) | 1.205 (1.046–1.389)** | 1.019 (0.875–1.187) | 0.812 (0.671–0.983)* | |
| DUP | 0.944 (0.791–1.127) | 1.108 (0.939–1.308) | 0.985 (0.830–1.170) | 0.965 (0.820–1.136) | |
| PANSS | Positive | 1.011 (0.953–1.073) | 1.025 (0.972–1.081) | 1.031 (0.973–1.091) | 0.939 (0.891–0.990) |
| Negative | 0.951 (0.887–1.019) | 0.979 (0.919–1.042) | 1.005 (0.942–1.071) | 1.058 (0.996–1.124) | |
| General | 1.002 (0.959–1.045) | 1.006 (0.965–1.049) | 0.975 (0.933–1.018) | 1.024 (0.985–1.064) | |
| CTQ-SF | Emotional Abuse | 0.841 (0.742–0.954)** | 1.093 (0.993–1.204) | 0.916 (0.823–1.018) | 1.131 (1.022–1.252)* |
| Physical Abuse | 1.093 (0.923–1.294) | 0.914 (0.799–1.046) | 1.017 (0.881–1.175) | 0.927 (0.800–1.074) | |
| Sexual Abuse | 0.904 (0.775–1.053) | 1.084 (0.974–1.205) | 1.145 (1.029–1.274)* | 0.777 (0.655–0.922) | |
| Emotional Neglect | 1.079 (0.978–1.192) | 1.014 (0.923–1.114) | 1.004 (0.918–1.098) | 0.946 (0.862–1.038) | |
| Physical Neglect | 0.799 (0.681–0.938)** | 1.040 (0.898–1.204) | 0.913 (0.791–1.053) | 1.275 (1.105–1.472)** | |
| Nagelkerke’s R2 | 0.267 | 0.191 | 0.137 | 0.329 |
Results in bold are statistically significant.
PANSS Positive and negative symptom scale, CTQ-SF Childhood trauma questionnaire – Short form, DUP Duration of untreated psychosis.
*p < 0.05; **p < 0.01.
Discussion
This research is the first attempt to identify potential hidden profiles of stable patients suffering from schizophrenia and receiving antipsychotic treatment according to their AS, and to discriminate their clinical characteristics based on childhood traumas, positive, negative and general psychotic symptomatology and clinical variables (i.e. frequency of hospitalizations, age of onset, etc.). In addition, we examined the differences between profiles concerning various psychopathological variables, including CTA, psychotic symptoms, and clinical data such as the age of onset of the disorder and the frequency of hospital admissions.
The present results partially confirmed our hypotheses. This analysis identified four distinct profiles. As anticipated, we found a high AS/high psychotic symptoms profile (Profile 2) and a low AS/low psychotic symptoms profile (Profile 1). However, instead of a single intermediate profile, our findings revealed two intermediate AS profiles (Profile 3 and Profile 4).
Profile 1 is characterized by low levels of AS, as well as milder positive, negative, and general psychotic symptoms. Although these differences are not statistically significant, Profile 1 also exhibits a low impact from CTA and a later age of onset. This combination of features and outcomes suggests a less severe condition with fewer risk factors typically associated with youth. This data is particularly relevant due to the limited research on these specific aspects. In fact, if on the one hand a high level of AS, especially if juvenile, intuitively and scientifically correlates with higher psychotic symptoms, the opposite, although conceivable, is not widely investigated3,35. Furthermore, the higher age of onset observed in this group may support the thesis that lower levels of AS are associated with later onset. This is because marked AS is often linked to abnormal dopaminergic circuits and structural brain anomalies, which are typically associated with an earlier and more acute onset of psychotic symptoms36. Therefore, the later onset seen in this group could suggest that underlying biological vulnerabilities, such as these aberrant circuits and abnormalities, are less pronounced, thus contributing to a later and potentially less severe manifestation of the disorder.
Profile 2 presents a high level of AS in all domains, associated with more marked psychotic symptoms, greater number of hospitalizations and high level of childhood trauma, outlining a juvenile, acute and severe clinical manifestation. This too finds support in the literature on the subject, which has long supported the idea of a mediating effect of aberrant salience between childhood traumas and psychotic symptoms, which would be more marked when the other two variables are present19,37. Consequently, some authors have proposed that AS could be directly correlated not only with general psychotic symptoms but specifically with first-rank symptoms, and, therefore, ASI could serve as a tool for delineating psychopathological dimensions within the schizophrenic spectrum, rather than relying solely on categorical diagnoses38. Furthermore, the most striking result was the association between the frequency of hospitalizations and membership in the identified profile. It is crucial to emphasize that a higher frequency of hospital admissions indicates more relapses, with a known detrimental impact on the prognosis of the disorder39–41. In summary, the characteristics of Profile 2 underscore the critical need for early intervention and targeted treatment strategies to mitigate the long-term impact of frequent hospitalizations and severe psychopathology in this high-risk group.
Profile 3 involves intermediate levels of AS, with a marked sense sharpening and a significant association with childhood sexual abuse. Therefore, it could be speculated that this condition could be related to the presence of a sexual trauma as a triggering element even in the absence of a high initial level of other psychopathological elements. This association of variables also finds support in the literature, if we consider how sexual abuse in childhood impacts the possibility of developing major psychiatric disorders in adulthood42,43. These mechanisms of this connection are undeniably intricate, with hints of cross-contributions at genetic, neurophysiological, behavioral, cognitive, and emotional levels44Most theories highlight that child sexual abuse emerges as a an important precursor to psychosis, offering theoretical insights into the generation of psychotic symptoms and clinical pathways to improve cognitive-behavioral treatment approaches45,46.
Finally, Profile 4 appears to be characterized by a high level of feelings of increased significance, impending understanding, and heightened emotionality among the ASI domains, with a reduced number of hospitalizations and higher average age. Further, belonging to this profile is associated with high level of physical neglect and emotional abuse. This description seems to match that of a chronic and less productive condition, with fewer positive symptoms and acute relapses, not necessarily corresponding to a less severe form in the past, but certainly no longer as active anymore. This is not surprising given the history of schizophrenia, its nomenclature, its chronic-relapsing natural history and the high risk of cognitive impairment associated with it47. In the context of CTA, our findings are consistent with those of Gil and colleagues, who investigated the impact of specific types of childhood adversity on functional capacity in schizophrenia. They found a significant correlation between disability in schizophrenia and experiences of physical neglect and emotional abuse. Particularly notable was the strong association between functional outcome and physical neglect48. What had not been sufficiently explored before is the association between different levels of AS and CTA. Although our study provides cross-sectional data and does not track changes in AS over time, it is conceptualized that AS could vary similarly to other clinical and psychopathological variables, such as the number of relapses, hospitalizations, and symptomatology (e.g., positive, negative and general). Future longitudinal studies would be necessary to explore how AS changes over time and its relationship to these variables. The diminished cognitive engagement and emotional reactivity in Profile 4 may contribute to the reduced frequency of acute episodes, suggesting a state of cognitive impairment where the individual experiences less pronounced symptom fluctuations but continues to be affected by the long-term effects of prior trauma and ongoing cognitive impairment.
Finally, it is relevant to note how a clinical stratification of schizophrenia is not only desirable, to better characterize the syndrome, but also emerging in the literature. In fact, our results fit into a context of growing evidence regarding the characterization of schizophrenia in different phenotypic profiles based on gray matter volume, neurocognition, polygenic risk scores, and longitudinal functioning trajectories49,50.
While the innovative viewpoint presented in this research offers the potential for a more precise delineation of the existing clinical phenotyping of schizophrenia based on the interrelationships among childhood trauma, AS, and psychotic symptomatology, it is crucial to consider several limitations when interpreting these findings, which make it difficult to generalize the results to the entire population with schizophrenia.
First, the retrospective nature and self-report modality of CTQ and ASI may be influenced by recall biases, which could compromise accuracy and validity, thus influencing the observed number of profiles. However, this limitation is partially addressed by studies showing a strong validity of these instruments even in populations affected by schizophrenia and with a long history of illness37.
Secondly, our sample consisted of individuals undergoing antipsychotic treatments. While this adheres to clinical standards and international treatment guidelines and evidence51, it could potentially affect the expression and associations between AS and positive/negative symptoms. Thus, to attain a more comprehensive understanding, it is advisable to replicate our findings in a drug-naïve sample, preferably at the onset of the disorder or within an at-high-risk population35,52, in order to mitigate this potential bias. Third, the cross-sectional nature of the current study precludes adequate interpretation of the derived clinical profiles on temporal stability, illness trajectory, or outcomes of symptomatology in schizophrenia. Future research should employ a longitudinal approach, allowing for profile stability assessment, assessment of premorbid adjustment profile stability, and prediction of covariates using latent transition analysis (LTA). Lastly, it is unclear whether clinical profiles simply reflect a linear severity continuum or if they represent distinct variations in a subset of individuals that correspond to different underlying biological mechanisms, trajectories, or prognoses.
The implications of the study have significant relevance for clinical practice. On one hand, these findings align with prior research, suggesting that the diagnosis of schizophrenia alone does not allow us to understand the broad clinical and phenotypic complexity of this disorder, which may present completely different pictures53–55. Our results also emphasize the importance of reinforcing social adjustment during the prodromal phase to improve patients’ subjective disorder assessment. Social adjustment during this critical phase can significantly influence how individuals perceive and interpret their early symptoms, which may affect their willingness to seek help and adhere to treatment. Establishing stronger social connections and support systems early on can help patients gain a clearer understanding of their condition, thereby minimizing the risk misinterpretation or denial of symptoms56,57.
Moreover, building profiles based on clinical features may help better identify the pharmacological, psychosocial, psychotherapeutic or cognitive rehabilitation treatment needs of individuals diagnosed with schizophrenia or from socio-health contexts with limited resources for the treatment of mental disorders, thus moving towards an individualization of diagnosis and therapy.
Conclusion
Subtyping individuals with schizophrenia based on AS has identified four distinct profiles: one characterized by less-impaired global phenotype in adults (Profile 1), another by early onset and severe symptomatology (Profile 2), a third by intermediate AS symptoms and correlations to sexual abuse (Profile 3), and a fourth with an almost chronic trend (Profile 4). It is interesting to note that a modern statistical approach like LPA, based on psychopathological features, results in a clinical stratification reminiscent of the different subtypes of schizophrenia present up to DSM-IV-TR (i.e., paranoid, disorganized/hebephrenic, catatonic, undifferentiated, and residual types). This study has paved the way for a new understanding of the role of AS in the clinical phenotyping of patients with schizophrenia, revealing the existence of different clinical subtypes and their associations with childhood trauma experiences and symptoms. Future studies should investigate whether the four different identified profiles also correlate with diverse treatment outcomes.
Acknowledgements
The authors express gratitude to the participants who took part in the study.
Author contributions
Matteo Aloi: Conceptualization; methodology; writing – original draft; writing – review and editing. Renato de Filippis: Data curation; writing – original draft; writing – review and editing. Elvira Anna Carbone: Data curation; writing – review and editing. Marianna Rania: Data curation; writing – review and editing. Angela Bertua: Data curation; writing – review and editing. Marisa Golia: Data curation; writing – review and editing. Rosina Nicoletta: Data curation; writing – review and editing. Cristina Segura-Garcia: Supervision; writing – review and editing. Pasquale De Fazio: Supervision; writing – review and editing.
Data availability
The data that support the findings of this study are available on request from the corresponding author.
Competing interests
In the last three years, Dr. de Filippis has received speaker fee from Angelini, Janssen Pharmaceutica and Lundbeck, and travel support from Janssen Pharmaceutica, Lundbeck, Otsuka and ROVI Pharma Industrial Services. All other authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kahnt, T. & Tobler, P. N. Reward, Value, and Salience. Decis. Neurosci., 2017, 109–120 (2017).
- 2.Kapur, S. Psychosis as a state of aberrant salience: a framework linking biology, phenomenology, and pharmacology in schizophrenia. Am. J. Psychiatry160, 13–23 (2003). [DOI] [PubMed] [Google Scholar]
- 3.Pugliese, V. et al. Aberrant salience correlates with psychotic dimensions in outpatients with schizophrenia spectrum disorders. Ann. Gen. Psychiatry21, 25 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kapur, S. How antipsychotics become anti-‘psychotic’ – from dopamine to salience to psychosis. Trends Pharm. Sci.25, 402–406 (2004). [DOI] [PubMed] [Google Scholar]
- 5.Van Os, J. Salience syndrome’ replaces ‘schizophrenia’ in DSM‐V and ICD‐11: psychiatry’s evidence‐based entry into the 21st century? Acta Psychiatr. Scand.120, 363–372 (2009). [DOI] [PubMed] [Google Scholar]
- 6.Hengartner, M. P. & Moncrieff, J. Inconclusive Evidence in Support of the Dopamine Hypothesis of Psychosis: Why Neurobiological Research Must Consider Medication Use, Adjust for Important Confounders, Choose Stringent Comparators, and Use Larger Samples. Front. Psychiatry9, 10.3389/fpsyt.2018.00174 (2018). [DOI] [PMC free article] [PubMed]
- 7.Moncrieff, J. A Critique of the Dopamine Hypothesis of Schizophrenia and Psychosis. Harv. Rev. Psychiatry17, 214–225 (2009). [DOI] [PubMed] [Google Scholar]
- 8.Lau, C.-I., Wang, H.-C., Hsu, J.-L., & Liu, M.-E. Does the dopamine hypothesis explain schizophrenia? Rev. Neurosci.24, 10.1515/revneuro-2013-0011 (2013). [DOI] [PubMed]
- 9.Mallikarjun, P. K. et al. Aberrant salience network functional connectivity in auditory verbal hallucinations: a first episode psychosis sample. Transl. Psychiatry8, 69 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Palaniyappan, L. & Liddle, P. F. Does the salience network play a cardinal role in psychosis? An emerging hypothesis of insular dysfunction. J. Psychiatry Neurosci.37, 17–27 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Varese, F. et al. Childhood Adversities Increase the Risk of Psychosis: A Meta-analysis of Patient-Control, Prospective- and Cross-sectional Cohort Studies. Schizophr. Bull.38, 661–671 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McCutcheon, R. A., Bloomfield, M. A. P., Dahoun, T., Mehta, M. & Howes, O. D. Chronic psychosocial stressors are associated with alterations in salience processing and corticostriatal connectivity. Schizophr. Res.213, 56–64 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stahl, S. M. Stahl’s Essential Psychopharmacology (Cambridge University Press; 2021) 10.1017/9781108975292.
- 14.Carbone, E. A., et al. Adverse childhood experiences and clinical severity in bipolar disorder and schizophrenia: A transdiagnostic two-step cluster analysis. J. Affect Disord.259, 10.1016/j.jad.2019.08.049 (2019). [DOI] [PubMed]
- 15.Bruni, A. et al. Childhood adversities are different in Schizophrenic Spectrum Disorders, Bipolar Disorder and Major Depressive Disorder. BMC Psychiatry18, 391 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Os, J. & Reininghaus, U. Psychosis as a transdiagnostic and extended phenotype in the general population. World Psychiatry15, 118–124 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van Os, J. et al. Evidence, and replication thereof, that molecular-genetic and environmental risks for psychosis impact through an affective pathway. Psychol. Med.52, 1910–1922 (2022). [DOI] [PubMed] [Google Scholar]
- 18.Pugliese, V., et al. Cognitive biases are associated with aberrant salience experience in schizophrenia spectrum disorders. Spanish J. Psychiatry Ment. Heal.10.1016/j.sjpmh.2023.07.001 (2023). [DOI] [PubMed]
- 19.De Fazio, P., Pugliese, V., Cattolico, M., Aloi, M. & Segura-Garcia, C. The relationship between childhood trauma and aberrant salience: a preliminary study in patients with Schizophrenia. J. Psychopathol.26, 28–35 (2020). [Google Scholar]
- 20.Muscatello, M. R. A. et al. The wounds of childhood: Early trauma subtypes, salience and hyperarousal in a sample of adult psychiatric patients. Int. J. Soc. Psychiatry66, 3–9 (2020). [DOI] [PubMed] [Google Scholar]
- 21.Gibson, W. A. Three multivariate models: Factor analysis, latent structure analysis, and latent profile analysis. Psychometrika24, 229–252 (1959). [Google Scholar]
- 22.Lazarsfeld, P. F. & Henry, N. W. Latent Structure Analysis (Houghton Mifflin; 1968).
- 23.Williams, G. A. & Kibowski, F. Latent class analysis and latent profile analysis. In: Handbook of Methodological Approaches to Community-Based Research Qualitative, Quantitative, and Mixed Methods, (eds Jason, L. A. & Glenwick, D. S.) 143–151 (Oxford University Press, 2016).
- 24.American Association Psychiatric. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®), 5th ed. (American Psychiatric Association; 2013). 10.1176/appi.books.9780890425596.744053.
- 25.First, M.B., Williams, J.B.W., Karg, R.S., Spitzer, R.L. Structured Clinical Interview for DSM-5 Disorders, Clinician Version (SCID-5-CV) . Arlington, VA, American Psychiatric Association (2016).
- 26.World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA310, 2191 (2013). [DOI] [PubMed] [Google Scholar]
- 27.Gardner, D. M., Murphy, A. L., O’Donnell, H., Centorrino, F. & Baldessarini, R. J. International consensus study of antipsychotic dosing. Am. J. Psychiatry167, 686–693 (2010). [DOI] [PubMed] [Google Scholar]
- 28.Cicero, D. C., Kerns, J. G. & McCarthy, D. M. The Aberrant Salience Inventory: A New Measure of Psychosis Proneness. Psychol. Assess.22, 688–701 (2010). [DOI] [PubMed] [Google Scholar]
- 29.Raballo, A., Scanu, R., Petretto, D. R. & Preti, A. Aberrant salience and psychosis risk symptoms in Italian undergraduate students: Further validation of the Aberrant Salience Inventory. Early Inter. Psychiatry8, 134 (2014). [Google Scholar]
- 30.Innamorati, M. et al. Factorial validity of the Childhood Trauma Questionnaire in Italian psychiatric patients. Psychiatry Res.245, 297–302 (2016). [DOI] [PubMed] [Google Scholar]
- 31.Kay, S. R., Fiszbein, A. & Opler, L. A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull.13, 261–276 (1987). [DOI] [PubMed] [Google Scholar]
- 32.Rosenberg, J., Beymer, P., Anderson, D., van Lissa, C. J. & Schmidt, J. tidyLPA: An R Package to Easily Carry Out Latent Profile Analysis (LPA) Using Open-Source or Commercial Software. J. Open Source Softw.3, 978 (2018). [Google Scholar]
- 33.Ramaswamy, V., Desarbo, W. S., Reibstein, D. J. & Robinson, W. T. An Empirical Pooling Approach for Estimating Marketing Mix Elasticities with PIMS Data. Mark. Sci.12, 103–124 (1993). [Google Scholar]
- 34.Nylund-Gibson, K. & Choi, A. Y. Ten frequently asked questions about latent class analysis. Transl. Issues Psychol. Sci.4, 440–461 (2018). [Google Scholar]
- 35.Lisi, G. et al. Aberrant salience in adolescents is related to indicators of psychopathology that are relevant in the prodromal phases of psychosis. Early Inter. Psychiatry15, 856–864 (2021). [DOI] [PubMed] [Google Scholar]
- 36.Bromberg-Martin, E. S., Matsumoto, M. & Hikosaka, O. Dopamine in Motivational Control: Rewarding, Aversive, and Alerting. Neuron68, 815–834 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.de Filippis, R. et al. Aberrant salience mediates the interplay between emotional abuse and positive symptoms in schizophrenia. Compr. Psychiatry133, 152496 (2024). [DOI] [PubMed] [Google Scholar]
- 38.Ballerini, A. et al. Aberrant salience relationship with first rank symptoms. Ann. Gen. Psychiatry21, 8 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sánchez-Torres, A. M. et al. Relapse, cognitive reserve, and their relationship with cognition in first episode schizophrenia: a 3-year follow-up study. Eur. Neuropsychopharmacol.67, 53–65 (2023). [DOI] [PubMed] [Google Scholar]
- 40.Siafis, S. et al. Relapse in clinically stable adult patients with schizophrenia or schizoaffective disorder: evidence-based criteria derived by equipercentile linking and diagnostic test accuracy meta-analysis. Lancet Psychiatry11, 36–46 (2024). [DOI] [PubMed] [Google Scholar]
- 41.Emsley, R., Chiliza, B., Asmal, L. & Harvey, B. H. The nature of relapse in schizophrenia. BMC Psychiatry13, 50 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hailes, H. P., Yu, R., Danese, A. & Fazel, S. Long-term outcomes of childhood sexual abuse: an umbrella review. Lancet Psychiatry6, 830–839 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chen, L. P. et al. Sexual abuse and lifetime diagnosis of psychiatric disorders: systematic review and meta-analysis. Mayo Clin. Proc.85, 618–629 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bebbington, P. Childhood sexual abuse and psychosis: aetiology and mechanism. Epidemiol. Psichiatr Soc.18, 284–293 (2009). [PubMed] [Google Scholar]
- 45.Morrison, A. P. A cognitive behavioural perspective on the relationship between childhood trauma and psychosis. Epidemiol. Psichiatr Soc.18, 294–298 (2009). [PubMed] [Google Scholar]
- 46.Whiffen, V. E. & Macintosh, H. B. Mediators of the link between childhood sexual abuse and emotional distress: a critical review. Trauma Violence Abus.6, 24–39 (2005). [DOI] [PubMed] [Google Scholar]
- 47.Harding, C. M., Zubin, J. & Strauss, J. S. Chronicity in schizophrenia: fact, partial fact, or artifact? Hosp. Community Psychiatry38, 477–486 (1987). [DOI] [PubMed] [Google Scholar]
- 48.Gil, A. et al. The association of child abuse and neglect with adult disability in schizophrenia and the prominent role of physical neglect. Child Abus. Negl.33, 618–624 (2009). [DOI] [PubMed] [Google Scholar]
- 49.Koutsouleris, N., et al. Distinct multimodal biological and functional profiles of symptom-based subgroups in recent-onset psychosis. Res. Sq.10.21203/rs.3.rs-3949072/v1 (2024).
- 50.de Filippis, R., et al. Applying a clinical staging model in patients affected by Schizophrenia Spectrum Disorder. Front. Psychiatry15, 1387913 (2024). [DOI] [PMC free article] [PubMed]
- 51.de Filippis, R. et al. Current and emerging long-acting antipsychotics for the treatment of schizophrenia. Expert Opin. Drug Saf.20, 771–790 (2021). [DOI] [PubMed] [Google Scholar]
- 52.Raballo, A. et al. Tracking salience in young people: A psychometric field test of the Aberrant Salience Inventory (ASI). Early Inter. Psychiatry13, 64–72 (2019). [DOI] [PubMed] [Google Scholar]
- 53.Gratton, C. & Mittal, V. A. Embracing the Complexity of Heterogeneity in Schizophrenia: A New Perspective From Latent Clinical-Anatomical Dimensions. Schizophr. Bull.46, 1337–1338 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ahmed, A. O., Strauss, G. P., Buchanan, R. W., Kirkpatrick, B. & Carpenter, W. T. Schizophrenia heterogeneity revisited: Clinical, cognitive, and psychosocial correlates of statistically-derived negative symptoms subgroups. J. Psychiatr. Res.97, 8–15 (2018). [DOI] [PubMed] [Google Scholar]
- 55.Misiak, B. et al. Toward a unified theory of childhood trauma and psychosis: A comprehensive review of epidemiological, clinical, neuropsychological and biological findings. Neurosci. Biobehav. Rev.75, 393–406 (2017). [DOI] [PubMed] [Google Scholar]
- 56.van Os, J., Guloksuz, S., Vijn, T. W., Hafkenscheid, A. & Delespaul, P. The evidence‐based group‐level symptom‐reduction model as the organizing principle for mental health care: time for change? World Psychiatry18, 88–96 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yung, A. R. & McGorry, P. D. The Prodromal Phase of First-episode Psychosis: Past and Current Conceptualizations. Schizophr. Bull.22, 353–370 (1996). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.