Video
Introduction
Pancreaticoduodenectomy (Whipple) is a complex surgery associated with significant postoperative morbidity ranging from 30% to 60%. Delayed gastric emptying and bile reflux gastritis are well-known problems in long-term survivors. In particular, refractory, severe bile acid reflux following Whipple is challenging to manage.1,2 Surgical interventions like Roux-en-Y reconstruction, Billroth II, and Braun enteroenterostomy have been shown to overcome bile reflux for those who have already failed medical and lifestyle modification.3 We present the first case demonstrating the successful management of refractory bile acid reflux in a patient following Whipple with an EUS-guided Braun enteroenterostomy (anastomosis between the afferent and efferent limbs).
Case
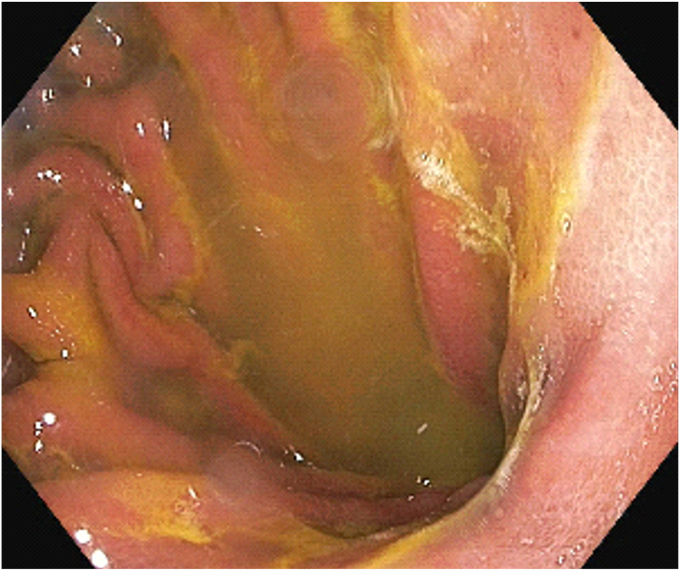
A 63-year-old female with a history of chronic pancreatitis and pancreatic head mass of unclear etiology status following a robotic-assisted Whipple procedure 3 years prior presented with severe persistent nausea and bilious emesis since surgery. An upper endoscopy showed a sliding hiatal hernia with Los Angeles (LA) grade B reflux esophagitis and diffuse bile acid gastropathy with a large amount of bile pooled in the stomach (Fig. 1). Her symptoms were refractory to lifestyle modifications and multiple medications, including antacids, maximal dose of proton pump inhibitors, cholestyramine, and antiemetics like ondansetron and promethazine, all of which were unsuccessful in controlling her symptoms. After a multidisciplinary discussion, a decision was made to pursue an EUS-guided enteroenterostomy as an alternative to surgical Braun enteroenterostomy because of the patient’s reluctance to undergo another surgery.
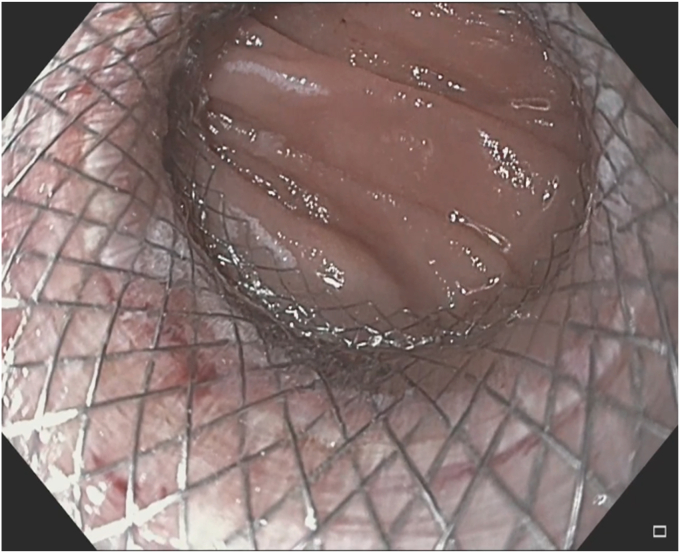
Figure 1.
Diffuse bile acid gastropathy with a large amount of bile pooled in the gastric cavity.
Method
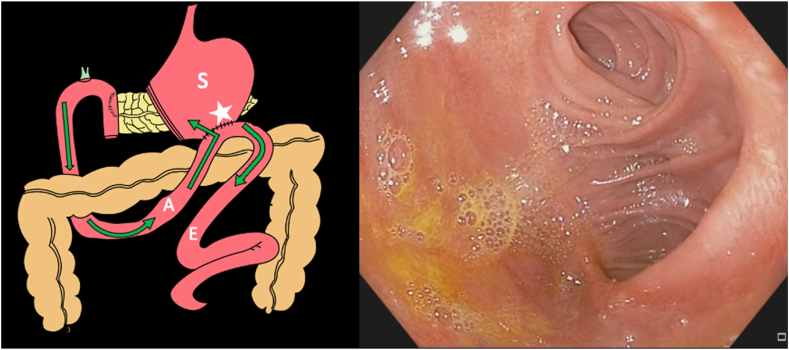
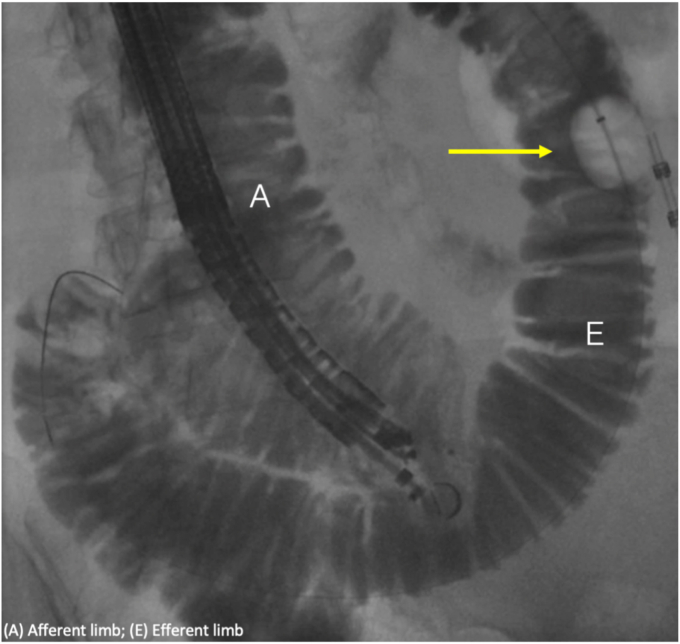
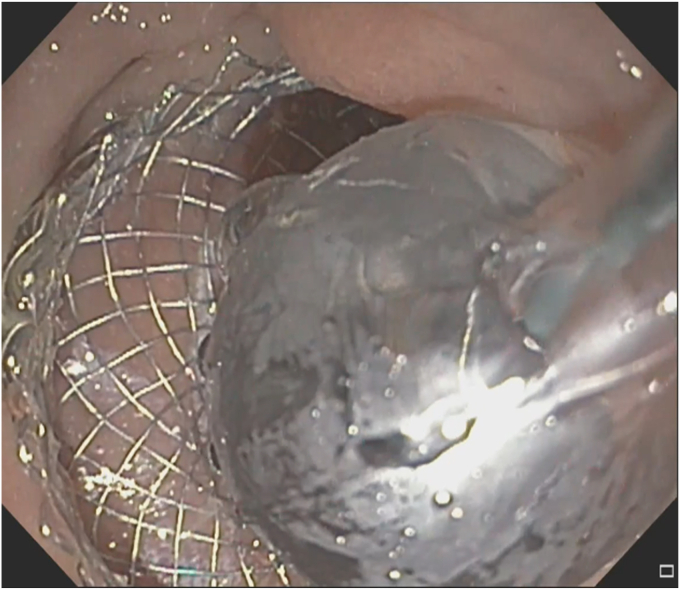
A Whipple anatomy with gastro-jejunal anastomosis was visualized on endoscopy (Fig. 2; Video 1, available online at www.videogie.org). The pancreatico-biliary (PB) limb (afferent limb) and an efferent limb were identified. A small bowel follow-through was performed. Under endoscopic and fluoroscopic guidance, a 15- to 18-mm extraction balloon was passed into the efferent limb, and a mixture of contrast and sterile water was flushed into the small bowel for identification and distention of the efferent limb (Video 1). EUS was then introduced into the PB limb, and using EUS and fluoroscopic visualization a loop of distended small bowel was identified in the efferent limb (Fig. 3). Once an adequate position without intervening vessels was identified, a 20- × 10-mm lumen-apposing metal stent (LAMS) with a cautery enhanced tip was placed from the PB limb into the efferent limb creating an anastomosis. The LAMS was then dilated using a through-the-scope dilation balloon for better visualization of the patent anastomosis (Figs. 4 and 5).
Figure 2.
Depiction of a post-Whipple surgical anatomy, with green arrows representing the flow of bile acid from the liver (not pictured) (left). The endoscopic view of the opening of the afferent and efferent limbs as seen from the stomach (right). A, Afferent limb; E, efferent limb; S, stomach; star, gastrojejunal anastomosis that defines the separation point between the 2 limbs.
Figure 3.
Fluoroscopic imaging showing the biliary extraction balloon at the tip of the yellow arrow, the efferent limb, the EUS endoscope intubating the afferent limb, and the easier angulation angle of the afferent compared to the efferent limbs. A, Afferent limb; E, efferent limb.
Figure 4.
Dilation of the lumen-apposing metal stent to 15 mm using a through-the-scope dilation balloon after placement.
Figure 5.
Endoscopic visualization of the fully dilated patent lumen-apposing metal stent seen from the afferent into the efferent limb.
The postoperative course was uneventful, and the patient was discharged home the same day. The patient's symptoms of bilious emesis and nausea improved significantly following the procedure. The LAMS was removed after 6 months. Follow-up endoscopy at 9 months revealed a patent enteroenterostomy with continued resolution of symptoms related to bile reflux (Fig. 6). Repeat endoscopy 18 months following LAMS removal showed a persistently patent fistula without evidence of closure. Further repeat endoscopies will only be scheduled if the patient begins to develop new bile acid reflux symptoms.
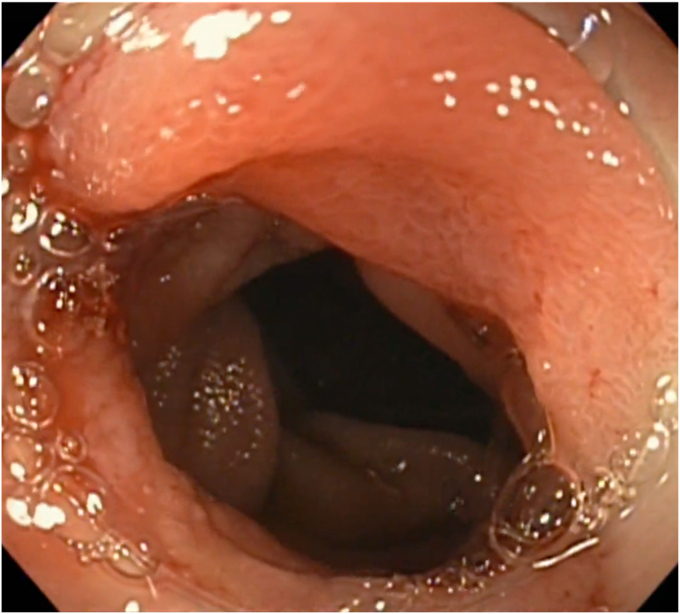
Figure 6.
Patent enteroenterostomy following lumen-apposing metal stent removal 9 months following deployment.
Discussion
Our case highlights the use of an EUS-guided enteroenterostomy as a minimally invasive endoscopic alternative to Braun enteroenterostomy to manage severe, intractable bile reflux after Whipple surgery. Although medical and lifestyle modifications are used commonly in the management of bile acid reflux, for intractable cases, surgical interventions are often pursued. While effective in improving bile acid reflux, these surgical procedures have an inherent risk of prolonged structural adverse events in up to 30% of cases and nonnegligible morbidity and mortality rates associated with an irreversible intervention.4 Endoscopic Braun enteroenterostomy is a promising alternative to surgical procedures, especially in patients who are poor candidates or refuse surgery. However, further larger studies are needed to study the efficacy and safety of these interventions.
Disclosure
The authors disclosed no financial relationships relevant to this publication.
Supplementary data
Endoscopic Braun enteroenterostomy for the management of severe bile acid reflux following Whipple surgery.
References
- 1.Gong E.J., Park C.H., Jung D.H., et al. Efficacy of endoscopic and surgical treatments for gastroesophageal reflux disease: a systematic review and network meta-analysis. J Pers Med. 2022;12:621. doi: 10.3390/jpm12040621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Karim S.A.M., Abdulla K.S., Abdulkarim Q.H., Rahim F.H. The outcomes and complications of pancreaticoduodenectomy (Whipple procedure): cross sectional study. Int J Surg. 2018;52:383–387. doi: 10.1016/j.ijsu.2018.01.041. [DOI] [PubMed] [Google Scholar]
- 3.Siriwardana R.C., Lokubandara R.W.M.A., De Silva Hewavisenthi S.J., Liyanage S.K., Jayatunge D.S.P., Liyanage C.A.H. Quality of life and impact of bile reflux after retro colic retro gastric gastrojejunostomy in Whipple surgery. BMC Gastroenterol. 2017;17:19. doi: 10.1186/s12876-017-0573-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yadlapati R., Hungness E.S., Pandolfino J.E. Complications of antireflux surgery. Am J Gastroenterol. 2018;113:1137–1147. doi: 10.1038/s41395-018-0115-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Endoscopic Braun enteroenterostomy for the management of severe bile acid reflux following Whipple surgery.