Video
Case presentation
A 67-year-old man presented to another hospital with acute necrotizing pancreatitis due to long-term alcohol use. Magnetic resonance imaging and MRCP showed a 15-cm acute pancreatic fluid collection (PFC). The patient improved with conservative treatment and was discharged. Two weeks later, he returned with abdominal pain, vomiting, and abdominal distention. CT of the abdomen and pelvis revealed a 19 × 13-cm volume of fluid containing multiple foci of gas with mass effect on the stomach. The patient received antibiotics and a left upper quadrant percutaneous drain. Serial abscessograms over the next few months showed complete collapse of the pseudocyst. Drain output remained persistent, with up to 100 to 150 mL of clear fluid every day. The patient was referred to our institution for treatment of pancreaticocutaneous fistula.
Procedure/endoscopic method
The main steps of the endoscopic procedure are outlined in Figure 1. On initial endoscopic retrograde cholangiopancreatogram, only superficial cannulation could be performed because of the location of the major papilla on the rim of a diverticulum (Figs. 2 and 3). An attempt at rendezvous maneuver was performed with endoscopic ultrasound-guided puncture of the upstream pancreatic duct (PD) via a transgastric approach (Fig. 4). A 19-gauge access needle (Cook Medical, Bloomington, Ind, USA) was used to puncture the PD in the body, after which a contrast was injected. Next, a pancreatogram was obtained, which showed complete disruption of the PD in the mid body (Fig. 5). The abrupt cutoff of the PD confirmed complete PD disruption, and a 0.035-inch wire failed to pass through the disruption.
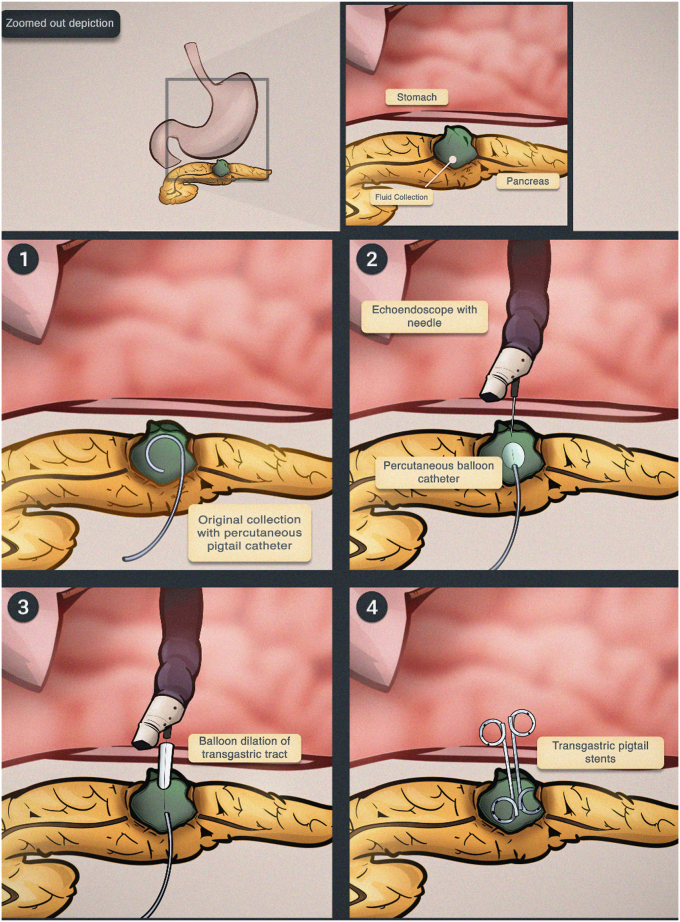
Figure 1.
Graphic illustration of the main steps of the endoscopic techniques used in this case.
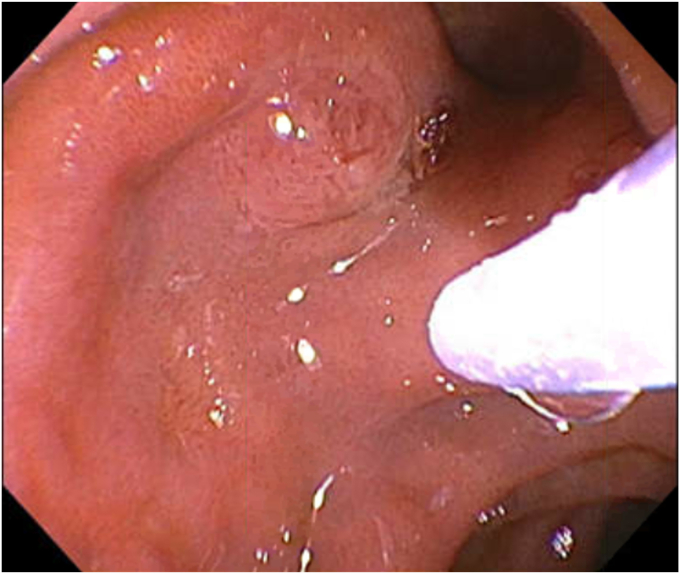
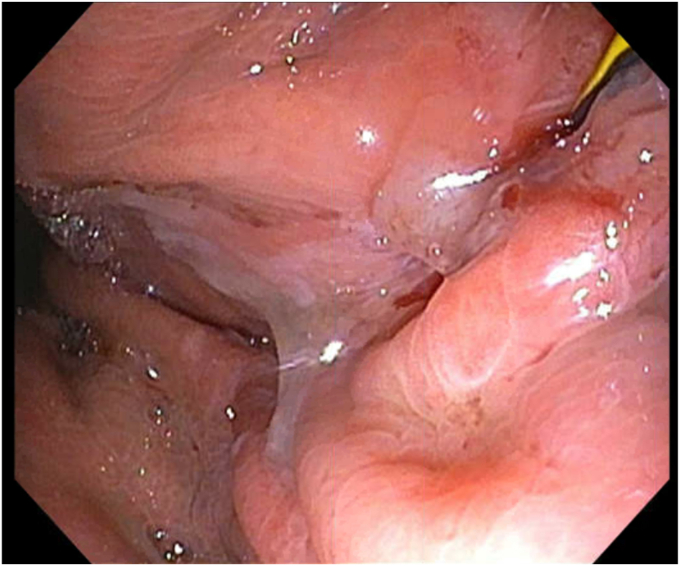
Figure 2.
A major papilla can be seen at the rim of a diverticulum.
Figure 3.
On initial endoscopic retrograde cholangiopancreatogram, only superficial cannulation could be performed.
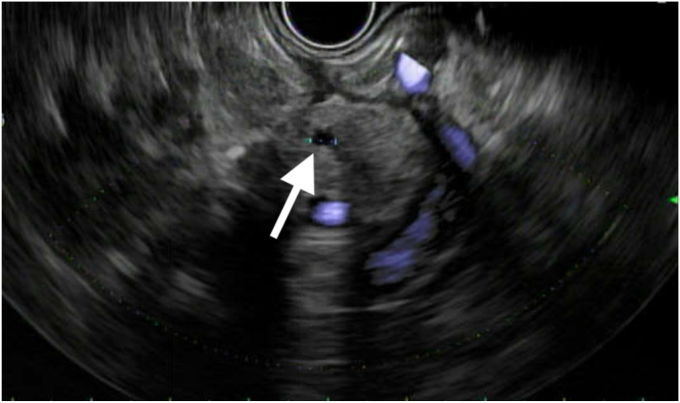
Figure 4.
EUS showing the upstream nondilated pancreatic duct (solid arrow) before attempting to cannulate via a transgastric approach.
Figure 5.
The fluoroscopic view shows the EUS-guided puncture of the pancreatic duct in the mid-body where contrast injection illustrates a complete pancreatic duct disruption (solid arrow).
Pancreaticogastrostomy or pancreatic tail resection was considered, but given the morbidity associated with those approaches, a hybrid procedure using EUS and a percutaneous approach was planned in collaboration with interventional radiology (IR). The percutaneous pigtail drain was identified within the fistula tract using the linear array echoendoscope. Contrast was injected through the drain, demonstrating a 19-mm residual collection with fistula to the main PD in the body and tail (Fig. 6). The percutaneous drain was removed over 2 stiff hydrophilic coated guidewires (GLIDEWIRE; Terumo, Tokyo, Japan). A Fogarty balloon catheter (Edwards Lifesciences, Irvine, Calif, USA) and an endovascular snare catheter (Merit, South Jordan, Utah, USA) were advanced over both wires into the residual peripancreatic collection. The balloon was inflated as a target for needle puncture. The stomach wall and the balloon within the fistula were punctured under endosonographic guidance with a 19-gauge access needle. A long 0.035-inch stiff guidewire (Jagwire; Boston Scientific, Marlborough, Mass, USA) was inserted through the needle into the fistula cavity under fluoroscopic guidance (Fig. 7). The wire was captured by the IR staff using the snare and pulled out through the abdominal wall in a rendezvous style (Fig. 8). A 6F flexor sheath (Cook Medical) was advanced over the wire and through the gastric wall to the gastric lumen, in which a second 0.035-inch stiff guidewire (Jagwire) was advanced through the sheath and snared by the endoscopist for through-and-through access (Fig. 9). The transgastric tract was dilated with an 8-mm balloon dilator (after docking with the flexor sheath to ease passage across the gastric wall), and two 4-cm, 7F double-pigtail stents were then placed into the fistula cavity through the newly dilated tract using a 7F pushing catheter over each of the 2 wires (Fig. 10). The endoscope was withdrawn, and the procedure was completed (Video 1, available online at www.videogie.org).
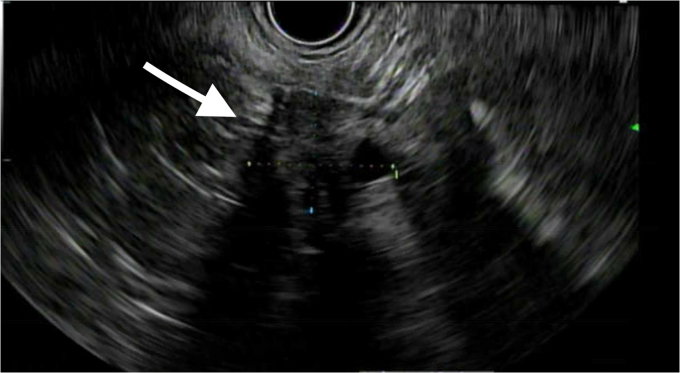
Figure 6.
EUS image showing the residual fluid collection (solid arrow).
Figure 7.
The figure shows a long 0.035-inch stiff guidewire (Jagwire) that was inserted through the 19-gauge access needle (not visible in this image) into the fistula cavity.
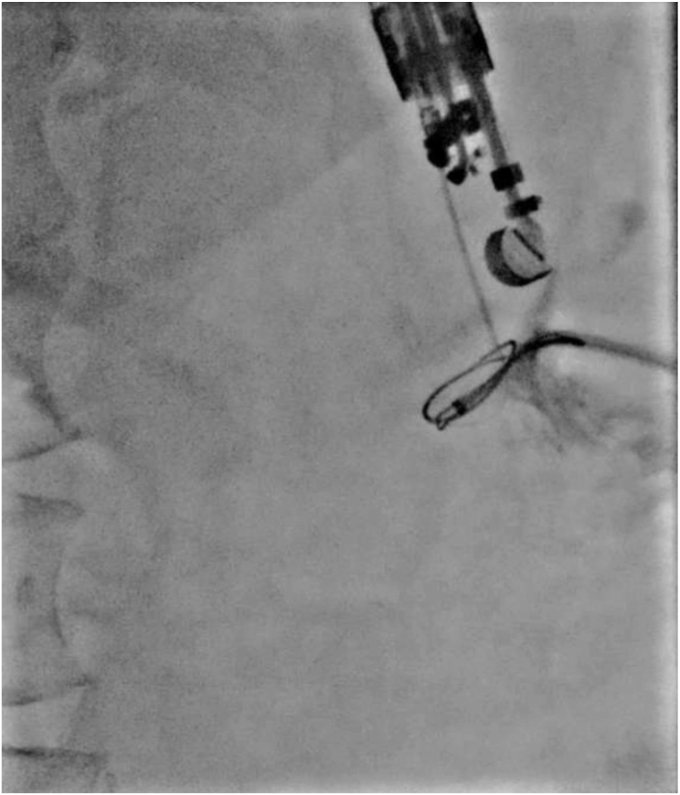
Figure 8.
Fluoroscopic view shows the 0.035-inch stiff guidewire (Jagwire) that was captured by IR team using an endovascular snare to pull out via the abdominal wall (not visible in this image).
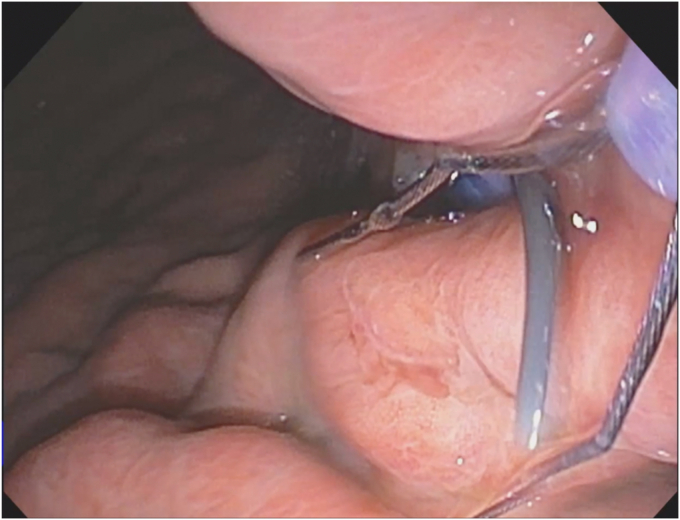
Figure 9.
A second 0.035-inch stiff guidewire (Jagwire) was advanced through the sheath into the gastric lumen to be snared via the endoscope with a plan to pull it out orally (not shown in this image).
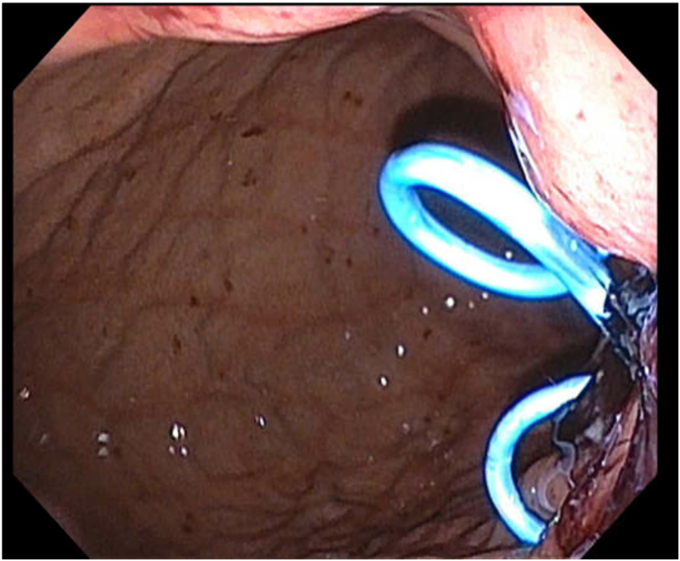
Figure 10.
Two 4-cm, 7F double-pigtail stents (cystogastrostomy catheters) were placed into the fistula cavity.
Outcome
The patient reported no further percutaneous drainage over the next 6 months. These stents will remain in situ without any planned removal and were seen to be in a good position on the plain abdominal x-ray, obtained 2 months later (Fig. 11).
Figure 11.
An abdominal x-ray obtained 2 months later confirmed the cystogastrostomy stents in a good position.
Discussion, conclusion, and clinical implications
Disconnected PD syndrome is a challenging clinical scenario, but it can be managed endoscopically in most cases.1,2 Endoscopic transmural drainage of the resulting PFC can provide definitive therapy by allowing passage of fluid across a transmural tract.3,4 Transmural drainage also obviates the need for percutaneous drainage of PFCs in disrupted PD syndrome.5
Disclosure
None of the authors have any disclosures to make.
Supplementary data
This video demonstrates a case of disrupted PD with pancreaticocutaneous fistula after percutaneous pseudocyst drain. The steps of a hybrid endoscopic and interventional radiology approach to convert to internal drainage with transgastric stents are outlined.
References
- 1.Kozarek R. Endoscopic therapy of complete and partial pancreatic duct disruptions. Gastrointest Endosc Clin N Am. 1998;8:39–53. [PubMed] [Google Scholar]
- 2.Nadkarni N.A., Kotwal V., Sarr M.G., et al. Disconnected pancreatic duct syndrome: endoscopic stent or surgeon’s knife? Pancreas. 2015;44:16–22. doi: 10.1097/MPA.0000000000000216. [DOI] [PubMed] [Google Scholar]
- 3.Bakker O.J., van Santvoort H.C., van Brunschot S., et al. Endoscopic transgastric vs surgical necrosectomy for infected necrotizing pancreatitis: a randomized trial. JAMA. 2012;307:1053–1061. doi: 10.1001/jama.2012.276. [DOI] [PubMed] [Google Scholar]
- 4.Khan M.A., Kahaleh M., Khan Z., et al. Time for a changing of guard: from minimally invasive surgery to endoscopic drainage for management of pancreatic walled-off necrosis. J Clin Gastroenterol. 2019;53:81–88. doi: 10.1097/MCG.0000000000001141. [DOI] [PubMed] [Google Scholar]
- 5.Ross A.S., Irani S., Gan S.I., et al. Dual-modality drainage of infected and symptomatic walled-off pancreatic necrosis: long-term clinical outcomes. Gastrointest Endosc. 2014;79:929–935. doi: 10.1016/j.gie.2013.10.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video demonstrates a case of disrupted PD with pancreaticocutaneous fistula after percutaneous pseudocyst drain. The steps of a hybrid endoscopic and interventional radiology approach to convert to internal drainage with transgastric stents are outlined.