Abstract
Chronic low back pain (LBP) is a common musculoskeletal disorder and is often accompanied by functional leg length inequality (FLLI). However, little was known about the effects of gluteal muscle control training in patients with LBP and FLLI. This study was designed to investigate the effects of gluteal control training in patients with LBP and FLLI. This is a double-blinded, randomized controlled study design. Forty-eight LBP patients with FLLI were randomized to the gluteal control training (GT) (47.58 ± 9.42 years) or the regular training (RT) (47.38 ± 11.31 years) group and received allocated training for six weeks. The outcome measures were pelvic inclination (PI), ilium anterior tilt difference (IATD), FLLI, visual analogue scale (VAS), patient specific-functional scale (PSFS), Oswestry disability index (ODI), hip control ability, global rating of change scale (GRoC), and lower extremity strength and flexibility. The intervention effects were compared using two-way repeated measures analysis of variance and chi-square tests with α = 0.05. The results indicated that the GT group showed greater improvement (P < 0.01) in PI (1.03 ± 0.38∘ vs. 1.57 ± 0.51∘), IATD (0.68 ± 0.66∘ vs. 2.31 ± 0.66∘), FLLI (0.3 ± 0.22 vs. 0.59 ± 0.13 cm), VAS (1.41 ± 1.32 vs. 3.38 ± 1.51), hip control ability (2.20 ± 0.45 vs. 0.89 ± 0.74), GRoC at 3rd and 6th week as compared to the RT group. Hip strength and flexibility also improved more in the GT group (P < 0.05). In conclusion, gluteal control training was more effective in improving low back pain and dysfunctions, and should be integrated in the management plan in patients with LBP and FLLI.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-74348-x.
Keywords: Gluteal control training, Leg length inequality, Low back pain, Pelvic alignment
Subject terms: Pain management, Rehabilitation
Introduction
Chronic low back pain (CLBP) is a common musculoskeletal disorder that not only affects individuals’ physical function and daily lives but can also impact their psychological status and social functions1,2. Although various structural abnormalities have been identified contributing to the development of CLBP, mechanical LBP stands for more than 90% of all CLBP3. Different types of exercise intervention have been proposed for managing CLBP, and most research evidence showed that exercise intervention focusing on trunk muscle training would improve pain and disability associated with CLBP4–8.
Among factors associated with mechanical LBP, functional leg length inequality (FLLI) has been shown to relate to pelvic obliquity and rotational malalignment. Symmetrical pelvic alignment is essential for reducing the consequences of FLLI, and pelvic symmetry depends on precise control of the gluteal muscle groups and muscle balance in the pelvic girdle2,9–12. FLLI associated pelvic malalignment could lead to asymmetric mechanical forces and excessive load on the muscle tissues in the lumbar region, and thus cause pain, dysfunction as well as altered motor control in the lumbosacral region9–11,13.
Gluteal muscles play an important role in the force transmission from the lower extremities to the pelvic girdle and therefore supply pelvic stability and contribute support for the lumbar spine12,14–16. It has been shown that balanced gluteal muscle control is essential for pelvic symmetry2,9–12, and thus hip control training is particularly important in people with LBP and FLLI. Previous studies demonstrated that intervention targeted on the hip joint improved pain and disability in patients with CLBP14–19. However, most of these studies only focused on hip muscle strength training instead of hip motor control training, and none of these studies assessed the effect of gluteal muscle control training in the subgroup of patients who had both CLBP and FLLI.
The purpose of this study is to investigate whether gluteal control training, compared to regular training only, has better therapeutic effects in CLBP patients with FLLI. We hypothesized that gluteal control training would result in more improvement in pelvic alignment, FLLI, pain, and dysfunction.
Results
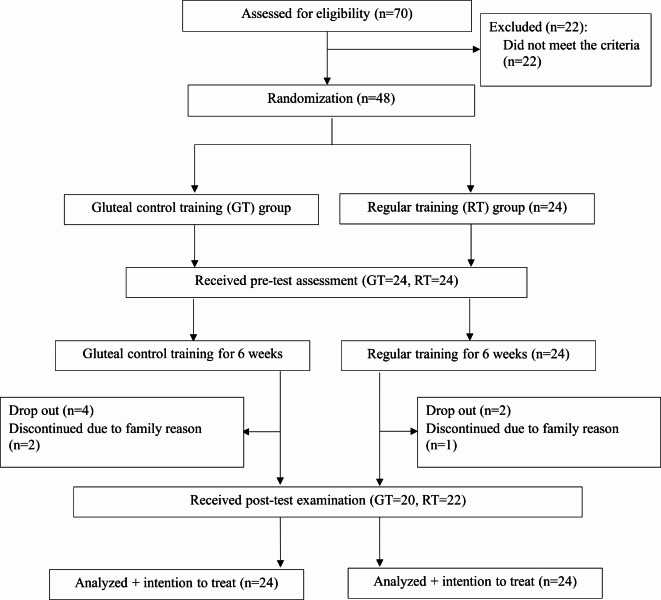
Recruitment of patients took place from December 2016 to May 2017. Forty-eight patients were recruited, four in the gluteus control training (GT) group, and two people in the regular training (RT) group dropped out of the study (Fig. 1). This study was originally designed to perform an intention-to-treat (ITT) analysis. To have a more comprehensive and robust evaluation of the treatment effects, the results of the per-protocol analysis were also described.
Fig. 1.
Flow chart of the study.
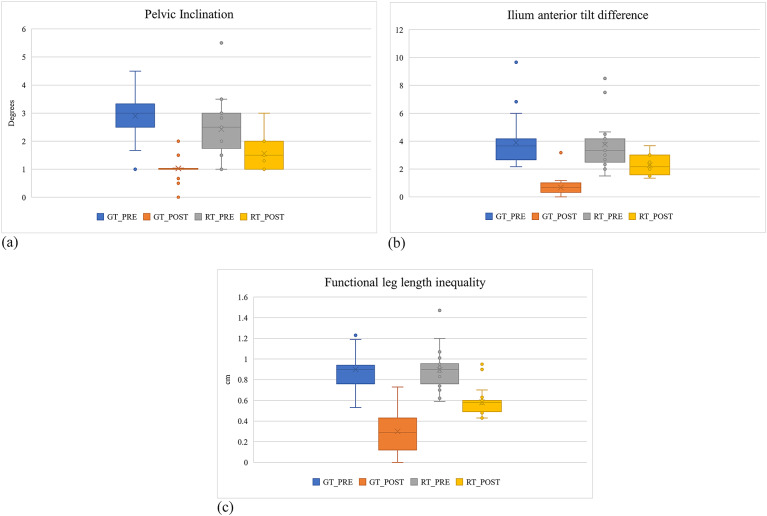
Intention to treat (ITT) analysis. For the ITT analysis, and the missing data were imputed using the group average values. Table 1 summarizes the basic data of the participants. There was no significant group difference at baseline. However, the pain duration seemed longer for the RT group (25 ± 19.52 months for the GT group, 38.58 ± 23.55 months for the RT group, p = 0.06). Table 2 and Fig. 2 summarize the comparisons of the pelvic alignment, FLLI, and hip control ability. After six weeks of training, significant time by group interactions were found for PI (pelvic inclination), FLLI, hip control ability (p < 0.001), and IATD (ilium anterior tilt difference) (p = 0.002), and significant time effects were found for all four variables with p < 0.001, indicating that both groups improved in pelvic alignment, functional leg length, and hip control ability; and gluteal control training was more effective in improving these variables.
Table 1.
Baseline characteristics (mean ± SD).
| GT N = 24 |
RT N = 24 |
P value | |
|---|---|---|---|
| Sex (male/female) | (10/14) | (11/13) | 0.77b |
| Age (years) | 47.58 ± 9.42 | 47.38 ± 11.31 | 0.27a |
| Height (cm) | 163.71 ± 9.77 | 163.71 ± 11.31 | 0.13a |
| Weight (kg) | 63.46 ± 10.65 | 64.81 ± 8.89 | 0.28a |
| BMI (weight/height2) | 23.59 ± 2.78 | 24.06 ± 2.22 | 0.69a |
| Recurrent times (times) | 3.63 ± 1.47 | 4.21 ± 1.31 | 0.37a |
| Pain duration (months) | 25 ± 19.52 | 38.58 ± 23.55 | 0.06a |
| Affected side match dominate side (ipsilateral/contralateral) | 10/14 | 9/15 | 0.77b |
Abbreviations: GT: gluteal control training; RT: regular training; BMI: body mass index.
aIndependent t test;b chi-square test.
Table 2.
Comparisons of pelvic alignment, functional leg length, and hip control ability before and after intervention (mean ± SD).
| Primary outcome | GT (N = 24) |
RT (N = 24) |
Time x group (p) | Time effect (p) | ||
|---|---|---|---|---|---|---|
| PRE | POST | PRE | POST | |||
| Pelvic alignment | ||||||
| PI (°)abc | 2.90 (0.74) | 1.03 (0.37) | 2.43 (1.07) | 1.56 (0.51) | 0.002* | < 0.001† |
| IATD (°)abc | 3.90 (1.75) | 0.67 (0.65) | 3.76 (1.78) | 2.27 (0.65) | 0.007* | < 0.001† |
| FLLI (cm)abc | 0.90 (0.20) | 0.30 (0.21) | 0.90 (0.19) | 0.58 (0.13) | < 0.001* | < 0.001† |
| Hip control ability abc | 3.75 (0.44) | 0.85 (0.67) | 3.76 (0.44) | 2.14 (0.64) | < 0.001* | < 0.001† |
GT: gluteal control training; RT: regular training; FLLI: functional leg length inequality; PI: pelvic inclination; IATD: ilium anterior tilt difference; PRE: pre-test; POST: post-test.
*Significant time x group interaction (p < 0.05) assessed by two-way repeated measures analysis of variance (ANOVA).
†Significant time effect (p < 0.05) assessed by two-way repeated measures ANOVA.
aSignificant between-group post-test differences (p < 0.05) assessed by multiple comparisons with Bonferroni correction.
bSignificant GT group pre-post differences (p < 0.05) assessed by multiple comparisons with Bonferroni correction.
cSignificant RT group pre-post differences (p < 0.05) assessed by multiple comparisons with Bonferroni correction.
Fig. 2.
Box-and-whisker plots of primary outcomes (GT_PRE: Gluteal training group pre-test, GT_POST: Gluteal training group post-test, RT_PRE: Regular training group pre-test, RT_POST: Regular training group post-test).
Tables 3 and 4 show the group comparisons in pain, function, and GRoC (Global Rating of Change). Both groups showed improvement in pain (VAS) and function (Oswestry Disability Index, ODI and Patient Specific Functional Scale, PSFS) (significant time effects, p < 0.05) after six weeks of training, with the GT group demonstrating significantly greater improvement when compared to the RT group (significant group by time interactions, p < 0.001). For GRoC, the GT group had a higher percentage of “significant improvement” in the overall change category compared to the RT group at the third week (p = 0.005) and sixth week (p = 0.02) (Table 4).
Table 3.
Comparisons of the pain scale and functional disability before and after intervention (mean ± SD).
| GT (N = 24) |
RT (N = 24) |
Time x group (p) | Time effect (p) | ||||
|---|---|---|---|---|---|---|---|
| PRE | POST | PRE | POST | ||||
| Pain scaleabc | VAS | 6.00 (1.28) | 1.30 (1.21) | 6.02 (1.04) | 3.44 (1.06) | < 0.001* | < 0.001† |
| Disability indexabc | ODI | 21.09 (10.00) | 7.51 (5.34) | 22.40 (7.85) | 12.15 (6.93) | 0.04* | < 0.001† |
| Functional scaleabc | PSFS | 4.94 (1.28) | 8.23 (1.18) | 4.42 (1.37) | 6.84 (1.39) | 0.013* | < 0.001† |
GT: gluteal control training; RT: regular training; VAS: visual analogue scale; ODI: Oswestry disability index; PSFS: patient specific functional scale; PRE: pre-test; POST: post-test.
* Significant time x group interaction (p < 0.05) assessed by two-way repeated measures analysis of variance (ANOVA).
† Significant time effect (p < 0.05) assessed by two-way repeated measures ANOVA.
a Significant between-group post-test differences (p < 0.05) assessed by multiple comparisons with Bonferroni correction.
b Significant GT group pre-post differences (p < 0.05) assessed by multiple comparisons with Bonferroni correction.
c Significant RT group pre-post differences (p < 0.05) assessed by multiple comparisons with Bonferroni correction.
Table 4.
Comparisons of the global rating of change scale (mean ± SD).
| GT (N = 21) |
RT (N = 21) |
p value | |
|---|---|---|---|
| Week 3 | |||
| Above 4 point | 17 | 9 | 0.005* |
| Less 4 point | 4 | 12 | |
| Week 6 | |||
| Above 4 point | 21 | 15 | 0.02* |
| Less 4 point | 0 | 6 | |
*p < 0.05 significant difference assessed using chi-square test.
The effects of intervention on lower extremity muscle strength and flexibility (affected side) are summarized in Tables 5 and 6. After six weeks of intervention, both groups showed improvement in muscle strength of hip musculatures (significant time effects with p ≤ 0.008) except the hip flexors. Compared to the RT group, the GT group had greater improvement in hip extensor, abductor, and adductor muscles strength (p = 0.033, 0.014, 0.008 respectively). After six weeks of intervention, both groups improved muscle flexibility of the hamstrings, iliotibial band, and rectus femoris of the affected side (significant time effects, p < 0.001) with greater improvement in the GT group (hamstrings p = 0.035, iliotibial band p = 0.004, rectus femoris p = 0.029).
Table 5.
Comparisons of the lower extremity muscle strength before and after intervention (kg) (mean ± SD).
| GT (N = 24) |
RT (N = 24) |
Time x group (p) | Time effect (p) | |||
|---|---|---|---|---|---|---|
| PRE | POST | PRE | POST | |||
| Hip extensorsbc | 8.90 (2.03) | 11.57 (2.25) | 9.17 (2.28) | 10.12 (3.12) | 0.033* | < 0.001† |
| Hip flexors | 13.15 (4.44) | 14.13 (2.97) | 12.24 (2.97) | 12.41 (2.48) | 0.46 | 0.091 |
| Hip abductorsbc | 7.77 (1.78) | 10.26 (2.20) | 8.00 (1.89) | 8.72 (2.08) | 0.014* | < 0.001† |
| Hip adductorsb | 7.78 (2.04) | 9.36 (2.12) | 8.53 (2.26) | 8.21 (2.19) | 0.008* | 0.008† |
| Hip external rotatorsbc | 7.34 (1.77) | 8.65 (2.01) | 7.21 (1.59) | 7.95 (1.74) | 0.24 | < 0.001† |
| Hip internal rotatorsb | 7.75 (1.98) | 8.73 (1.52) | 7.94 (1.94) | 8.59 (1.76) | 0.72 | 0.003† |
| Knee extensors | 19.63 (8.08) | 21.51 (6.44) | 21.25 (8.09) | 19.88 (6.22) | 0.07 | 0.41 |
Abbreviations: GT: gluteal control training; RT: regular training; PRE: pre-test; POST: post-test.
*Significant time x group interaction (p < 0.05) assessed by two-way repeated measures analysis of variance (ANOVA).
†Significant time effect (p < 0.05) assessed by two-way repeated measures ANOVA.
aSignificant between-group post-test differences (p < 0.05) assessed by multiple comparisons with Bonferroni correction.
bSignificant GT group pre-post differences (p < 0.05) assessed by multiple comparisons with Bonferroni correction.
cSignificant RT group pre-post differences (p < 0.05) assessed by multiple comparisons with Bonferroni correction.
Table 6.
Comparisons of lower extremity muscle flexibility before and after intervention (mean ± SD).
| GT (N = 24) |
RT (N = 24) |
Time x group (p) | Time effect (p) | |||
|---|---|---|---|---|---|---|
| PRE | POST | PRE | POST | |||
| Hamstring (°)b | 38.90 (9.25) | 46.64 (4.64) | 44.33 (10.38) | 47.49 (6.00) | 0.035* | < 0.001† |
| ITB (°)abc | 9.79 (4.15) | 16.66 (2.95) | 8.81 (3.39) | 12.71 (2.66) | 0.004* | < 0.001† |
| Rectus femoris (°)ab | 39.60 (9.23) | 45.30 (7.20) | 37.19 (7.64) | 39.22 (6.57) | 0.029* | < 0.001† |
GT: gluteal control training; RT: regular training; PRE: pre-test; POST: post-test.
*Significant time x group interaction (p < 0.05) assessed by two-way repeated measures analysis of variance (ANOVA).
†Significant time effect (p < 0.05) assessed by two-way repeated measures ANOVA.
aSignificant between-group post-test differences (p < 0.05) assessed by multiple comparisons with Bonferroni correction.
bSignificant GT group pre-post differences (p < 0.05) assessed by multiple comparisons with Bonferroni correction.
cSignificant RT group pre-post differences (p < 0.05) assessed by multiple comparisons with Bonferroni correction.
Per-protocol analysis. For the per-protocol analysis, the drop-out data were excluded from the data set, and the final analyses included 20 subjects in the GT group and 22 in the RT group. The comparisons of the baseline characteristics showed similar results to the ITT analysis except pain duration. After excluding the drop-outs, the pain duration was more comparable between the two groups (28.50 ± 20.68 months for the GT group, 36.64 ± 23.67 months for the RT groups, p = 0.62).
The results of the per-protocol analyses of the primary outcomes, including pelvic alignment, FLLI, and hip control ability, showed similar trends to those of ITT analyses. There were significant group-by-time interactions and time effects for PI, IATD, FLLI, and hip control ability (p < 0.001). Regarding the pain scale (VAS), functional disability (ODI and PSFS), GroC, and lower extremity flexibility, we also found significant time effects (p < 0.05) and group-by-time interactions (p < 0.05), which are akin to the results from ITT analyses.
For the comparisons of muscle strength, the results of the per-protocol analyses revealed similar findings as the ITT analyses for the hip muscle strength, except that a significant time effect (p = 0.009) and group by time interaction (p = 0.039) were identified for the hip flexors. In addition, the GT group had greater improvement in knee extensors (significant time by group effect with p = 0.043).
Discussion
This is the first randomized controlled interventional study to investigate the effect of gluteal control training in patients having LBP with FLLI. Our data supported the hypotheses that gluteal control training resulted in greater improvement in pelvic alignment, functional leg length inequality, hip joint motor control ability, hip muscle strength and flexibility, pain, function, and perceived overall changes when compared to regular training.
Our study found an average leg length difference of 0.9 cm in our participants, which was similar to those reported by Giles et al.9 The functional leg length discrepancy was believed to relate to asymmetrical pelvic alignment. Young et al. proposed that pelvic obliquity > 1.2 degrees could result in FLLI;12 Hagins et al. found 56% of healthy individuals had an IATD less than 2 degrees20. Our participants with LBP had an average of PI angle of 2.64 degrees and 3.77 degrees of IATD, indicating that our participants of LBP presented with FLLI combined with asymmetric pelvic alignment.
Previous studies have shown an association between soft tissue imbalance and pelvic malalignment, and indicated that gluteal dysfunction might increase the likelihood of developing low back pain12,21–23. Findings of our study supported this rationale that gluteal control training resulted in significantly greater improvement in pelvic alignment (PI: 2.9 to 1.03 degrees, IATD: 3.9 to 0.67 degrees) and FLLI (0.9 to 0.3 cm) (Table 2), along with reduction in pain and dysfunction. These post-treatment data also fell in the normal range reported previously12,20, indicating that gluteal training is an effective intervention strategy for correcting pelvic alignment associated functional leg length inequality in patients with chronic LBP.
Various lumbar exercises have been found effectively improving pain and disability in patients with LBP24. Our findings were consistent with previous studies that both gluteal control training and regular lumbar exercise training reduced pain and improved disability;18 the GT group which received gluteal muscle control training to address soft tissue imbalance and correct pelvic malalignment, showed more improvement in pain and disability as compared to the RT group (Table 3). It was believed that leg length discrepancy had a direct impact on functional activities such as standing and walking25. Our gluteal training successfully improved pelvic alignment and leg length symmetry, and thus reduced the load on the back muscles, leading to reduction of pain and disability. Fritz et al. have proposed that achieving a 50% improvement in the ODI represented successful treatment26. With this regard, the GT group outperformed the RT group by having more than 60% improvement in ODI in our participants with LBP and FLLI. Previous studies of Fukuda et al. and Ahn et al. tried to examine the effects of additional gluteal muscle strengthening in patients with CLBP17,18. Although Ahn et al. found more improvement in pain and quality of life for the group receiving gluteal strengthening17, both studies failed to identified additional benefits of gluteal strengthening for function and hip strength. These two studies did not screen for FLLI in patient recruitment, and they both used hip strengthening exercise instead of gluteal control training, which might explain the inconsistencies between their results and our data.
The improvement in pain and disability was reflected by the results of the Patient-Specific Functional Scale (PSFS) and Global Rating of Change (GRoC) scale. PSFS is a commonly used assessment tool to describe functional improvements. In this study, both types of exercises improved PSFS (GT: 3.27, RT:2.7) (Table 3), and the improvement exceeded the minimum clinically important difference (MCID) of PSFS (2 points)26. GRoC is a clinical tool used to subjectively quantify a patient’s improvement or deterioration over time27. Our data showed that the GT group and the RT group had self-perceived improvement rates of 88% and 40% at the third week, and 100% and 75% at the sixth week, respectively (Table 4). In addition, the GT group demonstrated a greater improvement in PSFS and GRoC, demonstrating that gluteal control training was more effective for improving the self-perceived outcomes in patients with LBP and FLLI.
The hip motor control was assessed using the prone hip extension test described by Murphy et al.28 Patients with poor hip control might exhibit excessive lumbar extension and/or anterior pelvic tilt during the test, which might have arisen from imbalances in the lumbar-pelvic-hip muscle group29, particularly for people with stiff anterior soft tissues in the hip joint, thigh, and lumbar spine29. After six weeks of training, both groups demonstrated significant improvement in hip control ability, with greater improvement for the GT group as compared to the RT group (Table 2). We believed that training associated improvement in pelvic alignment and muscle strength and flexibility contributed to the enhanced hip control. This was particularly true for the GT group which received training addressing the gluteal control ability.
After six weeks of exercise training, both groups demonstrated significant strength gain in hip musculatures except hip flexors, with greater improvement for the hip extensors, abductors, and adductors (time by group interactions, p = 0.036, 0.022, 0.008) for the GT group when compared to the RT group (Table 5). The strength gain of the GT group in the hip and knee musculatures was more prominent when data from dropouts were excluded (per-protocol analysis), with significant strength improvement in all hip musculatures for both groups, and greater improvement for the hip extensors, flexors, abductors, and adductors, and knee extensors for the GT group. Various forms of exercise have been recommended for managing LBP with evidence showing beneficial effects on pain and dysfunction, and muscle performance of the lower back24. However, the effect of exercise training on hip muscle strength was less explored in patients with LBP14,16,19,30,31, despite impaired hip muscle performance observed in this group of patients13,15,32. Although the exercise training in this study was designed to improve motor control (10 s hold for each repetition and 10 repetitions for each exercise) rather than for strength grain, our data showed both groups had strength improvement in the hip muscles. This might be explained by corrected pelvic alignment and FLLI after training, which promotes a better length-tension relationship in the lumbo-pelvic-hip muscles, enabling more efficient generation of muscle force and thus increasing muscle strength33. As the GT group received training targeted on gluteal control, more strength gain in hip extensors, abductors and adductors was found accompanied by greater improvement in pelvic alignment and leg length symmetry. Fukuda et al. conducted a study assessing the effect of hip muscle strengthening in addition to manual therapy and stabilization exercise in patients with CLBP, and found no extra benefits of hip strengthening exercise for pain, disability and hip extensors strength19. Possible explanations for the different results included firstly, we specifically recruited the subgroup of patients who presented with both CLBP and FLLI, while Fukuda et al. did not screen their patients of LBP for specific subgroups. In addition, we have used gluteal control training which was different from the hip strengthening exercise used by Fukuda et al.
Previous research observed inadequate flexibility in certain hip muscles in patients with LBP, and suggested that these compensatory alterations occurred for the need of pelvic stability34–36. After six weeks of training, we found gluteal control training resulted in more improvement in flexibility of the hamstrings, rectus femoris, and iliotibial band compared to the regular lumbar training (Table 6). Our results were supported by Park et al. (2016) that motor control training effectively improved hamstring flexibility and reduced pain in patients with LBP17. Improved hip muscle flexibility might be a combined result of better length-tension relationship in the lumbo-pelvic-hip region, pelvic alignment and movement control33.
Limitations of this study included the difficulty in controlling communication among participants, which may affect the credibility of the results. The patients with low back pain caused by sacroiliac joint problems were not completely excluded, so the generalization of the study results should be cautious. The pain duration in the ITT analysis showed a notable between-group difference, which might attribute to a less significant treatment effect of the RT group. Nevertheless, the per-protocol analysis has shown a similar pain duration between the two groups, and similar results favoring the gluteal control training. In addition, we only assessed the short-term effects of the six-week interventions and long-term effects and pain recurrence rates were not evaluated. Future research should have stricter inclusion and exclusion criteria for better control and conduct long-term follow-up on the effectiveness of gluteal muscle control training, as well as explore multiple aspects of functional performance.
Conclusions
Six-week gluteal muscle control training significantly improved pelvic alignment, reduced functional leg length inequality, improved pain and function, enhanced hip joint control, and hip muscle strength and flexibility in LBP patients with FLLI. We thus suggested clinicians to integrate gluteal control training into the intervention programs when managing people with low back pain and functional leg length inequality for greater treatment efficacy.
Methods
Study design
This was a double-blinded randomized controlled trial. The exercise interventions were conducted by two physical therapists with more than 5 years of experience in exercise instruction for patients with LBP. All the measurements were performed by the first author (XX) who was blind to the participant grouping. The study protocol was approved by the Institutional Review Board of Yang-Ming University (now National Yang Ming Chiao Tung University) (Approval No: YM106055F) and prospectively registered with the ClinicalTrials.gov (Clinical trial No: NCT03554746, Date:2018/05/30). This study has been conducted in accordance with the principles set forth in the Helsinki Declaration.
Participants
Figure 1 shows the flowchart of the study. The sample size of this study was calculated based on the FLLI in our pilot study (n = 15) that 22 participants in each group were required to reach the effect size of 0.88 (Power: 0.8, Alpha: 0.05). The inclusion criteria were: chronic non-specific LBP > 12 weeks; the maximum Visual Analog Scale (VAS) score for pain in the past four weeks ≥ 5; FLLI > 0.5 cm and the ilium anterior tilt difference (IATD) > 2 degrees. The exclusion criteria included a history of vertebral fractures or lumbar spine surgery, congenital musculoskeletal abnormalities, recent diagnosis of traumatic conditions, tumors, pregnancy, spinal scoliosis or central nervous system symptoms, sacroiliac joint dysfunction, structural leg length discrepancy > 1 cm, body mass index (BMI) > 30. Seventy people were screened and 48 patients were recruited. After signing the written consent, participants were randomly assigned to either the gluteal control training (GT) group (receiving regular training with additional gluteal control training, n = 24), or the regular training (RT) group (receiving regular training only, n = 24) using sealed envelopes.
Procedures and instrumentation
The participants first wrote informed consent and filled out an information sheet to provide their personal information. The principle investigator then conducted the baseline assessment, followed by six weeks of intervention and the identical assessment as the post-intervention evaluation.
The primary outcome measures of this study were pelvic alignment which was measured as pelvic inclination (PI) angle and the ilium anterior tilt difference (IATD), and functional leg length inequality (FLLI). The secondary outcome measures included pain intensity, functional disability, participant’s perceived functional ability, hip motor control ability, perceived overall improvement, lower limb muscle strength, and muscle flexibility.
The PI and IATD were measured in the standing position using the palpation meter (PALM; Performance Attainment Associates, St. Paul, MN). The PI angle was the angle formed between the line connecting the bilateral superior border of the iliac crests and the horizontal line. The IATD is the inclination angle between the line connecting the anterior superior iliac spine (ASIS) and the posterior superior iliac spine and the horizontal line was measured on both sides and the bilateral difference was calculated34. Three measurements were performed and averaged. The between-day measurement reliability of these two outcomes was assessed in our pilot study using intra-class correlation coefficients (ICC3,3) and was between 0.96 and 0.99.
The FLLI was measured using the block-in method. The participant was instructed to stand in a relaxed position. The assessor attached the labels to bilateral ASISs and a 20 cm ruler with a level gauge attached it was used to check the level of ASISs. Wooden boards (30 × 20 cm) of three thickness (0.12 cm, 0.28 cm, and 0.36 cm) were used to place underneath the foot of the shorter leg to adjust the level of ASISs until the level was even. The final thickness of the wooden block was measured as the FLLI37. Three measurements were performed and averaged. This method was validated using X-ray imaging38 in our pilot study with the Spearman correlation coefficient 0.90 between the two methods. The between-day ICC of this test was 0.96.
The VAS was used to assess the participants’ pain levels in the past month on a 100-cm line. The Oswestry Disability Index (ODI) Chinese version 2.1 was used to evaluate functional disability39,40. The Patient Specific Functional Scale (PSFS) were used to assess participant’s perceived functional ability by asking the participants to identify three activities that they found challenging to perform in their daily lives and rate their ability to perform each activity on a scale of 0 to 10. The scores were averaged to represent the participant’s perceived functional ability39. Perceived overall improvement was measured using the Global Rating of Change (GRoC) scale, which assesses participants’ self-perceived overall improvement on a scale ranging from − 7 to + 7. Participants completed the GRoC scale immediately after the third and sixth weeks of treatment, with improvements above + 4 as “significant improvement” and scores from 0 to + 3 as “non-significant improvement”27.
Lower limb isometric muscle strength (extensors, flexors, abductors, adductors, and external and internal rotators of the hip, and knee extensors) was measured using a dynamometer (Commander™ Muscle Tester, JTECH MEDICAL, Utah, USA) with the methods described by Hislop et al.41. Muscle flexibility of the hamstring, rectus femoris, and tensor fascia lata-iliotibial tract complex was measured using an inclinometer (iPhone APP, Angle Meter). The hamstring flexibility was measured with the participant supine with hip and knee joints flexed to 90 degrees, and passive knee extension was performed until resistance was felt. The angle of knee extension was recorded by a smartphone. The flexibility of the rectus femoris was measured using Ely’s test angle, and the flexibility of the tensor fascia lata-iliotibial tract complex was measured using Ober’s test angle42. Three measurements were performed and the data was averaged. The between-day measurement reliability of these measures was between 0.81 and 0.99.
Hip motor control ability was assessed based on the method described by Murphy et al.28. The participant was instructed to perform hip extension in a prone position until the hip was lifted 20 cm above the horizontal plane. The assessor observed and recorded the occurrence of any abnormal movements such as spinous process rotation, lateral shift of the lumbar spine, lumbar extension, and pelvic raise. One point was recorded for each abnormal movement observed. Three trials of assessment were performed, and the average score was recorded. The measurement reliability of hip motor control was 0.85.
Intervention
Two physical therapists (one for the GT and one for the RT group) performed the allocated intervention three times per week for approximately one hour each session for six weeks. Each session included general physical therapy (superficial heating and lumbar traction) for 20 min and allocated exercise training for 20 min. Exercise training for the RT group focused on trunk muscle strengthening, consisting of the transverse abdominis exercise series, lower trunk rotation exercise series, curl-up exercise series, and erector spinae exercise series. Exercise training for the GT group consisted of trunk muscle training (transverse abdominis exercise series) and gluteal control training including hip abduction-external rotator series, hip extensor series, and hip abductor-internal rotator series. Each exercise series was performed for ten repetitions, with each repetition held for ten seconds. The difficulty of each exercise series was enhanced each week. These exercise series are illustrated in Supplement 1.
Statistical analysis
Statistical Product and Service Solutions (SPSS) version 22.0 (IBM Corp., USA) was used for statistical analysis, with a significance level set at 0.05. Two analyses, including intention-to-treat (ITT) and per-protocol analysis, were adopted for this trial. All subjects receiving randomization were taken into ITT analysis and subjects with missing data were imputed using the group average values. For per-protocol analysis, the subjects with missing data were dropped out for statistical analysis. Chi-square tests and independent t-tests were performed to compare the baseline data. Two-way repeated-measures analysis of variance (ANOVA) was used to analyze the group differences after six weeks of intervention, and GRoC was analyzed using chi-square tests.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author contributions
Wen-Hung Huang: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original Draft, Chun-Kai Tang: Writing – original draft, Writing – review & editing, Yi-Fen Shih: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing; Funding acquisition (NSTC 112-2410-H-A49 -056 -MY2).
Data availability
Data is provided within the manuscript.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Arab, A. M., Ghamkhar, L., Emami, M. & Nourbakhsh, M. R. Altered muscular activation during prone hip extension in women with and without low back pain. Chiropr. Man Therap.19, 18. 10.1186/2045-709X-19-18 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nourbakhsh, M. R. & Arab, A. M. Relationship between mechanical factors and incidence of low back pain. J. Orthop. Sports Phys. Ther.32, 447–460. 10.2519/jospt.2002.32.9.447 (2002). [DOI] [PubMed] [Google Scholar]
- 3.Chien, J. J. & Bajwa, Z. H. What is mechanical back pain and how best to treat it?. Curr. Pain Headache Rep.12, 406–411. 10.1007/s11916-008-0069-3 (2008). [DOI] [PubMed] [Google Scholar]
- 4.Smith, B. E., Littlewood, C. & May, S. An update of stabilisation exercises for low back pain: A systematic review with meta-analysis. BMC Musculoskelet. Disord15, 416. 10.1186/1471-2474-15-416 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kendall, K. D., Schmidt, C. & Ferber, R. The relationship between hip-abductor strength and the magnitude of pelvic drop in patients with low back pain. J. Sport Rehabil.19, 422–435 (2010). [DOI] [PubMed] [Google Scholar]
- 6.Grimaldi, A. Assessing lateral stability of the hip and pelvis. Man. Ther.16, 26–32 (2011). [DOI] [PubMed] [Google Scholar]
- 7.Kim, S.-H. et al. Lumbopelvic motion during seated hip flexion in subjects with low-back pain accompanying limited hip flexion. Eur. Spine J.23, 142–148 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hides, J. A., Oostenbroek, T., Franettovich Smith, M. M. & Mendis, M. D. The effect of low back pain on trunk muscle size/function and hip strength in elite football (soccer) players. J. Sports Sci.34, 2303–2311 (2016). [DOI] [PubMed]
- 9.Giles, L. G. & Taylor, J. R. Low-back pain associated with leg length inequality. Spine6, 510–521, 10.1097/00007632-198109000-00014 (1981). [DOI] [PubMed]
- 10.Hoikka, V., Ylikoski, M. & Tallroth, K. Leg-length inequality has poor correlation with lumbar scoliosis. A radiological study of 100 patients with chronic low-back pain. Arch. Orthop. Trauma Surg.108, 173–175, 10.1007/BF00934262 (1989). [DOI] [PubMed]
- 11.McCaw, S. T. & Bates, B. T. Biomechanical implications of mild leg length inequality. Br. J. Sports Med.25, 10–13. 10.1136/bjsm.25.1.10 (1991). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Young, R. S., Andrew, P. D. & Cummings, G. S. Effect of simulating leg length inequality on pelvic torsion and trunk mobility. Gait Posture11, 217–223. 10.1016/s0966-6362(00)00048-5 (2000). [DOI] [PubMed] [Google Scholar]
- 13.de Sousa, C. S. et al. Lower limb muscle strength in patients with low back pain: A systematic review and meta-analysis. J. Musculoskelet. Neuronal Interact.19, 69–78 (2019). [PMC free article] [PubMed] [Google Scholar]
- 14.Bade, M. et al. Effects of manual therapy and exercise targeting the hips in patients with low-back pain-A randomized controlled trial. J. Eval. Clin. Pract.23, 734–740. 10.1111/jep.12705 (2017). [DOI] [PubMed] [Google Scholar]
- 15.Cooper, N. A. et al. Prevalence of gluteus medius weakness in people with chronic low back pain compared to healthy controls. Eur. Spine J.Bold">25, 1258–1265. 10.1007/s00586-015-4027-6 (2016). [DOI] [PubMed] [Google Scholar]
- 16.Peterson, S. & Denninger, T. Physical therapy management of patients with chronic low back pain and hip abductor weakness. J. Geriatr. Phys. Ther.00, 1–11 (2017). [DOI] [PubMed] [Google Scholar]
- 17.Park, K. N. et al. Effects of motor control exercise vs muscle stretching exercise on reducing compensatory lumbopelvic motions and low back pain: A randomized trial. J. Manip. Physiol. Ther.39, 576–585. 10.1016/j.jmpt.2016.07.006 (2016). [DOI] [PubMed] [Google Scholar]
- 18.Ahn, S. E., Lee, M. Y. & Lee, B. H. Effects of gluteal muscle strengthening exercise-based core stabilization training on pain and quality of life in patients with chronic low back pain. Medicina (Kaunas)60, 10.3390/medicina60060849 (2024). [DOI] [PMC free article] [PubMed]
- 19.Fukuda, T. Y. et al. Does adding hip strengthening exercises to manual therapy and segmental stabilization improve outcomes in patients with nonspecific low back pain? A randomized controlled trial. Braz. J. Phys. Ther.25, 900–907. 10.1016/j.bjpt.2021.10.005 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hagins, M. et al. Intratester and intertester reliability of the palpation meter (PALM) in measuring pelvic position. J. Manuf. Manip. Ther.6, 130–136 (1998). [Google Scholar]
- 21.Youdas, J. W., Garrett, T. R., Egan, K. S. & Therneau, T. M. Lumbar lordosis and pelvic inclination in adults with chronic low back pain. Phys. Ther.80, 261–275 (2000). [PubMed] [Google Scholar]
- 22.Knutson, G. A. Incidence of foot rotation, pelvic crest unleveling, and supine leg length alignment asymmetry and their relationship to self-reported back pain. J Manipulative Physiol Ther25, 110E. 10.1067/mmt.2002.121414 (2002). [DOI] [PubMed] [Google Scholar]
- 23.Badii, M. et al. Pelvic bone asymmetry in 323 study participants receiving abdominal CT scans. Spine28, 1335–1339, 10.1097/01.BRS.0000065480.44620.C5 (2003). [DOI] [PubMed]
- 24.Delitto, A. et al. Low back pain. J. Orthopaed. Sports Phys. Ther.42, A1–A57. 10.2519/jospt.2012.42.4.A1 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gurney, B. Leg length discrepancy. Gait PostureBold">15, 195–206. 10.1016/s0966-6362(01)00148-5 (2002). [DOI] [PubMed] [Google Scholar]
- 26.Fritz, J. M., Hebert, J., Koppenhaver, S. & Parent, E. Beyond minimally important change: Defining a successful outcome of physical therapy for patients with low back pain. Spine34, 2803–2809, 10.1097/BRS.0b013e3181ae2bd4 (2009). [DOI] [PubMed]
- 27.Kamper, S. J., Maher, C. G. & Mackay, G. Global rating of change scales: A review of strengths and weaknesses and considerations for design. J. Man Manip. Ther.17, 163–170. 10.1179/jmt.2009.17.3.163 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murphy, D. R. et al. Interexaminer reliability of the hip extension test for suspected impaired motor control of the lumbar spine. J. Manipul. Physiol. Ther.29, 374–377. 10.1016/j.jmpt.2006.04.012 (2006). [DOI] [PubMed] [Google Scholar]
- 29.Sahrmann, S. Diagnosis and Treatment of Movement Impairment Syndromes (Elsevier Health Sciences, 2002).
- 30.Bastos, R. M., Moya, C. R., de Vasconcelos, R. A. & Costa, L. O. P. Treatment-based classification for low back pain: Systematic review with meta-analysis. J. Man Manip. Ther.30, 207–227. 10.1080/10669817.2021.2024677 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alkhathami, K., Alshehre, Y., Brizzolara, K., Weber, M. & Wang-Price, S. Effectiveness of spinal stabilization exercises on movement performance in adults with chronic low back pain. Int. J. Sports Phys. Ther.18, 169–172. 10.26603/001c.68024 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nadler, S. F., Malanga, G. A., DePrince, M., Stitik, T. P. & Feinberg, J. H. The relationship between lower extremity injury, low back pain, and hip muscle strength in male and female collegiate athletes. Clin. J. Sport Med.10, 89–97. 10.1097/00042752-200004000-00002 (2000). [DOI] [PubMed] [Google Scholar]
- 33.Comerford, M. J. & Mottram, S. L. Movement and stability dysfunction–contemporary developments. Man Ther.6, 15–26. 10.1054/math.2000.0388 (2001). [DOI] [PubMed] [Google Scholar]
- 34.Youdas, J. W., Garrett, T. R., Harmsen, S., Suman, V. J. & Carey, J. R. Lumbar lordosis and pelvic inclination of asymptomatic adults. Phys. Ther.76, 1066–1081. 10.1093/ptj/76.10.1066 (1996). [DOI] [PubMed] [Google Scholar]
- 35.Van Wingerden, J., Vleeming, A., Kleinrensink, G. & Stoeckart, R. The Role of the Hamstrings in Pelvic and Spinal Function (Churchill Livingstone, 1997).
- 36.Arab, A. M. & Nourbakhsh, M. R. The relationship between hip abductor muscle strength and iliotibial band tightness in individuals with low back pain. Chiropr. Osteopat.18, 1. 10.1186/1746-1340-18-1 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sabharwal, S. & Kumar, A. Methods for assessing leg length discrepancy. Clin. Orthop. Relat. Res.466, 2910–2922. 10.1007/s11999-008-0524-9 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hankemeier, S. et al. Computer-assisted analysis of lower limb geometry: Higher intraobserver reliability compared to conventional method. Comput. Aided Surg.11, 81–86. 10.3109/10929080600628985 (2006). [DOI] [PubMed] [Google Scholar]
- 39.Maughan, E. F. & Lewis, J. S. Outcome measures in chronic low back pain. Eur. Spine J.19, 1484–1494 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lue, Y. J., Hsieh, C. L., Huang, M. H., Lin, G. T. & Lu, Y. M. Development of a Chinese version of the Oswestry Disability Index version 2.1. Spine33, 2354–2360, 10.1097/BRS.0b013e31818018d8 (2008). [DOI] [PubMed]
- 41.Hislop, H., Avers, D. & Brown, M. Daniels and Worthingham’s Muscle Testing-E-Book: Techniques of Manual Examination and Performance Testing (Elsevier Health Sciences, 2013).
- 42.Magee, D. J. Orthopedic Physical Assessment (Elsevier, 2014). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data is provided within the manuscript.