Abstract
Background
People who use drugs (PWUD) often face restricted healthcare access despite their heightened healthcare needs. Factors such as stigma, mistrust of the healthcare system, competing priorities, and geographical barriers pose significant healthcare access challenges. Telehealth offers an innovative solution to expand healthcare access for better inclusion of underserved populations in healthcare. We aimed to explore PWUDs’ perceptions of telehealth as a healthcare delivery modality.
Methods
We utilized purposive sampling to recruit participants (N = 57) for nine focus group discussions (FGDs) in Athens, Greece. Eligibility criteria required participants to be at least 18 years, with current or prior injection drug use, and current internet access. The FGDs followed a semi-structured interview guide, were audio recorded, transcribed verbatim, translated into English, and de-identified. We applied thematic analysis to analyze FGD transcripts.
Results
Participants’ mean (standard deviation) age was 47.9 (8.9) years, 89.5% (51/57) were male, 91.2% (52/57) were of Greek origin, and 61.4% (35/57) had attended at least 10 years of school. Three main themes emerged from the FGDs: (1) high internet utilization for healthcare-related purposes among PWUD, (2) highlighting telehealth benefits despite access obstacles and PWUDs’ concerns about diagnostic accuracy, and (3) approaches to overcome access obstacles and build digital trust. Participants extensively used the internet for healthcare-related processes, such as accessing healthcare information and scheduling provider appointments. Despite being telehealth-inexperienced, most participants expressed a strong willingness to embrace telehealth due to its perceived convenience, time-saving nature, and trusted digital environment. Some participants recognized that the inability to conduct physical examinations through telehealth reduces its diagnostic accuracy, while others expressed concerns about digital literacy and technological infrastructure accessibility. Most participants expressed a preference for video-based telehealth encounters over audio-only encounters. To build trust in telehealth and promote patient-centeredness, participants recommended an initial in-person visit, virtual eye contact during telehealth encounters, patient education, and partnerships with PWUD-supportive community organizations equipped with appropriate infrastructure.
Conclusions
PWUD frequently use the internet for health-related purposes and suggested several approaches to enhance virtual trust. Their insights and suggestions are practical guidance for policymakers seeking to enhance healthcare access for underserved populations through telehealth.
Trial registration
Supplementary Information
The online version contains supplementary material available at 10.1186/s12911-024-02718-6.
Keywords: Telehealth, Telemedicine, Healthcare access, People who use drugs
Background
People who use drugs (PWUD) typically have limited interactions with the healthcare system [1, 2]. Stigma in healthcare creates significant access barriers for PWUD [3, 4]. Negative experiences attributable to stigma in healthcare lead PWUD to mistrust healthcare providers, and they often conceal their drug use history during healthcare encounters. These sentiments and actions, in turn, lead to substandard patient-provider relationships and further marginalization of this population [5]. Consequently, despite being recognized as a group with heightened medical vulnerability and increased healthcare needs, PWUD typically remain medically underserved [6–8]. In addition to stigma, other frequent obstacles to healthcare access for PWUD include competing life and medical priorities, such as unstable housing status and mental health challenges, as well as financial and geographical barriers [9, 10]. These obstacles contribute to significant treatment gaps for PWUD leading to their increased morbidity and mortality [11]. A characteristic PWUD treatment gap is observed with two highly prevalent viral infections, hepatitis C virus (HCV) and HIV [12, 13]. Despite recent HCV and HIV treatment advances, access to highly efficacious treatments remains limited for PWUD [14–16]. Therefore, an urgent need exists to innovatively reform healthcare systems to address PWUD-related treatment gaps and ensure health equity [17–19].
In the realm of healthcare digitalization, internet-based healthcare delivery is an innovative approach that has the potential to expand healthcare access [20]. This concept aligns with the broader trend of integrating electronic healthcare into conventional healthcare delivery systems, utilizing approaches such as electronic health records (EHRs) and e-prescription systems. These systems have notably increased the overall efficiency of healthcare delivery and facilitated communication between patients and providers e.g. through patient portals [21, 22]. Telehealth, another healthcare digital cornerstone, has revolutionized interactions with healthcare providers [23]. Telehealth encompasses virtual visits through telemedicine, chat-based interactions, remote patient monitoring, and technology-enabled digital diagnostics and therapeutics [24]. Telemedicine, a subcategory of telehealth, is the delivery of clinical services at a distance usually through synchronous, two-way patient-provider videoconferencing [25]. Research data suggest that telehealth can be an effective approach to expand healthcare delivery for PWUD, particularly for the treatment of HCV, HIV, opioid use disorder, and mental health conditions [26–31].
Despite these advances, little is known about the experiences, perceptions, and attitudes of PWUD regarding accessing healthcare through telehealth [32]. Gaining insight into PWUDs’ attitudes toward telehealth will aid in identifying barriers and facilitators to its utilization and is crucial when designing interventions to increase telehealth utilization. We sought to identify the perspectives, attitudes, and beliefs of PWUD in Athens, Greece regarding telehealth as a healthcare delivery modality as well as perceived barriers and facilitators. Gaining insight into the views and needs of the PWUD population, along with their suggestions for improving telehealth delivery, could inform policies to expand digital healthcare access for PWUD.
Methods
Study population and recruitment
We recruited 57 PWUD through purposive sampling to participate in one of nine focus group discussions (FGDs) [33]. We defined PWUD as individuals with current or prior injection drug use. Our data collection focused on PWUD as an underserved group rather than a population defined by specific medical or social conditions. However, recognizing that PWUD often experience chronic conditions, such as HCV, HIV, as well as homelessness, we intentionally considered these additional factors and utilized, as participant recruitment sources, diverse community organizations that support underserved populations. Recruitment was conducted by study facilitators, i.e. staff with bachelor’s degrees in psychology or social work who were employed by various PWUD-supportive community organizations. These community organizations included the “Prometheus” Hellenic Liver Patient Association, the “My Athens” shelter for PWUD experiencing homelessness, the “Positive Voice” association of people living with HIV, and the “Network of Peer Users of Psychoactive Substances”. The study facilitators contacted prospective participants through in-person announcements or social media. Subsequently, prospective participants contacted the research project manager (Z.P.) directly or with the assistance of a study facilitator. The project manager then informed potential participants about the specifics of study participation. Individuals were deemed eligible to participate if they were at least 18 years old, had current or prior injection drug use, had current internet access, spoke Greek fluently, and were able to provide informed consent.
Data collection
We conducted nine FGDs, each comprising between 4 and 9 participants (N = 57), that occurred between May and September 2023. The FGDs occurred in private rooms on the premises of “Prometheus” and lasted a maximum of 90 min. Only the participants and the researchers were present at the time of the FGD. The research study manager (Z.P.) and the co-principal investigator (A.H.), both of whom were trained by an expert qualitative researcher (S.S.D.), coordinated the FGDs. The FGDs were audio-recorded, transcribed verbatim, and translated into English by a professional agency. We also made field notes during the FGD. The research project manager (Z.P.) verified the FGD transcripts for accuracy by comparing them with the recordings. After the completion of each FGD, we collected participants’ self-reported demographic information, including age, sex, ethnicity, and educational level. None of the participants terminated their participation in the FGD before its completion. We also provided participants with lunch and 10-euro compensation to cover the cost of transportation and time spent in the FGD.
FGDs are designed to encourage peer discussions and the sharing and generation of ideas [34, 35]. We designed a semi-structured interview guide that contained core questions and probes to promote discussions about telehealth as a healthcare delivery modality [see Additional file 1]. Our interview guide included open-ended, non-judgmental and non-leading questions, such as: “What are your thoughts about telemedicine?”, “What are your thoughts about seeing the doctor online versus up close [i.e., in person]?”, and “What would you suggest to make telemedicine attractive and more interesting to you?”. Prior to deployment, we pilot tested the interview guide in one pilot FGD with four study-eligible participants in accordance with the planned recruitment, enrollment, and informed consent study process. Following the pilot FGD, we made only a few minor language modifications to enhance comprehension by the study population and otherwise followed the exact study process for all subsequent FGDs.
Data analysis
We analyzed the FGD transcripts, including the pilot FGD, using thematic analysis [33–35]. The thematic analysis team consisted of 5 research members (Z.P., A.H.T., A.D., S.S.D., A.H.), including an expert in qualitative methodology (S.S.D.) and a member with extensive cultural expertise from significant research experience among Greek PWUD (A.H.). The iterative analysis process involved the initial review and analysis of the FGD transcripts and field notes by the research team. During this initial stage, each researcher independently coded and generated preliminary lower-level themes, as well as identified initial preliminary quotations [36]. To maintain rigor in the analytical approach, we encouraged the research team members to reflect on their pre-understandings and personal biases as they reviewed participants' beliefs. We held weekly meetings where researchers shared and compared their findings, simultaneously comparing them to previous FGD transcripts. When disagreements in the textual interpretations surfaced, we revisited the initial FGD transcript for review until we reached a consensus. During the ongoing analytical process, as new findings emerged, we coalesced previous themes to generate higher-level themes. When no new themes and insights were expected to emerge, even with additional FGDs, we determined that we had achieved theme saturation. This reflected the overall adequacy of the data collected, and we subsequently stopped further data collection [37]. The study adheres to the consolidated criteria for reporting qualitative research (COREQ) [see Additional file 2] [38].
Electronic healthcare in Greece
Healthcare in Greece is delivered through public providers under the National Healthcare System as well as private healthcare providers. The Greek National Healthcare System is funded through various sources, such as governmental funding, taxes, and social insurance contributions, with the goal of ensuring free or affordable healthcare access for the entire population [39, 40]. PWUD can access healthcare through designated shelters and substance use treatment organizations, such as the Organization Against Drugs (OKANA) and the Hellenic Therapy Center for Dependent Individuals (KETHEA) [41–43]. In terms of electronic healthcare, Greece employs an e-prescription system with national coverage exceeding 98%, facilitating 850,000 transactions daily [44–47]. This system includes features such as e-dispensation, which electronically transfers medical prescriptions to pharmacies, as well as e-referrals and e-appointments. However, EHR utilization remains low, challenged by a lack of systematic documentation and communication barriers [44]. The Hellenic Ministry of Health is working on enhancing medical professionals' access to an efficient EHR system, operated through an interoperability framework to facilitate healthcare data exchange across various organizations [48].
Moreover, limited telehealth usage exists in Greece; most telehealth expansion efforts have focused on extending healthcare access to remote areas especially those without sufficient healthcare resources, such as remote islands [49, 50]. The recent launch of the Telehealth Quality of Care Tool by the World Health Organization Regional Office for Europe in March 2024 seeks to improve telehealth standards and policies across Europe by providing a framework to assess and enhance telehealth quality [51]. This initiative is ongoing and encourages stakeholders to contribute to improved telehealth delivery. To date, no study has explored the role of telehealth in expanding healthcare access for marginalized communities, such as PWUD, in Greece.
Ethics
The study protocol was approved by the Institutional Review Boards of the Hellenic Scientific Society for the Study of AIDS, Sexually Transmitted and Emerging Diseases, and the University at Buffalo. The study adhered to the Helsinki Declaration principles. We obtained written informed consent from all study eligible participants prior to their participation and verbal consent before recording commenced, with documentation included in the recordings.
Results
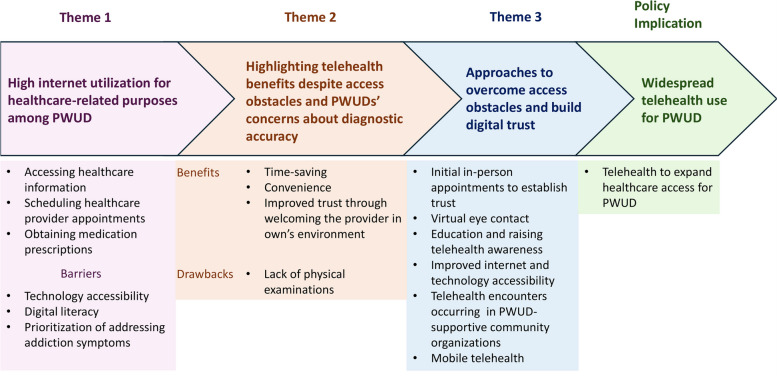
Our study participants had a mean (standard deviation) age of 47.9 (8.9) years, with 89.5% (51/57) being male, 91.2% (52/57) of Greek origin, and 61.4% (35/57) had attended at least 10 years of school. We performed thematic analysis on the interview guide responses and identified the following three major themes: (1) high internet utilization for healthcare-related purposes among PWUD, (2) highlighting telehealth benefits despite access obstacles and PWUDs’ concerns about diagnostic accuracy, and (3) approaches to overcome access obstacles and build digital trust. Figure 1 summarizes the themes we identified through the thematic analysis of FGDs (Fig. 1).
Fig. 1.
Building digital trust among people who use drugs (PWUD). We identified extensive use of the internet for healthcare purposes within a PWUD population with internet access (Theme 1). Despite limited experience with telehealth among FGD participants, they frequently used the internet for accessing healthcare information, scheduling appointments with healthcare providers, and obtaining medication prescriptions. Most participants perceived telehealth benefits, such as convenience, its time-saving nature, and the ease of establishing trust with healthcare providers (Theme 2). Participants agreed that these benefits outweigh telehealth’s perceived limitations, such as the inability to conduct physical examinations. However, some participants recognized that the inability to conduct physical examinations through telehealth results in reduced diagnostic accuracy compared to in-person assessments. These concerns led some participants to categorically oppose using telehealth. Participants also perceived major barriers to telehealth engagement, such as prioritization of addiction issues over healthcare, limited accessibility to technological infrastructure, and low digital literacy. Despite the reported perceived challenges, PWUD expressed a strong willingness to embrace telehealth as a healthcare delivery method and provided several suggestions to enable its widespread adoption within their communities. Participants’ suggestions included recommending an initial in-person visit before transitioning to telehealth, emphasizing the maintenance of eye contact during telehealth sessions to promote digital trust, and requesting education on how to effectively utilize telehealth services (Theme 3). Participants also believed that addressing technology accessibility limitations could be achieved through partnerships with community organizations that provide telehealth-related infrastructure, supported by physicians and the government. The identified themes support telehealth’s potential as an innovative solution to expand healthcare access for PWUD
Theme 1: High internet utilization for healthcare-related purposes among PWUD
All FGD participants were required to have internet access as a study inclusion criterion although the approaches used to access the internet varied among participants. Most frequently, participants reported accessing the internet through their personal cell phones, or less commonly, through their laptops, tablets, or through a friend’s cell phone. Participants experiencing homelessness reported accessing the internet mostly at the shelters where they resided. The shelters’ staffs were generally eager to assist shelter residents in using the computers if requested, as explained by one participant experiencing homelessness: “They [shelters’ staffs] only provide the internet connection, but if you need to do something on a computer, they help you do it” [participant 09–04].
A substantial proportion of participants reported using the internet for healthcare processes. Some participants described using the internet to access health information online. For example, one participant with a history of HCV shared: “I go to a website for hepatitis, for example, and I read about how it is transmitted, what medicines you have to take, and what treatments are available” [participant 07–08]. Another participant explained: “I mostly use Google to search and find medical forums. Because I find it more reliable and more focused on what I want” [participant 06–04]. Moreover, some participants described using the internet to schedule healthcare provider appointments with whom they would subsequently meet in person, as one participant mentioned: “I have done it [used the internet] at first, mainly to book an appointment at a hospital” [participant 07–08].
Another common reason for healthcare-related internet usage among participants was to obtain medication prescriptions. Some participants had experience using the government-supported e-prescription system in Greece. One participant explained: “So, I have registered on e-prescription and my prescriptions come on my phone, and I go to the pharmacy to get my medicines” [participant 09–06]. Alternatively, some participants would receive their medication prescriptions from their healthcare provider through social media platforms. For example, one participant shared: “The doctor has sent the prescription on Facebook Messenger, I went to the pharmacy and said, ‘Can you please give me those now?’” [participant 02–03]. In both scenarios, participants expressed appreciation for the convenience and practicality of receiving prescriptions remotely.
Participants also identified factors that could challenge telehealth utilization among individuals in their community. Participants experiencing homelessness considered internet access to be “a luxury for a homeless person”. One participant characteristically said: “Let’s see someone being homeless for six months and then let him talk about telemedicine. He [the person experiencing homelessness] has other needs and telemedicine comes after those” [participant 09–07]. Participants who did not experience homelessness also reported challenges accessing technological infrastructure and expressed concerns about their digital literacy. For example, one participant explained: “I have a small phone with buttons, and it is not easy to go online. I have to find someone to help me” [participant 07–04]. FGD participants also shared that they would frequently sell their phones to purchase illicit drugs. One participant described: “I might sell the cell phone, because when I am in pain, I will not bother with the phone, I will sell it to get my fix” [participant 08–02]. Prioritizing issues related to substance use was common among participants, such as one participant who shared:
I cannot say anything on telehealth, because right now I am just trying to rehabilitate. Yes, I don’t think of anything else. It is my number one obstacle; I cannot see beyond that. I cannot think of other stuff. [participant 06-05].
Theme 2: Highlighting telehealth benefits despite access obstacles and PWUDs’ concerns about diagnostic accuracy
Participants identified telehealth aspects that they considered as benefits and drawbacks as well as possible barriers to using telehealth. Overall, participants predominately focused on telehealth’s benefits and perceived it as a positive healthcare innovation, with some participants considering telehealth the “inevitable” future of healthcare. The vast majority of FGD participants expressed positive attitudes and a strong willingness to embrace telehealth even though they had limited direct personal experience. One participant perceived the value of telehealth as a means of addressing the imbalance between physician shortages and the increasing number of citizens, stating: “I understand that nowadays the numbers of doctors and citizens are such that, at some point, it has to come into our lives, it is inevitable” [participant 02–02]. Participants described various perceived telehealth benefits, with reduced travel and healthcare wait times being the most frequently reported. For example, one participant shared: “One of the advantages of telemedicine is that you can get informed and do what you need to do, wherever you are” [participant 04–04]. Another participant said: “I don’t have to go anywhere, use public transportation, waste money, make appointments. I can find him [healthcare provider] anytime I want” [participant 05–06]. FGD participants also believed that the healthcare provider’s entry into the patient’s environment through telehealth enables trust-building and ultimately improves communication with healthcare providers. For instance, one participant stated:
I also believe that the environment is very important for drug users, especially for drug users, and with telemedicine, you are entering into another person’s environment. I mean, the other person accepts you and perhaps he opens up to you. [participant 01-01].
Apart from the benefits, participants also discussed aspects of telemedicine they considered drawbacks. The inability to perform a physical examination was the most commonly perceived drawback of telehealth. Furthermore, some FGD participants recognized that the inability to conduct physical examinations through telehealth results in reduced diagnostic accuracy compared to in-person assessments. The participants most concerned by the inability to perform a physical examination also tended to be unwilling to engage in care through telehealth at all. For example, one participant shared: “I don’t feel as safe as I would if we were face-to-face [with a healthcare provider]. He might need to check something on me, listen to my heart, listen to my lungs. This cannot be done through telemedicine” [participant 06–01]. Similarly, another participant stated: “If something is wrong with you, you have to go to the doctor, and he will listen to you with the stethoscope, isn’t that right?” [participant 08–02]. Although concerns regarding confidentiality, privacy, and security were expressed less frequently than those related to the inability to perform a physical examination, some participants did affirm their concerns about these issues in the digital environment. For instance, one participant shared: “I believe that there is no confidentiality and that things leak over the internet” [participant 08–05].
When we explored participants’ views on receiving care through telemedicine at an opioid agonist treatment (OAT) program, most found the idea helpful and expressed willingness to participate. For example, one participant shared: “I would be interested in going to an [OAT program] and learning how to use telemedicine and how it can offer more help for my condition. It would be good” [participant 06–01]. Another participant, who was also willing to participate, highlighted the need for assistance with telemedicine at the OAT program, stating: “There must be someone there [at the OAT program] to guide us, it is not that easy … Someone has to show you” [participant 06–05]. Other participants agreed, emphasizing the importance of guidance when using telemedicine “It is good and important to have someone who can guide those who don’t have the experience or the knowledge to use it” [participant 06–03]. Those who were against participating in telemedicine encounters integrated into an OAT program mainly reported privacy and confidentiality concerns. For example, one participant explained: “I have been witnessing lately the lack of confidentiality [at OAT program]. Confidentiality is breached very easily. I mean, the whole team knows about my personal matters” [participant 01–01].
Theme 3: Approaches to overcome access obstacles and build digital trust
When asked about approaches to enhance the appeal of telehealth, FGD participants made various recommendations. An often-cited suggestion was to schedule an initial in-person appointment preceding telehealth encounters to establish patient-physician relationships and build trust. One participant said:
I think it has to do with the first contact ... seeing a doctor online for the first time, I don’t know how comfortable I would feel, because I have never done it, but it will certainly be different than seeing him up close [i.e., in person]. I am talking about the first approach. [participant 02-02].
Participants also suggested that maintaining virtual eye contact during video-based telehealth encounters helps build trust across the screen, while audio-only encounters were viewed less favorably. For example, one participant explained how video calls are preferred over audio-only calls: “Because you can see from the other person’s eyes if they are telling the truth or not. On the phone [without the video], it is something colder” [participant 05–07].
Participants also emphasized the importance of raising awareness about telehealth, either “through TV, radio, media, etc.” or directly from their healthcare provider. They had numerous questions about telehealth including those summarized by the following participant: “How it [telehealth] helps me personally and the doctor? … I mean, [telehealth] for what specialties? Are they general practitioners, psychiatrists, psychologists? I don’t know how it would help me” [participant 02–04]. Overall, participants agreed that “awareness among all sectors and all vulnerable groups” was considered critical for telehealth expansion among underserved populations. Participants also identified the need to improve access to technological infrastructure, such as the internet and devices that can access the internet. Participants suggested having telehealth encounters in convenient settings that could provide telehealth-related equipment. For example, one participant experiencing homelessness recommended: “To have a place where we can go and be checked through telemedicine, with laptops, for example. A place within an organization” [participant 06–04]. Another participant suggested a mobile telehealth approach, as follows: “To have some vans and have two specialized IT people with computers going around the streets, similar to how they distribute syringes” [participant 07–08].
Lastly, participants recommended that telehealth expansion into underserved populations requires government support. One participant stated: “They should give more money for this purpose [telehealth]. Greece is full of bright minds. They should provide the funds for this purpose and not waste them elsewhere” [participant 05–07]. Participants also encouraged physicians to take the lead on providing suggestions related to telehealth expansion. Participants felt that optimal results for telehealth expansion would occur when physicians collaborate with the government. For example, one participant suggested: “The medical community must put pressure on the ministries, and the specialists need to come up with better solutions and proposals” [participant 07–08].
Discussion
All of our study participants lacked formal telehealth experience, an anticipated finding since Greece has limited telehealth usage [52]. We found, however, that participants frequently used the internet for healthcare processes, such as accessing health information, scheduling appointments, obtaining medication prescriptions, and contacting their healthcare providers through social media. They described these experiences positively. Moreover, participants understood that telehealth can be an alternative to traditional in-person encounters and perceived several benefits of telehealth, including convenience, reduced wait and travel times, and improved communication with healthcare providers. Our participants’ impressions of telehealth’s benefits align with findings from studies with telehealth-experienced participants [53, 54].
Our participants considered telehealth a personalized form of healthcare delivery since it permits provider entry into the patient’s environment. They perceived that engaging with a provider in their own space signifies their own acceptance of the provider, creating an opportunity to “open up” to their provider, fostering a strong sense of trust that enhances the doctor-patient relationship. These findings are consistent with another study showing that PWUD significantly value empathy and trust during telemedicine encounters [27]. The stigma towards PWUD typically encountered in conventional healthcare settings presents a major barrier to accessing healthcare [5]. Our findings suggest that the participants’ perceived sense of acceptance fostered through telehealth indicates its potential, not only to overcome structural and geographical barriers to healthcare access, but also to reduce stigma and enhance trust-building in the patient-provider relationship.
With regard to telehealth’s drawbacks, participants most frequently identified the inability to perform a physical examination, an observation supported by others [23]. Homelessness, lack of technological infrastructure, and competing priorities related to substance use were perceived by participants as the major barriers to telehealth access. Participants identified that partnerships with PWUD-supportive community organizations equipped with suitable technological infrastructure could address barriers related to accessibility and digital literacy. Morris et al. also demonstrated that providing HCV treatment for PWUD experiencing homelessness in community settings is feasible, acceptable, and resulted in high cure rates [55]. Additionally, our study participants requested education and awareness about telehealth. Moreover, they recommended approaches to improve the acceptability of telemedicine, including scheduling an initial in-person appointment and ensuring providers maintain eye contact with patients during telehealth encounters. Meeting the provider “up close” or “face-to-face” (i.e., in person) helps foster a trusting relationship and to overcome PWUDs' mistrust of the healthcare system related to long-standing stigma [3, 56].
When planning an intervention, policymakers should engage the priority population in decision-making and planning processes [57]. Similar to our findings, a recent study reported that homelessness was associated with lower odds of internet and mobile technology use and high device and mobile phone number turnover rates [58]. Our findings support the high device turnover rate as a common practice among PWUD, mainly driven by the physiological need to address withdrawal symptoms with money earned through cell phone sales. Furthermore, to overcome technology accessibility barriers, participants suggested a telehealth approach using mobile vans to deliver care and expand healthcare access, an approach described by Wungjiranirun et al. [59]. Educational interventions to ensure adequate digital literacy, including topics such as telehealth operation, advantages, limitations, and potential health benefits, are an additional consideration when designing telehealth systems. Therefore, when planning telehealth interventions for PWUD at the community level, access to technological infrastructure, housing status, and education to promote digital literacy should be considered to ensure digital health equity [60, 61].
While the above-mentioned recommendations can increase the acceptability and accessibility of telehealth at the community level, assistance with using telemedicine for PWUD may accomplish these objectives at the patient-level. Our participants requested to have “someone who can guide those who don’t have the experience or the knowledge to use it”. In a research study where telemedicine was integrated into OAT programs for HCV treatment, case managers familiar to the participants assisted with the use of technological equipment and the telemedicine encounters [62]. This approach resulted in excellent HCV cure rates with minimal reinfections over a two-year follow up period. As described by the study participants, telemedicine could be further integrated outside of OAT programs into other locations where PWUD congregate, such as homeless shelters and community organizations. Lastly, participants perceived that governmental and expert support, including physician advocacy, is crucial to promote telehealth utilization.
Our participants included a male-predominant Greek population with current internet access largely from a government-supported healthcare environment, potentially limiting the generalizability of our results to individuals without internet access [63] or those from different healthcare systems [39, 40]. We recruited participants through community organizations that support PWUD, with the primary objective of exploring their perceptions and experiences of internet and telehealth use, rather than focusing on specific medical or social conditions. While we considered factors, such as homelessness and chronic illnesses like HIV and HCV during recruitment, further research that collects data on the specific medical and social characteristics of the population could provide greater clarity on the topic of digital healthcare access among underserved populations. Additionally, we acknowledge the limitations inherent to qualitative research and FGDs, such as the potential for groupthink and researcher-associated bias [64, 65]. Nevertheless, the relatively large sample size enabled us to achieve saturation thereby increasing the rigor of our findings [37, 66].
Conclusions
PWUD in Greece, largely inexperienced with telehealth, demonstrated its strong acceptance as a healthcare delivery modality. They perceived numerous telehealth benefits, including convenience and ease of patient-provider communication. PWUD also perceived that healthcare providers’ virtual entry into their personal space through telehealth could foster a stronger sense of trust in the patient-provider relationship.
A major cited limitation was the inability to perform a physical examination. Participants suggested that an initial, in-person appointment and virtual eye contact during telehealth encounters are crucial for establishing trusting patient-provider relationships in the digital setting. Participants viewed homelessness and access to technological infrastructure as two major barriers to telehealth implementation for PWUD. They suggested that partnering with PWUD-supportive community organizations equipped with suitable technological infrastructure, along with physician advocacy, should be encouraged to enhance government support for the expansion of telehealth for underserved populations.
Supplementary Information
Acknowledgements
Not applicable.
Abbreviations
- PWUD
People who use drugs
- HCV
Hepatitis C virus
- EHR
Electronic health record
- FGD
Focus group discussion
- OAT
Opioid agonist treatment
Authors’ contributions
Z.P. is the research study manager, wrote the paper, collected the data, performed the analysis, and contributed substantially to the study design. E.D., V.T., and G.T. collected the data. A.D. is a co-investigator and performed analysis. S.S.D. conceived, designed, and performed the analysis. A.H. is the co-principal investigator, performed analysis, and made substantial contributions to the study design. A.H.T. is the principal investigator, conceived and designed the study as well as performed the analysis. All authors provided intellectual input, drafted text, and approved the final copy.
Funding
Supported by a grant from the Troup Fund of the Kaleida Health Foundation grant awarded to AT. Clintrials.gov registration number: NCT05794984. Trial registry name: “Telemedicine and Social Media for People Who Inject Drugs (PWID) in Greece”. URL:
Data availability
The FGD transcripts and analyses are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
The study protocol was approved by the Institutional Review Boards of the Hellenic Scientific Society for the Study of AIDS, Sexually Transmitted and Emerging Diseases and the University at Buffalo. The study adhered to the Helsinki Declaration principles. We obtained written informed consent from all study eligible participants prior to their participation and verbal consent before recording commenced, with documentation included in the recordings.
Consent for publication
Not applicable.
Competing interests
A.H.T. received grants from Merck, Gilead, and Abbott Laboratories and has served as an advisor at Gilead. The remaining authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Russell C, Ali F, Nafeh F, LeBlanc S, Imtiaz S, Elton-Marshall T, Rehm J. A qualitative examination of substance use service needs among people who use drugs (PWUD) with treatment and service experience in Ontario, Canada. BMC Public Health. 2021;21(1):2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moallef S, Homayra F, Milloy MJ, Bird L, Nosyk B, Hayashi K. High prevalence of unmet healthcare need among people who use illicit drugs in a Canadian setting with publicly-funded interdisciplinary primary care clinics. Subst Abus. 2021;42(4):760–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Muncan B, Walters SM, Ezell J, Ompad DC. “They look at us like junkies”: influences of drug use stigma on the healthcare engagement of people who inject drugs in New York City. Harm Reduct J. 2020;17(1):53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chan Carusone S, Guta A, Robinson S, Tan DH, Cooper C, O’Leary B, et al. “Maybe if I stop the drugs, then maybe they’d care?”—hospital care experiences of people who use drugs. Harm Reduct J. 2019;16(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang JE, Lindenfeld Z, Hagan H. Integrating Harm Reduction into Medical Care: Lessons from Three Models. J Am Board Fam Med. 2023;36(3):449–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sun J, Mehta SH, Astemborski J, Piggott DA, Genberg BL, Woodson-Adu T, et al. Mortality among people who inject drugs: a prospective cohort followed over three decades in Baltimore, MD. USA Addiction. 2022;117(3):646–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roussos S, Angelopoulos T, Cholongitas E, Savvanis S, Papadopoulos N, Kapatais A, et al. High levels of all-cause mortality among people who inject drugs from 2018 to 2022. Int J Drug Policy. 2024;126:104356. [DOI] [PubMed] [Google Scholar]
- 8.Mayer S, Langheimer V, Nolan S, Boyd J, Small W, McNeil R. Emergency department experiences of people who use drugs who left or were discharged from hospital against medical advice. PLoS ONE. 2023;18(2):e0282215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beaulieu T, Ti L, Milloy MJ, Nosova E, Wood E, Hayashi K. Major depressive disorder and access to health services among people who use illicit drugs in Vancouver, Canada. Subst Abuse Treat Prev Policy. 2018;13(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heidari O, Tormohlen K, Dangerfield Ii DT, Tobin KE, Farley JE, Aronowitz SV. Barriers and facilitators to primary care engagement for people who inject drugs: A systematic review. J Nurs Scholarsh. 2023;55(3):605–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lanièce Delaunay C, Maheu-Giroux M, Marathe G, Saeed S, Martel-Laferrière V, Cooper CL, et al. Gaps in hepatitis C virus prevention and care for HIV-hepatitis C virus co-infected people who inject drugs in Canada. Int J Drug Policy. 2022;103:103627. [DOI] [PubMed] [Google Scholar]
- 12.Cepeda JA, Vickerman P, Bruneau J, Zang G, Borquez A, Farrell M, et al. Estimating the contribution of stimulant injection to HIV and HCV epidemics among people who inject drugs and implications for harm reduction: A modeling analysis. Drug Alcohol Depend. 2020;213:108135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fast Facts: HIV in the United States 2024. Centers for Disease Control and Prevention. 2024. https://www.cdc.gov/hiv/data-research/facts-stats/index.html#:~:text=HIV%20infections%20among%20people%20who%20inject%20drugs%20(PWID),of%20estimated%20new%20HIV%20infections. Accessed 30 Apr 2024.
- 14.Aponte-Meléndez Y, Mateu-Gelabert P, Eckhardt B, Fong C, Padilla A, Trinidad-Martínez W, et al. Hepatitis C virus care cascade among people who inject drugs in puerto rico: Minimal HCV treatment and substantial barriers to HCV care. Drug Alcohol Depend Rep. 2023;8:100178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lazarus JV, Villota-Rivas M, Fernández I, Gea F, Ryan P, López SA, et al. A cascade of care analysis on the elimination of hepatitis C from public hospitals in Madrid. Commun Med. 2022;2(1):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reddon H, Fairbairn N, Grant C, Milloy MJ. Experiencing homelessness and progression through the HIV cascade of care among people who use drugs. AIDS. 2023;37(9):1431–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Falade-Nwulia O, Sutcliffe CG, Mehta SH, Moon J, Chander G, Keruly J, et al. Hepatitis C Elimination in People With HIV Is Contingent on Closing Gaps in the HIV Continuum. Open Forum Infect Dis. 2019;6(10):ofz426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uusküla A, Feelemyer J, Des Jarlais DC. HIV treatment, antiretroviral adherence and AIDS mortality in people who inject drugs: a scoping review. Eur J Public Health. 2023;33(3):381–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bhatt J, Bathija P. Ensuring Access to Quality Health Care in Vulnerable Communities. Acad Med. 2018;93(9):1271–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stoumpos AI, Kitsios F, Talias MA. Digital Transformation in Healthcare: Technology Acceptance and Its Applications. Int J Environ Res Public Health. 2023;20(4). [DOI] [PMC free article] [PubMed]
- 21.Keasberry J, Scott IA, Sullivan C, Staib A, Ashby R. Going digital: a narrative overview of the clinical and organisational impacts of eHealth technologies in hospital practice. Aust Health Rev. 2017;41(6):646–64. [DOI] [PubMed] [Google Scholar]
- 22.Aldughayfiq B, Sampalli S. Digital Health in Physicians’ and Pharmacists’ Office: A Comparative Study of e-Prescription Systems’ Architecture and Digital Security in Eight Countries. OMICS. 2020;25(2):102–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gajarawala SN, Pelkowski JN. Telehealth Benefits and Barriers. J Nurse Pract. 2021;17(2):218–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Telehealth: Defining 21st Century Care 2024. American Telehealth Association. 2024. https://www.americantelemed.org/resource/why-telemedicine/. Accessed 10 Mar 2024.
- 25.Why use telehealth? Telehealth.HHS.gov. 2024. https://telehealth.hhs.gov/patients/why-use-telehealth#what-is-telehealth. Accessed 10 Mar 2024.
- 26.Hammerslag LR, Mack A, Chandler RK, Fanucchi LC, Feaster DJ, LaRochelle MR, et al. Telemedicine Buprenorphine Initiation and Retention in Opioid Use Disorder Treatment for Medicaid Enrollees. JAMA Netw Open. 2023;6(10):e2336914-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Talal AH, Sofikitou EM, Wang K, Dickerson S, Jaanimägi U, Markatou M. High Satisfaction with Patient-Centered Telemedicine for Hepatitis C Virus Delivered to Substance Users: A Mixed-Methods Study. Telemed J E Health. 2023;29(3):395–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Talal AH, Markatou M, Liu A, Perumalswami PV, Dinani AM, Tobin JN, Brown LS. Integrated Hepatitis C-Opioid Use Disorder Care Through Facilitated Telemedicine: A Randomized Trial. JAMA. 2024;331(16):1369–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rosato V, Nevola R, Conturso V, Perillo P, Mastrocinque D, Pappalardo A, et al. Telemedicine Improves HCV Elimination among Italian People Who Use Drugs: An Innovative Therapeutic Model to Increase the Adherence to Treatment into Addiction Care Centers Evaluated before and during the COVID-19 Pandemic. Biology. 2022;11(6):800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Corneli A, Perry B, Des Marais A, Choi Y, Chen H, Lilly R, et al. Participant perceptions on the acceptability and feasibility of a telemedicine-based HIV PrEP and buprenorphine/naloxone program embedded within syringe services programs: a qualitative descriptive evaluation. Harm Reduct J. 2022;19(1):132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fast N, van Kessel R, Humphreys K, Ward NF, Roman-Urrestarazu A. The Evolution of Telepsychiatry for Substance Use Disorders During COVID-19: a Narrative Review. Curr Addict Rep. 2023;10(2):187–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aronowitz SV, Engel-Rebitzer E, Dolan A, Oyekanmi K, Mandell D, Meisel Z, et al. Telehealth for opioid use disorder treatment in low-barrier clinic settings: an exploration of clinician and staff perspectives. Harm Reduct J. 2021;18(1):119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.The AC, Convenience ITA, Samples P. Indian J. Psychol Med. 2021;43(1):86–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Powell RA, Single HM. Focus groups. Int J Qual Health Care. 1996;8(5):499–504. [DOI] [PubMed] [Google Scholar]
- 35.Wong LP. Focus group discussion: a tool for health and medical research. Singapore Med J. 2008;49(3):256–60 quiz 61. [PubMed] [Google Scholar]
- 36.Sundler AJ, Lindberg E, Nilsson C, Palmér L. Qualitative thematic analysis based on descriptive phenomenology. Nurs Open. 2019;6(3):733–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57. [DOI] [PubMed] [Google Scholar]
- 39.Tsagkaris C, Papazoglou AS, Moysidis DV, Papadakos SP, Papadakis M. Striving to afford free health care in Greece during COVID-19. Lancet. 2023;402(10408):1128–9. [DOI] [PubMed] [Google Scholar]
- 40.Economou C. Greece: Health system review. Health Syst Transit. 2010;12(7):1–177, xv−xvi. [PubMed] [Google Scholar]
- 41.Greece Country Drug Report 2019. European Monitoring Center for Drugs and Drug Addiction. 2019. https://www.ektepn.gr/sites/default/files/2020-06/CDR%202017_en_0.pdf. Accessed 1 May 2024.
- 42.The Organisation Against Drugs (ΟΚΑΝΑ). https://www.okana.gr/el/about-us. 2021. Accessed 15 May 2024.
- 43.Shelter for homeless drug addicts. Adopt your city. 2022. https://adoptathens.gr/en/thematic-area/koinoniki-allileggyi/. Accessed 15 May 2024.
- 44.Kotsiopoulos I. Digital Transformation of the Healthcare Sector in Greece 2022. 2022. https://www.ihe-europe.net/sites/default/files/PDF%20EXP%2022/1-IHE_ExP_DAY_PPT_Kotsiopoulos_v2.pdf. Accessed 16 May 2024.
- 45.Hellenic National ePrescription Homepage. 2024. https://www.e-prescription.gr/. Accessed 16 May 2024.
- 46.National Organization for Health Care Services Homepage. 2024. https://www.eopyy.gov.gr/. Accessed 16 May 2024.
- 47.eAppointments Homepage for citizens. 2024. https://www.e-syntagografisi.gr/p-rv/p. Accessed 16 May 2024.
- 48.Katehakis DG, Kouroubali A, Fundulaki I. Towards the Development of a National eHealth Interoperability Framework to Address Public Health Challenges in Greece. 2018. Semantic Web Technologies for Health Data Management. https://ceur-ws.org/Vol-2164/paper6.pdf. Accessed 16 May 2024.
- 49.Telemedicine services extended to new islands in Greece. European Comission. 2020. https://ec.europa.eu/regional_policy/en/newsroom/news/2020/12/12-03-2020-telemedicine-services-extended-to-new-islands-in-greece. Accessed 20 May 2024.
- 50.Politis A, Vorvolakos T, Kontogianni E, Alexaki M, Georgiou EE, Aggeletaki E, et al. Old-age mental telehealth services at primary healthcare centers in low- resource areas in Greece: design, iterative development and single-site pilot study findings. BMC Health Serv Res. 2023;23(1):626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Telehealth quality of care tool: web annex. World Health Organization. 2024 https://www.who.int/europe/publications/i/item/WHO-EURO-2024-9501-49273-73635. Accessed 29 Mar 2024.
- 52.Myloneros T, Sakellariou D. The effectiveness of primary health care reforms in Greece towards achieving universal health coverage: a scoping review. BMC Health Serv Res. 2021;21(1):628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Powell RE, Henstenburg JM, Cooper G, Hollander JE, Rising KL. Patient Perceptions of Telehealth Primary Care Video Visits. Ann Fam Med. 2017;15(3):225–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sugarman DE, Busch AB, McHugh RK, Bogunovic OJ, Trinh CD, Weiss RD, Greenfield SF. Patients’ perceptions of telehealth services for outpatient treatment of substance use disorders during the COVID-19 pandemic. Am J Addict. 2021;30(5):445–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Morris MD, McDonell C, Luetkemeyer AF, Thawley R, McKinney J, Price JC. Community-Based Point-of-Diagnosis Hepatitis C Treatment for Marginalized Populations: A Nonrandomized Controlled Trial. JAMA Netw Open. 2023;6(10):e2338792-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Biancarelli DL, Biello KB, Childs E, Drainoni M, Salhaney P, Edeza A, et al. Strategies used by people who inject drugs to avoid stigma in healthcare settings. Drug Alcohol Depend. 2019;198:80–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fernandez ME, Ruiter RAC, Markham CM, Kok G. Intervention mapping: theory- and evidence-based health promotion program planning: perspective and examples. Front Public Health. 2019;7:209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ozga JE, Paquette C, Syvertsen JL, Pollini RA. Mobile phone and internet use among people who inject drugs: Implications for mobile health interventions. Subst Abus. 2022;43(1):592–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wungjiranirun M, Kanner R, Laguardia YS, Valadao E, Duarte M, McKinney J, et al. Zooming to a cure: harnessing telemedicine to offer mobile hepatitis C testing and treatment. Hepatology. 2020;72:417A. [Google Scholar]
- 60.Campanozzi LL, Gibelli F, Bailo P, Nittari G, Sirignano A, Ricci G. The role of digital literacy in achieving health equity in the third millennium society: A literature review. Front Public Health. 2023;11:1109323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Haimi M. The tragic paradoxical effect of telemedicine on healthcare disparities- a time for redemption: a narrative review. BMC Med Inform Decis Mak. 2023;23(1):95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Talal AH, Jaanimägi U, Davis K, Bailey J, Bauer BM, Dharia A, et al. Facilitating engagement of persons with opioid use disorder in treatment for hepatitis C virus infection via telemedicine: Stories of onsite case managers. J Subst Abuse Treat. 2021;127:108421. [DOI] [PubMed] [Google Scholar]
- 63.Carminati L. Generalizability in qualitative research: a tale of two traditions. Qual Health Res. 2018;28(13):2094–101. [DOI] [PubMed] [Google Scholar]
- 64.Kitzinger J. Qualitative research. Introducing focus groups BMJ. 1995;311(7000):299–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bergen N, Labonté R. “Everything Is Perfect, and We Have No Problems”: Detecting and Limiting Social Desirability Bias in Qualitative Research. Qual Health Res. 2020;30(5):783–92. [DOI] [PubMed] [Google Scholar]
- 66.Malterud K, Siersma VD, Guassora AD. Sample Size in Qualitative Interview Studies: Guided by Information Power. Qual Health Res. 2016;26(13):1753–60. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The FGD transcripts and analyses are available from the corresponding author upon reasonable request.