Abstract
Background
The aim of the study was to evaluate the effectiveness of a novel e-learning module in teaching the physical exam of the temporomandibular joint (TMJ) in Juvenile idiopathic arthritis (JIA.).
Methods
An e-learning module was developed to convey the TMJ physical examination maneuvers that are considered to be best practice in JIA. Pediatric rheumatology fellows were randomized to two groups. One group received an article describing the physical examination skills while the second group received both the article and module. All participants completed a written pre-test, an in-person objective structured clinical examination (OSCE), a written post-test, and a follow-up survey.
Results
Twenty-two pediatric rheumatology fellows enrolled, with 11 per group. Written test: The two groups improved equally, although there was a trend toward improved defining of maximal incisal opening (MIO) in the module group. OSCE: The mean OSCE score was 11.1 (SD 3.3) in the article group and 13.5 (SD 1.9) in the module group (p = 0.06); significant differences were seen in measuring MIO (p = 0.01), calculating maximal unassisted mouth opening (MUMO; p = 0.01), and assessment of facial symmetry (p = 0.03), all favoring the module. Enjoyment scores in the module group were higher than in the article group (mean 7.7/10 vs. 5.9/10, p = 0.02). The two groups self-reported performing TMJ examinations at comparable rates three months following the intervention.
Conclusions
The study demonstrated that a formalized educational program improved knowledge of the physical exam of the TMJ in JIA. Learners viewing the module were more adept at obtaining quantitative TMJ measurements.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12969-024-01026-7.
Keywords: Temporomandibular joint, Arthritis, Juvenile, Education, Medical
Background
Arthritis of the temporomandibular joint (TMJ) occurs in up to 53% of patients with juvenile idiopathic arthritis (JIA), frequently leading to dentofacial deformity and dysfunction [1, 2]. The TMJ has been termed the “forgotten joint” of JIA [3] and may present as the first or only joint involved [4]. Furthermore, TMJ arthritis is often initially asymptomatic leading to diagnostic delays [1, 5]. The effects of TMJ arthritis can have a severe negative impact on health-related quality of life that may persist into adulthood [6, 7]. In a cross-sectional study of adults with a history of TMJ arthritis and JIA, 62% experienced TMJ pain, 43% had functional limitation, and 76% had facial asymmetry [6]. This occurs despite the introduction of biologics in the treatment of JIA [8].
Early detection and treatment are believed to reduce joint damage and minimize resulting facial deformity. Gadolinium-enhanced magnetic resonance imaging (MRI) is currently the diagnostic standard to diagnose TMJ arthritis [9]. The clinical orofacial examination is useful to detect signs of active TMJ arthritis, to assess response to therapy, and to detect abnormalities caused by prior TMJ arthritis [10]. However, differences in how clinical orofacial exams are conducted has led to discrepancies among research studies and potential under-recognition of this clinical problem. Many specialists are involved in treating these patients, including rheumatologists, maxillofacial surgeons, orthodontists, and orofacial pain specialists, among whom inconsistent orofacial examinations are performed.
While TMJ arthritis is a well-recognized problem in JIA, pediatric rheumatology training programs do not routinely teach a standardized TMJ examination technique. Trainees often lack exposure to teachers or multidisciplinary clinics with expertise in this disorder. Pediatric rheumatologists, however, often serve as the main care providers for susceptible patients and are best positioned to recognize early TMJ arthritis. Screening practices for TMJ arthritis vary among both adult and pediatric rheumatologists [11, 12]. A pediatric rheumatology fellowship curriculum to improve and standardize the TMJ examination technique could improve recognition and treatment of one of the most debilitating outcomes in JIA.
The Temporomandibular Joint Juvenile Arthritis Work Group (TMJaw), a multi-disciplinary group of international experts, established consensus-based recommendations for the clinical orofacial examination in JIA [13]. In 2019, this group published a standardized, short (less than 3 min) physical examination protocol to be used routinely in the clinical setting [14]. However, this tool is not being used broadly for teaching JIA examination techniques to trainees, in part because the print description of the techniques is long, and technical. In this study, we developed and evaluated an e-learning module based on the TMJaw standardized protocol with the goal of teaching the TMJ examination protocol to pediatric rheumatology trainees, so that it can be incorporated into their routine musculoskeletal physical examination for use in all patients with JIA.
Methods
E-learning module
A 25-minute e-learning module consisting of instructive video clips and interactive questions was developed utilizing the input of both TMJ content experts and a medical education e-learning team. The module includes background information about TMJ arthritis (2 min) and uses a video narrator to review the elements of a structured physical exam: history (1 min), palpation (2 min), assessment of deviation (5 min), inspection for symmetry and profile changes (6 min), and measurements of range of motion (6 min). The module provides a mnemonic for the steps of the physical exam: STOMPS: S = symptoms (history); T = TMJ palpation; O = opening deviation; M = maximal unassisted mouth opening; P = profile; S = symmetry. Throughout the module there are 8 interactive components, spaced between video demonstrations. These include multiple choice questions, simulated measurements and calculations, and identification of anatomic landmarks. At the conclusion of the module, the entire TMJ exam is demonstrated, beginning to end, in less than 3 min. Consent was obtained to use demonstrative patient photographs. The module used standardized operational terminology and definitions for patients with JIA [13]. The platform housing the module displayed the most recent logon but did not capture how long each participant spent viewing the module nor how many times it was reviewed. During the study, the module was embargoed; following the conclusion of this study, the module became freely available and can be accessed by creating an account [15].
Pre- and post-tests
A written assessment was developed to evaluate knowledge acquisition among fellows following the e-learning intervention. A convenience sample of pediatrics residents and oral and maxillofacial surgery (OMS) trainees participated in beta testing to assess baseline knowledge and ensure that our assessment tool discriminated between content-naïve pediatrics residents and mastery-level OMS trainees. Questions that did not discriminate well between pediatric resident knowledge (which was assumed to be minimal) and OMS residents (which was assumed to be adequate) were modified until they performed well as a tool for discriminating between groups of trainees. The final test consisted of 10-items, weighted by content, with a maximum possible score of 7; the pre-test was identical to the post-test. Power calculation was based on an alpha of 0.05 and a beta of 0.80. Sigma was calculated based on the difference between the mean performances on pre-test validation of 27 pediatrics residents (4.85, SD 1.1) and 9 OMS residents (6.44, SD 1.24). This suggested a sample size of 9 per group would adequately power the study for a non-inferiority knowledge assessment.
Study participants
Pediatric rheumatology fellows were recruited by email to participate in a study to assess the TMJ module. Fellows were offered a $50 gift card for their participation. Twenty-two fellows were recruited with 11 in each group. Block randomization was performed, and fellows were stratified by post-graduate year, with an equal number of first year fellows and more senior fellows in each group. All participants completed a written pre-test before the learning intervention. Two weeks later, they were given access to the learning materials.The control group received the published article that describes the TMJaw physical examination protocol [14], while the e-learning module intervention group received both the article and access to the e-learning module. Fellows received their learning intervention two weeks prior to their in-person objective structured clinical examination (OSCE) and written post-test evaluation. The learning intervention could be accessed multiple times at any point from its release two weeks before the OSCE until the day of the OSCE.
OSCE
An in-person OSCE was developed and took place in conjunction with the Childhood Arthritis and Rheumatology Research Alliance Scientific Meeting in March 2023. A prompt posted outside of the OSCE room explained the clinical scenario: A patient with well-controlled polyarticular JIA, treated with methotrexate, with a normal peripheral joint examination, mentions having jaw pain with chewing. Fellows were instructed to take a TMJ-focused history and to perform a thorough examination of the TMJ. No time limit was imposed. Evaluators were blinded to the participant group. A content expert (CR) evaluated all the test patients for accurate measurements before the OSCE. Participants were scored on an evaluation form that listed all the key TMJ examination components. The maximum possible OSCE score was 18. Evaluators met before and after the OSCE to review scoring and ensure consistency.
Follow-up survey
All participants completed a 5-item follow-up survey three months after the OSCE. The survey assessed frequency of TMJ exam performance in clinical practice, confidence in TMJ examination skills, and satisfaction with the learning experience.
Study data were collected and managed using REDCap (Research Electronic Data Capture) electronic data capture tools hosted at Children’s National Hospital [16]. REDCap is a secure, web-based application designed to support data capture for research studies, providing (1) an intuitive interface for validated data entry; (2) audit trails for tracking data manipulation and export procedures; (3) automated export procedures for seamless data downloads to common statistical packages; and (4) procedures for importing data from external sources.
Statistics
Crosstab tables and Chi-squared tests were used to assess categorical variables across groups. For continuous measures when comparing the two groups, the Wilcoxon Rank Sum tests was used and when comparing paired data the Wilcoxon signed-rank test was used due to the small sample size.
This study was deemed exempt by the Institutional Review Board of Children’s National Hospital and consent was waived (Pro00014662).
Results
Twenty-two pediatric rheumatology fellows were enrolled; 11 fellows were randomized to receive the previously published TMJaw article alone (article group), and 11 fellows were randomized to receive both the article and the e-learning module (module group). Each group had an equal number of fellows from each year of training. Both groups self-reported that they spent an equal amount of time preparing for the OSCE: mean of 34.1 min in article group, 35.5 min in module group (p = 0.57). All fellows in the module group accessed the module.
Pre- and post-tests
Out of a maximum score of 7, the article group scored a mean of 3.00 (SD 1.09) on the pre-test and 5.23 (SD 1.19) on the post-test (p = 0.001). The module group scored a mean of 2.68 (SD 0.78) on the pre-test and 5.00 (SD 0.97) on the post-test (p = 0.001). There was no statistically significant difference between the two groups on the postscore (p = 0.59) or the difference between pre and post scores (p = 0.96). The module participants were better able to identify the correct definition of maximal unassisted mouth opening (MUMO) on a multiple-choice question, although it was not statistically significant (p = 0.06). On the pre-test, two participants in the article group and none in the module group answered the question ascertaining MUMO correctly. On the post-test, six participants in the article group and ten participants in the module group answered this question correctly (p = 0.06). Both groups improved in recognition of patient profiles and facial asymmetry on photographs in the written evaluation.
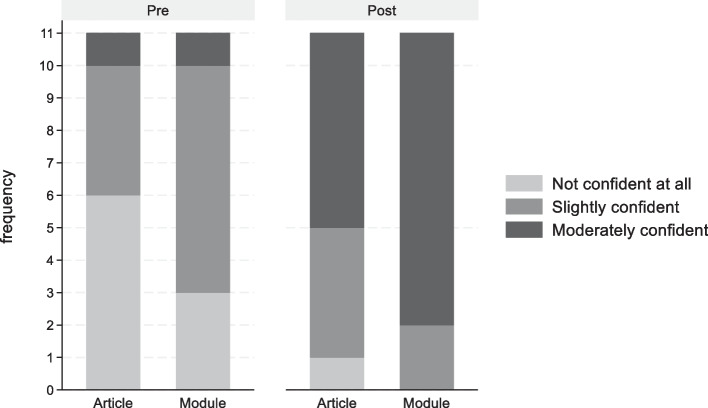
When asked if confident in their TMJ exam skills at baseline, 66% of the article group was not confident compared to 33% in the module group. This was not statistically significant. Overall, both groups reported an increase in confidence in their TMJ physical exam skills after the intervention (Fig. 1). 73% in each group increased their confidence, with no statistical difference in the improvement rates between the two groups. However, this improvement in each group was significantly different (p < 0.001).
Fig. 1.
Self-reported confidence in TMJ physical exam skills before and after the learning intervention for all participants. No difference in the rate of improved confidence was noted between groups
OSCE
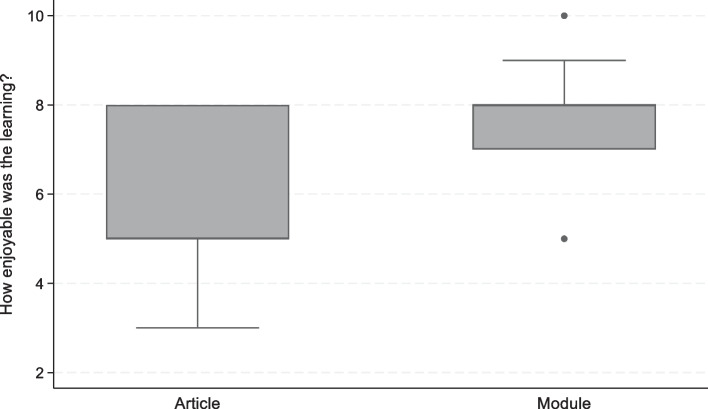
Out of a total score of 18, the mean score on the OSCE was 11.1 (SD 3.3) in the article group and 13.5 (SD 1.9) in the module group, though this did not reach statistical significance (p = 0.06). Significant differences were seen in learning domains related to measuring the maximal incisal opening (MIO), calculating the MUMO, and assessment of facial symmetry (Table 1), with the module group having superior measurement scores in all three domains. There were no significant differences between the groups on their performance related to history taking, palpating the TMJ in the correct location, assessing for mandibular deviation, or evaluating facial profile. When asked to rank how enjoyable the learning experience was, the article group rated a mean of 5.9/10, while the module group rated it 7.7/10, (p = 0.017) (Fig. 2).
Table 1.
TMJ-focused OSCE scores by learning group
| Exam element (/total possible score) | Article only Mean (SD) Median (IQR) |
Module Mean (SD) Median (IQR) |
P value (Wilcoxon Rank Sum Test) |
|---|---|---|---|
| OSCE total score (/18) | 11.09 (3.27) | 13.54 (1.91) | 0.059 |
| 11 (8 to 15) | 14 (12 to 15) | ||
| History taking (/4) | 2.82 (1.08) | 3.09 (0.94) | 0.581 |
| 3 (2 to 4) | 3 (2 to 4) | ||
| Palpation (/3) | 2.27 (0.90) | 2 (0.63) | 0.214 |
| 2 (2 to 3) | 2 (2 to 2) | ||
| Mandibular deviation (/4) | 2.09 (1.37) | 2.54 (1.13) | 0.418 |
| 2 (1 to 3) | 3 (1 to 3) | ||
| Measurement of MIO (/3) | 2.36 (1.21) | 4.09 (1.38) | 0.005 |
| 3 (2 to 3) | 5 (3 to 5) | ||
| MUMO calculation (/2) | 0.36 (0.81) | 1.45 (0.93) | 0.012 |
| 0 (0 to 0) | 2 (0 to 2) | ||
| Facial Symmetry (/1) | 0.63 (0.50) | 1 (0) | 0.030 |
| 1 (0 to 1) | 1 (1 to 1) | ||
| Profile (/1) | 0.91 (0.30) | 0.81 (0.40) | 0.543 |
| 1 (1 to 1) | 1 (1 to 1) |
OSCE objective structured clinical examination, MIO Maximal incisal opening, MUMO maximal unassisted mouth opening
Fig. 2.
Participant response to “How enjoyable was the learning?”
Follow up survey
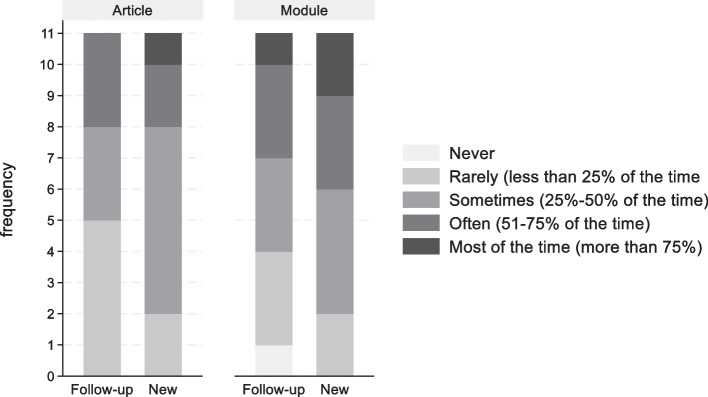
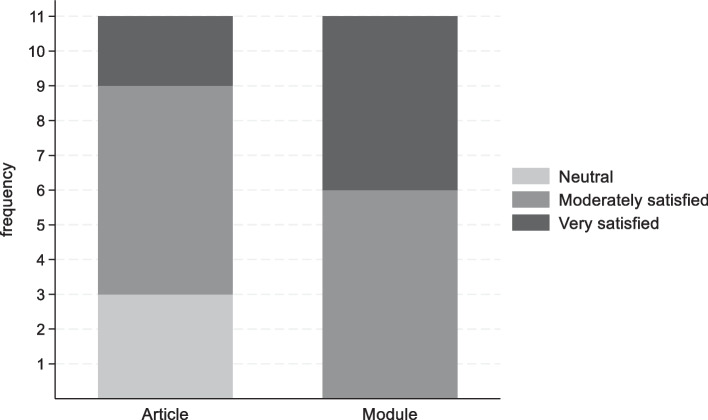
Three months after the OSCE, there was no difference in the reported rates of performing the full 3-minute TMJ examination protocol when evaluating new or follow-up JIA patients in practice. In the article group, 3 participants (27%) perform the protocol often or most of the time for new and follow-up JIA patients. In the module group, 5 participants (45.45%) perform the protocol often or most of the time for new JIA patients and 4 participants (36.36%) perform the protocol often or most of the time for follow-up JIA patients (Fig. 3). One participant in the module group reported that they never performed the full TMJ exam protocol for follow up patients. All participants in the module group were moderately or very satisfied with the learning intervention compared with only 8/11 (72.73%) in the article group (Fig. 4).
Fig. 3.
After the training that you received; how often do you perform the full standardized screening examination of the TMJ when evaluating patients [during new patient consultation visits or during follow-up visits]?
Fig. 4.
How satisfied were you with the TMJ examination education that you received in preparation for the TMJ OSCE at the CARRA meeting?
Discussion
Recently, there has been increased recognition of the importance of the clinical examination of the TMJ in children with JIA. Along with the ankle, wrist, hip, and sacroiliac joint, the TMJ is considered a key risk factor for poor outcomes in JIA and thus the presence of TMJ arthritis is conditionally recommended to guide treatment decisions [17]. Recommendations for the management of orofacial manifestations of JIA [18] have highlighted the critical role of a standardized clinical TMJ examination.
We therefore used the TMJaw brief standardized orofacial examination to develop a novel educational module to teach TMJ examination. In our study, both the original article and the module were shown to be effective in improving learners’ knowledge of the TMJ examination in a sample of pediatric rheumatology fellows. The module was superior in teaching objective measurements of oral aperture.
Accurate assessment of mouth opening has important clinical implications for children with JIA. Limited mouth opening [19] and mandibular deviation at maximal mouth opening [10, 20] have been shown to be predictive of active TMJ inflammation in JIA. Assessment of mouth opening capacity is the most common outcome used to assess TMJ arthritis in clinical studies [14].
There is a paucity of data regarding evidence-based pharmacologic treatment in patients with JIA and TMJ involvement. To our knowledge, there is no prospective study in the biologic era which addresses or provides specific guidance on TMJ arthritis management in JIA. TMJ outcomes are not routinely evaluated in clinical trials for JIA. Of 224 clinical trials involving JIA, only six studies reported on TMJ status [21]. While standardized terminology to describe TMJ arthritis in JIA exists [13], it is still not widely used. This lack of consistent assessment and description can lead to discrepancies and difficulty comparing research studies, which may impede meaningful advancement in understanding of TMJ involvement in JIA. The question of optimal management of TMJ arthritis can only be addressed with use of standardized TMJ examination and inclusion of TMJ outcomes in prospective, controlled trials of patients with juvenile arthritis.
We herein describe the first e-learning module that teaches JIA TMJ examination best practices. The e-module can be completed within 25-minutes and uses interactive techniques and adult learning theory to teach the five key TMJ examination domains, using the STOMPS mnemonic as a guide. Fellows using the e-learning module rated their enjoyment of the model as a 7.7/10, which significantly exceeded fellows’ enjoyment of the article as a means of learning the TMJ physical examination.
It is important to note that both groups improved significantly in their post-test knowledge levels and confidence after reviewing the materials, meaning that the article and the e-module were both effective learning tools. The e-module was superior for teaching fellows to perform measurement techniques, which is the most complex of the physical examination techniques included in the TMJ protocol. It is also notable that the fellows assigned the e-learning module enjoyed the learning experience more than those who used the article alone to prepare for the OSCE. In a real-world setting, where trainees would not be expected to perform an OSCE following an assigned curriculum, fellows may be more likely to complete an enjoyable e-learning self-study module than they would be to spend the same amount of time reading an article.
Although the learning materials were made available to the trainees 2 weeks prior to the OSCE, most participants viewed the module the day of the OSCE. Fellows using the 25 min-module, with access to the article, self-reported spending an average of 35.5 min preparing for the OSCE, which is comparable to the article group, which reported spending 34.1 min using the article to prepare. It is difficult to ascertain whether the participants in the module group accessed the article and duration spent in the module.
Unfortunately, after 3 months, less than half of all participants reported consistently performing the full TMJ examination protocol in practice, and there was no difference between the groups. One participant in the module group reported never performing the TMJ exam for follow up patients. While there was improvement in rates of performing this examination, barriers likely still exist but were not specifically assessed in this study. In a large multinational JIA registry, the TMJ was measured quantitatively in 8% of visits [22], compared with 27–45% of the learners who completed this study, so there is reason to believe that a structured curriculum in TMJ examination may lead to increased dedicated examination of these joints.
In terms of study weaknesses, the p values of the two groups were just shy of statistical significance, and a larger sample size may have led to more significant results. Unfortunately, while the study was powered for the pre/post-test, it was not possible to fully power the OSCE. While we are able to confirm that each participant assigned to the module did access the module, we are unable to ascertain the duration that the participants spent on the study materials and which material was used as their primary source. We did not measure inter-rater variability for the OSCE; however, all evaluators received the same training on scoring procedures and were blinded to trainees’ study groups. It is also important to note that an OSCE inherently forces observation in a simulated environment, which is an assessment of what one can do, rather than what one does in an authentic clinical setting. Nevertheless, OSCE exam scores have been shown to correlate with clinical evaluations in pediatric residents [23], and the ability to effectively examine the TMJ will enable a trainee to get more effective data if/when wanting to assess for disease activity. We note that video monitoring could have provided more objective scoring of the trainees and allowed specific feedback to further improve trainees’ skills and satisfaction with the training. Finally, sustained impact could have been assessed by performing a follow up OSCE. However, this was not logistically feasible to coordinate.
There were several strengths to this study. With expert collaboration, we developed a novel learning tool to teach a new standardized physical exam of the TMJ in JIA. The tool includes helpful video demonstrations, didactics, interactive questions, and a mnemonic to provide organization to the performance of the physical examination. To evaluate our tool, we conducted a randomized, blinded, in-person assessment of clinical skills among a target group of learners. All the subjects completed all the study activities including the follow-up survey 3 months later. While the article was also helpful in teaching many of the examination skills, the module was more effective in teaching the quantitative measurements.
Conclusions
This 25-minute interactive e-learning module improved pediatric rheumatology trainees’ understanding of the TMJ examination (knowledge) and resulted in better ability to perform MIO and MUMO measurements (skills). The module’s ability to effectively teach quantitative measurement is critical both for clinical care and for standardization in TMJ research studies. Trainees who participated in the interactive module reported more enjoyment of the learning process. Widespread use of this TMJ educational module will help improve clinical care by increasing early detection of TMJ involvement in patients with JIA, prompting appropriate treatment and ongoing monitoring. Future steps include further refinement of the content to focus on areas where learners had less improvement. The material will be included in an extended training event for pediatric rheumatology fellows and additionally will be offered to researchers who collect JIA measures.
Supplementary Information
Acknowledgements
The authors wish to acknowledge the Arthritis Foundation for their ongoing financial support of CARRA. We are thankful to Alex Bryant, Holly Bloom, and Kurt Sidenstick for their expertise in developing the e-learning module. We appreciate our colleagues who beta-tested the module and are grateful to the fellows who participated in this study.
Abbreviations
- CARRA
Childhood Arthritis and Rheumatology Research Alliance
- JIA
Juvenile idiopathic arthritis
- MIO
maximal incisal opening
- MRI
Magnetic resonance imaging
- MUMO
Maximal unassisted mouth opening
- OMS
Oral and Maxillofacial Surgery
- OSCE
Objective structured clinical examination
- SD
Standard deviation
- TMJaw
Temporomandibular Joint Juvenile Arthritis Work Group
- TMJ
Temporomandibular joint
Authors’ contributions
Conception and design of the study e-learning module (NP, RES, MAL, CMR, PS, MT, TR.) Acquisition of data (NP, RES, MAL, CMR, MT, TR.) Analysis (NP, RES, MAL, CMR, JEB, PS, MT, TR.) Manuscript preparation (NP, TR.) Manuscript revisions (NP, RES, MAL, CMR, JEB, PS, MT, TR.) All authors read and approved the final manuscript.
Funding
This project is supported by both a George Washington University School of Medicine and Health Science Education Research Grant as well as a Childhood Arthritis and Rheumatology Research Alliance (CARRA) - Arthritis Foundation small grant.
Data availability
The datasets generated and analyzed during the current study are not publicly available due participant confidentiality.
Declarations
Ethics approval and consent to participate
This study was deemed exempt by the Institutional Review Board of Children’s National Hospital and consent was waived (Pro00014662).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Nancy Pan, Email: pann@hss.edu.
for the CARRA TMJ arthritis Workgroup:
References
- 1.Stoustrup P, Glerup M, Bilgrau AE, Küseler A, Verna C, Christensen AE, et al. Cumulative incidence of orofacial manifestations in early juvenile idiopathic arthritis: a regional, three-year cohort study. Arthritis Care Res. 2020;72:907–16. [DOI] [PubMed] [Google Scholar]
- 2.Stoll ML, Kau CH, Waite PD, Cron RQ. Temporomandibular joint arthritis in juvenile idiopathic arthritis, now what? Pediatr Rheumatol Online J. 2018;16:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arabshahi B, Cron RQ. Temporomandibular joint arthritis in juvenile idiopathic arthritis: the forgotten joint. Curr Opin Rheumatol. 2006;18:490–5. [DOI] [PubMed] [Google Scholar]
- 4.Hügle B, Spiegel L, Hotte J, Wiens S, Herlin T, Cron RQ, et al. Isolated arthritis of the Temporomandibular Joint as the initial manifestation of Juvenile Idiopathic Arthritis. J Rheumatol. 2017;44:1632–5. [DOI] [PubMed] [Google Scholar]
- 5.Klenke D, Quast A, Prelog M, Holl-Wieden A, Riekert M, Stellzig-Eisenhauer A, et al. TMJ pathomorphology in patients with JIA-radiographic parameters for early diagnosis. Head Face Med. 2018;14:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Resnick CM, Dang R, Henderson LA, Zander DA, Daniels KM, Nigrovic PA, et al. Frequency and morbidity of Temporomandibular Joint involvement in adult patients with a history of Juvenile Idiopathic Arthritis. J Oral Maxillofac Surg off J Am Assoc Oral Maxillofac Surg. 2017;75:1191–200. [DOI] [PubMed] [Google Scholar]
- 7.Glerup M, Stoustrup P, Matzen LH, Rypdal V, Nordal E, Frid P, et al. Longterm outcomes of temporomandibular joints in Juvenile Idiopathic Arthritis: 17 years of followup of a nordic Juvenile Idiopathic Arthritis Cohort. J Rheumatol. 2020;47:730–8. [DOI] [PubMed] [Google Scholar]
- 8.Giancane G, Muratore V, Marzetti V, Quilis N, Benavente BS, Bagnasco F, et al. Disease activity and damage in juvenile idiopathic arthritis: methotrexate era versus biologic era. Arthritis Res Ther. 2019;21:168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tolend MA, Twilt M, Cron RQ, Tzaribachev N, Guleria S, von Kalle T, et al. Toward establishing a standardized magnetic resonance imaging scoring system for temporomandibular joints in Juvenile Idiopathic Arthritis. Arthritis Care Res. 2018;70:758–67. [DOI] [PubMed] [Google Scholar]
- 10.Stoustrup P, Twilt M, Spiegel L, Kristensen KD, Koos B, Pedersen TK, et al. Clinical orofacial examination in juvenile idiopathic arthritis: international consensus-based recommendations for monitoring patients in clinical practice and research studies. J Rheumatol. 2017;44:326–33. [DOI] [PubMed] [Google Scholar]
- 11.Ringold S, Tzaribachev N, Cron RQ. Management of temporomandibular joint arthritis in adult rheumatology practices: a survey of adult rheumatologists. Pediatr Rheumatol Online J. 2012;10:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Foeldvari I, Tzaribachev N, Cron RQ. Results of a multinational survey regarding the diagnosis and treatment of temporomandibular joint involvement in juvenile idiopathic arthritis. Pediatr Rheumatol Online J. 2014;12:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stoustrup P, Resnick CM, Pedersen TK, Abramowicz S, Michelotti A, Küseler A, et al. Standardizing terminology and assessment for orofacial conditions in juvenile idiopathic arthritis: international, multidisciplinary Consensus-based recommendations. J Rheumatol. 2019;46:518–22. [DOI] [PubMed] [Google Scholar]
- 14.Stoustrup P, Herlin T, Spiegel L, Rahimi H, Koos B, Pedersen TK, et al. Standardizing the clinical orofacial examination in juvenile idiopathic arthritis: an interdisciplinary, consensus-based, short screening protocol. J Rheumatol. 2020;47(9):1397–404. [DOI] [PubMed] [Google Scholar]
- 15.Pan N, Ronis T, Resnick CM, Sadun R, Lerman M, Stoustrup P, et al. Musculoskeletal examination of the temporomandibular joint in Juvenile idiopathic arthritis. Available from: https://childrensmedicaleducation.org/learnmeded/. Cited 2024 May 10. [DOI] [PMC free article] [PubMed]
- 16.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Onel KB, Horton DB, Lovell DJ, Shenoi S, Cuello CA, Angeles-Han ST, et al. 2021 American College of Rheumatology Guideline for the treatment of juvenile idiopathic arthritis: therapeutic approaches for Oligoarthritis, Temporomandibular Joint Arthritis, and systemic juvenile idiopathic arthritis. Arthritis Rheumatol Hoboken NJ. 2022;74:553–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stoustrup P, Resnick CM, Abramowicz S, Pedersen TK, Michelotti A, Küseler A, et al. Management of orofacial manifestations of juvenile idiopathic arthritis: Interdisciplinary consensus-based recommendations. Arthritis Rheumatol Hoboken NJ. 2023;75:4–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abramowicz S, Susarla HK, Kim S, Kaban LB. Physical findings associated with active temporomandibular joint inflammation in children with juvenile idiopathic arthritis. J Oral Maxillofac Surg off J Am Assoc Oral Maxillofac Surg. 2013;71:1683–7. [DOI] [PubMed] [Google Scholar]
- 20.Kristensen KD, Stoustrup P, Küseler A, Pedersen TK, Twilt M, Herlin T. Clinical predictors of temporomandibular joint arthritis in juvenile idiopathic arthritis: a systematic literature review. Semin Arthritis Rheum. 2016;45:717–32. [DOI] [PubMed] [Google Scholar]
- 21.Kinard B, Goldberg B, Kau C, Abramowicz S. Clinical trials of temporomandibular joint involvement of juvenile idiopathic arthritis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2021;131:617–9. [DOI] [PubMed] [Google Scholar]
- 22.Costello A, Twilt M, Lerman MA, CARRA Registry Investigators. Provider assessment of the temporomandibular joint in juvenile idiopathic arthritis: a retrospective analysis from the CARRA database. Pediatr Rheumatol Online J. 2024;22:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carraccio C, Englander R. The objective structured clinical examination: a step in the direction of competency-based evaluation. Arch Pediatr Adolesc Med. 2000;154:736–41. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and analyzed during the current study are not publicly available due participant confidentiality.