Abstract
Introduction
Childhood malnutrition is a complex issue with a range of contributing factors. The consequences of malnutrition are severe, particularly for children. This study aims to identify the factors contributing to inequality gaps in childhood malnutrition. Our study provides insights into modifiable elements to inform interventions targeted at distinct contexts and populations to improve child nutrition.
Methods
This study utilized data from the Demographic and Health Surveys (DHS) of 27 countries. First, the risk differences (RDs) between the prevalence of childhood malnutrition among the determinant variables, household income, and maternal education categories were calculated. The Blinder‒Oaxaca decomposition was subsequently used to determine the extent to which the difference in childhood malnutrition prevalence between low-income and high-income groups and maternal education levels results from the contributory effects of the explanatory variables: child and maternal individual-level compositional factors.
Results
We examined data from 138,782 children in 27 countries from 2015 to 2020. The prevalence of childhood malnutrition (10.5%) varied across countries, ranging from 6.5% in Burundi to 29.5% in Timor Leste. On average, the prevalence of childhood malnutrition was 11.0% in low-income households and 10.7% among mothers without education. Some nations had pro-low-income (i.e., malnutrition concentrated among children from poor households) or pro-no-maternal education (i.e., malnutrition concentrated among children from mothers with no formal education) inequality in childhood malnutrition, but most did not. We found a complex interplay of compositional effects, such as the child’s age, maternal education, maternal health behavior, and place of residence, that influence the inequality in childhood malnutrition rates across 10 pro-low-income countries. In addition, we also found that a complex mix of compositional effects, such as the household wealth index, maternal health behavior, and maternal age, contribute to childhood malnutrition inequality between educated and uneducated mothers across the 7 pro-no maternal education countries.
Conclusion
The prevalence of childhood malnutrition varies among low-income, high-income, and no maternal education-maternal education groups. This study highlights the need for a country-specific approach to addressing childhood malnutrition, with policies and interventions tailored to each country’s specific context.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-20378-z.
Keywords: Child, Malnutrition, Income, Education
Background
Childhood malnutrition is a complex issue with a range of contributing factors. Multiple studies have identified poverty as the most pervasive cause of malnutrition [1–3]. Other factors identified include food insecurity, parental education, government policies, and socioeconomic inequalities [1–3]. Feei et al. (2022) identified poverty not only as a cause of malnutrition but also as a consequence of malnutrition [4]. They described the interconnectedness of these factors as a vicious cycle. Additionally, climate change has been noted as a critical factor in childhood malnutrition, primarily affecting food availability, access, and utilization, as well as water, sanitation, and exposure to health risks and diseases [5].
The consequences of malnutrition are severe, particularly for children. Malnutrition predisposes children to various illnesses, ranging from kwashiorkor to diet-related noncommunicable diseases, and reduces productivity during adulthood [6]. Additionally, childhood malnutrition can severely affect a child’s cognitive and physical growth, leading to decreased quality of life in adults [6–8]. Therefore, malnutrition during childhood can have long-term effects on health outcomes later in life.
The double burden of childhood malnutrition is an evolving global health challenge that refers to the coexistence of undernutrition and overweight or obesity within individuals, households, and populations [9, 10]. On an individual level, this may entail the simultaneous occurrence of various forms of malnutrition at different life stages [9, 10]. Similarly, double-burdened households simultaneously experience multiple forms of malnutrition among their members [9, 10]. This reflects the prevalence of multiple forms of malnutrition in specific geographic areas at the population level [9, 10]. It is a complex and multifaceted issue that affects both developing and developed countries, with exceptionally high rates among children in low- and middle-income countries.
Several studies have noted the associations between socioeconomic determinants and childhood malnutrition [11–16]. Two studies highlighted the importance of socioeconomic factors in understanding childhood malnutrition disparities [12, 16]. In addition, social globalization has been associated with increased odds of double-burden of malnutrition [14]. A lower wealth index, maternal education, and living in rural areas have been noted to be significantly associated with childhood malnutrition [11, 13, 15, 17].
Although significant progress has been made in terms of global health and well-being, childhood malnutrition inequality remains a knotty issue, especially given the evolving double burden. To address this, it is crucial to gain a comprehensive understanding of the determinants and associated factors. Decomposition analysis allows us to examine all aspects of inequality by breaking it down into contributing factors [18]. Using this method, we can identify the specific factors responsible for the differences between the two groups and determine their role in moderating childhood malnutrition inequality [18]. This information is essential for designing effective and targeted interventions. Additionally, studies on the decomposition analysis of childhood malnutrition are limited, and there is a lack of research on interventions targeted at the double burden of malnutrition [19]. Therefore, our study aims to identify the extent of income and maternal education inequalities in childhood malnutrition across 27 countries.
Methods
Study design and data sources
This study utilized data from the Demographic and Health Surveys (DHS) conducted by ICF International. The DHS surveys are household surveys that collect nationally representative data on various healthcare areas, such as maternal and child health, child survival, HIV/AIDS and other sexually transmitted infections (STIs), and reproductive health [20]. These surveys are conducted every five years in more than 90 low- and middle-income countries (LMICs) [20]. The surveys follow a stratified multistage cluster sample design to collect data from women and men aged between 15 and 49 years and their young children under the age of five, living in randomly selected households within clusters that serve as the primary sampling unit [20]. For this analysis, the Children’s Recode of the most recent DHS surveys was used. Only country datasets with a full complement of our explanatory variables were included in this analysis. We excluded children with missing or flagged weight-for-height Z scores from our analysis.
Outcome variable
We employed the WHO child growth standard weight-for-height to determine the outcome variable, with the weight and height z-scores obtained from weight and length measurements [21]. The z-scores had been precalculated and were available in the DHS dataset for children under the age of five. Moderately and severely wasted children are classified as those with z-scores below − 2 and − 3 standard deviations, respectively, whereas those with z-scores above + 2 standard deviations are considered overweight [21]. Children with z-scores between the two aforementioned standard deviations are classified as not wasted or as having excess weight [21]. Consequently, we created the outcome variable as a factor variable with two categories: not wasted or overweight and wasted or overweight. We selected weight for height as the anthropometric indicator because of its comparative robustness [22].
Determinant variables
Two determinant variables were used in this study, which was informed by findings from our previous study: poverty level (categorized as low-income or high-income) and maternal education (categorized as no maternal education or maternal education) [23]. In addition, the maternal education variable was recoded into two categories: not educated (no education at all) and educated (a minimum of primary school education). In addition, the DHS dataset included a household wealth quintile variable, a proxy measure derived from asset ownership, which was originally divided into five categories of 20% each [24]. However, this study’s wealth determinant variable was reclassified into two categories: low income (lower 40%) and high income (upper 60%).
Explanatory variables
We controlled for child and maternal individual-level factors. Child-level factors such as age, sex, diarrhea and fever occurrence in the two weeks before the survey, breastfeeding status at the time of the survey, place of residence, and childbirth type were considered. Maternal individual-level variables such as age, employment status, marital status, and maternal health behavior were also considered. Maternal health behavior was obtained through principal component analysis of three individual-level factors: the mother’s knowledge of Oral Rehydration Salts (ORS), the place of delivery, and immunization records. The maternal education and wealth index also separately doubled as explanatory variables for the income and maternal education decomposition analyses.
Statistical analyses
We conducted a descriptive analysis of the variables, with respondents’ distributions expressed as absolute numbers (percentages) and means (SDs) for categorical and continuous variables, respectively. The analysis was adjusted for sample weight. Additionally, Pearson chi-square tests were performed to assess the relationships between the determinants and explanatory variables.
The risk differences (RDs) between the prevalence of childhood malnutrition among the determinant variables’ categories were calculated separately. For example, suppose that the risk difference is greater than 0. This indicated a higher prevalence of childhood malnutrition among children in poor households (pro-low income inequality) and those born to mothers with no education (pro-no maternal education inequality), and vice versa. The prevalence of childhood malnutrition and the distribution of RDs for each determinant variable were visualized via charts.
We employed the logit Fairlie decomposition technique, a nonlinear variant of the Oaxaca-Blinder decomposition technique. The Fairlie technique decomposes the difference in proportions on the basis of either a probit or logit model. This method was then used to examine outcome differences after adjusting for explanatory variables through logistic regression, with datasets from countries with significant pro-low income and pro-no maternal education inequalities.
Blinder‒Oaxaca decomposition is a counterfactual method that determines the extent to which the difference in the prevalence of childhood malnutrition between the categories of the determinant variables results from the contributory effects of the characteristics [18, 25, 26]. The method divides the childhood malnutrition variable between two groups into two parts: the “explained” or compositional portion and the “unexplained” or structural portion [18, 25, 26]. The “explained” or compositional portion refers to differences attributable to the explanatory variables, whereas the “unexplained” or structural portion captures differences arising from variations in the relationship between explanatory variables and any unmeasured variables [18, 25, 26]. All tests were two-tailed, and p < 0.05 was considered significant.
Descriptive and decomposition analyses were performed using STATA 17, and all charts and figures were drawn with R, a language and environment for statistical computing [27–29].
Results
Survey and sample characteristics
The study analyzed data from 138,782 children residing in 13,788 communities across 27 countries from DHS surveys conducted between 2015 and 2020. The number of children per country ranged from 1,082 in South Africa to 12,033 in Benin, with a median of 466 clusters (Table 1). Most countries included in the study were in Africa, accounting for 18 of 27 countries (Table 1). The remaining six countries were from Asia, while one country each was from the Americas, Europe, and Oceania regions (Table 1). The percentage of children who were wasted or overweight was 10.5%, which varied across countries, with Burundi having the lowest rate at 6.5% and Timor Leste having the highest rate at 29.5% (Table 1).
Table 1.
Description of demographic and health survey data by country and childhood malnutrition prevalence from 2015–2020
| Continent | Country | Survey Year | Number of Children | Number of Clusters | Malnutrition (%) | Low Income Households (%) | No Maternal Education (%) |
|---|---|---|---|---|---|---|---|
| Europe | Albania | 2018 | 2,462 | 631 | 412 (18.3) | 44.5 | 1.1 |
| Africa | Angola | 2016 | 6,407 | 625 | 514 (8.6) | 45.4 | 28.9 |
| Asia | Armenia | 2016 | 1,561 | 304 | 265 (17.7) | 40.4 | 0.0 |
| Africa | Benin | 2018 | 12,033 | 555 | 846 (7.0) | 41.6 | 65.7 |
| Africa | Burundi | 2017 | 6,052 | 554 | 404 (6.5) | 42.5 | 47.5 |
| Africa | Cameroon | 2019 | 4,477 | 428 | 725 (15.5) | 46.0 | 27.0 |
| Africa | Gambia | 2020 | 3,811 | 279 | 264 (7.5) | 42.4 | 44.7 |
| Africa | Guinea | 2018 | 3,430 | 399 | 502 (15.1) | 47.1 | 76.6 |
| Americas | Haiti | 2017 | 5,598 | 449 | 393 (7.4) | 46.6 | 20.1 |
| Africa | Liberia | 2020 | 2,457 | 324 | 179 (8.2) | 48.1 | 36.3 |
| Africa | Malawi | 2016 | 5,178 | 850 | 379 (7.3) | 47.5 | 13.4 |
| Asia | Maldives | 2017 | 2,362 | 260 | 268 (13.3) | 44.7 | 1.2 |
| Africa | Mali | 2018 | 8,588 | 345 | 977 (10.9) | 42.0 | 73.1 |
| Asia | Nepal | 2016 | 2,369 | 375 | 260 (11.0) | 42.2 | 34.5 |
| Africa | Nigeria | 2018 | 11,405 | 1,378 | 1,028 (9.0) | 38.0 | 38.8 |
| Asia | Pakistan | 2018 | 4,151 | 554 | 331 (9.5) | 42.0 | 48.6 |
| Oceania | Papua New Guinea | 2018 | 3,290 | 674 | 602 (18.2) | 40.4 | 24.9 |
| Africa | Rwanda | 2020 | 3,809 | 500 | 271 (6.9) | 43.4 | 12.0 |
| Africa | Senegal | 2019 | 5,531 | 214 | 531 (10.4) | 46.8 | 64.1 |
| Africa | Sierra Leone | 2019 | 4,144 | 564 | 425 (10.5) | 48.1 | 54.2 |
| Africa | South Africa | 2016 | 1,082 | 466 | 171 (16.2) | 47.5 | 2.1 |
| Asia | Tajikistan | 2017 | 5,867 | 366 | 546 (8.8) | 39.2 | 2.7 |
| Africa | Tanzania | 2016 | 8,962 | 607 | 748 (8.5) | 46.4 | 21.5 |
| Asia | Timor-Leste | 2016 | 5,718 | 455 | 1,706 (29.5) | 39.9 | 24.4 |
| Africa | Uganda | 2016 | 4,413 | 688 | 337 (7.8) | 43.2 | 11.2 |
| Africa | Zambia | 2019 | 8,711 | 545 | 821 (9.6) | 47.7 | 10.2 |
| Africa | Zimbabwe | 2015 | 4,914 | 399 | 486 (9.4) | 44.4 | 1.2 |
| 138,782 | 13,788 | 14,390 (10.5) | 43.6 | 33.5 |
On average, 43.6% of the households fell into the low-income category, while 33.5% of the mothers had no formal education (Table 1). Guinea had the highest percentage of mothers with no education at 76.6%, whereas Armenia (0%) and Albania (1.1%) had the lowest percentages. Sierra Leone and Liberia had the highest percentage of low-income households at 48.1%, whereas Nigeria had the lowest at 38% (Table 1).
The mean age of the children included in the study was 28 months, and the study population was evenly split between males and females, with males accounting for 50.6% of the total population (Table 2). Approximately one-third of the mothers of the children had no education (33.5%) and lived in urban areas (33.0%), whereas just over half (56.4%) were in the middle to richest wealth quintiles (Table 2). Most of the mothers of the children in the study were married, between 25 and 34 years old, and employed (Table 2). We found statistically significant income differences in all the explanatory variables except for the child’s age, sex, childbirth type, and maternal employment (Table 2). Similarly, we also found statistically significant maternal education differences in all the explanatory variables except the child’s sex and diarrhea experience in the two weeks preceding the survey (Table 2).
Table 2.
Descriptive statistics of pooled sample characteristics of the demographic and health survey data
| Variables | Overall | Household Income | Maternal Education | ||||
|---|---|---|---|---|---|---|---|
| N = 138,782 | High Income | Low Income | P value1 | Maternal Education | No Maternal Education | P value1 | |
| Age in months Mean (SD) | 28.4 (17.3) | 28.4 | 28.4 | 0.87 | 28.0 | 29.2 | < 0.001 |
| Sex | 0.49 | 0.85 | |||||
| Male | 69,116 (50.6) | 50.7 | 50.4 | 50.5 | 50.6 | ||
| Female | 67,589 (49.4) | 49.3 | 49.6 | 49.5 | 49.4 | ||
| Childbirth Type | 0.08 | 0.004 | |||||
| Single Birth | 132,734 (97.1) | 97.0 | 97.2 | 97.2 | 96.8 | ||
| Multiple Births | 3,972 (2.9) | 3.0 | 2.8 | 2.8 | 3.2 | ||
| Diarrhea in the last 2 weeks preceding the survey | < 0.001 | 0.10 | |||||
| No Diarrhea | 116,081 (85.2) | 85.8 | 84.3 | 85.0 | 85.5 | ||
| Had Diarrhea | 20,213 (14.8) | 14.2 | 15.7 | 15.0 | 14.5 | ||
| Child Fever in the last 2 weeks preceding the survey | < 0.001 | < 0.001 | |||||
| No Fever | 107,760 (79.0) | 80.3 | 77.4 | 79.4 | 78.2 | ||
| Had Fever | 28,623 (21.0) | 19.7 | 22.6 | 20.6 | 21.8 | ||
| Currently Breastfeeding | < 0.001 | < 0.001 | |||||
| No | 84,532 (63.0) | 64.5 | 60.9 | 63.3 | 62.3 | ||
| Yes | 49,715 (37.0) | 35.5 | 39.1 | 36.7 | 37.7 | ||
| Maternal Age (Y) | < 0.001 | < 0.001 | |||||
| 15–24 years | 36,601 (26.8) | 25.6 | 28.4 | 30.11 | 20.2 | ||
| 25–34 years | 68,629 (50.2) | 52.3 | 47.5 | 50.9 | 48.9 | ||
| 35–49 years | 31,476 (23.0) | 22.1 | 24.2 | 19.0 | 31.0 | ||
| Maternal Education* | < 0.001 | ||||||
| No Education | 45,750 (33.5) | 23.4 | 46.6 | N/A | N/A | N/A | |
| Primary | 42,928 (31.4) | 28.4 | 35.3 | ||||
| Secondary | 39,992 (29.3) | 38.8 | 16.9 | ||||
| Higher | 8,029 (5.8) | 9.4 | 1.3 | ||||
| Maternal Marital Status | < 0.001 | < 0.001 | |||||
| Never Married | 6,530 (4.8) | 5.4 | 4.0 | 6.4 | 1.6 | ||
| Married/In Union | 123,035 (90.0) | 89.9 | 90.1 | 87.7 | 94.6 | ||
| Divorced/Widowed/Separated | 7,141 (5.2) | 4.7 | 5.9 | 6.0 | 3.8 | ||
| Maternal Employment | 0.08 | < 0.001 | |||||
| Not Employed | 56,486 (41.3) | 41.7 | 40.8 | 44.1 | 35.8 | ||
| Employed | 80,194 (58.7) | 58.3 | 59.2 | 55.9 | 64.3 | ||
| Residence | < 0.001 | < 0.001 | |||||
| Urban | 45,119 (33.0) | 51.6 | 9.0 | 39.1 | 20.8 | ||
| Rural | 91,587 (67.0) | 48.5 | 91.0 | 60.9 | 79.2 | ||
| Wealth Index* | < 0.001 | ||||||
| Poorest | 30,506 (22.3) | N/A | N/A | N/A | 16.4 | 34.0 | |
| Poorer | 29,057 (21.3) | 18.6 | 26.6 | ||||
| Middle | 27,761 (20.3) | 20.5 | 19.9 | ||||
| Richer | 26,495 (19.4) | 22.3 | 13.5 | ||||
| Richest | 22,885 (16.7) | 22.2 | 5.9 | ||||
| Maternal Health Behavior | < 0.001 | < 0.001 | |||||
| First Quantile (Least) | 47,853 (35.9) | 27.0 | 47.5 | 32.9 | 41.8 | ||
| Second Quantile | 44,560 (33.5) | 34.6 | 31.9 | 34.0 | 32.4 | ||
| Third Quantile | 24,083 (18.1) | 22.6 | 12.3 | 18.6 | 17.1 | ||
| Fourth Quantile | 6,321 (4.8) | 5.9 | 3.2 | 5.5 | 3.2 | ||
| Fifth Quantile (Highest) | 10,402 (7.8) | 9.9 | 5.1 | 9.0 | 5.4 | ||
1Pearson’s X^2
* Variable separately doubles as determinant and explanatory variables for the decomposition analyses
Household wealth
Magnitude and variations in inequality
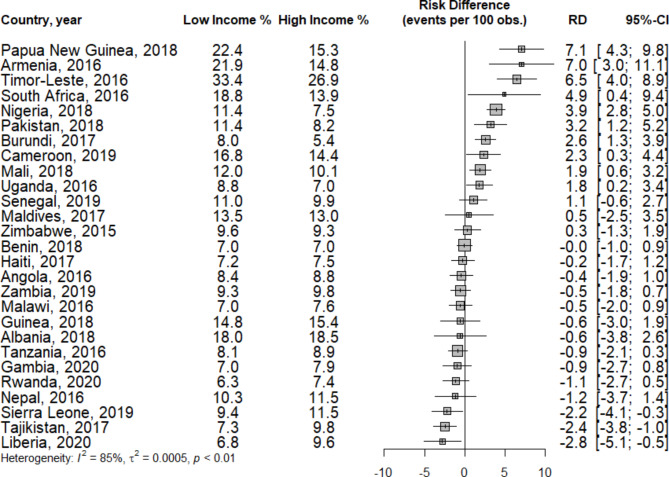
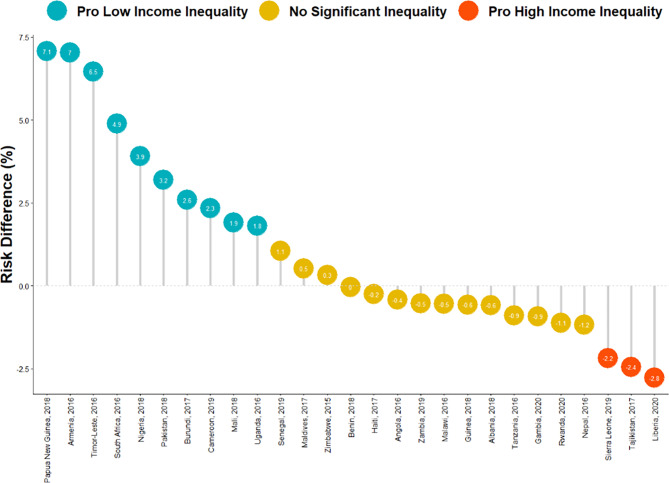
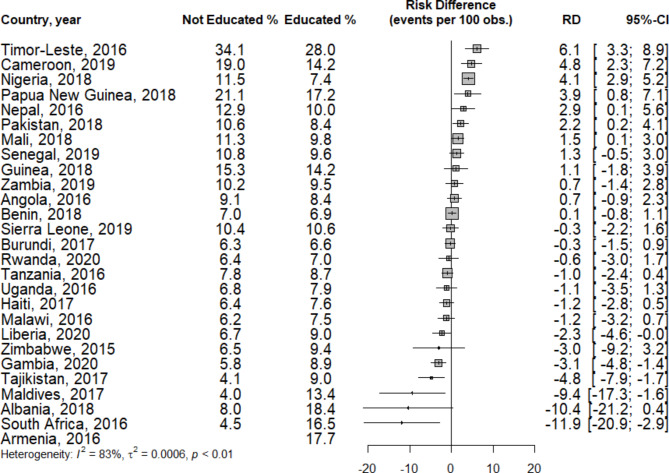
Figures 1 and 2 display the inequality in childhood malnutrition between children residing in low-income and high-income households across the 27 countries examined in this study. In low-income households, the prevalence of childhood malnutrition was highest in Timor-Leste (33.4%), whereas Rwanda had the lowest rate, recorded at 6.3%. For high-income households, Burundi had the lowest prevalence of childhood malnutrition at 5.4%, whereas Timor-Leste had the highest at 26.9%. The majority of the countries (14) did not exhibit significant inequality. However, in 10 countries (Armenia, Burundi, Cameroon, Mali, Nigeria, Pakistan, Papua New Guinea, South Africa, Timor Leste, Uganda), children living in low-income households had a significantly greater prevalence of malnutrition (pro-low-income inequality), with risk differences ranging from 1.8% (95% CI 0.1–3.4) in Uganda to 7.1% (95% CI 4.3–9.8) in Papua New Guinea. In contrast, only three countries (Liberia, Tajikistan, and Sierra Leone) presented significant pro-high-income inequality, with risk differences of -2.8% (95% CI -5.1–0.5), -2.4% (95% CI -3.8–1.0), and − 2.2% (95% CI 4.1–0.3), respectively.
Fig. 1.
Forest plot of the risk difference in the prevalence of childhood malnutrition between children in low-income and high-income households, by country
Fig. 2.
Risk difference in the prevalence of childhood malnutrition between children in low-income and high-income households, by country
Decomposition of inequality
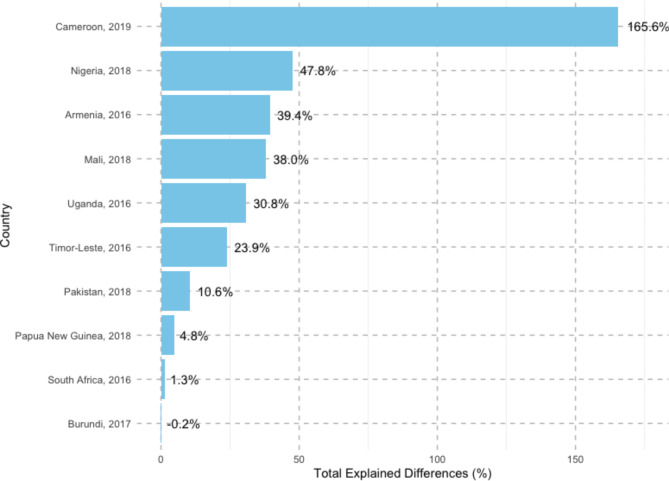
Figure 3 illustrates the proportion of differences in childhood malnutrition prevalence between low-income and high-income households in the 10 pro-low-income inequality countries, which can be attributed to explanatory variables (explained or compositional effects). The largest explained difference is observed in Cameroon, where 165.6% of the gap in childhood malnutrition between households is attributed to these factors. In contrast, the explained differences are much smaller in other countries, including Nigeria (47.8%), Armenia (39.4%), Mali (38.0%), Uganda (30.8%), and Timor-Leste (23.9%). The explanatory variables accounted for an even smaller portion of the differences in Pakistan (10.6%), Papua New Guinea (4.8%), and South Africa (1.3%). Burundi (-0.2%) presents a negatively explained difference, indicating a very slight narrowing of the relative gap by the explanatory variables, structural effects not accounted for by the explanatory variables, and other unmeasured determinants responsible for the differences in childhood malnutrition prevalence between low-income and high-income households.
Fig. 3.
Total compositional differences in childhood malnutrition between children in low-income and high-income households, by country1
1Logit Fairlie Decomposition Analysis estimates of the total explained difference as a portion of the overall difference
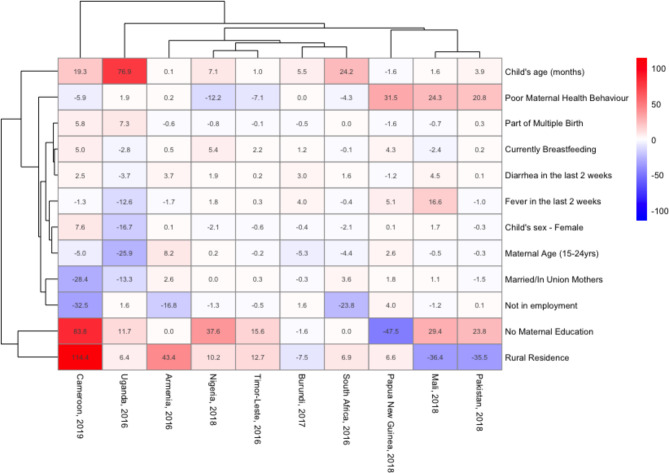
The key explanatory variables driving the explained differences in childhood malnutrition prevalence between low-income households and high-income households differed across countries. Figure 4 highlights the contribution and magnitude of the decomposition of inequality caused by the compositional effects of explanatory variables, with a negative percentage indicating a narrowing of the relative gap and a positive percentage indicating a widening gap between low-income and high-income households. Armenia and Cameroon experienced the most significant widening of the relative gap in rural residence among the explanatory variables. No maternal education contributed the most to the widening gap in Nigeria, Timor Leste, Mali, and Pakistan. Moreover, the child’s age contributed the most to the widening gap in Uganda, South Africa, and Burundi and poor maternal health behavior in Papua New Guinea.
Fig. 4.
Compositional effects of the determinants of childhood malnutrition in low-income and high-income households, by country1
1 Logit Fairlie Decomposition Analysis estimates of the compositional explained difference attributable to the explanatory variables
In contrast, maternal unemployment most narrowed the gap in Cameroon, Armenia, and South Africa. Rural residence had the highest negative percentage contribution among the explanatory variables in Pakistan, Mali, and Burundi. Poor maternal health behavior in Nigeria and Timor Leste, no maternal education in Papua New Guinea, and maternal age in Uganda were the factors that most narrowed the gap.
Among these explanatory variables, no maternal education and rural residence contributed the most and were clustered together. The child’s age and poor maternal health behavior also had significant contributions. The child’s sex, maternal age, and fever during the two weeks preceding the survey and birth type, breastfeeding status, and diarrhea during the two weeks preceding the survey formed two separate clusters, which were then clustered together at a higher level and joined by the maternal unemployment and marital status cluster.
Maternal education
Magnitude and variations in inequality
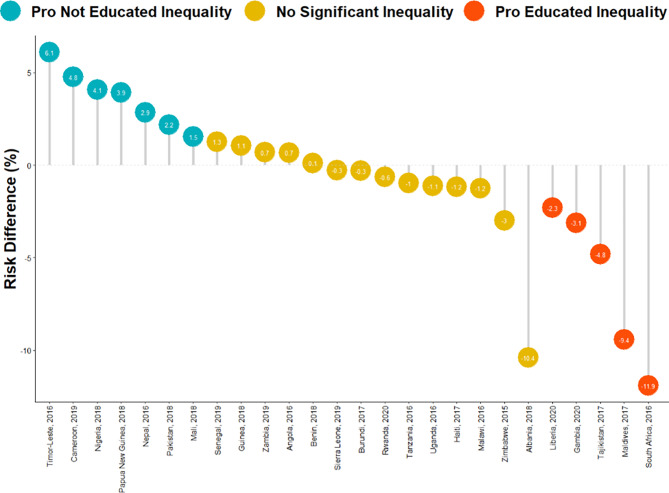
Figures 5 and 6 depict the childhood malnutrition inequality measure between children of uneducated mothers and those with educated mothers across 27 countries. Among children with educated mothers, Timor-Leste had the highest prevalence (28.0%) of childhood malnutrition, whereas Burundi had the lowest, at 6.6%. For children with uneducated mothers, Maldives (4.0%) and Timor-Leste (34.1%) presented the lowest and highest prevalence rates of childhood malnutrition, respectively. Notably, all the women respondents in Armenia were educated.
Fig. 5.
Forest plot of the risk difference in the prevalence of childhood malnutrition between children of uneducated mothers and those of educated mothers, by country
Fig. 6.
Risk difference in the prevalence of childhood malnutrition between children of uneducated mothers and those of educated mothers, by country
Among these countries, 14 displayed no significant inequality. However, 7 countries, Cameroon, Mali, Nepal, Nigeria, Pakistan, Papua New Guinea, and Timor Leste, exhibited pro-no-maternal education inequality, with a significantly higher prevalence of childhood malnutrition among mothers with no education. The risk differences ranged from 1.5% (95% CI 0.1–3.0) in Mali to 6.1% (95% CI 3.3–8.9) in Timor Leste. On the other hand, 5 countries (Gambia, Liberia, Maldives, South Africa, and Tajikistan) had significant pro-maternal education inequality, with risk differences varying from − 11.9% (95% CI -20.9– -2.9) in South Africa to -2.3% (95% CI -4.6–0.004) in Liberia. All mothers of children in Armenia were educated, and hence, no results were returned.
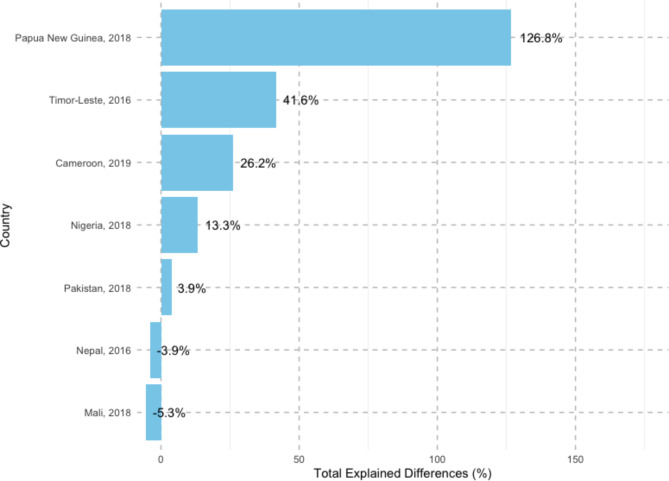
Decomposition of inequality
Figure 7 shows the percentage of differences in the prevalence of childhood malnutrition in educated and uneducated mothers in the 7 pro-no maternal education countries attributable to explanatory variables (explained or compositional effects). Papua New Guinea (126.8%) exhibited the largest explained difference, followed by Timor-Leste (41.6%), Cameroon (26.2%), Nigeria (13.3%), and Pakistan (3.9%). These countries are listed in descending order of explained differences in childhood malnutrition between these two groups of mothers. In contrast, Nepal (-3.9%) and Mali (-5.3%) show negative total explained differences, indicating a narrowing of the relative gap and that the difference is due to structural effects and unmeasured variables (Fig. 7).
Fig. 7.
Total compositional differences in childhood malnutrition between children born to uneducated and educated mothers, by country1
1 Logit Fairlie Decomposition Analysis estimates of the total explained difference as a portion of the overall difference
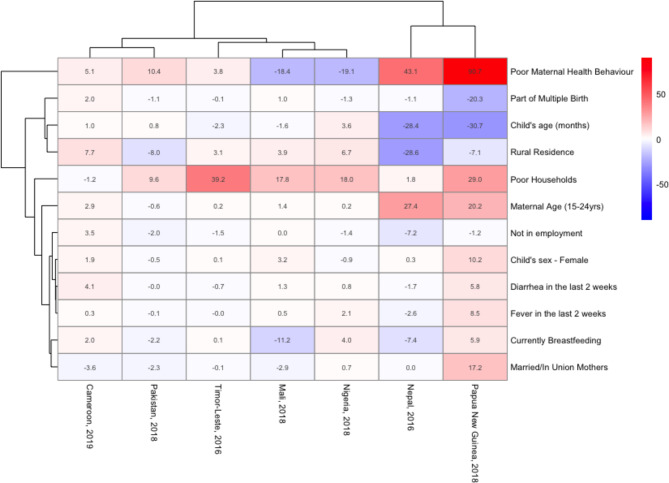
Figure 8 provides a detailed breakdown of the contribution and magnitude of the key explanatory variables driving the explained differences in childhood malnutrition inequality, with a negative percentage contribution indicating a reduction in the relative gap and a positive percentage contribution indicating an increase in the relative gap among educated and uneducated mothers. Among the explanatory variables, poor households had the most significant relative gap widening in Timor Leste, Mali, and Nigeria. In Nepal, Papua New Guinea, and Pakistan, poor maternal health behavior accounted for the greatest contribution to widening the gap; rural residence made the highest percentage contribution in Cameroon. Conversely, poor maternal health behavior had the most significant gap-narrowing effect in Nigeria and Mali. Rural residence in Nepal and Pakistan, the child’s age in Papua New Guinea and Timor Leste, and marital status in Cameroon were the factors that narrowed the gap the most. Among the explanatory variables, poor households, poor maternal health behavior, and maternal age contributed the most and were the most consistent contributors in at least 5 countries.
Fig. 8.
Compositional effects of the determinants of childhood malnutrition in children born to uneducated and educated mothers, by country1
1 Logit Fairlie Decomposition Analysis estimates of the compositional explained difference attributable to the explanatory variables
Discussion
The prevalence of childhood malnutrition (10.5%) varied across countries, ranging from 6.5% in Burundi to 29.5% in Timor Leste. The prevalence of childhood malnutrition in low-income households was 11.0%, and it was 10.7% among mothers without education. Our review of childhood malnutrition inequality revealed that 10 countries had a significantly greater prevalence of malnutrition among children living in low-income households (pro-low-income inequality). In comparison, only three countries showed significant pro-high-income inequality. However, in our exploration of childhood malnutrition inequality between educated and uneducated mothers, 7 had pro-no-maternal education inequality, and five had pro-maternal education inequality.
Among the 10 pro-low-income countries, Cameroon (165.6%) had the largest explained difference (compositional effects) in childhood malnutrition between households, whereas the least explained differences were observed in countries such as Pakistan (10.6%), Papua New Guinea (4.8%), and South Africa (1.3%). Burundi (-0.2%) showed a slight negative explained difference (-0.2%), indicating a narrowing of the gap by the explanatory variables. The explanatory variables contributing to the most significant widening of the gap varied among countries. This included the child’s age, maternal education, maternal health behavior, and place of residence. Conversely, factors such as maternal employment, maternal age, maternal marital status, and child sex significantly contributed to narrowing the gap in several countries. The analysis results revealed the influence of maternal education on childhood malnutrition inequality in the 7 pro-no maternal education inequality countries, with Papua New Guinea showing the largest explained difference (126.8%), followed by Timor-Leste, Cameroon, Nigeria, and Pakistan. In contrast, Nepal and Mali presented negative explained differences, suggesting a narrowing of the malnutrition gap between educated and uneducated mothers by the explanatory variables. Factors such as the household wealth index, maternal health behavior, and maternal age contributed the most to the gap across the pro-no maternal education inequality countries. Notably, childbirth type, child age, place of residence, and breastfeeding status played significant roles in narrowing the relative gap in several countries.
Prior decomposition studies assessing childhood malnutrition income inequality have also revealed that maternal education, maternal health behavior, place of residence, and child’s age widened the relative gap, similar to our findings of the most significant explanatory variables across 10 pro-low-income countries [30–34]. Low levels of education among mothers in low-income households have been linked with limited knowledge of nutrition, inadequate dietary practices, diminished decision-making power, and poor health-seeking behavior [33, 35]. In rural areas, children’s nutritional outcomes are affected by their corresponding lower parental income levels, unsanitary living conditions, and larger family sizes [36, 37]. Maternal health behavior also plays a pivotal role in shaping children’s nutritional outcomes, with those with better access to facilities, health information, and healthcare services and greater financial resources being more likely to provide their children with better nutritional options [36, 38]. Moreover, the dire economic situation of low-income households has been postulated to be associated with poor health behaviors, unhealthy eating habits, limited access to healthcare services, and substandard living conditions, all of which negatively impact child health [33, 39, 40]. Additionally, child age has also been previously highlighted as a significant predictor of malnutrition, particularly among younger children who are more vulnerable to nutritional deficiencies [41, 42].
Similar to our findings from exploring childhood malnutrition inequality between educated and uneducated mothers, household wealth, maternal age, and poor maternal health behaviors have previously been identified as significant contributors to education inequality [43–45]. As discussed earlier, there is an interconnectedness between the household wealth index and maternal education. Improving a household’s economic conditions directly enhances nutritional availability and indirectly influences other determinants, such as health behaviors [46]. With respect to maternal age, younger mothers often provide poorer quantity and quality of care and nursing for their children because of psychological and physiological immaturity, readiness for pregnancy and childbirth, and typically disadvantageous socioeconomic and power dynamics [47, 48]. Conversely, other studies have noted that older maternal age can be associated with childhood malnutrition due to factors such as reduced metabolic activity, a sedentary lifestyle, and overall maternal health status [49, 50].
In addition to the diverse range of the most significant compositional contributors to inequality between income and education groups, the number and magnitude of the compositional contributors varied within countries and between countries. Furthermore, within groups, contributors to the widening of the relative inequality gap in one country could be the reverse in another country and vice versa. Moreover, some of these compositional contributors had similar percentage contributions across countries and between groups.
This contrasting and varied impact of socioeconomic determinants, such as income, education, residence, and employment, may depend on the country’s profile. For example, children from lower socioeconomic backgrounds in high-income countries and those from higher socioeconomic backgrounds in low- to middle-income countries are most at risk of being overweight [51, 52]. In high-income countries, poor dietary and lifestyle practices among children from lower socioeconomic backgrounds have been identified as key contributors to this increased risk [53]. Similarly, in low- to middle-income countries, being overweight is often seen as a status symbol among children from higher socioeconomic backgrounds [53]. Conversely, children from higher socioeconomic backgrounds in high-income countries tend to adopt healthier diets and lifestyles, resulting in better nutrition, unlike their counterparts in low- to middle-income countries [53]. On the other hand, children from lower socioeconomic backgrounds in low- to middle-income countries are more likely to face challenges such as food availability and accessibility, limited access to healthcare, and poor educational environments, leading to childhood undernutrition [53].
A systematic review and meta-analysis by Alao et al. (2021) revealed a consistently greater risk of child undernutrition in lower socioeconomic households, regardless of the country’s economic profile [40]. Furthermore, similar patterns of inequality were noted in countries with comparable socioeconomic profiles [40]. They also observed regional clustering of child undernutrition in contiguous countries, likely due to shared geopolitical, environmental, and food security challenges [40].
The intersectionality between income, education, and the explanatory variables at the individual, community, and structural levels demonstrates how multiple disadvantages compound to exacerbate malnutrition and drive health disparities [54]. An unaccounted biological factor, race, has long been considered a key driver of health inequalities [55]. For example, marginalized racial groups with lower socioeconomic status face a heightened risk of childhood malnutrition [56]. Additionally, traditional gender roles in childcare and household responsibilities increase children’s vulnerability to malnutrition [57, 58]. Gender inequality, particularly in female-headed households, also contributes to elevated risk [57, 58]. Environmental factors, such as climate change, further exacerbate these issues by reducing crop yields, diminishing nutrient quality, and lowering dietary diversity, all of which negatively impact food security and childhood nutrition [59].
Our results underscore the intricate blend of factors shaping malnutrition inequality, further highlighting their importance in regional, subregional, and global responses to malnutrition.
Policy and practice implications
This study highlights the need for a country-specific approach to addressing childhood malnutrition. The prevalence of childhood malnutrition and the factors contributing to childhood malnutrition inequality vary significantly across countries, with the household wealth index, maternal health behavior, place of residence, maternal education, and child and maternal ages being key contributors. Therefore, policies and response programs must be tailored to each country’s context, addressing the underlying factors contributing to childhood malnutrition.
Additionally, our study revealed significant low-income/high-income and no-maternal education/maternal education disparities in childhood malnutrition prevalence. These findings suggest the need for targeted interventions that address the specific needs of these groups. For example, interventions to improve maternal education, increase access to healthcare services, and improve maternal health behavior in low-income households can help reduce the prevalence of childhood malnutrition in this group.
Fundamentally, policymakers should prioritize nutrition-specific interventions, such as micronutrient supplementation and infant and young child feeding practices [60]. Concurrently, investments in nutrition-sensitive interventions, including agriculture and social welfare systems, are equally important [61]. Broader socioeconomic policies that aim to reduce poverty, improve education, and enhance living conditions in poor communities must also be integrated [62, 63].
Finally, our analysis provides valuable insights into the factors contributing to childhood malnutrition in different countries and highlights the need for further research. Governments and international organizations should prioritize the collection of high-quality data on childhood malnutrition prevalence and invest in research to better understand the underlying factors and inform transformative interventions.
Study limitations
The limitations of our study are primarily due to the use of secondary data. The explanatory variables we could select were dependent on availability, and there is a possibility of recall bias in the data. Household income information was unavailable in the DHS survey, so we relied on household wealth index quintiles from asset ownership as a substitute. The Blinder-Oaxaca decomposition method used in this study does not establish causality but provides strong evidence of disparities between the two groups. A key strength of our study was the use of nationally representative and generalizable DHS datasets from 27 countries across five continents, which are typically high quality with high response rates, a sound methodology, and well-documented data sources. In addition, these surveys utilize standardized modules and protocols, enabling cross-country comparisons.
Conclusions
We examined childhood malnutrition prevalence across 27 countries from studies conducted between 2015 and 2020 and provided evidence on inequality in low- and high-income households and maternal education levels. The results showed that the prevalence of childhood malnutrition varied across countries. While most countries did not exhibit significant inequality, some showed pro-low-income or pro-no-maternal education inequality. The most common causes of inequality were the household wealth index, maternal health behavior, place of residence, maternal education, and child and maternal age. At the same time, other explanatory variables contributed to inequality in different countries. This study highlights the importance of addressing the socioeconomic determinants of childhood malnutrition to reduce inequality and improve child health.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank the DHS program for their support: free access to the dataset used.
Author contributions
All the authors participated in discussions about the data source and planning of the analyses and critically revised successive versions of the paper. MAI and OAU conceived the study, MAI and S.A. performed the analyses, and MAI prepared the first draft of the paper. All the authors have reviewed and approved the final version of the paper.
Funding
None declared.
Data availability
All the data and datasets generated and/or analyzed during the current study are available on the DHS program website https://dhsprogram.com/data.
Declarations
Ethics approval and consent to participate
This study is based on a secondary dataset from the DHS; therefore, ethical approval was not needed.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.UNICEF. State of the World’s children 2019: children, food and nutrition. Unicef. 2019. 1–258 p.
- 2.Poda GG, Hsu CY, Chao JCJ. Factors associated with malnutrition among children < 5 years old in Burkina Faso: evidence from the demographic and health surveys IV 2010. Int J Qual Health Care. 2017;29(7):901–8. [DOI] [PubMed] [Google Scholar]
- 3.Bain LE, Awah PK, Geraldine N, Kindong NP, Sigal Y, Bernard N, et al. Malnutrition in Sub - Saharan Africa: Burden, causes and prospects. Pan Afr Med J. 2013;15:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Feei MZ, Wang CW, Lee YY, Editorial. Malnutrition: a cause or a consequence of poverty? Front Public Health. 2022;9. [DOI] [PMC free article] [PubMed]
- 5.FAO, IFAD, UNICEF, WFP, WHO. Food Security and Nutrition in the World the State of Building Climate Resilience for Food Security and Nutrition. Volume 7. Food and Agriculture Organization of the United Nations; 2018. pp. 820–1.
- 6.Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382(9890):427–51. [DOI] [PubMed] [Google Scholar]
- 7.UNICEF/WHO/WORLD BANK. Levels and trends in child malnutrition UNICEF / WHO / World Bank Group. Joint Child Malnutrition Estimates Key findings of the 2021 edition. Vol. 24, World Health Organization. 2021.
- 8.Wells JC, Sawaya AL, Wibaek R, Mwangome M, Poullas MS, Yajnik CS, et al. The double burden of malnutrition: aetiological pathways and consequences for health. Lancet. 2020;395(10217):75–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO. The double burden of malnutrition. Geneva; 2017.
- 10.WHO. Double-duty actions for nutrition policy brief. Who/Nmh/Nhd/172. 2017;5:10.
- 11.Nguyen PH, Scott S, Headey D, Singh N, Tran LM, Menon P, et al. The double burden of malnutrition in India: Trends and inequalities (2006–2016). PLoS ONE. 2021;16(2):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perez-Escamilla R, Bermudez O, Buccini GS, Kumanyika S, Lutter CK, Monsivais P et al. Nutrition disparities and the global burden of malnutrition. BMJ. 2018;361. [DOI] [PMC free article] [PubMed]
- 13.Ghattas H, Acharya Y, Jamaluddine Z, Assi M, El Asmar K, Jones AD. Child-level double burden of malnutrition in the MENA and LAC regions: prevalence and social determinants. Matern Child Nutr. 2020;16(2):e12923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seferidi P, Hone T, Duran AC, Bernabe-Ortiz A, Millett C. Global inequalities in the double burden of malnutrition and associations with globalisation: a multilevel analysis of Demographic and Health Surveys from 55 low-income and middle-income countries, 1992–2018. Lancet Glob Health. 2022;10(4):e482–90. [DOI] [PMC free article] [PubMed]
- 15.Shinsugi C, Gunasekara D, Gunawardena NK, Subasinghe W, Miyoshi M, Kaneko S, et al. Double burden of maternal and child malnutrition and socioeconomic status in urban Sri Lanka. PLoS ONE. 2019;14(10):e0224222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Popkin BM, Corvalan C, Grummer-Strawn LM. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet. 2020;395(10217):65–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Otten HS, Seferidi P. Prevalence and socioeconomic determinants of the double burden of malnutrition in mother{extendash}child pairs in Latin America and the Caribbean. BMJ Nutr Prev Health. 2022. [DOI] [PMC free article] [PubMed]
- 18.Rahimi E, Hashemi Nazari SS. A detailed explanation and graphical representation of the Blinder-Oaxaca decomposition method with its application in health inequalities. Emerg Themes Epidemiol. 2021;18(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Menon S, Peñalvo JL. Actions targeting the double burden of Malnutrition: a scoping review. Nutrients. 2020;12(1). [DOI] [PMC free article] [PubMed]
- 20.Croft TN, Blake W, Zachary, Courtney K. Allen. Guide to DHS Statistics - DHS-8 [Internet]. 2023. Available from: www.DHSprogram.com.
- 21.World Health Organization. WHO Child Growth standards. Dev Med Child Neurol. 2006;51(12):1002–1002. [Google Scholar]
- 22.de Onis M, Blössner M. The World Health Organization Global Database on child growth and malnutrition: methodology and applications. Int J Epidemiol. 2003;32(4):518–26. [DOI] [PubMed] [Google Scholar]
- 23.Ijaiya MA, Anjorin S, Uthman OA. Individual and contextual factors associated with childhood malnutrition: a multilevel analysis of the double burden of childhood malnutrition in 27 countries. Glob Health Res Policy. 2022;7(1):44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rutstein SO. Steps to constructing the new DHS Wealth Index. 2016;6.
- 25.Blinder A. Wage discrimination: reduced form and structural estimates. J Hum Resour. 1973;8(4):436–55. [Google Scholar]
- 26.Oaxaca R. Male-female wage differentials in Urban Labor Markets. Int Econ Rev (Philadelphia). 1973;14(3):693–709. [Google Scholar]
- 27.StataCorp. Stata Statistical Software. College Station, TX: StataCorp LLC; 2021. [Google Scholar]
- 28.R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2020. [Google Scholar]
- 29.Jann B. The Blinder-Oaxaca decomposition for linear regression models. The Stata Journal. 2008;8(4): 453 - 479.
- 30.Novignon J, Aboagye E, Agyemang OS, Aryeetey G. Socioeconomic-related inequalities in child malnutrition: evidence from the Ghana multiple indicator cluster survey. Health Econ Rev. 2015;5(1):34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Singh SK, Srivastava S, Chauhan S. Inequality in child undernutrition among urban population in India: a decomposition analysis. BMC Public Health. 2020;20(1):1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chauhan BG, Chauhan S, Chaurasia H. Decomposing the gap in child malnutrition between poor and non-poor in Sierra Leone. J Public Health (Bangkok). 2019;27(1):119–27. [Google Scholar]
- 33.Kumar A, Singh A. Decomposing the gap in Childhood Undernutrition between Poor and non–poor in Urban India, 2005–06. PLoS ONE. 2013;8(5):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bhusal UP. Poor and non-poor gap in under-five child nutrition: a case from Nepal using Blinder-Oaxaca decomposition approach. BMC Health Serv Res. 2022;22(1):1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miller JE, Rodgers YV. Mother’s education and children’s nutritional status: new evidence from Cambodia. Asian Dev Rev. 2009;26(1):131–65. [Google Scholar]
- 36.Fagbamigbe AF, Kandala NB, Uthman AO. Demystifying the factors associated with rural–urban gaps in severe acute malnutrition among under-five children in low- and middle-income countries: a decomposition analysis. Sci Rep. 2020;10(1). [DOI] [PMC free article] [PubMed]
- 37.Tariq I, Khan JI, Malik MA. Decomposing acute malnutrition by educational inequality of mother’s among under five children in Jammu and Kashmir. Sci Rep. 2023;13(1). [DOI] [PMC free article] [PubMed]
- 38.Mussa R. A matching decomposition of the rural–urban difference in malnutrition in Malawi. Health Econ Rev. 2014;4(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Monazza A, Geeta K. Parental education and child health: Understanding the pathways of impact in Pakistan. CSAE WPS/2. 2010.
- 40.Alao R, Nur H, Fivian E, Shankar B, Kadiyala S, Harris-Fry H. Economic inequality in malnutrition: a global systematic review and meta-analysis. BMJ Glob Health [Internet]. 2021;6(12). https://gh.bmj.com/content/6/12/e006906 [DOI] [PMC free article] [PubMed]
- 41.Al-zangabila K, Poudel Adhikari S, Wang Q, Sunil TS, Rozelle S, Zhou H. Alarmingly high malnutrition in childhood and its associated factors: a study among children under 5 in Yemen. Medicine. 2021;100(5). [DOI] [PMC free article] [PubMed]
- 42.Lopes WC, Marques FKS, De Oliveira CF, Rodrigues JA, Silveira MF, Caldeira AP, et al. Infant feeding in the first two years of life. Revista Paulista De Pediatria. 2018;36(2):164–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Paramashanti BA, Dibley MJ, Alam A, Huda TM. Wealth- and education-related inequalities in minimum dietary diversity among Indonesian infants and young children: a decomposition analysis. Glob Health Action. 2022;15(1):2040152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fagbamigbe AF, Kandala NB, Uthman OA. Decomposing the educational inequalities in the factors associated with severe acute malnutrition among under-five children in low- and middle-income countries. BMC Public Health. 2020;20(1):555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Musheiguza E, Mahande MJ, Malamala E, Msuya SE, Charles F, Philemon R et al. Inequalities in stunting among under-five children in Tanzania: decomposing the concentration indexes using demographic health surveys from 2004/5 to 2015/6. Int J Equity Health. 2021;20(1). [DOI] [PMC free article] [PubMed]
- 46.Kia AA, Goodarzi S, Asadi H, Khosravi A, Rezapour A. A Decomposition Analysis of Inequality in Malnutrition among under Five Children in Iran: Findings from Multiple Indicator Demographic and Health Survey, 2010 [Internet]. Vol. 48, Iran J Public Health. 2019. http://ijph.tums.ac.ir [PMC free article] [PubMed]
- 47.Wemakor A, Garti H, Azongo T, Garti H, Atosona A. Young maternal age is a risk factor for child undernutrition in Tamale Metropolis, Ghana. BMC Res Notes. 2018;11(1). [DOI] [PMC free article] [PubMed]
- 48.Nguyen PH, Sanghvi T, Tran LM, Afsana K, Mahmud Z, Aktar B et al. The nutrition and health risks faced by pregnant adolescents: insights from a cross-sectional study in Bangladesh. PLoS ONE. 2017;12(6). [DOI] [PMC free article] [PubMed]
- 49.Sarker AR, Hossain Z, Morton A. Drivers and distribution of the household-level double burden of malnutrition in Bangladesh: analysis of mother–child dyads from a national household survey. Public Health Nutr. 2022;25(11):3158–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.UNICEF. The Impact of Poor Sanitation on Nutrition. Sanitation and Hygiene Applied Research for Equity. 2014;1–12.
- 51.Noonan RJ. Prevalence of childhood overweight and obesity in Liverpool between 2006 and 2012: evidence of widening socioeconomic inequalities. Int J Environ Res Public Health. 2018;15(12). [DOI] [PMC free article] [PubMed]
- 52.World Health Organization. Report of the Commission on Ending Childhood Obesity. Geneva; 2016.
- 53.Wu S, Ding Y, Wu F, Li R, Hu Y, Hou J et al. Socio-economic position as an intervention against overweight and obesity in children: a systematic review and meta-analysis. Sci Rep. 2015;5. [DOI] [PMC free article] [PubMed]
- 54.Simkus A, Holtz KD, Twombly EC. An intersectionality framework for identifying relevant covariates in health equity research. Frontiers in Public Health. Volume 12. Frontiers Media SA; 2024. [DOI] [PMC free article] [PubMed]
- 55.López N, Health, Inequities, Social Determinants, and Intersectionality [Internet]., Washington DC. 2016 [cited 2024 Sep 28]. (Discussion Paper). https://nam.edu/wp-content/uploads/2016/12/Health-Inequities-Social-Determinants-and-Intersectionality.pdf
- 56.Taborda Restrepo PA. Intersectional configuration of infant mortality due to malnutrition in Colombia: a mini-review. Front Public Health. 2024;12. [DOI] [PMC free article] [PubMed]
- 57.Mkandawire E, Bisai C, Dyke E, Dressel A, Kantayeni H, Molosoni B et al. A qualitative assessment of gender roles in child nutrition in Central Malawi. BMC Public Health. 2022;22(1). [DOI] [PMC free article] [PubMed]
- 58.Ashagidigbi WM, Ishola TM, Omotayo AO. Gender and occupation of household head as major determinants of malnutrition among children in Nigeria. Sci Afr. 2022;16.
- 59.World Food Programme. Climate Crisis and Malnutrition A case for acting now OVERVIEW [Internet]. 2021 [cited 2024 Sep 28]. https://www.wfp.org/publications/climate-crisis-and-malnutrition-case-acting-now
- 60.Bhutta ZA, Das JK, Rizvi A, Gaffey MF, Walker N, Horton S et al. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? The Lancet [Internet]. 2013;382(9890):452–77. https://www.sciencedirect.com/science/article/pii/S0140673613609964 [DOI] [PubMed]
- 61.Ruel MT, Alderman H. Nutrition-sensitive interventions and programmes: how can they help to accelerate progress in improving maternal and child nutrition? Lancet. 2013;382(9891):536–51. [DOI] [PubMed] [Google Scholar]
- 62.Marmot M, Friel S, Bell R, Houweling TAJ, Taylor S. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372(9650):1661–9. [DOI] [PubMed] [Google Scholar]
- 63.Haines A, Sanders D, Lehmann U, Rowe AK, Lawn JE, Jan S, et al. Achieving child survival goals: potential contribution of community health workers. Lancet. 2007;369(9579):2121–31. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All the data and datasets generated and/or analyzed during the current study are available on the DHS program website https://dhsprogram.com/data.