Abstract
Transmigration of mandibular canine teeth is a rare dental anomaly characterized by the tooth's aberrant migration through the alveolar bone. This deviation from the expected eruption pathway can lead to tooth impaction, root resorption, periodontal problems, and aesthetic concerns. The exact cause of transmigration is not fully understood, but it is believed to be influenced by a combination of genetic, developmental, and environmental factors. Early diagnosis and appropriate treatment are essential to prevent complications and achieve optimal functional and aesthetic outcomes.
This case report presents a 19-year-old female with impacted left mandibular canine teeth. An interdisciplinary approach involving orthodontic therapy and surgical exposure to disimpact the transmigrated canine into the normal occlusal position. The treatment utilized modified orthodontic mechanics, including uprighting springs and temporary anchorage devices (TADs) to treat transmigration. This case also highlights the importance of early diagnosis and timely intervention for transmigrated canine teeth to prevent complications and achieve optimal aesthetic and functional outcomes.
Keywords: impaction, mandibular canine, tads, transmigration, uprighting spring
Introduction
The incidence of impaction in mandibular canines is significantly lower than that of impacted maxillary canines. While mandibular canine impaction ranges from 0.05% to 0.4%, maxillary canine impaction is more prevalent, occurring in 0.9%-2.2% of the cases [1]. Impacted teeth usually stay on the same side of the jaw, but sometimes they can move to a different location. An impacted tooth that crosses over the midline to the other side of the jaw is said to have undergone transmigration [2]. Transmigration is uncommon and only occurs with impacted canines. These teeth can move from one side of the jaw to the other. There is limited information on the transmigration of lateral incisors or premolars [3].
The aetiology and exact mechanism of canine transmigration remain uncertain. However, several factors, including premature deciduous tooth loss, primary canine retention, dental crowding, odontomas, supernumerary teeth, and increased length of canine crowns, are believed to contribute to this phenomenon. Individuals with canine transmigration frequently exhibit additional dental abnormalities, such as missing mandibular lateral incisors or second premolars, enamel developmental issues, fewer teeth overall, or impacted maxillary canines [4].
Canine transmigration is more prevalent on the left side of the mandible than on the right and occurs more frequently in females compared to males in a 1.6:1 ratio. Unilateral transmigration occurs more frequently than bilateral transmigration. Interestingly, bilateral transmigration of impacted mandibular canines can occur even in the presence of adequate eruption space. Transmigration can lead to root resorption, increase sensitivity of neighbouring teeth and potentially causing discomfort or pain for the patient [5].
Mupparapu's classification categorizes transmigrated mandibular canines into five types, with type 1 being the most prevalent. Early detection and evaluation of the degree of transmigrated canine are essential for preventing impaction and mitigating related aesthetic and functional complications [6]. Untreated or improperly managed impacted canines can result in adverse sequelae, including external root resorption of adjacent teeth, particularly the incisors, aesthetic compromise, misalignment of neighbouring teeth, reduced dental arches, increased incidence of cyst formation with impaction, and ultimately, Irremediable damage that may lead to tooth loss [4].
This case study presents a comprehensive approach to managing a transmigrated mandibular canine in a 19-year-old female, involving a collaborative effort between orthodontic and surgical treatment modalities. The treatment plan incorporated modified orthodontic techniques and surgical intervention to successfully address the transmigration.
Case presentation
A 19-year-old female presented to our dental clinic with a concerns of forwardly placed upper front teeth and spacing in both upper and lower teeth. Extraoral examination exhibited a convex facial profile with obtuse nasolabial angle and competent lips (Figure 1).
Figure 1. Pre-treatment extraoral photographs: frontal view (A), frontal smiling view (B), and profile view (C).
Intraoral examination revealed that the patient had retained deciduous canines in the first and third quadrants with an unerupted canine in the third quadrant and a palatally present canine in the first quadrant. She also had crossbite in relation to the left side with the lower midline shifted toward the right by 1mm. She presented with class II molar on the right and class 1 molar on the left side (Figure 2).
Figure 2. Pre-treatment intraoral photographs: right occlusion (A), anterior occlusion (B), left occlusion (C), maxillary arch (D), mandibular arch (E).
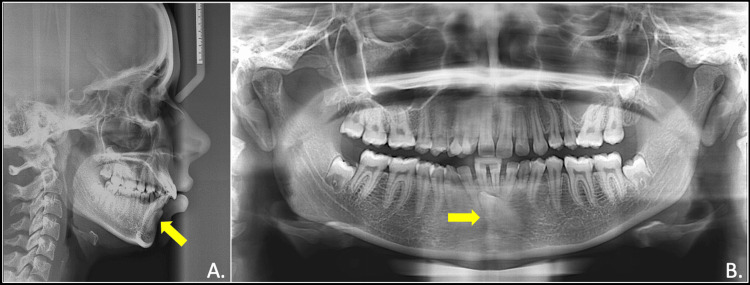
The panoramic radiograph examination showed unfavourable eruption pathway for the mandibular permanent left canines and developing third molars in upper left, lower right, and left quadrants. Cephalometric analysis revealed class I skeletal base and a normodivergent growth pattern with proclined and forwardly placed maxillary and mandibular incisors. The lips were normally placed in relation to the E-line (aesthetic line) (Figure 3).
Figure 3. Pre-treatment radiographs showing impacted mandibular canine (yellow arrow): lateral cephalogram (A) and OPG (B).
OPG: orthopantomogram
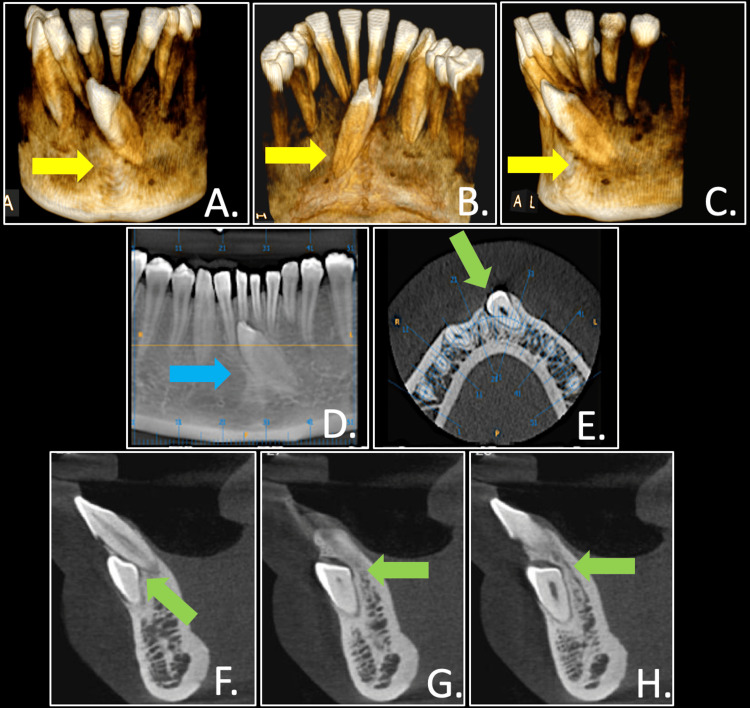
A cone beam computed tomography (CBCT) scan with 6-FOV (field of view), 0.2 mm voxel size, a 10-second exposure period was obtained. The crown of the impacted canine was positioned on the labial side, below the tips of the mandibular incisors (Figure 4).
Figure 4. Pre-treatment CBCT scan showing impacted mandibular canine in relation with mandibular incisors and alveolar bone in three dimension: hard tissue reconstruction (A to C) (yellow arrows), reconstructed OPG section focusing on canine impaction (D) (blue arrow), axial and sagittal views (E to H) (green arrows).
CBCT: cone beam computed tomography; OPG: orthopantomogram
Treatment objectives
The main goals of the treatment were to (1) establish a level and aligned dental arch, (2) guide the impacted canine into its correct position within the dental arch, (3) correct the axial inclination of upper and lower incisors, (4) address the scissor bite, and (5) achieve a normal overjet and overbite.
Treatment alternatives
The ideal treatment plan was the extraction of all first premolars and extraction of deciduous maxillary canine and deciduous mandibular canine bringing the impacted left mandibular canine in arch and finishing the case in Angles class I molar and canine relationship bilaterally. The other alternative plan was to extract the deciduous maxillary canine and deciduous mandibular canine along with impacted canine, followed by space closure to achieve ideal molar and canine relation with reshaping lower left mandibular premolar to canine. Another plan was to extract deciduous maxillary and deciduous mandibular canine and to bring the impacted transmigrated lower left canine back to occlusion. Out of these plans, the patient rejected the extraction plans of permanent teeth and wanted to go with extraction plan of deciduous teeth, which included getting impacted canine back to its original position.
Treatment progress
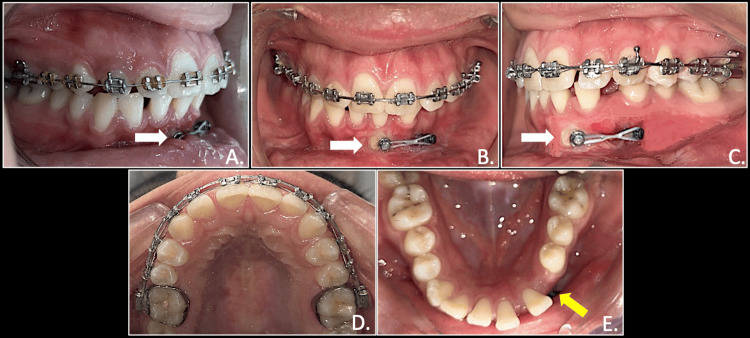
The treatment started with the extraction of deciduous maxillary and mandibular canines. Orthodontic therapy was initiated with fixed appliance using 0.022 MBT (McLaughlin, Bennett, and Trevisi) bracket system, placed in the upper arch. Bonding was done and the initial 0.014NiTi (nickel titanium) wire was placed. In the next subsequent appointment, the impacted canine exposure was carried out using an open window technique. Once the exposure of transmigrated canine was achieved, a bracket was bonded to the canine. Inter-radicular temporary anchorage device (TAD) of size 1.5mm x 6mm was placed in the lower left quadrant at the canine and premolar regions. Since the impacted canine was close to the root surface of mandibular incisors, an uprighting spring (0.017 x 0.025 TMA (titanium molybdenum alloy)) was used from TAD to the exposed canine bracket for correcting the inclination and keep the canine away from the root of incisors (Figure 5).
Figure 5. Uprighting spring made up of 0.017 x 0.025 TMA wire placed to the bracket the canine and TAD.
TMA: Titanium molybdenum alloy; TADs: temporary anchorage devices
It took around six months to correct the inclination of the canine. The uprighting spring was activated every month. While the inclination of impacted canine was being corrected, the maxillary arch progressed further from initial NiTi wires to stainless steel (SS) archwire as the treatment progressed (0.014 NiTi, 0.016 NiTi, 0.018 SS, 0.017 x 0.025 SS and 0.019 x 0.025 SS wire). Once the 0.018 SS archwire was placed, 0.012 NiTi archwire was given as a piggyback wire for repositioning of in-standing maxillary canine, which got aligned and got corrected as the treatment progressed.
Once the canine was upright, another TAD of size 1.5mm x 8mm was inserted between the first and second premolar. An elastomeric chain (e-chain) exerting force from TAD was attached to the canine for pulling in the desired direction (Figure 6).
Figure 6. Elastic force traction for retraction of mandibular canine from TAD to round button on canine (white arrows): right occlusion (A), anterior in occlusion (B), left occlusion (C), maxillary arch (D), mandibular arch showing space available for permanent mandibular canine after extraction of deciduous canine (E).
TADs: Temporary anchorage devices
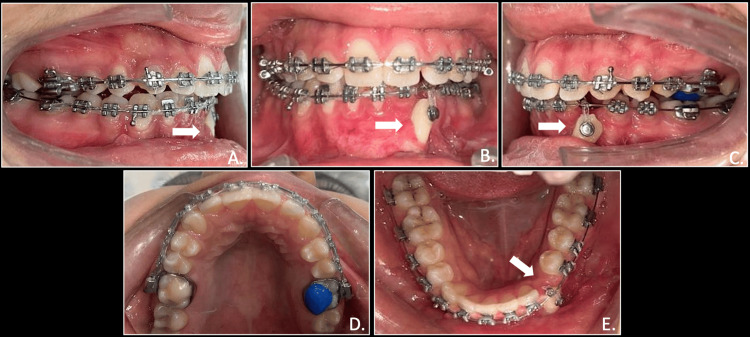
The e-chain was changed every four weeks and it took approximately three months for the canine to get repositioned in its original place. The lower arch was then bonded with 0.014 NiTi wire, followed by 0.016 NiTi, 0.018 SS, 0.017 x 0.025 SS, and 0.019 x 0.025 SS wire. Elastic force traction continued in vertical direction using modified biomechanics on rigid stainless steel wire. Once the transmigrated canine reached near the occlusal plane, a piggyback was given with 0.012 NiTi on 0.018 SS wire. This was followed by 0.014 NiTi for full mandibular arch and then wire sequence were followed from NiTi to SS wires including canine along with all lower teeth together. It was noticed that that the root positioning of the lower left canine brought into the mandibular arch was not appropriate. So, to correct it, root torquing was incorporated using Warren torquing spring, which was activated every month for two months on 0.019 x 0.025 SS wire till accurate root torque and positioning were achieved (Figure 7).
Figure 7. Elastic force traction of mandibular canine in vertical plane from rigid arch wire(white arrows): right occlusion (A), anterior in occlusion (B), left occlusion (C), maxillary arch (D), mandibular arch (E).
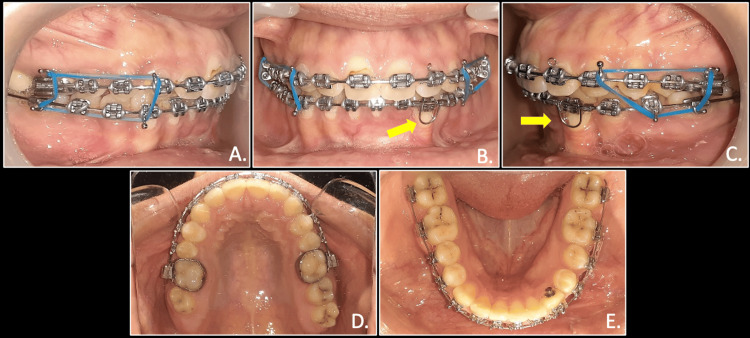
Further to correct the scissor bite with respect to the left side, arch coordination using AJ Wilcock stainless steel wires were done for maxillary and mandibular arches. Finally, settling elastics were given to achieve stable buccal occlusion and appropriate molar and canine relation (Figure 8).
Figure 8. Finishing stage with settling elastics and Warren root torquing spring placed to provide lingual root torque for mandibular left canine: right occlusion (A), anterior in occlusion (B) (yellow arrows), left occlusion (C) (yellow arrows), maxillary arch (D), mandibular arch (E).
Treatment results
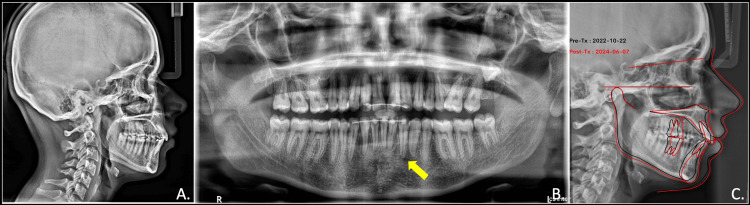
The post-treatment assessment revealed favourable alignment, with class II molar and canine on the right and class 1 molar and canine on the left side with ideal overjet and overbite. The maxillary midline aligned with the facial midline, and a harmonious smile arc was achieved. The post-treatment radiographic evaluation revealed root parallelism of all the teeth with adequate bone support for the transmigrated canine. Post-treatment cephalogram analysis showed slightly proclined and forwardly placed maxillary as well as mandibular incisors. The pre-treatment and post-treatment cephalometric superimposition showed maintenance of dento-skeletal and soft tissue parameters (Figure 9).
Figure 9. Post-treatment radiographs showing the final position of the mandibular canine and associated dental and bony components: lateral cephalogram (A), OPG showing root parallelism and adequate bony support around the canine (B) (yellow arrow). Pre and post-treatment cephalometric superimposition (C) .
OPG: orthopantomogram
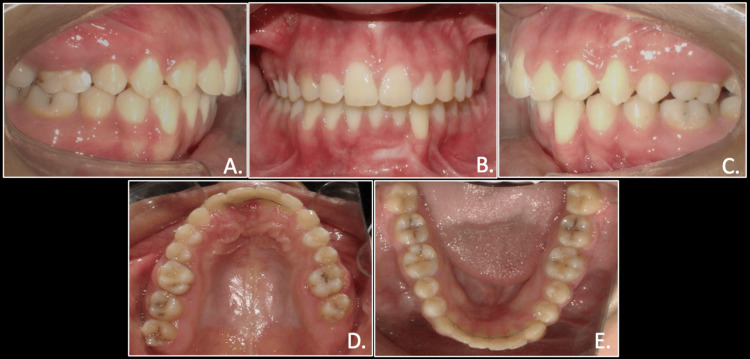
The post-treatment assessment of the transmigrated canine revealed no further root resorption and no signs of mobility. The overall treatment lasted for one year and eight months, and the patient expressed satisfaction with the results. A lingual bondable permanent retainer was delivered in mandibular and maxillary arches (Figures 10, 11).
Figure 10. Post-treatment extraoral photographs: frontal view (A), frontal smiling view (B), and profile view (C).
Figure 11. Post-treatment intraoral photographs: right occlusion (A), anterior in occlusion (B), left occlusion (C), maxillary arch (D), and mandibular arch (E).
Discussion
Mandibular canine transmigration is less frequent compared to maxillary canine impaction, occurring approximately 20 times less often. Mupparapu's classification categorizes canine transmigration considering their location and interaction with the surrounding teeth, identifying 45% as mesioangular, 20% as horizontal and situated beneath the tips of the mandibular incisors, and 1.5% emerging vertically along the midline [6]. While canine transmigration has been classified, clear guidelines are not available for its management. Wertz et al. in 1994 suggest that if the tip of a transmigrated canine extended past the adjacent incisor tooth, it may be challenging to utilise orthodontic treatment modalities to direct it into the proper alignment. In contrast, other authors propose extraction if the transmigrated canine is causing root resorption of the neighbouring teeth or is associated with a cyst [7].
In this case, the left mandibular canine was classified as type 1 by Mupparapu’s classification as it was impacted and positioned buccally and mesioangularly. Due to the retention of the primary deciduous canine and the partial resorption of its root, replacing the permanent canine with the primary canine was not feasible. Therefore, extracting the primary canine and guiding the transmigrated permanent canine into position was the most viable solution. Due to the unusual position of the mesioangularly impacted left canine, the treatment plan required complex three-dimensional orthodontic movements. To address this, modified biomechanics were employed, utilizing an uprighting spring (0.017 x 0.025 TMA) in conjunction with a miniscrew as an anchorage unit to correct the canine's inclination. Once the canine was upright, the mechanics were modified, and another miniscrew was placed between the lower left first and second premolars to retract the transmigrated canine.
After the retraction of canine, it was effectively integrated into the arch through elastic traction force, although it was challenging as the movement of the canine through the cortical bone required enhanced anchorage control, here provided by using TAD. To enhance the predictability of tooth outcomes movement and for appropriate biomechanical planning, three-dimensional CBCT imaging was done.
Due to the unpredictable onset of root resorption in impacted teeth, all such teeth should be considered at significant risk for external root resorption or harm to adjacent teeth. Regular radiographic assessments, such as orthopantomography, are essential for monitoring these risks [8,9]. Vuchkova and Farah reported in 2010 that over the past 50 years, 185 cases of transmigrated mandibular canines have been documented [10]. While several treatment options have been described, the most common approach involves extracting the transmigrated tooth. Following the extraction of the transmigrated tooth, the treatment plan typically involves either orthodontic correction of the malocclusion or no further treatment [4,11,12].
Given the uncertain outcome of repositioning transmigrated mandibular canines [13], Orthodontic-surgical repositioning of transmigrated mandibular canines has been sparsely documented in the literature [1,14,15]. Wertz in 1994 suggested that surgical repositioning of transmigrated mandibular canines should be considered when non-extraction orthodontic treatment is deemed appropriate [7]. A long-term follow-up study by Becker and Chaushu in 2005 indicates that surgical repositioning of transmigrated mandibular canines followed by extrusion with minimal orthodontic forces offers the most promising long-term outcome, as it effectively mitigates the risks of ankylosis and external root resorption [16]. A comprehensive review of the literature on transmigrate mandibular canine and modified orthodontic treatment used for successful disimpaction of canine is depicted in Table 1.
Table 1. Review of transmigrated mandibular canine cases.
| Reference | Transmigrated Mandibular Canine (Mupparapu Classification) | Side | Deviation of Transmigrated Canine from Midline | Mechanics Used |
| Pinto et al.(2020) [17] | Type 2 | Right | Along the lower edge of mandible, under the roots of lower incisors | Extraction of transmigrated canine as associated with cyst. |
| Bhullar et al.(2017) [18] | Type 1 | Left | At the midline, with crown close to roots of mandibular central incisors | Extraction of transmigrated canine. |
| Type 1 | Right | Along the lower edge of the mandible, under the roots of lower incisors | Extraction of transmigrated canine. | |
| Type 5 | Right | At the midline, just apical to the roots of retained deciduous central incisors | Extraction of retained deciduous central incisors followed by surgical exposure and orthodontic traction of 43 in their place. Reshaping of canine as incisor was done at the end of the treatment. | |
| Tarsariya et al.(2015) [19] | Type 6 | Right | The canine impacted vertically beyond the body of the mandible on the contralateral side in the midramus region | No treatment |
| Type 4 | Right | Along the lower edge of the mandible, under the roots of the premolars incisors | ||
| Type 2 | Right | Along the lower edge of the mandible, under the roots of lower incisors | ||
| Type 5 | Right | Impacted vertically below the apices of incisors in midline | ||
| Camilleri and Scerri (2003) [3] | Type 2 | Right | Along the lower edge of the mandible, under the roots of lower incisors | No treatment |
| Type 1 | Right | At the midline, with the crown close to the roots of the mandibular central incisors | ||
| Type 2 | Right | Along the lower edge of the mandible, under the roots of lower incisors | ||
| Type 1 | Left | At the midline, with the crown close to the roots of the mandibular central incisors |
The primary objective of this case report was to evaluate the efficacy of a novel treatment approach for managing transmigrated mandibular canines. The treatment plan successfully achieved its goals, resulting in a satisfactory aesthetic outcome despite minimal gingival recession. The key factors contributing to the treatment's success were the judicious application of light continuous forces and the patient's unwavering motivation. Moreover, diagnosis using three-dimensional imaging played a pivotal role in preventing potential complications, particularly root resorption of adjacent teeth.
Conclusions
The interdisciplinary management of transmigration by orthodontic-surgical synergy is a viable therapeutic modality. To mitigate potential iatrogenic damage to the teeth and supporting structures, application of light orthodontic forces and meticulous care are imperative. Dentists should expeditiously identify transmigrations and assess for orthodontic evaluation for comprehensive evaluation and treatment.
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: Ashish K. Singh, Dhruv Ahuja, Puneet Batra, Priya Dogra, Toni Lego
Acquisition, analysis, or interpretation of data: Ashish K. Singh, Dhruv Ahuja, Puneet Batra, Priya Dogra, Toni Lego
Drafting of the manuscript: Ashish K. Singh, Dhruv Ahuja, Puneet Batra, Priya Dogra, Toni Lego
Critical review of the manuscript for important intellectual content: Ashish K. Singh, Dhruv Ahuja, Puneet Batra, Priya Dogra, Toni Lego
References
- 1.Correction of bilateral impacted mandibular canines with a lip bumper for anchorage reinforcement. Agarwal S, Yadav S, Shah NV, Valiathan A, Uribe F, Nanda R. Am J Orthod Dentofacial Orthop. 2013;143:393–403. doi: 10.1016/j.ajodo.2011.12.030. [DOI] [PubMed] [Google Scholar]
- 2.Abberantly placed impacted mandibular canine. Bahl R, Singla J, Gupta M, Malhotra A. Contemp Clin Dent. 2013;4:217–219. doi: 10.4103/0976-237X.114850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Transmigration of mandibular canines - a review of the literature and a report of five cases. Camilleri S, Scerri E. https://pubmed.ncbi.nlm.nih.gov/14719743/ Angle Orthod. 2003;73:753–762. doi: 10.1043/0003-3219(2003)073<0753:TOMCRO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Combined orthodontic-surgical management of a transmigrated mandibular canine. Cavuoti S, Matarese G, Isola G, Abdolreza J, Femiano F, Perillo L. Angle Orthod. 2016;86:681–691. doi: 10.2319/050615-309.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Intrabony migration of impacted teeth. Shapira Y, Kuftinec MM. https://pubmed.ncbi.nlm.nih.gov/14719741/ Angle Orthod. 2003;73:738–743. doi: 10.1043/0003-3219(2003)073<0738:IMOIT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Patterns of intra-osseous transmigration and ectopic eruption of mandibular canines: review of literature and report of nine additional cases. Mupparapu M. Dentomaxillofac Radiol. 2002;31:355–360. doi: 10.1038/sj.dmfr.4600732. [DOI] [PubMed] [Google Scholar]
- 7.Treatment of transmigrated mandibular canines. Wertz RA. Am J Orthod Dentofacial Orthop. 1994;106:419–427. doi: 10.1016/S0889-5406(94)70064-8. [DOI] [PubMed] [Google Scholar]
- 8.Predictive factors associated with adjacent teeth root resorption of palatally impacted canines in Arabian population: a cone-beam computed tomography analysis. Al-Kyssi HA, Al-Mogahed NM, Altawili ZM, Dahan FN, Almashraqi AA, Aldhorae K, Alhammadi MS. BMC Oral Health. 2022;22:220. doi: 10.1186/s12903-022-02249-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Resorption of incisors after ectopic eruption of maxillary canines: a CT study. Ericson S, Kurol PJ. Angle Orthod. 2000;70:415–423. doi: 10.1043/0003-3219(2000)070<0415:ROIAEE>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Canine transmigration: comprehensive literature review and report of 4 new Australian cases. Vuchkova J, Farah CS. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:0–53. doi: 10.1016/j.tripleo.2009.12.031. [DOI] [PubMed] [Google Scholar]
- 11.Dental transmigration: an observational retrospective study of 52 mandibular canines. Martínez-Rodríguez C, Martínez-Rodríguez N, Alamán-Fernández JM, Ruiz-Sáenz PL, Santos-Marino J, Martínez-González JM, Barona-Dorado C. Biology (Basel. 2022;30:11. doi: 10.3390/biology11121751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Transmigrated mandibular permanent canine: a case report. Dhawan P, Roychoudhury A, Prakash H, Duggal R. https://pubmed.ncbi.nlm.nih.gov/11692828/ J Indian Soc Pedod Prev Dent. 2001;19:80–83. [PubMed] [Google Scholar]
- 13.Transmigration of mandibular canines. Umashree N, Kumar A, Nagaraj T. Case Rep Dent. 2013:697671. doi: 10.1155/2013/697671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prevalence, etiology, clinical features and management associated with impacted and transmigrated mandibular canines: a systematic review. Sathyanarayana HP, Nucci L, d'Apuzzo F, Perillo L, Padmanabhan S, Grassia V. BMC Oral Health. 2023;7:975. doi: 10.1186/s12903-023-03717-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Orthodontic surgical treatment of impacted mandibular canines: systematic review and case report. Inchingolo AD, Carpentiere V, Piras F, et al. Appl Sci. 2022;12:8008. [Google Scholar]
- 16.Long-term follow-up of severely resorbed maxillary incisors after resolution of an etiologically associated impacted canine. Becker A, Chaushu S. Am J Orthod Dentofacial Orthop. 2005;127:650–654. doi: 10.1016/j.ajodo.2004.03.031. [DOI] [PubMed] [Google Scholar]
- 17.Transmigration of a mandibular canine: case report. Pinto L, Mengoni G, Ruscica C, et al. J Osseointegration. 2020;12:236–240. [Google Scholar]
- 18.Mandibular canine transmigration: report of three cases and literature review. Bhullar MK, Aggarwal I, Verma R, Uppal AS. J Int Soc Prev Community Dent. 2017;7:8–14. doi: 10.4103/jispcd.JISPCD_231_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Unusual intrabony transmigration of mandibular canine: case series (report of 4 cases) Tarsariya VM, Jayam C, Parmar YS, Bandlapalli A. BMJ Case Rep. 2015;11:2014205398. doi: 10.1136/bcr-2014-205398. [DOI] [PMC free article] [PubMed] [Google Scholar]