Abstract
Background:
Type 2 diabetes mellitus (T2DM) is associated with a wide range of health outcomes, including an increased risk of depression and anxiety and a decline in quality of life. Even though the significance of biopsychological factors in the mental health status of T2DM patients has been discussed in other studies, the role of environmental factors has been lacking. Therefore, this review aimed to identify the relationship between environmental factors and mental health status among T2DM patients.
Methods:
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension for scoping reviews was utilized in this study. Using predetermined keywords, a systematic search was conducted on three electronic databases from 2005 to 2023, namely, Web of Science, Scopus, and PubMed. Articles written in English, and studies focusing on the research question are among the inclusion criteria. Ten articles were extracted that were relevant to the research question.
Results:
Poor socioeconomic status, urban areas, the influence of neighborhood, greenness, and air pollution had associations with mental health status among T2DM patients.
Conclusion:
The possible implications of these factors for mental health demand further research and policy consideration.
Keywords: Mental health, Diabetes mellitus, Environmental factors, Risk factor
Introduction
Type 2 diabetes mellitus (T2DM) and mental health issues are among the public health problems. T2DM is among the most prevalent noncommunicable disease in developing countries and has a rapid pattern of improvement worldwide (1). Globally, 422 million adults suffered from diabetes mellitus in 2016, and this number is predicted to grow to 642 million people by the end of 2040 (1). Furthermore, T2DM has imposed a significant economic and health burden on patients, communities, and the country (2). In addition to microvascular and macrovascular complications, anxiety and depression were more prevalent among T2DM patients (3). People with T2DM were more likely to develop depression and anxiety by two to three folds compared to individuals without diabetes(4). Patients with T2DM who suffer from depression and anxiety have a higher risk of complications within five years(5). As a whole, T2DM has caused psychological, emotional, and social implications on patients (2). Unresolved psychosocial issues among T2DM patients negatively impact their well-being and quality of life (6).
Mental Health Status among Patients with Type 2 Diabetes Mellitus
Individuals with T2DM should receive comprehensive and holistic consideration, rather than just clinical treatment. Individuals with T2DM regularly experience negative emotions and self-care burdens from the treatment, which predisposes to depression, anxiety, and stress (7). The co-occurrence of diabetes and depression provides a formidable therapeutic challenge since the presence of one disorder exacerbates the effects of the other (8). The World Health Organization has estimated that 322 million individuals (4.4% of the worldwide population) experienced depression, while more than 260 million individuals (3.6% of the worldwide population) have anxiety disorders. In 2019, a study by Global Burden of Disease, Injury, and Risk Factors (GBD) showed that the two most frequent types of mental disorders were depression and anxiety, both of which listed among the top 25 of global disease burden in 2019 (9).
Psychological problems such as depression, anxiety, and stress in people with T2DM have major implications for: i) quality of life (10), ii) financial burden (2), and iii) morbidity (11). People with T2DM who suffers from mental health problem were at higher risk of complications caused by severe self-care deficit, non-compliance with treatment, and uncontrolled sugar levels (12). With regards to morbidity and mortality, depression was linked with an elevated risk of cardiac disease and a mortality rate of 50% (11). By 2030, mental illness is anticipated to make a significant contribution to the financial strain of health care expenses and become the primary reason of disease burden in middle- and high-income nations (13). Therefore, it is vital to identify associated factors of mental health status among individuals with T2DM. Based on existing literature, there are multiple factors that influence mental health status such as sociodemographic factors, biological factors, social factors, and nutritional factors (3,14). In several studies focusing on general population, environmental conditions with surrounding greenery has been linked to good mental health status (15,16). However, there are limited studies that discussed about the environmental factors among T2DM patients in detail. Environmental factors need to be understood before tailoring policies to improve mental health.
Hence, we aimed to identify the association between environmental factors and mental health status among T2DM patients.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension for scoping reviews was utilized in this study. This review was initiated by the development of relevant research questions with the help of all authors. The search was undertaken systematically through the identification, screening, and eligibility processes. Three major databases, Scopus, Web of Science, and PubMed were used during the identification process from 2005 until 2023. Full-text and original publications were chosen to extract the relevant information for addressing the research questions.
Research Question Formulation
The PICo (Population, Interest, and Context) framework, which is a modified version of the PICO (Patient, Intervention, Comparison, and Outcome) framework specified for qualitative questions was utilized to formulate relevant research questions (17). Based on this framework, three significant aspects were included namely T2DM patients (Population), mental health (Interest), and environmental factors (Context). These were then combined into the main research question of “What is the relationship between environmental factors and mental health status among T2DM patients?”
The Systematic Search Strategy
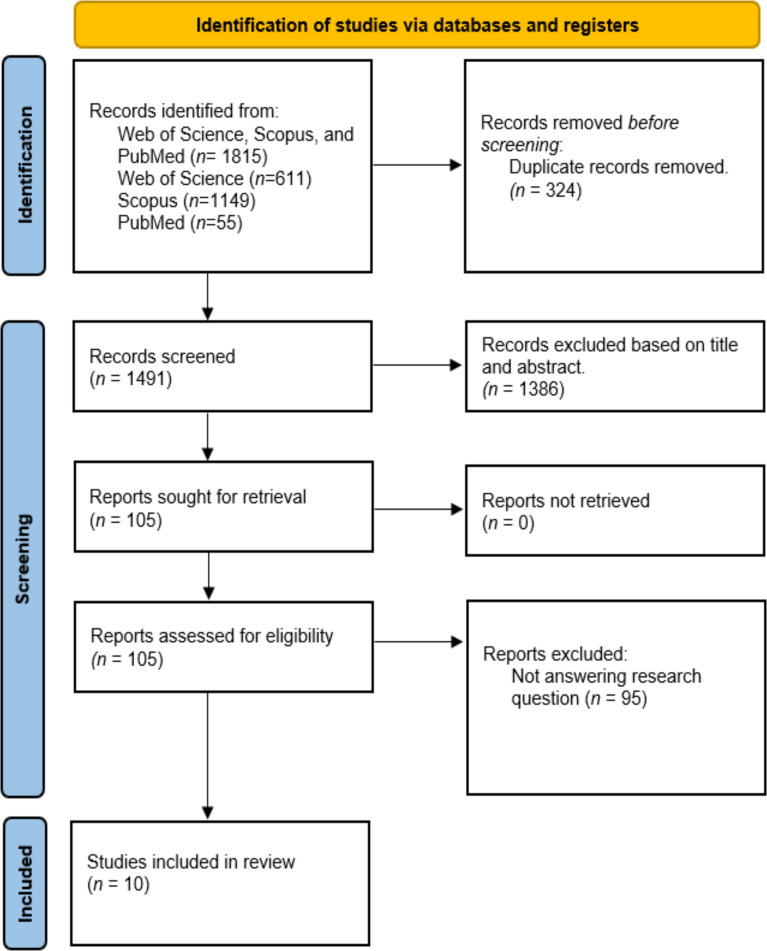
The search was then performed following the PRISMA flow, as shown in Fig. 1.
Fig. 1:
PRISMA flow diagram
Identification
Using synonyms and variations discovered while browsing for articles in databases, keywords were chosen during this identification phase. Titles and abstracts of the articles were evaluated by three authors in relevance to the research question. The search string used was shown in Table 1. The Medical Subject Headings (MeSH) terms were utilized to generate suitable keywords during the identification stage. Afterwards, specific search strings were developed via Boolean operators and the identified keywords. The systematic literature search included the publications between 2005 until 2023, using the search strings in three main databases: PubMed, Web of Science, and Scopus, as shown in Table 1.
Table 1:
Summary of the research methodology
| Method | Description | |
|---|---|---|
| Research Question Formulation | Formulation of research question. | |
| The Systematic Search Strategy | Develop search strings based on identified relevant keywords, and search databases using the search strings. | |
| Identification of the information | Databases | Search Strings |
| PubMed | (“Environmental factors” OR “environment*”) AND (“mental health” OR “depression” OR “anxiety”) AND (“determinants” OR “risk factors” OR “predictors”) AND (“diabetes*” OR “diabetes mellitus”) | |
| Scopus | (“Environmental factors” OR “environment*”) AND (“mental health” OR “depression” OR “anxiety”) AND (“determinants” OR “risk factors” OR “predictors”) AND (“diabetes*” OR “diabetes mellitus”) | |
| Web of Science | (“Environmental factors” OR “environment*”) AND (“mental health” OR “depression” OR “anxiety”) AND (“determinants” OR “risk factors” OR “predictors”) AND (“diabetes*” OR “diabetes mellitus”) | |
| Screening by using inclusion and exclusion criteria. | Establish the inclusion and exclusion criteria for literature selection in this review, and filter studies using the criteria. | |
| Data extraction dan synthesis | Extraction of relevant data from the individual studies, continued with evaluation of the pooled data. | |
The symbol * was used as truncation and wildcard function to increase the variability of selected keywords
Overall, 1815 different hits were obtained from the search, including 611 from Web of Science, 1149 from Scopus and 55 articles from PubMed. Prior to the screening stage, 324 duplicate articles were removed. Any articles related to the study objectives were included in the discussion. Selected articles were imported into Mendeley ver. 1.19.8 after evaluation complete. Browsing records from the database were retrieved, organised, and screened in an Excel spreadsheet. The abstracts were then evaluated, after which unrelated articles were eliminated.
Screening by using inclusion and exclusion criteria
In this stage, all authors screened the relevance of each article’s title and abstract. The article selection criteria were as follows: 1) written in English, and 2) discussed on the relationship between environmental factors and mental health status among T2DM patients. There were no restrictions on the types of study design in the studies that were selected, which include cohort, case-control, or clinical trials, and any type of reviews. The publication dates in this article span from 2005 until 2023. Editorial letters, reports, conference proceedings, book chapters, and systematic review papers were all omitted (Table 2).
Table 2:
Inclusion criteria for the review
| Aspects | Inclusion Criteria |
|---|---|
| Population | Type 2 Diabetes Mellitus |
| Interest | Mental health issues namely depression, anxiety, and stress |
| Context | Any environmental factors related to mental health status |
Data extraction and synthesis
Subsequently, following an assessment of the article titles and abstracts, 1384 irrelevant publications that differed from the study’s research topics were eliminated. The remaining 105 articles were sought for retrieval to check for their accessibility. All three authors reviewed all full-text articles and removed non-related articles. Data from the ten included studies, including the authors’ names, study location, study design, and summary of findings, were extracted by the authors and gathered in an Excel file before being tabulated into suitable tables under the results section. In our review, the information is shown in Table 3. Further data analyses were then performed on the findings of the studies, leading to the development of specific categories.
Table 3:
Findings from all the included studies
| Author | Location | Study Design | Finding | Environmental factors | ||
|---|---|---|---|---|---|---|
| 1. | Camara et al. (18) | Guinea | Cross-sectional study | Associated factors of depression were urban residence, older age, and no previous HbA1c measurement. | Urban | Physical environmental factor |
| 2. | Asefa et al. (19) | Ethiopia | Cross-sectional study | Among T2DM patients, being male, urban residence, single marital status, diabetes mellitus for 5 years and more, and having sexual dysfunction were associated with higher risk of depression. | Urban | Physical environmental factor |
| 3. | Liu et al. (20) | Taiwan | Cross-sectional study | Prevalence of comorbid depression is directly proportional with the level of urbanization. T2DM patients from urban areas were at the highest risk of comorbid depression. | Urban | Physical environmental factor |
| 4. | Akter & Nazef(21) | Bangladesh | Cross-sectional study | Older age, urban residency, housewife, widow, lower education level, and low income were significantly associated with depression | Urban and low socioeconomic income | Physical and social environmental factor |
| 5. | Cho et al. (22) | Korea | Ecological study | SO2, PM10, NO2, and CO significantly increased the risk of emergency department visits for depressive episode, especially among T2DM patients. | Air pollution | Physical environmental factor |
| 6. | De Groot. (23) | United States of America | Cross-sectional study | Poverty increases the risk of depression in diabetes. | Low socioeconomic status (Poverty) | Social environmental factor |
| 7. | Osborn et al.(24) | United States of America | Cross-sectional study | Having diabetes was associated with the presence and severity of depressive symptoms in a large, low-income sample of racially diverse adults | Low socioeconomic status | Social environmental factor |
| 8. | Ganasegaran et al.(25) | Malaysia | Cross-sectional study | Monthly household income was significantly associated with depression | Low socioeconomic status | Social environmental factor |
| 9. | O’Donnell et al.(26) | United States of America | Cross-sectional study | Patients in areas with a high level of social affluence, residential stability, and neighbourhood advantagewere substantially less likely to develop a persistent pattern of depressive symptoms. | Influence of neighbourhood | Social environmental factor |
| 10. | Gariepy et al.(27) | Canada | Cohort Study | Neighbourhood greenness was associated with a lower risk of depression | Neighbourhood greenness | Physical environmental factor |
SO2 =Sulphur dioxide, PM10, =Particulate Matter 10, NO2 =Nitrogen dioxide, CO=Carbon dioxide
Results
After screening and selection of articles according to the criteria of inclusion, there was ten articles that are related to environmental factors and mental health status among T2DM patients. Subsequently, information from the literature was divided into two major sections, namely social environmental factors including low socioeconomic status and influence of neighbourhood and for physical environmental factors including urban factors, neighbourhood greenness and air pollution.
Descriptive findings of included studies (n=10)
Two included studies were from the United States of America, while the rest were from Guinea, Ethiopia, Taiwan, Bangladesh, Korea, Canada, and Malaysia. Majority (eight articles) were cross-sectional studies, one cohort study and one ecological study.
Discussion
In this section, we will discuss how environmental factors affect the mental health status of T2DM patients. The environmental factors were further categorised into social environmental factors and physical environmental factors.
Social environment refers to the immediate physical surroundings, interpersonal interactions, and cultural contexts in which certain groups of people act and interact (28).
Diabetes mellitus and its complications were common in lower socioeconomic group. In our review, four articles found that low socioeconomic status was associated with poor mental health status among T2DM patients (21,23–25). T2DM and depression are common in low-income people around the world due to poor access to diabetes care and its high costs (29). An increment in T2DM incidence, delayed diabetes diagnosis, suboptimal diabetes treatment and management, decreased resource availability and accessibility, and a higher probability of encountering difficult situations were significantly associated with poverty (30,31).
In Scotland, people in the poorest neighbourhoods had higher rates of mental health problems and a lower degree of well-being as compared to people in the wealthiest neighbourhoods (32). Consistent with other study which showed depression and poor health outcomes are both linked to poverty (33,34).
In the United States, patients who live in areas with high levels of social wealth, home stability, and neighbourhood advantages are significantly less likely to experience a recurrent pattern of depressive symptoms (26). Increased vulnerability to negative neighbourhood influences may increase the likelihood of depression in diabetic patients or alter the course of their depression (35). The stress imposed by unpleasant neighbourhoods contributes to depression in addition to the consequences of the individual’s own personal stressors, such as unfavourable occurrences in the family or workplace and, negative neighbourhoods appear to amplify the negative impact of personal stressors and interfere with the creation of interpersonal ties, raising the likelihood of depression (36).
Physical environment encompasses the human environment as well as physical aspects.
By 2060, 80% of the world’s population is anticipated to reside in megacities, signalling a rapid shift in the global population from rural to urban areas (37). Rapid urbanisation is related to a rise in the urban population, resulted in new emerging mental health issues (38). Living in more populated places was linked to greater despair and anxiety in comparison to people who lived in less populated areas. Previous study in developed country has revealed that residing in rapidly urbanising regions is associated with an increased risk of mental disorders (39). This was influenced by socioeconomic and environmental disparities between the different locations.
In our review, four studies found that T2DM patients residing in urban regions were more inclined to exhibit symptoms of depression compared to those living in rural areas (18–21). In Taiwan, urbanisation increased the prevalence of comorbid depression, with urban-dwelling diabetic patients having the highest risk (20). Compared to rural residents, urban dwellers struggle considerably to manage their lives, and research has found that the duration of DM increases the likelihood of developing depression (19). They are prone to being vulnerable to contextual stressors related to their physical environment, such as traffic jams, noise, and violence, which can cause discomfort and impair psychological states (40).
Personal and community social support may play a protective role in the prevention of mental illness. Indeed, the rhythm of urban life, daily responsibilities, workplace stressors, and higher average time spent travelling may make it challenging to maintain effective social interactions in urban settings(38). Other than that, due to development conditions, it may contribute to less green area, and this will negatively impact mental health (41). More research and policy consideration are needed to address the possible impacts of unprecedented urbanisation on mental health (42).
Urban green space is one of the most crucial environmental elements since it promotes urban residents’ health (43). Green space, such forests and parks, is now widely regarded as a health-promoting feature of residential surroundings, and has been related to advantages such as mental fatigue recovery (44). Exposure to greenness is recognised to promote health in a variety of ways, including the promotion of physical activity, the increase of social contact, and the reduction of noise and air pollution (43). A greener neighbourhood was contributed to a lower risk of depression among T2DM patients in our review (27). This suggests that living in a green environment, such as a neighbourhood with many trees, may have a greater impact on people with diabetes (27).
Although there is strong evidence linking neighbourhood greenspace to mental health and well-being levels, global urbanisation has reduced the access to and involvement with green spaces (41). People in urban region with more green space had better wellbeing, fewer mental health issues, and less anxiety and depression than people in urban areas with less green space (45). Furthermore, there was evidence that living in a greener environment reduced the incidence of depression.
One of the biggest environmental problems facing the world is ambient air pollution. According to the Global Burden of Diseases report (GBD), air pollution caused 4.90 million deaths. The detrimental impact of air pollution on mental health, especially depression, have gained attention and had an impact on worldwide public health more recently (46). Greater levels of air pollution might impair health status, as well as people’s contentment and self-perceived health, all linked to mental health status (47,48).
PM10, CO, NO2, and SO2 were substantially linked with emergency visits for depressive episodes in T2DM patients (22). A study in developed nations concluded that greater air pollution may influence people’s mental status, particularly their risk of developing depression (49). This was similar to another study which found that older adult representative samples from the United States who participated in the research showed a significant relationship between PM2.5 and moderate-to-severe depression symptoms (50). This consistent finding from a systematic review and meta-analysis provided evidence for the association between depression and exposure to PM2.5, PM10, NO2, SO2, and CO (46). There are possibilities underlying the neuroinflammation mechanism for the effect of air pollution on mental health (51). PM10 may cause neural damage and changes in neurotransmitter levels. Indirectly, air pollution contributes to fewer outdoor physical activities, and poor physical activities are associated with depressive symptoms and lead to higher levels of cortisol, which contribute to stressful condition (52,53).
Limitation
The studies selected in our review were limited to open access articles published in English language only, thus it may not represent all related literatures linked to the topic. In addition, there are also possibilities that some studies focused on similar topics were eliminated during the screening process due to the different keywords and titles used by the studies.
Conclusion
This review provides an overview of the relationship between environmental factors and mental health outcomes in T2DM patients. The environmental factors were further categorized into social environmental factors and physical environmental factors. The social environmental factors including poor socioeconomic status and the influence of neighborhood, have been shown to give a higher risk of mental health problems among T2DM patients. Meanwhile, the physical environmental factors are fewer green areas, urban areas, and air pollution. Future research should explore the implications of poor socioeconomic status, urbanization, green spaces, and air pollution on the mental health among T2DM patients.
Journalism Ethics considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
We would like to thank the Department of Public Health Medicine, Faculty of Medicine, National University of Malaysia, for the technical support and for providing the grant to conduct this research (FF-2022-252).
Footnotes
Conflict of interest
The authors declare that there is no conflict of interests.
References
- 1.Ogurtsova K, da Rocha Fernandes JD, Huang Y, et al. (2017). IDF Diabetes Atlas: Global Estimates for the Prevalence of Diabetes for 2015 and 2040. Diabetes Res Clin Pract, 128:40–50. [DOI] [PubMed] [Google Scholar]
- 2.International Diabetes Federation Type 2 Diabetes. Available at: https://idf.org/about-diabetes/type-2-diabetes/
- 3.van Duinkerken E, Moreno AB, Eto FN, et al. (2020). Biopsychosocial Factors Associated with a Current Depressive Episode in Diabetes: The ELSA-Brasil Study. Diabet Med, 37:1742–1751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chireh B, Li M, D’Arcy C. (2019). Diabetes Increases the Risk of Depression: A Systematic Review, Meta-Analysis and Estimates of Population Attributable Fractions Based on Prospective Studies. Prev Med Rep, 14: 100822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang MC, Lin K Der, Chen HJ, et al. (2018). Validity of a Short Food Frequency Questionnaire Assessing Macronutrient and Fiber In-takes in Patients of Han Chinese Descent with Type 2 Diabetes. Int J Environ Res Public Health, 15(6):1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Feng X, Astell-burt T. (2017). Impact of a Type 2 Diabetes Diagnosis on Mental Health, Quality of Life, and Social Contacts : A Longitudinal Study. BMJ Open Diabetes Res Care, 5(1):e000198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jeon EJ. (2018). Diabetes and Depression. Yeungnam Univ J Med, 35:27–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Holt RIG, De Groot M, Golden SH. (2014). Diabetes and Depression. Curr Diab Rep, 14(6):491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abbafati C, Abbas KM, Abbasi-Kangevari M, et al. (2020). Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet, 396(10258):1204–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Verma SK, Luo N, Subramaniam M, et al. (2010). Impact of Depression on Health Related Quality of Life in Patients with Diabetes. Ann Acad Med Singap, 39(12):913–917. [PubMed] [Google Scholar]
- 11.Farooqi A, Khunti K, Abner S, et al. (2019). Comorbid Depression and Risk of Cardiac Events and Cardiac Mortality in People with Diabetes: A Systematic Review and Meta-Analysis. Diabetes Res Clin Pract, 156:107816. [DOI] [PubMed] [Google Scholar]
- 12.Alhunayni NM, Mohamed AE, Hammad SM. (2020). Prevalence of Depression among Type-II Diabetic Patients Attending the Diabetic Clinic at Arar National Guard Primary Health Care Center, Saudi Arabia. Psychiatry J, 2020: 9174818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vos T, Allen C, Arora M, et al. (2016). Global, Regional, and National Incidence, Prevalence, and Years Lived with Disability for 310 Diseases and Injuries, 1990–2015: A Systematic Analysis for the Global Burden of Disease Study 2015. Lancet, 388(10053):1545–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Amsah N, Isa Z, Ahmad N. (2022). Biopsychosocial and Nutritional Factors of Depression among Type 2 Diabetes Mellitus Patients : A Systematic Review. Int J Environ Res Public Health, 19(8):4888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.James P, Banay RF, Hart JE, et al. (2015). A Review of the Health Benefits of Greenness. Curr Epidemiol Rep, 2(2):131–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weimann H, Rylander L, Albin M, et al. (2015). Effects of Changing Exposure to Neighbourhood Greenness on General and Mental Health: A Longitudinal Study. Health Place, 33:48–56. [DOI] [PubMed] [Google Scholar]
- 17.Moola S, Munn Z, Sears K, et al. (2015). Conducting Systematic Reviews of Association (Etiology): The Joanna Briggs Institute’s Approach. Int J Evid Based Healthc, 13:163–169. [DOI] [PubMed] [Google Scholar]
- 18.Camara A, Baldé NM, Enoru S, et al. (2015). Prevalence of Anxiety and Depression among Diabetic African Patients in Guinea: Association with HbA1c Levels. Diabetes Metab, 41:62–68. [DOI] [PubMed] [Google Scholar]
- 19.Asefa A, Zewudie A, Henok A, et al. (2020). Depression and Its Associated Factors among Diabetes Mellitus Patients Attending Selected Hospitals in Southwest Ethiopia: A Cross-Sectional Study. Psychiatry J, 2020: 6486030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lin CH, Lee YY, Liu CC, et al. (2012). Urbanization and Prevalence of Depression in Diabetes. Public Health, 126:104–111. [DOI] [PubMed] [Google Scholar]
- 21.Akter N, Latif ZA. (2021). Assessment of Depression and Its Associated Factors among Patients with Type 2 Diabetes. Sri Lanka J Diabetes Endocrinol Metab, 11:14. [Google Scholar]
- 22.Cho J, Choi YJ, Suh M, et al. (2014). Air Pollution as a Risk Factor for Depressive Episode in Patients with Cardiovascular Disease, Diabetes Mellitus, or Asthma. J Affect Disord, 157:45–51. [DOI] [PubMed] [Google Scholar]
- 23.De Groot M, Doyle T, Hockman E, et al. (2007). Depression Among Type 2 Diabetes Rural Appalachian Clinic Attendees. Diabetes Care, 30:1602–1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Osborn CY, Patel KA, Liu J, et al. (2011). Diabetes and Co-Morbid Depression among Racially Diverse, Low-Income Adults. Ann Behav Med, 41:300–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ganasegeran K, Renganathan P, Manaf RA, et al. (2014). Factors Associated with Anxiety and Depression among Type 2 Diabetes Outpatients in Malaysia: A Descriptive Cross-Sectional Single-Centre Study. BMJ Open, 4(4):e004794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Donnell AO, Vries HF De, Wiebe DJ, et al. (2015). Neighborhood Social Environment and Patterns of Depressive Symptoms Among Patients with Type 2 Diabetes Mellitus. Community Ment Health J, 51(8):978–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gariepy G, Kaufman JS, Blair A, et al. (2015). Place and Health in Diabetes : The Neighbourhood Environment and Risk of Depression in Adults with Type 2 Diabetes. Diabet Med, 32(7):944–50. [DOI] [PubMed] [Google Scholar]
- 28.Barnett E, Casper M. (2001). A Definition of “Social Environment”. Am J Public Health, 91(3):465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lund C, Breen A, Flisher AJ, et al. (2010). Poverty and Common Mental Disorders in Low and Middle Income Countries: A Systematic Review. Soc Sci Med, 71(3):517–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hsu CC, Lee CH, Wahlqvist ML, et al. (2012). Poverty Increases Type 2 Diabetes Incidence and Inequality of Care Despite Universal Health Coverage. Diabetes Care, 35(11):2286–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kuruvilla A, Jacob KS. (2007). Poverty, Social Stress & Mental Health. Indian J Med Res, 126(4):273–8. [PubMed] [Google Scholar]
- 32.Knifton L, Inglis G. (2020). Poverty and Mental Health: Policy, Practice and Research Implications. BJPsych Bull, 44(5):193–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.De Groot M, Anderson R, Freedland KE, et al. (2001). Association of Depression and Diabetes Complications: A Meta-Analysis. Psychosom Med, 63(4):619–30. [DOI] [PubMed] [Google Scholar]
- 34.Mendenhall E, Kohrt BA, Norris SA, et al. (2017). Non-Communicable Disease Syndemics: Poverty, Depression, and Diabetes among Low-Income Populations. Lancet, 389(10072):951–963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Evans GW. (2003). The Built Environment and Mental Health. J Urban Health, 80(4):536–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cutrona CE, Wallace G, Wesner KA. (2006). Neighborhood Characteristics and Depression: An Examination of Stress Processes. Curr Dir Psychol Sci, 15(4):188–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bhugra D, Castaldelli-Maia JM, Torales J, et al. (2019). Megacities, Migration, and Mental Health. Lancet Psychiatry, 6(11):884–885. [DOI] [PubMed] [Google Scholar]
- 38.Ventriglio A, Torales J, Castaldelli-Maia JM, et al. (2021). Urbanization and Emerging Mental Health Issues. CNS Spectr, 26(1):43–50. [DOI] [PubMed] [Google Scholar]
- 39.Wang R, Xue D, Liu Y, et al. (2018). The Relationship between Urbanization and Depression in China: The Mediating Role of Neighborhood Social Capital. Int J Equity Health, 17(1):105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Geng C, Shaikh AS, Han W, et al. (2019). Vitamin D and Depression: Mechanisms, Determination and Application. Asia Pac J Clin Nutr, 28(4):689–694. [DOI] [PubMed] [Google Scholar]
- 41.Alcock I, White MP, Wheeler BW, et al. (2014). Longitudinal Effects on Mental Health of Moving to Greener and Less Green Urban Areas. Environ Sci Technol, 48(2):1247–1255. [DOI] [PubMed] [Google Scholar]
- 42.Chen J, Chen S, Landry PF. (2015). Urbanization and Mental Health in China: Linking the 2010 Population Census with a Cross-Sectional Survey. Int J Environ Res Public Health, 12(8):9012–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Song H, Lane KJ, Kim H, et al. (2019). Association between Urban Greenness and Depressive Symptoms : Evaluation of Greenness Using Various Indicators. Int J Environ Res Public Health, 16(2):173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Beyer KMM, Kaltenbach A, Szabo A, et al. (2014). Exposure to Neighborhood Green Space and Mental Health : Evidence from the Survey of the Health of Wisconsin. Int J Environ Res Public Health, 11(3):3453–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Barton J, Rogerson M. (2017). The Importance of Greenspace for Mental Health. BJPsych Int, 14(4):79–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zeng Y, Lin R, Liu L, et al. (2019). Ambient Air Pollution Exposure and Risk of Depression: A Systematic Review and Meta-Analysis of Observational Studies. Psychiatry Res, 276:69–78. [DOI] [PubMed] [Google Scholar]
- 47.Chen C, Liu C, Chen R, et al. (2018). Ambient Air Pollution and Daily Hospital Admissions for Mental Disorders in Shanghai, China. Sci Total Environ, 613–614:324–330. [DOI] [PubMed] [Google Scholar]
- 48.Sun J, Lu C, Xie J. (2022). The Impact of Sustained Exposure to Air Pollutant on the Mental Health: Evidence from China. Sustainability, 14(11):6693. [Google Scholar]
- 49.Wang R, Xue D, Liu Y, et al. (2018). The Relationship between Air Pollution and Depression in China: Is Neighbourhood Social Capital Protective? Int J Environ Res Public Health, 15(6):1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pun VC, Manjourides J, Suh H. (2017). Association of Ambient Air Pollution with Depressive and Anxiety Symptoms in Older Adults: Results from the NSHAP Study. Environ Health Perspect, 125(3):342–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Block ML, Calderón-Garcidueñas L. (2009). Air Pollution: Mechanisms of Neuroinflammation and CNS Disease. Trends Neurosci, 32(9):506–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ard K, Colen C, Becerra M, et al. (2016). Two Mechanisms: The Role of Social Capital and Industrial Pollution Exposure in Explaining Racial Disparities in Self-Rated Health. Int J Environ Res Public Health, 13(10):1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tomei F, Rosati MV, Ciarrocca M, et al. (2003). Plasma Cortisol Levels and Workers Exposed to Urban Pollutants. Ind Health, 41(4):320–326. [DOI] [PubMed] [Google Scholar]