Abstract
Background:
Low back pain (LBP) is a prevalent health issue that imposes heavy burdens on personal health status and social healthcare. Dynamic Neuromuscular Stabilization (DNS)/Vojta therapy has demonstrated effectiveness in managing conditions related to musculoskeletal system. However, its effects on individuals with LBP remain incompletely understood. We aimed to evaluate the effects of DNS/Vojta therapy on pain intensity and physical function in individuals with LBP.
Methods:
A search of studies was conducted on several academic databases from inception through April 13, 2023. This study included clinical trials that evaluated the effects of DNS/Vojta therapy on the outcomes in individuals with LBP. The methodological quality of studies was assessed using PEDro scale, Cochrane Collaboration tool, and ROBINS-I scale. Meta-analysis was performed using Review Manager software (RevMan version 5.4.1, The Cochrane Collaboration, 2020).
Results:
This systematic review and meta-analysis identified twelve eligible studies, which demonstrated that DNS/Vojta therapy significantly alleviated pain intensity (SMD=−1.09; 95%Cl [−1.74, −0.44]; Z=3.28; P=0.001), reduced disability severity (SMD=−0.91; 95%Cl [−1.48, −0.34]; Z=3.12; P=0.002), and improved quality of life (SMD=1.05; 95%CI [0.14, 1.96]; Z=2.27; P=0.02) in individuals with LBP, while no significant improvements were observed in static and dynamic balance ability or spine flexibility.
Conclusion:
DNS/Vojta therapy is a promising approach for providing great benefits for individuals with LBP, particularly in terms of reducing pain intensity and disability severity, and improving quality of life, which is worth further in clinical application.
Keywords: Dynamic neuromuscular stabilization, Vojta therapy, Low back pain, Meta-analysis
Introduction
Low back pain (LBP) is a painful condition related to the musculoskeletal system, which is usually accompanied by increased muscle tension or stiffness localized below the costal margin and above the inferior gluteal folds (1). These changes can restrict normal movement, decrease work efficiency and quality of life for individuals who experience LBP. It is estimated that more than 80% of working-age individuals experienced LBP resulting in significant productivity losses and increased burden of public health (2,3).
Active rehabilitation interventions, such as exercise and manual therapy, have demonstrated efficacy in treating LBP and improving physical function (3,4). However, inadequate appropriate rehabilitation is a major reason for prolonged clinical symptoms in some individuals with LBP (5). Conventional interventions used by rehabilitation therapists fail to address other pathological changes present in individuals with LBP, such as abnormal breathing patterns, resulting in limited efficacy for this population (6). Despite the existence of specific exercises and therapies that target changes associated with LBP, such as breathing exercises and postural re-education, these interventions lack sufficient intensity of muscle group training and systematic theoretical support, resulting in limited effectiveness (7,8). As a result, researchers have been focused on identifying more comprehensive and effective methods for treating individuals with LBP (9).
Dynamic Neuromuscular Stabilization (DNS)/Vojta therapy is a rehabilitation intervention method designed based on developmental kinesiology and can be used to treat abnormal conditions (10–13). Its designers emphasize the importance of early infant movement patterns in developing proper motor control and postural stability (13–15). They hypothesized that if neural networks between the brainstem and the spinal cord were affected, there would be a disruption in the central nervous system (CNS) to regulate normal motor function, which would lead to altered biomechanics of movement resulting in abnormal conditions such as LBP (10,14,15). Therefore, this therapy aims to reawaken the regulation of the CNS in motor function, thereby restoring the ideal movement pattern (10,14,15). In contrast to conventional interventions (e.g., transcutaneous electrical nerve stimulation, ultrasound, strengthening and stretching exercises), the DNS/Vojta therapy protocol enables rehabilitation therapists to apply targeted pressure on specific points of the body in order to provide afferent stimulation for adjusting breathing patterns and eliciting genetically predetermined CNS motor programs (16). In 2011, researchers discovered the efficacy of DNS/Vojta therapy in managing chronic pain (13). A systematic review in 2022 provided preliminary evidence supporting the potential benefits of DNS/Vojta therapy for individuals with musculoskeletal disorders, including LBP (17). However, the lack of quantitative analysis undermines the persuasiveness of the conclusion. None of the reviews have employed statistical analysis to measure and compare outcomes between DNS/Vojta therapy and conventional interventions. This analytical gap impedes researchers from identifying the specific aspects in which DNS/Vojta therapy benefits individuals with LBP.
Over the past decade, there has been a notable increase in studies utilizing rigorous experimental designs to evaluate the efficacy of DNS/Vojta therapy for individuals with LBP. To further enhance our understanding of its potential benefits, we aimed to conduct an in-depth analysis of available data and assess the impact of DNS/Vojta therapy on pain intensity and physical function among those with LBP, hoping to provide a more robust and evidence-based understanding of the potential benefits of DNS/Vojta therapy for individuals with LBP.
Materials and Methods
This systematic review with meta-analysis aimed to examine the effects of DNS/Vojta therapy on pain intensity and physical function in individuals with LBP. This review was conducted following the Cochrane Handbook for Systematic Reviews and presented in conformance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (18,19). This study protocol was registered on the International Prospective Register of Systematic Reviews (PROSPERO: CRD42023417197).
Data sources and search strategies
Two researchers (LYK and ZQZ) independently conducted a comprehensive search for multiple academic databases, including Web of Science, MEDLINE, EMBASE, PubMed, Cochrane Library, etc. The retrieve date was set from database inception through April 13, 2023. They searched for studies that referred to individuals with LBP treated with DNS or Vojta therapy, using the keywords “dynamic neuromuscular stabilization”, “DNS”, “Vojta”, and “Vojta therapy”, together with “low back pain”.
Eligibility criteria
Eligibility criteria for inclusion of the studies regarding PICOS: Participants (P), Intervention (I), Comparator (C), Outcomes (O) and Study Design (S), was followed to determine eligible studies in this systematic review with meta-analysis.
The inclusion criteria were as follows: 1) Participants diagnosed with LBP, including postpartum women, individuals with lumbar disc herniation, scoliosis, or non-specific low back pain; 2) Intervention methods consisted of DNS or Vojta therapy; 3) Comparison groups consisted of non-intervention, conventional intervention or usual care alone; 4) Outcomes were assessed using validated scales or tests to measure pain intensity and physical function in individuals with LBP; 5) All types of clinical trials were considered, including randomized control trials (RCTs) and controlled trials (CTs); 6) No restriction was set for the study setting or language of the publication.
The exclusion criteria comprised: 1) Individuals with comorbid pain conditions or neurological disorders, as well as those exhibiting cognitive dysfunction; 2) Studies focused on intervention methods other than DNS or Vojta therapy; 3) Studies evaluated outcomes without pain intensity and physical function; 4) Case reports, case series, animal studies, in vitro studies, review studies, review papers, editorials letters to the editor & monographs were excluded from consideration.
Study selection
All retrieved records from the databases were exported to EndNote20 for de-duplication. Initially, two independent researchers (LYK and ZQZ) screened the titles and abstracts of the records for eligibility using inclusion and exclusion criteria. Subsequently, the same researcher evaluated potential studies’ full texts to determine their ultimate inclusion in this review. Finally, any disagreements were resolved by consensus with a third researcher (YYL).
Data extraction and quality assessment
Relevant data were extracted from the studies, and any disagreements between reviewers were resolved through discussion with a third reviewer. In cases where data was found to be missing, the study authors were contacted via email to obtain the necessary information. If researchers were not able to obtain information from the authors, they followed the guidelines outlined in the Cochrane Handbook for Systematic Reviews (18).
The risk of bias for the RCTs was evaluated using the PEDro scale and Cochrane Collaboration tool (20–22). The risk of bias for the CTs was evaluated using the ROBINS-I scale (23,24). The PEDro scale comprises 11 items related to the validity of RCTs, assessed by the following cut-points: 9–10 (excellent), 6–8 (good), 4–5 (fair), and less than 4 (poor) (21). The Cochrane bias risk assessment tool evaluates 6 domains and uses three terms: “low risk”, “high risk”, and “unclear risk” (22). The ROBINS-I consists of 7 domains, and the risk of bias judgment of each domain is categorized as low, moderate, serious, and critical risk of bias or no information (24). The overall risk of bias judgment of CTs was determined by the severest risk of bias category among seven domains. Two authors (LYK and ZQZ) assessed the risk of bias of studies of the included studies. If two authors conflicted in their decision, they discussed to reach an agreement. If the discussion remained in conflict, it was resolved by the third author (YYL). The robvis tool was used to visualize the risk of bias in each study assessed by PEDro scale, Cochrane Collaboration tool, and ROBINS-I (25).
Data synthesis and analysis
Extracted outcome data were accomplished by the change in the mean and standard deviation (SD) values between pre- and post-intervention (26). When studies reported median and quartile data instead of mean and SD, mean and SD were extrapolated from the sample size, median and quartile (27,28).
The data was synthesized according to the outcome assessed and were combined for meta-analysis. Quantitative meta-analysis was performed by Review Manager software (RevMan version 5.4.1, The Cochrane Collaboration, 2020) with a random-effects model for all outcomes. Forest plots were used for graphical representation. For studies using different measurement tools to measure the same outcome, researchers calculated standardized mean difference (SMD) with 95%CI; For studies using the same measurement tools, researchers computed standardized mean difference (MD) with 95%CI. I2 was examined to assess study heterogeneity. A value of 0% means an absence of heterogeneity, and larger values show increasing levels of heterogeneity (I2<25% as low, I2≤50% as moderate, I2>50% as high) (29). The reasons for high heterogeneity were explored. According to the known confounder, subgroup analyses were stratified by intervention duration.
Publication bias
Publication bias was assessed by Egger’s Rank Correlation Test using the Stata statistical software (STATA 15.1) (30). Once significant publication bias was found, the researchers conducted the trim-and-fill analysis to estimate the influence of publication bias on the outcome of the meta-analysis.
Results
Search results
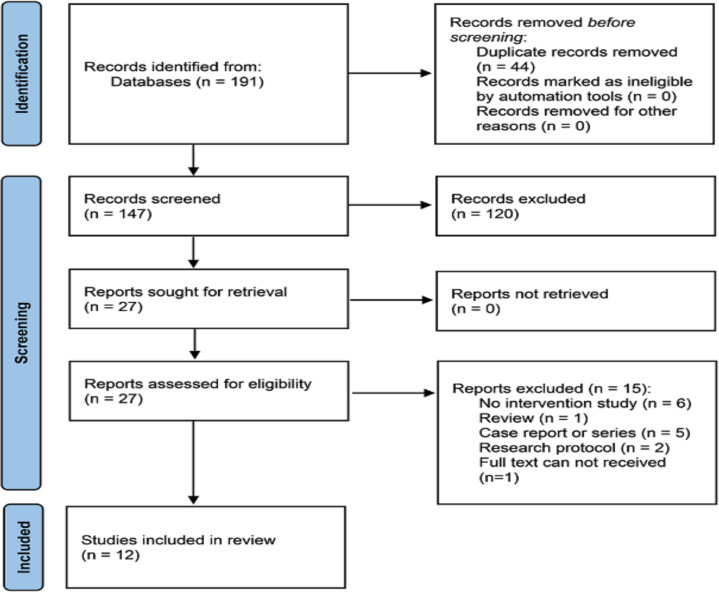
A flowchart of the study search and selection is shown in Fig. 1. Searches of the databases found 191 studies. Finally, 12 full-text studies were retrieved, in which nine RCTs and three CTs qualified for inclusion (31–42).
Fig. 1:
Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flow diagram
Seven studies included participants with non-specific LBP (31,33,34,38–40,42). 2 studies included individuals with obese postpartum with LBP (36,37). 3 studies included individuals suffering from LBP due to lumbosciatica syndrome, scoliosis, and lumbar disc protrusion (32,35,41). All studies had an intervention duration of at least 2 weeks, including 2 studies with an intervention duration of 2 weeks (32,41), 2 studies of 4 weeks (34,40), 4 studies of 6 weeks (36–38,42), and 4 studies of 8 weeks (31,33,35,39). The characteristics of the included studies are shown in Table 1.
Table 1:
Characteristics of twelve included studies
| Author, Year | Classification | Population details (Simple size/Age) | Intervention details | Intervention duration | ||
|---|---|---|---|---|---|---|
|
| ||||||
| Control | Experimental | Control | Experimental | |||
| Xu et al., 2019 (31) | Non-specific LBP | N=21 Age:48.6±8.7yr |
N=20 Age:46.0±9.2yr |
Conventional lumbar stability training and physiotherapy | DNS/Vojta therapy and physiotherapy | 8 weeks |
| Juárez-Albuixec et al., 2020 (32) | Lumbosciatica syndrome | N=6 | N=6 | TENS intervention | DNS/Vojta therapy | 15 days |
| Yang et al., 2021 (33) | Non-specific LBP | N=30 Age:35.13±7.95yr |
N=30 Age:33.90±9.04yr |
Rehabilitation education and core muscle strength training | DNS/Vojta therapy, rehabilitation education and core muscle strength training | 8 weeks |
| Hamed et al., 2021 (34) | Non-specific LBP | N=20 Age:26.45±4.75yr |
N=20 Age:26.05±4.6yr |
Conventional TENS and hot application | DNS/Vojta therapy, conventional TENS, and hot application | 4 weeks |
| Park et al., 2021 (35) | Scoliosis | N=14 Age:16.68±3.99yr |
N=14 Age:15.94±3.75yr |
Trunk stabilization exercise | DNS/Vojta therapy and trunk stabilization exercise | 8 weeks |
| Ghavipanje et al., 2022a (36) | Obese Postpartum With LBP | N=20 Age:29.35±3.48yr |
N=20 Age:29.25±4.14yr |
General exercise | DNS/Vojta therapy | 6 weeks |
| Ghavipanje et al., 2022b (37) | Obese Postpartum With LBP | N=12 Age:29.25±4.02yr |
N=12 Age:28.58±4.98yr |
Breathing exercises | DNS/Vojta therapy and breathing exercises | 6 weeks |
| Najafi Ghagholestani et al., 2022 (38) | Non-specific LBP | N=12 Age:35.33±12.91yr |
N=12 Age:38.19±8.54yr |
No intervention | DNS/Vojta therapy | 6 weeks |
| Mousavi et al., 2022 (39) | Non-specific LBP | N=10 Age:42.4±11.8yr |
N=10 Age:47.8±9.82yr |
Core stability exercise | DNS/Vojta therapy | 8 weeks |
| Lin et al., 2022 (40) | Non-specific LBP | N=22 Age:82.1±2.2yr |
N=22 Age:81.4±3.2yr |
Conventional core stability training | DNS/Vojta therapy and conventional core stability training | 4 weeks |
| Iosub et al., 2023 (41) | Lumbar disc protrusion | N=39 Age:50.33±14.02yr |
N=38 Age:50.24±12.25yr |
Conservatory physical therapy program | DNS/Vojta therapy and conservatory physical therapy | 2 weeks |
| Karartı et al., 2023 (42) | Non-specific LBP | N=36 Age:67.75±1.33yr |
N=36 Age:68.08±1.54yr |
Conventional physiotherapy | DNS/Vojta therapy and conventional physiotherapy | 6 weeks |
Abbreviation: LBP: Low Back Pain; DNS: Dynamic Neuromuscular Stabilization; TENS: Transcutaneous Electrical Nerve Stimulation
Outcome measures
The outcomes considered in this meta-analysis were pain intensity and physical function. Physical function was analyzed from disability severity, static balance ability, dynamic balance ability, spinal flexibility and quality of life.
Regarding pain intensity, seven studies used the Visual Analogue Scale (32,33,35,38–41), and one used the Numeric Pain Rating Score (36). Regarding disability severity, six studies used the Oswestry Disability Index or Modified Oswestry Disability Index (33,34,36,38,40,41), and two used the Roland Morris Questionnaire (31,32). Regarding static balance ability, one study used the Romberg test (37), and one study used the Stork test (39). Regarding dynamic balance ability, two studies used the Timed Up and Go test (37,42). Regarding spinal flexibility, two studies used the Fingertips to Floor test (32,41). Regarding the quality of life, two studies used the World Health Organization Quality of Life and one used the 36-item Short-Form (37,39,42).
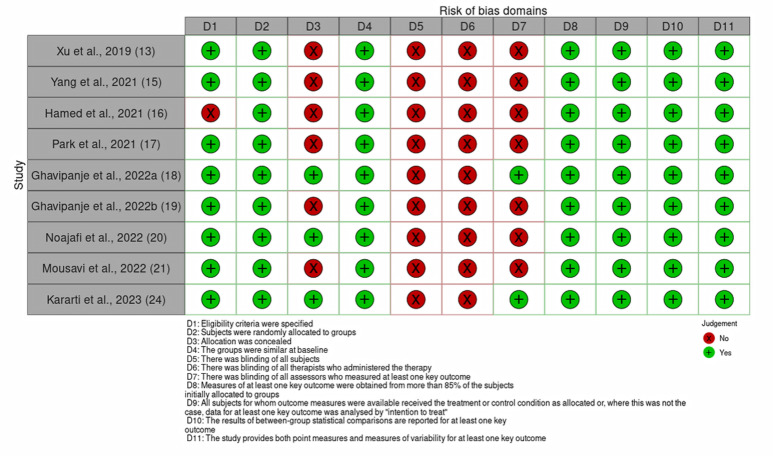
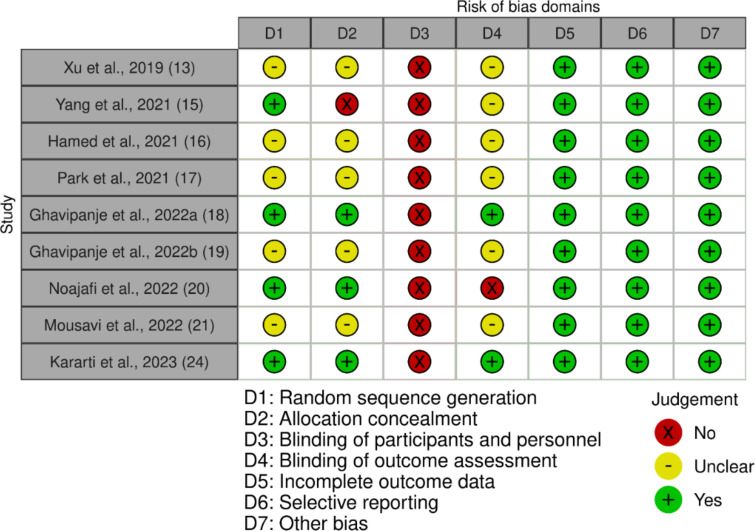
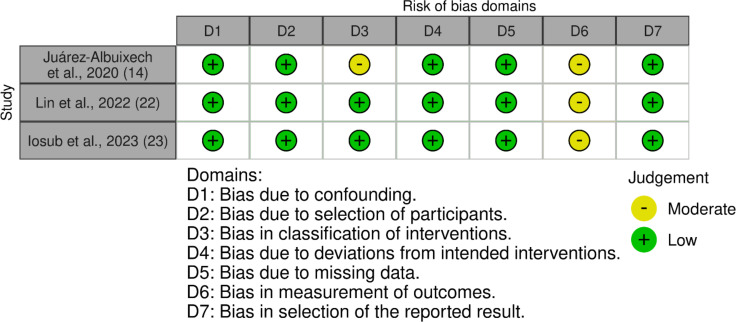
Study quality and risk of bias
The methodological quality of the included RCTs is shown in Figs. 2 and 3. All nine RCTs were assessed by PEDro scale, and scored as 6–8 points, demonstrating good quality (21). These RCTs were also assessed by Cochrane Collaboration tool, and most showed “unclear” and “high” risk of bias regarding blind method usage. The methodological quality of the included CTs is shown in Fig. 4. Assessed by ROBINS-I, all CTs have a moderate risk of bias in measurement of outcomes, and they had a moderate overall risk of bias (24).
Fig. 2:
Methodological quality of randomized control trials assessed by PEDro scale
Fig. 3:
Methodological quality of randomized control trials assessed by Cochrane Collaboration tool
Fig. 4:
Methodological quality of controlled trials assessed by ROBINS-I
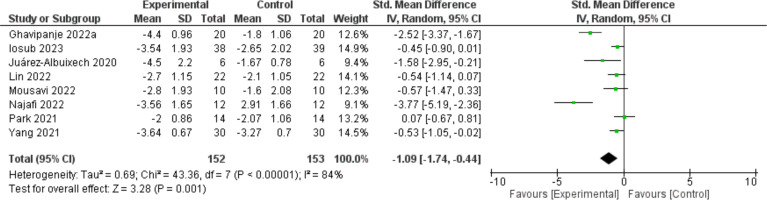
Pain intensity
Fig. 5 shows the results of DNS/Vojta therapy on pain intensity in individuals with LBP, which were measured in eight studies. Experimental group exhibited significantly lower pain intensity compared to control group (SMD=−1.09; 95%Cl [−1.74, −0.44]; Z=3.28; P=0.001). Heterogeneity of the effect size was high (I2=84%).
Fig. 5:
Forest plots of pain intensity
Physical function
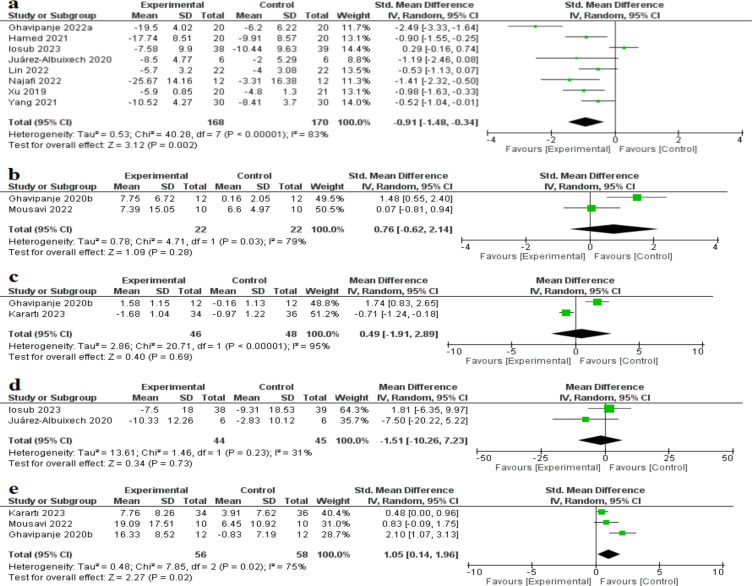
Fig. 6a shows the results of DNS/Vojta therapy on disability severity in individuals with LBP. Experimental group exhibited significantly lower disability severity compared to control group (SMD=−0.91; 95%Cl [−1.48, −0.34]; Z=3.12; P=0.002). Heterogeneity of the effect size was high (I2=83%).
Fig. 6:
Forest plots of (a) disability severity, (b) static balance ability, (c) dynamic balance ability, (d) spinal flexibility, (e) quality of life
Fig. 6b shows the results of DNS/Vojta therapy on static balance ability in individuals with LBP. Experimental group did not exhibit significantly higher persistent time in the test compared to control group (SMD=0.76; 95%Cl [−0.62, 2.14]; Z=1.09; P=0.28). Heterogeneity of the effect size was high (I2=79%).
Fig. 6c shows the results of DNS/Vojta therapy on dynamic balance ability. Experimental group did not exhibit significantly lower time consumption in the Timed Up and Go test compared to control group (MD=0.49; 95%Cl [−1.91, 2.89]; Z=0.40; P=0.69). Heterogeneity of the effect size was high (I2=95%).
Fig. 6d shows the results of DNS/Vojta therapy on spinal flexibility in individuals with LBP. Experimental group did not exhibit a significant change in spinal flexibility compared to control group (MD=−1.51; 95%Cl [−10.26, 7.23]; Z=0.34; P=0.73). Heterogeneity of the effect size was moderate (I2=31%).
Fig. 6e shows the results of DNS/Vojta therapy on quality of life in individuals with LBP. Experimental group exhibited a significant change in quality of life compared to control group (SMD=1.05; 95%CI [0.14, 1.96]; Z=2.27; P=0.02). Heterogeneity of the effect size was high (I2=75%).
Subgroup analysis
Subgroup analysis was performed for pain intensity and disability severity. The heterogeneity of all subgroups significantly decreased. No significant changes in pain intensity were found when intervention duration was set for 2 weeks or 4 weeks (N=2, SMD=−0.82, 95%CI [−1.87, 0.23], P=0.120; N=1, SMD=−0.54, 95%CI [−1.14, 0.07], P=0.080). Significant changes in pain intensity were found when intervention duration was set at 6 weeks or 8 weeks (N=2, SMD=−3.01, 95%CI [−4.22, −1.81], P<0.001; N=2, SMD=−0.38, 95%CI [−0.76, 0.00], P=0.050).
No significant changes in disability severity were found when intervention duration was set for 2 weeks (N=2, SMD=−0.33 95%CI [−1.76,1.10], P=0.066). Significant changes in disability severity were found when intervention duration was set at more than or equal to 4 weeks (N=2, SMD=−0.70, 95%CI [−1.14, −0.26], P=0.002; N=2, SMD=−1.96, 95%CI [−3.02, −0.91], P<0.001; N=2, SMD=−0.70, 95%CI [−1.14, 0.27], P=0.002). Due to the limited number of articles included, no subgroup analysis was conducted on static balance ability, dynamic balance ability, spinal flexibility and quality of life.
Assessment of publication bias
Egger’s Test was used to assess publication bias in outcomes of pain intensity, disability severity and quality of life, and only the disability severity indicated potential publication bias (N=8, t=−2.90, P=0.027, 95%CI [−11.28, −0.96]). The result of the trim-and-fill analysis in the outcome of disability severity noted no trimming performed and data unchanged, indicating the outcome of the meta-analysis in disability severity was reliable.
Discussion
The results of this meta-analysis confirmed that DNS/Vojta therapy can significantly alleviate pain intensity. The effectiveness of this therapy in pain intensity can be attributable to increased proprioception and restored integrity of cortical information processing. Compared with healthy individuals, individuals with LBP have a significant decline in proprioception which serves as essential for normal motor control (43). The absence of proprioceptive information congruent with motor intention activates cortical center monitoring incongruence of sensation, leading to pathological pain (43). DNS/Vojta therapy integrates brain stimulation with postural awareness. Individuals with LBP need to preserve postures through isometric muscle contractions when therapists put pressure on these individuals’ body-specific points, which can fully stimulate muscles, joints, and tendons, strengthening the proprioception of individuals with LBP (34,44). Besides, exteroceptors and enteroceptors are connected to the reflex locomotions contained in DNS/Vojta therapy, and the enteroceptors act as a source of afferent stimulation to the CNS (34). By providing feedback from receptors, CNS perceives the correct movement pattern, restoring the integrity of cortical information processing (10,14,45).
This study also found that DNS/Vojta therapy can significantly reduce disability severity in individuals with LBP. Individuals with LBP often modify their muscle activity to alleviate pain perception, which can lead to abnormal tissue loading, impaired movement quality, limited ability to perform functional tasks, and even disability. Through repetitive muscle activation training, a key component of DNS/Vojta therapy, the innate correct physiological patterns can be integrated into the spontaneous mobility, realizing the normal kinesiological responses that coordinated activation of abdominal muscles and the autochthonous muscles of the spine (32). DNS/Vojta therapy can activate the core and deep spinal muscles, establishing a balance between these muscles, correcting muscle coordination patterns, and promoting optimal joint alignment (10,15). By coordinating and executing optimal muscle movement strategies, the human body can meet the demands placed on joints during functional tasks, preventing joint overload caused by excessive myofascial activation, avoiding excessive extension or tightening of the soft tissue structures around the joints (10,14,46). These factors could directly contribute to improving the movement quality of individuals with LBP and help prevent the occurrence and progression of disability.
Except for the muscles in the abdomen and back, diaphragm is a deep muscle used to maintain postural stability (47). If the breathing pattern is abnormal, the function of the diaphragm will be negatively influenced, and then there will be impaired quality of movement pattern (47,48). Like yoga and pilates therapy, DNS/Vojta therapy offers an effective breath training protocol combined with postural alignment and core strengthening exercises for individuals with LBP (49,50). By utilizing subconscious stimulation of specific zones, DNS/Vojta therapy reflexively mediates the dynamic co-activation of diaphragm and other core stabilization muscles (51,52), to generate the torque required for joint motion. In the included studies of this review, during training, individuals with LBP must maintain intra-abdominal pressure, making the pointer of the pressure biofeedback instrument displays a stable value, achieving a dynamic and stable waist and abdomen (33,38). After undergoing a period of training, individuals with LBP experience improvements in respiration and the coordination of local and global muscle groups, ensuring the generation and transmission of force normally during limb movements, resulting in high-quality functional movements (14,46).
Subgroup analyses were performed in this study to account for the high heterogeneity in pain intensity and disability severity outcomes, stratified by the confounder-intervention duration. The subgroup analyses indicated that interventions lasting two or four weeks did not lead to significant improvements in LBP-related pain or its intensity. Pain intensity could be alleviated when the intervention duration was equal to or exceeded 6 weeks. A previous meta-analysis revealed that the effects of exercise therapy for individuals with LBP had fluctuations when the duration was within 12 weeks (53). Intensive pain rehabilitation programs lasting more than one hundred hours resulted in more significant improvements in pain intensity compared to programs lasting less than thirty hours (55). Thus, based on current evidence, a longer DNS/Vojta therapy duration can lead to greater therapeutic benefits in alleviating pain for individuals with LBP. This may be attributed to DNS/Vojta therapy differs from conventional muscle function training, it emphasizes the re-mastery of standard movements by CNS, and high demands are placed on the plasticity of the brain (10,54). Individuals with LBP have to consume more time to master the training movements included in DNS/Vojta therapy, resulting in a longer intervention duration, these individuals have higher proficiency in training movements and better therapeutic effects (14). In addition, the subgroup analyses also found that when the intervention duration exceeded 4 weeks, the disability severity caused by LBP in individuals could be effectively improved, suggesting that a longer intervention duration could realize the effectiveness of DNS/Vojta in improving physical function.
Individuals with LBP often subconsciously avoid actions that exacerbate pain or prevent them from completing tasks normally due to limited joint mobility, leading to a decrease in daily activity levels and overall quality of life (55,56). The previous qualitative study has found that pain and relevant clinical symptoms are significant barriers to activity participation in individuals with LBP (57). This meta-analysis suggests that DNS/Vojta therapy can effectively improve the quality of life of individuals with LBP. As mentioned earlier, individuals with LBP can experience significant improvements in pain intensity and disability severity after undergoing DNS/Vojta therapy, enabling them to complete various daily tasks better, which might be the direct reason for the significant improvement in their quality of life.
To our knowledge, this is the first meta-analysis to assess the effects of DNS/Vojta therapy on pain intensity and physical function in individuals with LBP. However, due to DNS/Vojta therapy is still not widely used in adult patients, the current number of RCTs targeting individuals with LBP undergoing DNS/Vojta therapy for pain intensity is relatively small. For these reasons, more high-quality RCTs are necessary to further support our findings.
Conclusion
DNS/Vojta therapy provides a promising intervention method for individuals with LBP by focusing on the activation of deep stabilizing muscles and improving overall motor control, improving the pain and disability of this population and their quality of life. The appropriate intervention duration is a crucial factor that affects outcomes. Rehabilitation therapists should set the intervention duration of DNS/Vojta therapy for individuals with LBP at least 4 weeks. If rehabilitation therapists want to achieve improvement in pain intensity for these patients, the intervention duration should be at least 6 weeks.
Journalism Ethics considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
This study was supported by Jiangsu University Philosophy and Social Science Research Major Project (2023SJZD143).
Footnotes
Conflict of interest
All authors declare no conflict of interest relevant to this article.
References
- 1.Vlaeyen JWS, Maher CG, Wiech K, et al. (2018). Low back pain. Nat Rev Dis Primers, 4(1): 52. [DOI] [PubMed] [Google Scholar]
- 2.Vujcic I, Stojilovic N, Dubljanin E, et al. (2018). Low Back Pain among Medical Students in Belgrade (Serbia): A Cross-Sectional Study. Pain Res Manag, 2018:8317906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.George SZ, Fritz JM, Silfies SP, et al. (2021). Interventions for the Management of Acute and Chronic Low Back Pain: Revision 2021. J Orthop Sports Phys Ther, 51(11):CPG1–CPG60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anderson BE, Bliven KCH. (2017). The Use of Breathing Exercises in the Treatment of Chronic, Nonspecific Low Back Pain. J Sport Rehabil, 26(5):452–458. [DOI] [PubMed] [Google Scholar]
- 5.Shahidi B, Padwal J, Lee E, et al. (2022). Factors impacting adherence to an exercise-based physical therapy program for individuals with low back pain. PLoS One, 17(10):e0276326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferreira PH, Ferreira ML, Maher CG, et al. (2010). Changes in recruitment of transversus abdominis correlate with disability in people with chronic low back pain. Br J Sports Med, 44(16):1166–1172. [DOI] [PubMed] [Google Scholar]
- 7.Elwy AR, Groessl EJ, Eisen SV, et al. (2014). A systematic scoping review of yoga intervention components and study quality. Am J Prev Med, 47(2):220–232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cavalcanti IF, Antonino GB, Monte-Silva KKD, et al. (2020). Global Postural Re-education in non-specific neck and low back pain treatment: A pilot study. J Back Musculoskelet Rehabil, 33(5):823–828. [DOI] [PubMed] [Google Scholar]
- 9.Mikkonen J, Luomajoki H, Airaksinen O, et al. (2023). Protocol of identical exercise programs with and without specific breathing techniques for the treatment of chronic non-specific low back pain: randomized feasibility trial with two-month follow-up. BMC Musculoskelet Disord, 24(1):354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frank C, Kobesova A, Kolar P. (2013). Dynamic neuromuscular stabilization & sports rehabilitation. Int J Sports Phys Ther, 8(1):62–73. [PMC free article] [PubMed] [Google Scholar]
- 11.Kolar P, Kobesova A. (2010). Postural-locomotion function in the diagnosis and treatment of movement disorders. Clinical Chiropractic, 13(1):58–68. [Google Scholar]
- 12.Żurawski A, Kiebzak W, Zmyślna A, et al. (2019). Efficacy of the use of the McKenzie and Vojta methods to treat discopathy-associated syndromes in the pediatric population. Int J Occup Med Environ Health, 32(1):33–41. [DOI] [PubMed] [Google Scholar]
- 13.Juehring DD, Barber MR. (2011). A case study utilizing Vojta/Dynamic Neuromuscular Stabilization therapy to control symptoms of a chronic migraine sufferer. J Bodyw Mov Ther, 15(4):538–541. [DOI] [PubMed] [Google Scholar]
- 14.Mahdieh L, Zolaktaf V, Karimi MT. (2020). Effects of dynamic neuromuscular stabilization (DNS) training on functional movements. Hum Mov Sci, 70:102568. [DOI] [PubMed] [Google Scholar]
- 15.Yoon HS, Cha YJ, You JSH. (2020). Effects of dynamic core-postural chain stabilization on diaphragm movement, abdominal muscle thickness, and postural control in patients with subacute stroke: A randomized control trial. NeuroRehabilitation, 46(3):381–389. [DOI] [PubMed] [Google Scholar]
- 16.Juárez-Albuixech ML, Redondo-González O, Tello-Díaz-Maroto I, et al. (2021). Feasibility and efficacy of the Vojta therapy in subacromial impingement syndrome: a randomized controlled trial. J Exerc Rehabil, 17(4):256–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boleti M, Charalampopoulos G. The effect of the Dynamic Neuromuscular Stabilization (DNS) program on the rehabilitation of musculoskeletal and other diseases: A systematic review [Master thesis]. University of West Attica, Faculty of Health and Care Sciences, Department of Physiotherapy, Greece; 2022.
- 18.Higgins JPT, Thomas J, Chandler J, et al. (2019). Cochrane Handbook for Systematic Reviews of Interventions. 2nd Edition. Chichester (UK): John Wiley & Sons. [Google Scholar]
- 19.Page MJ, Moher D, Bossuyt PM, et al. (2021). PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ, 372:n160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de Morton NA. (2009). The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother, 55(2):129–133. [DOI] [PubMed] [Google Scholar]
- 21.Cashin AG, McAuley JH. (2020). Clinimetrics: Physiotherapy Evidence Database (PEDro) Scale. J Physiother, 66(1):59. [DOI] [PubMed] [Google Scholar]
- 22.Higgins JP, Altman DG, Gøtzsche PC, et al. (2011). Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ, 343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jeyaraman MM, Rabbani R, Al-Yousif N, et al. (2020). Interrater reliability and concurrent validity of ROBINS-I: protocol for a cross-sectional study. Syst Rev, 9(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sterne JA, Hernán MA, Reeves BC, et al. (2016). ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ, 355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McGuinness LA, Higgins JPT. (2021). Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods, 12(1):55–61. [DOI] [PubMed] [Google Scholar]
- 26.Moheboleslam Z, Mohammad Rahimi N, Aminzadeh R. (2022). A Systematic Review and Meta-analysis of Randomized Controlled Trials of Stabilizing Exercises for Lumbopelvic Region Impact in Postpartum Women With Low Back and Pelvic Pain. Biol Res Nurs, 24(3): 338–349. [DOI] [PubMed] [Google Scholar]
- 27.Luo D, Wan X, Liu J, et al. (2018). Optimally estimating the sample mean from the sample size, median, mid-range, and/or midquartile range. Stat Methods Med Res, 27(6):1785–1805. [DOI] [PubMed] [Google Scholar]
- 28.Wan X, Wang W, Liu J, et al. (2014). Estimating the sample mean and standard deviation from the sample size, median, range and/or inter-quartile range. BMC Med Res Methodol, 14:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bocchino M, Rea G, Capitelli L, et al. (2023). Chest CT Lung Abnormalities 1 Year after COVID-19: A Systematic Review and Meta-Analysis. Radiology, 308(1):e230535. [DOI] [PubMed] [Google Scholar]
- 30.StataCorp (2023). Stata Statistical Software: Release 18. College Station, TX: StataCorp LLC. www.stata.com/support/faqs/resources/citing-software-documentation-faqs/ [Google Scholar]
- 31.Xu C, Wang YR, Lu J, et al. (2019). Clinical efficacy of dynamic neuromuscular stabilization (DNS) in pain intensity and lumbar stabilizing muscle thickness in non-specific chronic lower back pain patients. Chinese Manipulation & Rehabilitation Medicine, 10(11):6–8. [Google Scholar]
- 32.Juárez-Albuixech ML, Redondo-González O, Tello I, et al. (2020). Vojta Therapy versus transcutaneous electrical nerve stimulation for lumbosciatica syndrome: A quasi-experimental pilot study. J Bodyw Mov Ther, 24(1):39–46. [DOI] [PubMed] [Google Scholar]
- 33.Yang KN, Li JH, Wu FC, et al. (2021). Study on the effect of dynamic neuromuscular stabilization technique for chronic low back pain. West China Medical Journal, 36(8):1062–1067. [Google Scholar]
- 34.Hamed WM, Ibrahim AH, Shalaby AS. (2021). Effect of vojta method on quality of life in patients with chronic non-specific low back pain. Egyptian Journal of Applied Science, 36(5): 29–40. [Google Scholar]
- 35.Park I, Park C, Kim K, et al. (2021). The effects of dynamic neuromuscular stability exercise on the scoliosis and pain control in the youth baseball players. Journal of Mechanics in Medicine and Biology, 21(9):2140030. [Google Scholar]
- 36.Ghavipanje V, Rahimi NM, Akhlaghi F. (2022). Six Weeks Effects of Dynamic Neuromuscular Stabilization (DNS) Training in Obese Postpartum Women with Low Back Pain: A Randomized Controlled Trial. Biol Res Nurs, 24(1):106–114. [DOI] [PubMed] [Google Scholar]
- 37.Ghavipanje V, Rahimi NM, Akhlaghi F. (2022b). The effect of 6 weeks dynamic neuromuscular stabilization (DNS) breathing exercises on postpartum balance and quality of life in primiparous women with low back pain. Iranian Journal of Obstetrics, Gynecology and Infertility, 25(5):78–86. [Google Scholar]
- 38.Najafi Ghagholestani B, Gandomi F, Assar S, et al. (2022). Effects of Dynamic Neuromuscular Stabilization and Aquatic Exercises on the Pain, Disability, Lumbopelvic Control, and Spinal Posture of Patients With Non-specific Low Back Pain. Iranian Rehabilitation Journal, 20(3): 333–344. [Google Scholar]
- 39.Mousavi SMS, Mirsafaei RR. (2022). Effect of Central Stability and Dynamic Neuromuscular Stabilization Exercises on Pain, Flexibility, Balance, Muscle Endurance and Quality of Life in Men With Nonspecific Chronic Low Back Pain. Journal of Guilan University of Medical Sciences, 31(2):136–149. [Google Scholar]
- 40.Lin T, Zhang JM, Wang TY. (2022). The rehabilitation effect of dynamic neuromuscular stabilization technology on elderly chronic non-specific low back pain. Zhongguo Xiangcun Yiyao, 29(21):21–22. [Google Scholar]
- 41.Iosub ME, Ianc D, Sîrbu E, et al. (2023). Vojta Therapy and Conservative Physical Therapy versus Physical Therapy Only for Lumbar Disc Protrusion: A Comparative Cohort Study from Romania. Appl Sci, 13:2292. [Google Scholar]
- 42.Karartı C, Özsoy İ, Özyurt F, et al. (2023). The effects of dynamic neuromuscular stabilization approach on clinical outcomes in older patients with chronic nonspecific low back pain: a randomized, controlled clinical trial. Somatosens Mot Res, 40(3):116–125. [DOI] [PubMed] [Google Scholar]
- 43.Sakai Y, Watanabe T, Wakao N, et al. (2022). Proprioception and Geriatric Low Back Pain. Spine Surg Relat Res, 6(5):422–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kolar P, Kobesova A, Valouchova P, et al. (2014). Dynamic neuromuscular stabilization: assessment methods. Recognizing and Treating Breathing Disorders (Second Edition), 93–98. [Google Scholar]
- 45.O’Sullivan P. (2005). Diagnosis and classification of chronic low back pain disorders: maladaptive movement and motor control impairments as underlying mechanism. Man Ther, 10(4):242–255. [DOI] [PubMed] [Google Scholar]
- 46.Purva Gulrandhe, Kovela RK. (2023). The Effect of Dynamic Neuromuscular Stabilisation on Core Strength: A Literature Review. Journal of Clinical and Diagnostic Research, 17:1–5. [Google Scholar]
- 47.Sannasi R, Dakshinamurthy A, Dommerholt J, et al. (2023). Diaphragm and core stabilization exercises in low back pain: A narrative review. J Bodyw Mov Ther, 36:221–227. [DOI] [PubMed] [Google Scholar]
- 48.Wang LM, Bi HY. (2022). Study of dynamic neuromuscular stabilization technique on balance and walking function of patients with Parkinson’s disease. Journal of Apoplexy and Nervous Diseases, 39(6):514–517. [Google Scholar]
- 49.Groessl EJ, Liu L, Schmalzl L, et al. (2020). Secondary Outcomes from a Randomized Controlled Trial of Yoga for Veterans with Chronic Low-Back Pain. Int J Yoga Therap, 30(1), 69–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Joyce AA, Kotler DH. (2017). Core Training in Low Back Disorders: Role of the Pilates Method. Curr Sports Med Rep, 16(3):156–161. [DOI] [PubMed] [Google Scholar]
- 51.Abadi Marand L, Noorizadeh Dehkordi S, Roohi-Azizi M, et al. (2022). Effect of dynamic neuromuscular stabilization on balance and trunk function in people with multiple sclerosis: protocol for a randomized control trial. Trials, 23(1):69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Abadi Marand L, Noorizadeh Dehkordi S, Roohi-Azizi M, et al. (2023). Effect of Dynamic Neuromuscular Stabilization on Balance, Trunk Function, Falling, and Spasticity in People With Multiple Sclerosis: A Randomized Controlled Trial. Arch Phys Med Rehabil, 104(1):90–101. [DOI] [PubMed] [Google Scholar]
- 53.Maia LB, Amarante LG, Vitorino DFM, et al. (2021). Effectiveness of conservative therapy on pain, disability and quality of life for low back pain in pregnancy: A systematic review of randomized controlled trials. Braz J Phys Ther, 25(6):676–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Guzman J, Esmail R, Karjalainen K, et al. (2001). Multidisciplinary rehabilitation for chronic low back pain: systematic review. BMJ, 322(7301):1511–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhu K, Devine A, Dick IM, et al. (2007). Association of back pain frequency with mortality, coronary heart events, mobility, and quality of life in elderly women. Spine (Phila Pa 1976), 32(18):2012–2018. [DOI] [PubMed] [Google Scholar]
- 56.Huijnen IPJ, Kindermans HPJ, Seelen HAM, et al. (2011). Effects of self-discrepancies on activity-related behaviour: explaining disability and quality of life in patients with chronic low back pain. Pain, 152(9):2165–2172. [DOI] [PubMed] [Google Scholar]
- 57.Boutevillain L, Dupeyron A, Rouch C, et al. (2017). Facilitators and barriers to physical activity in people with chronic low back pain: A qualitative study. PLoS One, 12(7):e0179826. [DOI] [PMC free article] [PubMed] [Google Scholar]