Abstract
Penetrating traumatic aortic injury (PTAI) is increasing in prevalence given the rise in firearm violence in the United States and is associated with significant morbidity and mortality. These injuries often result in hemorrhagic shock, with patients presenting in extremis or pulseless, traditionally requiring open approaches for repair. A rare but potentially devastating complication of firearm-related PTAI is bullet embolization. This case report describes the successful resuscitation and endovascular treatment of a patient with a firearm-induced PTAI complicated by acute limb ischemia secondary to bullet arterial embolization to the common femoral artery requiring arteriotomy for bullet removal.
Keywords: Vascular trauma, TEVAR, Thoracotomy, Aorta, Thoracic, Wounds, Gunshot
Traumatic aortic injury (TAI) is highly lethal, with approximately 80% of victims dying at the scene.1 Patients with penetrating TAI (PTAI) who arrive to a hospital are almost always in extremis or without signs of life,2 are more likely to require a resuscitative thoracotomy compared to those with blunt TAI (BTAI) (12.7% vs 6.1%, respectively), and have significantly higher mortality (43.1% vs 18.3%, respectively).3 As firearm-related injuries rise across the United States,4,5 PTAI is also likely to increase in incidence. Although thoracic endovascular aortic repair (TEVAR) has become the dominant surgical approach to TAIs,6,7 studies evaluating its use address BTAI given the higher prevalence in patients surviving to operation. To date, the use of TEVAR for PTAI has only been presented in case reports.8,9
Although a potential complication of firearm-related vascular trauma, bullet embolization remains a seldom reported phenomenon, most often described in a military setting with an incidence of 0.3% to 1.1%.10,11 Bullet embolization from firearm-related PTAI is sparsely documented.12 We present a case of PTAI causing hemorrhagic shock necessitating resuscitative thoracotomy and emergent TEVAR complicated by acute limb ischemia (ALI) secondary to bullet embolization to the right common femoral artery (CFA). Consent was obtained for report of the case and associated images.
Case report
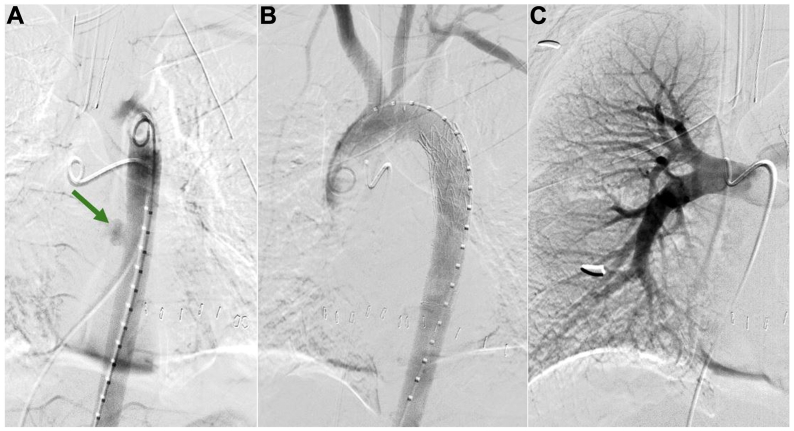
A 17-year-old boy presented after sustaining gunshot wounds to the right chest and upper extremity. Prior to hospital arrival, the patient was hypotensive (systolic blood pressure approximately 70 mm Hg), underwent bilateral chest needle decompression, and received one push of epinephrine by paramedics. Upon transfer to the trauma bay bed, the patient went into pulseless electrical activity arrest. A resuscitative thoracotomy with simultaneous right tube thoracostomy was performed with return of 950 mL of blood. At the same time, a massive transfusion protocol was activated using rapid infusion. Upon entry into the left chest, a periaortic hematoma was visualized, suspicious for thoracic aortic injury. Return of spontaneous circulation was achieved with cardiac massage and rapid transfusion. Systolic pressures improved to >160 mm Hg. With the extent of vascular injury unknown and the patient stabilizing, a computed tomography arteriogram (CTA) of the chest, abdomen, and pelvis was performed, revealing TAI of the midthoracic descending aorta with active extravasation into the mediastinum and in the region of the right lung hilum (Fig 1). Ballistic fragments were identified in the right lung middle lobe and right groin; however, it was unclear if the bullet was intravascular given evidence of distal perfusion.
Fig 1.
Initial computed tomography angiogram of the chest demonstrated a penetrating thoracic aortic injury with active extravasation into the mediastinum (A) as well as multiple foci of active extravasation within the right lung hilum that could not be localized (B). Areas of extravasation are identified with green arrows.
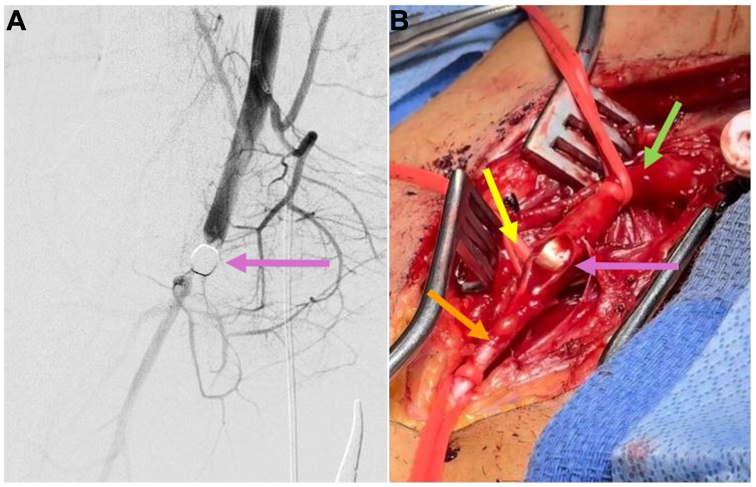
The patient remained hemodynamically stable with ongoing balanced transfusion. He was taken emergently to the hybrid operating room for endovascular repair of his TAI and interrogation of the pulmonary vasculature within 3 hours of initial injury. During ultrasound-guided access, the ballistic fragment made visualization of the right CFA difficult. Thus, right common femoral vein and left CFA access were obtained. The initial aortogram demonstrated extravasation at the mid-thoracic descending aorta (Fig 2, A-C). A Gore TAG 26 mm × 21 mm × 10 mm stent graft (W. L. Gore & Associates, Flagstaff, AZ) was deployed with resolution of aortic extravasation (Fig 2, A-C). The main pulmonary artery (PA) and selective bilateral PA angiograms demonstrated a possible small pseudoaneurysm of a right interlobar PA without extravasation (Fig 2, A-C). Right chest tube output remained minimal after initial insertion; no coiling was performed.
Fig 2.
On aortogram, there was active extravasation appreciated in the mid-thoracic descending aorta (A) that was adequately managed with one Gore TAG stent graft (B). On selective right pulmonary artery (PA) angiography, there was no obvious large pseudoaneurysm or active extravasation requiring intervention at this time (C).
Upon TEVAR completion, the patient did not have palpable distal pulses or Doppler signals in the right lower extremity. An angiogram demonstrated a ballistic fragment within the right CFA (Fig 3, A and B) that had not been palpable on physical examination. A standard right CFA exposure was performed with control of the CFA, superficial femoral artery (SFA), and profunda femoris using Potts ties. The patient was heparinized. A linear arteriotomy was made on the anterior wall of the CFA with removal of the bullet at the bifurcation of the SFA and profunda (Fig 3, A and B). Good forward and backward bleeding were confirmed with no endothelial damage appreciated. A patch angioplasty was performed with bovine pericardium and running 6-0 Prolene sutures. With percutaneous access maintained, suction thrombectomy was performed of the SFA, popliteal, and tibial arteries with completion angiography ensuring no remaining distal clot. The groin incision was closed in layers. A four-compartment right lower extremity fasciotomy was performed given ischemia time of >4 hours. The thoracotomy was closed with bilateral chest tubes in place. The patient was transferred to the intensive care unit.
Fig 3.
Right lower extremity arteriogram demonstrated a bullet fragment within the common femoral artery (CFA) limiting antegrade blood flow (A). Right femoral cutdown was performed with control of the right CFA (green arrow), profunda femoris (yellow arrow), and superficial femoral artery (SFA) (orange arrow) with CFA arteriotomy performed for bullet removal (purple arrow) (B).
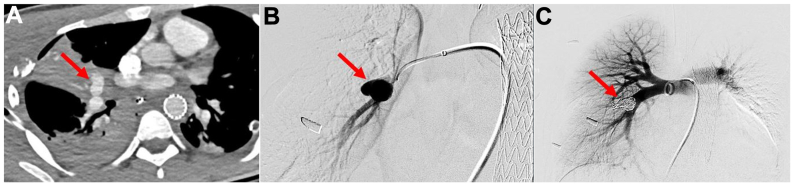
The patient recovered well with distal pulses appreciated in all four extremities. Repeat CTA revealed a 1.9 × 1.0-cm PA pseudoaneurysm for which the patient underwent percutaneous coiling with three 10 mm × 30-cm and two 14 mm × 50-cm interlocking detachable coils (Boston Scientific, Natick, MA) via right common femoral vein access (Fig 4). His fasciotomy was closed on postoperative day 10. He was discharged home on postoperative day 15.
Fig 4.
Repeat computed tomography angiogram demonstrated a large 1.9 × 1.0-cm right pulmonary artery (PA) pseudoaneurysm (PSA) (A) which was confirmed on invasive angiography (B). This was adequately treated with coil embolization with angiogram demonstrating no further pseudoaneurysm sac filling (C). The PSA is identified with red arrows.
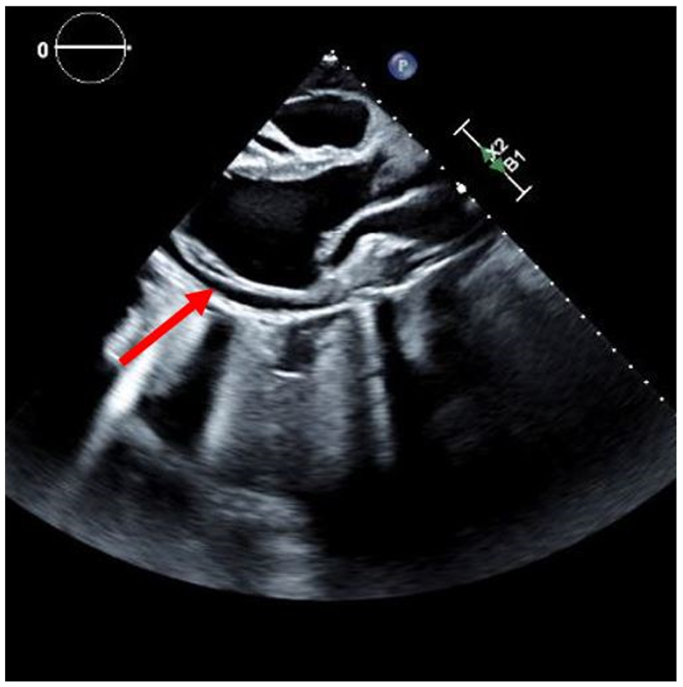
Ten days after discharge, the patient was readmitted with symptomatic pericardial effusion identified on echocardiogram (Fig 5). He underwent a pericardial window with fluid and tissue analysis confirming reactive etiology. He has since recovered appropriately. Follow-up CTA confirmed stable TEVAR and PA pseudoaneurysm coiling.
Fig 5.
Transthoracic echocardiogram revealed a moderate to large pericardial effusion identified with a red arrow.
Discussion
This case illustrates the successful use of TEVAR for PTAI complicated by ALI secondary to bullet arterial embolization. The rarity of using TEVAR for PTAI stems from the challenging clinical presentation, where most patients arrive at the hospital in extremis or pulseless.2 Traditionally, open repair has been the gold standard; however, TEVAR has emerged as a valuable alternative in TAI management.7
TEVAR for TAI has shown a significant decrease in mortality and low rates of neurological complications such as stroke or paralysis.13, 14, 15 Although most of these studies address BTAI, they may apply to patients with PTAI suitable for TEVAR who self-select based on injury extent and hemodynamic stability with resuscitation. Further research and collective experience in using TEVAR for PTAI are warranted to refine treatment strategies and optimize outcomes in this challenging patient population.
In civilian settings, lower energy weapons with smaller caliber bullets are more common, with a greater risk of incomplete vascular penetration and potential embolization.16, 17, 18 In reported cases, venous entry was more frequent than arterial entry (56% vs 27%, respectively) with the right ventricle and PA as the most frequent embolus destinations.19 In this case, early identification of ALI secondary to bullet arterial embolization was facilitated by the distal pulse examination and angiography after completion of the TEVAR. Preoperatively, the patient had thready distal lower extremity pulses likely owing to his shock state. This case is unusual in its presentation; arterial bullet emboli more frequently affect the left lower extremity than the right given the decreased angle of the iliac artery bifurcation.18,20 Invasive angiography is particularly beneficial in patients presenting in extremis, obtunded, or unable to describe the symptoms indicative of distal ischemia.21,22 Maintaining a high index of suspicion for bullet embolization in patients with vascular trauma and no identifiable exit wound is crucial. This case underscores the importance of integrating advanced imaging modalities such as angiography into the diagnostic and therapeutic algorithm for managing PTAI and its potential complications.
Conclusions
TEVAR offers a minimally invasive approach when patients present with focal injury, hemodynamic stability, or responsive to resuscitation. Arterial bullet embolization requires prompt recognition to prevent consequences of ALI.
Disclosures
None.
Footnotes
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Goldman M., Williams T.K. In: Current Therapy of trauma and surgical Critical care. Asensio J.A., editor. Elsevier; 2023. Thoracic aortic injury; pp. 317–322.e1. [Google Scholar]
- 2.Demetriades D., Theodorou D., Murray J., et al. Mortality and prognostic factors in penetrating injuries of the aorta. J Trauma Acute Care Surg. 1996;40:761–763. doi: 10.1097/00005373-199605000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Slocum C., Chiba H., Emigh B., et al. Nationwide analysis of penetrating thoracic aortic injury: injury patterns, management, and outcomes. J Surg Res. 2023;284:290–295. doi: 10.1016/j.jss.2022.11.077. [DOI] [PubMed] [Google Scholar]
- 4.Network GBoDC . Global burden of disease study 2019 (GBD 2019) results. Institute for Health Metrics and Evaluation Population Health Building/Hans Rosling Center; Seattle, WA: 2020. [Google Scholar]
- 5.Fowler K.A., Dahlberg L.L., Haileyesus T., Annest J.L. Firearm injuries in the United States. Prev Med. 2015;79:5–14. doi: 10.1016/j.ypmed.2015.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ultee K.H.J., Soden P.A., Chien V., et al. National trends in utilization and outcome of thoracic endovascular aortic repair for traumatic thoracic aortic injuries. J Vasc Surg. 2016;63:1232–1239.e1. doi: 10.1016/j.jvs.2015.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee W.A., Matsumura J.S., Mitchell R.S., et al. Endovascular repair of traumatic thoracic aortic injury: clinical practice guidelines of the Society for Vascular Surgery. J Vasc Surg. 2011;53:187–192. doi: 10.1016/j.jvs.2010.08.027. [DOI] [PubMed] [Google Scholar]
- 8.Huang X., Chen F., Yu C., Chen E., Zhou D. A rare case of penetrating thoracic aortic injury. Int J Surg Case Rep. 2023;106 doi: 10.1016/j.ijscr.2023.108184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sarquis L.M., Michaelis W., Santos Filho A.L., et al. Endovascular treatment of penetrating thoracic aorta injury–case report. J Vasc Bras. 2020;19 doi: 10.1590/1677-5449.200132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rich N.M., Collins G.J., Jr., Andersen C.A., McDonald P.T., Kozloff L., Ricotta J.J. Missile emboli. J Trauma. 1978;18:236–239. doi: 10.1097/00005373-197804000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Aidinian G., Fox C.J., Rasmussen T.E., Gillespie D.L. Varied presentations of missile emboli in military combat. J Vasc Surg. 2010;51:214–217. doi: 10.1016/j.jvs.2009.06.054. [DOI] [PubMed] [Google Scholar]
- 12.Biswas S., Cadot H., Abrol S. Gunshot wound of the thoracic aorta with right popliteal artery embolization: a case report of bullet embolism with review of relevant literature. Case Rep Emerg Med. 2013;2013 doi: 10.1155/2013/198617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karmy-Jones R., Ferrigno L., Teso D., Long I.I.I.W.B., Shackford S. Endovascular repair compared with operative repair of traumatic rupture of the thoracic aorta: a nonsystematic review and a plea for trauma-specific reporting guidelines. J Trauma Acute Care Surg. 2011;71:1059–1072. doi: 10.1097/TA.0b013e3182288783. [DOI] [PubMed] [Google Scholar]
- 14.Xenos E.S., Abedi N.N., Davenport D.L., et al. Meta-analysis of endovascular vs open repair for traumatic descending thoracic aortic rupture. J Vasc Surg. 2008;48:1343–1351. doi: 10.1016/j.jvs.2008.04.060. [DOI] [PubMed] [Google Scholar]
- 15.Hoffer E.K., Forauer A.R., Silas A.M., Gemery J.M. Endovascular stent-graft or open surgical repair for blunt thoracic aortic trauma: systematic review. J Vasc Intervent Radiol. 2008;19:1153–1164. doi: 10.1016/j.jvir.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 16.Maio V.J.D., Teal D.F. Gunshot wounds: practical aspects of firearms, ballistics, and forensic techniques. Plast Reconstr Surg. 1994;94:207. [Google Scholar]
- 17.Kani K.K., Porrino J.A., Chew F.S. Low-velocity, civilian firearm extremity injuries—review and update for radiologists. Skeletal Radiol. 2022;51:1153–1171. doi: 10.1007/s00256-021-03935-0. [DOI] [PubMed] [Google Scholar]
- 18.Shannon J.J., Jr., Vo N.M., Stanton P.E., Jr., Dimler M. Peripheral arterial missile embolization: a case report and 22-year literature review. J Vasc Surg. 1987;5:773–778. [PubMed] [Google Scholar]
- 19.Kuo A.H., Gregorat A.E., Restrepo C.S., Vinu-Nair S. Systematic review of civilian intravascular ballistic embolism reports during the last 30 years. J Vasc Surg. 2019;70:298–306.e6. doi: 10.1016/j.jvs.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 20.GARzoN A., Gliedman M.L. Peripheral embolization of a bullet following perforation of the thoracic aorta. Ann Surg. 1964;160:901–904. doi: 10.1097/00000658-196411000-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mattox K.L., Beall Jr AC., Ennix C.L., DeBakey M.E. Intravascular migratory bullets. Am J Surg. 1979;137:192–195. doi: 10.1016/0002-9610(79)90143-0. [DOI] [PubMed] [Google Scholar]
- 22.Kuo E.C., Harding J., Ham S.W., Magee G.A. Successful treatment and survival after gunshot wound to the aortic arch with bullet embolism to superficial femoral artery. J Vasc Surg Cases Innov Tech. 2019;5:283–288. doi: 10.1016/j.jvscit.2019.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]