Abstract
Background
The WHO-5 well-being index is a brief rating scale extensively used to evaluate well-being symptoms. Despite the increasing number of studies validating this instrument across different samples from different countries, its psychometric properties remain unexplored in the Philippine context. Bridging this gap, the present study assessed the psychometric properties of the WHO-5 in Filipinos amid the pandemic.
Methods
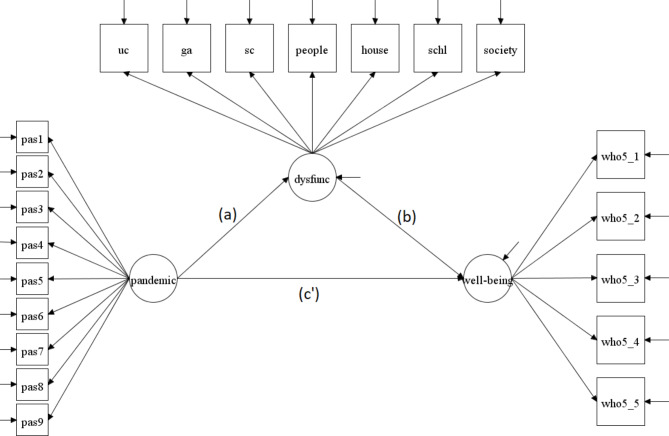
In study one, exploratory structural equation modeling (ESEM) was conducted using a sample of Filipinos (N = 2,521) from the general population and a unidimensional model of well-being was extracted. In study two, confirmatory factor analysis (CFA) was employed to examine the one-factor model in 1,289 Filipino government workers. In study three, nomological validity was examined by performing a mediation analysis using 407 Filipino left-behind emerging adult children with dysfunctionality as mediator, pandemic-related adversities as independent variable, and well-being as the dependent variable.
Results
The results of ESEM and CFA provided support for the WHO-5 one-factor model. Moreover, the negative relationship of well-being to anxiety, depression, and distress lend evidence to the scale’s criterion validity. The results of the mediation analysis performed in study three implied that those who experienced pandemic-related adversities tended to have greater dysfunctionality, and in turn, had lower levels of well-being.
Conclusions
Overall, the findings suggest that the WHO-5 well-being index is a psychometrically sound tool for measuring Filipinos’ well-being.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40359-024-01941-0.
Keywords: Psychometric properties, Validity, WHO-5 well-being index, Well-being, COVID-19 pandemic, Filipinos
Background
Mental health was traditionally perceived as a unidimensional construct. It was assumed that the absence of disorder symptoms equates to the presence of positive affect and higher functionality [1]. However, empirical and pragmatic observations asserted that there are individuals with mental health issues who do not experience high levels of happiness, and there are those who demonstrate elevated well-being despite suffering from a mental health problem [2, 3]. Thus, following the orthodox portrayal of mental health may not fully explain the psychological experiences of individuals [1]. The accuracy of measurement and treatment formulation can then be compromised as a result.
To address this limitation, several studies proposed a two-continua approach in conceptualizing psychological health. Psychological health was defined as comprising of two components: mental health disorders and well-being [4]. Whereas mental health disorders represent the negative aspect of psychological health characterized by depression, anxiety, and other forms of disorders, well-being embodies the positive feature of psychological health, signifying affirmative psychological functioning such as feelings of satisfaction, positive affect, and a sense of purpose in life [5, 6]. In the present study, the focal investigation is on the positive mental health component, well-being and its assessment.
The WHO-5 well-being index
The five-item World Health Organization Well-being Index (WHO-5) [7] is a widely used assessment instrument for well-being symptoms in both clinical [7–9] and non-clinical samples [10–13]. The WHO-5 comprises five positively formulated items that ask how an individual has felt over two weeks, answerable in under a minute [7]. While well-validated but longer well-being measures exist [14, 15], such parsimonious structure of the WHO-5 has made it efficient and convenient in monitoring well-being symptoms [16].
At present, the WHO-5 has been translated into more than 30 languages such as Chinese, Malay, Swedish, and Turkish [7, 17–20]. This has also been utilized in global research studies [7], validated across different countries [12, 13, 16, 21] and used to examine how well-being is linked with other constructs (e.g., depression, distress, anxiety, resilience) [11, 22, 23]. Despite these extensive studies substantiating the efficiency of the WHO-5 in evaluating well-being, there are only a few validation studies conducted in Asia [9, 18, 24], and none of these had been conducted in the Philippines. This study intends to bridge this gap by investigating the psychometric applicability of the WHO-5 in Filipino samples. The study offers the opportunity to understand the well-being of Filipinos, which has implications for tailoring intervention programs to safeguard their well-being. Moreover, previous research asserted that psychological tests, though substantiated in other contexts, should not be considered equally applicable in other settings as this might provide results that are not representative of the population being assessed [25]. Set against this backdrop, this study becomes relevant as this follows this proposition of validating psychological tools in the context where the assessment is to be made, thereby allowing accurate symptom detection [25, 26].
The latent factor structure of the WHO-5
The literature exploring the components of the WHO-5 purported the unidimensional structure of well-being [9, 12, 13]. Numerous research showed that all well-being symptoms as assessed by the WHO-5 are strongly engrained onto a single component, making it a single construct [12, 27]. The one-factor well-being model has been widely supported in the literature across different samples, including adolescents [28], pregnant women [29], and adults [20].
COVID-19 pandemic’s impact on Well-Being
Evidence on the negative impact of COVID-19 pandemic on well-being exists [31]. For instance, among medical professionals, it was noted that the level of subjective well-being was remarkably low [32]. Similarly, diminished well-being was also observed during the pandemic in the general population [32], pregnant women [29], adults [33], medical professionals [31], university students [34], and recovered COVID-19 patients [30]. Overall, the findings point out that individuals during the pandemic reported poor well-being [31, 35].
Notwithstanding the increasing research that has examined the well-being of individuals amid the pandemic, its extent in Asians, particularly among Filipinos, needs further investigation. The substantial decline in one’s well-being had been credited to the sordid situations (e.g., economic stress, job loss, death of loved ones) entailed by the quarantine measures taken to control the COVID-19 pandemic [36, 37]. However, reports showing how the pandemic negatively influenced one’s well-being require a valid, reliable, and contextually relevant psychological tool to help in the efficient assessment and monitoring of well-being symptoms. This is relevant as the debilitation of well-being could result in the development of pathological symptoms (e.g., depression, anxiety) and functional impairment [5, 6].
The present study
The current study comprised three stages, with each phase aiming to provide psychometric evidence for the WHO-5 as a tool that can be used in the assessment of well-being symptoms amid the COVID-19 pandemic. Specifically, the three studies aimed to: (1) determine evidence of validity by exploratory structural equation modeling (ESEM); (2) confirm the construct- and criterion-related validity of the factor structure model, and; (3) examine the nomological validity of the scale by examining the mediating role of dysfunctionality in the relationship between pandemic-related adversities and well-being. The ESEM analysis performed in study 1 is an encompassing combination of the best aspects of Confirmatory Factor Analysis (CFA) or Structural Equation Modeling (SEM) and traditional Exploratory Factor Analysis (EFA) [38]. It is primarily a confirmatory approach that allows researchers more control over the expected factor structure. After the unidimensional structure of the WHO-5 was established in study 1, study 2 tested the one-factor model of the WHO-5 among Filipino government workers. Lastly, study 3 was conducted to execute a crucial step in scale validation through testing well-being’s (as measured by WHO-5) nomological relationships with other constructs or variables [39] in a sample of Filipino left-behind emerging adult children. Well-being as measured by the WHO-5 has been shown to be significantly and moderately correlated with depression as measured by the Patient Health Questionnaire-9 or PHQ-9 (r=-.52) among people with infertility [11], significantly and strongly correlated with distress as measured by the Kessler Psychological Distress Scale or K-10 (r=-.075) among adults in New Zealand [40], and significantly and moderately correlated with anxiety as measured by the Generalized Anxiety Disorder Scale-7 or GAD-7 (r=-.035) among adolescents in Ghana [41].
The conduct of three studies to assess the WHO-5’s psychometric properties is aligned with a contemporary view of validity that stresses the importance of drawing from various sources of evidence using three different samples to aid in establishing the validity of inferences made [42].
Methods
Study 1
Participants and procedures
In study 1, data were collected from 2,521 Filipinos who worked in various occupations, such as essential non-government workers, and faculty and staff. The sample comprised 60% females (n = 1,512) and 40% males (n = 1,009), whose ages ranged from 18 to 68 years old (mean = 29.71, SD = 10.96). The majority of respondents were single (60.29%, n = 1,520). The participants were invited to answer a brief web-based anonymous survey by providing a link that redirects them to the Google Forms platform. They were given a thorough explanation on the purpose of the study and their rights as participants. Answering the questionnaire was voluntary and the participants’ identities were anonymous. If they decided to take part in the study, participants signified their consent by ticking the box labeled “yes.” The conduct of this study was appraised and approved by the ethics review committee of the College of Education in Mindanao State University-Iligan Institute of Technology, Philippines.
Measures
Well-being
The World Health Organization-Five Well-Being Index (WHO-5) [7] is a self-report scale which measures the participants’ level of well-being. Participants were asked to rate five (5) positively worded items about how they have been feeling in response to the COVID-19 pandemic (i.e., I have felt cheerful and in good spirits). Using a 6-point Likert scale ranging from 0 (at no time) to 5 (all of the time), participants were asked to indicate the frequency of their experiences in the last two weeks. Previous studies provided evidence of good psychometric properties for this scale [12, 16, 43]. In this sample, the WHO-5 had a Cronbach’s alpha of 0.95.
Data analysis
Before performing factor analysis, this study calculated Horn’s parallel analysis using the 5 items from the WHO-5 scale. By employing parallel analysis, estimated eigenvalues were randomly simulated to identify the number of factors that would be retained. The retention of a factor is based on the rule of which eigenvalues of the actual data are higher than those of the average simulated random eigenvalues. Eigenvalues obtained from the randomly simulated data are kept within a confidence interval of 0.05 in order to attain more accurate results. In this study, 5,000 iterations were generated to calculate the mean eigenvalues. Utilizing the suggested number of factors from parallel analysis, exploratory structural equation modeling (ESEM) analysis using the geomin method with oblique rotation was performed. ESEM is a technique which allows simultaneous computation of both confirmatory factor analysis (CFA) and exploratory factor analysis (EFA) models [44]. ESEM approach is superior to EFA and CFA since, unlike EFA, ESEM allows the correlation between item uniqueness, and unlike CFA, it allows all items to load on all factors (i.e., cross-loadings). ESEM is an integrative approach that uses the best aspects of CFAs/SEMs and traditional EFAs [38]. As mentioned in the background, ESEM allows researchers more control over the expected factor structure. Furthermore, ESEM provides a reliable method of evaluating model adequacy (i.e., goodness-of-fit indices).
The goodness-of-fit is based on the following indices: chi-square (χ²), comparative fit index (CFI), Tucker-Lewis index (TLI), and standardized root mean squared residual (SRMR). CFI and TLI values of ≥ 0.90 were regarded as adequate fit, while values of ≥ 0.95 were considered an excellent fit. SRMR values of < 0.05 suggest excellent fit, whereas values between 0.05 and 0.10 signify adequate fit [45]. SRMR was used instead of the root mean square error of approximation (RMSEA) as it is less sensitive to misspecification (e.g., smaller degrees of freedom, correlated residuals) as compared to other fit indices [46]. Maximum likelihood estimation was used as the estimation method. The use of this estimator was deemed sufficient for our purposes, as it was the estimation method recommended for models with continuous indicators [47]. All statistical analyses in studies one, two, and three were performed using Mplus version 7.11 [48].
Study 2
Participants and procedures
The participants in study 2 comprised 1,289 Filipino government workers. Law enforcers (48.41%, n = 624), civil servants (44.38%, n = 572), and healthcare workers (7.21%, n = 93) were among the participants. This study had 53.76% (n = 693) males and 46.24% (n = 596) females, whose ages ranged from 20 to 69 years old (mean = 34.12, SD = 9.12). The majority were married (53.45%, n = 689), Bachelor’s degree holders (87.28%, n = 1,125), and had been in the public service for more than 10 years (42.90%, n = 553).
The scales used in this study were translated to Bisaya (local dialect) and Filipino language through a forward-backward translation process. In this method, a language expert initially translated the English version of the scales to Bisaya and Filipino, and another expert back-translated the Bisaya and Filipino translations to English. An item-to-item comparison was then conducted to guarantee semantic equivalence. The translated scales were reviewed, discussed, and finalized for administration by a team composed of a clinical psychologist, psychometricians, and language experts.
The participants were invited to answer a brief web-based anonymous scales (i.e., Google Form platform). Before responding to the scales, the participants were given an informed consent form with a thorough explanation on the purpose of the study and their rights as participants. They signified their consent by ticking the box labeled “Yes, I agree to take the assessment.” Answering the questionnaire was voluntary and the participants’ identities were anonymous. The ethics committee of the College of Education in Mindanao State University-Iligan Institute of Technology, Philippines reviewed the procedures of the study and gave the ethical clearance for its implementation.
Measures
Well-being
To confirm the results of ESEM in study 1, the WHO-5 scale [7] was used. This scale assesses how participants have been feeling for the past two weeks in response to the COVID-19 pandemic. Participants were asked to rate a five-item self-report scale with six-point Likert scale ranging from 0 (at no time) to 5 (all of the time). The final score was calculated by multiplying the total raw score (score range: 0–25) by four, where zero represents the lowest possible well-being and 100 reflecting the highest possible well-being state. This scale has been found to demonstrate good internal reliability and validity [12, 16, 43]. In this study, the WHO-5 had a Cronbach’s alpha of 0.93.
Psychological distress
The Kessler Psychological Distress Scale (K-10) [49] was utilized to measure the individual’s level of psychological distress for the last 30 days. This 10-item scale uses a five-point Likert scale, which ranges from 0 (none of the time) to 4 (all of the time). A sample item is, “During the last 30 days, about how often did you feel hopeless?” A higher score on this scale indicates greater levels of psychological distress. This scale showed high internal reliability and validity in previous studies [50, 51], including one study among Filipino teachers [52]. In this study, the K-10 had a Cronbach’s alpha of 0.97.
Major depression
The Patient Health Questionnaire-9 (PHQ-9) [53] was used to evaluate symptoms of major depressive disorder by asking the respondents how often they have been bothered by specific problems over the last two weeks. Using the Diagnostic and Statistical Manual of Mental Disorders’ (DSM-5’s) nine-item criteria, the PHQ-9 uses a four-point Likert scale ranging from 0 (not at all) to 3 (nearly every day). A sample item is, “feeling tired or having little energy.” Research has demonstrated PHQ-9’s validity and reliability [47, 48]. The scale has also been validated among Filipino and Indonesian migrant domestic workers in Macao [54, 55], among university students in Africa [56], and among Brazilian older adults [57]. In this study, the PHQ-9 had an internal consistency of 0.94.
Generalized anxiety
The Generalized Anxiety Disorder-7 scale (GAD-7) [58] was used to measure the individual’s symptoms of generalized anxiety disorder. The GAD-7 is a 7-item scale that measures how often the individual has been bothered by the symptoms for the past two weeks. This scale uses a four-point Likert scale ranging from 0 (not at all) to 3 (nearly every day). A sample item is, “worrying too much about different things.” There is validity evidence for the GAD-7 in various research [58–60]. The scale’s psychometric properties have also been validated among Filipino migrant domestic workers in Macao [54], and a repurposed GAD-7 anchored in COVID-19 pandemic experiences has been validated previously using a factor-and person-centered approach [61]. In this study, the GAD-7 had a Cronbach’s alpha of 0.94.
Data analysis
Confirmatory factor analysis (CFA) was employed to confirm the well-being model extracted from study 1. Maximum likelihood estimation with robust standard errors was used as the estimation method. This is the estimation method recommended for models with continuous indicators [47]. The goodness-of-fit of the model is based on the following indices: Satorra-Bentler chi-square (S-Bχ²), CFI, TLI, and SRMR. The cut-off values for these fit indices were shown in study 1. To provide criterion-related evidence of validity, the final score of the WHO-5 was correlated with scores on measures of psychological distress, major depression, and generalized anxiety. Cohen’s d was used to measure the effect size on the strength of the relationship between the variables; values of 0.2, 0.5, and 0.8 suggest small, medium, and large effect sizes, respectively [62]. The effect size of the strength of the relationship between the variables was determined using the calculated Pearson r − value; values of 0.2, 0.5, and 0.8 suggest small, medium, and large effect sizes, respectively [63, 64].
Study 3
Participants and procedures
Using purposive sampling, respondents were selected on the basis that either one or both of their parents were working as overseas Filipino workers (OFW), and that they were at least 18 years old. This sample was labelled, “left-behind emerging adult children (LBEAC),” and 407 of them participated in this study. They came from public and private schools in a semi-urban city in the southern Philippines.
The participants were predominantly female (71%, n = 289), incoming freshmen or in their first-year college (68.30%, n = 278), and with ages ranging from 18 to 28 years old (mean = 19.95, SD = 1.79).
Data collection for study 3 transpired through a digital platform to prevent the spread of COVID-19. Communication letters were sent via electronic mail to relevant school authorities from the different public and private secondary and tertiary institutions in Northern Mindanao, asking permission to conduct the assessment. Given the peculiarity of the participants, a respondent-driven method known as the snowball technique [62] was utilized as the main sampling procedure – a participant was asked to nominate another respondent suitable for the assessment. They were invited to answer the survey by providing a link that redirects them to a web-based platform. An informed consent form that stipulated the nature and purpose of the study, participants’ rights, and obligations of the researchers, was given to the participants. Participants were informed that answering the questionnaire was voluntary and that their identities would be treated with utmost confidentiality. If they decided to take part in the study, respondents signified their consent by ticking the box labeled “yes”. The conduct of this study was reviewed and approved by the ethics review committee of the College of Education in Mindanao State University-Iligan Institute of Technology, Philippines.
Measures
Well-being
To provide evidence for construct-related validity, the WHO-5 [7] was employed as a criterion variable. Participants were asked about how they have been feeling for the past two weeks using a six-point Likert scale (0 = at no time; 5 = all of the time). Higher scores on this scale represent the best possible state of well-being. This scale was found to demonstrate good internal reliability and validity [12, 16, 43]. In this sample, the WHO-5 had a Cronbach’s alpha of 0.94.
COVID-19 pandemic-related adversities
A nine-item pandemic-related adversity checklist was devised to assess the participant’s experience amidst the COVID-19 pandemic. The checklist comprised nine situations that families of OFWs might have encountered during the pandemic. These items were generated through a literature review and interviews. Several pandemic-related articles showing the predictors of distress and common mental health symptoms were reviewed to draft the initial checklist of pandemic-related stressors. Considering the nature of the target sample, interviews with select individuals possessing the target sample characteristics (i.e., parents who are overseas Filipino workers and are at least 18 years old) were conducted to contextualize the items to the migration setting amid the pandemic. Following the interviews, the items were refined and finalized by a clinical psychologist and psychometricians for administration.
During the scale administration, participants were instructed to indicate whether they experienced the situation (1 = yes) or not (0 = no). Sample items are the following: “the migrant parent(s) lost his/their job abroad”, “the migrant parent(s) got infected with COVID-19”, “financial burden associated with the migration situation”, and “deteriorating family relationships in relation to the migration situation.” The frequency distribution of the respondents’ experiences is presented in Supplementary Table 1. In this study, this scale obtained an internal consistency of 0.82.
Dysfunctionality
The adult self-administered version of the World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0) [65] was employed to evaluate the individual’s level of functioning across seven domains: understanding and communicating (e.g., Concentrating on doing something for ten minutes?), getting around (e.g., Standing for long periods, such as 30 min?), self-care (e.g., Washing your whole body?), getting along with people (e.g., Dealing with people you do not know?), life activities-household (e.g., Taking care of your household responsibilities?), life activities-school (e.g., Your day-to-day work/school?), and participation in society (e.g., How much of a problem did you have because of barriers or hindrances around you?). The WHODAS 2.0 is a 36-item scale that evaluates the intensity of difficulty experienced in doing specific activities during the past 30 days. Participants rated each item from 1 (none) to 5 (extreme or cannot do). A composite score was calculated by summing the score of each item wherein higher rating denoted greater difficulty in fulfilling their daily tasks or functions. The WHODAS was proven to be reliable and valid in previous research [66, 67]. In this study, the WHODAS yielded- a Cronbach’s alpha of 0.97.
Data analysis
Nomological evidence of validity was extracted through mediation analysis. This analysis intended to examine the influence of pandemic-related adversities on students’ well-being through dysfunctionality. The mediation model’s goodness-of-fit was determined by the following indices: S-Bχ², CFI, TLI, and SRMR/WRMR. In addition, the measurement model of the scales used in this study were calculated to secure their validity and provide support to the structural mediation model. Similar cut-off values for the goodness-of-fit indicated in study 1 were applied. Maximum likelihood estimation with robust standard errors was used as the estimation method. It is the estimation method recommended for models with continuous indicators [47]. This estimator further guarantees robustness to non-normality, which means that the analysis can provide accurate results even under non-normal data distribution [68]. Meanwhile, in examining the measurement model of the COVID-19 Pandemic Adversity Checklist, the weighted least square mean and variance adjusted estimator (WLSMV) was utilized as the estimation method considering the scale’s nature of data (i.e., binary). WLSMV is the suggested estimation method for models with binary data [69, 70].
Results and discussion
Study 1
The mean score of the WHO-5 is 64.93 (SD = 24.72). Results of parallel analysis revealed a one-factor solution, which accounted for 40.04% of the variance (see Table 1). The ESEM one-factor solution yielded an excellent fit with χ2 (5, n = 2,521) = 350.74, p < .001, CFI = 0.97, TLI = 0.95, and SRMR = 0.02. In addition, the factor loadings of the one-factor, ranging from 0.88 to 0.91, signify that the items explain a sufficient amount of the variance in the well-being factor (see Table 2). The current finding is consistent with previous studies suggesting that the one-factor solution best fits the WHO-5 well-being [9, 11, 71] (see Table 3).
Table 1.
Study 1 results of parallel analysis
| Factor | Eigenvalues for sample correlation matrix | Average Eigenvalue from Parallel Analysis | 95th Percentile Eigenvalues from Parallel Analysis |
|---|---|---|---|
| 1 | 4.201a | 1.055 | 1.081 |
| 2 | 0.303 | 1.024 | 1.042 |
| 3 | 0.178 | 1.000 | 1.013 |
| 4 | 0.174 | 0.975 | 0.992 |
| 5 | 0.144 | 0.945 | 0.966 |
Note: a where eigenvalues from actual data is larger than 95th percentile eigenvalues from parallel analysis
Table 2.
Standardized factor loadings for 1-factor ESEM (study 1)
| Items | Factor loadings |
|---|---|
| 1. I have felt cheerful and in good spirits. | 0.876 |
| 2. I have felt calm and relaxed. | 0.907 |
| 3. I have felt active and vigorous. | 0.913 |
| 4. I woke up feeling fresh and rested. | 0.889 |
| 5. My daily life has been filled with things that interest me. | 0.888 |
Notes: ESEM; Geomin with oblique rotation. All factor loadings are significant at p < .01
Table 3.
Orrelations of well-being with psychological distress, major depression, and generalized anxiety
| 1 | 2 | 3 | 4 | |
|---|---|---|---|---|
| 1. Wellbeing | --- | −0.24** | −0.23** | −0.23** |
| 2. Psychological Distress | --- | 0.81** | 0.77** | |
| 3. Major Depression | --- | 0.83** | ||
| 4. Generalized Anxiety | --- | |||
| α | 0.93 | 0.97 | 0.94 | 0.94 |
| Mean | 68.63 | 7.63 | 5.60 | 4.77 |
| SD | 20.56 | 8.63 | 6.07 | 5.05 |
Note: All correlations are standardized and significant at p < .01 level; n = 1289; α = Cronbach’s Alpha; SD = Standard Deviation
Study 2
Table 4 presents the correlation between well-being with psychological distress, major depression, and generalized anxiety, internal consistency, mean, and standard deviation of the variables measured in study 2. In establishing the criterion-related validity, results showed well-being is significantly negatively linked with psychological distress, major depression, and generalized anxiety, with r − values of − 0.24, − 0.23, and − 0.23, respectively. Utilizing these correlation coefficients as a measure of effect size following the guidelines of Cohen [63, 64], it can be inferred that the magnitude of the strength of association between these variables suggest a small effect size. These outcomes signify that they are correlated and yet are independent measures, implying that they are evaluating distinct constructs. Such results supplement evidence to the postulation that well-being and mental health disorders are two distinct components of mental health; while well-being is a measure of positive mental health, psychological distress, major depression, and generalized anxiety cover the negative facets of mental health [5, 6]. Moreover, the negative correlation results are consistent with previous research indicating that higher levels of anxiety and depression are associated with individual’s decreased well-being and quality of life [57, 58]. Similarly, an individual’s enhanced psychological well-being had been found to be linked with lower levels of anxiety and depression [74, 75]. The average score of the respondents on the WHO-5 was 68.63 (SD = 20.56). The CFA results of the one-factor WHO-5 obtained a good fit with S-Bχ2 (5, n = 1,289) = 128.20, p < .001, CFI = 0.96, TLI = 0.92, and SRMR = 0.04. The standardized factor loadings, ranging from 0.79 to 0.90, confirmed that the five WHO-5 items are well-embedded in a single well-being factor (see Table 4).
Table 4.
Standardized factor loadings for 1-factor CFA (study 2)
| Items | Factor loadings |
|---|---|
| 1. I have felt cheerful and in good spirits. | 0.794 |
| 2. I have felt calm and relaxed. | 0.838 |
| 3. I have felt active and vigorous. | 0.903 |
| 4. I woke up feeling fresh and rested. | 0.863 |
| 5. My daily life has been filled with things that interest me. | 0.865 |
Note: All factor loadings are significant at p < .01
Study 3
In study 3, the WHO-5 had an average score of 48.75 (SD = 26.32). The fit indices of the measurement model showed excellent fit for the one-factor WHO-5 (S-Bχ2 [5, n = 407] = 18.59, p < .01, CFI = 0.99, TLI = 0.979, and SRMR = 0.02) and the one-factor pandemic-related adversities (S-Bχ2 [27, n = 407] = 60.269, p < .01, CFI = 0.99, TLI = 0.99, and WRMR = 0.95). Similarly, the seven-factor WHODAS showed good fit with S-Bχ2 (14, n = 407) = 95.73, p < .001, CFI = 0.94, TLI = 0.91, SRMR = 0.04.
Zero-order correlation results revealed that while the pandemic distress (independent variable) is significantly positively linked with dysfunctionality (mediating variable), it is not significantly related to well-being (dependent variable). The results further show dysfunctionality is significantly negatively correlated with well-being (see Supplementary Table 2). Guided by the assertion of previous studies that a mediation analysis does not necessarily require establishing an association between the independent and dependent variable, the mediation analysis was still performed [76, 77].
The fit indices of the mediation model (see Fig. 1) exhibited an adequate fit with S-Bχ2 (186, n = 407) = 466.016, p < .001, CFI = 0.94, TLI = 0.93, and SRMR = 0.05. Table 5 shows the standardized coefficients of the mediation analysis. Findings show that the path between the individual’s pandemic-related adversities and dysfunctionality, as well as the path between dysfunctionality and well-being, was found to be significant. It is significant to note that the pathway linking pandemic distress and well-being was not direct but indirect (via dysfunctionality), suggesting a complete or full mediation result. This finding denotes that the pandemic distress was associated with well-being due to its association with dysfunctionality. These results imply that the pandemic-related adversities experienced by the individuals are related to difficulties with their daily functioning, and that this dysfunctionality is associated with lower levels of well-being.
Fig. 1.
Mediation model of pandemic-related distress and well-being through dysfunctionality
Table 5.
Results of mediation analyses between pandemic distress and wellbeing
| Independent Variable (IV) | Mediating Variable (M) | Dependent Variable (DV) | Effect of IV on M (a) | Effect of M on DV (b) | Direct Effect (c’) | Total Effect (c) | Indirect Effects | Std. Error | BC 95% CI | |
|---|---|---|---|---|---|---|---|---|---|---|
| LL | UL | |||||||||
| Pandemic distress | Dysfunctionality | Wellbeing | 0.104* | -0.262** | -0.286 | -0.493 | -0.207* | 0.116 | -0.398 | -0.017 |
Note: All coefficients are standardized; All latent structural model. *p< .05, **p< .01
General discussion
The primary objective of the present study was to assess the psychometric properties of the WHO-5 well-being scale anchored in COVID-19 pandemic experiences. Results of any validation effort are posited to be contingent upon the context in which the studies were conducted and the characteristics of the sample used [39], further justifying the conduct of this study. To the authors’ knowledge, none so far have investigated the validity of WHO-5 in a Filipino sample within the context of the COVID-19 pandemic.
Consolidated evidence from the three studies demonstrated the psychometric soundness of the WHO-5. In study 1, using ESEM, construct-related validity was evident with the one-factor model’s adequate to excellent fit indices. In study 2, construct- and criterion-related evidence of validity were apparent with CFA’s excellent fit indices confirming one-factor model and well-being’s significant relationship with lower anxiety and depression. In study 3, nomological validity was corroborated with a mediation model showing that experiencing pandemic-related adversities tends to increase one’s dysfunctionality, and ultimately, lowers the levels of well-being.
The latent factor structure of WHO-5: construct-related evidence of Validity
Results of the first two studies show support for the one-factor model of well-being. This model had been validated in previous studies across various cultures and population groups such as adolescents and students [61, 78], pregnant women [29], adults [20], and recovered COVID-19 patients [30].
Findings complement previous research asserting that all well-being items are strongly entrenched onto one dimension, suggesting a single construct [12, 27]. Examining the items, it could be said that these indicators reflect the characteristic of those with higher subjective well-being. For instance, cheerfulness [79–81], calm and peaceful [82–84], lots of energy [85–87], fresh and rested [88–90], and interested in things [91, 92] are indices of subjective well-being.
The average variance extracted (AVE) of the variables used in the three studies was further investigated. The results showed values ranging from 0.59 to 0.80, which surpassed the suggested acceptable AVE value of 0.50 [93] (see Supplementary Table 3). This finding implies that the average variances of items can be accounted for well by the latent factor of the variables more than the error of their respective measurement items [93]. In addition, the McDonald’s omega and composite reliability were calculated to add confirmation to the study variables’ reliability. Reflected in Supplementary Table 3, the omega (values ranged from 0.92 to 0.97) and composite reliability (values ranged from 0.92 to 0.98) results indicate that the scales obtained high reliability.a.
Evidence of criterion-related validity: well-being and its relationship with anxiety, depression, and distress
Results revealed the WHO-5 scores to be significantly negatively related to major depression, psychological distress, and generalized anxiety. These results corroborated previous research suggesting the negative association of well-being as measured by the WHO-5 with psychological distress and common psychological disorders [72–74].
This negative association between well-being (in the form of emotional vitality and life interest) and psychopathological symptoms can generally be understood using the broaden-and-build theory [94, 95]. Fredrickson (2004) proposed that the experience of positive emotions (i.e., cheerfulness, happiness, life interest) unlocks the cognitive capacity to think freely, thoughtfully, and creatively. This generates an affirmative outlook to see the world from a positive and broader perspective, enabling people’s ability to think and create possible coping strategies when faced with stressful situations [94, 96–98]. Thus, it stimulates creative and flexible thinking, better adaptive psychosocial functioning, and more effective coping mechanisms which, in turn, lowers the susceptibility to experience mental health problems [94, 98–100].
Alternatively, those who exhibit lower levels of well-being, characterized by unhappiness and lack of interest in life, adopt a pessimistic thinking approach towards stressful situations [101, 102]. They perceive these situations as a dead end and tend to focus on the worst things that could happen [101, 103]. Such thinking style narrows their capacity to make ways to manage stressful situations, thereby increasing their risk of developing mental health problems [83, 101, 103].
Pandemic-related adversities, dysfunctionality, well-being: nomological validity of the WHO-5 scale
Another method that can help augment evidence of validity is by means of establishing nomological validity (i.e., mediation analysis). In this study, a mediation analysis was conducted, exploring how the link between pandemic-related adversities and well-being was mediated by dysfunctionality. The mediation results demonstrated that the pandemic-related adversities are likely to enhance dysfunctionality, ultimately resulting in lower well-being. These findings imply that those who experienced distressing situations brought about by the pandemic tend to have difficulties in fulfilling daily tasks, and in turn, possess lower levels of well-being. These findings are parallel to previous research showing that those who were exposed to sordid circumstances (e.g., financial insecurity, deteriorating family relationships, and family member’s job loss) consequent to the COVID-19 pandemic tend to have problems in responding to daily activities [104], and are less likely to exhibit positivity and satisfaction in life [105–107].
These findings could be meaningfully understood against the theoretical backdrop of the conservation of resources theory (COR) [108], particularly on the notion of resource loss in the face of a stressful event. COR theory posits that stressful events entail a constellation of hazards nested within individuals and communities which preclude and drain resources [109, 110]. For instance, the 2008 Sichuan earthquake caused 69,227 deaths and 374,643 injuries; its resultant economic losses totaled more than ¥845 billion yuan [111, 112]. The consequent economic losses brought a plight of under- and unemployment among individuals that challenged the ability to meet their needs [111]. Moreover, many survivors lost their family members and homes [113], resulting in poor physical and mental well-being of individuals.
Adopting this perspective in the current study, the COVID-19 pandemic crisis caused distressing events that housed hazards for losing resources among individuals. The preventive measures (e.g., mandatory lockdowns and quarantine) implemented to help curb the spread of the virus forced people to stay home and maintain physical distance; this limited the capacity to fulfill their typical work duties, social interactions, and life routine, resulting in exhaustion and the eventual development of distressing symptoms [114]. Following these safety measures further impacted the labor market, causing some to lose jobs and take pay cuts (Akbari et al., 2023). The loss or restraint in socioeconomic resources could limit one’s ability to satiate necessities and, in turn, might lead to the deterioration of well-being. Specifically, the pandemic crisis has brought radical stressful situations in the migration setting that brought the risk of loss of essential resources to children of economic migrant workers (or the LBEAC). For instance, the migrant parents losing jobs or experiencing salary cuts due to the economic decline involved the risk of losing an important family resource (i.e., family economic resource). The loss (or threat of loss) of financial resources could hinder the ability of family members to access goods and services to suffice daily needs [112, 115], restricting the functional capability to fulfill daily roles. These functional limitations, in turn, could hamper their ability to experience well-being [116, 117]. Another example is the event of their migrant parent(s) contracting the COVID-19 virus or worrying about the health status of their migrant parents abroad. This distressing event entailed the risk of losing a family resource known to substantially affect well-being [110, 118].
Limitations
This study has several caveats that warrant acknowledgment. First, the participants were recruited through a non-probability sampling method which could introduce selection bias and provide inaccurate results [119, 120]. Thus, there must be discretion in interpreting the data as a representative sample of the Filipino population. Future research may utilize probability sampling techniques with measures that reduce biases of all forms to improve the generalizability of the findings. Second, this study used a cross-sectional design which limits temporal comparison as data were obtained at a specific timeframe only. Future researchers may collect longitudinal data over multiple points in time as this approach may yield information on how the WHO-5 changes or remains stable throughout the pandemic. Third, the WHO-5 is a self-report measure that makes responses vulnerable to social desirability bias. Future research may administer scales that statistically control for potential biases. Fourth, the COVID-19 Pandemic Adversity Checklist’s psychometric properties (e.g., face and content validity) were not established before its administration in this study. Despite showing demonstrable validity and reliability indices in the present sample, it is recommended to investigate and establish its psychometric properties in future research to ensure the scale’s adequacy to measure pandemic-related stressors. Lastly, while the use of maximum likelihood estimation method was sufficient for our study’s purposes [47], its use may have impacted the results. Therefore, future researchers may consider employing alternative estimation methods such as diagonally weighted least squares (DWLS) or mean-and variance-adjusted LR test statistic (MLMV) as they are deemed by other scholars to be more suitable [25]. Lastly, the present study did not investigate the psychometric equivalence of well-being across group characteristics (e.g., gender) or measurement occasions. Future researchers may consider exploring the measurement invariance of the WHO-5 well-being index scale to add support for its validity and clarify whether well-being has the same or different meaning for different groups or at different times; this can help formulate a more tailor-fitted intervention promoting well-being.
Conclusion
Overall, the results provided evidence for the WHO-5 as a psychometrically sound tool for measuring well-being symptoms. The unidimensional structure of the questionnaire was confirmed in ESEM and CFA in the two sample sets. The criterion-related validation findings reflected significant negative relationships of the WHO-5 to psychological distress, major depression, and anxiety. The findings further revealed that dysfunctionality mediated the link between pandemic-related adversity and well-being. This implies that experiencing pandemic-related adversities results in greater dysfunctionality, which eventually could lead to lower levels of well-being. All these results substantiated the use of the WHO-5 to measure well-being symptoms. Considering the need to validate psychological tests in samples where assessment is to be made [25, 26], the validation of the WHO-5 could bridge the gap in the lack of tests assessing well-being in an Asian sample (i.e., Filipinos) in the context of the COVID-19 pandemic. This tool may then guide the practitioners in crafting, implementing, and evaluating programs to enhance well-being in the midst of these dire times.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author contributions
The main and the second authors were involved in writing and conceptualization, the corresponding author contributed to writing and analysis, and the fourth author was involved in conceptualization and data analysis. The corresponding author will be responsible for the final approval of proofs, should the article be accepted for publication.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Data availability
The datasets analyzed in the current study will be made available upon reasonable request.
Declarations
Human ethics and consent to participate
This study had been conducted in accordance with the ethical standards of the American Psychological association and of the 1964 Declaration of Helsinki and its later amendments. Ethics approval for the study was granted by the ethics review committee of the College of Education in Mindanao State University-Iligan Institute of Technology, Philippines. Informed consent was obtained from all the participants prior to data collection.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Black L, Panayiotou M, Humphrey N. The dimensionality and latent structure of mental health difficulties and wellbeing in early adolescence. Hashimoto K, ed. PLoS ONE. 2019;14(2):e0213018. 10.1371/journal.pone.0213018 [DOI] [PMC free article] [PubMed]
- 2.Keyes CLM. Mental Illness and/or Mental Health? Investigating axioms of the Complete State Model of Health. J Consult Clin Psychol. 2005;73(3):539–48. 10.1037/0022-006X.73.*3.539. [DOI] [PubMed]
- 3.Keyes CLM, Shmotkin D, Ryff CD. Optimizing well-being: the empirical encounter of two traditions. J Pers Soc Psychol. 2002;82(6):1007–22. 10.1037/0022-3514.82.6.1007. [PubMed] [Google Scholar]
- 4.Ryff CD, Keyes CLM. The structure of Psychological Well-being revisited. J Pers Soc Psychol. 1995;69(4):719. 10.1037/0022-3514.69.4.719. [DOI] [PubMed] [Google Scholar]
- 5.Lamers SMA, Westerhof GJ, Glas CAW, Bohlmeijer ET. The bidirectional relation between positive mental health and psychopathology in a longitudinal representative panel study. J Posit Psychol. 2015;10(6):553–60. 10.1080/17439760.2015.1015156. [Google Scholar]
- 6.Grant F, Guille C, Sen S. Well-Being and the Risk of Depression under Stress. Laks J, ed. PLoS ONE. 2013;8(7):e67395. 10.1371/journal.pone.0067395 [DOI] [PMC free article] [PubMed]
- 7.Topp CW, Østergaard SD, Søndergaard S, Bech P. The WHO-5 well-being index: a systematic review of the literature. Psychother Psychosom. 2015;84(3):167–76. 10.1159/000376585. [DOI] [PubMed] [Google Scholar]
- 8.Bonnín CM, Yatham LN, Michalak EE, et al. Psychometric properties of the well-being index (WHO-5) Spanish version in a sample of euthymic patients with bipolar disorder. J Affect Disord. 2018;228:153–9. 10.1016/j.jad.2017.12.006. [DOI] [PubMed] [Google Scholar]
- 9.Dadfar M, Momeni Safarabad N, Asgharnejad Farid AA, Nemati Shirzy M, Ghazie Pour Abarghouie F. Reliability, validity, and factorial structure of the World Health Organization-5 Well-Being Index (WHO-5) in Iranian psychiatric outpatients. Trends Psychiatry Psychother. 2018;40(2):79–84. 10.1590/2237-6089-2017-0044. [DOI] [PubMed] [Google Scholar]
- 10.Akhtar M, Kroener-Herwig B. Coping styles and Socio-demographic variables as predictors of Psychological Well-Being among International Students belonging to different cultures. Curr Psychol. 2019;38(3):618–26. 10.1007/s12144-017-9635-3. [Google Scholar]
- 11.Omani-Samani R, Maroufizadeh S, Almasi-Hashiani A, Sepidarkish M, Amini P. The WHO-5 Well-Being Index: A Validation Study in People with Infertility. ijph. Published online July 4, 2020. 10.18502/ijph.v48i11.3525 [PMC free article] [PubMed]
- 12.Faruk MO, Alam F, Chowdhury KUA, Soron TR. Validation of the Bangla WHO-5 well-being index. Glob Ment Health. 2021;8:e26. 10.1017/gmh.2021.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lara-Cabrera M, Betancort M, Muñoz-Rubilar A, Rodríguez-Novo N, Bjerkeset O, De Las Cuevas C. Psychometric properties of the WHO-5 well-being index among nurses during the COVID-19 pandemic: a cross-sectional study in three countries. IJERPH. 2022;19(16):10106. 10.3390/ijerph191610106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Longo Y, Jovanović V, Sampaio De Carvalho J, Karaś D. The General factor of Well-Being: multinational evidence using Bifactor ESEM on the Mental Health Continuum–Short Form. Assessment. 2020;27(3):596–606. 10.1177/1073191117748394. [DOI] [PubMed] [Google Scholar]
- 15.Monteiro F, Fonseca A, Pereira M, Canavarro MC. Measuring Positive Mental Health in the Postpartum period: the Bifactor structure of the Mental Health Continuum–Short Form in Portuguese Women. Assessment. 2021;28(5):1434–44. 10.1177/1073191120910247. [DOI] [PubMed] [Google Scholar]
- 16.Chan L, Liu RKW, Lam TP, Chen JY, Tipoe GL, Ganotice FA. Validation of the World Health Organization Well-Being Index (WHO-5) among medical educators in Hong Kong: a confirmatory factor analysis. Med Educ Online. 2022;27(1):2044635. 10.1080/10872981.2022.2044635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Löve J, Andersson L, Moore CD, Hensing G. Psychometric analysis of the Swedish translation of the WHO well-being index. Qual Life Res. 2014;23(1):293–7. 10.1007/s11136-013-0447-0. [DOI] [PubMed] [Google Scholar]
- 18.Fung Sfu, Kong CYW, Liu Y, man, et al. Validity and psychometric evaluation of the Chinese Version of the 5-Item WHO well-being index. Front Public Health. 2022;10:872436. 10.3389/fpubh.2022.872436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Suhaimi AF, Makki SM, Tan KA, Silim UA, Ibrahim N. Translation and validation of the malay version of the WHO-5 well-being index: reliability and validity evidence from a sample of type 2 diabetes Mellitus patients. IJERPH. 2022;19(7):4415. 10.3390/ijerph19074415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eser E, Çevik C, Baydur H, et al. Reliability and validity of the Turkish version of the WHO-5, in adults and older adults for its use in primary care settings. Prim Health Care Res Dev. 2019;20:e100. 10.1017/S1463423619000343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Caycho-Rodríguez T, Vilca LW, Valencia PD, et al. Is the meaning of subjective well-being similar in latin American countries? A cross-cultural measurement invariance study of the WHO-5 well-being index during the COVID-19 pandemic. BMC Psychol. 2023;11(1):102. 10.1186/s40359-023-01149-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chow KM, Tang WKF, Chan WHC, Sit WHJ, Choi KC, Chan S. Resilience and well-being of university nursing students in Hong Kong: a cross-sectional study. BMC Med Educ. 2018;18(1):13. 10.1186/s12909-018-1119-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Winzer R, Vaez M, Lindberg L, Sorjonen K. Exploring associations between subjective well-being and personality over a time span of 15–18 months: a cohort study of adolescents in Sweden. BMC Psychol. 2021;9(1):173. 10.1186/s40359-021-00673-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barua A, Kar N. Screening for depression in elderly Indian population. Indian J Psychiatry. 2010;52(2):150. 10.4103/0019-5545.64595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bernardo ABI. Lost in translation? Challenges in using psychological tests in the Philippines. Silliman J. 2011;52(1):19–41. [Google Scholar]
- 26.Ali GC, Ryan G, De Silva MJ. Validated Screening Tools for Common Mental Disorders in Low and Middle Income Countries: A Systematic Review. Burns JK, ed. PLoS ONE. 2016;11(6):e0156939. 10.1371/journal.pone.0156939 [DOI] [PMC free article] [PubMed]
- 27.Sischka PE, Costa AP, Steffgen G, Schmidt AF. The WHO-5 well-being index–validation based on item response theory and the analysis of measurement invariance across 35 countries. J Affect Disord Rep. 2020;1:100020. 10.1016/j.jadr.2020.100020. [Google Scholar]
- 28.De Wit M, Pouwer F, Gemke RJBJ, Delemarre-van De Waal HA, Snoek FJ. Validation of the WHO-5 well-being index in adolescents with type 1 diabetes. Diabetes Care. 2007;30(8):2003–6. 10.2337/dc07-0447. [DOI] [PubMed] [Google Scholar]
- 29.Mortazavi F, Mehrabadi M, KiaeeTabar R. Pregnant women’s well-being and worry during the COVID-19 pandemic: a cross-sectional study. BMC Pregnancy Childbirth. 2021;21(1):59. 10.1186/s12884-021-03548-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dai Z, Wang H, Xiao W, et al. The association of mindfulness and psychological well-being among individuals who have recovered from COVID-19 in Jianghan District, Wuhan, China: a cross-sectional study. J Affect Disord. 2022;319:437–45. 10.1016/j.jad.2022.09.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Badahdah AM, Khamis F, Mahyijari NA. The psychological well-being of physicians during COVID-19 outbreak in Oman. Psychiatry Res. 2020;289:113053. 10.1016/j.psychres.2020.113053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pieh C, Probst T, Budimir S, Humer E. Diminished well-being persists beyond the end of the COVID-19 lockdown. Gen Hosp Psychiatry. 2021;70:137–8. 10.1016/j.genhosppsych.2021.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Faulkner J, O’Brien WJ, McGrane B, et al. Physical activity, mental health and well-being of adults during initial COVID-19 containment strategies: a multi-country cross-sectional analysis. JSAMS. 2021;24(4):320–6. 10.1016/j.jsams.2020.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Holm-Hadulla RM, Klimov M, Juche T, Möltner A, Herpertz SC. Well-being and Mental Health of students during the COVID-19 pandemic. Psychopathol. 2021;54(6):291–7. 10.1159/000519366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lades LK, Laffan K, Daly M, Delaney L. Daily emotional well-being during the COVID‐19 pandemic. Br J Health Psychol. 2020;25(4):902–11. 10.1111/bjhp.12450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict. 2022;20(3):1537–45. 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Qiu M, Sha J, Utomo S. Listening to forests: comparing the Perceived restorative characteristics of natural soundscapes before and after the COVID-19 pandemic. Sustainability. 2020;13(1):293. 10.3390/su13010293. [Google Scholar]
- 38.Marsh HW, Morin AJ, Parker PD, Kaur G. (2014). Exploratory structural equation modeling: An integration of the best features of exploratory and confirmatory factor analysis. Annu Rev Clin Psychol. 2014;10:85–110. 10.1146/annurev-clinpsy-032813-153700 [DOI] [PubMed]
- 39.Jebb AT, Ng V, Tay L. A review of Key Likert Scale Development advances: 1995–2019. Front Psychol. 2021;12(1590). 10.3389/fpsyg.2021.637547. [DOI] [PMC free article] [PubMed]
- 40.Tanveer S, Schluter PJ, Beaglehole B, Porter RJ, Boden J, Sulaiman-Hill R, Scarf D, Dean S, Assad F, Hasnat MA, Bell C. The COVID Psychosocial impacts Scale: a reliable and valid tool to examine the psychosocial impacts of the COVID-19 pandemic. Int J Environ Res Public Health. 2023;20(11):5990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Adjorlolo S. Generalised anxiety disorder in adolescents in Ghana: examination of the psychometric properties of the Generalised anxiety Disorder-7 scale. Afr J Psychol Assess. 2019;1(1). 10.4102/ajopa.v1i0.10.
- 42.Zumbo BD. Structural equation modeling and test validation. Brian Everitt and David C. Howell, Encyclopedia of statistics in behavioral science. John Wiley & Sons Ltd.; 2005. pp. 1951–8.
- 43.Low KY, Pheh KS, Tan CS. Validation of the WHO-5 as a screening tool for depression among young adults in Malaysia. Curr Psychol. 2023;42(10):7841–4. 10.1007/s12144-021-02152-1. [Google Scholar]
- 44.Asparouhov T, Muthén B. Exploratory structural equation modeling. Struct Equation Modeling: Multidisciplinary J. 2009;16(3):397–438. 10.1080/10705510903008204. [Google Scholar]
- 45.Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38(1):1–10. 10.1007/BF02291170. [Google Scholar]
- 46.Kenny DA, Kaniskan B, McCoach DB. The performance of RMSEA in Models with Small degrees of Freedom. Sociol Methods Res. 2015;44(3):486–507. 10.1177/0049124114543236. [Google Scholar]
- 47.Swami V, Maïano C, Morin AJ. (2023). A guide to exploratory structural equation modeling (ESEM) and bifactor-ESEM in body image research. Body Image. 2023;47(101641). 10.1016/j.bodyim.2023.101641
- 48.Muthén LK, Muthén BO. Mplus (Version 7.11) [Computer Software]. Los Angeles: Author; 2013. [Google Scholar]
- 49.Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SL, Walters EE, Zaslavsky AM. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959 – 76. 10.1017/s0033291702006074. PMID: 12214795. [DOI] [PubMed]
- 50.Hoffman J, Cossie Q, Ametaj AA, et al. Construct validity and factor structure of the Kessler-10 in South Africa. BMC Psychol. 2022;10(1):177. 10.1186/s40359-022-00883-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Naisanga M, Ametaj A, Kim HH, et al. Construct validity and factor structure of the K-10 among Ugandan adults. J Affect Disord. 2022;311:143–7. 10.1016/j.jad.2022.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mordeno IG, Piape QT, Roño AGR, Abejar WAC, Ferolino MAL, Mendoza NB. Repurposing the K-10=: the factor structure and Latent Profile of COVID-19 pandemic-anchored psychological distress symptoms among Filipino teachers. J Psychoeduc Assess. 2024;0(0). 10.1177/07342829241229768.
- 53.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hall BJ, Patel A, Lao L, Liem A, Mayawati EH, Tjipto S. Structural validation of the Patient Health Questionnaire-9 (PHQ-9) among Filipina and Indonesian female migrant domestic workers in Macao: STRUCTURAL VALIDATION OF PHQ-9. Psychiatry Res. 2021;295(113575). 10.1016/j.psychres.2020.113575. [DOI] [PubMed]
- 55.Garabiles MR, Lao CK, Yip P, Chan EW, Mordeno I, Hall BJ. Psychometric validation of PHQ–9 and GAD–7 in Filipino migrant domestic workers in Macao (SAR), China. J Pers Assess. 2020;102(6):833–44. 10.1080/00223891.2019.1644343. [DOI] [PubMed] [Google Scholar]
- 56.Makhubela M, Khumalo IP. Psychometric evaluation of the PHQ-9 in university students: factorial validity and measurement equivalence across three African countries. Curr Psychol. 2022;118061–9. 10.1007/s12144-022-02997-0.
- 57.Moreno-Agostino D, Chua KC, Peters TJ, Scazufca M, Araya R. Psychometric properties of the PHQ-9 measure of depression among Brazilian older adults. Aging Ment Health. 2022;26(11):2285–90. 10.1080/13607863.2021.1963951. [DOI] [PubMed] [Google Scholar]
- 58.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092. 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 59.Dhira TA, Rahman MA, Sarker AR, Mehareen J. Validity and reliability of the Generalized Anxiety Disorder-7 (GAD-7) among university students of Bangladesh. Innamorati M, ed. PLoS ONE. 2021;16(12):e0261590. 10.1371/journal.pone.0261590 [DOI] [PMC free article] [PubMed]
- 60.Monterrosa-Blanco A, Cassiani-Miranda CA, Scoppetta O, Monterrosa-Castro A. Generalized anxiety disorder scale (GAD-7) has adequate psychometric properties in Colombian general practitioners during COVID-19 pandemic. Gen Hosp Psychiatry. 2021;70:147–8. 10.1016/j.genhosppsych.2021.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mordeno IG, Gallemit IMJS, Ducay JL, Abdullah SP, Suba SMS, Edaros ND. Validating repurposed GAD-7 anchored in COVID‐19 pandemic experiences: a factor‐and person‐centered approach. Psychol Schools. 2024;61(3):1069–89. 10.1002/pits.23100. [Google Scholar]
- 62.Sullivan GM, Feinn R. (2012). Using effect size—or why the P value is not enough. J Grad Med Educ. 2012;4(3), 279–282. 10.4300/JGME-D-12-00156.1 [DOI] [PMC free article] [PubMed]
- 63.Cohen J. A power primer. Psychol Bull. 1992;112(1):155–9. [DOI] [PubMed] [Google Scholar]
- 64.Cohen J. Statistical power analysis for the behavioral sciences. Routledge; 2013.
- 65.Goodman LA. Snowball sampling. Ann Math Stat. 1961;1:148–70.
- 66.Üstün TB, Chatterji S, Kostanjsek N, et al. Developing the World Health Organization Disability Assessment schedule 2.0. Bull World Health Organ. 2010;88(11):815–23. 10.2471/BLT.09.067231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bejer A, Ćwirlej-Sozańska A, Wiśniowska-Szurlej A, et al. Psychometric properties of the Polish version of the 36-item WHODAS 2.0 in patients with hip and knee osteoarthritis. Qual Life Res. 2021;30(8):2415–27. 10.1007/s11136-021-02806-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Satorra A, Bentler PM. Corrections to test statistics and standard errors in covariance structure analysis. In: von Eye A, Clogg CC, editors. Latent variables analysis: applications for developmental research. Sage Publications, Inc.; 1994. pp. 399–419.
- 69.Brauer K, Ranger J, Ziegler M. Confirmatory factor analyses in psychological test adaptation and development. PTAD. 2023. 10.1027/2698-1866/a000034. [Google Scholar]
- 70.Park CG. Implementing alternative estimation methods to test the construct validity of likert-scale instruments. Korean J Women Health Nurs. 2023;29(2):85. 10.4069/kjwhn.2023.06.14.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Midhage R, Hermansson L, Söderberg P, et al. Psychometric evaluation of the Swedish self-rated 36-item version of WHODAS 2.0 for use in psychiatric populations – using classical test theory. Nord J Psychiat. 2021;75(7):494–501. 10.1080/08039488.2021.1897162. [DOI] [PubMed] [Google Scholar]
- 72.Hajos TRS, Pouwer F, Skovlund SE, et al. Psychometric and screening properties of the WHO-5 well‐being index in adult outpatients with type 1 or type 2 diabetes mellitus. Diabet Med. 2013;30(2). 10.1111/dme.12040. [DOI] [PubMed]
- 73.Bellali T, Manomenidis G, Meramveliotaki E, Minasidou E, Galanis P. The impact of anxiety and depression in the quality of life and psychological well-being of Greek hematological cancer patients on chemotherapy. Psychol Health Med. 2020;25(2):201–13. 10.1080/13548506.2019.1695864. [DOI] [PubMed] [Google Scholar]
- 74.Sønderskov KM, Dinesen PT, Vistisen HT, Østergaard SD. Variation in psychological well-being and symptoms of anxiety and depression during the COVID-19 pandemic: results from a three-wave panel survey. Acta Neuropsychiatr. 2021;33(3):156–9. 10.1017/neu.2020.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ceri V, Cicek I. Psychological Well-Being, depression and stress during COVID-19 pandemic in Turkey: a comparative study of Healthcare professionals and Non-healthcare professionals. Psychol Health Med. 2021;26(1):85–97. 10.1080/13548506.2020.1859566. [DOI] [PubMed] [Google Scholar]
- 76.Agler R, De Boeck P. On the interpretation and use of mediation: multiple perspectives on mediation analysis. Front Psychol. 2017;8:293306. 10.3389/fpsyg.2017.01984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Preacher KJ, Hayes AF. Assessing mediation in communication research). London: The; 2008. pp. 13–54. https://quantpsy.org/pubs/preacher_hayes_2008.pdf. Sage sourcebook of advanced data analysis methods for communication research.
- 78.Downs A, Boucher LA, Campbell DG, Polyakov A. Using the WHO–5 well-being index to identify College students at risk for Mental Health problems. JCSD. 2017;58(1):113–7. 10.1353/csd.2017.0008. [Google Scholar]
- 79.Lau C, Chiesi F, Saklofske DH. The combinative role of traits cheerfulness and seriousness relating to resiliency and well-being: a moderated mediation model. Pers Individ Dif. 2019;151:109515. 10.1016/j.paid.2019.109515. [Google Scholar]
- 80.Lau C, Chiesi F, Hofmann J, Ruch W, Saklofske DH. Cheerfulness and life satisfaction mediated by self-esteem and behavioral activation: a serial mediation model. Pers Individ Dif. 2020;166:110175. 10.1016/j.paid.2020.110175. [Google Scholar]
- 81.Ruch W, Hofmann J. A temperament approach to humor. In: Gremigni P, editor. Humor and Health Promotion. Hauppauge, NY: Nova Science; 2012. pp. 79–113. [Google Scholar]
- 82.Lee C, Leoutsakos J, Lyketsos CG, Steffens DC, Breitner JCS, Norton MC. Latent class-derived subgroups of depressive symptoms in a community sample of older adults: the Cache County study. Int J Geriat Psychiatry. 2012;27(10):1061–9. 10.1002/gps.2824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Huppert FA, So TTC. Flourishing across Europe: application of a new conceptual Framework for defining well-being. Soc Indic Res. 2013;110(3):837–61. 10.1007/s11205-011-9966-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Longo Y, Coyne I, Joseph S, Gustavsson P. Support for a general factor of well-being. Pers Individ Dif. 2016;100:68–72. 10.1016/j.paid.2016.03.082. [Google Scholar]
- 85.de Bloom J, Geurts SAE, Taris TW, Sonnentag S, De Weerth C, Kompier MAJ. Effects of vacation from work on health and well-being: lots of fun, quickly gone. Work Stress. 2010;24(2):196–216. 10.1080/02678373.2010.493385. [Google Scholar]
- 86.Elliott J, Fallows A, Staetsky L, et al. The health and well-being of cancer survivors in the UK: findings from a population-based survey. Br J Cancer. 2011;105(S1):S11–20. 10.1038/bjc.2011.418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Mayer A, Smith EK. Exploring the link between energy security and subjective well-being: a study of 22 nations. Energ Sustain Soc. 2019;9(1):34. 10.1186/s13705-019-0216-1. [Google Scholar]
- 88.Delgado-Lobete L, Montes-Montes R, Vila-Paz A, et al. Subjective well-being in Higher Education: Psychometric properties of the satisfaction with life and subjective vitality scales in Spanish University students. Sustainability. 2020;12(6):2176. 10.3390/su12062176. [Google Scholar]
- 89.Guérin ED, Vitality. Well-Being, and quality of life: a conceptual examination emphasizing their similarities and differences with Special Application in the physical activity domain. JPAH. 2012;9(6):896–908. 10.1123/jpah.9.6.896. [DOI] [PubMed] [Google Scholar]
- 90.Ryan RM, Frederick C. On Energy, personality, and Health: subjective vitality as a dynamic reflection of well-being. J Pers. 1997;65(3):529–65. 10.1111/j.1467-6494.1997.tb00326.x. [DOI] [PubMed] [Google Scholar]
- 91.Kapteyn A, Lee J, Tassot C, Vonkova H, Zamarro G. Dimensions of Subjective Well-Being. Soc Indic Res. 2015;123(3):625–60. 10.1007/s11205-014-0753-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Nima AA, Cloninger KM, Persson BN, Sikström S, Garcia D. Validation of Subjective Well-being measures using item response theory. Front Psychol. 2020;10:3036. 10.3389/fpsyg.2019.03036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hair JF Jr, Hult GTM, Ringle CM, Sarstedt M, Danks NP, Ray S. (2021). Partia least squares structural equation modeling (PLS-SEM) using R: A workbook Springer Nature; 2021:197.
- 94.Fredrickson BL. The broaden–and–build theory of positive emotions. Huppert FA, Baylis N, Keverne B, eds. Phil Trans R Soc Lond B. 2004;359(1449):1367–1377. 10.1098/rstb.2004.1512 [DOI] [PMC free article] [PubMed]
- 95.Fredrickson BL, Branigan C. Positive emotions broaden the scope of attention and thought-action repertoires. Cogn Emot. 2005;19(3):313–32. 10.1080/02699930441000238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Park N. The role of Subjective Well-being in positive Youth Development. ANNALS Am Acad Political Social Sci. 2004;591(1):25–39. 10.1177/0002716203260078. [Google Scholar]
- 97.Proctor CL, Linley PA, Maltby J. Youth Life satisfaction: a review of the literature. J Happiness Stud. 2009;10(5):583–630. 10.1007/s10902-008-9110-9. [Google Scholar]
- 98.Proctor C, Linley PA, Maltby J. Very happy youths: benefits of very high life satisfaction among adolescents. Soc Indic Res. 2010;98(3):519–32. 10.1007/s11205-009-9562-2. [Google Scholar]
- 99.Stiglbauer B, Gnambs T, Gamsjäger M, Batinic B. The upward spiral of adolescents’ positive school experiences and happiness: investigating reciprocal effects over time. J Sch Psychol. 2013;51(2):231–42. 10.1016/j.jsp.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 100.Suldo SM, Huebner ES. Does life satisfaction moderate the effects of stressful life events on psychopathological behavior during adolescence? Sch Psychol Q. 2004;19(2):93–105. 10.1521/scpq.19.2.93.33313. [Google Scholar]
- 101.Lyubomirsky S, Dickerhoof R, Boehm JK, Sheldon KM. Becoming happier takes both a will and a proper way: an experimental longitudinal intervention to boost well-being. Emotion. 2011;11(2):391–402. 10.1037/a0022575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Feliu-Soler A, De Diego-Adeliño J, Luciano JV, et al. Unhappy while depressed: examining the dimensionality, reliability and validity of the subjective happiness scale in a Spanish sample of patients with depressive disorders. IJERPH. 2021;18(20):10964. 10.3390/ijerph182010964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Lightsey OR. Thinking positive as a stress buffer: the role of positive automatic cognitions in depression and happiness. J Couns Psychol. 1994;41(3):325. 10.1037/0022-0167.41.3.325. [Google Scholar]
- 104.Gassman-Pines A, Ananat EO, Fitz-Henley J. COVID-19 and parent-child Psychological Well-being. Pediatrics. 2020;146(4):e2020007294. 10.1542/peds.2020-007294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Christner N, Essler S, Hazzam A, Paulus M. Children’s psychological well-being and problem behavior during the COVID-19 pandemic: An online study during the lockdown period in Germany. Slobodskaya HR, ed. PLoS ONE. 2021;16(6):e0253473. 10.1371/journal.pone.0253473 [DOI] [PMC free article] [PubMed]
- 106.Mureșan GM, Văidean VL, Mare C, Achim MV. Were we happy and we didn’t know it? A subjective dynamic and financial assessment pre-, during and post-COVID-19. Eur J Health Econ. 2023;24(5):749–68. 10.1007/s10198-022-01506-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wang MT, Henry DA, Del Toro J, Scanlon CL, Schall JD. COVID-19 employment status, Dyadic Family Relationships, and child Psychological Well-Being. J Adolesc Health. 2021;69(5):705–12. 10.1016/j.jadohealth.2021.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hobfoll SE. Conservation of resources: a new attempt at conceptualizing stress. Am Psychol. 1989;44:513–24. 10.1037/0003-066X.44.3.513. [DOI] [PubMed] [Google Scholar]
- 109.Layne CM, Beck C, Rimmasch H, Southwick J, Moreno M, Hobfoll S. Chapter 2: promoting resilient posttraumatic adjustment in childhood and beyond. In: Brom D, Pat-Horencyzk R, Ford J, editors. Treating traumatized children: risk, resilience, and recovery. Routledge; 2009. pp. 13–47.
- 110.Holmgreen L, Tirone V, Gerhart J, Hobfoll SE. Conservation of resources Theory: Resource caravans and passageways in Health contexts. In: Cooper CL, Quick JC, editors. The Handbook of Stress and Health. 1st ed. Wiley; 2017. pp. 443–57. 10.1002/9781118993811.ch27.
- 111.Yang J, Chen J, Liu H, Zheng J. Comparison of two large earthquakes in China: the 2008 Sichuan Wenchuan Earthquake and the 2013 Sichuan Lushan Earthquake. Nat Hazards. 2014;73(2):1127–36. 10.1007/s11069-014-1121-8. [Google Scholar]
- 112.Zhang R, Lu Y, Du H. Vulnerability and resilience in the wake of COVID-19: family resources and children’s well-being in China. Chin Sociol Rev. 2022;54(1):27–61. 10.1080/21620555.2021.1913721. [Google Scholar]
- 113.Fan F, Zhang Y, Yang Y, Mo L, Liu X. Symptoms of posttraumatic stress disorder, depression, and anxiety among adolescents following the 2008 Wenchuan earthquake in China. J Trauma Stress. 2011;24(1):44–53. 10.1002/jts.20599. [DOI] [PubMed] [Google Scholar]
- 114.Akbari M, Seydavi M, Babaeifard M, Firoozabadi MA, Nikčević AV, Spada MM. Psychometric properties and psychological correlates of the COVID-19 anxiety syndrome scale: a comprehensive systematic review and meta-analysis. Clin Psychol Psychother. 2023;30(5):931–49. 10.1002/cpp.2861. [DOI] [PubMed] [Google Scholar]
- 115.Dodgen D, Donato D, Dutta T, Kelly N, La Greca A, Morganstein J, Reser J, Ruzek J, Schweitzer S, Shimamoto MM, Tart KT, Ursano R. Chapter 8: Mental Health and Well-Being. In Crimmins J, Balbus JL, Gamble CB, Beard JE, Bell D, Dodgen RJ, Eisen, eds. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment. Washington, DC: U.S. Global Change Research Program; 2016:217–246. 10.7930/J0TX3C9H
- 116.Nguyen C, Ranque B, Baubet T et al. Clinical, Functional and Health-Related Quality of Life Correlates of Clinically Significant Symptoms of Anxiety and Depression in Patients with Systemic Sclerosis: A Cross-Sectional Survey. Kuwana M, ed. PLoS ONE. 2014;9(2):e90484. 10.1371/journal.pone.0090484 [DOI] [PMC free article] [PubMed]
- 117.Stein LA, Goldmann E, Zamzam A, et al. Association between anxiety, Depression, and post-traumatic stress disorder and outcomes after ischemic stroke. Front Neurol. 2018;9:890. 10.3389/fneur.2018.00890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Mordeno IG, Gallemit IMJS, Lantud SSB, Hall BJ. Personal psychological resources mediate parent–child relationship and mental health among left-behind children. PsyCh J. 2019;8(3):318–29. 10.1002/pchj.288. [DOI] [PubMed] [Google Scholar]
- 119.Galloway A. Non-probability / purposive sampling. Published 2005. Accessed February 09, 2023. hospi-web.qmuc.ac.uk/imrestxt/sampling/puposive.htm
- 120.Kunda Z, Spencer SJ. When do stereotypes come to mind and when do they color judgment? A goal-based theoretical framework for stereotype activation and application. Psychol Bull. 2003;129(4):522–44. 10.1037/0033-2909.129.4.522. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets analyzed in the current study will be made available upon reasonable request.