Abstract
Purpose.
One criticism of published curricula addressing implicit bias is that few achieve skill development in implicit bias recognition and management (IBRM). To inform the development of skills-based curricula addressing IBRM, we conducted a scoping review of the literature inquiring, “What interventions exist focused on IBRM in professions related to social determinants of health: education, law, social work, and the health professions inclusive of nursing, allied health professions, and medicine?”
Methods.
Authors searched eight databases for articles published from 2000–2020. Included studies: 1) described interventions related to implicit bias; and 2) addressed knowledge, attitude and/or skills as outcomes. Excluded were interventions solely focused on reducing/neutralizing implicit bias. Article review for inclusion and data charting occurred independently and in duplicate. Investigators compared characteristics across studies; data charting focused on educational and assessment strategies.
Results.
Fifty-one full-text articles for data charting and synthesis, with more than 6568 learners, were selected. Educational strategies included provocative/engagement triggers, the Implicit Association Test, reflection and discussion, and various active learning strategies. Most assessments were self-report, with fewer objective measures. Eighteen funded studies utilized federal, foundation, institutional, and private sources.
Conclusion.
This review adds to the literature by providing tangible examples of curricula to complement existing frameworks, and identifying opportunities for further research in innovative skills-based instruction, learner assessment, and development and validation of outcome metrics. Continued research addressing IBRM would enable learners to develop and practice skills to recognize and manage their implicit biases during clinical encounters, thereby advancing the goal of improved, equitable patient outcomes.
Implicit biases are developed over time. They are a consequence of an individual’s lived experience, socialization process, and are often rooted in systemic discrimination (Feagin and Bennefield 2014). Research on implicit bias has demonstrated that clinician bias and point of care discrimination contribute to less effective communication behaviors and disparate medical decision-making (Cooper et al. 2012; Penner et al. 2016; Hagiwara et al. 2017; Blair et al. 2013; Green et al. 2007; Sabin, Rivara, and Greenwald 2008; Sabin and Greenwald 2012; Daugherty et al. 2017; Colon-Emeric et al. 2017; Stepanikova 2012; Hausmann et al. 2015; Zestcott, Blair, and Stone 2016). To address the contribution of implicit bias to health disparities, calls to action continue from accreditation bodies, and professional organizations: Health professions educators are tasked to develop interventions to address implicit biases held among learners (Australian Medical Council Limited 2012; Butkus et al. 2018; Committee on Accreditation of Canadian Medical Schools 2018; Liaison Committee on Medical Education 2020).
Two approaches are generally used in implicit bias interventions (Sukhera et al. 2019). One seeks to develop interventions to “de-bias,” or, reduce/neutralize implicit bias; those utilizing this approach measure participant implicit bias, deliver an intervention, and subsequently measure the same implicit bias. For example, experiments have measured racial implicit bias in volunteers, followed by seating them in rooms with pictures of famous, beloved Black people and infamous, despised White people (Dasgupta and Greenwald 2001). After being exposed to these images, the measured implicit bias is less anti-Black (i.e. closer to neutral) (Dasgupta and Greenwald 2001). Unfortunately, two reviews focused on these “de-biasing” interventions identified several drawbacks to this approach: 1) few interventions reduce implicit bias; 2) successful interventions only have modest effects on bias reduction that are short-lived (hours to days); and most importantly, 3) even interventions resulting in a modest, short-lived effect on bias reduction still have no effect on behaviors (Forscher et al. 2019; FitzGerald et al. 2019). Additionally, these efforts are often focused on one specific type of implicit bias at a time (e.g., race, obesity, gender, etc.). Therefore, even if successful, “de-biasing” learners would be of limited utility as educators would need to design separate interventions targeting each specific implicit bias. That is, educators would need to design modules for each specific implicit bias (e.g., race, gender, body habitus). All individuals possess a myriad of implicit biases. Therefore; this approach would present another obstacle to integration into already crowded health professions curricula (Gonzalez, Garba, et al. 2018).
In the second approach, educators design instruction enabling learners to become aware of their biases and provide opportunities for discussion and reflection (Sukhera et al. 2019). The expectation is that increased awareness is a precursor to behavior modification to mitigate the influence of implicit bias in these encounters. Increasing awareness of implicit bias without concurrent skill development to address this bias in clinical encounters can have unintended consequences such as avoidance of Black persons when an individual becomes aware of implicit racial bias (Burgess et al. 2007). Further, a 2012 framework provided medical educators with a developmental model to assist individuals in developing strategies to mitigate the influence of implicit biases in their clinical encounters. Teal and colleagues suggested individuals must move beyond awareness of implicit biases to acceptance of bias in themselves, adaptation of their behaviors, and ultimately integration of these new behaviors into their daily clinical practice (Teal et al. 2012). The lead author (CMG) published evidence that increased awareness, accompanied by reflection and discussion is not enough for medical students to identify how to mitigate the influence of their implicit biases on their future clinical care: Students were accepting of implicit bias in themselves and did not want to provide biased care to their future patients, but were unable to articulate strategies beyond superficial, hopeful strategies (e.g., “strive to be the best physician I can be for my future patients”, and “it [implicit bias] is something I have to work on”) in order to provide equitable care to all patients (Gonzalez, Noah, et al. 2021).
In light of these limitations, we advocate for a third approach- implicit bias recognition and management (IBRM) (Sukhera, Watling, and Gonzalez 2020). The IBRM approach moves beyond the ineffectiveness of “de-biasing” approaches, and the shortcomings of approaches merely striving to increase awareness and essentially assuming behavior change due to the lack of opportunities for skill development and practice. IBRM instruction provides learners with the necessary opportunities for skill development and practice to recognize the influence of bias and to manage its negative effects to improve the outcomes of their encounters; initial evidence suggests this approach is effective across various types of implicit bias, thereby obviating the need to create specific instruction for each type of implicit bias (Gonzalez et al. 2020). Frameworks exist to guide the integration of IBRM instruction into health professions curricula (Teal et al. 2012; Sukhera and Watling 2018; Sukhera, Watling, and Gonzalez 2020; Gonzalez, Lypson, and Sukhera 2021). Evidence from investigations of patients’ perceptions of bias in their clinical encounters has identified targets for patient outcomes-oriented IBRM curricular interventions (Gonzalez, Deno, et al. 2018). Despite these frameworks and identified targets, we know of no published interventions in compulsory curricula within the medical literature that enable skill development to achieve IBRM in clinical encounters. Obstacles to effective implementation of IBRM curricula include lack of experience with implicit bias instruction in faculty’s previous education and training, limited curricular time, and the absence of accepted standard approaches to such instruction (Gonzalez, Garba, et al. 2018).
These obstacles and the lack of published skills-based IBRM curricula in medical education continue to challenge the development of instruction in IBRM. Without a broad, contextual understanding of the available literature, we risk remaining unaware of our blind spots and of opportunities to build on existing knowledge in IBRM. Therefore, we conducted a scoping review of implicit bias curricula across various disciplines. The rationale for choosing to broaden our search beyond the health professions education literature was twofold. First, we expanded our reach and ability to find skills-based curricula, given challenges with identifying these within the medical education literature. Second, given that implicit bias contributes to health disparities through communication behaviors and medical decision-making (Zestcott, Blair, and Stone 2016), we sought to learn from potential interventions that are focused on implicit bias but that we might find in other professions. This allows us to view techniques focused on professionals’ communication behaviors and decision-making. To achieve this, we included literature from professions related to the social determinants of health (e.g., law, education, social work, medicine, nursing, and allied health professions). In keeping with two commonly identified reasons to conduct a scoping review (Arksey and O’Malley 2005), the objectives of this scoping review are: 1) to identify and categorize implicit bias curricula thereby serving as a resource for health professions educators; and 2) to identify gaps in the literature to inform recommendations to advance innovation and research in IBRM instruction.
Methods
Arksey and O’Malley’s five stage framework provides broad guidance for conducting scoping reviews (Arksey and O’Malley 2005); opportunities to clarify and enhance the five stages have been identified (Levac, Colquhoun, and O’Brien 2010). We therefore prepared and conducted this review adhering to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) Extension for Scoping Reviews criteria (Tricco et al. 2018). These criteria provide detailed guidance inclusive of the stages suggested by Arksey and O’Malley and further expand on prior frameworks by including sources of funding for included studies. This criterion is important to disseminate as we undertake to expand and inform the current research agenda in implicit bias instruction; educators and researchers may seek to avail themselves of these funding sources in future research in IBRM.
Study question
Recognizing the dearth of skills-based IBRM curricula in the medical education literature, and aiming to inform the development of future skills-based curricula in IBRM, we conducted a scoping review seeking to answer the question: What curricular interventions exist focused on implicit bias within professions related to the social determinants of health (World Health Organization 2021): education, law, social work, and the health professions inclusive of nursing, allied health professions, and medicine? In accordance with scoping review methodology, we sought to map the broad scope of available interventions to inform future curriculum development efforts and identify gaps for future research, rather than to rate the quality of the evidence (Arksey and O’Malley 2005).
We (CMG, MLL) have experience teaching IBRM (Gonzalez, Kim, and Marantz 2014; Gonzalez, Fox, and Marantz 2015; Lypson et al. 2016; Gonzalez et al. 2020; Gonzalez, Walker, et al. 2021; Gonzalez, Nava, et al. 2021; Rodriguez et al. 2021). Additionally, our instruction has always been guided by Transformative Learning Theory (TLT) (Mezirow 1997) as both a framework and explanatory model of instruction (Sukhera, Watling, and Gonzalez 2020). We sought to identify published instruction that would inform one or more of the four major components of TLT as it relates to IBRM: 1) An experience, a “disorienting dilemma” that challenges learner assumptions; 2) Critical reflection on the meaning of that experience; 3) Guided discourse to expand on learners’ reflections; and 4) action/behavior change related to IBRM (Sukhera, Watling, and Gonzalez 2020).
Search strategy
Two authors (EK) and (CMG) began the review by conducting a preliminary search in three databases, Embase, PsycINFO, and JSTOR. An experienced medical librarian (RS) conducted a systematic search of existing, relevant literature for implicit bias and interventions across eight databases on December 17, 2016 and June 30, 2020. The search was performed in the following databases: PubMed (via ncbi.nlm.nih.gov), Embase (via embase.com including MEDLINE), CINAHL (via EBSCOhost), ERIC (via OVID), JSTOR Archive Collection (via jstor.org), Lexis-Nexis Academic (via Lexis-Nexis), PsycINFO (via American Psychological Association/PsycNET) and Web of Science Core Collection (via webofknowledge.com). A combination of multiple synonyms, controlled vocabulary search terms (MeSH terms in PubMed and Emtree in Embase) and exhaustive text words in title and/or abstract was used to search the databases for articles added by the publisher. We hand searched reference sections of selected articles. We additionally searched MedEdPORTAL, an online repository of health professions curricula (www.mededportal.org). Implicit bias as it relates to health disparities has become more frequently studied in recent years (e.g. there are no articles in PubMed prior to the year 2000). All searches included articles from January 1, 2000 to the day of the search. The complete search strategy is available in Appendix 1.
Study selection
We included studies meeting the following criteria: 1) described and/or evaluated an educational intervention related to implicit bias, in professional fields related to many of the social determinants of health; and 2) addressed learner outcomes such as knowledge, attitudes, and/or skills. Due to the numerous aforementioned drawbacks, we excluded interventions seeking to reduce/neutralize implicit bias as the only outcome. Conference abstracts, dissertations, and non-English articles were excluded. Each reference retrieved through the search process was reviewed independently by at least two investigators (CMG, CMO, SAW, EK). In keeping with the subjectivist nature of scoping reviews (Thomas et al. 2020), if at least one investigator thought there was sufficient evidence in the abstract for full-text review, or if the reference did not have an available abstract, it was selected for full-text review. Articles chosen for full text review were reviewed independently and in duplicate by the team. Disagreements on inclusion for data charting were resolved by discussion and consensus. Interrater reliability calculated by Cohen’s Kappa showed excellent agreement (κ=0.95) for the initial search, likely reflecting that we asked a “what” question, rather than a “how” question, which would be subject to more interpretation (Thomas et al. 2020). The same procedures were followed for the subsequent search.
The process for identifying and selecting studies for inclusion in the review is depicted in Figure 1. Of the 2431 potentially relevant articles published from January 1, 2000 through June 30, 2020, using the inclusion and exclusion criteria and screening for duplicates, reviewers removed 2113 articles during the abstract review phase. A resultant 318 available full text articles were assessed for eligibility for inclusion in the review analysis. After further review, a total of 267 full text articles did not fulfill inclusion criteria leaving 51 full text articles for data charting.
Figure 1.
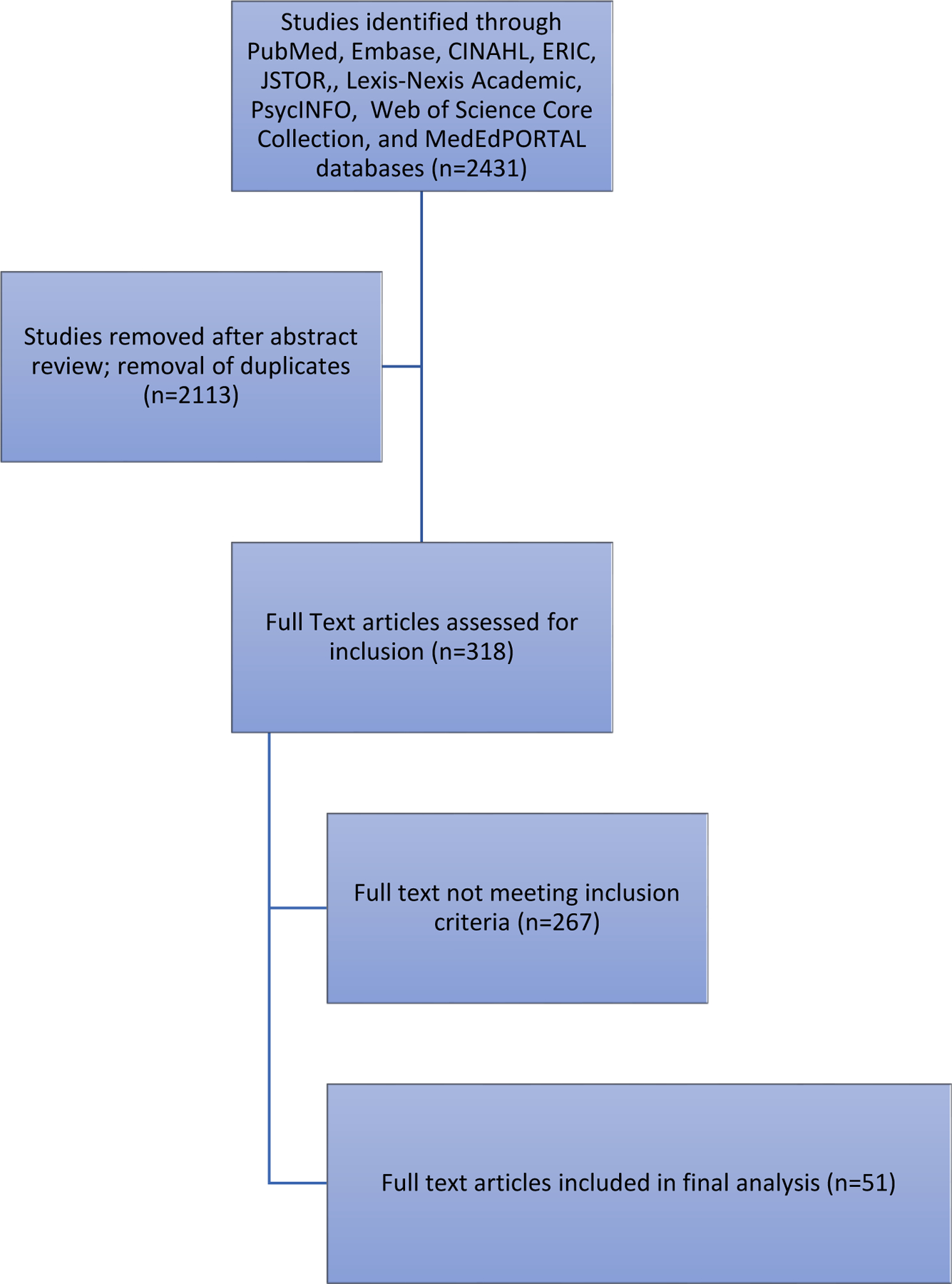
Identification and selection process for articles describing interventions related to implicit bias recognition and management during scoping review across fields related to the determination of health and published from 2000–2020.
Data charting
We utilized a constructivist epistemological stance throughout our data charting, in order to broadly consider inclusion of components of instruction in the skills required for successful IBRM in physician communication and medical decision-making and to synthesize the data in keeping with our stated goals. A data charting form was developed, piloted, and revised in an iterative process. Data were charted independently and in duplicate by at least two investigators for every full text article. We charted number of learners, population of professionals, stage of career experience, study design, type of bias addressed, educational strategies within the intervention, target outcomes, and duration of outcomes (Tricco et al. 2018). We refer to all participants as learners when describing the interventions, regardless of profession or career stage due to their engagement in skill development. The lived experiences and expertise of curriculum developers and educators may impact curricular content, facilitation of learning, and research, however, for two reasons, we did not chart data on who was delivering the curricula and/or conducting the research. First, we found that details regarding facilitators’/researchers’ identities were not readily available due to the absence of reflexivity statements within included articles. Second, issues of equity, inclusivity, accessibility, and representation matter greatly, are not specific or more relevant to implicit bias instruction, and are relevant to all areas of scholarship (Rakhra et al. 2021; Chaiyachati et al. 2022).
Synthesis of results
CMG and MLL are general internists and educators who have collaborated on qualitative research following constructivist grounded theory, CMO (also a general internist and educator), EK, and SAW (both medical students at the time) joined CMG’s research team and, although they brought their unique lenses based on their lived experiences, they were trained to conduct the scoping review through the lens adopted by the first and senior authors. RS, a medical librarian, searched relevant databases with search terms derived from that same lens. The epistemological underpinnings of our approach are that implicit bias instruction should follow the skills-based behaviorally-oriented IBRM approach, and that the ultimate goal of IBRM instruction should be to improve patient outcomes as we strive to achieve health equity. Based on that approach, we analyzed studies and synthesized articles along comparisons of educational strategies and assessments. We compared educational strategies, methods employed to achieve the goals or learning objectives (Thomas et al. 2016), in order to identify similar approaches. Similar articles were then grouped together within broader themes aligned with our TLT-informed IBRM approach to instruction. We compared types of assessments, when available in an article, and grouped similar articles.
Results
Table 1 describes characteristics of the individual interventions. Disciplines with published interventions included medicine (N=33), nursing (N=13), pharmacy (N=3), undergraduate education (N=3), law (N=4), post-secondary faculty and administrators (N=3), health professions administrators (N=2), dentistry (N=1), other allied health professions (N=1), and state workers from miscellaneous professions (N=1). In Table 2 articles are categorized by study design, types of learners, types of bias addressed, and number of sessions. Most were single-group studies (N=43), interventions spanned professional disciplines, some targeting more than one discipline; participants included learners across the spectrum of training and practice within their respective professions. The majority of studies focused on a single bias, most commonly implicit bias related to race and/or ethnicity. Sexual orientation, gender, culture/religion, bias from patients toward clinicians, age, weight, socioeconomic status/class, incarceration status, disability, mental illness, and veteran status were other biases addressed. Of the 51 interventions, most (N=32) were stand-alone sessions, however N=14 included more than one session. Other interventions consisted of a series of seven (N=2), eight (N=1), or fourteen (N=1) sessions. Another (N=1) included an implicit bias exercise within ongoing clinical documentation. Educational strategies and assessments varied widely and are discussed further below.
Table 1.
Details of interventions included in scoping review of implicit bias interventions across multiple professional disciplines related to the social determinants of health (2000–2020).
| Reference # | Citation | Study Design | Target population | Bias | Target Outcome | Summary of educational components |
|---|---|---|---|---|---|---|
| 1 | Avant ND, Gillespie GL. Pushing for health equity through structural competency and implicit bias education: A qualitative evaluation of a racial/ethnic health disparities elective course for pharmacy learners. Currents in Pharmacy Teaching and Learning. 2019. | Qualitative inquiry | Pharmacy students | Race/ethnicity | Knowledge and attitudes | Facilitated discussion, social-identity mapping, photo presentations. |
| 2 | Bordt RL. Only some are dead men walking: Teaching about race discrimination and the death penalty. Teach Sociol. 2004;32(4):358–373. | Single group– no outcomes measured | Undergraduate students (criminology and contemporary society courses) | Race | N/A | Description of hypothetical court case, analysis of different conclusions based on race, IAT, and facilitated discussions. |
| 3 | Brockett M. Training teaches Annapolis police about implicit bias. In:2016:STATE AND REGIONAL NEWS. | Single group- no outcomes measured | Community leaders (focused on law) | Race | N/A | Didactics, strategy identification, case-based discussions. |
| 4 | Brooks KC, Rougas S, George P. When race matters on the wards: talking about racial health disparities and racism in the clinical setting. MedEdPORTAL. 2016;12:10523. | Single group- no outcomes measured | Medical students | Race | N/A | Direct readings and case-based discussions. |
| 5 | Cahn PS. Recognizing and Reckoning With Unconscious Bias: A Workshop for Health Professions Faculty Search Committees. MedEdPORTAL. 2017;13:10544. | Single group- no outcomes measured | Department chairs, search committee chairs, search committee members, administrators. | Race | N/A | Didactics, viewing images as prompts for discussion, applications of concepts to crafting an announcement for new position. |
| 6 | Capers Q, Clinchot D, McDougle L, Greenwald AG. Implicit Racial Bias in Medical School Admissions. Academic medicine : journal of the Association of American Medical Colleges. 2017;92(3):365–369. | Post-training survey | Medical students, faculty | Race | Knowledge, attitudes and behaviors – measure of impact during following admission cycle. | Pre-session IAT. Facilitated discussion on strategies to mitigate implicit bias. |
| 7 | Carnes M, Devine PG, Isaac C, et al. Promoting Institutional Change Through Bias Literacy. J Divers High Educ. 2012;5(2):63–77. | Post-workshop evaluation and qualitative interviews | STEMM* faculty and administrators | Gender | Self-reported knowledge, attitude, skills, and intention to change. | IAT, didactics, case-based discussion, strategy identification. |
| 8 | Chapman MV, Hall WJ, Lee K, et al. Making a difference in medical trainees’ attitudes toward Latino patients: A pilot study of an intervention to modify implicit and explicit attitudes. Social science & medicine (1982). 2018;199:202–208. | Sequential cohort, posttest design with comparison group | Pediatric and medicine Residents | Ethnicity | Attitudes | Narrative photography and facilitated discussion. |
| 9 | Clementz L, McNamara M, Burt NM, Sparks M, Singh MK. Starting With Lucy: Focusing on Human Similarities Rather Than Differences to Address Health Care Disparities. Academic medicine: journal of the Association of American Medical Colleges. 2017;92(9):1259–1263. | Post-training survey | Medicine residents, nurse practitioner residents and students, and health psychology residents. | Culture, race, gender | Knowledge and attitude | Museum tour, didactics, facilitated discussions, and case-based discussions. |
| 10 | Even-Zohar A, Werner S. The Effect of Educational Interventions on Willingness to Work with Older Adults: A Comparison of Students of Social Work and Health Professions. Journal of Gerontological Social Work. 2020;63(1–2):114–132. | Pre/post-test with comparison group | First-year social work, nursing, speech therapy and physiotherapy students | Age | Self-reported: knowledge, attitudes, and behaviors toward older adults, and willingness to work with older adults | Observations of a simulations and a video. |
| 11 | Fix RL. Justice Is Not Blind: A Preliminary Evaluation of an Implicit Bias Training for Justice Professionals. Race and Social Problems. 2020;12:362–374. | Pre/post-test | Criminal justice professionals: pretrial court, police department and specialty court, healthcare, business, retail, and educational system. | Race | Knowledge and empathy | Didactics, facilitated discussions and case-based discussions, IAT, video observation and debrief. |
| 12 | Gandhi M, Johnson M. Creating more effective mentors: Mentoring the mentor. AIDS and Behavior. 2016;20(Suppl 2):294–303. | Pre/post questionnaires | Mid-level (advanced Asst. Prof. and Assoc. Prof.) and Senior (Full Prof.) HIV researchers. | Race | Enhance mentoring capabilities of diverse mentees | 2 day “Mentoring the Mentors” Workshop - included sessions on unconscious bias, microaggressions, and diversity supplements. |
| 13 | Gatewood E, Broholm C, Herman J, Yingling C. Making the invisible visible: Implementing an implicit bias activity in nursing education. Journal of Professional Nursing. 2019;35:447–451. | Post-test | BSN-DNP nursing students | Race | Self-reported awareness of bias, identification of strategies, and ability to manage implicit bias | Didactics, directed readings, IAT, reflection with facilitated discussion, strategy identification. |
| 14 | Geller G, Watkins PA. Addressing Medical Students’ Negative Bias Toward Patients with Obesity Through Ethics Education. AMA J Ethics. 2018;20(10):E948–959. | Pre/post questionnaires | Medical students | Weight | Attitudes | IAT, facilitated discussion on weight, shared personal experiences, and ethics discussions. |
| 15 | Ghoshal RA, Lippard C, Ribas V, Muir K. Beyond Bigotry: Teaching about Unconscious Prejudice. Teach Sociol. 2013;41(2):130–143. | Pre/post questionnaires | Undergraduate students | Race | Views on seriousness of unconscious prejudice/acknowledgement of personal prejudice. | Didactics, facilitated discussions, IAT. |
| 16 | Goldenberg MN, Cyrus KD, Wilkins KM. ERASE: A New Framework for Faculty to Manage Patient Mistreatment of Trainees. Academic Psychiatry. 2019;43:396–399. | Pre/post-test | Residents and practicing Physicians | Bias from patients towards providers | Perceived self-efficacy and attitude around trainee mistreatment. | Didactics, guided discussion about challenges and barriers to addressing patient bias, applied a framework to a case and identified strategies to address the bias. |
| 17 | Gonzalez CM, Fox AD, Marantz PR. The Evolution of an Elective in Health Disparities and Advocacy: Description of Instructional Strategies and Program Evaluation. Acad Med. 2015;90(12):1636–1640. | Pre/post questionnaires | Medical students | Race | Knowledge and attitudes | Elective including didactics, role-play, IAT and debrief, discussion and reflection. |
| 18 | Gonzalez CM, Kim MY, Marantz PR. Implicit bias and its relation to health disparities: a teaching program and survey of medical students. Teach Learn Med. 2014;26(1):64–71. | Post-training survey | Medical students | Age, race/ethnicity, sex, sexual orientation, religion | Explore attitudes towards implicit bias; increase awareness and understanding of health care disparities. | Directed readings, IAT, and reflective narrative assignment. Facilitated discussion during session. |
| 19 | Harrison-Bernard LM, Augustus-Wallace AC, Souza-Smith FM, Tsien F, Casey GP, Gunaldo TP. Knowledge gains in a professional development workshop on diversity, equity, inclusion, and implicit bias in academia. Adv Physiol Educ. 2020;44:286–294. | Pre/post-test | University faculty administrators and staff who interact with students | Race, sexual orientation, socioeconomic status | Knowledge | Didactics, video observation with debrief, active-learning of matching of vocabulary words with group discussion, reflection and facilitated discussions. |
| 20 | Hofmeister S, Soprych A. Teaching resident physicians the power of implicit bias and how it impacts patient care utilizing patients who have experienced incarceration as a model. Int J Psychiatry Med. 2017;52(4–6):345–354. | Single group- no outcomes measured | Faculty teaching medical residents | Incarceration, race | N/A | Exercises addressing assumptions, expectations, bias, and worldview, self-reflections, strategy identification |
| 21 | Hunsinger M, Christopher M, Schmidt AM. Mindfulness Training, Implicit Bias, and Force Response Decision-Making. Mindfulness. 2019;10:2555–2566. | Randomized controlled trial | Professional law enforcement officers | Race | Shooter bias task, self-efficacy for change, mindfulness questionnaire. | Didactics, mindfulness practice, facilitated discussion. Application of material learned to professional contexts. |
| 22 | Johnson R, Richard-Eaglin A. Combining SOAP Notes with Guided Reflection to Address Implicit Bias in Health Care. Journal of Nursing Education. 2020;59(1):59. | Post-test | DNP students | Not specified | Attitudes in reflections | IAT, written reflections, faculty gave feedback and suggested strategies. |
| 23 | Kanter et al. Addressing microaggressions in racially charged patient-provider interactions: a pilot randomized trial. BMC Medical Education. 2020;20:88 | Randomized controlled trial | Medical students and residents | Race | Learner attitudes and observer ratings of standardized patient interactions with a specifically incorporated racial challenge. | Didactics, eye-contact mindfulness exercise, personal narrative exercises, and role-play. |
| 24 | Klein EW, Nakhai M. Caring for LGBTQ patients: Methods for improving physician cultural competence. International Journal of Psychiatry in Medicine. 2016;51(4):315–324. | Single group- no outcomes measured | Family medicine residents | Sexual orientation | N/A | Bias awareness through group word-cloud for LGBTQ; education on non-judgmental, open history taking and therapeutic relationship building; discussion of LGBTQ disparities. |
| 25 | Kokas M, Fakhoury JW, Hoffert M, Whitehouse S, Van Harn M, Baker-Genaw K. Health Care Disparities: a Practical Approach to Teach Residents about Self-Bias and Patient Communication. Journal of Racial and Ethnic Health Disparities. 2019;6:1030–1034. | Pre/post-test | Medical residents | Race | Survey for consideration of race in clinical care | Didactics, self-questioning, think-pair-share worksheet exercise, video observation and debrief, practice asking open-ended questions. |
| 26 | Lypson ML, Ross PT, Zimmerman N, Goldrath KE, Ravindranath D. Where Do Soldiers Really Come From? A Faculty Development Workshop on Veteran-Centered Care. Acad Med. 2016;91(10):1379–1383. | Post-workshop survey | Healthcare professionals | Veteran status | Knowledge, attitude, skill. | Multipronged workshop using images, critical thinking and reflective writing. |
| 27 | Marion GS, Hairston JM, Davis SW, Kirk JK. Using Standardized Patient Assessments to Evaluate a Health Literacy Curriculum. Family Medicine. 2018;50(1):52–57. | Pre/post rated standardized patient exercises | Medical students | Age | Skills | Health literacy assessment curriculum, including: IAT, debriefing and two videos depicting implicit bias. |
| 28 | Mayfield JJ, Ball EM, Tillery KA, et al. Beyond Men, Women, or Both: A Comprehensive, LGBTQ-Inclusive, Implicit-Bias-Aware, Standardized-Patient-Based Sexual History Taking Curriculum. MedEdPORTAL. 2017;13:10634. | Pre/post questionnaires | Medical students | Sexual orientation | Knowledge and comfort | Pre-session videos and reading on sexual history taking and sexuality IAT; lecture and small group standardized patient cases. |
| 29 | McElfish PA, Long CR, Rowland B, Moore S, Wilmoth R, Ayers B. Improving Culturally Appropriate Care Using a Community-Based Participatory Research Approach: Evaluation of a Multicomponent Cultural Competency Training Program, Arkansas, 2015–2016. Preventing chronic disease. 2017;14:E62. | Post-training survey | Healthcare professionals and administrators, office personnel | Culture | Knowledge, skills/competence, behavior, attitudes | Multiple-module cultural competency training. |
| 30 | McMichael B, Nickel A, Duffy EA, Skjefte L, Lee L, Park P, Nelson SC, Puumala S, Kharbanda AB. The Impact of Health Equity Coaching on Patient’s Perceptions of Cultural Competency and Communication in a Pediatric Emergency Department: An Intervention Design. Journal of Patient Experience. 2019;6(4):257–264. | Post-test | Medical and nursing practicing professionals | Race | Self-reported comfort | Didactics service learning, guided reflection, and presentations to peers. |
| 31 | Medlock M, Weissman A, Wong S, et al. Racism as a unique social determinant of mental health: development of a didactic curriculum for psychiatry residents. MedEdPORTAL. 2017;13:10618. | Single group-no outcomes measured | Residents | Race | N/A | Directed readings and didactic session |
| 32 | Motzkus C, Wells RJ, Wang X, Chimienti S, Plummer D, Sabin J, et al. (2019) Pre-clinical medical student reflections on implicit bias: Implications for learning and teaching. PLoS ONE 14(11): e0225058. | Post-test | Medical students | Not specified | Attitudes in reflections | IAT and written reflections |
| 33 | O’Connor MR, Barrington WE, Buchanan DT, Bustillos D, Eagen-Torkko M, Kalkbrenner A, Laing SS, Reding KW, de Castro AB. Short-Term Outcomes of a Diversity, Equity, and Inclusion Institute for Nursing Faculty. Journal of Nursing Education. 2019;58(11):633–640. | Pre/post-test | Nursing faculty/administrators | Race | Self-efficacy in teaching diversity, equity and inclusion. | Provocative triggers to read aloud instances of discrimination, strategy identification, self-reflection and debrief, role-playing, application of material to professional setting. |
| 34 | Osman NY, Gottlieb B. Mentoring across differences. MedEdPORTAL. 2018;14:10743 | Single group- no outcomes measured | Mentors- faculty, deans, chiefs, chairs, etc. in medicine, nursing, and pharmacy | Race, gender | N/A | Directed readings, didactics, case-based, experiential group discussions |
| 35 | Perdomo J, Tolliver D, Hsu H, et al. Health Equity Rounds: and interdisciplinary case conference to address implicit bias and structural racism for faculty and trainees. MedEdPORTAL. 2019;15:10858. | Single group- no outcomes measured | Students, residents, physicians | Race | N/A | Case presentation (sometimes including patients and their families), discussion, guided reflections, perspective taking, reflective writing, integration of quality improvement tools, think-pair-share. |
| 36 | Poitevien P, Osman C. Tackling Implicit and Explicit Bias Through Objective Structured Teaching Exercises for Faculty. Journal of graduate medical education. 2018;10(3):353–354. | Pre/post questionnaires | Faculty teaching residents | Religion (bias from patients toward providers) and immigration status | Skills | Simulation for managing explicit bias against residents and implicit bias in patient care. |
| 37 | Rizk N, Jones S, Shaw MH, Morgan A. Using forum theater as a teaching tool to combat patient bias directed toward health care professionals. MedEdPORTAL. 2020;16:11022. | Post-test | Residents and practicing medical, nursing, social work and staff professionals | Bias from patients towards providers | Self-reported satisfaction (for grand rounds) and knowledge (for workshops) | Didactics, observation of behaviors in videos, role-play, strategy identification and practice, writing of cases for use in forum theater. |
| 38 | Russell J, Summers A. Reflective decision-making and foster care placements. Psychology, Public Policy, and Law. 2013;19(2):127–136. | Randomized controlled trial and quasi-experimental designs | Judges | Race | Knowledge and skill | Reflection and decision-making deliberation, bench card to guide judicial practice/decision making. |
| 39 | Sandoval RS, Afolabi T, Said J, Dunleavy S, Chatterjee A, Ölveczky D. Building a tool kit for medical and dental students: addressing microaggressions and discrimination on the wards. MedEdPORTAL. 2020;16:10893. | Pre/post-test | Medical and dentistry students | Bias from patients towards providers | Knowledge of microaggressions, perception of barriers to addressing microaggressions. | Didactic, case-based discussion and strategy identification. |
| 40 | Schultz PL, Baker J. Teaching Strategies to Increase Nursing Student Acceptance and Management of Unconscious Bias. J Nurs Educ. 2017;56(11):692–696. | Pre/post questionnaires | Graduate nursing students | Race | Knowledge, attitudes, self-efficacy | IAT, debriefing, strategy identification, perspective-taking, written reflections. |
| 41 | Sherman MD, Ricco JA, Nelson SC, Nezhad SJ, Prasad S. Implicit Bias Training in a Residency Program: Aiming for Enduring Effects. Fam Med. 2019;51(8):677–681. | Single group- no outcomes measured | Residents and practicing physicians | Race | N/A | Didactics, group discussion and reflection |
| 42 | Shields SA, Zawadzki MJ, Johnson RN. The impact of the Workshop Activity for Gender Equity Simulation in the Academy (WAGES–Academic) in demonstrating cumulative effects of gender bias. Journal of Diversity in Higher Education. 2011;4(2):120–129. | Randomized controlled trial | Postsecondary academic administrators and faculty. | Gender | Knowledge | Game-like simulation to condense career advancements for 2 academics (2 teams) with different experiences followed by group discussion. |
| 43 | Song AY, Baylor College of Medicine Committee on the Social Determinants of Health, Poythress EL, Bocchini CE, Kass JS. Reorienting orientation: introducing the social determinants of health to first-year medical students. MedEdPORTAL. 2018;14:10752. | Pre/post test | Medical Students | Race/ethnicity, sexual orientation, socioeconomic status, gender | No outcomes reported related to implicit bias | Privilege walk, reflections, facilitated discussion, and case-based discussions. |
| 44 | Sukhera J, Miller K, Scerbo C, Milne A, Lim R, Watling C. Implicit Stigma Recognition and Management for Health Professionals. Acad Psychiatry. 2020;44:59–63. | Pre/post-test | Medical and nursing practicing professionals | Mental illness | Attitudes | Didactics, group discussion, role-play, case-based discussion, and sorting exercise highlighting demonstrations of implicit bias. Privilege walk exercise followed by think-pair-share. |
| 45 | Teal CR, Shada RE, Gill AC, et al. When best intentions aren’t enough: helping medical students develop strategies for managing bias about patients. J Gen Intern Med. 2010;25 Suppl 2:S115–118. | Pre/post questionnaires | Medical students | Disabilities and second bias of student’s choice | Knowledge and skill | IAT and facilitated peer group discussions about IAT tests and clinical experiences re: bias. |
| 46 | Teall AM, Graham M, Jenkins N, Ali A, Pryba J, Overcash J. Faculty Perceptions of Engaging Students in Active Learning to Address Implicit Bias Using Videos Exemplifying the Prenatal Visit of a Lesbian Couple. J Transcult Nurs. 2019:1043659619828109. | Post-training survey | Nursing faculty | Sexual orientation | N/A | Video observation and guided debrief. |
| 47 | White AA, Logghe HJ, Goodenough DA, et al. Self-Awareness and Cultural Identity as an Effort to Reduce Bias in Medicine. Journal of racial and ethnic health disparities. 2018;5(1):34–49. | Single group- no outcomes studied | Medical students | Ethnicity | N/A | Fourteen-session course on culture, self-reflection, and medicine. |
| 48 | Wijayatunga NN, Kim Y, Butsch WS, Dhurandhar EJ. The effects of a teaching intervention on weight bias among kinesiology undergraduate students. Int J Obes (Lond). 2019. | Randomized controlled trial | Undergraduate kinesiology students | Weight | No outcomes related to implicit weight bias | Didactics and facilitated discussion. |
| 49 | Wu D, Saint-Hilaire L, Pineda A, et al. The Efficacy of an Antioppression Curriculum for Health Professionals. Family medicine. 2019;51(1):22–30. | Pre/post questionnaires | Medical and nursing students, residents, and faculty | Race | Knowledge, attitudes | Three-part workshop including unconscious bias education, ally-ship education and skills practice. |
| 50 | Zeidan A, Tiballi A, Woodward M, et al. Targeting Implicit Bias in Medicine: Lessons from Art and Archaeology. Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health. 2019;21(1):1–3. | Pre/post-test | Medical Students and Residents | Not specified | Self-reported attitudes about implicit bias and self-reported feeling more empowered to address their biases | Didactics, deep description exercise about artifact at museum, reflective discussion to tie the exercise back to the clinical environment. |
| 51 | Zeidan AJ, Khatri UG, Aysola J, et al. Implicit Bias Education and Emergency Medicine Training: Step One? Awareness. AEM Educ Train. 2019;3(1):81–85. | Post-training survey | Emergency medicine faculty and residents | Race | Knowledge and confidence | IAT and facilitated discussion |
Table 2.
Interventions included in scoping review of implicit bias interventions across multiple professional disciplines related to the social determinants of health categorized by study design, learner level, bias addressed, and number of sessions within intervention (2000–2020).
| Study Design | Number of studies (%) N=51 | Study Number* |
|---|---|---|
| Single group or cross-sectional or post-test | 25 (49%) | 1, 2, 3, 4, 5, 6, 7, 9, 13, 18, 20, 22, 24, 26, 29, 30, 31, 32, 34, 35, 37, 41, 46, 47, 51 |
| Pre-test/post-test single group | 18 (35%) | 11, 14, 15, 16, 17, 19, 25, 27, 28, 33, 36, 39, 40, 43, 44, 45, 49, 50 |
| Pre-test/post-test two groups | 3 (6%) | 8**, 10, 12 |
| Randomized controlled | 5 (10%) | 21, 23, 38, 42, 48 |
| Learners (may target more than one group of learners therefore no % included) | ||
| Medical students | 16 | 4, 6, 14, 17, 18, 23, 27, 28, 32, 35, 39, 43, 45, 47, 49, 50 |
| Other health professions students/trainees | 8 | 1, 9, 10, 13, 22, 39, 40, 49 |
| Practicing healthcare professionals | 18 | 6, 7, 12, 16, 20, 26, 29, 30, 33, 34, 35, 36, 37, 41, 44, 46, 49, 51 |
| Medical residents | 13 | 8, 9, 16, 23, 24, 25, 31, 35, 37, 41, 49, 50, 51 |
| Leadership/administration | 7 | 5, 7, 19, 29, 33, 34, 42 |
| Undergraduate students | 3 | 2, 15, 48 |
| Law professionals | 4 | 3, 11, 21, 38 |
| Miscellaneous professionals | 1 | 11 |
| Types of bias addressed (may address more than one therefore no % reported) | ||
| Race or ethnicity | 31 | 1, 2, 3, 4, 5, 6, 8, 9, 11, 12, 13, 15, 17, 18, 19, 20, 21, 23, 25, 30, 31, 33, 34, 35, 38, 40, 41, 43, 47, 49, 51 |
| Sexual orientation | 6 | 18, 19, 24, 28, 43, 46 |
| Gender | 5 | 7, 9, 34, 42, 43 |
| Culture/religion | 4 | 9, 18, 29, 36 |
| Bias from patients toward providers | 4 | 16, 36, 37, 39 |
| Age | 3 | 10, 18, 27 |
| Weight | 2 | 14, 48 |
| Socioeconomic status/class | 2 | 19, 43 |
| Incarceration status | 1 | 20 |
| Disability | 1 | 45 |
| Mental illness | 1 | 44 |
| Veteran status | 1 | 26 |
| Immigration status | 1 | 36 |
| Not specified or learner choice | 4 | 22, 32, 45, 50 |
| Number of Sessions | ||
| Stand-alone/single | 32 (63%) | 3, 4, 5, 6, 7, 8, 9, 11, 13, 14, 16, 18, 19, 20, 23, 24, 25, 26, 27, 30, 32, 36, 38, 39, 40, 42, 44, 45, 46, 48, 50, 51 |
| More than one session | 14 (27%) | 1, 2, 10, 12, 15, 17, 28, 29, 31, 33, 34, 41, 43, 49 |
| Seven sessions | 2 (4%) | 35, 37 |
| Eight sessions | 1 (2%) | 21 |
| Fourteen sessions | 1 (2%) | 47 |
| Ongoing | 1 (2%) | 22 |
Study numbers refer to numerical order listed in Table 1.
Post-test only
Data synthesis: Educational strategies
Educators reported a wide array of educational strategies. Implicit bias instruction is potentially emotionally charged (Gonzalez et al. 2019; Sukhera et al. 2018); N=4 were intentional in efforts to de-stigmatize implicit bias to further engage learners in instruction. This was accomplished through several methods: 1) timing implicit bias instruction within a larger course after rapport has been established among students and with the instructor, demonstrating that implicit bias is related to the context in which individuals are socialized, and having instructors share their own Implicit Association Test (IAT- described further below) results (Ghoshal et al. 2013); 2) introducing implicit bias as a concept earlier in instruction to allow for increased comfort with the topic before any skill-building exercises began, and adding nonclinical scenarios to demonstrate the ubiquitous nature of implicit bias (Gonzalez, Fox, and Marantz 2015); 3) using a nonjudgmental, compassionate tone and creating a brave space (Wu et al. 2019); and 4) being explicit about the safety of the learning environment and that discomfort can be expected when discussing implicit bias (Kokas et al. 2019). Didactic components of N=8 studies focused on delivery of background information on implicit bias, its potential influence on interpersonal encounters, and bias reduction strategies, among others (Gandhi and Johnson 2016; Carnes et al. 2012; Capers et al. 2017; McElfish et al. 2017; Schultz and Baker 2017; Harrison-Bernard et al. 2020; McMichael et al. 2019; Sherman et al. 2019). Based on our analysis of the reported interventions, the most commonly used educational strategies that moved beyond engaging learners and delivering didactics included: 1) creating experiences to serve as provocative/engagement triggers; 2) the use of Implicit Association Test (IAT) (Project Implicit 2011); 3) reflection and discussion; and 4) miscellaneous active learning strategies. Active learning refers to a range of instructional strategies that engage learners as active participants in their learning where students “do” and think about what they are doing (Thomas et al. 2016). The IAT is a publicly available online response latency test. It pairs value-laden words and images (Greenwald, McGhee, and Schwartz 1998). The difference in speed of pairing images and words (e.g. pictures of Black people and “good” words compared to pictures of White people and “bad” words followed by the opposite pairings) is considered representative of implicit bias. It was frequently used as a provocative/engagement trigger (Teal et al. 2010; Ross et al. 2011), therefore we describe it as a distinct educational strategy.
Provocative/Engagement triggers
Provocative/Engagement triggers are a mechanism to capture learners’ attention and root them in the content of the session (Ross et al. 2011). They enable learners to become aware of biases about which they may not have been previously aware (Ross et al. 2011; Ring J 2008). One method used in N=3 studies provided two or more versions of a written case or other exercise to learners (Mayfield et al. 2017; Bordt 2004; Shields, Zawadzki, and Johnson 2011). Cases or exercises were identical to each other, except for a characteristic about the person(s) involved (e.g. race). Learners were required to make independent decisions individually or in small groups (using the same version of the case/exercise). Facilitators then debrief with learners on the effect of the single variation (e.g. race) in the case and how that impacted decision-making. Learners have the opportunity to identify their biases and reflect on the impact of those biases on decision-making. These three interventions included a facilitated discussion for reflection and debriefing. The types of cases and biases explored included: 1) Criminal justice and race (Bordt 2004); 2) Academic career trajectory and gender identity (Shields, Zawadzki, and Johnson 2011); and 3) Standardized patients presenting varied sexual orientations (Mayfield et al. 2017).
Other provocative/engagement triggers (N=5) were “thought exercises.” In one setting, a class was conducted for community leaders that replicated training undertaken by local police officers. Learners were presented with a blurry photograph and were asked their initial impressions of the image. This was then followed by a “reveal” and a facilitated reflective discussion of the actual image (Brockett 2016). Another approach generated word clouds in response to family medicine residents brainstorming of their first thoughts when hearing the words lesbian, gay, bisexual, transgender and queer (Klein and Nakhai 2016). Pediatric residents voiced opinions and heard the perspectives of fellow residents during a photo documentary about Latino patients (Chapman et al. 2018), while photograph elicitation was used to explore medical faculty biases towards veterans (Lypson et al. 2016). Finally, learners were asked to rank pictures of individuals by warmth and competence; subsequent discussion highlighted the implicit bias involved (Sukhera et al. 2020).
The biases of faculty in post-graduate medical education when teaching residents about patients experiencing incarceration were highlighted by two types of provocative/engagement triggers. Learners participated in a categorization exercise (N=1) and reflected on assumptions made about facilitators’ experiences with incarceration (Hofmeister and Soprych 2017). Completing a “deep description” (N=1) of an artifact in a museum similarly highlighted for learners the assumptions made when filling in pieces of a story; subsequent discussion drew parallels to the clinical environment (Zeidan, Tiballi, et al. 2019). Anonymized student narratives of experiences with discrimination prepared faculty learners for activities on facilitating conversations on racism (N=1) (O’Connor et al. 2019). Privilege walks (N=2), exercises in which learners step forward in response to various prompts (e.g. one of my parents graduated college) that acknowledge not everyone is starting from the same place in life, were another provocative trigger utilized to highlight assumptions and biases for learners that they may not have been aware of (Sukhera et al. 2020; Song et al. 2018).
Overall, interventions using provocative/engagement triggers raise awareness of bias, with most incorporating discussions with learners about this newly raised awareness. No interventions included further strategy identification or skill development and practice, and therefore moved learners little beyond awareness.
Implicit Association Test
The IAT was a component of N=18 studies. It was most often used as a specific type of provocative/engagement trigger to raise awareness about bias. In N=15 instances, learners took the IAT prior to instruction (Teal et al. 2010; Gonzalez, Kim, and Marantz 2014; Gandhi and Johnson 2016; Carnes et al. 2012; Capers et al. 2017; Geller and Watkins 2018; Marion et al. 2018; Mayfield et al. 2017; Wu et al. 2019; Zeidan, Khatri, et al. 2019; Schultz and Baker 2017; Medlock et al. 2017; Motzkus et al. 2019; Johnson and Richard-Eaglin 2020; Fix 2020). The other N=3 interventions that used the IAT provided some instruction and context prior to having learners take the test (Gonzalez, Fox, and Marantz 2015; Ghoshal et al. 2013; Gatewood et al. 2019). IATs chosen focused on gender (N=1) (Carnes et al. 2012), race/ethnicity (N=6) (Capers et al. 2017; Zeidan, Khatri, et al. 2019; Ghoshal et al. 2013; Medlock et al. 2017; Fix 2020; Gatewood et al. 2019), sexuality (N=1) (Mayfield et al. 2017), and weight (N=1) (Geller and Watkins 2018). The remaining interventions (N=5) instructed the learners to take any IAT (Teal et al. 2010; Gonzalez, Kim, and Marantz 2014; Marion et al. 2018; Schultz and Baker 2017; Motzkus et al. 2019); or did not specify which IAT(s) learners completed (N=4) (Gonzalez, Fox, and Marantz 2015; Gandhi and Johnson 2016; Wu et al. 2019; Johnson and Richard-Eaglin 2020). N=16 interventions allowed time for learners to debrief their experience of taking the IAT and their reaction to their results; in these instances, the IAT was a tool used to raise awareness of implicit bias in learners and facilitate further discussion (Teal et al. 2010; Gonzalez, Fox, and Marantz 2015; Gonzalez, Kim, and Marantz 2014; Gandhi and Johnson 2016; Carnes et al. 2012; Capers et al. 2017; Geller and Watkins 2018; Marion et al. 2018; Wu et al. 2019; Zeidan, Khatri, et al. 2019; Schultz and Baker 2017; Ghoshal et al. 2013; Medlock et al. 2017; Motzkus et al. 2019; Johnson and Richard-Eaglin 2020; Gatewood et al. 2019). N=1 intervention did not report a debrief, and instead instructed learners to keep their IAT “results in mind” when interviewing a standardized patient (Mayfield et al. 2017); another (N=1) did not further specify its use (Fix 2020).
Reflection and discussion
Once learners were aware of implicit bias, many interventions incorporated facilitated reflection exercises. Learners often reflected on assumptions they made in response to the provocative/engagement triggers and on the process of taking the IAT, their results, and/or potential implications. Beyond reflections related to the two aforementioned educational strategies, learners considered and re-considered their possible decisions if the hypothetical variables were different (N=1) (e.g. a White person instead of a Black person) (Brockett 2016). Additional points discussed in reflection exercises (N=7) included a self-exploration, critiques of the instruction itself, and the role of structural inequities in the development of implicit bias (Carnes et al. 2012; Avant and Gillespie 2019; Ghoshal et al. 2013; Bordt 2004; Russell and Summers 2013; Kokas et al. 2019; O’Connor et al. 2019). N=3 interventions discussed the influence of implicit bias on policies, and potential benefits of implicit bias awareness at the organizational level (Carnes et al. 2012; Russell and Summers 2013; Sherman et al. 2019). Reflective writing exercises accompanied (N=4) discussions (Lypson et al. 2016; White et al. 2018; Schultz and Baker 2017; Perdomo et al. 2019). Nursing students attached a written reflection, guided by faculty-provided prompts, to submitted patient care notes and received feedback and suggestions for bias mitigation (N=1) (Johnson and Richard-Eaglin 2020). N=5 articles asked learners to observe simulations and/or videos to facilitate exploration of bias (White et al. 2018; Russell and Summers 2013; Wijayatunga et al. 2019; Even-Zohar and Werner 2020; Song et al. 2018). Another N=6 articles described video observation of behaviors (biased and not biased) followed by guided debrief (Geller and Watkins 2018; Marion et al. 2018; Teall et al. 2019; Fix 2020; Harrison-Bernard et al. 2020; Kokas et al. 2019).
Active learning
The remainder of the educational strategies comprised a multitude of active learning strategies that moved learners beyond reflection and discussion. Learners engaged deeply with material and participated in discussions in N=15 interventions, achieved strategy identification in N=12 interventions, and achieved skill development and practice in N=6 interventions.
Interventions engaging learners deeply with material highlighted the variety of available active learning educational strategies (Queen’s University 2021). Perspective-taking exercises (N=6) provided learners with opportunities to consider the point of view of another as it may relate to race and intersectionality (Avant and Gillespie 2019), sexual orientation (Klein and Nakhai 2016), disability (White et al. 2018), and the patient experience (Schultz and Baker 2017; Perdomo et al. 2019; Sukhera et al. 2020). Active engagement of learners also could be found in N=5 interventions involving think-pair-share activities (Carnes et al. 2012; Russell and Summers 2013; Kokas et al. 2019; Perdomo et al. 2019; Sukhera et al. 2020). Think-pair-share exercises enable learners to think about a question or problem posed by a facilitator, formulate an answer, and then discuss with another learner; both learners engage with the material and have the option to share with the larger group (Lyman 1987). Mapping exercises were conducted in N=2 interventions. Intersectionality and the experience of perceived bias was explored through identity mapping followed by discussion; these discussions led to the recognition of the contrasting issues of privileged and oppressed aspects of identity within the same individual (Avant and Gillespie 2019). Learners in a diversity training for academia performed a group-matching exercise of terms and definitions. Terms and definitions were discussed by the group; this was followed by group brainstorming to further hone concepts of implicit bias (Harrison-Bernard et al. 2020). Mindfulness training (N=1) occurred followed by personal narrative sharing in pairs, and by group discussion (Hunsinger, Christopher, and Schmidt 2019). Emergency department clinicians participated in service learning and developed presentations to share with their peers (N=1) (McMichael et al. 2019).
Active learning principles were used to achieve strategy identification. After reviewing case studies focused on interpersonal encounters, learners brainstormed novel options to re-conceptualize biased beliefs, and identify strategies to manage and mitigate bias (N=10) (Gandhi and Johnson 2016; Clementz et al. 2017; Wu et al. 2019; Perdomo et al. 2019; Sukhera et al. 2020; Sandoval et al. 2020; Song et al. 2018; Osman and Gottlieb 2018; Brooks, Rougas, and George 2016; Goldenberg, Cyrus, and Wilkins 2019). Another intervention (N=1) enhanced the relevance of bias instruction to learners by choosing discipline-specific tasks (for faculty search committees) during which learners identify sources of bias and ways to mitigate the effects of bias (Cahn 2017). Application of concepts to typical professional activities also occurred after mindfulness trainings seeking to mitigate implicit bias (N=1) (Hunsinger, Christopher, and Schmidt 2019).
Still, other interventions (N=6) moved beyond strategy identification to skill development and practice. They utilized role-plays with structured debriefs (N=4) focused on effective mentoring of diverse faculty (Gandhi and Johnson 2016), addressing bias in clinical encounters (Gonzalez, Fox, and Marantz 2015; Kanter et al. 2020), and on facilitating conversations about racism (O’Connor et al. 2019). In the latter intervention, learners additionally applied implicit bias concepts to create or transform one of their own class activities (O’Connor et al. 2019). Another intervention (N=1) utilized trained actors to portray standardized learners (SL); one SL was on the receiving end of bias from a patient, and the other SL expressed implicit bias during simulated patient care, enabling faculty learners to practice skills with the SL (Poitevien and Osman 2018). Finally, forum theater builds on role-play techniques and was used to provide learners with the opportunity to experience a challenge within a scene and then practice new skills (N=1): Learners brainstormed strategies to respond to patients demonstrating bias toward trainees, and then practiced skills to advocate for mistreated trainees (Rizk et al. 2020).
Data synthesis: Assessment strategies
Table 3 categorizes interventions by assessment strategies; it details the outcomes assessed, the results, and provides evidence of construct validity of the assessments (if any was provided by the authors). Of the N=51 studies, N=14 articles did not include any assessment of learners, N=28 studies included assessment data based solely on learner self-report about knowledge, attitudes and/or skills in various constructs of interest including implicit bias at the personal and/or systemic level, strategies to manage implicit bias in oneself, addressing perceived bias from others, perceptions of obese or older individuals, caring for veterans, delivering care to minority populations, medical school admissions, teaching encounters, and mentoring. The remaining N=9 studies reported objective assessments of learners. Constructs of interest included parental placements of children compared to foster care placements, knowledge tests, performance in standardized patient exercises, ethnocultural empathy, stigma, considerations of race in clinical care, and shooter bias. N=9 studies provided some evidence of construct validity for their assessments. These included interrater reliability (Marion et al. 2018), internal consistency (Shields, Zawadzki, and Johnson 2011; Kokas et al. 2019; Hunsinger, Christopher, and Schmidt 2019; Fix 2020; Even-Zohar and Werner 2020; Chapman et al. 2018; Kanter et al. 2020), and multiple types of construct validity, including internal consistency, convergent validity, and face validity (Sukhera et al. 2020). Only N=1 study assessed learners to the level of actual behaviors affecting the intended ultimate beneficiaries of the intervention (children and families experiencing foster care placement) (Russell and Summers 2013). N=29 studies reported improvement in their assessments related to implicit bias. N=4 studies reported qualitative analysis of self-reported attitudes only in the form of learner written reflections (and therefore could not quantify change) (Avant et al. 2018; Motzkus et al. 2019; McMichael et al. 2019; Johnson and Richard-Eaglin 2020), N=1 did not provide numerical data for their quantitative assessments (Rizk et al. 2020), and N=3 studies reported negative data including no change in objective knowledge assessments (Sandoval et al. 2020), self-reported changes in attitudes (Geller and Watkins 2018), and no change in willingness to work with older adults (Even-Zohar and Werner 2020).
Table 3.
Interventions included in scoping review of implicit bias interventions across multiple professional disciplines related to the social determinants of health categorized by self-reported and objective assessments detailing outcome(s) measured, results, and timing of assessment (2000–2020).
| Study Number* | Outcome Assessed** | Results of Assessment | Timing of Assessment |
|---|---|---|---|
| Assessment: Self-Report | |||
| 1 | Attitudes through written reflections | Qualitatively analyzed in aggregate, unable to quantify change | Immediate |
| 6 | Awareness of bias and its influence in medical school admissions decisions | Increased awareness | 16+ weeks |
| 7 | Knowledge and commitment to change | Increased across all measures | 16+ weeks |
| 8 | Empathy- Ethnocultural empathy scale and Jefferson Empathy Scale, Patient-Practitioner Orientation Scale (Patient Centeredness) internal consistency for the three ranged from 0.82 to 0.87 | Intervention group had significantly higher (better) scores on the three scales as compared to the comparison group. | Immediate |
| 9 | Confidence | Increased | Immediate |
| 10 | Frabroni scale of aging (explicit bias)- Internal consistency was 0.72–0.82; Facts on aging quiz- Internal consistency at 0.38–0.40; Relating to older people alpha = 0.57–0.67) | No change in willingness to work with older adults. Did not report the changes in explicit bias but rather looked at the correlations of explicit bias with the other variables. | 1–16 weeks |
| 12 | Skills in mentoring, communication, fostering independence, and addressing diversity in the mentoring relationship | Increased across all constructs | 1–16 weeks |
| 13 | Awareness of bias and the importance of managing it for clinical care, identification of strategies | Increased awareness and recognition of managing bias in nursing care would be helpful. Strategies were analyzed qualitatively in aggregate, unable to quantify change. | Immediate |
| 14 | Knowledge and attitudes | 53% reported no change in self-reported attitudes on post-session follow up | 16+ weeks |
| 15 | Attitudes on racism and prejudice | Increase in acceptance of racial prejudice in self and general population, no change in concern about having implicit bias | Immediate |
| 16 | Skills and attitude around trainee mistreatment | Improved attitudes, increased self-efficacy in recognizing and addressing mistreatment | Immediate |
| 18 | Attitudes | Differences noted between “deniers” and “accepters” of implicit bias potentially influencing some clinical decisions and behaviors | Immediate |
| 22 | Attitudes through written reflections | Qualitatively analyzed in aggregate, unable to quantify change | Immediate |
| 25 | Racial Attributes in Clinical Evaluation survey (internal consistency α=0.885) | Self-reported increased consideration of race in clinical care as compared to pre/post. | 16+ weeks |
| 26 | Knowledge, confidence, and attitudes | Increased across all constructs | Immediate |
| 28 | Knowledge and comfort | Increased across all constructs | Unspecified |
| 29 | Knowledge, competence, and performance | Increased across all constructs | 16+ weeks |
| 30 | Attitudes through written reflections | Qualitatively analyzed in aggregate, unable to quantify change | Immediate |
| 32 | Attitudes through written reflections | Qualitatively analyzed in aggregate, unable to quantify change | Immediate |
| 33 | Self-efficacy | Increase in 13 of 17 self-efficacy measures | Immediate |
| 36 | Skills in recognizing and addressing bias and in teaching trainees about bias | Increased across all constructs | Immediate |
| 37 | Knowledge | No numerical values provided | Immediate |
| 40 | Attitudes and strategies | Decrease in skepticism of IAT results, strategies reflected awareness and acceptance of bias within oneself | Immediate |
| 44 | Mental illness clinician attitudes scale (good face validity, internal consistency α=0.72, moderate convergent validity to similar scales r=0.32–0.49), brief mental illness attitudes scale (internal consistency α > 0.8 and consistent two factor solution), self-reported attitudes through qualitative interviews (conducted months after intervention) | Improvements in explicit attitudes regarding mental illness, but only in the pediatric clinical contexts, not adult emergency contexts; any improvements were not sustained six months later; qualitative interviews did not quantify change | Immediate |
| 45 | Strategies | Change in strategies from pre-post with less internal feedback and humanism strategies and more reflection and debriefing strategies. | Immediate |
| 49 | Knowledge and confidence | Increased across all measures | Immediate |
| 50 | Attitudes | Improved attitudes regarding awareness of implicit bias and its potential influence on clinical care pre/post | Immediate |
| 51 | Knowledge and confidence | Increase in knowledge and confidence to address own biases | Immediate |
| Assessment: Objective | |||
| 11 | Knowledge (true and false questions- with internal consistency of α=0.74) and the Scale of Ethnocultural Empathy (adapted a previously validated scale for their purposes) | Increased across all constructs | Immediate |
| 17 | Knowledge, and self-reported attitudes and confidence | Increased across all constructs | 1–16 weeks |
| 19 | Knowledge, and self-reported attitudes and confidence | Increased across all constructs | Immediate |
| 21 | Shooter Bias Task and a Five Facet Mindfulness Questionnaire- short form (internal consistency for subscales used ranged from alpha 0.70 to 0.86) | Improved control for Black targets pre/post, no change for the Five Facets Mindfulness Questionnaire | 1–16 weeks |
| 23 | Skills assessed through trained observer ratings of participants in standardized patient interactions, self-reported attitudes using Everyday Multicultural Competencies/Revised Scale of Ethnocultural Empath- the Acting as an Ally subscale (internal consistency α>0.70 at both time points), feelings thermometers about various ethnic/racial groups (explicit attitudes- internal consistency α > 0.94 at both time points), Working Alliance Inventory (internal consistency α > 0.85), interaction closeness mean composite score (internal consistency α > 0.67). | Improved emotional rapport building, fewer microaggressions, improved self-reported explicit attitudes and increased self-reported working alliance and interaction closeness with Black standardized patient. | 2 days |
| 27 | Common Ground instrument (Inter-rater reliability = 0.85 for the overall global ratings and 0.92 for the overall checklist assessment) and health literacy skills checklist | Increased across all constructs | 1–16 weeks |
| 38 | Outcomes related to intended ultimate beneficiaries (parents and children in contact with the foster care system) | Increased parental placement of children (as opposed to foster care placement) | Unspecified |
| 39 | Knowledge, self-reported awareness and self-efficacy | No change in knowledge or self-reported awareness, reduction of perceived challenges to addressing microaggressions | Immediate |
| 42 | Knowledge (internal consistency of measures α= 0.87–0.91) | Increased scores for learners in intervention versus control condition | Immediate |
Study numbers refer to numerical order listed in Table 1. References 2, 3, 4, 5, 20, 24, 31, 34, 35, 41, 43, 46, 47, 48 did not report any assessments of learners.
If an intervention included objective and self-reported assessments, it is listed within the objective assessments portion of the table.
For the N=37 studies reporting assessment of learners, the timing varied widely (Table 3). Most (N=24) of the interventions included an assessment that was limited to during or immediately post-intervention, another (N=1) at two days. N=5 interventions assessed the impact of the intervention at one week or more but up to a 16-week time frame. N=5 interventions included an assessment at 16 weeks or longer post-intervention. N=2 interventions did not specify the timing of the interventions.
Overall, interventions relied mostly on learner self-report for their assessments, and the overwhelming majority demonstrated gains in participants perceived knowledge, attitudes, and confidence. Given the variety of educational strategies, biases targeted, and assessment strategies that were often developed specifically for each intervention and mostly relied on self-report, it is not possible to compare studies and identify any particular approach that yielded superior results compared to others. Data charting identified a clear gap in assessments focused on learner behaviors affecting an intervention’s intended beneficiaries (e.g. patient outcomes), as well as a dearth of assessment strategies yielding objective and long-term outcomes.
Discussion
This review provides tangible examples of curricula to complement existing frameworks (Teal et al. 2012; Sukhera and Watling 2018; Sukhera, Watling, and Gonzalez 2020; Gonzalez, Lypson, and Sukhera 2021). Educators engaged learners in provocative/engagement triggers, used the IAT, undertook reflection activities, and delivered varied active learning exercises. Approaches to assessment varied, were most often conducted immediately after the session, and most often used learner self-report. A variety of biases were addressed across multiple professions and levels of learner experience. These examples, from across various professions related to the social determinants of health, may inform health professions educators’ efforts in developing novel curricula in IBRM. Given the global interest to address social inequities and racism (Crear-Perry et al. 2020), educators may choose to adapt curricula described in this review, that may be from other disciplines (despite the limited unifying data, given the urgency of this complex problem), but that align closely with existing institutional resources, thereby optimizing feasibility.
We also identified gaps in IBRM curricula, most notably in educational strategies fostering skill development and in assessments incorporating outcome metrics with evidence of construct validity. These gaps highlight opportunities to conduct future research, which we expand upon below. To our knowledge, our review is unique in searching across multiple disciplines including healthcare, education, social work, and law, professions related to the social determinants of health (World Health Organization 2021).
Implications for curriculum development and future research
The gaps identified through data charting highlight the ongoing need to expand current approaches to curriculum development in IBRM. We are calling on educators and investigators to design opportunities for learners to develop and practice skills in IBRM, to develop learner assessments with evidence of construct validity, and to conduct rigorous program evaluations of curricula in IBRM. Curricula that engage learners with provocative/educational triggers allow for experiential learning and organic discoveries to expand horizons and begin paradigm shifts (Van Schalkwyk et al. 2019; Sukhera, Watling, and Gonzalez 2020). However, awareness of one’s own implicit bias often goes against learners’ self-identities of good people who would do the right thing (Gonzalez et al. 2019). Intentional approaches identified through data charting exemplify efforts to de-stigmatize and normalize implicit bias (Gonzalez, Fox, and Marantz 2015; Wu et al. 2019; Ghoshal et al. 2013; Kokas et al. 2019); such ongoing efforts could assist both facilitators and learners in their ability to engage with discomfort and move deeper into continued exploration of previously unrecognized bias (Gonzalez et al. 2019).
As noted above, novel approaches to active learning have been identified as one approach to implicit bias instruction. Most identified interventions utilizing active learning as an educational strategy did not empower learners with skills in IBRM that they can use during clinical encounters. Given our stated position that instruction in IBRM should take a skills-based, behavioral approach, and that the ultimate goal of instruction in IBRM should be to improve patient outcomes, we suggest that curriculum developers and educators set a knowledge foundation of the impact of implicit bias on healthcare disparities (Zestcott, Blair, and Stone 2016) and foster learner attitudes of acceptance of bias in oneself and its potential influence on clinical care (Teal et al. 2012). Educators in IBRM should then strive to provide opportunities for skill development and practice based on the robust literature demonstrating associations between physician implicit bias and their communication behaviors (Cooper et al. 2012; Penner et al. 2016; Hagiwara et al. 2017); this can be accomplished through role-plays and standardized patient simulations.
Educators could advocate for increased time in the compulsory curricula, as suggested by existing frameworks (Teal et al. 2012; Sukhera and Watling 2018; Sukhera, Watling, and Gonzalez 2020; Gonzalez, Lypson, and Sukhera 2021). Additional sessions should focus on moving the learner beyond awareness and recognition of bias, to developing and practicing skills to manage the effects of bias in clinical encounters: Our (CMG) previous work suggests that medical students need additional sessions dedicated to skill development and practice as they are unable to move from awareness and acceptance of implicit bias to strategy identification to mitigate the impact of implicit bias on their future clinical encounters on their own (Gonzalez, Noah, et al. 2021). Additional curricular time and intentional skills-based curriculum development as described above would empower learners and not leave them grasping for strategies to provide excellent, equitable care.
We found no published curricular interventions that demonstrate changes in outcomes for patients, who are the intended beneficiaries of such interventions. In keeping with our position that enhanced patient outcomes should be a goal of IBRM instruction focused on the patient-physician encounter, we suggest aligning assessment strategies for implicit bias with theoretical frameworks such as educationally sensitive patient outcomes (ESPO) (Kalet et al. 2010): Educationally sensitive refers to patient outcomes that are expected to change in response to instruction delivered to a learner (Kalet et al. 2010). ESPO are a concept adapted from ambulatory sensitive patient conditions, which are studied by health services researchers; educators interested in studying ESPO may benefit from collaborating with health services researchers and combining their respective areas of expertise (Kalet et al. 2010). Educators can assess ESPO related to communication skills within IBRM through checklists and global rating scales.
The gaps identified in assessment strategies in existing implicit bias interventions present opportunities to advance research in IBRM by developing and obtaining construct validity evidence for novel outcome metrics focused on knowledge, attitudes, and skills related to IBRM. Educators can collaborate with psychometricians to move beyond internal consistency (the most commonly identified type of construct validity in our data charting) to evaluate convergent/divergent validity, and even more importantly, consequential validity (Downing 2003). Adapted scales could additionally assess behaviors identified by patients in our (CMG, MLL) previous work to be restorative for the patient-physician relationship, even after bias is perceived; these behaviors include acknowledging perceived or actual bias in real time during the encounter (Gonzalez, Deno, et al. 2018). Learner assessments, in aggregate, would facilitate program evaluations of the impact of curricula on learners knowledge, skills, and attitudes in IBRM (Thomas et al. 2016). Aggregate learner assessments that include ESPO could evaluate an intervention’s efficacy in ways that are relevant to patient outcomes and health equity, and would be an important component of a rigorous program evaluation. Qualitative investigations of learners’ perspectives prior to, during, and post-instruction would also guide revisions to enhance learner engagement and efficacy of instruction and help identify blind spots we have as educators in the development of instruction (Gonzalez et al. 2020; Gonzalez et al. 2019).
Finally, we suggest educators designing instruction in implicit bias have formal training in curriculum development, given the potential for unintended consequences of such instruction (Burgess et al. 2007). They should also have a significant understanding of the implicit bias and health equity literature, or partner with someone who does, in order to develop sound, evidence-based interventions, and to minimize efforts required to create new interventions, when some may already exist in the literature. As has been demonstrated in other disparities-related curricular development initiatives (Cene et al. 2010; Kelley et al. 2008), we recommend collaborating with patients and/or community members from diverse backgrounds in the development of implicit bias instruction, and especially on standardized patient simulations focused on IBRM to enhance the fidelity of the simulations and their relevance from the patients’ perspective, uncover any blind spots in the simulations, and proactively mitigate unintended consequences such as reinforcing negative stereotypes (Dijk, Duijzer, and Wienold 2020; Asmerom et al. 2022). Community member and patient perspectives can inform the development of ESPO as well. Finally, collaborating with psychometricians may enhance educators’ approaches to assessment and will increase the proportion of assessments with evidence of construct validity.
Limitations
Limiting to English only studies, we may have missed additional perspectives in the non-English literature. In addition, as this was a scoping review, we did not assess the quality of the included studies. It is not known if the paucity of interventions in professions outside of the health professions is secondary to our search strategy or to a true dearth of published interventions addressing implicit bias. We only identified three interventions with negative data and are unable to assess the impact of publication bias on the reporting of other interventions with negative data. Strengths of this review include an exhaustive search, and the inclusion of multiple professions beyond healthcare. In addition, this review ensured that articles included learners from early pre-professional stages to practicing professionals.
Conclusion
Our scoping review identified and categorized implicit bias curricula utilizing a broad range of educational strategies and approaches to assessment. The curricula identified may serve as a resource for health professions educators seeking to deliver instruction in IBRM. The gaps we highlight call for continued research to develop instruction enabling learners to develop and practice skills in IBRM in clinical encounters, to develop robust assessments with validated outcome metrics, and to conduct rigorous program evaluations. Successfully addressing these gaps could mitigate the contribution of clinicians’ implicit biases to health disparities thereby contributing to the ultimate goal of improved, equitable patient outcomes.
Supplementary Material
Funding/Support:
Dr. Gonzalez is supported by NIH/National Institute for Minority Health and Health Disparities grant number K23MD014178 and was previously supported while conducting this scoping review by the Harold Amos Medical Faculty Development Program of the Robert Wood Johnson Foundation grant number 70639, and by the Macy Faculty Scholars Program of the Josiah Macy Jr. Foundation.
N=18 studies received support from the following funders listed: varied institutes within the National Institutes of Health (NIH) (N=9) (Teal et al. 2010; Gandhi and Johnson 2016; Gonzalez, Kim, and Marantz 2014; Gonzalez, Fox, and Marantz 2015; Chapman et al. 2018; McElfish et al. 2017; Harrison-Bernard et al. 2020; McMichael et al. 2019; Hunsinger, Christopher, and Schmidt 2019); Health Resources and Services Administration (N=2) (Marion et al. 2018; Gonzalez, Fox, and Marantz 2015); department of Veterans Affairs funding mechanisms (N=2) (Teal et al. 2010; Clementz et al. 2017); center for Disease Control and Prevention (N=1) (McElfish et al. 2017); foundations and professional societies (N=3) (Gonzalez, Fox, and Marantz 2015; Sukhera et al. 2020; Kokas et al. 2019); and institutional funds (N=5) (Gonzalez, Fox, and Marantz 2015; Wu et al. 2019; O’Connor et al. 2019; Rizk et al. 2020; Kanter et al. 2020). N=1 study listed a broad array of foundation and individual private support (White et al. 2018). This scoping review was funded by the NIH, Robert Wood Johnson Foundation, and the Josiah Macy, Jr. Foundation. Funders had no role in the writing of this review.
Footnotes
Other disclosures: None
Contributor Information
Cristina M. Gonzalez, professor of medicine, Albert Einstein College of Medicine and Montefiore Medical Center, Bronx, NY..
Chavon M. Onumah, internal medicine residency program director and assistant professor of medicine in the Department of Medicine, The George Washington University School of Medicine and Health Sciences, Washington, DC..
Sydney A. Walker, resident, Department of Pediatrics, University of Utah School of Medicine, Salt Lake City, Utah..
Elisa Karp, attending physician in the Department of Pediatrics, North Central Bronx Hospital, Bronx NY..
Rachel Schwartz, medical librarian, Albert Einstein College of Medicine, Bronx, NY..
Monica L. Lypson, Vice Dean for Education and the Rolf H. Scholdager Professor of Medicine, Columbia University Vagelos College of Physicians & Surgeons, Columbia University Irving Medical Center..
References
- Arksey Hilary, and O’Malley Lisa. 2005. ‘Scoping studies: towards a methodological framework’, International Journal of Social Research Methodology, 8: 19–32. [Google Scholar]
- Asmerom B, Legha RK, Mabeza RM, and Nunez V 2022. ‘An Abolitionist Approach to Antiracist Medical Education’, AMA J Ethics, 24: E194–200. [DOI] [PubMed] [Google Scholar]
- Australian Medical Council Limited. 2012. ‘Standards for Assessment and Accreditation of Primary Medical Programs by the Australian Medical Council, 2012’, Accessed October 16, 2020. https://www.amc.org.au/wp-content/uploads/2019/10/Standards-for-Assessment-and-Accreditation-of-Primary-Medical-Programs-by-the-Australian-Medical-Council-2012.pdf
- Avant ND, and Gillespie GL 2019. ‘Pushing for health equity through structural competency and implicit bias education: A qualitative evaluation of a racial/ethnic health disparities elective course for pharmacy learners’, Currents in Pharmacy Teaching and Learning. [DOI] [PubMed] [Google Scholar]
- Avant ND, Weed E, Connelly C, Hincapie AL, and Penm J 2018. ‘Qualitative Analysis of Student Pharmacists’ Reflections of Harvard’s Race Implicit Association Test’, Curr Pharm Teach Learn, 10: 611–17. [DOI] [PubMed] [Google Scholar]
- Blair IV, Steiner JF, Fairclough DL, Hanratty R, Price DW, Hirsh HK, Wright LA, Bronsert M, Karimkhani E, Magid DJ, and Havranek EP 2013. ‘Clinicians’ implicit ethnic/racial bias and perceptions of care among Black and Latino patients’, Ann Fam Med, 11: 43–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bordt RL 2004. ‘Only some are dead men walking: Teaching about race discrimination and the death penalty’, Teaching Sociology, 32: 358–73. [Google Scholar]
- Brockett Megan. 2016. “Training teaches Annapolis police about 'implicit bias&apos.” In, STATE AND REGIONAL NEWS. [Google Scholar]
- Brooks KC, Rougas S, and George P 2016. ‘When Race Matters on the Wards: Talking About Racial Health Disparities and Racism in the Clinical Setting’, MedEdPORTAL, 12: 10523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess D, van Ryn M, Dovidio J, and Saha S 2007. ‘Reducing racial bias among health care providers: lessons from social-cognitive psychology’, Journal of general internal medicine, 22: 882–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butkus R, Serchen J, Moyer DV, Bornstein SS, Hingle ST, Health, and Public Policy Committee of the American College of Physicians. 2018. ‘Achieving Gender Equity in Physician Compensation and Career Advancement: A Position Paper of the American College of Physicians’, Ann Intern Med, 168: 721–23. [DOI] [PubMed] [Google Scholar]
- Cahn PS 2017. ‘Recognizing and Reckoning With Unconscious Bias: A Workshop for Health Professions Faculty Search Committees’, MedEdPORTAL, 13: 10544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capers Q IV, Clinchot D, McDougle L, and Greenwald AG 2017. ‘Implicit Racial Bias in Medical School Admissions’, Acad Med, 92: 365–69. [DOI] [PubMed] [Google Scholar]
- Carnes M, Devine PG, Isaac C, Manwell LB, Ford CE, Byars-Winston A, Fine E, and Sheridan JT 2012. ‘Promoting Institutional Change Through Bias Literacy’, J Divers High Educ, 5: 63–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cene CW, Peek ME, Jacobs E, and Horowitz CR 2010. ‘Community-based teaching about health disparities: combining education, scholarship, and community service’, Journal of general internal medicine, 25 Suppl 2: S130–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaiyachati KH, Beidas RS, Lane-Fall MB, Rendle KA, Shelton RC, and Kaufman EJ 2022. ‘Weaving Equity into the Fabric of Medical Research’, Journal of general internal medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman MV, Hall WJ, Lee K, Colby R, Coyne-Beasley T, Day S, Eng E, Lightfoot AF, Merino Y, Siman FM, Thomas T, Thatcher K, and Payne K 2018. ‘Making a difference in medical trainees’ attitudes toward Latino patients: A pilot study of an intervention to modify implicit and explicit attitudes’, Soc Sci Med, 199: 202–08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clementz L, McNamara M, Burt NM, Sparks M, and Singh MK 2017. ‘Starting With Lucy: Focusing on Human Similarities Rather Than Differences to Address Health Care Disparities’, Acad Med, 92: 1259–63. [DOI] [PubMed] [Google Scholar]
- Colon-Emeric CS, Corazzini K, McConnell E, Pan W, Toles M, Hall R, Batchelor-Murphy M, Yap TL, Anderson AL, Burd A, and Anderson RA 2017. ‘Study of Individualization and Bias in Nursing Home Fall Prevention Practices’, J Am Geriatr Soc, 65: 815–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee on Accreditation of Canadian Medical Schools. 2018. ‘CACMS Standards and Elements’, Accessed October 3, 2020. https://cacms-cafmc.ca/accreditation-documents/2019-2020/standards-and-elements.
- Cooper LA, Roter DL, Carson KA, Beach MC, Sabin JA, Greenwald AG, and Inui TS 2012. ‘The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care’, Am J Public Health, 102: 979–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crear-Perry J, Maybank A, Keeys M, Mitchell N, and Godbolt D 2020. ‘Moving towards anti-racist praxis in medicine’, Lancet, 396: 451–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dasgupta N, and Greenwald AG 2001. ‘On the malleability of automatic attitudes: combating automatic prejudice with images of admired and disliked individuals’, Journal of personality and social psychology, 81: 800–14. [DOI] [PubMed] [Google Scholar]
- Daugherty SL, Blair IV, Havranek EP, Furniss A, Dickinson LM, Karimkhani E, Main DS, and Masoudi FA 2017. ‘Implicit Gender Bias and the Use of Cardiovascular Tests Among Cardiologists’, J Am Heart Assoc, 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dijk SW, Duijzer EJ, and Wienold M 2020. ‘Role of active patient involvement in undergraduate medical education: a systematic review’, BMJ Open, 10: e037217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downing SM 2003. ‘Validity: on meaningful interpretation of assessment data’, Med Educ, 37: 830–7. [DOI] [PubMed] [Google Scholar]
- Even-Zohar A, and Werner S 2020. ‘The Effect of Educational Interventions on Willingness to Work with Older Adults: A Comparison of Students of Social Work and Health Professions’, Journal of gerontological social work, 63: 114–32. [DOI] [PubMed] [Google Scholar]
- Feagin J, and Bennefield Z 2014. ‘Systemic racism and U.S. health care’, Soc Sci Med, 103: 7–14. [DOI] [PubMed] [Google Scholar]
- FitzGerald C, Martin A, Berner D, and Hurst S 2019. ‘Interventions designed to reduce implicit prejudices and implicit stereotypes in real world contexts: a systematic review’, BMC Psychol, 7: 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fix Rebecca L. 2020. ‘Justice is not blind: A preliminary evaluation of an implicit bias training for justice professionals’, Race and Social Problems, 12: 362–74. [Google Scholar]
- Forscher PS, Lai CK, Axt JR, Ebersole CR, Herman M, Devine PG, and Nosek BA 2019. ‘A meta-analysis of procedures to change implicit measures’, Journal of personality and social psychology, 117: 522–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandhi Monica, and Johnson Mallory. 2016. ‘Creating more effective mentors: Mentoring the mentor’, AIDS and Behavior, 20: 294–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gatewood E, Broholm C, Herman J, and Yingling C 2019. ‘Making the invisible visible: Implementing an implicit bias activity in nursing education’, Journal of professional nursing : official journal of the American Association of Colleges of Nursing, 35: 447–51. [DOI] [PubMed] [Google Scholar]
- Geller G, and Watkins PA 2018. ‘Addressing Medical Students’ Negative Bias Toward Patients With Obesity Through Ethics Education’, AMA J Ethics, 20: E948–59. [DOI] [PubMed] [Google Scholar]
- Ghoshal RA, Lippard C, Ribas V, and Muir K 2013. ‘Beyond Bigotry: Teaching about Unconscious Prejudice’, Teaching Sociology, 41: 130–43. [Google Scholar]
- Goldenberg MN, Cyrus KD, and Wilkins KM 2019. ‘ERASE: a New Framework for Faculty to Manage Patient Mistreatment of Trainees’, Acad Psychiatry, 43: 396–99. [DOI] [PubMed] [Google Scholar]
- Gonzalez CM, Deno ML, Kintzer E, Marantz PR, Lypson ML, and McKee MD 2018. ‘Patient perspectives on racial and ethnic implicit bias in clinical encounters: Implications for curriculum development’, Patient Educ Couns, 101: 1669–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ———. 2019. ‘A Qualitative Study of New York Medical Student Views on Implicit Bias Instruction: Implications for Curriculum Development’, Journal of general internal medicine, 34: 692–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez CM, Fox AD, and Marantz PR 2015. ‘The Evolution of an Elective in Health Disparities and Advocacy: Description of Instructional Strategies and Program Evaluation’, Acad Med, 90: 1636–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez CM, Garba RJ, Liguori A, Marantz PR, McKee MD, and Lypson ML 2018. ‘How to Make or Break Implicit Bias Instruction: Implications for Curriculum Development’, Acad Med, 93: S74–S81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez CM, Kim MY, and Marantz PR 2014. ‘Implicit bias and its relation to health disparities: a teaching program and survey of medical students’, Teach Learn Med, 26: 64–71. [DOI] [PubMed] [Google Scholar]
- Gonzalez CM, Lypson ML, and Sukhera J 2021. ‘Twelve tips for teaching implicit bias recognition and management’, Medical teacher: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez CM, Nava S, List J, Liguori A, and Marantz PR 2021. ‘How Assumptions and Preferences Can Affect Patient Care: An Introduction to Implicit Bias for First-Year Medical Students’, MedEdPORTAL, 17: 11162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez CM, Noah YS, Correa N, Archer-Dyer H, Weingarten-Arams J, and Sukhera J 2021. ‘Qualitative analysis of medical student reflections on the implicit association test’, Med Educ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez CM, Walker SA, Rodriguez N, Karp E, and Marantz PR 2020. ‘It Can Be Done! A Skills-Based Elective in Implicit Bias Recognition and Management for Preclinical Medical Students’, Acad Med, 95: S150–S55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez CM, Walker SA, Rodriguez N, Noah YS, and Marantz PR 2021. ‘Implicit Bias Recognition and Management in Interpersonal Encounters and the Learning Environment: A Skills-Based Curriculum for Medical Students’, MedEdPORTAL, 17: 11168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green AR, Carney DR, Pallin DJ, Ngo LH, Raymond KL, Iezzoni LI, and Banaji MR 2007. ‘Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients’, Journal of general internal medicine, 22: 1231–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwald AG, McGhee DE, and Schwartz JL 1998. ‘Measuring individual differences in implicit cognition: the implicit association test’, Journal of personality and social psychology, 74: 1464–80. [DOI] [PubMed] [Google Scholar]
- Hagiwara N, Slatcher RB, Eggly S, and Penner LA 2017. ‘Physician Racial Bias and Word Use during Racially Discordant Medical Interactions’, Health Commun, 32: 401–08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison-Bernard LM, Augustus-Wallace AC, Souza-Smith FM, Tsien F, Casey GP, and Gunaldo TP 2020. ‘Knowledge gains in a professional development workshop on diversity, equity, inclusion, and implicit bias in academia’, Advances in physiology education, 44: 286–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hausmann LR, Myaskovsky L, Niyonkuru C, Oyster ML, Switzer GE, Burkitt KH, Fine MJ, Gao S, and Boninger ML 2015. ‘Examining implicit bias of physicians who care for individuals with spinal cord injury: A pilot study and future directions’, J Spinal Cord Med, 38: 102–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmeister S, and Soprych A 2017. ‘Teaching resident physicians the power of implicit bias and how it impacts patient care utilizing patients who have experienced incarceration as a model’, Int J Psychiatry Med, 52: 345–54. [DOI] [PubMed] [Google Scholar]
- Hunsinger Matthew, Christopher Michael, and Schmidt Andi M. 2019. ‘Mindfulness training, implicit bias, and force response decision-making’, Mindfulness, 10: 2555–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson R, and Richard-Eaglin A 2020. ‘Combining SOAP Notes With Guided Reflection to Address Implicit Bias in Health Care’, J Nurs Educ, 59: 59. [DOI] [PubMed] [Google Scholar]
- Kalet AL, Gillespie CC, Schwartz MD, Holmboe ES, Ark TK, Jay M, Paik S, Truncali A, Hyland Bruno J, Zabar SR, and Gourevitch MN 2010. ‘New measures to establish the evidence base for medical education: identifying educationally sensitive patient outcomes’, Acad Med, 85: 844–51. [DOI] [PubMed] [Google Scholar]
- Kanter JW, Rosen DC, Manbeck KE, Branstetter HML, Kuczynski AM, Corey MD, Maitland DWM, and Williams MT 2020. ‘Addressing microaggressions in racially charged patient-provider interactions: a pilot randomized trial’, BMC Med Educ, 20: 88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley L, Chou CL, Dibble SL, and Robertson PA 2008. ‘A critical intervention in lesbian, gay, bisexual, and transgender health: knowledge and attitude outcomes among second-year medical students’, Teach Learn Med, 20: 248–53. [DOI] [PubMed] [Google Scholar]
- Klein EW, and Nakhai M 2016. ‘Caring for LGBTQ patients: Methods for improving physician cultural competence’, International Journal of Psychiatry in Medicine, 51: 315–24. [DOI] [PubMed] [Google Scholar]
- Kokas M, Fakhoury JW, Hoffert M, Whitehouse S, Van Harn M, and Baker-Genaw K 2019. ‘Health Care Disparities: a Practical Approach to Teach Residents about Self-Bias and Patient Communication’, Journal of Racial and Ethnic Health Disparities, 6: 1030–34. [DOI] [PubMed] [Google Scholar]
- Levac D, Colquhoun H, and O’Brien KK 2010. ‘Scoping studies: advancing the methodology’, Implement Sci, 5: 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liaison Committee on Medical Education. 2020. ‘Functions and structure of a medical school: standards for accreditation of medical education prgrams leading to the M.D. degree.’, Liaison Committee on Medical Education, Accessed June 26, 2020. https://lcme.org/publications/. [Google Scholar]
- Lyman F 1987. ‘Think-Pair-Share: An Ending Teaching Technique’, MAA-CIE Cooperative News, 1: 1–2. [Google Scholar]
- Lypson ML, Ross PT, Zimmerman N, Goldrath KE, and Ravindranath D 2016. ‘Where Do Soldiers Really Come From? A Faculty Development Workshop on Veteran-Centered Care’, Acad Med, 91: 1379–83. [DOI] [PubMed] [Google Scholar]
- Marion GS, Hairston JM, Davis SW, and Kirk JK 2018. ‘Using Standardized Patient Assessments to Evaluate a Health Literacy Curriculum’, Fam Med, 50: 52–57. [DOI] [PubMed] [Google Scholar]
- Mayfield JJ, Ball EM, Tillery KA, Crandall C, Dexter J, Winer JM, Bosshardt ZM, Welch JH, Dolan E, Fancovic ER, Nanez AI, De May H, Finlay E, Lee SM, Streed CG, and Ashraf K 2017. ‘Beyond Men, Women, or Both: A Comprehensive, LGBTQ-Inclusive, Implicit-Bias-Aware, Standardized-Patient-Based Sexual History Taking Curriculum’, MedEdPORTAL, 13: 10634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McElfish PA, Long CR, Rowland B, Moore S, Wilmoth R, and Ayers B 2017. ‘Improving Culturally Appropriate Care Using a Community-Based Participatory Research Approach: Evaluation of a Multicomponent Cultural Competency Training Program, Arkansas, 2015–2016’, Preventing chronic disease, 14: E62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMichael B, Nickel A, Duffy EA, Skjefte L, Lee L, Park P, Nelson SC, Puumala S, and Kharbanda AB 2019. ‘The Impact of Health Equity Coaching on Patient’s Perceptions of Cultural Competency and Communication in a Pediatric Emergency Department: An Intervention Design’, J Patient Exp, 6: 257–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medlock M, Weissman A, Wong SS, Carlo A, Zeng M, Borba C, Curry M, and Shtasel D 2017. ‘Racism as a Unique Social Determinant of Mental Health: Development of a Didactic Curriculum for Psychiatry Residents’, MedEdPORTAL, 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mezirow J 1997. ‘Transformative Learning: Theory to Practice. In Transformative learning in action: insights from practice.’, New Directions for Adult and Continuing Education, 74: 5–12. [Google Scholar]
- Motzkus C, Wells RJ, Wang X, Chimienti S, Plummer D, Sabin J, Allison J, and Cashman S 2019. ‘Pre-clinical medical student reflections on implicit bias: Implications for learning and teaching’, PLoS One, 14: e0225058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor MR, Barrington WE, Buchanan DT, Bustillos D, Eagen-Torkko M, Kalkbrenner A, Laing SS, Reding KW, and de Castro AB 2019. ‘Short-Term Outcomes of a Diversity, Equity, and Inclusion Institute for Nursing Faculty’, J Nurs Educ, 58: 633–40. [DOI] [PubMed] [Google Scholar]
- Osman NY, and Gottlieb B 2018. ‘Mentoring Across Differences’, MedEdPORTAL, 14: 10743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penner LA, Dovidio JF, Gonzalez R, Albrecht TL, Chapman R, Foster T, Harper FW, Hagiwara N, Hamel LM, Shields AF, Gadgeel S, Simon MS, Griggs JJ, and Eggly S 2016. ‘The Effects of Oncologist Implicit Racial Bias in Racially Discordant Oncology Interactions’, J Clin Oncol, 34: 2874–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perdomo J, Tolliver D, Hsu H, He Y, Nash KA, Donatelli S, Mateo C, Akagbosu C, Alizadeh F, Power-Hays A, Rainer T, Zheng DJ, Kistin CJ, Vinci RJ, and Michelson CD 2019. ‘Health Equity Rounds: An Interdisciplinary Case Conference to Address Implicit Bias and Structural Racism for Faculty and Trainees’, MedEdPORTAL, 15: 10858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poitevien P, and Osman C 2018. ‘Tackling Implicit and Explicit Bias Through Objective Structured Teaching Exercises for Faculty’, Journal of graduate medical education, 10: 353–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Project Implicit. 2011. ‘Implicit Association Test’, Accessed October 29, 2021. https://implicit.harvard.edu/implicit/.
- Queen’s University. 2021. ‘Teaching and Learning in Higher Education’, Accessed November 19, 2021. https://www.queensu.ca/teachingandlearning/modules/students/22_active_learning_strategies.html.
- Rakhra A, Ogedegbe G, Williams O, Onakomaiya D, and Ovbiagele B 2021. ‘Representation of Racial/ Ethnic Minority Individuals in the Leadership of Major Medical Journals’, J Health Dispar Res Pract, 14: 69–81. [PMC free article] [PubMed] [Google Scholar]
- Ring J, Nyquist J, Mitchell S, Flores H, Samaniego L. 2008. Curriculum for Culturally Responsive Health Care: The Step-by-Step Guide for Cultural Competence Training (Radcliffe Publishing: Oxford: ). [Google Scholar]
- Rizk N, Jones S, Shaw MH, and Morgan A 2020. ‘Using Forum Theater as a Teaching Tool to Combat Patient Bias Directed Toward Health Care Professionals’, MedEdPORTAL, 16: 11022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez N, Kintzer E, List J, Lypson M, Grochowalski JH, Marantz PR, and Gonzalez CM 2021. ‘Implicit Bias Recognition and Management: Tailored Instruction for Faculty’, J Natl Med Assoc [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross PT, Kumagai AK, Joiner TA, and Lypson ML 2011. ‘Using film in multicultural and social justice faculty development: scenes from Crash’, The Journal of continuing education in the health professions, 31: 188–95. [DOI] [PubMed] [Google Scholar]
- Russell Jesse, and Summers Alicia. 2013. ‘Reflective decision-making and foster care placements’, Psychology, Public Policy, and Law, 19: 127–36. [Google Scholar]
- Sabin JA, and Greenwald AG 2012. ‘The influence of implicit bias on treatment recommendations for 4 common pediatric conditions: pain, urinary tract infection, attention deficit hyperactivity disorder, and asthma’, Am J Public Health, 102: 988–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabin JA, Rivara FP, and Greenwald AG 2008. ‘Physician implicit attitudes and stereotypes about race and quality of medical care’, Med Care, 46: 678–85. [DOI] [PubMed] [Google Scholar]
- Sandoval RS, Afolabi T, Said J, Dunleavy S, Chatterjee A, and Olveczky D 2020. ‘Building a Tool Kit for Medical and Dental Students: Addressing Microaggressions and Discrimination on the Wards’, MedEdPORTAL, 16: 10893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schultz PL, and Baker J 2017. ‘Teaching Strategies to Increase Nursing Student Acceptance and Management of Unconscious Bias’, J Nurs Educ, 56: 692–96. [DOI] [PubMed] [Google Scholar]
- Sherman MD, Ricco J, Nelson SC, Nezhad SJ, and Prasad S 2019. ‘Implicit Bias Training in a Residency Program: Aiming for Enduring Effects’, Fam Med, 51: 677–81. [DOI] [PubMed] [Google Scholar]
- Shields Stephanie A., Zawadzki Matthew J., and Johnson R. Neill. 2011. ‘The impact of the Workshop Activity for Gender Equity Simulation in the Academy (WAGES–Academic) in demonstrating cumulative effects of gender bias’, Journal of Diversity in Higher Education, 4: 120–29. [Google Scholar]
- Song AY, Poythress EL, Bocchini CE, and Kass JS 2018. ‘Reorienting Orientation: Introducing the Social Determinants of Health to First-Year Medical Students’, MedEdPORTAL, 14: 10752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stepanikova I 2012. ‘Racial-ethnic biases, time pressure, and medical decisions’, J Health Soc Behav, 53: 329–43. [DOI] [PubMed] [Google Scholar]
- Sukhera J, Miller K, Scerbo C, Milne A, Lim R, and Watling C 2020. ‘Implicit Stigma Recognition and Management for Health Professionals’, Acad Psychiatry, 44: 59–63. [DOI] [PubMed] [Google Scholar]
- Sukhera J, Milne A, Teunissen PW, Lingard L, and Watling C 2018. ‘The Actual Versus Idealized Self: Exploring Responses to Feedback About Implicit Bias in Health Professionals’, Acad Med, 93: 623–29. [DOI] [PubMed] [Google Scholar]
- Sukhera J, and Watling C 2018. ‘A Framework for Integrating Implicit Bias Recognition Into Health Professions Education’, Acad Med, 93: 35–40. [DOI] [PubMed] [Google Scholar]
- Sukhera J, Watling CJ, and Gonzalez CM 2020. ‘Implicit Bias in Health Professions: From Recognition to Transformation’, Acad Med, 95: 717–23. [DOI] [PubMed] [Google Scholar]
- Sukhera J, Wodzinski M, Rehman M, and Gonzalez CM 2019. ‘The Implicit Association Test in health professions education: A meta-narrative review’, Perspect Med Educ, 8: 267–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teal CR, Gill AC, Green AR, and Crandall S 2012. ‘Helping medical learners recognise and manage unconscious bias toward certain patient groups’, Medical Education, 46: 80–8. [DOI] [PubMed] [Google Scholar]
- Teal CR, Shada RE, Gill AC, Thompson BM, Fruge E, Villarreal GB, and Haidet P 2010. ‘When best intentions aren’t enough: helping medical students develop strategies for managing bias about patients’, Journal of general internal medicine, 25 Suppl 2: S115–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teall AM, Graham M, Jenkins N, Ali A, Pryba J, and Overcash J 2019. ‘Faculty Perceptions of Engaging Students in Active Learning to Address Implicit Bias Using Videos Exemplifying the Prenatal Visit of a Lesbian Couple’, J Transcult Nurs: 1043659619828109. [DOI] [PubMed] [Google Scholar]
- Thomas A, Lubarsky S, Varpio L, Durning SJ, and Young ME 2020. ‘Scoping reviews in health professions education: challenges, considerations and lessons learned about epistemology and methodology’, Advances in health sciences education : theory and practice, 25: 989–1002. [DOI] [PubMed] [Google Scholar]
- Thomas Patricia A., Kern David E., Hughes Mark T., and Chen Belinda Y. 2016. Curriculum development for medical education: A six-step approach (Johns Hopkins University Press: Baltimore, MD: ). [Google Scholar]
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tuncalp O, and Straus SE 2018. ‘PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation’, Ann Intern Med, 169: 467–73. [DOI] [PubMed] [Google Scholar]
- Van Schalkwyk SC, Hafler J, Brewer TF, Maley MA, Margolis C, McNamee L, Meyer I, Peluso MJ, Schmutz AM, Spak JM, Davies D, and Initiative Bellagio Global Health Education. 2019. ‘Transformative learning as pedagogy for the health professions: a scoping review’, Med Educ, 53: 547–58. [DOI] [PubMed] [Google Scholar]
- White AA 3rd, Logghe HJ, Goodenough DA, Barnes LL, Hallward A, Allen IM, Green DW, Krupat E, and Llerena-Quinn R 2018. ‘Self-Awareness and Cultural Identity as an Effort to Reduce Bias in Medicine’, J Racial Ethn Health Disparities, 5: 34–49. [DOI] [PubMed] [Google Scholar]
- Wijayatunga NN, Kim Y, Butsch WS, and Dhurandhar EJ 2019. ‘The effects of a teaching intervention on weight bias among kinesiology undergraduate students’, Int J Obes (Lond) [DOI] [PubMed] [Google Scholar]
- World Health Organization. 2021. ‘Social Determinants of Health’, Accessed November 11, 2021. https://www.who.int/social_determinants/en/.
- Wu D, Saint-Hilaire L, Pineda A, Hessler D, Saba G, Salazar R, and Olayiwola JN 2019. ‘The Efficacy of an Antioppression Curriculum for Health Professionals’, Fam Med, 51: 22–30. [DOI] [PubMed] [Google Scholar]
- Zeidan AJ, Khatri UG, Aysola J, Shofer FS, Mamtani M, Scott KR, Conlon LW, and Lopez BL 2019. ‘Implicit Bias Education and Emergency Medicine Training: Step One? Awareness’, AEM Educ Train, 3: 81–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeidan A, Tiballi A, Woodward M, and Di Bartolo IM 2019. ‘Targeting Implicit Bias in Medicine: Lessons from Art and Archaeology’, The western journal of emergency medicine, 21: 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zestcott CA, Blair IV, and Stone J 2016. ‘Examining the Presence, Consequences, and Reduction of Implicit Bias in Health Care: A Narrative Review’, Group Process Intergroup Relat, 19: 528–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


