Abstract
Background and Objectives
Raising dementia awareness is essential for building a dementia-friendly community. However, existing studies have underexplored the effects of virtual reality (VR) dementia educational programs for the general public on enhancing positive attitude toward dementia. This study aimed to examine the effectiveness of a VR dementia-friendly educational program called the Drive for Dementia Readiness Inside Virtual Reality (DRIVE) program to improve attitude toward dementia of the general public.
Research Design and Methods
A two-arm randomized controlled trial was conducted. Eligibility criteria for participants included being 16 years and older in Japan and having no professional license in healthcare and social care. We randomized individuals to attend a multielement VR dementia-friendly educational program (intervention), including simulation, VR films, short films, lectures, and discussions or a lecture-based program (control). Data were collected 3 times, including at baseline, postintervention, and 3-month follow-up. The primary outcome was attitude toward dementia. The secondary outcomes were intention of helping behavior for people living with dementia and knowledge of dementia.
Results
We recruited 157 community residents, among whom 130 were included in the analysis. Although the mean changes in attitude score were not significantly different between the groups (Hedge’s g = 0.26), the intention of helping behavior score was significantly higher in the intervention group (g = 0.49).
Discussion and Implication
The DRIVE, a VR-based multielement dementia-friendly educational intervention, was shown as a promising tool for significantly affecting the intention of helping behavior for people living with dementia to establish dementia-friendly communities.
Clinical Trials Registration Number
UMIN000044901
Keywords: Attitude, Dementia-friendly, Education, Helping behavior, Virtual reality
Dementia is a general term used to describe symptoms that result in cognitive impairment due to organic brain damage. The number of community-dwelling people living with dementia has been increasing globally owing to population aging—there is an expected increase to grow from 57 million in 2019 to 153 million in 2050 (GBD 2019 Dementia Forecasting Collaborators, 2022). Approximately 50% of people aged 60 years in Japan were estimated to be at risk of developing some type of dementia during their lifetime, experiencing specific symptoms such as memory loss and communication difficulties (Yoshida et al., 2020).
In 2017, World Health Organization recognized “dementia awareness and friendliness” as one of the most prioritized action areas in public health, emphasizing the importance of nation-level initiatives to build a dementia-friendly community (DFC; Alzheimer’s Disease International, 2020b; World Health Organization, 2017; World Health Organization & Alzheimer’s Disease International, 2012). Dementia-friendly community is defined as “a place or culture in which people living with dementia and their carers are empowered, supported, and included in society, understand their rights, and recognize their full potential” (Alzheimer’s Disease International, 2020a). Educational approaches for raising dementia awareness are effective in constructing DFCs (Herrmann et al., 2018; Phillipson et al., 2019).
In Japan, the National Dementia Policy Framework was established to foster dementia awareness and promote DFCs in 2019 (Ministry of Health, Labor, and Welfare, 2019). Prior to this, in 2007, the country rolled out a nationwide lecture-style dementia awareness-raising initiative called “Dementia Supporter Training” to assist Japanese community residents in acquiring accurate knowledge of dementia (Alzheimer’s Disease International, 2020a; Community-Based Co-Operation Policy-Alliance of Local Governments, 2020). However, it is still unclear what effect this program has on increasing helping behaviors for people living with dementia (Kim et al., 2011).
Virtual reality (VR) technology in dementia education has received considerable scholarly attention in recent years. VR can induce a sense of presence in the virtual environment through electronic images and sounds that enable us to take someone else’s perspective (Herrera et al., 2018). It can help us understand one’s feelings in a short time. VR has effects on generating prosocial behavior (Nelson et al., 2020; Rosenberg et al., 2013). VR has been widely introduced in dementia education to understand symptoms of dementia, targeting various participants such as healthcare students and caregivers (Adefila et al., 2016; Gilmartin-Thomas et al., 2018; Stargatt et al., 2021; Wijma et al., 2018).
In previous research involving community residents, VR-based dementia educational programs improved attitude toward dementia (Sari et al., 2020) and empathy (Papadopoulos et al., 2021). However, existing studies suffer from following three limitations: (1) no intervention study with a control group and an adequate sample size was conducted, (2) no theoretical framework was used in the development of programs, (3) no study clarified the long-term effects of the intervention (Hirt & Beer, 2020; Matsumoto et al., 2023). Furthermore, most of the previous VR-based dementia programs focus only on experiences of dementia symptoms (Sari et al., 2020). They are insufficient to experience the subjective emotions of people living with dementia to lead to helping behaviors. A VR-based dementia program focused on the subjective experience of people living with dementia to increase empathy (Papadopoulos et al., 2021). Therefore, to promote helping behaviors for people living with dementia, it is crucial to adopt a new approach that provides a first-person perspective experience of people living with dementia, including their life history, values, social relationships, and the difficulties associated with dementia symptoms.
In this study, we developed a new dementia-friendly educational program using VR technology for the purpose of gaining a first-person perspective into the lives of people living with dementia and enhancing positive attitudes toward dementia. The scenario of the VR program was designed to be realistic; using several scenes involve situations where people living with dementia experience some trouble in the community due to dementia symptoms, leading participants to empathize with them. As mere knowledge delivery is not effective in changing people’s helping behavior, we used the Instructional Design to promote active learning. Additionally, we employed educational materials such as short films to stimulate participants’ motivation to learn about dementia. This study aimed to examine the effect of the multielement dementia-friendly educational program using VR on the general public’s attitude toward dementia, intention of helping behavior, and knowledge of dementia to support people living with dementia in the community.
Method
Design
This study was named DRIVE (Drive for Dementia Readiness Inside Virtual Reality). The DRIVE study adopted a longitudinal, non-blind, parallel-arm randomized controlled trial (RCT) design. The participants were individually randomized to either the intervention group, receiving a VR-based dementia-friendly educational program, or the control group, receiving the classroom-style dementia training program.
All participants were provided with written documents about the study, and written informed consent was obtained from all the participants. The DRIVE study was approved by the university’s Research Ethics Committee (No. 2020348NI-(2)) and registered at the UMIN Clinical Trials Registry. The report on this study was in accordance with the CONSORT 2010 Statement (Schulz et al., 2010).
Sample and Setting
Participants were required to (1) be over 16 years old; (2) have never attended the Japanese dementia training program; (3) have no professional license in healthcare and social care; and (4) be fluent in Japanese.
We provided nine sessions (mean number of participants per session was 16.4 [range 6–22]) in eight districts in Nerima City, the Metropolitan area in Tokyo, from August to December 2021. The sampling design employed convenience sampling. For recruitment, we distributed program leaflets at community general support centers (CGSCs), local clinics, and public libraries. The CGSC is a Japanese public consultation support center that provides comprehensive support for older adults and their families, including healthcare, welfare, and long-term care services. The participants applied for this study via the Internet, e-mail, telephone, or facsimile.
Sample Size
For the sample size estimation, we set the power to 0.8 and a two-tailed alpha level of 0.05, and the effect size of Cohen’s d = 0.5 for the primary outcome, attitude toward dementia. This effect size was calculated based on previous studies (Igarashi et al., 2020; Sari et al., 2020). These studies used the same attitude scale (Kim & Kuroda, 2011) to evaluate a dementia-friendly educational program using gamification cards or VR experiences subjects among the community residents in Japan, similar to the current study sample. The estimated sample size was 61 participants for each group.
Randomization
Randomization was performed for each session at an individual level, with a 1:1 ratio. After finishing recruitment and fixing the list order, an allocation director who was not involved in the recruitment opened the predesigned allocation list. Only the allocation director was aware of the blocking specifications. The participants were not informed of their allocation until the commencement of the program.
Procedure
The intervention and control programs were conducted in two separate rooms in the same building. Participants responded to questionnaires three times, including a baseline before the intervention (T0), a postintervention (T1), and a 3-month follow-up questionnaire (T2) by mail.
Interventions
The DRIVE Study Group
A VR-based multielement dementia-friendly educational program was newly developed for this study. DRIVE takes 90 min and consists of five parts: (1) simulation, (2) short films, (3) VR films, (4) lectures, and (5) discussions. The core part of this dementia educational program is the VR film. The contents of short films and lectures were consistently developed based on the contents of VR films. The component of discussion is also overlapped with the VR films to reinforce the learning effects of the VR experience. Those five components were developed and integrated based on the principles of Instructional Design, including the Experimental Learning Model (Kolb, 1984), the First Principle of Instruction (Merrill, 2002), and the Seven Design Principles of Jasper (Cognition and Technology Group at Vanderbilt, 1992). The theory-based program development could promote participants’ active learning to understand dementia accurately and intend to offer helping behavior. The contents and duration are as follows (Table 1).
Table 1.
Overview of the VR Dementia-friendly Educational Program
| Module # | Content Details |
Time (min) |
|---|---|---|
| 1 | Simulation | 5 |
| Displaying a fictional situation in which people living with dementia is in trouble, participants discuss their opinions on how they react. | ||
| 2 | Short film (unfriendly scenario) | |
| Viewing a story about a female person living with dementia, participants contemplate her background and the responses of surrounding people. | 10 | |
| 3 | VR film (unfriendly scenario) | 5 |
| Participants experience a perspective of a female person living with dementia to feel her emotions and the responses of surrounding people. | ||
| 4 | Discussion (1) | 5 |
| Participants exchange their impressions after experiencing VR films and viewing short films with an unfriendly scenario. | ||
| 5 | Lecture (1) | 20 |
| A lecture provides relevant information on dementia (e.g., types, causes, symptoms, and prevention). | ||
| 6 | VR film (friendly scenario) | 5 |
| Participants learn good responses and perceive a positive emotional change in people living with dementia through a comparison between the scenarios. | ||
| 7 | Short film (friendly scenario) | 10 |
| Participants find the differences in emotions of people living with dementia and surrounding people’s responses between the two scenarios. | ||
| 8 | Lecture (2) | 15 |
| A lecture provides relevant information (e.g., treatment, public service, and correct communication) by linking to VR and short films. | ||
| 9 | Discussion (2) | 15 |
| Participants take part in a role-playing game allocated to the short films’ characters and discuss how to support people living with dementia in the community and cooperate with other characters from their own positions. |
Notes: VR = virtual reality.
All the program components were developed and integrated based on the principle of Instructional Design.
Simulation
Participants joined a group simulation game (Igarashi et al., 2020). They are given a fictional situation in which a person living with dementia is in trouble, and they are instructed to think about whether they would offer help or not. They then discussed the situation and how they would or would not offer help. This part was developed as an ice-breaking and stimulating activity to start thinking about how they would help people living with dementia.
Short films
A short film was shown about an older woman who may have dementia. The film covered her life history, values, and relationships with her family and community members. There are two parallel scenarios with unfriendly and friendly communications, presented in that order. Unfriendly communication entails “poor” involvement practices that may cause distress in people living with dementia when interacting with participants and includes denying their words and actions without considering dementia symptoms. Friendly communication refers to “good” involvement practices that ensure people living with dementia feel comfortable during interactions and include listening attentively to and accepting the opinions of people living with dementia. The contrast between the two scenarios would allow the participants to experience the differences in the main character’s emotions subjectively. The purpose was for participants to learn the appropriate way to communicate with people living with dementia naturally. The scenarios were created based on interviews with people living with dementia and their families, reviewing articles, and advice from researchers who have expertise on dementia care. We used a screen to show the film like a movie theater.
VR films
Two 5-min VR films were shown. Each VR film was composed of a series of five scenes in the short film that were captured from a first-person view of an older female person living with dementia (the main character). Similar to the short films, the VR films had two scenarios with friendly and unfriendly communication to help participants learn person-centered communication with people living with dementia by comparing the two communication styles. In each scene, the participants experienced her perspective in symptoms-related situations regarding dementia. The five scenes in the VR were: (1) memory loss/comprehension (having tea with her friends at a café and being unable to catch up with the chatting), (2) impaired judgment (being unable to unlock the door of a restroom), (3) memory loss (forgetting the name of an acquaintance she met on the street), (4) disorientation (getting lost on the way to home), and (5) disorientation (getting yelled at by her son for getting lost).VR films’ 360-dimensional videos were filmed by a VR camera of insta360 OneX2 (Insta360, Co., Ltd., Shenzhen, China). Head-mounted displays (HMDs) were used for Pico G2 4K (Pico Technology Co., Ltd., Beijing, China) to view the VR films. Using a wireless playback system, the application software called “Showtime VR” (Showtime VR Sp. z o.o., Warszawa, Poland) was used so that up to 10 people could experience the VR films simultaneously.
To ensure the sense of presence as people living with dementia, HMDs and disposable earphones were used for the VR experience by blocking visual and auditory information from the outside. A simultaneous wireless playback system for the VR films was introduced so that all participants would start and finish the VR films synchronized and share their impressions immediately after the VR experience. Before the VR experience, participants were instructed on how to use the HMDs and the risks of VR experiences (e.g., VR motion sickness). To guarantee a smooth VR experience, the research staff supported the participants in wearing the HMDs and addressed any potential technical problems that may arise.
Considering the potential side effects of psychological distress due to viewing the unfriendly scenario, the participants were informed in advance that they could stop watching VR at any time and asked if they experienced any distress after every VR film session. Moreover, a preliminary study conducted on a total of 10 healthcare and social care professionals confirmed that there were no adverse effects during or after the VR experiences using the same VR films used within the DRIVE study.
Lectures
The lectures were developed and abridged from the Japanese lecture-style Dementia Supporter Training program, which includes the same contents as the lecture of the control group. It includes types of dementia, causes, symptoms, prevention, diagnosis, treatment, local consultation service in the community, appropriate communication, and the role of the Dementia Supporters. The researcher, a qualified instructor of the Dementia Supporter Training program, explained the symptoms of dementia and good communication with people living with dementia by linking the film and VR scenarios.
Discussions
The program contained two discussion periods. Discussions were held among the participants for 5–10 min. These discussions aim to promote participants’ active learning to understand dementia deeply. In the first discussion, participants exchanged their impressions after the unfriendly short film and VR film. In the second discussion, each participant plays a role in the film: a person living with dementia (the main character), a family member (her son), a friend, a community member, and a store clerk. Participants think about how they could offer help to the person living with dementia from their role and discuss how they would cooperate with other characters.
Control group
The control group received the 60–90 min classroom-style Dementia Supporter Training program, using the standardized textbook and DVD published in Japan. The Dementia Supporter Training program is government-led and constitutes the most common teaching material in Japan for the general public to learn about dementia. Its contents included fundamental knowledge of dementia, the same as the intervention group’s lecture. The official instructors of local healthcare professionals at CGSCs delivered the program to the control group. The participants in the control group, if wished, could experience VR films after the postintervention (T1) survey.
Measures
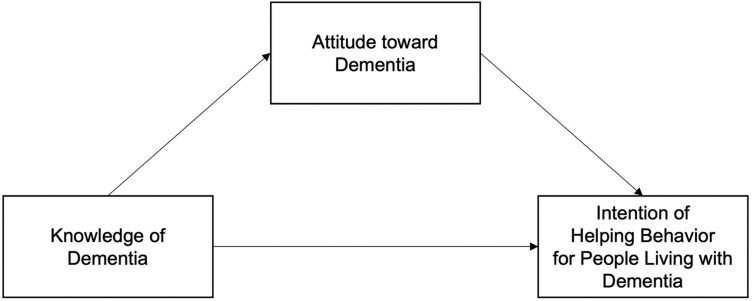
Dementia-friendly initiatives aim to facilitate helping behaviors for people living with dementia through educational interventions. In this regard, it is crucial to clarify whether knowledge and attitude lead to helping behavior. Previous studies have identified attitudes toward dementia that mediate the relationship between knowledge of dementia and intention of helping behavior for people living with dementia (Lane & Yu, 2020; Li et al., 2023; Matsumoto et al., 2022). These studies were developed using the Theory of Planned Behavior (Ajzen, 1991) or the bystander effect theory (Latané & Darley, 1970) as a theoretical rationale. However, there are limited intervention studies to empirically examine the relationship between the attitude associated with knowledge and the intention of helping behavior, specifically based on VR education.
We applied Lane & Yu (2020) and Matsumoto et al.’s (2022) models as a theoretical framework for setting the outcomes in this study. This model includes three concepts that contribute to developing DFCs: knowledge of dementia, attitude toward dementia, and intention of helping behavior for people living with dementia (Figure 1). In this study, this model was substantiated based on two hypotheses: (1) gaining greater knowledge of dementia directly facilitates helping intention for people living with dementia; (2) attitude was a mediate factor in relation to knowledge, which represents a reasonable factor in formulating intention of helping behavior. Thus, we hypothesized that if knowledge and attitude improve, intention should also improve.
Figure 1.
Theoretical framework of the study.
The primary outcome is the Attitude toward Dementia scale (Kim & Kuroda, 2011; Supplementary Appendix 1). Attitude toward dementia consists of positive and negative perceptions of dementia. Attitude is commonly measured as a primary outcome in dementia-friendly education (Gilmartin-Thomas et al., 2018; Kim et al., 2011; Phillipson et al., 2019; Sari et al., 2020; Stargatt et al., 2021). This scale has 14 items with a 4-point Likert scale ranging from 1 (disagree) to 4 (agree). It consists of four subscales: tolerance (five items), refusal (four items), feeling of distance (three items), and affinity (two items). Tolerance was measured as the positive perception toward dementia using the following: “I do not mind more interaction with people living with dementia in daily life”; refusal was measured as the negative perception toward dementia using the following: “I would like to avoid interacting with people living with dementia as much as possible”; feeling of distance was measured as the negative perception toward dementia using the following: “If a family member has dementia, I would be concerned about what people around me would think”; and affinity was measured as the positive perception toward dementia using the following: “If people living with dementia need some help, I would offer it without hesitation” The total score ranged from 14 to 56, with a higher score indicating a more positive attitude. The construct validity and content validity of this scale have been established (Kim & Kuroda, 2011). The Cronbach’s alphas for tolerance, refusal, feeling of distance, affinity, and total score in this study were 0.71, 0.64, 0.60, 0.74, and 0.81, respectively.
One of the secondary outcomes was intention of helping behavior for people living with dementia, which was measured using an original scale based on a previous study (Matsumoto et al., 2022; Supplementary Appendix 2). It was used as an alternative indicator of actual helping behavior by employing a common situation that all the participants could respond to. We measured intention of helping behavior using four vignettes when the general public met a person living with dementia who would need help, extracted from previous interviews with people living with dementia and their families. An example of the vignette is “During your job as a clerk in a supermarket, you see an older woman buy bananas multiple times. She also bought many bananas the previous day.” For each vignette, the participants were asked about intention of helping behavior (“You will help people living with dementia”). The question for each vignette was rated on a 4-point Likert scale from 1 (disagree) to 4 (agree); each question of the four vignettes was summed up. Intention scores ranged from 4 to 16, with a higher score indicating a higher degree of helping behaviors. The construct validity and face validity of this scale have been established (Matsumoto et al., 2022). The Cronbach’s alphas for intention of helping behavior in this study were 0.78.
Knowledge of dementia was another secondary outcome, which was measured using 10 items of the Dementia-Related Knowledge Scale (Mikami et al., 2017), which assesses the knowledge of the symptoms and treatments of dementia. Although this knowledge scale asks respondents to answer with a 4-point Likert scale from disagree to agree, we modified the answer options to “yes” and “no” so that correct answers were clearer. This change ensured that participants’ knowledge was accurately measured. The correct answers for each question scored 1 point; the total score ranged from 0 to 10, with a higher score indicating a higher level of knowledge of dementia. The construct validity of the original scale has been established (Mikami et al., 2017).
We collected demographic attributes, including age, gender, living arrangement, involvement with people living with dementia, and experience of helping and caregiving for older adults (including people living with dementia). The participants also answered questions about their experience of attending dementia lectures and whether they knew the CGSC.
Statistical Analysis
After calculating descriptive statistics, chi-squared test and Student’s t test were used to examine the homogeneity of the baseline participants’ characteristics between the two groups. The main analysis was to compare the changes in the primary and secondary outcomes from T0 to T1 between the intervention and control groups using Student’s t test and estimate the effect size (Hedges’ g). Small effect sizes range from 0 to 0.17, moderate effect sizes from 0.18 to 0.43, and large effect sizes from 0.44 to 0.84 (Brydges, 2019). As post hoc analysis, the changes from T0 to T1 scores in each group were examined using paired t test. All participants who completed the T0 and T1 surveys were included in the analyses. To compare the scores among three-time points (T0–T2) in the intervention group, a one-way repeated measures analysis of variance was performed. Complete case analysis was used to handle missing values. For sensitivity analysis to confirm the consistency of results in the main analysis, analysis of covariance (ANCOVA) was conducted for the primary outcome. The following variables were used as adjustment variables: involvement with people living with dementia, experience of helping older adults, experience of caregiving older adults, and knowing CGSC. We also conducted subgroup analyses based on age, gender, experience of helping older adults, and experience of caregiving older adults to examine the robustness of the results. Statistical analysis was performed using IBM SPSS Statistics version 28.0 for Windows (IBM Corp., Armonk, NY, USA).
Results
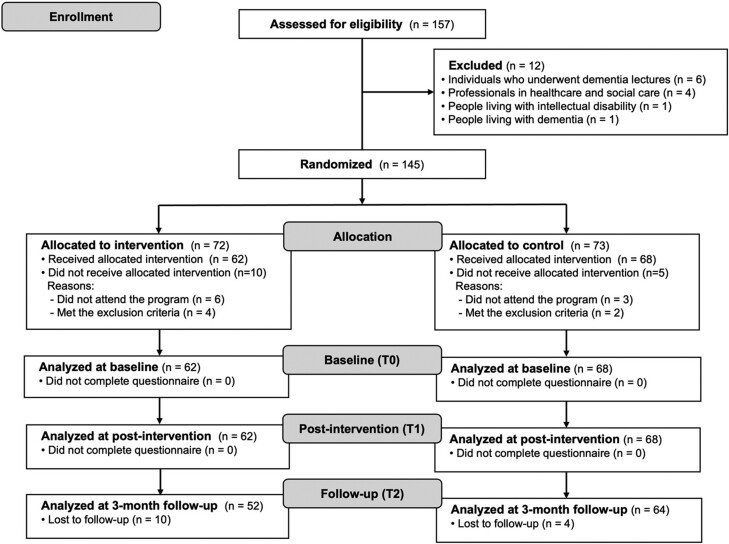
Characteristics of the Participants
A total of 157 participants were assessed for eligibility in the study (Figure 2). Twelve of them were excluded because they did not meet the inclusion criteria; six people previously attended the dementia training program, four people had a professional license in healthcare or social care, and two people had an intellectual disability or dementia who could not answer a questionnaire. A total of 145 participants were randomized and allocated to the intervention or control groups. Of these, 15 participants were not included in the analysis: nine were absent from the program, and six met the exclusion criteria (e.g., had experience attending the dementia training program and having licenses in healthcare/social care). A total of 116 people completed the study from T0 to T2 (80.0%). A total of 14 participants dropped out of the T2 survey because the questionnaire was not returned by the due date.
Figure 2.
Flow diagram of the study.
Table 2 presents the baseline characteristics of the participants. The mean age (standard deviation [SD]) of the participants was 63.9 (SD = 13.6) years old. Most participants were female (71%), 29% lived with a spouse only, and 65% had experience helping older adults. There were no significant differences in participants’ characteristics and the scores of outcomes at the baseline survey (T0) between the intervention and control groups. None of the participants reported serious adverse events such as VR motion sickness after experiencing VR films. We measured the degree of VR motion sickness objectively by the Simulator Sickness Questionnaire and confirmed that it did not occur (Ito et al., 2023).
Table 2.
Baseline Characteristics of Participants
| Total (n = 130) |
Intervention (n = 62) |
Control (n = 68) |
||||||
|---|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | |||
| Mean | ± SD | Mean | ± SD | Mean | ± SD | p Value | ||
| Age | 63.9 | ± 13.6 | 62.1 | ± 14.6 | 65.6 | ± 12.5 | .142 | b |
| Gender, female | 92 | (70.8) | 46 | (74.2) | 46 | (67.6) | .412 | a |
| Living arrangement | ||||||||
| Living alone | 30 | (23.3) | 10 | (16.4) | 20 | (29.4) | .217 | a |
| Living with spouse only | 37 | (28.7) | 19 | (31.1) | 18 | (26.5) | ||
| Others | 62 | (48.1) | 32 | (52.5) | 30 | (44.1) | ||
| Involvement with people living with dementia | ||||||||
| Continuous | 23 | (18.3) | 6 | (10.2) | 17 | (25.4) | .087 | a |
| Once or short-term | 28 | (22.2) | 14 | (23.7) | 14 | (20.9) | ||
| Never | 75 | (59.5) | 39 | (66.1) | 36 | (53.7) | ||
| Experience of helping older adults, yes | 84 | (65.1) | 43 | (70.5) | 41 | (60.3) | .225 | a |
| Experience of caregiving | ||||||||
| Yes | 65 | (50.4) | 32 | (52.5) | 33 | (48.5) | .656 | a |
| For people living with dementia | 47 | (36.2) | 22 | (35.5) | 25 | (36.8) | .358 | a |
| Experience of attending dementia lectures, yes | 15 | (11.6) | 4 | (6.5) | 11 | (16.4) | .078 | a |
| Knowing the CGSC, yes | 104 | (80.6) | 48 | (77.4) | 56 | (83.6) | .376 | a |
| Attitude | ||||||||
| Total score | 40.4 | ± 5.7 | 40.1 | ± 5.4 | 40.7 | ± 6.0 | .549 | b |
| Tolerance | 16.1 | ± 2.4 | 16.1 | ± 2.3 | 16.2 | ± 2.5 | .875 | b |
| Refusal | 9.9 | ± 1.9 | 9.7 | ± 2.0 | 10.2 | ± 1.8 | .154 | b |
| Feeling of distance | 8.0 | ± 2.0 | 8.1 | ± 1.8 | 8.0 | ± 2.2 | .783 | b |
| Affinity | 6.4 | ± 1.4 | 6.2 | ± 1.5 | 6.5 | ± 1.2 | .236 | b |
| Intention of helping behavior | 11.5 | ± 2.6 | 11.5 | ± 2.5 | 11.5 | ± 2.8 | .979 | b |
| Knowledge | 8.8 | ± 1.3 | 9.0 | ± 1.2 | 8.7 | ± 1.3 | .217 | b |
Note: a = chi-squared test; b = Student’s t test; CGSC = community general support center; SD = standard deviation.
Changes in Attitude Toward Dementia
There was no significant difference in the change of the total scores of the Attitude toward Dementia Scale between the two groups (p = .162, Hedge’s g = 0.26 [95% confidence interval (CI): −0.11–0.63]; Table 3). In the pre-and postintervention comparison, the attitude total score significantly improved after the intervention in the intervention group (Supplementary Appendix Table 1). In the comparison among the three-time points in the intervention group, the total score at T2 was significantly improved compared to T0 (p < .001, mean changes between two-time points (MC) = 3.3 [95% CI: 1.84–4.66]; Table 4).
Table 3.
Comparison of Changes in the Main Outcome Scores Between the Two Groups (T1–T0)
| Intervention | Control | |||||||
|---|---|---|---|---|---|---|---|---|
| (n = 62) | (n = 68) | |||||||
| Mean | (SD) | Mean | (SD) | p Value | g | LCL | UCL | |
| Attitude | ||||||||
| Total score | 3.7 | (4.5) | 2.6 | (4.0) | .162 | 0.26 | −0.11 | 0.63 |
| Tolerance | 1.4 | (2.0) | 0.8 | (2.2) | .140 | 0.27 | −0.09 | 0.62 |
| Refusal | 1.2 | (2.0) | 0.7 | (1.6) | .132 | 0.27 | −0.08 | 0.62 |
| Feeling of distance | 0.6 | (1.5) | 0.8 | (1.6) | .510 | −0.12 | −0.46 | 0.23 |
| Affinity | 0.5 | (1.2) | 0.4 | (1.0) | .634 | 0.08 | −0.26 | 0.43 |
| Intention of helping behavior | 2.3 | (2.4) | 1.1 | (2.5) | .006 * | 0.49 | 0.14 | 0.85 |
| Knowledge | −0.2 | (1.3) | 0.3 | (1.1) | .042 * | −0.41 | −0.80 | −0.01 |
Notes: LCL = 95% lower confidence limit of corrected Hedge’s g; SD = standard deviation; UCL = 95% upper confidence limit of corrected Hedge’s g.
* p < .05. Effect sizes were calculated using Student’s t test by corrected Hedge’s g (small: from 0 to 0.17, moderate: from 0.18 to 0.43, large: from 0.44 to 0.84).
Table 4.
Changes in the Outcome Scores at Three-Time Points in the Intervention Group (n = 52)
| T0 | T1 | T2 | T1–T0 | T2–T1 | T2–T0 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) |
Mean (SD) |
Mean (SD) |
p Value | MC | p Value | LCL | UCL | MC | p Value | LCL | UCL | MC | p Value | LCL | UCL | |
| Attitude | ||||||||||||||||
| Total score | 40.0 (5.1) | 44.1 (4.5) | 43.3 (4.8) | <.001 | 4.1 | .001 | 2.44 | 5.65 | −0.7 | .276 | −1.93 | 0.35 | 3.3 | .001 | 1.84 | 4.66 |
| Tolerance | 16.2 (2.4) | 17.6 (2.2) | 16.7 (2.1) | <.001 | 1.4 | .001 | 0.72 | 2.18 | −0.9 | .005 | −1.57 | −0.23 | 0.5 | .276 | −0.24 | 1.34 |
| Refusal | 9.4 (2.0) | 10.8 (1.9) | 10.6 (2.0) | <.001 | 1.4 | .001 | 0.65 | 2.08 | −0.2 | 1.000 | −0.85 | 0.48 | 1.2 | .001 | 0.62 | 1.75 |
| Feeling of distance | 8.0 (1.7) | 8.6 (2.0) | 8.8 (1.4) | .003 | 0.6 | .031 | 0.04 | 1.11 | 0.2 | .975 | −0.37 | 0.87 | 0.8 | .005 | 0.22 | 1.44 |
| Affinity | 6.3 (1.4) | 6.8 (1.0) | 6.9 (1.1) | <.001 | 0.5 | .001 | 0.20 | 0.96 | 0.1 | 1.000 | −0.25 | 0.44 | 0.5 | .001 | 0.34 | 1.01 |
| Intention | 11.6 (2.4) | 13.8 (2.0) | 12.9 (2.3) | <.001 | 2.2 | .001 | 1.40 | 3.00 | −0.9 | .011 | −1.67 | −0.17 | 2.2 | .001 | 0.50 | 2.05 |
| Knowledge | 9.0 (1.2) | 8.7 (1.3) | 9.0 (1.1) | .206 | −0.3 | .750 | −0.81 | 0.29 | 0.3 | .209 | −0.11 | 0.72 | 0.0 | 1.000 | −0.34 | 0.44 |
Notes: LCL = 95% lower confidence limit of the mean change of the outcome score; MC = mean changes between two-time points; SD = standard deviation; UCL = 95% upper confidence limit of the mean change of the outcome score.
Bold characters indicate p < .05. Difference at three-time points tested by repeated measures one-way ANOVA. Difference between two-time points tested by Bonferroni’s multiple comparisons.
Changes in Intention of Helping Behavior for People Living With Dementia
The intervention group had significantly greater changes in the intention scores than the control group (p = .006, g = 0.49 [95% CI: 0.14–0.85]; Table 3). The intention scores significantly improved after the intervention in the intervention group (Supplementary Appendix Table 1). In the comparison among the three-time points in the intervention group, the intention score at T2 was significantly improved compared to T0 (p = .001, MC = 2.2 [95% CI: 0.50–2.05]; Table 4).
Changes in Knowledge of Dementia
There was a significantly larger change in knowledge scores in the control group than in the intervention group (p = .042, g = −0.41 [95% CI: −0.80 to −0.01]; Table 3). There was no significant pre-post change in the knowledge score in each group (Supplementary Appendix Table 1). In the comparison among the three-time points in the intervention group, the knowledge score at T2 was not significantly improved compared to T0 (Table 4).
Sensitivity Analysis
For the primary outcome, attitude toward dementia, a sensitivity analysis using ANCOVA was conducted (Supplementary Appendix Table 2). There was no significant difference between the two groups after adjusting for covariates. This result was consistent with that of Student’s t test (primary analysis). In the subgroup analysis, for females and those who had experience helping older adults, the intervention group had significantly greater changes in the total attitude scores than the control group (g = 0.58, g = 0.52, respectively; Supplementary Appendix Table 3).
Discussion
This study examined the effectiveness of a VR-based multielement dementia-friendly educational program applying an RCT. Although there was no significant difference in improving attitude toward dementia between the two groups, the improvement in intention of helping behaviors for people living with dementia was significantly greater in the intervention group than in the control group. To the best of our knowledge, this study is the first RCT to examine the effects of a dementia-friendly educational program using VR on the general public based on a theoretical model. The current results could be significant insights for designing a new strategy for evidence-based dementia-friendly educational approaches targeted to the general public for promoting helping behaviors for people living with dementia.
Although the DRIVE program demonstrated a moderate effect size compared to the lecture-style program, no significant difference was observed in the improvement of attitude toward dementia between the two groups (T0–T1). The reason we could not detect the superiority of the DRIVE program compared to the control group may be the lack of sample size calculation. We could not include an estimation of the effect size of the control group’s intervention. Previous studies reported that VR-based dementia educational interventions had significant effects on enhancing positive attitude toward dementia (Gilmartin-Thomas et al., 2018; Sari et al., 2020; Stargatt et al., 2021). Our results suggest that the VR-based dementia educational program could contribute to improving attitude toward dementia. To reinforce the effectiveness of the intervention, it is desirable to calculate the effect size considering the control group’s intervention.
The “Tolerance” subscale, which improved more in the VR-based program (g = 0.27), included items regarding the positive perception of communicating with people living with dementia. The multisensory VR dementia educational program for healthcare students improved the subdomain “comfort” score of the Dementia Attitudes Scale (DAS), which evaluated the person’s comfortability in interacting with people living with dementia (Gilmartin-Thomas et al., 2018). Thus, a positive experience of virtual communication with people living with dementia might further improve the participants’ positive perception of interacting with people living with dementia rather than the lecture-based educational program.
One of the secondary outcomes, intention of helping behaviors for people living with dementia, significantly improved more in the intervention group than the control group. However, knowledge of dementia, another secondary outcome, was significantly more improved in the control group. Lane and Yu’s model (2020), which hypothesizes that knowledge can affect intention of helping behavior directly and be indirectly mediated by attitude, was not supported by our results. VR creates a simulation of a body in space and can be replaced with virtual bodies; consequently, it enables the individual to become someone else temporarily, leading to feeling empathy (Herrera et al., 2018). Empathy is categorized into cognitive and affective (emotional) empathy while observing someone else’s experience in a specific situation (Gladstein, 1983). It promotes prosocial behavior, such as helping behavior (Rosenberg et al., 2013; Slater et al., 2019). Slater et al. (2019) reported that VR stimulates strong “emotional empathy.” Thus, this VR-based educational program could potentially induce emotional empathy in the participants directly without mediating knowledge. Consequently, it elicits a positive attitude toward dementia and intention of helping behaviors. This finding can offer valuable insights into developing a new theoretical framework to promote helping behaviors by working directly on attitude without passing through knowledge using VR intervention.
The improvement in knowledge of dementia was significantly larger in the control group than in the intervention group. The lecture-style program could be more effective in imparting knowledge to participants regarding symptoms of dementia. On the contrary, knowledge of the experiences of people living with dementia, including their psychological distress and desirable communication, which participants learn through the DRIVE program, was not included in the current scale.
In the intervention group, significantly higher scores of attitude toward dementia were observed at T2 than at T0. We confirmed the long-term effects of the VR-based dementia educational program on participants’ attitude toward dementia. Regarding the changes in subscale scores, scores for “Refusal,” “Sense of Distance,” and “Affinity” were significantly higher and sustained at T2 than at T0. “Refusal” and “Sense of Distance” express negative perceptions toward dementia, a concept similar to stigma. The current study showed the long-term effects of decreased negative perception of dementia at 3 months. On the contrary, the sustainability of anti-stigma educational interventions is doubtful (Mehta et al., 2015). Further robust research is needed to examine the long-term effects of VR interventions.
In subgroup analysis as sensitivity analysis, the total attitude scores of females and those who had experience of helping older adults were significantly higher in the intervention group. An existing study similarly reported the sex difference in empathy occurrence favoring females (Eisenberg & Lennon, 1983). Regarding the helping experience, Rosenberg et al. (2013) demonstrated that people who experienced helping others in VR space increased their helping behavior. From the current findings, positive perceptions of dementia may be more effectively reinforced through VR simulation in the case of those who have experience interacting with and helping people living with dementia.
There are two major points regarding the uniqueness of the VR experience, effectiveness, and efficiency. First, participants can gain vivid experiences from other people’s perspectives, such as virtually “being there” which is known as the term “presence” from early research using a VR environment (Zelter, 1992). Secondly, participants can accurately understand the characteristics of the experiences of people living with dementia through VR, even for as short a time as 10 min. According to Anderson’s model of cognitive skill acquisition, where knowledge is a model that can be transformed from a declarative level to a procedural level through experience (Anderson, 1982), even short experiences via VR is expected to effectively function to translate declarative knowledge into a form that can be observed as direct procedure. That is, VR can provide a high efficiency of learning in gaining a precise understanding of people living with a disease or disability. A previous study using 2D audiovisual materials for nursing students demonstrated a small effect size (r = 0.27) in the change of the Attitude toward Dementia Scale (Suzuki et al., 2023). The DRIVE program had a large effect size (g = 0.82, Supplementary Appendix Table 1) using the same scale. Thus, VR experience could have the potential advantage of a high learning effect compared to the traditional approach. The results implying the use of HMDs having positive effects in learning generally follow other various studies outcomes using HMDs for learning purposes in various research fields (Lasse et al., 2018).
The current study findings may offer useful implications for public health policy, potentially informing the development of new strategies to disseminate and implement evidence-based approaches for enhancing dementia awareness. Specifically, this study stresses the importance of focusing on stimulating the attitude for the improvement in intention of helping behavior. Not only lecture-based materials but also combining VR first-person experience and audiovisual materials could be helpful in increasing dementia awareness. Further studies on how to approach the uninterested population; effectively provide tailored educational programs for individuals from diverse cultural backgrounds; and reflect the wishes and voices of people living with dementia for dementia educational materials are warranted. If helping behavior for people living with dementia is spread among the general public, it could potentially contribute to reducing the stigma toward dementia, improving healthcare access for early diagnosis of dementia, and promoting social inclusion for people living with dementia and their carers to live well in their communities.
This study has several limitations. First, the generalizability of the study is limited. The participants were relatively old (mean age, 63.9 years old). Participants’ characteristics, who had strong interests in dementia, might have affected the external validity of the study. Second, the sample size was insufficient to show the dominance of the VR-based intervention. Third, this study examined the effects of the combined intervention program, including simulation, short films, VR films, lectures, and discussions. Further research is crucial to identify the impact of each interventional component on improving the study outcomes. Additionally, this VR intervention requires investment in terms of both money for purchasing VR equipment and time to attend the 90-min program. Although there are certainly challenges to the dissemination of VR, the VR market size is projected to grow globally in education and healthcare (Fortune Business Insights, 2023). VR will be easier to procure in the future than now, and users will become more familiar with VR operations. Moreover, the missing data on participants who dropped out could have influenced the findings regarding the long-term effects of the intervention. Finally, we did not measure actual helping behavior. Future studies should measure actual helping behavior as an intervention outcome.
Despite the above limitations, while the VR-based dementia-friendly educational program did not significantly improve attitude toward dementia compared to the lecture-style dementia training program, the VR educational program significantly improved intention of helping behavior than the lecture-based program. Attitude toward dementia was improved after the intervention in the intervention group. The results suggest that a VR-based, multielement dementia-friendly educational program could foster an empathetic attitude and intention of helping behaviors toward people living with dementia in the general public, encouraging dementia awareness and consequently contributing to establishing DFCs.
Supplementary Material
Data Availability
The conditions of our ethics approval do not allow us to publicly share the current study data with nonmembers of the research group. The study protocol has been preregistered in the UMIN Clinical Trials Registry (https://center6.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000051276).
Contributor Information
Haruno Suzuki, Department of Physiological Nursing, School of Nursing, University of California, San Francisco, San Francisco, California, USA; Department of Gerontological Home Care and Long-term Care Nursing, Graduate School of Medicine, The University of Tokyo, Tokyo, Tokyo, Japan.
Ayumi Igarashi, Department of Gerontological Home Care and Long-term Care Nursing, Graduate School of Medicine, The University of Tokyo, Tokyo, Tokyo, Japan.
Hiroshige Matsumoto, Department of Community Health Nursing, Graduate School of Medicine, The University of Tokyo, Tokyo, Tokyo, Japan.
Haruna Kugai, Global Nursing Research Center, Graduate School of Medicine, The University of Tokyo, Tokyo, Tokyo, Japan.
Manami Takaoka, Department of Gerontological Home Care and Long-term Care Nursing, Graduate School of Medicine, The University of Tokyo, Tokyo, Tokyo, Japan.
Mariko Sakka, Faculty of Medicine, University of Tsukuba, Tsukuba, Ibaraki, Japan.
Kenichiro Ito, Information Technology Center, The University of Tokyo, Tokyo, Tokyo, Japan.
Yasuhiro Hagiwara, Department of Biostatistics, Graduate School of Medicine, The University of Tokyo, Tokyo, Tokyo, Japan.
Noriko Yamamoto-Mitani, Department of Gerontological Home Care and Long-term Care Nursing, Graduate School of Medicine, The University of Tokyo, Tokyo, Tokyo, Japan.
Funding
This study was supported by a grant from the Japan Society for the Promotion of Science KAKENHI [19H03956].
Conflict of Interest
None.
References
- Adefila, A., Graham, S., Clouder, L., Bluteau, P., & Ball, S. (2016). myShoes—The future of experiential dementia training?. Journal of Mental Health Training, Education and Practice, 11(2), 91–101. 10.1108/jmhtep-10-2015-0048 [DOI] [Google Scholar]
- Ajzen, I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50(2), 179–211. 10.1016/0749-5978(91)90020-t [DOI] [Google Scholar]
- Alzheimer’s Disease International. (2020a). Dementia friendly communities. https://www.alzint.org/what-we-do/policy/dementia-friendly-communities/. Accessed 18 September 2024. [Google Scholar]
- Alzheimer’s Disease International. (2020b). From plan to Impact III—Maintaining dementia as a priority in unprecedented times. https://www.alzint.org/resource/from-plan-to-impact-iii/. Accessed 18 September 2024. [Google Scholar]
- Anderson, J. R. (1982). Acquisition of cognitive skill. Psychological Review, 89(4), 369–406. 10.1037//0033-295x.89.4.369 [DOI] [Google Scholar]
- Brydges, C. R. (2019). Effect size guidelines, sample size calculations, and statistical power in gerontology. Innovation in Aging, 3(4), igz036. 10.1093/geroni/igz036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cognition and Technology Group at Vanderbilt (1992). The Jasper experiment: An exploration of issues in learning and instructional design. Educational Technology, Research and Development, 40(1), 65–80. 10.1007/BF02296707 [DOI] [Google Scholar]
- Community-Based Co-Operation Policy-Alliance of Local Governments. (2020). Research reports on support measures for people living with dementia and their families by the dementia supporter training program(in Japanese). https://jichitai-unit.ne.jp/network/group-overview.html. Accessed 18 September 2024. [Google Scholar]
- Eisenberg, N., & Lennon, R. (1983). Sex differences in empathy and related capacities. Psychological Bulletin, 94(1), 100–131. 10.1037//0033-2909.94.1.100 [DOI] [Google Scholar]
- Fortune Business Insights. (2023). Virtual reality market size, share & COVID-19 impact analysis, by component (hardware, software, and content), by device type (head mounted display (HMD), VR simulator, VR classes, treadmills & haptic gloves, and others), by industry (gaming, entertainment, automotive, retail, healthcare, education, aerospace & defense, manufacturing, and others) and regional forecast, 2023-2030. https://www.fortunebusinessinsights.com/industry-reports/virtual-reality-market-101378. Accessed 18 September 2024. [Google Scholar]
- GBD 2019 Dementia Forecasting Collaborators (2022). Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: An analysis for the Global Burden of Disease Study 2019. Lancet Public Health, 7(2), e105–e125. 10.1016/S2468-2667(21)00249-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilmartin-Thomas, J. F. -M., McNeil, J., Powell, A., Malone, D. T., Wolfe, R., Larson, I. C., O’Reilly, C. L., Kirkpatrick, C. M., Kipen, E., Petrovich, T., & Bell, J. S. (2018). Impact of a virtual dementia experience on medical and pharmacy students’ knowledge and attitudes toward people with dementia: A Controlled Study. Journal of Alzheimer's Disease, 62(2), 867–876. 10.3233/JAD-170982 [DOI] [PubMed] [Google Scholar]
- Gladstein, G. A. (1983). Understanding empathy: Integrating counseling, developmental, and social psychology perspectives. Journal of Counseling Psychology, 30(4), 467–482. 10.1037//0022-0167.30.4.467 [DOI] [Google Scholar]
- Herrera, F., Bailenson, J., Weisz, E., Ogle, E., & Zaki, J. (2018). Building long-term empathy: A large-scale comparison of traditional and virtual reality perspective-taking. PLoS One, 13(10), e0204494. 10.1371/journal.pone.0204494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrmann, L. K., Welter, E., Leverenz, J., Lerner, A. J., Udelson, N., Kanetsky, C., & Sajatovic, M. (2018). A systematic review of dementia-related stigma research: Can we move the stigma dial? American Journal of Geriatric Psychiatry, 26(3), 316–331. 10.1016/j.jagp.2017.09.006 [DOI] [PubMed] [Google Scholar]
- Hirt, J., & Beer, T. (2020). Use and impact of virtual reality simulation in dementia care education: A scoping review. Nurse Education Today, 84, 104207. 10.1016/j.nedt.2019.104207 [DOI] [PubMed] [Google Scholar]
- Igarashi, A., Matsumoto, H., Takaoka, M., Kugai, H., Suzuki, M., & Yamamoto-Mitani, N. (2020). Educational program for promoting collaboration between community care professionals and convenience stores. Journal of Applied Gerontology, 39(7), 760–769. 10.1177/0733464819871878 [DOI] [PubMed] [Google Scholar]
- Ito, K., Suzuki, H., Kugai, H., Takaoka, M., Matsumoto, H., Sakka, M., Yamamoto-Mitani, N., & Igarashi, A. (2023). HMD in general public for training: Case study of standardized dementia-friendly initiative in Japan. 2023 IEEE International Conference on Consumer Electronics (ICCE), 1–3. e518. 10.1109/ICCE56470.2023.10043560 [DOI]
- Kim, K., & Kuroda, K. (2011). Factors related to attitudes toward people with dementia: Development attitude toward dementia scale and dementia knowledge scale (in Japanese). Bulletin of Social Medicine, 28(1), 43–55. [Google Scholar]
- Kim, K., Zheng, X., Masui, K., & Kuroda, K. (2011). A follow up study of attitudes towards dementia among persons who received an educational lecture (in Japanese). Journal of Japanese Society for Dementia Care, 10(1), 88–96. [Google Scholar]
- Kolb, D. A. (1984). Experiential learning: Experience as the source of learning and development. Prentice Hall. [Google Scholar]
- Lane, A. P., & Yu, F. C. H. (2020). Person-centered attitudes mediate the association between dementia knowledge and help-giving intentions in Singapore. International Psychogeriatrics, 32(3), 413–414. 10.1017/S1041610219000796 [DOI] [PubMed] [Google Scholar]
- Lasse, J., & Flemming, K. (2018). A review of the use of virtual reality head-mounted displays in education and training. Education and Information Technologies, 23(4), 1515–1529. 10.1007/s10639-017-9676-0 [DOI] [Google Scholar]
- Latané, B., & Darley, J. M. (1970). The unresponsive bystander: Why doesn’t he help? Appleton-Century-Crofts. [Google Scholar]
- Li, Y. -T., Bai, J. -X., He, J. -M., Yang, S. -W., & Huang, H. -L. (2023). The mediating role of attitudes towards dementia on the relationship between dementia knowledge and behaviors towards persons with dementia: A cross-sectional study. Journal of Multidisciplinary Healthcare, 16, 4213–4225. 10.2147/JMDH.S443189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsumoto, H., Igarashi, A., Sakka, M., Takaoka, M., Kugai, H., Ito, K., & Yamamoto-Mitani, N. (2022). A two-step model for encouraging the general public to exhibit helping behaviors toward people living with dementia. Innovation in Aging, 6(3), igac023. 10.1093/geroni/igac023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsumoto, H., Maeda, A., Igarashi, A., Weller, C., & Yamamoto-Mitani, N. (2023). Dementia education and training for the general public: A scoping review. Gerontology & Geriatrics Education, 44(2), 154–184. 10.1080/02701960.2021.1999938 [DOI] [PubMed] [Google Scholar]
- Mehta, N., Clement, S., Marcus, E., Stona, A. -C., Bezborodovs, N., Evans-Lacko, S., Palacios, J., Docherty, M., Barley, E., Rose, D., Koschorke, M., Shidhaye, R., Henderson, C., & Thornicroft, G. (2015). Evidence for effective interventions to reduce mental health-related stigma and discrimination in the medium and long term: Systematic review. British Journal of Psychiatry, 207(5), 377–384. 10.1192/bjp.bp.114.151944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrill, M. D. (2002). First principles of instruction. Educational Technology, Research and Development, 50(3), 43–59. 10.1007/bf02505024 [DOI] [Google Scholar]
- Mikami, M., Nakao, R., Horikawa, R., Sugiyama, K., Sawada, Y., Kirino, M., & Takemoto, Y. (2017). Developing a scale to assess dementia-related knowledge among local residents (in Japanese). Bulletin of Social Medicine, 34(2), 35–44. [Google Scholar]
- Ministry of Health, Labor, and Welfare. (2019). National Dementia Policy Framework (in Japanese). https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000076236_00002.html. Accessed 18 September 2024. [Google Scholar]
- Nelson, K. M., Anggraini, E., & Schlüter, A. (2020). Virtual reality as a tool for environmental conservation and fundraising. PLoS One, 15(4), e0223631. 10.1371/journal.pone.0223631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papadopoulos, C., Kenning, G., Bennett, J., Kuchelmeister, V., Ginnivan, N., & Neidorf, M. (2021). A visit with Viv: Empathising with a digital human character embodying the lived experiences of dementia. Dementia (London, England), 20(7), 2462–2477. 10.1177/1471301221998888 [DOI] [PubMed] [Google Scholar]
- Phillipson, L., Hall, D., Cridland, E., Fleming, R., Brennan-Horley, C., Guggisberg, N., Frost, D., & Hasan, H. (2019). Involvement of people with dementia in raising awareness and changing attitudes in a dementia friendly community pilot project. Dementia (London, England), 18(7–8), 2679–2694. 10.1177/1471301218754455 [DOI] [PubMed] [Google Scholar]
- Rosenberg, R. S., Baughman, S. L., & Bailenson, J. N. (2013). Virtual superheroes: Using superpowers in virtual reality to encourage prosocial behavior. PLoS One, 8(1), e55003. 10.1371/journal.pone.0055003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sari, D. W., Igarashi, A., Takaoka, M., Yamahana, R., Noguchi-Watanabe, M., Teramoto, C., & Yamamoto-Mitani, N. (2020). Virtual reality program to develop dementia-friendly communities in Japan. Australasian Journal on Ageing, 39(3), e352–e359. 10.1111/ajag.12797 [DOI] [PubMed] [Google Scholar]
- Schulz, K. F., Altman, D. G., Moher, D., & CONSORT, G. (2010). CONSORT 2010 statement: Updated guidelines for reporting parallel group randomized trials. British Medical Journal, 340, c332. 10.1136/bmj.c332 [DOI] [PubMed] [Google Scholar]
- Slater, P., Hasson, F., Gillen, P., Gallen, A., & Parlour, R. (2019). Virtual simulation training: Imaged experience of dementia. International Journal of Older People Nursing, 14(3), e12243. 10.1111/opn.12243 [DOI] [PubMed] [Google Scholar]
- Stargatt, J., Bhar, S., Petrovich, T., Bhowmik, J., Sykes, D., & Burns, K. (2021). The effects of virtual reality-based education on empathy and understanding of the physical environment for dementia care workers in Australia: A controlled study. Journal of Alzheimer's Disease, 84(3), 1247–1257. 10.3233/JAD-210723 [DOI] [PubMed] [Google Scholar]
- Suzuki, H., Igarashi, A., Sakai, S., Sakka, M., Takaoka, M., Matsumoto, H., Ito, K., Kugai, H., & Yamamoto-Mitani, N. (2023). Effects of a dementia educational program to experience the first-person perspective among nursing students: A prospective observational study (in Japanese). Japanese Society for Dementia Care, 22(2), 393–403. [Google Scholar]
- Wijma, E. M., Veerbeek, M. A., Prins, M., Pot, A. M., & Willemse, B. M. (2018). A virtual reality intervention to improve the understanding and empathy for people with dementia in informal caregivers: Results of a pilot study. Aging & Mental Health, 22(9), 1115–1123. 10.1080/13607863.2017.1348470 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2017). Global action plan on the public health response to dementia 2017–2025. https://www.who.int/publications/i/item/global-action-plan-on-the-public-health-response-to-dementia-2017---2025. Accessed 18 September 2024. [Google Scholar]
- World Health Organization & Alzheimer’s Disease International. (2012). Dementia: A public health priority. https://apps.who.int/iris/handle/10665/75263. Accessed 18 September 2024. [Google Scholar]
- Yoshida, D., Ohara, T., Hata, J., Shibata, M., Hirakawa, Y., Honda, T., Furuta, Y., Oishi, E., Sakata, S., Kanba, S., Kitazono, T., & Ninomiya, T. (2020). Lifetime cumulative incidence of dementia in a community-dwelling elderly population in Japan. Neurology, 95(5), e508–e518. 10.1212/WNL.0000000000009917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zelter, D. (1992). Autonomy, interaction, and presence. Presence: Teleoperators and Virtual Environments, 1(1), 127–132. 10.1162/pres.1992.1.1.127 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.