Abstract
Objective:
Müllerian duct Anomalies (MDA) are rare but well-known entity. Most of the MDAs are asymptomatic, and are undiagnosed; However, MDAs may present with infertility, bad obstetric history or other associated anomalies which further fuel the suspicion of MDAs. This case series comprises of 6 problem-pregnancies, their course and management.
Case report:
Primigravida with bicornuate uterus presented at 23 weeks with hand prolapse, requiring hysterotomy. A G2P1L0 presented at 36 weeks with footling presentation, managed by a preterm CS. Primigravida presented at 24 weeks with Didelphys uterus with partial longitudinal vaginal septum, needing hysterotomy. Primigravida at 37 weeks presented with abruptio placenta, managed by CS.
Conclusion:
Though the incidence of MDAs is low, but the outcomes can be rather distressing for both mother and fetus. Once identified, adverse outcomes must be anticipated and prepared for, and these are best managed at tertiary hospitals. Apart from counselling we should also meticulously document, improve awareness regarding MDAs and their outcomes. Early diagnosis and timely management can hit the jackpot in terms of pregnancy outcomes.
Keywords: Conduplicato Corpore, Couvelaire Uterus, Hysterotomy, Müllerian Duct Anomalies, Obstetric Outcomes
Introduction
Müllerian duct develops into female reproductive tract, which further forms a functional reproductive-tract. Altercations of development lead to Müllerian Duct Anomalies (MDA), which are recently classified by ASRM (American Society for Reproductive Medicine). The overall incidence of MDA is about 7% in general population, and as high as 18% in women with recurrent pregnancy losses (1).
Most of the MDAs are quiescent, usually diagnosed following adverse pregnancy outcomes. MDAs are associated with malpresentation, preterm deliveries, preterm premature rupture of membranes, fetal growth restriction, low birth weight, operative deliveries, other associated anomalies, abnormal placentation, and hypertensive disorders of pregnancy (2–6).
Recent boost of favourable outcomes among MDAs have been attributable to surgical-corrections and Assisted Reproductive Techniques (ART). Despite the progress, the outcomes are compromised either on maternal or fetal aspect, as there are anatomical limitations. However, MDAs are detectable and amenable to enhance pregnancy outcomes. This study is an attempt to describe variable presentations and course of pregnancy outcomes among MDAs, at Tertiary Hospital.
Case report
Case 1: A 27-year-old, Primigravida at 23 weeks with married life of 10months, presented with complaints of leaking per-vaginum for 7 hours, intermittent pain abdomen since 4 hours and mass per-vaginum since 30 minutes.
Patient was booked at a Primary Health Centre (PHC); first ANC-visit at 2 months of pregnancy, without any radiological confirmation of pregnancy. Experienced quickening at around 4months of gestation. On examination, per-abdomen, uterus corresponding to 20weeks size, fetal heart not localized. On Local examination, cyanosed hand prolapsed through introitus. On per-vaginum examination, cervix 6cm dilated, absent membranes no liquor draining, fetal arm and hand in vagina with pulseless cord prolapse. On ultrasonography; single uterine gestation corresponding to 21–22 weeks, with absent cardiac activity, Placenta anterior upper segment and nil liquor.
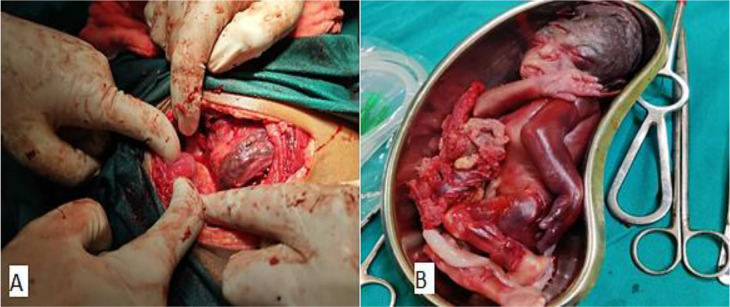
Emergency hysterotomy, failure to expel following 4 hours of Injection Oxytocin: During the operation bicornuate uterus was noted, abnormal vasculature was noted along the anterior surface of the uterus, and dead male abortus of 490 grams was extracted (Figure 1).
Figure 1:
Bicornuate Uterus with tortuous vessels (A) and stillborn fetus (B)
Case 2: A 26-year-old, G2P1L0 at 36 weeks 2 days of gestation with Breech Presentation, with married life of 4years, presented with complaints of pain abdomen since 3hours.
Patient visited and then followed up at our centre from third trimester. Patient has had history of midtrimester loss 3 years ago, presented with pain abdomen at 28 weeks of gestation and expelled a grossly normal female fetus of 660grams. Following which patient was evaluated and detected to have Müllerian anomaly –likely Unicornuate. Patient had rather uneventful trimesters during current pregnancy.
On examination, stable vitals, per-abdomen, uterus corresponds to 36weeks, breech presentation with 2uterine contractions lasting for 10 seconds over a period of 10minutes, and fetal heart sounds localized. On per-speculum, no leak noted. On pervaginum examination, cervix soft, posterior, 2 cm dilated with cervical length of 2.5 cm, intact membranes and presenting part high up.
Emergency CS (Cesarean Section) was done, intraoperatively, alive fetus presented as footling breech and delivered by breech extraction. Left Unicornuate uterus associated with Atrophic Uterine remnant noted (Figure 2).
Figure 2:

Unicornuate Uterus
Case 3: A 21-year-old female presented to Outpatient Department with complaints of nausea, vomiting since 2 months, and abdominal discomfort since 1 week. On evaluation, patient was amenorrhoeic since 4months, urine-pregnancy-kit was positive. On Abdominal examination, uterus corresponds to 24weeks gestation.
On per speculum examination, a thick septum noted, either side of the septum cervices were noted. Ultrasonography; single live intrauterine gestation corresponding to 27weeks, with Lumbosacral open spina bifida, Gross Hydrocephalus and Arnold Chiari II malformation, placenta-fundal and posterior, Müllerian Anomaly could not be assessed due to advanced gestational age.
Medical termination of pregnancy with Tab Mifepristone 200mg was given orally, 36hours later Tab Misoprostol 400mcg was given 4hourly for 4doses per vaginally. Hysterotomy was performed as medical management failed, intraoperatively two non-communicating uterine cavities with intrauterine pregnancy in left cornua, an incision was made and extracted dead-macerated male fetus of 520 grams, with tobacco-coloured liquor. Fallopian tubes found to arise from respective uterine cavities. Patient was diagnosed as Didelphys uterus with partial longitudinal vaginal septum (Figure 3).
Figure 3:

Didelphys uterus
Case 4: A 24-year-old Primigravida at 37 weeks 6days of gestation in cephalic presentation, presented to Labour room with complaints of pain abdomen since 4hours associated with spotting per Vaginum since 1hour.
Patient had regular ANC visits at our centre from 24weeks of gestation, prior regular visits at PHC; uneventful trimesters. On examination, maternal tachycardia, and elevated blood pressure of 140/90 mmHg were noted. On per abdominal examination, uterus corresponds to term size, tense, 2 contractions lasting for 15seconds in 10minutes. On cardiotocography, fetal tachycardia (170–175 bpm) was noted. Per speculum examination revealed excessive show, on per Vaginum examination cervix was soft, 2–3cm dilated, 1cm long, vertex at −3station with intact membranes. Under aseptic precautions Artificial rupture of membranes was done and bloodstained liquor noted.
Emergency CS done, with Indication: Fetal Distress. Baby delivered by cephalic presentation. Retroplacental clots of 100grams and discoloration over the anterior uterine wall suggestive of Couvelaire uterus following Abruptio placenta. Estimated blood loss of 1200ml. Combined Bicornuate Septate Uterus noted, Bilateral Fallopian tubes and ovaries grossly normal (Figure 4).
Figure 4:
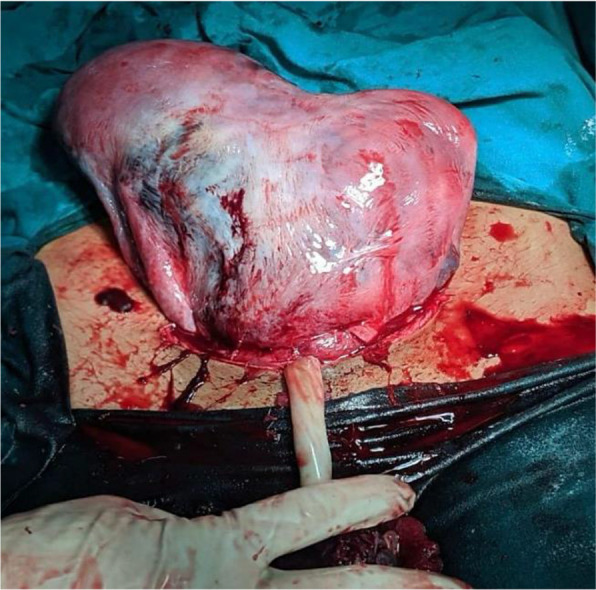
Couvelaire-Bicornuate Uterus
Case 5: A 26-year-old G2P1L1 at 37 weeks 5days of gestation in Breech Presentation in latent phase of labour with previous CS, with married life of 4 years presented with abdominal pain since 3 hours.
Patient has had uneventful trimesters during current pregnancy. History of Previous term CS, Indication: Breech presentation. Patient vitally stable, on examination, uterus corresponding to term size, breech presentation with 2uterine contractions lasting for 20seconds over a period of 10 minutes, Pfannenstiel scar noted, scar tenderness elicited. On per speculum, no leak noted. On per vaginal examination, cervix soft, mid-position, 4cm dilated with cervical length of 1.5cm, intact membranes and presenting part at –3station, pelvis gynecoid.
Emergency CS done, Indication Previous CS with Scar Tenderness. Intraoperatively, Lower uterine segment thinned out with scar dehiscence. Alive fetus presented as frank breech, delivered by Breech extraction. Combined Bicornuate Septate Uterus noted, Bilateral Fallopian tubes and ovaries grossly normal (Figure 5).
Figure 5:
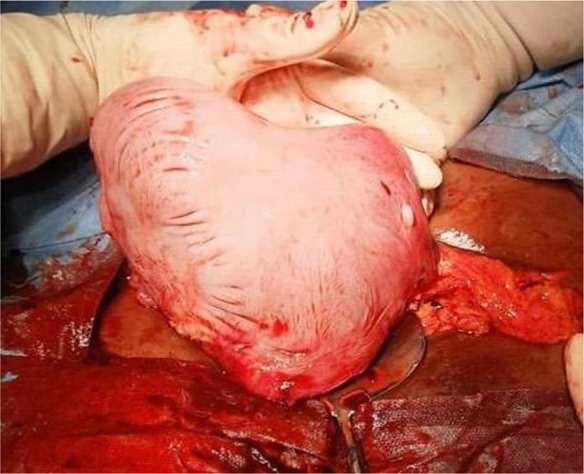
Bicornuate Uterus
Case 6: A 32-year-old Primigravida at 8weeks of gestation, with married life of 5years, presented with complaints of pain abdomen since 2days, associated with bleeding per-vaginum.
Patient was a case of Primary Infertility, both partners were prescribed treatment whose details were unavailable, following which patient was detected to be pregnant. Vitals were stable; uterus not palpable. Per-speculum: The os was open and bleeding was noted. Ultrasonography; multiple gestation sacs were noted in right horn of the bicornuate uterus. Patient was given tablet Misoprostol 1600 mcg per-vaginum in divided doses.
Products of conception were expelled. Two weeks later, ultrasonography revealed no retained products (Figure 6).
Figure 6:
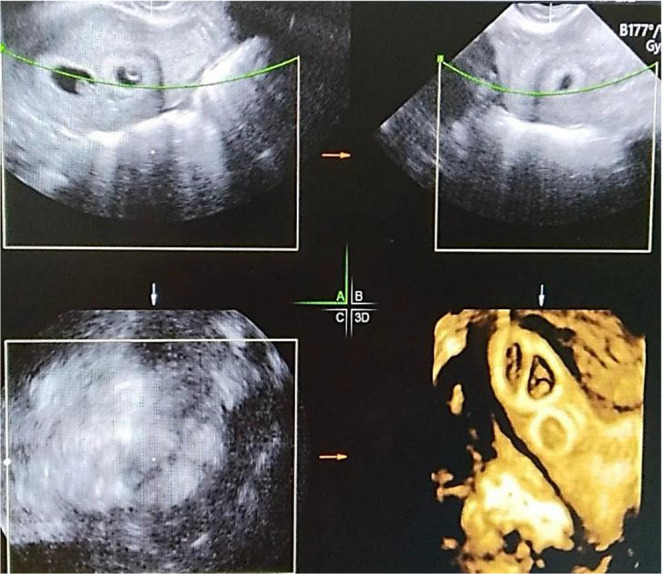
Ultrasonography of Bicornuate uterus with multiple gestation
Discussion
Majority of data concerning MDAs and their outcomes are documented as case reports or retrospective studies, whose results are inconclusive. With an overall incidence of 7% MDAs is a major section of patients who need assistance for an uneventful reproductive life (1).
About 60% second trimester losses, are attributed to MDAs (7). Most of these deliver vaginally among both normal or MDAs, the need for surgical intervention is unlikely, as large pelvis makes way for the small fetus by conduplicato corpore (8). Though, medical management is preferred mode for second trimester termination, uterine anomalies may hinder the usual flow of events averting vaginal delivery. R Tyler Hillman et al, Savita Singhal et al, and Lazenby et al performed hysterotomies for second trimester fetal demise and failed medical management, similar to our cases (9–11).
Si Wang et al have documented higher incidence of preterm labour, abruptio placenta, malpresentation and need for CS among MDAs (12). Ann Dekalo et al have conducted histopathological studies of placentas among MDAs, these had higher incidence of maternal vascular malperfusion (13). Likewise, the adverse outcomes noted in our study are attributed to MDAs. There also have been instances where pregnancies have delivered at term uneventfully, dismissing the fact all MDAs have poor outcomes.
Offer Erez et al conducted population-based study, to determine the success of vaginal birth after CS, among MDA and normal uterus, they concluded more than 60% of MDAs had repeated CS for malpresentations, preterm labour and PPROM (14). D J Ravasia et al, reported 8% of uterine rupture among MDAs attempting vaginal birth after CS, which is significantly high as compared to less than 1% among anatomically normal uterus (15–17). Hence it might be wise to avoid Trial of labour after CS among MDAs, signs of dehiscence manifest in early-labor as seen in our case.
The use of ART in Müllerian agenesis is well defined, however among MDAs is not well delineated. This is a grey-zone, where both the patient and the clinician fly partially blind. Many studies have studied infertility among MDAs but ART and their complications or outcomes have not been well known, thus making MDAs an essential consideration prior to any mode of ART.
Conclusion
The reproductive outcomes of these anomalies range from normal uncomplicated pregnancy to infertility or abnormal labour. The adverse outcome includes, preterm labour, malpresentation, mid-trimester loss, cervical incompetence, infertility.
The mere presence of these anomalies do not mandate surgical management or adverse outcome; however, these outcomes are guarded hence we as clinicians must we wary and watchful. Nevertheless, we as practitioner must anticipate and be vigilant to improve maternal mortality and morbidity. These are few of the many MDAs that have presented and were managed in our institutes, the alarming factor being many of these patients were completely unaware and unprepared for the consequences. This is where we as obstetricians have step-up to the task of managing and counselling the patients.
Acknowledgments
The authors appreciate the co-operation of Department of Obstetrics and Gynecology, KS Hedge Medical Academy, Mangalore & Department of Obstetrics and Gynecology, Vydehi Institute of Medical Sciences, Bangalore, Karnataka.
Footnotes
Conflict of Interests
Authors declare no conflict of interests.
Notes:
Citation: Koya S, Radhakrishnan K, Ravikumar S, Kaul S, Desai A. Anticipating and Executing off Beat Pregnancies in Müllerian Duct Anomalies: A Case Series. J Family Reprod Health 2024; 18(3): 200-5.
References
- 1.Bhagavath B, Ellie G, Griffiths KM, Winter T, Alur-Gupta S, Richardson C, et al. Uterine Malformations: An Update of Diagnosis, Management, and Outcomes. Obstet Gynecol Surv. 2017;72(6):377–392. [DOI] [PubMed] [Google Scholar]
- 2.Green LK, Harris RE. Uterine anomalies. Frequency of diagnosis and associated obstetric complications. Obstet Gynecol. 1976;47(4):427–9. [PubMed] [Google Scholar]
- 3.Engku-Husna EI, Nik-Ahmad-Zuky NL, Muhammad-Nashriq K. Müllerian duct anomalies with term pregnancy: a case report. J Med Case Rep. 2020;14(1):209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Joshi B, Kaushal A, Suri V, Gainder S, Choudhary N, Jamwal S, et al. Prevalence and Pregnancy Outcome of Mullerian Anomalies in Infertile Women: A Retrospective Study. J Hum Reprod Sci. 2021;14(4):431–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cahen-Peretz A, Sheiner E, Friger M, Walfisch A. The association between Müllerian anomalies and perinatal outcome. J Matern Fetal Neonatal Med. 2019;32(1):51–57. [DOI] [PubMed] [Google Scholar]
- 6.Heinonen PK. Gestational hypertension and preeclampsia associated with unilateral renal agenesis in women with uterine malformations. Eur J Obstet Gynecol Reprod Biol. 2004;114(1):39–43. [DOI] [PubMed] [Google Scholar]
- 7.Żyła MM, Wilczyński J, Nowakowska-Głąb A, Maniecka-Bryła I, Nowakowska D. Pregnancy and Delivery in Women with Uterine Malformations. Adv Clin Exp Med. 2015;24(5):873–9. [DOI] [PubMed] [Google Scholar]
- 8.Williams. Williams Textbook of Obstetrics. 25nd ed. New York: McGraw-Hill, 2018. [Google Scholar]
- 9.Mettam GR, Adams LB. How to prepare an electronic version of your article. In: Jones BS, Smith RZ, editors. Introduction to the electronic age, New York: E-Publishing Inc; 2009, p. 281–304. [Google Scholar]
- 10.Hillman RT, Chin HG, Mody SK. Management of Second Trimester Fetal Demise in a Noncommunicating Uterine Horn. Case Rep Obstet Gynecol. 2015;2015:927037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Singhal S, Agarwal U, Sharma D, Sirohiwal D. Pregnancy in asymmetric blind hemicavity of Robert’s uterus--a previously unreported phenomenon. Eur J Obstet Gynecol Reprod Biol. 2003;107(1):93–5. [DOI] [PubMed] [Google Scholar]
- 12.Lazenby GB, Huang C, Rahall AM, Fogelson NS. Pregnancy termination via laparotomy in a woman with bicornuate uterus. Contraception. 2007;75(3):241–3. [DOI] [PubMed] [Google Scholar]
- 13.Wang S, Wang K, Hu Q, Liao H, Wang X, Yu H. Perinatal outcomes of women with Müllerian anomalies. Arch Gynecol Obstet. 2023;307(4):1209–1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dekalo A, Feldstein O, Tal D, Friedman M, Schreiber L, Barda G, et al. The association of placental histopathological lesions and adverse obstetric outcomes in patients with Müllerian anomalies. Placenta. 2022;122:23–28. [DOI] [PubMed] [Google Scholar]
- 15.Erez O, Dukler D, Novack L, Rozen A, Zolotnik L, Bashiri A, et al. Trial of labor and vaginal birth after cesarean section in patients with uterine Müllerian anomalies: a population-based study. Am J Obstet Gynecol. 2007;196(6):537.e1–11. [DOI] [PubMed] [Google Scholar]
- 16.Ravasia DJ, Brain PH, Pollard JK. Incidence of uterine rupture among women with müllerian duct anomalies who attempt vaginal birth after cesarean delivery. Am J Obstet Gynecol. 1999;181(4):877–81. [DOI] [PubMed] [Google Scholar]
- 17.Motomura K, Ganchimeg T, Nagata C, Ota E, Vogel JP, Betran AP, et al. Incidence and outcomes of uterine rupture among women with prior caesarean section: WHO Multicountry Survey on Maternal and Newborn Health. Sci Rep. 2017;7:44093. [DOI] [PMC free article] [PubMed] [Google Scholar]