Abstract
Background
Prior studies demonstrate that eliminating hepatitis C virus (HCV) in the United States (US) heavily depends on treating incarcerated persons. Knowing the scope of the carceral HCV epidemic by state will help guide national elimination efforts.
Methods
Between 2019 and 2023, all state prison systems received surveys requesting data on hepatitis C antibody and viremic prevalence. We supplemented survey information with publicly available HCV data to corroborate responses and fill in data gaps.
Results
Weighting HCV prevalence by state prison population size, we estimate that 15.2% of the US prison population is HCV seropositive and 8.7% is viremic; 54.9% of seropositive persons have detectable RNA. Applying prevalence estimates to the total prison population at year-end 2021, 91 090 persons with HCV infection resided in a state prison.
Conclusions
With updated and more complete HCV data from all 50 states, HCV prevalence in state prisons is nearly 9-fold higher than the US general population. The heterogeneity in HCV prevalence by state prison system may reflect variable exposure before arrest and/or differences in treatment availability during incarceration. Elimination of HCV in the country depends on addressing the carceral epidemic, and one of the first steps is understanding the size of the problem.
Keywords: prison, corrections, criminal legal system, hepatitis C virus, seroprevalence
More than 2 million people remain chronically infected with hepatitis C virus (HCV) in the United States (US) despite the availability of direct-acting antiviral agents for >10 years and a cure rate of >95% [1]. Recently, the Biden administration proposed a national HCV elimination initiative to dramatically expand access to HCV treatment and bring the US in line with the World Health Organization's goal of eliminating HCV as a public health threat by 2030 [2].
For the US, HCV elimination will heavily depend on treating persons in custody, both because of the high number of people incarcerated in the US [3] and high HCV exposure prior to incarceration [4]. In 2003, the Centers for Disease Control and Prevention estimated that the seroprevalence of HCV ranged from 16% to 41% in state prison systems, substantially higher than the 1% in the general population [1, 5]. In 3 previous national surveys of prisons that were conducted from 1998 through 2016, HCV seroprevalence was within this range [6–8]. However, surveys that focus on seroprevalence do not inform healthcare planners on the progress toward HCV elimination [9, 10]. Data on the prevalence of HCV viremia is needed to determine the current burden of chronic HCV infection in each state prison system to clarify what steps are needed to achieve national elimination goals.
The objective of this article is to determine the overall prevalence of HCV viremia, rather than just antibody seroprevalence, in state prisons. We sought data by surveying state prison systems between 2019 and 2023 and used publicly available HCV data to corroborate survey responses and fill in the data gaps due to unreturned surveys and other missing information.
METHODS
For our fourth national survey of US prison systems on HCV prevalence, we contacted the Correctional Leaders Association in 2019 to ask prison commissioners to pass a digital link to a survey that used the Qualtrics (Provo, Utah) survey platform to their Medical Director. A PDF version of the survey was also included (see Supplement 1). Respondents were informed that proceeding with the survey would imply consent to participate in the study. Our research team completed any necessary forms that individual states required to submit a data request. Several states required a copy of the report be submitted to them prior to publication. We did not ask for the name of the respondent, but Qualtrics records the Internet Protocol (IP) address of those who completed the surveys. We confirmed that the geographic location of the IP address corresponded to the location of the central offices of the state prison system and then stripped the IP address from further data tables. If a survey response was not yet received or if the response required further inquiry, the investigative team attempted to contact the statewide Medical Director directly from late 2019 to early 2020. We made additional efforts from June 2022 through July 2023 to obtain either an initial response to the survey or updated data. Investigators fielded questions from respondents if a survey item needed clarification. Based on the requirement of several state systems, after the initial submission of this manuscript, we emailed prison officials in each state a letter that included the prevalence data for their respective state and the body of this manuscript and asked for confirmation of the data used to estimate the prevalence of HCV infection in 2021. The Correctional Leaders Association distributed a table summarizing results to date in June 2023. We made corrections requested by state systems.
The survey first questioned whether the prison system performed routine, nontargeted, HCV screening. If so, we queried whether HCV screening included entrants to the prison system, a cross-section of all persons in prison, or both. We also asked for the numbers screened for HCV antibody and HCV viremia, how many were positive for each test, and the time period in which screening was conducted since 2014. A subsequent round of surveys was conducted in 2022. Questions were revised for systems that had provided prior replies.
We then accessed data on HCV seroprevalence and viremia in state prison systems from published, peer-reviewed literature, documents used in litigation, and gray literature to obtain additional data. We used these data to both corroborate and supplement survey responses as well as to obtain HCV prevalence data for states that did not respond to the survey. A review of the English literature was conducted on 16 January 2023, using PubMed, searching under the terms (((HCV OR hepatitis C) AND (prison OR jail) AND (prevalence OR seroprevalence) AND (United States or US)) AND “2013” [Date–Publication]: “3000” [Date–Publication])) [11]. We examined HCV-related data published by STAT News in 2022 that they received from state prison systems [12]. We also searched the Special Report on Hepatitis C in Prisons and Jails, maintained by the University of Michigan's Civil Rights Litigation Clearinghouse, which collects documents from large-scale civil rights lawsuits [13]. When available, we also reviewed data on state websites.
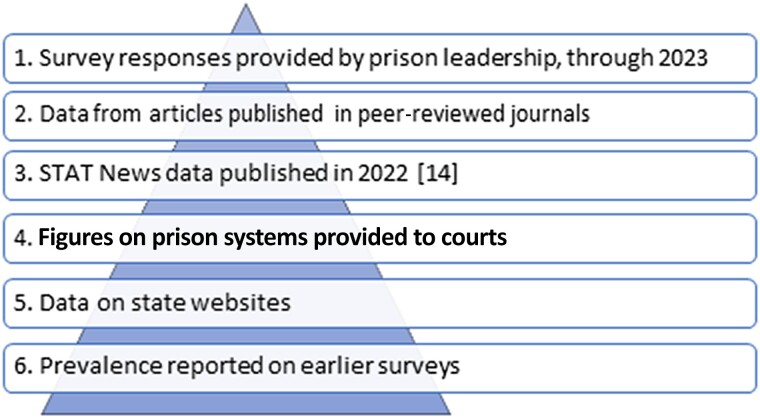
Preference regarding data sources roughly followed the hierarchy shown in Figure 1. Some states had >1 available data source. Categories of data used were not always mutually exclusive. In such cases, we preferentially chose prevalence figures based on the recency of data, consistency with historical values, and the methods of calculation used.
Figure 1.
Preferential order of data sources: hepatitis C virus prevalence in state prisons, United States.
For prison population size, we used the prison population data from year-end 2021 published by the Bureau of Justice Statistics (BJS) [14]. We calculated the number of cases of HCV infection in each state by multiplying the population size, the reported HCV seroprevalence (percentage with a positive HCV antibody), and the percentage with HCV viremia among those with antibodies. If the percentage of HCV antibody–positive individuals who were viremic was not available, we used a default value from the literature of 75% as it is expected that at least 25% of individuals have spontaneous clearance of the virus within a high-risk population, such as people who inject drugs [15]. If HCV prevalence data were known for both the cross-sectional population residing in the state facilities as well as those newly entering the system, we preferentially used the cross-sectional data as they are more stable over time. For the prison systems that could only provide a number of known positive cases after targeted or very limited testing, the seropositivity was calculated based on these numbers being the numerator; the total population was used as the denominator. In these rare instances, we note in Supplement 2 that the HCV prevalence estimate represents a basement estimate of the possible range. If HCV prevalence data were available for different time periods, we used the percentage available closest to 2021. When estimating the overall prevalence of chronic HCV in prison on the basis of absolute numbers reported, we multiplied the prevalence by the BJS year-end 2021 prison population data [14] to derive a weighted estimate of the prevalence of HCV antibodies and viremia on a single day in time, according to the method used previously [8]. We asked for longitudinal data and information on treatment, if available.
This project did not constitute human subjects research according to criteria of the Code of Federal Regulations, §45 CFR 46, incorporated in decision-making software developed by Emory University's Institutional Review Board.
RESULTS
Data on HCV testing and prevalence, of varying quality, were available from all 50 states (Table 1). Forty-seven state prison systems completed surveys, including 14 states that submitted subsequent updates of their data within the study period. Published articles were the main source for data in 2 states [16, 17] and corroborated data in other states [18, 19]. Data from a series of STAT News articles provided information for additional prison systems [12]. Summations of legal cases or papers filed in court contributed important information on HCV prevalence for 5 states.
Table 1.
Calculated Point Prevalence of Hepatitis C Virus Viremic Individuals in US Prison Systems by State, Using Population Figures From the Bureau of Justice Statistics for 31 December 2021a
| State | Year of Data Used for Rate | Data Source | Total Prison Population 2021, No.b | HCV Seroprevalence, % | Calculated No. HCV Antibody Positive | Percentage With HCV Viremia | Calculated No. HCV RNA Positive |
|---|---|---|---|---|---|---|---|
| Alabama | 2022 | 2 surveys | 25 032 | 13.2 | 3299 | 75c | 2474 |
| Alaskad | 2020 | 2 surveys | 4639 | 38.8 | 1799 | 63.2 | 1137 |
| Arizona | 2021 | Public reports [20] | 33 914 | 15.6 | 5292 | 75c | 3969 |
| Arkansas | 2023 | Survey | 17 022 | 13.4 | 2283 | 59.6 | 1361 |
| California | 2021 | 2 surveys | 101 441 | 26.2 | 26 527 | 27.9 | 7401 |
| Colorado | 2017 | Survey Lawsuit [21] |
15 865 | 12.6 | 2001 | 75c | 1501 |
| Connecticutd | 2015–2016 | Survey Lawsuit [22] |
9889 | 15.0 | 1478 | 77.7 | 1148 |
| Delawared | 2022 | Survey | 4810 | 12.9 | 622 | 75 | 467 |
| Florida | 2017–2019 | Survey STAT News |
80 417 | 11.6 | 9333 | 75c | 7000 |
| Georgia | 2019 | Survey Published paper [18] |
47 010 | 9.7 | 4569 | 62.5 | 2856 |
| Hawaii | 2022 | 2 surveys | 4102 | 13.4 | 548 | 74.3 | 407 |
| Idaho | 2021–2022 | Survey | 8907 | 32.7 | 2910 | 75c | 2183 |
| Illinois | 2022 | STAT News | 28 475 | 3.8 | 1068 | 75c | 800 |
| Indiana | 2021–2022 | Survey | 24 716 | 23.4 | 5791 | 56.6 | 3278 |
| Iowa | 2023 | 2 surveys | 8562 | 5.8 | 499 | 75c | 374 |
| Kansas | 2018–2019 | Survey | 8521 | 17.7 | 1509 | 59.6 | 899 |
| Kentucky | 2022 | Survey STAT News |
18 560 | 13.2 | 2454 | 75c | 1841 |
| Louisiana | 2022 | Survey Presentation [23] |
26 074 | 18.0 | 4700 | 13.5 | 635 |
| Maine | 2019 | Survey | 1577 | 25.6 | 404 | 69.6 | 281 |
| Maryland | 2019 | Survey | 15 134 | 11.4 | 1719 | 73.4 | 1262 |
| Massachusetts | 2021 | 2 surveys | 6148 | 2.8 | 172 | 75c | 129 |
| Michigan | 2022 | Survey | 32 186 | 11 | 3540 | 26 | 920 |
| Minnesota | 2019 | Survey | 8003 | 10.4 | 833 | 61.5 | 512 |
| Mississippi | 2022 | Survey | 17 332 | … | … | … | … |
| Missouri | 2017 | Survey | 23 422 | 13.7 | 3214 | 75c | 2411 |
| Montana | 2023 | Survey | 4313 | 24.5 | 1055 | 75c | 791 |
| Nebraska | 2018–2019 | Survey | 5600 | 8.3 | 466 | 75c | 350 |
| Nevada | 2019–2020 | Survey | 10 202 | 27.0 | 2755 | 74.1 | 2041 |
| New Hampshire | 2022 | 2 surveys | 2127 | 14.4 | 307 | 75c | 230 |
| New Jersey | 2022 | 2 surveys | 12 506 | 20.8 | 2599 | 14.6 | 379 |
| New Mexico | 2022 | 2 surveys | 5154 | 34.2 | 1760 | 64.7 | 1139 |
| New York | 2021 | Survey Public report [24] |
30 338 | 11.5 | 3492 | 12.1 | 423 |
| North Carolina | 2019 | Survey Lawsuit [25] |
28 995 | … | … | … | … |
| North Dakota | 2018 | Survey Published report [16] |
1689 | 18.1 | 306 | 75c | 230 |
| Ohio | 2023 | 2 surveys | 45 029 | 14.5 | 6534 | 84 | 5489 |
| Oklahoma | 2021 | Survey STAT News |
22 391 | 12.6 | 2826 | 75c | 2120 |
| Oregone | 2007 | Survey Lawsuit [26] |
13 198 | 23.0 | 3036 | 75c | 2277 |
| Pennsylvania | 2022 | 2 surveys | 37 194 | 22.0 | 8191 | 35.7 | 2927 |
| Rhode Islandd | 2022 | Survey | 2238 | 23.2 | 519 | 30.6 | 159 |
| South Carolina | 2018–2020 | Survey | 15 759 | 19.2 | 3026 | 75.9 | 2297 |
| South Dakota | 2021 | STAT News | 3353 | 15.2 | 509 | 75c | 382 |
| Tennessee | 2017–2018 | Survey Lawsuit [27] |
21 995 | 32.7 | 7199 | 75c | 5399 |
| Texas | 2022 | Survey | 133 772 | 9.7 | 12 989 | 62.4 | 8105 |
| Utah | 2019 | Survey | 5907 | 11.4 | 675 | 75c | 506 |
| Vermontd | 2018–2020 | Survey Published report [17] |
1287 | 15.7 | 202 | 86.9 | 176 |
| Virginia | 2017 | Public report | 30 357 | 10.8 | 3266 | 75c | 2450 |
| Washington | 2019 | Survey Published report [19] |
13 674 | 19.2 | 2621 | 41.8 | 1096 |
| West Virginia | 2019 | Survey | 5847 | … | … | … | … |
| Wisconsin | 2014–2015 | 2 surveys | 20 202 | 12.5 | 2527 | 71.0 | 1794 |
| Wyoming | 2019 | Survey | 2123 | 8.7 | 185 | 50.6 | 94 |
| Mean percentages | 15.2 | 54.9 | |||||
For derivation of rates, see the table in Supplement 2.
Abbreviation: HCV, hepatitis C virus.
See Supplement 2 for additional notes on derivation of numbers.
The size of the total prison population was based on statistics published by the Bureau of Justice for 2021 [14].
Seventy-five percent was used as the default value for percentage of seropositive persons with viremia if no other data available, per Smith et al [15].
In these unified jail/prison systems, population includes some individuals with short stays (awaiting trial).
Cited in contemporary survey, even though source of data is now dated.
The ability to provide informative data ranged considerably by state. For 4 states that returned their surveys, seroprevalence and prevalence of viremia were unable to be calculated from the responses given. However, most states could provide seroprevalence data for at least short time periods. States that reflexed all positive antibody tests to viral testing were able to provide more comprehensive data on the prevalence of HCV viremia. For a handful of states (ie, Alaska, California, Indiana, New York, North Dakota), detailed longitudinal data were obtained.
Weighting the seroprevalence data by state prison population size, among the 47 states from which prevalence data were available, the overall HCV antibody prevalence was 15.2% (range, 8.3% [Nebraska] to 38.8% [Alaska]). Some states reported only the prevalence of viremia, and by back-calculation the prevalence of antibody would be below that of Nebraska if viremic persons indeed represented 75% of all those with HCV antibodies.
The mean prevalence of HCV viremia was 8.7% of the state prison population (range, excluding states with no data on proportion of persons with antibodies who were viremic: 1.4% [New York] to 24.5% [Alaska]). Applying the 8.7% viremia prevalence estimate to the total US prison population at year-end 2021, there were 91 090 persons in prison who had HCV infection [15].
Among persons with a positive HCV antibody test and residing in a system with data on prevalence of viremia, on average 54.9% were viremic (range, 12.1% [New York] to 86.9% [Vermont]). Many states had a prevalence less than the 75% expected from spontaneous clearance alone; 8 prison systems reported viremia in <50% of the seropositive residents.
DISCUSSION
Accurate HCV prevalence data in carceral facilities is critical to guide progress toward US HCV elimination goals. Since our last survey of HCV prevalence in 2017, the preciseness of the data has improved as twenty-seven (54%) of systems provided prevalence of both antibody and viremia, when previously only HCV seroprevalence was reported [8]. We estimate that 91 090 persons, representing 1 in 11 people incarcerated, is currently living with HCV infection on any given day in state prison. Over a year the number of individuals with HCV who cycle through carceral institutions is an even larger number since one-third of state prison population turns over per year [28]. Prevalence of HCV antibodies continues to vary widely by state system, likely indicative of heterogenous injection drug use patterns by state. The percentage of persons with HCV antibodies who remain viremic also varies widely, which may reflect variable access to treatment [6–8, 18].
Cure of all persons with HCV infection is the ultimate goal for national elimination. To measure progress toward HCV elimination, one can examine the percentage of those who are HCV antibody positive and remain viremic. In our previous publication, we estimated that the HCV seroprevalence in prisons was 18% in 2017 [8]. Given the lack of HCV RNA data and severely limited access to treatment at that time, we assumed that 75% of those individuals remained viremic based on spontaneous clearance of the virus alone, resulting in an overall prevalence of concurrent viremia of 13.5%. Our estimate of the prevalence of HCV viremia in 2021 was 8.7%, which was based on measured values for HCV viremia for many states and was lower than the seroprevalence rate expected from spontaneous clearance alone, that is, 75% of the 15.2% seroprevalence would result in a calculated viremic prevalence of 11.4% rather than the 8.7% found. This new benchmark may be used for measuring future progress in US prison elimination efforts. However, differences in the derivation of HCV viremia between survey periods preclude a determination of statistical significance of the change between the 2 estimates.
While treatment data were not provided by all states, a handful of survey respondents reported treating more patients with HCV in the population of the state prison system than the number of patients with HCV entering the system in a year. In these states, it is expected that the seroprevalence of HCV would remain relatively stable over time, since an antibody test remains positive even after eradication of the virus in successfully cured persons. However, longitudinal trends among seropositive individuals in these states, such as California, illustrate that the percentage of HCV viremia is declining, often far below the 75% expected with spontaneous clearance alone (data not shown). It is possible that the reason the prevalence of viremia has fallen among seropositive individuals in the cross-sectional population (eg, 13.1% in Louisiana as of October 2021 and 27.9% in California as of year-end 2021) is directly related to the high rate of successful treatment in prison, in the community, or both. On the other hand, over the past few years in California, the percentage of HCV viremia among people entering the system has remained flat, highlighting the difference between the cross-sectional and entry populations. The decline in viremia within the cross-sectional population indicates that a commendable amount of HCV treatment and cure has been in prison rather than before admission in the surrounding community.
Another way to determine if progress is being made toward HCV elimination, is to compare the rate of HCV treatment to the rate of persons with HCV infection entering a system or facility. According to the Michigan Department of Corrections (MI DOC), approximately 539 persons were treated for HCV per year between 2018 and 2022. Given that the prison system reports that only 9 people with HCV are identified to have infection at entry to MI DOC per month or 108 people per year [29], the rate of HCV treatment is 5 times greater than the entry rate of persons with HCV. That means that 431 more persons with HCV infection are treated than who enter annually and eventually the prevalence of people with ongoing viremia within the cross-sectional prison population would approach zero, although treatment would need to continue for newly identified individuals at prison entry. With 11.1% seropositivity reported in MI DOC in 2016 [8], treating a backlog of 3200 cases could take the Michigan system approximately 8 years [29].
Many have opined on the reasons why progress toward nationwide HCV elimination has been not been faster, noting the limited availability of treatment in the carceral settings as a major factor [13–15]. Modeling has demonstrated that elimination of HCV in the US will necessitate treating persons in prisons [4]. This will require a multifold approach including programmatic change at the system and state level as well as federal involvement. Exemplary programs provide at least one-time testing, on an opt-out basis, of all persons in prison, not just those who disclose risk factors. However, even with more robust screening, treatment may not be feasible for every infected person entering a state carceral system. For example, in states with a unified jail and prison system (ie, Alaska, Connecticut, Delaware, Hawaii, Vermont, and Rhode Island), some individuals who are preadjudication leave in a matter of days, an insufficient time for treatment evaluation and therapy initiation. Nonetheless, other individuals awaiting trial in combined systems, and also stand-alone jails, do stay long enough to complete curative treatment while confined [30].
Payment for interventions that are cost-saving to the health system as a whole have been borne by the segment historically with the fewest resources. Although cost to the prison system has been one of the biggest barriers to more widespread HCV treatment in custody due to the loss of both public and private insurance, access to medications at a lower price may not be enough to increase elimination efforts. The financial barriers in purchasing medications for carceral facilities have been discussed elsewhere [31, 32]. Even though they are still not cheap, the cost of HCV medications has decreased significantly over time. However, current US Supreme Court case law establishes a reactive model of healthcare for prisons and necessitates only access to healthcare and the avoidance of deliberate indifference to known health problems requiring timely intervention, which may discourage screening for HCV infection [33]. In contrast to human immunodeficiency virus treatment, litigation has had a mixed outcome in increasing individual access to HCV treatment. Currently, there is not a legal imperative for carceral facilities to assume a public health approach to HCV elimination at a population level, but a moral appeal “to do the right thing.”
At the current rate of detection, referral to care and treatment in most prison systems, the journey to eliminate HCV could extend beyond the 2030 goal. More than 95% of persons in prisons are released back to the community, and even during incarceration transmission does not respect the walls of the facility [34]. By definition, carceral health is the public's health. As a nation, we will need not just interventions to help make treatment in custody settings affordable, but prisons must also have the needed infrastructure—a screening and treatment strategy, a healthcare workforce sufficiently large and trained, and a carceral environment that supports the rendering of clinical care.
There is hope that the newly proposed national HCV elimination initiative will provide additional resources to both carceral facilities and public health systems to improve every step of the HCV care cascade and help move the nation toward elimination by 2030. Our study fills an important gap by providing estimates of HCV burden in each state's prison facilities that could serve as a guidepost for allocating resources to manage HCV within this often-neglected population.
Limitations
First, the clinical diagnosis of HCV infection in the US consists of 2 steps: preliminary screening for HCV antibodies, indicating exposure, and follow-up HCV RNA testing, indicating ongoing infection. After antibody screening, many state prison systems do not reflexively test seropositive individuals. Therefore, the total number of individuals with viremia often had to be extrapolated based on the prevalence of viremia among those tested [32].
For states without viremia data, we had to rely on reported seroprevalence and calculate the rates of viremia based on published estimates of spontaneous HCV clearance. The viremia value used (75%) was greater than the overall average viremia (54.9%). Making reflexive testing the standard laboratory method for HCV diagnosis or moving toward a one-step point-of-care HCV RNA option would add precision to estimating how many individuals have ongoing infection. Alternatively, a viral antigen test or a qualitative HCV RNA could also be used as a one-step diagnostic strategy [35, 36]. However, viral antigen tests are less sensitive at lower viral loads, and qualitative HCV tests only suffice if the HCV viral load does not impact treatment decisions.
Second, many states report their nontargeted HCV screening from entry data. The HCV antibody prevalence among entrants can fluctuate considerably from year to year and only reflects the overall cross-sectional prison population if its prevalence at entry is stable for several years. Nonetheless, prison entry is often the one consistent time point at which everyone is medically evaluated and is operationally the only population that many prison systems systematically screen. Caution must be taken when applying prevalence estimates for the entering population to the total carceral population. Substituting prevalence of HCV from the entry cohort data and applying it to the cross-sectional population leads to a biased estimate if seroprevalence fluctuates or the proportion viremic falls due to aggressive treatment; however, often only entry data were available.
Third, since screening might aim only to find cases to treat rather than for surveillance, persons who report already knowing they have untreated HCV infection at prison entry may not undergo repeat testing. Testing only those with unknown status can skew the prevalence if the reported prevalence does not include persons already diagnosed as viremic.
Fourth, the survey and published estimates for HCV seroprevalence and viremia were reported for varying time periods: one as early as 2007; others as late as 2023. Although data closest to 2021 were prioritized if >1 period was available, the HCV data were not always from the desired year. Regardless of the year the HCV prevalence estimates were from, it was multiplied by the population of the state prison system from 2021. It is possible that the actual HCV seroprevalence and rates of viremia in 2021 had changed from the time the data were collected. However, we wanted to consistently use the prison population in 2021 to better reflect the number of people incarcerated in the US on a single day.
Other limitations are as follows: (1) HCV numbers and percentages reported in lawsuits are prior to litigation and some persons may have since been treated; (2) for some states that did not respond to the survey, we had to rely on other data sources of varying accuracy to estimate HCV viremia prevalence; (3) some states (eg, Alabama and New Hampshire) tested only individuals deemed high risk, which has been shown to lead to significant undercounting [19, 37]; and (4) data only reflect state prison systems, excluding the federal prison system, juvenile carceral system, or adult jails. Adult jails may have a similar prevalence to prisons [38], but the precise relationship between the rates in the 2 types of facilities has not been elucidated.
CONCLUSIONS
The prevalence of HCV infection in state prison populations, while heterogeneous, on average is 8.7 times greater than in the general US population. State systems with a low prevalence of viremia among seropositive individuals demonstrate that widespread cure is feasible. Elimination of HCV in the US depends on fully addressing the carceral epidemic, and determining the size of the burden by state is one of the first steps in understanding the challenges that lie ahead and to minimize the existing inequities between states.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Supplementary Material
Contributor Information
Anne C Spaulding, Department of Epidemiology, Rollins School of Public Health, Emory University, Atlanta, Georgia.
Shanika S Kennedy, Department of Epidemiology, Rollins School of Public Health, Emory University, Atlanta, Georgia.
Jeffery Osei, Department of Epidemiology, Rollins School of Public Health, Emory University, Atlanta, Georgia.
Ebrima Sidibeh, Department of Epidemiology, Rollins School of Public Health, Emory University, Atlanta, Georgia.
Isabella V Batina, Department of Epidemiology, Rollins School of Public Health, Emory University, Atlanta, Georgia.
Jagpreet Chhatwal, Massachusetts General Hospital Institute for Technology Assessment, Harvard Medical School, Boston.
Matthew J Akiyama, Department of Medicine, Albert Einstein College of Medicine; Department of Medicine, Montefiore Medical Center, New York, New York.
Lara B Strick, Department of Medicine, University of Washington, Seattle.
Notes
Acknowledgments. We thank the Correctional Leadership Association for their assistance in distributing the original survey in 2019 and the end results in 2023 to its members. We are also grateful for the help of prison staff who provided their state data. We are indebted to Jeffrey Lin for assistance with preparing the manuscript for publication.
Financial support. This work was supported by the National Science Foundation (award number 1722906 to A. C. S.).
Supplement sponsorship. This article appears as part of the supplement “Current Barriers and Strategies Toward HCV Elimination Globally,” sponsored by Gilead Sciences Hong Kong Ltd.
Potential conflicts of interest. A. C. S. reports funding from a Center for AIDS Research grant from the National Institute of Allergy and Infectious Diseases, National Institutes of Health (NIH) to institution; the National Institute on Drug Abuse, NIH (RADx-UP cooperative agreement to institution); the Bill & Melinda Gates Foundation (grant to institution); Ceres Nanosciences through NIH RADx Tech (grant to institution); TB Reach Grant (Health Through Walls) to institution; Gilead Sciences (investigator-initiated grant to institution); National Science Foundation (to institution); travel fees from the Infectious Diseases Society of America to attend IDWeek; and payment for speaking from the National Commission on Correctional Healthcare. L. B. S. reports payment for consulting with the U.S. District Court for the District of Arizona to monitor the AZ DOC for compliance with injunction including monitoring hepatitis C care; travel fees from the Infectious Disease Society of America to attend ID Week. All other authors report no potential conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Hofmeister MG, Rosenthal EM, Barker LK, et al. Estimating prevalence of hepatitis C virus infection in the United States, 2013–2016. Hepatology 2019; 69:1020–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fleurence RL, Collins FS. A national hepatitis C elimination program in the United States: a historic opportunity. JAMA 2023; 329:1251. [DOI] [PubMed] [Google Scholar]
- 3. Institute for Crime and Justice Policy Research at Birkbeck, University of London. World prison brief. 2021. https://www.prisonstudies.org/. Accessed 2 March 2023.
- 4. He T, Li K, Roberts MS, et al. Prevention of hepatitis C by screening and treatment in US prisons. Ann Intern Med 2016; 164:84–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Weinbaum C, Lyerla R, Margolis HS. Prevention and control of infections with hepatitis viruses in correctional settings. Waltham, MA: Massachusetts Medical Society, 2003.
- 6. Spaulding A, Greene C, Davidson K, Schneidermann M, Rich J. Hepatitis C in state correctional facilities. Prev Med 1999; 28:92–100. [DOI] [PubMed] [Google Scholar]
- 7. Varan AK, Mercer DW, Stein MS, Spaulding AC. Hepatitis C seroprevalence among prison inmates since 2001: still high but declining. Public Health Rep 2014; 129:187–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Spaulding AC, Anderson EJ, Khan MA, Taborda-Vidarte CA, Phillips JA. HIV and HCV in US prisons and jails: the correctional facility as a bellwether over time for the community's infections. AIDS Rev 2017; 19:134–47. [PubMed] [Google Scholar]
- 9. Akiyama MJ, Kronfli N, Cabezas J, et al. Hepatitis C elimination among people incarcerated in prisons: challenges and recommendations for action within a health systems framework. Lancet Gastroenterol Hepatol 2021; 6:391–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. World Health Organization (WHO) . Combating hepatitis B and C to reach elimination by 2030: advocacy brief. Geneva, Switzerland: WHO, 2016.
- 11. Civil Rights Litigation Clearinghouse . Special report: hepatitis C in prisons and jails. 2022. https://clearinghouse.net/. Accessed 28 December 2022.
- 12. Florko N. Hepatitis C in prisons—an 8 part series. 2022. https://www.statnews.com/2022/12/15/prisons-cant-afford-hep-c-drugs-but-some-figured-out-a-way/. Accessed 28 December 2022.
- 13. Civil Rights Litigation Clearinghouse, University of Michigan. 2023. https://clearinghouse.net/search/case/?search=hepatitis&special_collection=33558&ordering=-summary_approved_date. Accessed 4 April 2023.
- 14. Carson EA. Prisoners in 2021—statistical tables. Bureau of Justice Statistics. NCJ number 305125. 2022. https://bjs.ojp.gov/library/publications/prisoners-2020-statistical-tables. Accessed 28 December 2022.
- 15. Smith DJ, Jordan AE, Frank M, Hagan H. Spontaneous viral clearance of hepatitis C virus (HCV) infection among people who inject drugs (PWID) and HIV-positive men who have sex with men (HIV+ MSM): a systematic review and meta-analysis. BMC Infect Dis 2016; 16:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chandra Deb L, Hove H, Miller TK, et al. Epidemiology of hepatitis C virus infection among incarcerated populations in North Dakota. PLoS One 2022; 17:e0266047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hale AJ, Mathur S, Dejace J, Lidofsky SD. Statewide assessment of the hepatitis C virus care cascade for incarcerated persons in Vermont. Public Health Rep 2023; 138:265–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Spaulding AC, Chen J, Mackey CA, et al. Assessment and comparison of hepatitis C viremia in the prison systems of New Mexico and Georgia. JAMA Network Open 2019; 2:e1910900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Assoumou SA, Wang J, Tasillo A, et al. Hepatitis C testing and patient characteristics in Washington State's prisons between 2012 and 2016. Am J Prev Med 2019; 56:8–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Arizona Department of Corrections Rehabilitation and Reentry . Corrections at a glance. 2021. https://corrections.az.gov/sites/default/files/documents/reports/CAG/2021/cagdec-21.pdf. Accessed 9 July 2023.
- 21. Aragon v. Raemisch , 1:17-cv-01744 (US District Court for the District of Colorado, 2017).
- 22. Barfield v. Quiros , 3:18-cv-01198 (US District Court for the District of Connecticut, 2021).
- 23. Irvin R. Hepatitis C testing and treatment in Louisiana: a model for national hepatitis C elimination through corrections [webinar]. Johns Hopkins Medicine. 2022. https://www.globalhep.org/sites/default/files/content/webinar/files/2022-05/Irvin_Final%20NIDA%20HCV%20Webinar%20May%202022.pdf. Accessed 9 July 2023.
- 24. New York State Department of Health . Hepatitis B and C, annual report 2021. 2021. https://www.health.ny.gov/statistics/diseases/communicable/docs/2021_hepatitis_b_c_annual_report.pdf. Accessed 9 July 2023.
- 25. Buffkin v. Hooks , 1:18-cv-00502 (US District Court for the Middle District of North Carolina, 2018).
- 26. Anstett v. State of Oregon , 3:01-cv-01619 (US District Court for the District of Oregon, 2007).
- 27. Graham v. Parker , 3:01-cv-01619 (US District Court for the District of Oregon, 2016).
- 28. Bureau of Justice Statistics . Jail inmates in 2021—statistical tables. NCJ 304888. 2022. https://bjs.ojp.gov/sites/g/files/xyckuh236/files/media/document/ji21st.pdf. Accessed 2 March 2021.
- 29. Michigan Department of Corrections . Michigan legislative report. https://www.michigan.gov/corrections/public-information/statistics-and-reports/legislative-reports. Accessed 4 April 2023.
- 30. MacDonald R, Akiyama MJ, Kopolow A, et al. Feasibility of treating hepatitis C in a transient jail population. Open Forum Infect Dis 2017; 4:ofx142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Akiyama MJ, Feffer R, von Oehsen WH 3rd, Litwin AH. Drug purchasing strategies to treat people with hepatitis C in the criminal justice system. Am J Public Health 2018; 108: 607–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Spaulding AC, Adee MG, Lawrence RT, Chhatwal J, von Oehsen W. Five questions concerning managing hepatitis C in the justice system: finding practical solutions for hepatitis C virus elimination. Infect Dis Clin North Am 2018; 32:323–45. [DOI] [PubMed] [Google Scholar]
- 33. Estelle v. Gamble , 429 U.S. 97 (1976).
- 34. Hochstatter K, Tully D, Power K, et al. Hepatitis C virus transmission clusters in public health and correctional settings, Wisconsin, USA, 2016–2017. Emerg Infect Dis J 2021; 27:480–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sepúlveda-Crespo D, Treviño-Nakoura A, Bellon JM, et al. Diagnostic performance of the HCV core antigen test to identify hepatitis C in HIV-infected patients: a systematic review and meta-analysis. J Clin Microbiol 2023; 61:e01331–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Torrecillas M, Gómez-Muñoz N, Ocete MD, et al. One-step diagnosis strategy together with multidisciplinary telematics referral perform an effective approach for identifying and treating patients with active hepatitis C infection. Ann Hepatol 2022; 27:100542. [DOI] [PubMed] [Google Scholar]
- 37. Kuncio DE, Newbern EC, Fernandez-Viña MH, Herdman B, Johnson CC, Viner KM. Comparison of risk-based hepatitis C screening and the true seroprevalence in an urban prison system. J Urban Health 2015; 92:379–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Chak E, Talal AH, Sherman KE, Schiff ER, Saab S. Hepatitis C virus infection in USA: an estimate of true prevalence. Liver Int 2011; 31:1090–101. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.