Summary
Although advances in free flap surgery have allowed the reconstruction of a wide range of complex scalp defects, simpler local options continue to play a role. We describe how bipedicled or ‘bucket handle’ scalp flap with skin grafting of the donor site can be used to resurface large scalp defects of up to 15 cm x 20 cm.
This retrospective case series of 11 patients describes flap outcomes, post-operative complications, pathology and patient-related outcomes collected via a questionnaire.
Defect sizes ranged from 56 cm2 to 220 cm2. All 11 flaps survived with no readmissions or return to theatre. There were two minor post-operative infections. Pathologies requiring reconstruction were invasive squamous cell carcinoma involving the bone (45%), cranial bone necrosis after a cerebrovascular event (27%), trauma (9%) or cerebral malignancy (9%). Four patients (36%) underwent simultaneous cranial reconstruction with a cranioplasty plate. On an average, the patients who did not need to remain in the hospital for other reasons were discharged after two days. All patients reported subjective improvements in function post-operatively and that they were satisfied with the procedure.
This study suggests that large bipedicled scalp flaps with skin graft to the donor site are reliable, with positive patient-related outcomes and few post-operative complications. This technique is well suited for reconstructing long elliptical scalp defects created after the insertion of a cranioplasty plate. This procedure provides a robust alternative to patients who are unsuitable for free tissue transfer and those who may benefit from the short operative time and quick recovery time associated with a local flap.
KEY WORDS: Bipedicled, Scalp flap, Reconstruction, Cranioplasty, Split-Thickness Skin Graft
Introduction
Reconstruction of large scalp defects is challenging when they include areas of denuded bone or metal plates, and irradiated or chronically infected tissues. The development of free flaps has made it possible to cover numerous complex defects1 commonly using latissimus dorsi, anterolateral thigh or parascapular flaps.2 However, simpler local flaps also play an important role, especially for patients who are not suitable for free flap surgery. Over the last 20 years (Feb 2003–Sept 2022), the senior author has developed the use of a large bipedicled advancement flap, also known as a ‘bucket handle’ or ‘visor’ flap, with split-thickness skin graft (SSG) to the donor site, for scalp reconstruction in situations where a free flap is contra-indicated.
Tripier first described the use of a bipedicled, myocutaneous flap for eyelid reconstruction in 1889. His surgery involved transposition of a flap from a suitably lax upper eyelid to resurface a lower eyelid defect.3 In 1957 Crawford described a ‘double-pedicled’ flap as an alternative to cross-leg flaps for lower limb reconstruction.4 Bipedicled flaps have also been described for staged reconstruction of the helix of the ear, by raising a flap from the postauricular area.5 Bipedicled flaps with primary closure of the donor site have been described for forehead,6 trunk and extremity reconstructions.7 This technique has been further refined with V-Y modification to facilitate greater advancement of bipedicled flaps for the reconstruction of challenging sacral pressure sores.8
Therefore, bipedicled flaps are known for being versatile, and can be applied at multiple body sites and numerous defect sizes.9
For complex scalp defects involving soft tissue loss with denuded or absent bone, local flap reconstruction with primary closure of the donor site can be used for small to medium sized defects. Within these techniques is described a bipedicled flap with undermining and closure of its donor site for defects up to 50 cm2.10 These techniques have the advantage of minimal flap donor site morbidity, but are not suitable for larger defects in which primary closure of the donor site is not possible.
Despite the rich surgical history of bipedicled flaps, there are relatively few descriptions about their use in the reconstruction of larger scalp defects. The technique has several advantages: The procedure is simple, single stage and quick. In patients who are unsuitable for general anaesthesia, it can be done under local anaesthesia. In patients undergoing lengthy neurosurgical procedures such as excision of an intra-cerebral tumour with bony involvement, with a resultant full thickness scalp defect, the technique can offer a rapid and robust soft tissue coverage option. Unlike free flap reconstruction, the bipedicled flap does not need post-operative (post-op) monitoring, nor does it have the morbidity of a free flap donor site; therefore, patients can be discharged rapidly with a shorter recovery. The bipedicled flap adheres to the reconstructive principle of replacing like-for-like at the site of the primary reconstruction. This is particularly important in patients who have hair, as the flap provides a superior aesthetic outcome compared with a free flap which is generally hairless. Although the flap donor site has the disadvantage of being resurfaced with an SSG, this graft can be serially excised or reconstructed with a tissue expander should the patient desire further elective reconstruction. Finally, the use of the bucket flap does not destroy possibility of future free flap reconstruction as no major vessels in the area are sacrificed during the procedure.
Methods
We present a retrospective quantitative and qualitative case series of 11 patients who underwent scalp reconstruction using a bipedicled scalp advancement flap with SSG of the donor site between February 2003 and September 2022. We report on patient demographics, pathology, surgical technique and post-op outcomes including patient-related outcomes. A patient-related outcome measure (PROM) questionnaire specific to the procedure was designed by the authors and completed by all living patients. The questionnaire was based on the U.K. National Health Service (NHS) PROM questionnaires for common operations such as total hip replacement and total knee replacement11 and assessed the patients’ pain post-op and levels of satisfaction with the flap, grafted flap donor site on the scalp and SSG site (thigh), and their subjective level of function post-op and overall satisfaction with the procedure. Furthermore, patients were also questioned on whether they desired further surgery to improve the flap donor site. This study was conducted according to the principles of the Declaration of Helsinki (2013).12 Written consent was obtained from all patients whose images are included. The study was reviewed by the local ethics board of the hospital.
Surgical technique
The width of the bipedicled flap should be at least 8 cm wide at the centre and/or as wide as the defect that it will cover, but preferably at least 2 cm wider. This ensures that the flap is broad enough to cover the denuded bone or metal plate when advanced. In the authors experience, there is no need to triangulate a circular defect. The flap should be raised and advanced over the defect without concern about dogears (even if large), as these shrink rapidly 3–6 months post-op without the need for revision [Figure 1, Figure 2, Figure 3, Figure 4]. The flap can be raised rapidly using McIndoe scissors (or similar instruments) in the subgaleal plane, taking care to leave the periosteum intact so that the donor site can be grafted. Although the flap can work as a random pattern flap, the authors always attempt to include at least one of the (named) scalp vessels in the pedicle at each end of the flap. Therefore, flap orientation is commonly determined by the location of these vessels [Figure 5]. Once advanced, the donor site is resurfaced with a SSG (commonly harvested from the thigh) which is dressed with paraffin impregnated gauze and foam. The foam is stapled to the adjacent skin edges and this dressing is left in place for 7 days before inspection. In the authors experience, the procedure takes approximately 1 h.
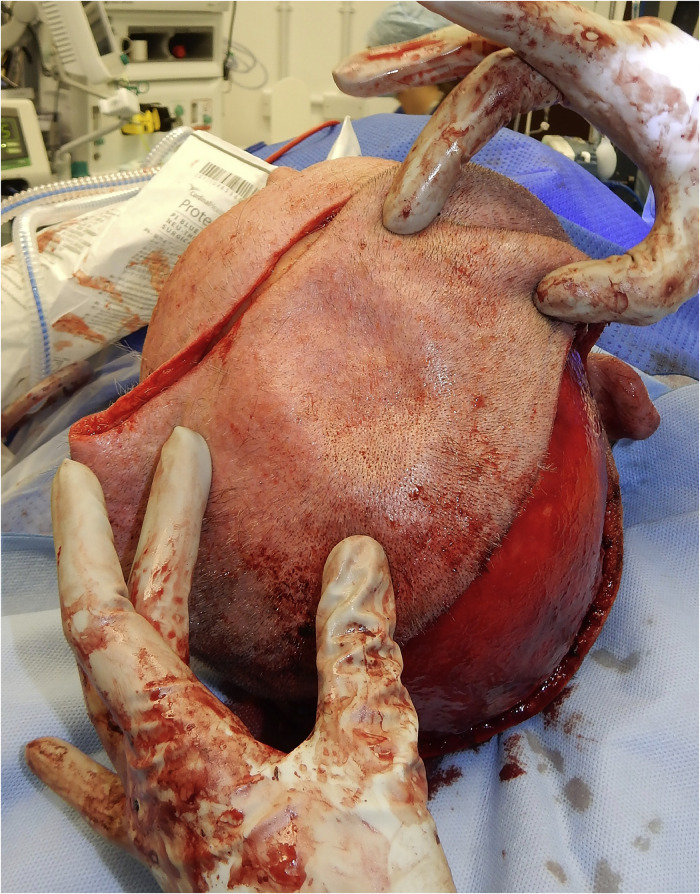
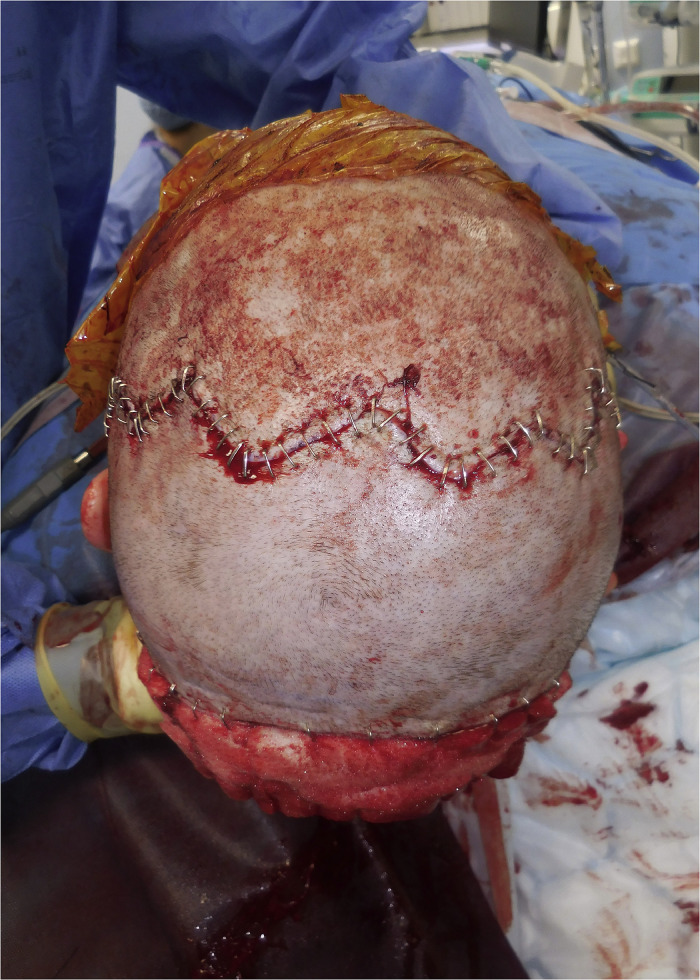
Figure 1.
Post squamous cell carcinoma debridement
Figure 2.
Mobilisation of flap
Figure 3.
Flap inset + dog ears
Figure 4.
Five-months post-op (no excision of dog ears)
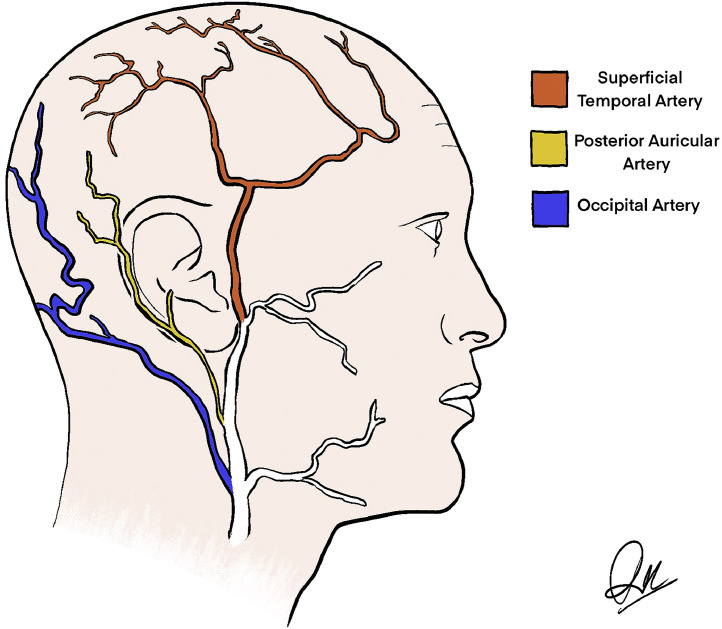
Figure 5.
Arteries of the scalp
Results
Eleven bipedicled flaps were performed for 11 patients over a 20-year period. Patient follow-up was between 5 to 51 months with an average of 20 months. Two patients (18%) were lost to long-term follow-up. Patient ages ranged between 34 to 88 years with an average age of 68 years [Table 1]. However, the majority were older adults with 7 (64%) of them over 70 years and 4 (36%) over 80 years old. One procedure (9%) was performed under local anaesthesia. The rest (91%) of the procedures were performed under general anaesthesia. Comorbidities are documented in Table 1 and included eight patients with hypertension and two patients with type-2 diabetes.
Table 1.
Patient Demographics
| PATIENT NUMBER | AGE AT TIME OF PROCEDURE (years) | FOLLOW-UP TIME (months) | SMOKING STATUS | DIABETIC STATUS | CO-MORBIDITIES |
|---|---|---|---|---|---|
| 1 | 80 | - | Non-smoker | Non-diabetic | Hypertension |
| 2 | 77 | 20 | Non-smoker | Type 2 diabetic | Hypertension, chronic kidney disease |
| 3 | 34 | 40 | Non-smoker | Non- diabetic | Nil |
| 4 | 58 | 24 | Non-smoker | Non-diabetic | Hypertension |
| 5 | 58 | 51 | Non-smoker | Non- diabetic | Hypertension, chronic kidney disease, previous cerebellar infarction, sickle cell trait |
| 6 | 88 | 10 | Non-smoker | Non- diabetic | Hypertension, atrial fibrillation, congestive cardiac failure, anaemia |
| 7 | 83 | 24 | Non-smoker | Non-diabetic | Hypertension, previous leiomyosarcoma |
| 8 | 80 | - | Non-smoker | Non- diabetic | Hypertension, atrial fibrillation |
| 9 | 79 | 5 | Non-smoker | Non-diabetic | Hypertension, atrial fibrillation, hypothyroidism |
| 10 | 43 | 32 | Non-smoker | Type 2 diabetic | Deep vein thrombosis, cerebellar infarction, asthma, wheelchair bound, previous cardiac arrest |
| 11 | 73 | 15 | Non-smoker | Non- diabetic | Heart bypass, previous brain tumour, Parkinsons, seizures |
The most common pathology necessitating reconstruction was invasive squamous cell carcinoma of the skin requiring excision of the underlying periosteum or bone (45%). Other patients in the series suffered from bone loss after a neurosurgical event requiring craniectomy (55%), for example, following a cerebrovascular event, trauma, or malignancy [Table 2]. Four (36%) of the 11 patients underwent simultaneous cranioplasty with a titanium plate which was then covered with the flap.
Table 2.
Operative Details
| PATIENT NUMBER | PATHOLOGY | CONCURRENT CRANIAL RECONSTRUCTION | ANAESTHETIC TYPE | DEFECT SIZE (cm) | DEFECT SIZE OVAL (cm2) | POST-OPERATIVE COMPLICATIONS | DAY HOME POST-OPERATIVELY |
|---|---|---|---|---|---|---|---|
| 1 | SCC involving bone | No | GA | 15×12 | 141 | No | - |
| 2 | SCC involving bone | No | GA | 13×12 | 122 | No | 2 |
| 3 | Blunt trauma | Yes | GA | 20×7 | 110 | No | 13 (neuro obs) |
| 4 | CVA + craniectomy | Yes | GA | 20×5 | 79 | No | Long stay (neuro obs) |
| 5 | CVA + craniectomy | No | GA | 20×5 | 79 | Minor wound infection | Long stay (rehab) |
| 6 | SCC involving bone | Yes | LA | 12×8 | 75 | No | 5 (hyponatraemia) |
| 7 | Sarcoma involving bone | No | GA | 9×8 | 56 | Minor wound infection | 2 |
| 8 | SCC involving bone | No | GA | 20×14 | 220 | No | - |
| 9 | SCC involving bone | No | GA | 15×12 | 141 | No | 1 |
| 10 | CVA + craniectomy | Yes | GA | 20×5 | 79 | No | Long stay (neuro obs) |
| 11 | Brain tumour + craniectomy | No | GA | 15×5 | 59 | No | Long stay (neuro obs) |
| SUMMARY |
SCC: 45% CVA: 27% Blunt trauma: 9% Sarcoma: 9% Brain tumour: 9% |
Yes: 36% No: 64% |
GA: 91% LA: 9% |
- | Average: 106 cm2 |
Minor wound infection: 18% No: 78% |
≤2 days admission: 33% Longer stay for non-flap related issues: 66% |
SCC = squamous cell carcinoma
CVA = cerebrovascular accident
GA = general anaesthesia
LA = local anaesthesia
The largest defect reconstructed measured 20 cm x 14 cm oval (220 cm2) whereas the smallest was 9 cm x 8 cm oval (56 cm2).a The average size of the defect was 106 cm2. In general, the defects post-excision of skin cancers were larger, requiring wider flaps. The defects secondary to cranioplasty are longer and elliptical, measuring (typically) 20 cm x 7 cm [Figure 6, Figure 7, Figure 8, Figure 9] and [Figure 10, Figure 11, Figure 12, Figure 13]
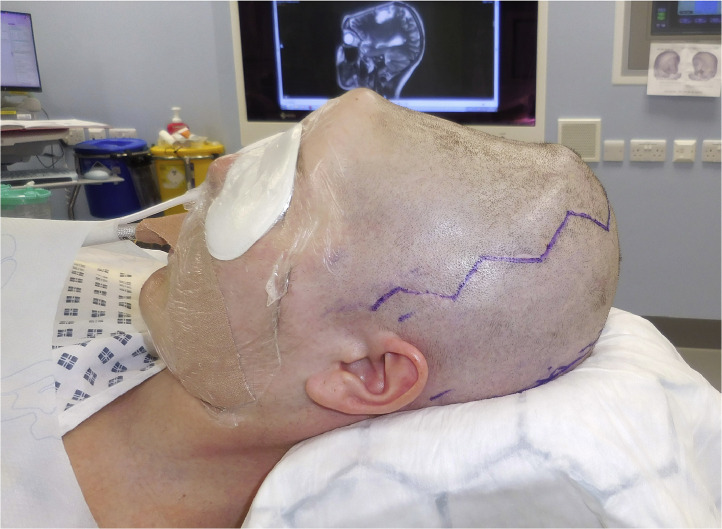
Figure 6.
Pre-operative—craniectomy for blunt trauma
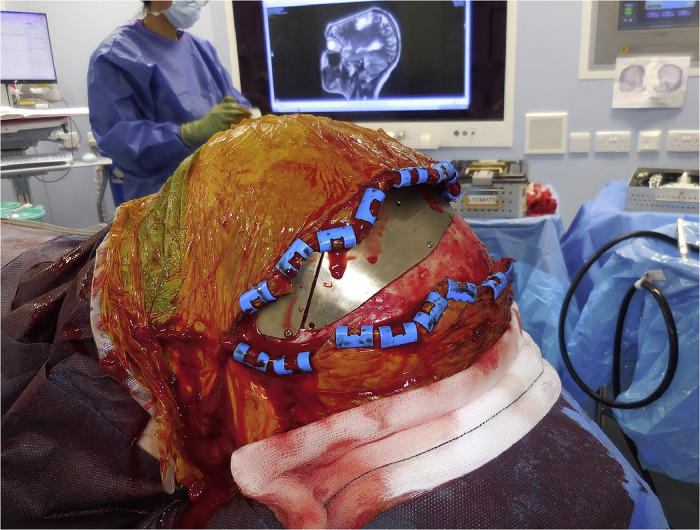
Figure 7.
Post-insertion of the cranioplasty plate
Figure 8.
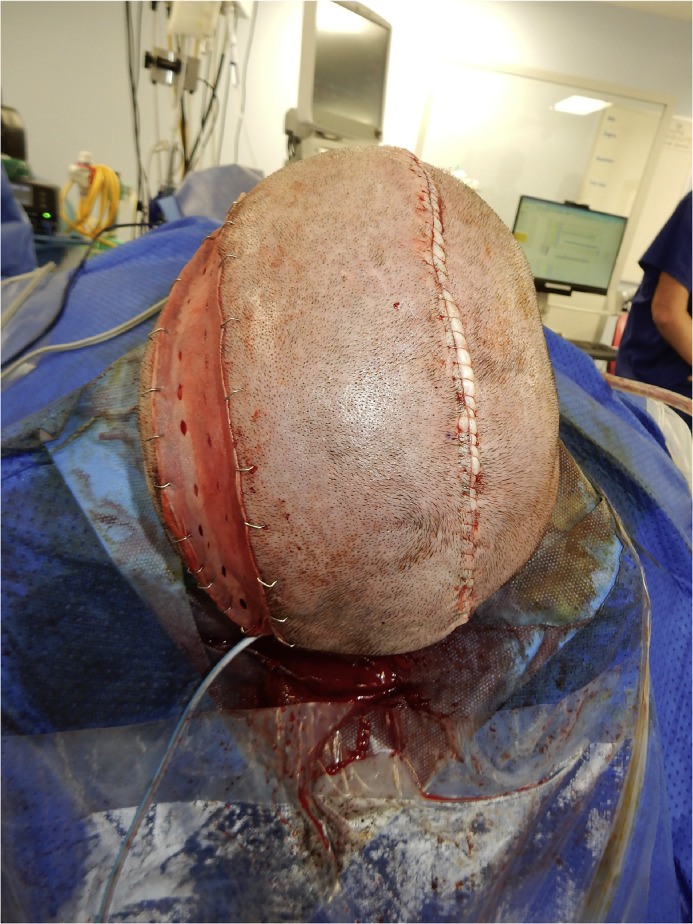
Flap inset
Figure 9.
One-month post-op
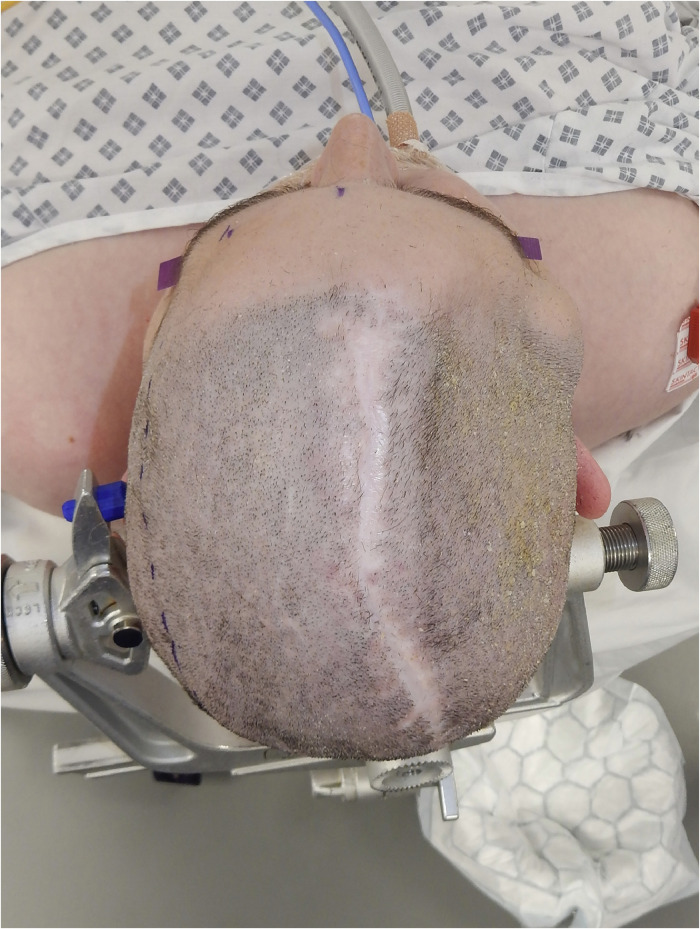
Figure 10.
Preoperative—craniectomy for infected bone flap post-craniotomy for CVA
Figure 11.
Post-insertion of the cranioplasty plate
Figure 12.
Flap inset
Figure 13.
Three-months post-op
All 11 flaps survived with no vascular issues and no returns to theatre. Two patients (18%) suffered minor wound infections which were managed with oral antibiotics. There were no other post-op complications [Table 2]. Three patients (33%) out of the 9, whose length of stay data were available were discharged home by day 2 post-op. Six patients (66%) required a longer admission due to non-flap related issues. The patient operated on under local anaesthesia was planned for a same day discharge but remained an inpatient owing to the coincidental finding of hyponatraemia.
Nine of 11 patients (82%) completed the PROM questionnaire [Table 3]. They reported on pain at the flap, skin graft and skin graft donor site as no pain, mild pain or severe pain. They reported on the appearance of the flap, skin graft and skin graft donor site as no dissatisfaction, mild dissatisfaction and significant dissatisfaction. None reported flap pain, one was slightly dissatisfied with the appearance of the flap. None reported donor site pain on the scalp. Four (44%) reported mild dissatisfaction with the appearance of the SSG. One (11%) reported pain at the skin graft donor site on the thigh and two (22%) reported dissatisfaction with the skin graft donor site on the thigh.
Table 3.
Patient-related outcome measures (PROM)
| PATIENT NUMBER | PAIN FLAP | APPEARANCE FLAP | PAIN GRAFT | APPEARANCE GRAFT | PAIN THIGH DONOR SITE | APPEARANCE THIGH DONOR SITE | LEVEL OF FUNCTION POST-OP (1-5) | OVERALL SATISFACTION WITH THE PROCEDURE (1-5) | DESIRES FURTHER RECONSTRUCTION |
|---|---|---|---|---|---|---|---|---|---|
| 1 | - | - | - | - | - | - | - | - | - |
| 2 | No | No | No | No | No | No | 4 | 4 | No |
| 3 | No | No | No | No | No | No | 4 | 5 | Possibly |
| 4 | No | No | No | No | No | No | 5 | 5 | No |
| 5 | No | Slightly concerned | No | No | No | Slightly dissatisfied | 4 | 5 | No |
| 6 | No | No | No | No | No | No | 5 | 4 | No |
| 7 | No | No | No | Slightly dissatisfied | Mild pain | No | 4 | 5 | No |
| 8 | - | - | - | - | - | - | - | - | - |
| 9 | No | No | No | Slightly dissatisfied | No | No | 5 | 5 | No |
| 10 | No | No | No | Slightly dissatisfied | No | No | 4 | 5 | No |
| 11 | No | No | No | Slightly dissatisfied | No | Slightly dissatisfied | 5 | 5 | No |
| SUMMARY |
No pain: 100% Mild pain: 0% Severe pain: 0% |
No dissatisfaction: 89% Mild dissatisfaction: 11% Significant dissatisfaction: 0% |
No pain: 100% Mild pain: 0% Severe pain: 0% |
No dissatisfaction: 56% Mild dissatisfaction: 44% Significant dissatisfaction: 0% |
No pain: 89% Mild pain: 11% Severe pain: 0% |
No dissatisfaction: 78% Mild dissatisfaction: 22% Significant dissatisfaction: 0 |
4-slightly better function: 56% 5-significantly better function: 44% |
4-slightly satisfied: 18% 5-very satisfied: 78% |
No: 89% Possibly: 11% Definitely: 0% |
Patients were asked to score their level of function post-op using a Likert scale of 1-5 with 1 indicating significantly poor function, 2 indicating slightly poor function, 3 indicating same as pre-op, 4 indicating slightly better function and 5 indicating significantly better function. The only scores reported were 4 and 5, with five patients (56%) scoring 4 and four patients (44%) scoring 5. Patients were asked to score their overall satisfaction with the operation on a scale of 1-5 with 1 being very dissatisfied, 2 being slightly dissatisfied, 3 being neither satisfied or dissatisfied, 4 being slightly satisfied and 5 being very satisfied. The only scores reported were 4 and 5, with two patients (22%) scoring 4 and seven patients (78%) scoring 5. Eight out of nine patients (89%) who completed the questionnaire indicated that they had no desire to undergo further elective reconstruction to remove the SSG on their scalp.
Discussion
This case series suggests that large bipedicled flaps are vascularly robust and versatile for resurfacing of scalp defects in a wide range of situations and in patients with underlying morbidities which preclude free flap surgery as an option. The outcomes are also acceptable from a patients’ perspective with minimal donor site (scalp and thigh) morbidity. Satisfaction with the appearance of the skin graft and graft donor site could have been improved with more in-depth pre-operative discussion on what to expect and illustrating the results using photographs from previous similar reconstructions.
For patients undergoing cranioplasty, it allows the potential for lifting the flap and cranioplasty plates to regain intra-cranial access in the future. In this instance, the flap can simply be raised and re-advanced into the new defect. Indeed, the large bucket handle flap appears to be particularly well suited for the reconstruction of the long elliptical defects produced by cranioplasty. In these situations, the flap need not be advanced very far and the resulting thin donor site can be covered by growing the hair long (where possible). Moreover, the SSGs applied to these long, thin defects tend to contract naturally. Therefore, there is a reduction in the size of the donor site over time.
Importantly, for patients undergoing cranioplasty and patients with skin cancer, subsequent reconstruction to remove and resurface the grafted donor sites should be possible with a tissue expander or by serial excision. However, none of the patients in this series have to date requested such a revision. We speculate that for older patients undergoing reconstruction in the context of skin cancer with bony invasion, further reconstruction was not of interest. Moreover, for the two younger patients in the study, the donor site was not easily visible as it was concealed by their long hair which decreased their desire for further reconstruction.
We recognise the limitations of this study in that it is a retrospective study with only a small number of patients. Thus, there is a lack of a comparison group such as matched patients undergoing free flap reconstruction for similar cranial defects. The study could have been improved by serial photography to understand the long-term aesthetic and morphological outcomes post-op as well as by using measurements to assess contraction of the skin grafts applied to the donor sites.
Nevertheless, the outcomes of this case series have been sufficiently encouraging and we feel confident in recommending this option as a simple and robust alternative to free flap surgery in selected patients, especially in the older adult who benefit particularly from the short operative times and low morbidity associated with the procedure.
Conflict of interest
None of the authors have any conflicts of interest regarding the content of the article.
Acknowledgments
Ethical approval
The study was reviewed by the local ethics board of the hospital who stated that formal ethical approval was not required for this study.
Patient consent
Patient consent for inclusion of images in the study was obtained from all patients whose images were used.
Funding
None.
Institution: Royal Free Hospital, Pond Street, London, NW3 2QG
Presentation: The content of this article has not been presented at any conferences or meetings.
Area of oval formula: A = pi * a/2 * b/2 where a and b are the largest and smallest diameters (perpendicular to one another).
References
- 1.Chang KP, et al. Free flap options for reconstruction of complicated scalp and calvarial defects: Report of a series of cases and literature review. Microsurgery. 2010;30:13–18. doi: 10.1002/micr.20698. [DOI] [PubMed] [Google Scholar]
- 2.Weitz J, et al. A standard algorithm for reconstruction of scalp defects with simultaneous free flaps in an interdisciplinary two-team approach. Front Oncol. 2019;9:1130. doi: 10.3389/fonc.2019.01130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elliot D, Britto JA. Tripier's innervated myocutaneous flap 1889. Br J Plast Surg. 2004;57:543–549. doi: 10.1016/j.bjps.2004.02.021. [DOI] [PubMed] [Google Scholar]
- 4.Crawford BS. The repair of defects of the lower limb, using a local flap. Br J Plast Surg. 1957;10:32–35. [Google Scholar]
- 5.Goldstein JA, Stevenson TR. Reconstruction of ear helix using self-tubing pedicle flap. Ann Plast Surg. 1988;21:149–151. doi: 10.1097/00000637-198808000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Stoner JG, Swanson NA. Use of the bipedicled scalp flap for forehead reconstruction. J Dermatol Surg Oncol. 1984;10:213–215. doi: 10.1111/j.1524-4725.1984.tb01210.x. [DOI] [PubMed] [Google Scholar]
- 7.Baker BG, Oudit D. The modified bipedicled flap for reconstruction of oncological skin defects of the trunk and extremities. J Plast Reconstr Aesthet Surg. 2020;73:913–920. doi: 10.1016/j.bjps.2019.11.030. [DOI] [PubMed] [Google Scholar]
- 8.Hartzell TL, Orgill BD, Chan R, Mathy JA, Orgill DP. V-Y modification of a bipedicle perforator flap. Plast Reconstr Surg. 2009;124:167–170. doi: 10.1097/PRS.0b013e3181a805e4. [DOI] [PubMed] [Google Scholar]
- 9.Dujon DG, Khan UD, Aslam S. Bipedicle flaps: Simple solutions for difficult problems in the extremities. Br J Plast Surg. 1997;50:641–645. doi: 10.1016/s0007-1226(97)90511-7. [DOI] [PubMed] [Google Scholar]
- 10.Ellis M, Hwang L, Ford NK, Slavin K. The role of the visor flap in scalp reconstruction: A case series of 21 patients. Oper Neurosurg (Hagerstown) 2018;15:651–655. doi: 10.1093/ons/opy042. [DOI] [PubMed] [Google Scholar]
- 11.https://www.england.nhs.uk/wp-content/uploads/2018/08/proms-guide-aug-18-v3.pdfhttps://regalchambers.co.uk/health-assessments/oxford-knee-score/https://goravdatta.com/oxford-hip-score/.
- 12.https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ Links checked and valid 7th August 2024