Abstract
Actinomyces spp. has been shown to form biofilms when exposed to copper, possibly enhancing its degradation. Fragmentation and migration of the copper coil on an intrauterine device (IUD) is rare, but the concomitant presence of Actinomyces spp. may increase its incidence. We present the first case of a fragmented copper IUD within its lifespan of 10 years, with documented Actinomyces genitourinary tract colonization in a premenopausal woman.
Keywords: Actinomyces, intrauterine device
KEY POINTS
Actinomyces spp. are more prevalent in the urogenital tract of women with IUDs due to the local tissue injury from the device inside the uterus, which creates an anaerobic environment that allows this organism to flourish.
Actinomyces spp. can form biofilms when exposed to copper, potentially enhancing its degradation, leading to fragmentation.
Patients with a copper IUD and Actinomyces identified on routine or symptomatic cervical sampling should be counseled regarding potential enhanced copper degradation, fragmentation, and migration of the copper coil.
CME
Credit Claim Process: To claim CME for this activity, read the entire article and go to ce.bswhealth.com/2024BUMC_Proceedings_Nov_IUD. You will register for the course, pay any relevant fee, take the quiz, complete the evaluation, and claim your CME credit.
Date for credit: November 1, 2024, to November 1, 2025.
For questions about CME credit, visit our website ce.bswhealth.com/contact-us
CASE SUMMARY
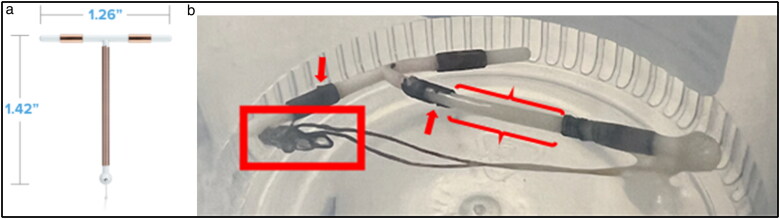
A 46-year-old premenopausal woman presented to the clinic with episodes of abnormal black, foul-smelling vaginal discharge for several years. She had a copper intrauterine device (IUD) in place for 9 years at the time of presentation. She denied fever, new sexual partners, vaginal irritation, and suprapubic pain. On the exam, there was no cervical motion tenderness, and the IUD strings were visible with a buildup of dark black, flaking, foreign material (Figure 1). Laboratory testing was negative for Candida, bacterial vaginosis, Trichomonas, syphilis, gonorrhea, and chlamydia. The Pap smear results were unremarkable except for the noted presence of Actinomyces spp. bacteria. After discussing various management options with the patient, she chose to have the IUD removed. Upon removal, it was noted that most of the copper coil was missing from the IUD and the remaining copper was black in color with a flaking appearance (Figure 1). Due to concern for retention or migration of the missing copper fragment, a pelvic x-ray was performed and was negative for radiopaque fragments. A subsequent computed tomography (CT) scan of the abdomen and pelvis did not reveal any retained metallic fragments within the pelvis. The patient’s symptoms had resolved at her 6-week follow-up.
Figure 1.
(a) Paragard IUD. (b) Paragard IUD postremoval in specimen container. Red arrows: fragmentation of the copper. Red box: knotted strings with buildup of black debris. Red braces: missing copper coil on long arm.
CLINICAL QUESTIONS
-
Women with IUDs have a higher incidence of what organism in the genitourinary tract?
Neisseria spp.
Lactobacillus spp.
Bacteroides spp.
Actinomyces spp.
-
Copper IUD fragmentation is appreciated on inspection of a removed copper IUD. Which imaging modality is most sensitive for identifying a retained copper fragment?
Transvaginal ultrasound
Computed tomography of the abdomen and pelvis
Magnetic resonance imaging of the abdomen and pelvis
Abdominal and pelvic radiograph
Answers are provided at the end of the article.
DISCUSSION
The copper IUD is an effective contraceptive choice due to the corrosion of copper and the oxidation of copper to black copper oxide, which inhibits transtubal sperm migration and prevents zygote formation. The corrosive and oxidative properties of the copper lead to breakdown of the copper coil over time, limiting its lifetime.1 The corrosion of copper within the coil is a normal and expected process and typically occurs in the cervical part of the device. It is proposed that the endometrial secretions near the cervix create a more favorable environment for corrosion compared to other areas of the endometrium. This often leads to a breakdown of copper, and potentially complete metal loss, along the long arm of the device rather than on the horizontal arms.2
Fragmentation and subsequent migration of the copper coil with an otherwise intact device on removal of a copper IUD appears to be a rare complication, with only two other cases reported since 2020.3 In the first case, the IUD had been in place for 12 years (2 years longer than its lifespan) and pelvic x-ray was positive for a radiopaque object in the left hemipelvis. Follow-up CT scan confirmed a metallic foreign body between the bladder and the uterus, suggesting the copper coil fragment had migrated out of the uterus. The second case involved a postmenopausal patient who had complete loss of copper coil on the long arm of the device when it was removed. Pelvic x-ray was negative for a radiopaque foreign body; however, a CT scan did show a linear metallic object next to the uterus in the hemipelvis. A suspected cause of the copper fragmentation in the two cases mentioned above was the presence of Actinomyces spp. within the urogenital tract; however, neither case reported whether Actinomyces spp. were present on cervical swab or culture.3,4
It is known that Actinomyces spp. can form biofilms when exposed to copper, potentially enhancing its degradation.4 It has been suggested that the presence of Actinomyces in the genitourinary tract of women with copper IUDs may enhance the degradation of the copper coil, increasing the risk of fragmentation.4,5 IUDs cause a local inflammatory response within the uterus, leading to tissue injury and necrosis. This process creates an anaerobic environment that is ideal for Actinomyces to flourish.6 The prevalence of Actinomyces among patients with IUDs is as high as 16%.5 The presence of Actinomyces spp. in the genital tract of women with IUDs more than doubles when the device is in place for longer than 4 years, therefore increasing the risk of developing further complications such as potential fragmentation and migration of the copper coil.5
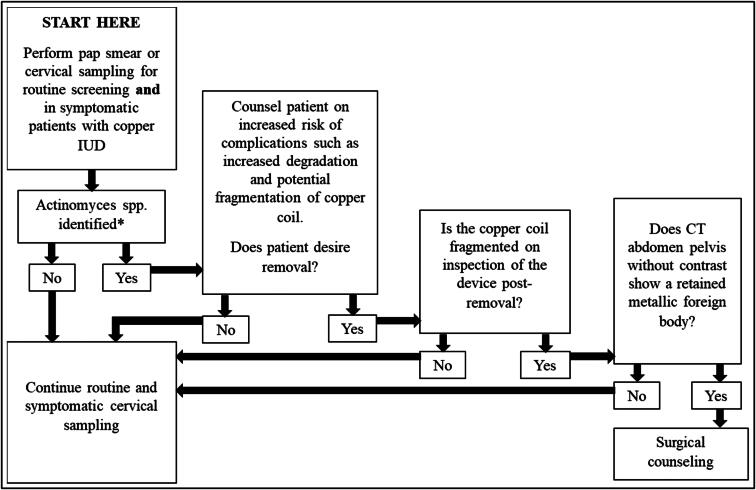
We have created an algorithm for management of Actinomyces spp. on routine or symptomatic cervical sampling of women with copper IUDs and copper coil fragmentation on removal of the device (Figure 2). We recommend counseling all patients with IUDs in place and Actinomyces found on cervical smear regarding potential complications such as copper coil fragmentation and migration. The timeline on when during the device’s life the risk for these potential complications increases is unknown. Our case, along with the evidence that Actinomyces spp. cause biofilm formation which potentially enhances copper oxidation and degradation, is highly suggestive of a causal relationship between Actinomyces and copper IUD fragmentation. If the patient chooses to have the IUD removed, we recommend close inspection of the device to ensure that the copper coil is not fragmented. If the coil is fragmented, we recommend obtaining a CT scan of the abdomen and pelvis without contrast rather than a radiograph to evaluate for the missing copper coil. If indeed a retained metallic foreign body is noted on CT, the patient should receive surgical counseling, as retained copper can cause peritoneal inflammation, increasing the risk of adhesions.3
Figure 2.
Management algorithm of Actinomyces spp. on cervical swab of patients with copper IUD in place. For this article, we are only discussing results for Actinomyces spp. identified on cervical sampling; however, if any other infectious organism is present on cervical sampling please treat appropriately.
ANSWERS TO CLINICAL QUESTIONS
Question 1, d. Neisseria spp., most notably Neisseria gonorrhoeae, are responsible for sexually transmitted infections in men and women. Having multiple sexual partners and having intercourse without using a condom can increase the risk of contracting a sexually transmitted infection, but having an IUD does not increase this risk. Lactobacillus and Bacteroides are normal pathogens in the vaginal flora; they are unchanged by the presence of an IUD. Actinomyces spp. are more prevalent in women with IUDs due to the local tissue injury from the device inside the uterus, which creates an anaerobic environment that allows this organism to flourish.
Question 2, b. CT scan of the abdomen and pelvis is the imaging modality most sensitive at locating retained metal fragments. The use of intravenous contrast in this study would potentially inhibit the ability to identify the metallic fragments. MRI is not recommended due to the magnetic field’s effect, which may cause the metal to migrate or heat up. Ultrasound may be able to identify a large fragment retained in the uterus; however, it is not as sensitive when trying to identify small fragments that may have migrated out of the uterus into the peritoneal cavity.
Disclosure statement/Funding
The planners and faculty for this activity have no relevant financial relationships or funding to disclose. The patient consented to publication of this case report.
References
- 1.Patai K, Balogh I, Szarvas Z.. Clinicopathological problems of the local tissue effect of the copper-releasing intrauterine contraceptive device (IUD). I. General characteristics of the copper-containing IUD (clinical study). Acta Chir Hung. 1989;30(2):129–132. [PubMed] [Google Scholar]
- 2.Berthou J, Chrétien FC, Driguez PA.. Dégradation in utero des DIU au cuivre en fonction du temps. Le phénomène de corrosion métallique. Etude au microscope électronique à balayage [Degradation of copper IUDs in utero. The process of metallic corrosion. A scanning electron microscope study]. Gynecol Obstet Fertil. 2003;31(1):29–42. doi: 10.1016/s1297-9589(02)00013-9. [DOI] [PubMed] [Google Scholar]
- 3.Dubovis M, Rizk N.. Retained copper fragments following removal of a copper intrauterine device: two case reports. Case Rep Womens Health. 2020;27:e00208. doi: 10.1016/j.crwh.2020.e00208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carrillo M, Valdez B, Vargas L, et al. In vitro Actinomyces israelii biofilm development on IUD copper surfaces. Contraception. 2010;81(3):261–264. doi: 10.1016/j.contraception.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 5.Evans DT. Actinomyces israelii in the female genital tract: a review. Genitourin Med. 1993;69(1):54–59. doi: 10.1136/sti.69.1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kelly J, Aaron J.. Pelvic actinomycosis and usage of intrauterine contraceptive devices. Yale J Biol Med. 1982;55(5-6):453–461. [PMC free article] [PubMed] [Google Scholar]