Abstract
Background
Hydatid disease, also known as echinococcosis, is an endemic parasitic infection, most commonly caused by Echinococcus granulosus. It may affect any organ resulting in the formation of hydatid cysts, but most frequently involves liver and lungs. Hydatid cyst arising primarily from axilla is an extremely rare manifestation of this condition, with only a few cases reported in medical literature.
Case presentation
Here we present the case of a 32-year-old Indian male farmer, who presented with a painless, slow-growing mass in the left axillary region of 8 months duration. Preoperative imaging led us to the diagnosis of primary axillary hydatid cyst, with no other associated cysts or masses anywhere else in the body. Following antihelmintic therapy, the cyst was surgically excised without rupture. The diagnosis was further confirmed by macroscopic and histopathological examination.
Conclusion
This case report highlights the importance of considering hydatid cyst in the differential diagnosis of palpable masses in the axillary region, especially in regions where the disease is endemic. Early recognition and accurate diagnosis are crucial for appropriate management and optimal patient outcomes.
Keywords: Hydatid cyst, Axilla, Echinococcosis
Background
Hydatid disease is a zoonotic disease caused by the larval form of Echinococcus granulosus and is still endemic in many agricultural and cattle-rearing countries [4, 19]. Dogs and other canids are the definitive host, and sheep are the common intermediate host. Humans are infected through the feco-oral route, by ingestion of food contaminated by dog feces that contain ova of the parasite or by direct contact with dogs.
Hydatid cysts are most commonly located in liver (50–80%) and lungs (15–47%), because the parasite’s embryos are mostly filtered by the hepatic sinusoids during their travel inside the portal system from the intestinal tissue after ingestion [8]. It has multiorgan involvement in 5–13% of cases, while 8–10% cases have rare localizations in the spleen, abdominal cavity, kidneys, brain, bone, pancreas, breast, pelvis, bladder, heart, ovaries, thyroid retroperitoneum, incision scar, or common bile duct [4, 19]. Primary soft-tissue involvement by hydatid cyst is unusual even in endemic areas, with an incidence of 0.5–4.7% [19]. Here, we report a rare case of primary axillary hydatid cyst without any other visceral involvement.
Case presentation
A 32-year-old Indian male farmer presented to us with complaints of a painless, gradually progressing swelling in the left axillary region for 8 months. There was no history of fever, weight loss, or any other swelling in the body.
On examination, there was a 10 × 8 cm soft-to-firm, well-defined, non-tender swelling in the left axillary region (Fig. 1). There was no other significant clinical finding.
Ultrasound sonography (USG) revealed a thick-walled lesion containing multiple cysts with no color uptake.
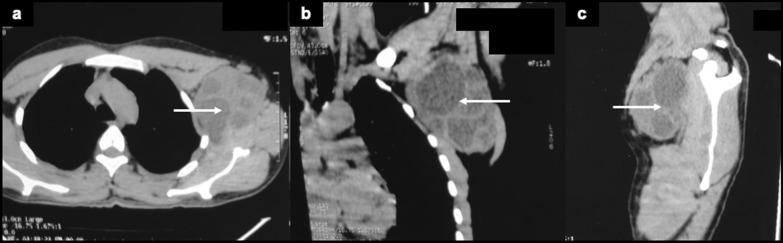
Contrast-enhanced computed tomography (CECT) showed a multi-loculated left axillary mass, with no evidence of any other organ involvement (Fig. 2).
Magnetic resonance imaging (MRI) revealed a 11 × 5.6 cm, heterogenous, T2 hyperintense cystic lesion with internal hypointense membranes and small cysts in intermuscular planes of left axilla, likely a hydatid cyst (Fig. 3)
Fig. 1.

Hydatid cyst in left axillary region
Fig. 2.
CECT scan—a Axial, b coronal, and c sagittal view showing the left axillary hydatid cyst (indicated by white arrows)
Fig. 3.

MRI—a T1 axial, b T1 coronal, c T2 axial, and d T2 coronal view showing the left axillary hydatid cyst (indicated by white arrows)
After diagnosis of primary hydatid cyst of axilla, our patient received albendazole 400 mg twice daily for three 28-day cycles separated by 2-week intervals. Thereafter, he underwent complete surgical excision of the axillary hydatid cyst. Care was taken to not breach the wall of the cyst to avoid spillage of the scolices and daughter cysts. On gross examination, multiple, thin-walled, white, opaque daughter cysts were found (Fig. 4a, b). Histopathology showed an acellular lamellated membrane, with an outer fibrotic layer consisting of palisading histiocytes and focal necrosis, suggestive of a hydatid cyst (Fig. 4c, d).
Fig. 4.

a Specimen of axillary hydatid cyst. b Cut open specimen showing the daughter cysts. c Low-power microscopic view d High-power microscopic view
The post-operative period was uneventful, and the patient was discharged with albendazole 400 mg twice daily for 4 weeks. The patient remains asymptomatic with no radiological evidence of recurrence at 18 months follow-up.
Discussion
Echinococcosis is a public health problem of global concern and is currently considered one of the “neglected tropical diseases” [20]. Hydatid cyst in the axilla can be considered to be primary only when no other cysts are present in any other part of the body [16]. Primary axillary hydatid cyst occurs as a result of dissemination of embryos of E. granulosus through hepatic and pulmonary filters, to eventually occupy atypical locations [7]. First reported in 1899, primary axillary hydatid cyst without involvement of any other organs is extremely rare, and only a handful of cases have been reported in published English literature since then. Table 1 summarizes the clinical presentations, investigations, and management of these cases [1–18]. Our case also showed primary involvement of axilla without evidence of any other visceral involvement.
Table 1.
Summary of reported cases of primary axillary hydatid cyst of axilla
| Author | Year | Age/gender | Clinical findings | Investigations | Preoperative diagnosis | Surgical intervention | Postoperative HPE |
|---|---|---|---|---|---|---|---|
| Jain et al. [1] | 2022 | 36/M | Painless swelling in the right axilla |
• USG • FNAC: suggestive of abscess • ZN stain: E. granulosus observed |
Primary axillary hydatid cyst | Total cystectomy | NA |
| Sisodia et al. [2] | 2022 | 25/M | Multiple erythematous papules and sinuses in the axilla | • Punch biopsy from axillary nodule | Axillary hydatid cyst with granulomatous reaction |
NA Patient lost follow up |
NA |
| Rai et al. [3] | 2020 | 45/M | Sudden increase in size of a chronic swelling in the right axilla |
• USG of the swelling suggested abscess • CT of the thorax • Postoperative CT of the abdomen and pelvis |
Axillary abscess | Incision and drainage, followed by evacuation of all daughter cysts | Confirmed as hydatid cyst |
| Karadeniz et al. [4] | 2018 | 40/F | Swelling and pain in the right axillary region |
• Mammary USG • Postoperative CT of the abdomen and thorax |
Axillary lymphadenopathy |
Axillary lymph node excision planned On exploration, found to be hydatid, so the cyst was excised with germinal membrane |
NA |
| Kafadar et al. [5] | 2017 | 24/F | Painful left axillary swelling |
• USG of axilla • CT of the abdomen and thorax • Breast MRI |
Cystic lesion in left axilla? Lymphocele | Total cystectomy | Confirmed as hydatid cyst |
| Umeshchandra et al. [6] | 2014 | 20/F | Painless swelling in left axilla |
• USG • FNAC: inconclusive • CXR and USG whole abdomen |
NA | Total cystectomy | Confirmed as hydatid cyst |
| Mercuţ et al. [7] | 2014 | 60/F | Painless swelling in the right axillary region |
• USG • CT of the thorax, abdomen, and pelvis • USG-guided puncture |
Primary axillary hydatid cyst | Total cystectomy | Confirmed as hydatid cyst |
| Yagmur et al. [8] | 2012 | 73/M | Pain and swelling in the left axilla |
• Echinococcal IHA: negative • Axillary USG: suggestive of multiloculated hydatid cyst • CT of the abdomen and thorax |
Primary axillary hydatid cyst | Complete excision of all cysts including the surrounding fibrous tissue | NA |
| Saylam et al. [9] | 2012 | 36/F | Painless soft swelling in right axilla |
• USG • CT of the thorax and abdomen • Echinococcal hemagglutination test: positive |
Cystic SOL in the right axilla | Excision of the cyst | Confirmed as hydatid cyst |
| Zangeneh et al. [10] | 2012 | 33/F | Painless right axillary swelling |
• USG axillary region • CXR and USG of the abdomen and pelvis • Hydatid IgG and ELISA test: negative |
Cystic SOL in right axilla | Excision of the cyst | Confirmed as hydatid cyst |
| Arsalane et al. [11] | 2012 | 43/M | Painless cystic swelling in left axilla | • USG and CT |
Hydatid cyst? Vascular malformation? |
Excision of the lesion | Confirmed as hydatid cyst |
| Ünalp et al. [12] | 2011 | 48/F | Painless swelling in the left axilla |
• USG • CT of the thorax • FNAC: suggested hydatid disease • Indirect echinococcal hemagglutination test: positive |
Primary axillary hydatid cyst | Complete excision of the cyst without rupture | Confirmed as hydatid cyst |
| Ozsoy et al. [13] | 2011 | 45/F | Painless mass in the left axilla |
• USG abdomen • CXR • USG axillary region • CT of abdomen, thorax and brain • Whole body bone scintigraphy • Hydatid serology: negative |
Axillary lymphadenopathy | Excision of the mass | Confirmed as hydatid cyst |
| Singh et al. [14] | 2009 | 28/M | Recurrent swelling in the left axilla | Recurrent subcutaneous hydatid cyst | Total cystectomy | Confirmed as hydatid cyst | |
| Borovik et al. [15] | 2006 | 31/F | Painful left axillary mass |
• Multiple excisional biopsies • Hydatid serological testing: positive |
Initially diagnosed as necrotic granulomatous lymphadenitis. Finally diagnosed as axillary hydatid | Treated with albendazole therapy | Confirmed as hydatid cyst |
| Losanoff et al. [16] | 2004 | 38/M | Painless pedunculated soft tumor in the left axilla |
• Hydatid serology: negative • Postoperative CT of the thorax and abdomen |
NA | Excision of mass under local anesthesia | Confirmed as hydatid cyst |
| Unal et al. [17] | 2001 | 53/F | Painful mass in right axilla |
• MRI: lobular cystic mass localized in right pectoralis major muscle • Echinococcal hemagglutination test: positive |
Primary axillary hydatid cyst | Excision of the cystic mass | Confirmed as hydatid cyst |
| Thomson [18] | 1899 | 2/F | Painless mass in the right axilla | NA | Cystic SOL in right axilla | Excision of the cystic mass | Confirmed as hydatid cyst |
CXR, chest radiography; ELISA, enzyme-linked immunoassay; FNAC, fine needle aspiration cytology; IHA, indirect hemagglutination; ZN, Ziehl–Neelsen
Clinical features depend on cyst site, size, pressure effects, and complications including rupture, infection, and immunologic reactions. Patients with axillary hydatid cyst usually present in the age between 25 and 45 years, with a female preponderance. The most common symptom is a gradually increasing mass with pain and discomfort. Our patient was a 32-year-old male and presented with a painless palpable mass in the left axilla, which is the common clinical feature. The differential diagnosis of a cystic axillary lesion can be:
-
(i)
Non-parasitic cysts (ganglionic or inclusion cysts and cystic hygroma).
-
(ii)
Parasitic cysts (coenurosis, toxoplasmosis, filariasis, and echinococcosis) [16].
Diagnosis is mainly based on radiological investigations and may be aided by serology. Ultrasonography, CECT, and MRI help to visualize the cyst’s relation to surrounding tissues, the wall of the cyst, and intraluminal daughter cysts. Imaging helps not only in diagnosis but also in cyst staging and follow-up after treatment [21]. However, when a cyst has atypical features, it is difficult to distinguish it from simple subcutaneous cyst, necrotic tumor, hematoma, or lymph node. In our patient, imaging confirmed the diagnosis and also helped in surgical planning. Serological tests can confirm diagnosis and are also useful for follow-up, but have a false positivity rate up to 33% [22]. Diagnostic aspiration cytology carries the risk of anaphylaxis, infection, and dissemination. In the cases reported so far in literature, some were diagnosed by radiological investigations [7, 8, 10, 11] and some by FNAC [1, 12] while most were diagnosed and confirmed only by intraoperative findings along with postoperative histopathological examination [2–6, 9, 13–18]. The indirect echinococcal hemagglutination test was positive in few cases [9, 12, 15, 17].
A preoperative diagnosis is important to avoid rupture and spillage of contents in systemic circulation during excision, which may lead to dissemination to distant organs to form additional cysts, local recurrence, and anaphylaxis.
Surgery remains the most effective treatment for soft-tissue hydatid disease. Total cystectomy with fibrous adventitia is the curative treatment [8]. The main principle of surgical treatment is to prevent complications such as compression of adjacent structures, infection, and cyst rupture.
Medical therapy is indicated for preoperative preparation, prophylaxis against postoperative recurrences, disseminated disease, pluri-visceral hydatid disease, and patients with contraindications for surgery or who cannot undergo radical surgery. Preoperative treatment with benzimidazole carbamate group of antibiotics has been reported to soften the cysts and to reduce intracystic pressure, enabling the surgical excision [23]. The most commonly used parasiticidal drugs from the above group are mebendazole (50 mg/kg/day) and albendazole (10 mg/kg/day in two divided doses), with the latter having better absorptive properties. It is recommended for a minimum period of 4 weeks preoperatively. Better results have been seen when three 28-day courses of 10 mg/kg/day in divided doses is given, separated by 2-week intervals. The drug acts by blocking glucose uptake in the parasite and depleting its glycogen store. However, experience with anti-helminthic agents in the treatment of soft-tissue hydatid disease is limited [7].
Our patient received albendazole 400 mg twice daily for three 28-day cycles separated by 2-week intervals. Following total cyst excision without rupture, he received postoperative albendazole 400 mg twice daily for another 4 weeks. No complications or recurrences were observed to date on follow-up.
Conclusion
Although primary axillary hydatid cyst is extremely rare, it should be considered as a differential diagnosis, when a patient presents with painless progressive cystic swelling in the axilla. Clinicians, particularly in endemic regions, should be aware of the possibility of hydatid cysts in patients presenting with soft-tissue masses anywhere in the body, to avoid preventable complications.
Acknowledgements
Not applicable.
Author contributions
The manuscript was conceptualized by SC. JC wrote the first draft. The draft was further modified by SC. UC prepared images of the slides and did a detailed literature review. All authors (JC, SC, PB, and UC) went through the final manuscript and approved it for submission.
Funding
No funding was received for this study.
Availability of data and materials
All data are included in the article.
Declarations
Ethics approval and consent to participate
As the report includes details of a patient, where standard care was given, the Institutional Ethics Committee approval was waived.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
None of the authors have any competing interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Jain MA, Jain C, Chakole S. Case presentation of axillary swelling as hydatid cyst. Med Sci. 2022;26(130):01–5. 10.54905/disssi/v26i130/ms523e2567. [Google Scholar]
- 2.Sisodia SM, Ansari SAH, Bera SK, Mahajan VR. Hydatid cyst of axilla masquerading as scrofuloderma. Sahel Med J. 2013;16(2):80. 10.4103/1118-8561.115271. [Google Scholar]
- 3.Rai L, Ahmed R, Abbasi M, Khan H, Abbas S. Primary hydatid cyst of the axilla presenting as axillary abscess. Eur J Med Case Rep. 2020. 10.24911/ejmcr/173-1583516292. [Google Scholar]
- 4.Karadeniz E, Yur M, Akçay MN, Atamanalp SS. Primary hydatid cyst in the axillary region: a case report. Iran J Parasitol. 2018;13(2):328–30. [PMC free article] [PubMed] [Google Scholar]
- 5.Kafadar MT, Çetinkaya İ. Primary hydatid disease of the axilla presenting as a cystic mass. J Surg Case Rep. 2017. 10.1093/jscr/rjx219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Umeshchandra DG, Patil SM, et al. Primary hydatid cyst in axillary region: a rare presentation. Scholars J Med Case Rep. 2014;2(7):464–6. 10.36347/sjmcr.2014.v02i07.013. [Google Scholar]
- 7.Mercuţ D, Andriţoiu A, Traşcă E, Siloşi C, Resceanu A, Mercuţ R. Primary axillary hydatid cyst. Chirurgia (Bucur). 2014;109(4):559–62. [PubMed] [Google Scholar]
- 8.Yagmur Y, Akbulut S. Unusual location of hydatid cysts: a case report and literature review. Int Surg. 2012;97(1):23–6. 10.9738/CC85.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saylam B, Vural V, Duzgun AP, Ozer MV, Coskun F. Primary hydatid cyst of the axilla: report of a case. Med Princ Pract. 2012;21(1):79–81. 10.1159/000331900. [DOI] [PubMed] [Google Scholar]
- 10.Zangeneh M, Amerion M, Siadat SD, Alijani M. Primary hydatid cyst of the axillary region: a case report. Case Rep Med. 2012;2012:1–4. 10.1155/2012/362610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arsalane A, El Hammoumi M, El Oueriachi F, Traibi A, Darbi A, el Kabiri H. Primary axillary hydatid cyst. Gen Thorac Cardiovasc Surg. 2012;60(6):359–62. 10.1007/s11748-012-0004-8. [DOI] [PubMed] [Google Scholar]
- 12.Ünalp HR, Kamer E, Rezanko T, Kılıç Ö, Tunakan M, Önal MA. Primary hydatid cyst of the axillary region: a case report. Balkan Med J. 2011;2011(2):209–11. [Google Scholar]
- 13.Ozsoy M, Keles C, Kahya M, Keles G. Primary echinococcal cyst in the axillary region. J Infect Dev Ctries. 2011;5(11):825–7. 10.3855/jidc.1589. [DOI] [PubMed] [Google Scholar]
- 14.Singh S, Khichy S, Singh M, Gill JS. Recurrent solitary hydatid cyst of the subcutaneous tissue. Indian J Surg. 2009;71(3):162–4. 10.1007/s12262-009-0044-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Borovik A, Massasso D, Gibson K. Axillary hydatid disease. Med J Aust. 2006;184(11):585. 10.5694/j.1326-5377.2006.tb00387.x. [Google Scholar]
- 16.Losanoff JE, Richman BW, Jones JW. Primary hydatid cyst of the axilla. ANZ J Surg. 2004;74(5):393–4. 10.1111/j.1445-1433.2004.03002.x. [DOI] [PubMed] [Google Scholar]
- 17.Unal AE, Ulukent SC, Bayar S, Demirkan A, Akgül H. Primary hydatid cyst of the axillary region: report of a case. Surg Today. 2001;31(9):803–5. 10.1007/s005950170051. [DOI] [PubMed] [Google Scholar]
- 18.Thomson PJ. Hydatid cyst of the axilla in a child. Lancet. 1899;153:25–6. [Google Scholar]
- 19.Sachar S, Goyal S, Goyal S, Sangwan S. Uncommon locations and presentations of hydatid cyst. Ann Med Health Sci Res. 2014;4(3):447–52. 10.4103/2141-9248.133476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Neglected tropical diseases. [Jan; 2024]. 2024. https://www.who.int/health-topics/neglected-tropical-diseases.
- 21.Abbasi B, et al. Computed tomography and magnetic resonance imaging of hydatid disease: a pictorial review of uncommon imaging presentations. Heliyon. 2021;7(5): e07086. 10.1016/j.heliyon.2021.e07086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Biava MF, Dao A, Fortier B. Laboratory diagnosis of cystic hydatic disease. World J Surg. 2001;25(1):10–4. 10.1007/s002680020002. [DOI] [PubMed] [Google Scholar]
- 23.Pawlowski Z, Eckert SJ, Vuitton DA, Ammann RW, Kern P, Craig PS, et al. Echinococcosis in humans: clinical aspects, diagnosis and treatment. In: Eckert J, Germmell MA, Meslin F-X, Pawlowski ZS, editors., et al., WHO/OIE Manual on Echinococcus in Humans and Animals: a Public Health Problem of Global Concern. Paris, France: World Organisation for Animal Health; 2011. p. 20–66. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are included in the article.