Abstract
Background
Distal radius fractures are highly prevalent among older adults. Ulnar styloid fractures frequently accompany distal radius fractures, raising concerns about treatment outcomes due to the risk of distal radioulnar joint (DRUJ) instability. This study investigated the necessity of surgical intervention (open reduction internal fixation; ORIF) for distal radius fractures in very old patients with coexisting ulnar styloid fractures.
Materials and methods
A retrospective analysis of 96 patients aged ≥ 80 years with AO classification 23-A2 to 23-B3 distal radius fractures with concomitant ulnar styloid fracture between 2019 and 2022 was performed. Patients were excluded if they were aged < 80 years, had a preinjury Barthel index of < 90, or had high-energy multiple trauma. The primary outcome was the Disabilities of the Arm, Shoulder, and Hand (DASH) score assessed at 3, 6, and 12 months. We compared the DASH score and their trajectories between the ORIF and conservative treatment groups.
Results
ORIF group demonstrated significantly better DASH functional scores (25.31 ± 4.71) at the 12-month follow-up compared with the conservative group (34.42 ± 8.03; p < 0.001). Treatment choice was identified as a significant predictor of DASH scores at 12 months, with ORIF significantly improved patient’s wrist function and demonstrated a β coefficient of − 9.11 (95% confidence interval: −11.95 to − 6.27, p < 0.001). The other factors investigated, namely age, lowest T-score, and medical history of diabetes mellitus, hypertension, coronary artery disease, cerebrovascular accidents, cancer, and dementia, did not exhibit a significant association with the 12-month DASH scores in the adjusted model (p > 0.05).
Conclusions
Our findings suggest that very old patients with distal radius fracture accompanied by ulnar styloid fractures may benefit from ORIF to achieve optimal long-term functional recovery.
Keywords: Distal radius fractures, Distal ulna fractures, Distal radioulnar joint instability, Elderly
Introduction
Distal radius fractures are a highly common upper extremity injury in adults aged older than 65 years. Predisposing factors in this population include low bone mineral density [1–5]. Notably, ulnar styloid fractures accompany distal radius fractures in approximately half of all cases (44–65%) [1, 2]. Concomitant fractures can compromise the stability of the distal radioulnar joint (DRUJ). DRUJ instability can lead to painful and limited forearm rotation, DRUJ arthritis, pain on the ulnar side of the wrist, decreased grip strength, and poor functional outcomes [3, 4].
The DRUJ, a complex synovial-lined pivot joint, forms a distal articulation between the ulnar head and the radial sigmoid notch. Biomechanical studies have suggested the critical role of DRUJ in maintaining wrist stability, particularly during forearm rotation. Although bony structures contribute approximately 20% to joint stability, the remaining 80% relies on a combination of intrinsic and extrinsic soft tissue stabilizers. The ulnar styloid serves as a vital anchor for the triangular fibrocartilage complex (TFCC) on the ulnar side. The TFCC complex acts as the primary stabilizer of the DRUJ. Other secondary stabilizing structures include the dorsal and volar radioulnar ligaments, distal interosseous membrane, extensor carpi ulnaris, palmar osteocartilaginous lip of the sigmoid notch, and pronator quadrates [5, 6]. Several anatomical and biomechanical studies have explored the influence of ulnar styloid fracture location and the quality of reduction of distal radius fractures on DRUJ stability [7–13]. Fractures at the base of the ulnar styloid can damage the deep fovea, the attachment point for the primary stabilizer TFCC, potentially leading to DRUJ instability [3, 4, 14]. However, adequate reduction of the distal radius alone in patients with ulnar styloid fractures can act as a protective factor, mitigating the development of DRUJ instability [7, 8, 15].
Distal radius fractures in older adults with multiple comorbidities are often left untreated, with research indicating no significant difference in patient outcomes based on treatment choice [9, 10, 16]. However, the patients in these studies did not present with ulnar styloid fractures, which can further destabilize the DRUJ. DRUJ instability can limit wrist function and range of motion, adversely affecting the daily activities of active older patients. Notably, no study has addressed the need for treating distal radius fractures with concurrent ulnar styloid fractures in this population. This study explored the potential compensatory mechanisms underlying the mitigation of DRUJ instability when treating distal radius fractures alone and neglecting the concurrent ulnar styloid fractures. We hypothesized that ORIF of the distal radius fracture alone could act as a protective factor in preventing DRUJ instability, complications and promise a good wrist functional outcome in the future.
Materials and methods
Patient population
A retrospective review of the data collected from 356 patients who had distal radius fractures classified as AO 23-A2 to AO 23-B3 between January 1, 2019, and December 31, 2022 was undertaken. Our study aimed to compare functional outcomes in older adults with distal radius fracture and ulnar styloid fractures who received either conservative or surgical treatment. The study was conducted in Hualien Tzu Chi Hospital and was in accordance with the Declaration of Helsinki and approved by the Research Ethics Committee of Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation (IRB112-035-B and date of approval: February/27/2023). Written informed consent for publication was obtained from all patients included in this study. From this cohort, 96 patients aged > 80 years with coexisting ulnar styloid fractures were included in the comparative analysis (Fig. 1). A rigorous exclusion process was implemented on the basis of the following criteria: age < 80 years (n = 52); preinjury Barthel index < 90 (n = 30); the presence of isolated distal radius fractures without ulnar styloid fractures (n = 82); the presence of accompanying ulnar neck (n = 7) or shaft fractures (n = 5); the presence of high-energy multiple trauma (n = 5); a follow-up period of less than 1 year (n = 45); loss to follow-up (n = 12), and repeated cases (n = 22). Following exclusion, the patients were included in this study.
Fig. 1.
Flow chart of patient selection of this study
Surgical and conservative treatment group
The patients were categorized into two groups based on their treatment modality: conservative management or surgical intervention. The surgical group consisted of patients who underwent open reduction and internal fixation (ORIF), while the conservative group included those who did not receive surgery. According to medical records, all patients were initially advised to undergo ORIF, primarily due to the presence of a concomitant ulnar styloid fracture, which raised concerns about DRUJ instability. However, the final decision regarding surgical intervention was made by the patients themselves, often in consultation with their families, taking into account personal preferences, concerns, and medical considerations. The surgical treatment group underwent treatment with ORIF of the distal radius alone by using the volar Henry approach and distal radius locking plates. Notably, ulnar styloid fractures were not fixed using Kirschner wires or plating. All of the surgical procedure was performed under propofol-based total intravenous general anesthesia method and the propofol dose was maintained with target-controlled infusion (TCI). All of the surgically treated patients were monitored by intra-operative bispectral index (BIS) monitors and the BIS levels were maintained between 40 and 60. All surgical procedures were performed by four experienced trauma surgeons, each with an annual caseload exceeding 100 trauma procedures.
All patients followed a standardized rehabilitation protocol to optimize functional recovery. Initially, supination sugar-tong splinting was applied for approximately 4 weeks following the injury to ensure proper immobilization and support. After this immobilization period, patients began with gentle passive range-of-motion exercises under the supervision of a physiotherapist, aimed at gradually restoring mobility while minimizing stress on the healing structures. As recovery progressed, active-assisted exercises were introduced to enhance wrist and forearm strength, followed by strengthening and endurance exercises as tolerated by the patient. Typically, full wrist mobility and load-bearing activities were reintroduced around 3 months post-injury, depending on individual recovery. Throughout the rehabilitation process, patient progress was closely monitored, and adjustments to the treatment plan were made to accommodate the pace of each patient’s recovery.
Primary and secondary outcomes
The primary outcome was the Quick Disabilities of the Arm, Shoulder, and Hand (Quick DASH) score assessed at 3, 6, and 12 months posttreatment. This comprehensive approach allowed for a detailed analysis of functional outcomes and recovery trajectories in this specific patient population of older adults.
Preoperative radiographs were employed to classify distal radius fractures and the associated ulnar styloid fractures according to the AO classification system. Postoperative radiographs were used to assess DRUJ incongruity, the quality of reduction of the distal radius fracture after ORIF with locking plate, and the progress of distal radius fracture with ulna styloid fracture in the nonsurgery group. Radiographic data were collected for all patients throughout a 1-year follow-up period. Demographic information and medical history were obtained for each participant. Medical history data focused on the presence of comorbidities such as diabetes mellitus, hypertension, congestive heart failure, coronary artery disease, arrhythmias, and cerebrovascular accidents.
All statistical analyses were performed using SPSS version 23.0 (IBM, Armonk, NY, USA). Categorical data are presented as frequencies and proportions. Chi-square tests were employed for assessing qualitative data. Age, T scores, and DASH score data were analyzed using descriptive statistics and presented using means and standard deviations. One-way analysis of variance was employed to compare continuous data between the conservative and surgical treatment groups. The Cochran-Armitage test was used to evaluate the temporal trends in DASH scores within each treatment group. Linear regression analysis was conducted to identify potential factors associated with the DASH score at the 12-month follow-up. The independent covariates included age, treatment group, lowest T score, and comorbidities with prevalence more than 6%. A p value of < 0.05 was considered statistically significant.
We used G*Power 3.1.9.2 to calculate the sample size needed. For evaluating the association between the DASH score at the 12-month follow-up and covariates via multiple linear regression, we set effect size of 0.24, α of 0.05, power (1-β) of 0.80, and number of predictors of 15 then got the estimated minimum sample size 92.
Results
Preoperative patient characteristics
A total of 96 patients were recruited and categorized by treatment modality into conservative (n = 57) and ORIF (n = 39) groups (Table 1). A significant difference in age between the groups was not observed (p = 0.248). The mean age for the entire cohort was 84.56 ± 4.29 years. The average T-score, which is an indicator of bone mineral density, was − 2.84 ± 0.73 across all patients, with no significant difference between the treatment groups (p = 0.532). The distribution of AO classification for distal radius fractures was comparable between groups (p = 0.633). Type 23-A2 fractures were present in 8 cases in the conservative group and 5 in the ORIF group; type 23-A3 in 14 and 10 cases; type 23-B1 in 15 and 10 cases; type 23-B2 in 13 and 9 cases; and type 23-B3 in 7 and 5 cases, respectively (Table 1). All ulnar styloid fractures of these patients were located at the base of the styloid process. They also underwent preoperative assessment of DRUJ stability using the ballottement test. The ballottement test was performed to evaluate DRUJ instability by palpating and attempting to displace the ulna relative to the radius. All of them exhibited a positive ballottement test preoperatively, indicating some degree of DRUJ instability. The prevalence of most comorbidities (e.g., diabetes mellitus, hypertension, cerebrovascular accidents, and liver cirrhosis) did not significantly differ between the groups (p = 0.297 to 1.000). However, a significantly higher prevalence (p = 0.024 to 0.045) of congestive heart failure, coronary artery disease, and arrhythmia was observed in the conservative group compared with the ORIF group.
Table 1.
Demographics (n = 96)
| Item | Group | p-value | ||
|---|---|---|---|---|
| Conservative | ORIF | Total | ||
| N | 57 | 39 | 96 | |
| Age | 84.98 ± 4.77 | 83.95 ± 3.44 | 84.56 ± 4.29 | 0.248 |
| Lowest T score | -2.80 ± 0.65 | -2.89 ± 0.84 | -2.84 ± 0.73 | 0.532 |
| Distal Radius Fracture AO classification | 0.633 | |||
| 23-A2 | 8 | 5 | 13 | |
| 23-A3 | 14 | 10 | 24 | |
| 23-B1 | 15 | 10 | 25 | |
| 23-B2 | 13 | 9 | 22 | |
| 23-B3 | 7 | 5 | 12 | |
| Medical history | ||||
| DM | 11 (19.3%) | 11 (28.2%) | 22 (22.9%) | 0.308 |
| HTN | 43 (75.4%) | 27 (69.2%) | 70 (72.9%) | 0.501 |
| CHF | 10 (17.5%) | 1 (2.6%) | 11 (11.5%) | 0.025* |
| CAD | 21 (36.8%) | 7 (17.9%) | 28 (29.2%) | 0.045* |
| Arrythmia | 11 (19.3%) | 1 (2.6%) | 12 (12.5%) | 0.024* |
| CVA | 6 (10.5%) | 7 (17.9%) | 13 (13.5%) | 0.297 |
| Liver cirrhosis | 1 (1.8%) | 0 (0.0%) | 1 (1.0%) | 1.000 |
| Cancer | 3 (5.3%) | 3 (7.7%) | 6 (6.3%) | 0.684 |
| CKD | 0 (0.0%) | 1 (2.6%) | 1 (1.0%) | 0.406 |
| Hypothyroidism | 0 (0.0%) | 1 (2.6%) | 1 (1.0%) | 0.406 |
| Dementia | 13 (22.8%) | 11 (28.2%) | 24 (25.0%) | 0.549 |
| Duodenal ulcer | 4 (7.0%) | 1 (2.6%) | 5 (5.2%) | 0.645 |
Data are presented as n or mean ± standard deviation; *p-value < 0.05 was considered statistically significant after test; DM diabetes mellitus; HTN hypertension; CHF congestive heart failure; CAD coronary artery disease; CVA cerebrovascular accident; CKD chronic kidney disease
Post-treatment functional score at follow-up duration
All of the quality of reduction of the distal radius fracture after ORIF with locking plate were recorded and the reduction was good including the parameter of radial height, radial inclination and volar tilting [17]. At the 3-month follow-up, the conservative group exhibited a significantly lower DASH score (43.19 ± 6.60) than did the ORIF group (49.54 ± 5.10; p < 0.001). The average DASH score for the entire cohort at 3 months was 45.77 ± 6.77. No statistically significant difference in DASH score was observed between the groups at the 6-month follow-up. The conservative group maintained a score of 38.65 ± 7.30, and the ORIF group maintained a score of 36.72 ± 4.55 (p = 0.146). At the 12-month follow-up, which represents a crucial benchmark in a patient’s recovery, the surgical group demonstrated significantly better functional outcomes than did the conservative treatment group. The DASH score in the ORIF group was 25.31 ± 4.71, and that in the conservative treatment group was 34.42 ± 8.03 (p < 0.001). These findings suggest that patients in the ORIF group achieved superior upper limb function at the 1-year follow-up mark (Table 2).
Table 2.
Functional DASH score at follow up duration (n = 96)
| Item | Group | p-value | ||
|---|---|---|---|---|
| Conservative | ORIF | Total | ||
| N | 57 | 39 | 96 | |
| Post-OP | ||||
| 3-month DASH score | 43.19 ± 6.60 | 49.54 ± 5.10 | 45.77 ± 6.77 | < 0.001* |
| 6-month DASH score | 38.65 ± 7.30 | 36.72 ± 4.55 | 37.86 ± 6.37 | 0.146 |
| 12-month DASH score | 34.42 ± 8.03 | 25.31 ± 4.71 | 30.72 ± 8.19 | < 0.001* |
Data are presented as n or mean ± standard deviation; *p-value < 0.05 was considered statistically significant after test; DASH disabilities of the arm, shoulder, and hand
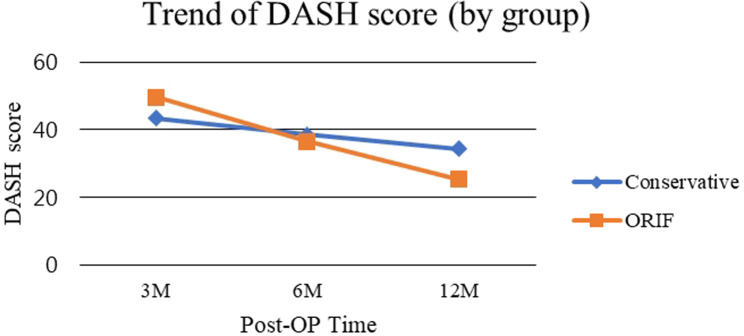
Both treatment groups exhibited significant improvements in upper limb function over the 1-year follow-up period (p for trend < 0.001). The average DASH score in the conservative group demonstrated a notable improvement, from 43.19 ± 6.60 at 3 months to 34.42 ± 8.03 at 12 months. Similarly, the DASH score in the ORIF group improved from 49.54 ± 5.10 at 3 months to 25.31 ± 4.71 at 12 months postoperatively (Table 3). A visual representation of the DASH scores over time is presented in Fig. 2. The conservative treatment group initially had lower scores compared with the ORIF group at 3 months. However, the trends intersected at 6 months, and by 12 months, the average DASH score in the conservative treatment group surpassed that of the score in the ORIF group.
Table 3.
The temporal trend of DASH score between the group (n = 96)
| Group | N | Post-OP 3 M | Post-OP 6 M | Post-OP12M | p for trend |
|---|---|---|---|---|---|
| Conservative | 57 | 43.19 ± 6.60 | 38.65 ± 7.30 | 34.42 ± 8.03 | < 0.001* |
| ORIF | 39 | 49.54 ± 5.10 | 36.72 ± 4.55 | 25.31 ± 4.71 | < 0.001* |
| Between Group p-value | < 0.001* | 0.146 | < 0.001* |
Data are presented as n or mean ± standard deviation; *p-value < 0.05 was considered statistically significant after test; DASH disabilities of the arm, shoulder, and hand
Fig. 2.
The plot chart of the temporal trend of DASH score between the group
Factors affecting functional score at 12th month follow-up
An adjusted linear regression analysis was conducted to identify factors influencing the DASH score at the 12-month follow-up, accounting for potential confounding variables. The analysis revealed that treatment choice was a statistically significant factor. Patients who underwent ORIF for their distal radius fracture demonstrated a β coefficient of − 9.11 (95% confidence interval: −11.95 to − 6.27, p < 0.001). This result implies that ORIF significantly improved a patient’s wrist function when accompanied by a concurrent ulnar styloid fracture. The other factors investigated, namely age, lowest T-score, and medical history of diabetes mellitus, hypertension, coronary artery disease, cerebrovascular accidents, cancer, and dementia, did not exhibit a significant association with the 12-month DASH scores in the adjusted model (p > 0.05; Table 4).
Table 4.
Factors associated with DASH score at 12M (n = 96)
| Item | Crude | Adjusted | ||
|---|---|---|---|---|
| β (95% CI) | p-value | β (95% CI) | p-value | |
| Age | 0.38 (0.001, 0.77) | 0.049* | 0.27 (-0.08, 0.62) | 0.127 |
| Group | ||||
| Conservative | Reference | Reference | ||
| ORIF | -9.11 (-11.95, -6.27) | < 0.001* | -8.88 (-11.98, -5.79) | < 0.001* |
| Lowest T score | -0.06 (-2.35, 2.23) | 0.959 | -0.63 (-2.65, 1.39) | 0.536 |
| DM (Y vs. N) | -0.34 (-4.31, 3.63) | 0.864 | 1.59 (-2.12, 5.29) | 0.398 |
| HTN (Y vs. N) | 1.88 (-1.85, 5.62) | 0.320 | 0.01 (-3.57, 3.59) | 0.996 |
| CHF (Y vs. N) | 2.88 (-2.32, 8.09) | 0.274 | 0.39 (-4.63, 5.42) | 0.877 |
| CAD (Y vs. N) | 0.95 (-2.71, 4.62) | 0.608 | -3.07 (-6.88, 0.74) | 0.113 |
| Arrythmia (Y vs. N) | 5.56 (0.64, 10.48) | 0.027* | 4.30 (-0.93, 9.52) | 0.106 |
| CVA (Y vs. N) | 0.06 (-4.82, 4.94) | 0.981 | 2.11 (-2.26, 6.48) | 0.340 |
| Cancer (Y vs. N) | -1.12 (-8.01, 5.77) | 0.747 | -1.18 (-7.27, 4.91) | 0.701 |
| Dementia (Y vs. N) | -1.68 (-5.52, 2.16) | 0.387 | -1.48 (-4.87, 1.91) | 0.387 |
Data are presented as β (95% CI); *p-value < 0.05 was considered statistically significant after test; CI confidence interval; DM diabetes mellitus; HTN hypertension; CHF congestive heart failure; CAD coronary artery disease; CVA cerebrovascular accident
Discussion
In our study, patients with a preinjury Barthel index score of < 90 were excluded because they were inactive and normally accompanied with multiple comorbidities and the functional restoration of the wrist was not as important as in active group. Thus, conservative treatment was normally adequate in this group and the potential benefit of surgical intervention might be limited. Therefore, we excluded inactive patients as to see the result of functional restoration in active elderly patients. Additionally, patients with high-energy multiple trauma were excluded due to the increased likelihood of comminuted distal radius fractures among such patients. These complex fractures often result in poorer long-term wrist function, regardless of the presence of ulnar styloid fractures. Furthermore, high-energy multiple trauma can lead to high morbidity in patients if accompanied by injuries to other visceral organs. All participants in our study had osteoporosis, a highly prevalent condition in the older adult population. Notably, these patients also reported engaging in a high level of daily activities, increasing their vulnerability to distal radius fractures with concomitant ulna styloid fractures. Significantly higher rates of congestive heart failure, coronary artery disease, and arrhythmia were observed in the conservative group. This might be partially explained by past clinical practices, where conservative treatment was often favored by clinicians for older patients with multiple comorbidities and distal radius fractures. This approach aimed to minimize surgical risks and the burden of anesthesia [18]. However, older adults are now more physically active than before, using their upper limbs extensively for various daily activities. Furthermore, the government is currently spreading awareness about the prevention of osteoporosis in older patients. Medications such as estrogen, raloxifene, bisphosphonate, and calcitonin are increasingly used by older patients to increase bone density and mitigate bone loss through anabolic or antiresorptive mechanisms. These advancements, along with an overall improvement in quality of life for older patients, have led to a shift in clinical priorities. In contemporary practice, restoring functional capacity in the wrist of an active older patient is considered highly important. Previous studies have demonstrated that the co-occurrence of distal radius fractures and ulnar styloid fractures can further compromise wrist function by increasing the likelihood of DRUJ instability, with more than two-thirds of such cases exhibiting reduced range of motion, compromised wrist function, and ulnar-sided wrist pain if the DRUJ instability is left untreated [14, 19, 20]. These findings, combined with the improved quality of life observed in older patients, underscore the importance of treating distal radius fractures accompanied by ulna styloid fractures. Our study results suggest that surgical intervention for distal radius fractures in patients aged > 80 years, when accompanied by ulnar styloid fractures, may lead to better long-term functional restoration of the wrist. While we acknowledge that our study population represents a subset of the broader elderly population, we believe our findings have implications for a wider group in three aspects. First, our results likely represent the upper end of the spectrum of benefits from surgical intervention. For less active elderly patients, we would expect benefits to fall somewhere between our findings and those of studies on less active populations. Second, our study provides a valuable reference point for surgeons when discussing treatment options with elderly patients across various activity levels. Third, the positive outcomes in our high-functioning group suggest that age alone should not be a contraindication for surgical intervention.
Several studies have evaluated the effects of different characteristics of distal radius fractures on DRUJ instability. Nakamura et al. identified a correlation between the quality of distal radius reduction and specific parameters influencing DRUJ stability. These parameters included coronal shift = 2 mm, radial inclination < 12°, dorsal or volar angulation > 20°, and radial shortening = 5 mm [21–23]. Theoretically, correction of these deformities can restore DRUJ stability, whereas malunion leads to malposition of the soft tissues, which perturbs the tension within the DRUJ [23]. Stabilizers of the DRUJ, particularly the dorsal and volar radioulnar ligaments, which originate from the ulnar styloid base, are invariably compromised during ulnar styloid fractures. This combined injury (ulnar styloid and distal radius fractures) can elevate the risk of DRUJ instability (10–19%) [7, 23]. Lindau, 2005 [5] established a relationship between ulnar styloid base fractures and injuries to the TFCC, the primary soft tissue stabilizer of the DRUJ. The TFCC’s anatomical insertion site is the ulnar fovea, located at the base of the ulnar styloid process. Studies investigating the influence of foveal and styloid insertions on the TFCC have revealed that disruption of the foveal insertion was critical for joint instability [4, 7, 12, 23, 24]. Conversely, nonbase fractures of the ulnar styloid process may preserve TFCC integrity and maintain DRUJ stability [7]. Bombaci et al. [25] reported a high incidence of TFCC injury when coexisting ulnar styloid fractures accompanied distal radius intra-articular fractures extending to the sigmoid notch. Additionally, ulnar styloid fractures with a displacement exceeding 2 mm have also been associated with DRUJ instability [14]. All of these studies again highlighted the critical point for the poorer outcome of our result in the conservative treated group that the accompanied ulnar styloid fracture causes progressive malreduction of the distal radius fracture with loss of volar tilting, radial inclination, radial height, DRUJ instability and eventually arthritic change.
The DRUJ relies on a combination of bony structures and surrounding soft tissues for stability. Because the radius of curvature of the sigmoid notch is greater than that of the seat of the ulnar head, bony stabilizers of the DRUJ only contribute approximately 20% to overall joint stability [26, 27]. Although ulnar styloid fractures are known risk factors for TFCC injuries, numerous studies have reported that the peripheral TFCC region has a robust blood supply, allowing for healing after ligament approximation through anatomical reduction and immobilization of the distal radius [5, 10, 28]. Jupiter explained that plate fixation approximated the distal oblique bundle of the interosseous membrane and reduced the ulnar head to the sigmoid notch [29], thereby promoting the healing potential of the TFCC. Given these considerations, ORIF of the ulnar styloid is generally not recommended due to the technical challenges and potential complications associated with fixation, such as hardware-related problems and injuries to the dorsal ulnar sensory nerve [9, 30]. Studies have demonstrated that most patients treated with anatomic reduction of the distal radius alone achieved favorable functional outcomes and grip strength and remained asymptomatic during follow-up [9, 30–32]. Sammer et al. [2] evaluated DRUJ stability by using patient-reported criteria after treating distal radius fractures alone with ORIF when accompanied by ulnar styloid fractures. Their 1-year follow-up using the Michigan Hand Outcomes Questionnaire revealed no instances of future DRUJ instability. Moreover, the study indicated that the size, displacement, and healing status of the ulnar styloid fracture did not affect study outcomes as long as the distal radius was adequately fixed. These findings support the conclusion that ulnar styloid fractures may not affect subjective outcomes in patients receiving ORIF for distal radius fractures [8, 12]. Similar results were reported by Kim et al. [7], who demonstrated that concomitant ulnar styloid fractures did not affect DRUJ stability in patients with rigid distal radial fixation. However, some studies have speculated that the vascularization of the peripheral articular disk might diminish with age, potentially affecting healing potential [33]. Our study demonstrated a significantly better DASH score in the conservative group compared with the surgical group at the 3-month follow-up. This could be attributed to the potential disruption of volar musculature structures and stabilizing soft tissues during ORIF surgery, requiring additional recovery and rehabilitation time. The plotted trends also demonstrate a clear improvement in DASH scores for the surgical group, ultimately leading to a significantly lower DASH score (p < 0.001) compared with the conservative group at the 12-month follow-up. Distal radius fractures with concomitant ulnar styloid fracture can introduce considerable instability at the fracture site and the DRUJ itself. In our study, most patients in the conservative group exhibited progressive fracture displacement, malunion, and DRUJ instability at the 12-month follow-up, leading to a decline in functional scores and persistent ulnar-sided wrist pain. Therefore, the conservative group demonstrated considerably lower functional outcomes compared with the ORIF group at the 1-year mark. These findings align with those of several studies, suggesting that active older patients benefit from the anatomical ORIF of distal radius fractures with concomitant ulnar styloid fractures in the long term.
The effect of ulnar styloid fractures co-occurring with distal radius fractures on wrist function outcomes remains a topic of debate [34–36]. Xing et al. demonstrated that malunited distal radius fractures with dorsal angulation resulted in significant changes in DRUJ contact characteristics, notably a reduction in the contact area during wrist extension and ulnar deviation along with an increase in the contact area during wrist flexion [34]. Additionally, a volar shift in the centroid of the contact area on the sigmoid notch was observed in malunited wrists across all positions. These biomechanical changes suggest potential implications for joint stability and function, highlighting the importance of achieving proper alignment during distal radius fracture treatment to preserve DRUJ mechanics and prevent functional impairment [34]. Conversely, Wijffels et al. reported that clinical DRUJ instability did not significantly influence the long-term functional outcomes of conservatively treated distal radius fractures, as evidenced by a similar range of motion, grip strength, and patient-reported outcomes for patients with and without DRUJ instability [35]. Similarly, Singh et al. reported that ulnar styloid fractures did not significantly affect DRUJ stability or functional outcomes in patients with distal radius fractures, regardless of the ulnar styloid fracture’s union status or location (tip or base) [36]. Our study’s findings, which demonstrate significant benefits of surgical intervention for distal radius fractures with concomitant ulnar styloid involvement in active elderly patients, may appear to diverge from some previous literature. However, this apparent discrepancy highlights a crucial distinction in our study population. Unlike many previous studies that examined isolated distal radius fractures, our cohort exclusively included cases with concomitant ulnar styloid fractures. This is a critical factor, as ulnar styloid fractures may significantly affect the stability of both the distal radius fracture and the DRUJ [8]. In our conservatively treated group, we observed that the presence of ulnar styloid fractures led to a cascade of events including progressive malreduction of the distal radius fracture, loss of volar tilting, radial inclination, and radial height, DRUJ instability, and eventually, arthritic changes. This sequence explains the poorer outcomes in our conservative group compared to the surgical group. Our findings do not necessarily contradict previous studies showing no significant differences between treatment modalities for isolated distal radius fractures [37], but rather suggest that the presence of ulnar styloid fractures may be a key factor in determining the optimal treatment approach. These results underscore the importance of carefully assessing for ulnar styloid involvement in distal radius fractures and considering surgical intervention more strongly when present, especially in active elderly patients. Future research directly comparing outcomes of distal radius fractures with and without ulnar styloid involvement and investigating the long-term impact of untreated ulnar styloid fractures on wrist function and arthritis development, would further clarify this important clinical issue.
While our study demonstrates the efficacy of surgical intervention for distal radius fractures with concomitant ulnar styloid involvement in active elderly patients, it’s important to address the role and limitations of conservative management in these cases. The primary factor for good functional outcomes in these fractures is anatomical reduction, which is particularly challenging to achieve and maintain with conservative methods when an ulnar styloid fracture is present [17]. Our experience with conservative treatments, including volar short arm splinting and long arm supination splinting, has shown limited success in consistently yielding satisfactory functional outcomes. This is primarily due to the difficulty in achieving and maintaining adequate fracture reduction, given the increased instability of the DRUJ caused by the ulnar styloid fracture. However, we acknowledge that conservative management might still have a role in certain situations, such as in patients with significant comorbidities precluding surgery, cases where initial reduction is anatomical and can be maintained with close follow-up, or in minimally displaced fractures in low-demand patients [37]. It’s crucial to emphasize that treatment decisions should be individualized based on factors such as fracture pattern, patient age, activity level, and overall health status. While our data strongly support ORIF as the most reliable treatment option for ensuring promising outcomes in most cases of distal radius fractures with concomitant ulnar styloid involvement, each patient’s situation should be carefully evaluated.
Following ORIF of the distal radius in patients with untreated ulnar styloid fractures, a thorough evaluation of DRUJ stability is essential. This assessment should compare stability of the affected DRUJ with the preoperative state of the contralateral DRUJ. The quality of reduction and hardware position should be re-evaluated and corrected in cases where the DRUJ instability persists, forearm rotation is limited, or joint laxity with positive piano sign is evident [2, 6]. In cases where DRUJ instability persists even after achieving an anatomical reduction of the distal radius fracture, the forearm can be stabilized and immobilized using a splint or cast, typically in a supination position, for at least 6 weeks. This is followed by a rehabilitation program to restore function [38–41]. TFCC injuries are a recognized cause of DRUJ instability and can lead to suboptimal outcomes. Traditionally, surgeons have recommended surgical repair of the TFCC in addition to ORIF of distal radius fractures [42]. However, a recent retrospective case series recommended TFCC treatment only in patients with persistent symptomatic DRUJ instability lasting more than 6 months after plate fixation and splinting of the distal radius fracture [43]. A study also suggested radioulnar pinning with Kirschner wires to enhance construct stability [38]. Conversely, Kim et al. [7] demonstrated that untreated ulnar styloid fractures did not cause DRUJ laxity during long-term follow-up when the distal radius fracture was fixed with a volar locking plate and the forearm was immobilized in supination for 1 month. Furthermore, the study highlighted the benefits of anatomic reduction with volar plating of the distal radius fracture in conjunction with supination splinting. This approach not only addresses initial DRUJ instability but also allows for early wrist mobilization without compromising the reduction [7]. Our study findings are consistent with those of the aforementioned studies, highlighting that reduction of the distal radius fracture is the primary intervention for stabilizing the DRUJ in the presence of concomitant ulnar styloid fractures. In our study, if DRUJ instability persisted after achieving anatomic reduction of the distal radius fracture, patients underwent DRUJ immobilization by supination sugar-tong splinting for approximately 4 weeks. All the patients who followed this recommendation achieved favorable functional outcomes without instability at the 1-year follow-up [44].
Our study offers valuable insights into the treatment outcomes of distal radius fractures with concomitant untreated ulnar styloid fractures in very old patients. However, several limitations must be acknowledged. First, the retrospective design of the study limited our ability to control for all potential confounding variables and standardize aspects of patient care and data collection. Postoperative assessments of DRUJ stability, such as the ballottement test, were not systematically performed, and we relied on functional outcomes like the DASH score as a proxy for postoperative joint stability. The lack of postoperative DRUJ assessments makes it difficult to definitively evaluate the efficacy of surgical versus conservative treatment in restoring stability. Additionally, patient autonomy played a significant role in treatment decision-making, with some patients opting for conservative management despite clinical recommendations for surgery, potentially introducing selection bias. This bias may have influenced the functional outcomes of patients who declined surgery, as their preferences or health concerns may have impacted their choices. Furthermore, the relatively small sample size of 96 patients and the single-institution setting may limit the generalizability of our findings and reduce the statistical power to detect smaller treatment effects. Lastly, we relied solely on clinical assessments without utilizing advanced imaging techniques, such as magnetic resonance imaging, computed tomography, or arthroscopy, which might have offered a more detailed evaluation of the posttreatment anatomical and functional integrity of the DRUJ. Despite these limitations, we believe our findings provide a foundation for future research. Prospective, multicenter studies with larger sample sizes and advanced imaging evaluations are necessary to refine management strategies for distal radius fractures, particularly in aging populations, where optimizing functional recovery and maintaining quality of life post-injury are essential.
Despite these limitations, our findings suggest that surgical treatment of distal radius fractures in active older patients with concomitant ulnar styloid fractures may be a favorable approach. This recommendation is based on the observed improvements in functional wrist restoration at the 1-year follow-up. Although conservative management and rehabilitation may be adequate for isolated distal radius fractures, our study suggests that it may not be suitable for cases with accompanying ulna styloid fractures. The decline in DASH scores in the conservative treatment group indicates that this treatment approach can contribute to instability at the fracture site and DRUJ, potentially leading to further malunion and eventually osteoarthritis. Conversely, ORIF reduction of the distal radius fracture appears to act as a protective factor when ulnar styloid fractures are present. Notably, our data did not reveal a correlation between age and functional outcomes, challenging the common perception regarding the limited recovery potential of older adults following fractures. Age, in this context, might be associated with factors such as increased resilience, adaptability, or even differences in post recovery activity levels. This observation raises pertinent questions about the psychological and physical aspects of recovery in older adults. Further research is warranted to investigate the potential benefits of tailored rehabilitation programs that leverage these factors to optimize outcomes. In summary, our study not only elucidated the functional outcomes of treating distal radius fractures in very old patients but also catalyzes a more comprehensive discussion on optimizing care strategies for this growing patient population.
Conclusions
Our study underscores the critical role of achieving anatomical reduction in distal radius fractures accompanied by ulnar styloid fractures for achieving long-term functional recovery in active older patients. Future research incorporating larger sample sizes, prospective designs, and advanced DRUJ imaging, will be invaluable in further refining treatment protocols for this vulnerable patient demographic.
Acknowledgements
This manuscript was edited by Wallace Academic Editing.
Abbreviations
- DRUJ
Distal radioulnar joint
- ORIF
Open reduction internal fixation
- DASH
Disabilities of the Arm, Shoulder, and Hand
- TFCC
Triangular fibrocartilage complex
- TCI
Target-controlled infusion
- BIS
Bispectral index
- Quick DASH
Quick Disabilities of the Arm, Shoulder, and Hand
Author contributions
Y.K.L. wrote the main manuscript text and finished the statistics of the article. I.-H.C., C.-H.P. and T.-K.Y. completed the data collection. J.-H.W. completed the analysis. C.-M.C.,Y.-C.C., H.-W.C.; and T.-C.Y. all participated in collecting relevant data. K.-T.Y. reviewed and revised the manuscript. W.-T.W. supervised the progression of the project. All authors reviewed the manuscript.
Funding
This research was funded by the TCMF-P 112-05, Buddhist Tzu Chi Medical Foundation.
Data availability
All Data is contained within the article.
Declarations
Ethics approval and consent to participate
We confirm that all experiments were performed in accordance with the Declaration of Helsinki. The study was approved by the Research Ethics Committee of Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation (IRB112-035-B and date of approval: February/27/2023). Each patient provided written informed consent before participating in the study.
Consent for publication
Written informed consent for publication was obtained from all patients included in this study.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wijffels MM, Keizer J, Buijze GA, Zenke Y, Krijnen P, Schep NW, et al. Ulnar styloid process nonunion and outcome in patients with a distal radius fracture: a meta-analysis of comparative clinical trials. Injury. 2014;45(12):1889–95. [DOI] [PubMed] [Google Scholar]
- 2.Sammer DM, Chung KC. Management of the distal radioulnar joint and ulnar styloid fracture. Hand Clin. 2012;28(2):199–206. [DOI] [PubMed] [Google Scholar]
- 3.Daneshvar P, Chan R, MacDermid J, Grewal R. The effects of ulnar styloid fractures on patients sustaining distal radius fractures. J Hand Surg Am. 2014;39(10):1915–20. [DOI] [PubMed] [Google Scholar]
- 4.Sachar K. Ulnar-sided wrist pain: evaluation and treatment of triangular fibrocartilage complex tears, ulnocarpal impaction syndrome, and lunotriquetral ligament tears. J Hand Surg Am. 2012;37(7):1489–500. [DOI] [PubMed] [Google Scholar]
- 5.Lindau T. Treatment of injuries to the ulnar side of the wrist occurring with distal radial fractures. Hand Clin. 2005;21(30):417–25. [DOI] [PubMed] [Google Scholar]
- 6.Ishikawa J, Iwasaki N, Minami A. Influence of distal radioulnar joint subluxation on restricted forearm rotation after distal radius fracture. J Hand Surg Am. 2005;30(6):1178–84. [DOI] [PubMed] [Google Scholar]
- 7.Kim JK, Koh YD, Do NH. Should an ulnar styloid fracture be fixed following volar plate fixation of a distal radial fracture? J Bone Joint Surg Am. 2010;92(1):1–6. [DOI] [PubMed] [Google Scholar]
- 8.Sammer DM, Shah HM, Shauver MJ, Chung KC. The effect of ulnar styloid fractures on patient-rated outcomes after volar locking plating of distal radius fractures. J Hand Surg Am. 2009;34(9):1595–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Souer JS, Ring D, Matschke S, Audige L, Marent-Huber M, Jupiter JB, et al. Effect of an unrepaired fracture of the ulnar styloid base on outcome after plate-and-screw fixation of a distal radial fracture. J Bone Joint Surg Am. 2009;91(4):830–8. [DOI] [PubMed] [Google Scholar]
- 10.Zenke Y, Sakai A, Oshige T, Moritani S, Nakamura T. The effect of an associated ulnar styloid fracture on the outcome after fixation of a fracture of the distal radius. J Bone Joint Surg Br. 2009;91(1):102–7. [DOI] [PubMed] [Google Scholar]
- 11.Nakamura T, Moy OJ, Peimer CA. Relationship between fracture of the Ulnar styloid process and DRUJ instability: a Biomechanical Study. J Wrist Surg. 2021;10(2):111–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim KW, Lee CH, Choi JH, Ahn JM, Gong HS. Distal radius fracture with concomitant ulnar styloid fracture: does distal radioulnar joint stability depend on the location of the ulnar styloid fracture? Arch Orthop Trauma Surg. 2023;143(2):839–45. [DOI] [PubMed] [Google Scholar]
- 13.Trehan SK, Gould HP, Meyers KN, Wolfe SW. The Effect of Distal Radius Fracture Location on Distal Radioulnar Joint Stability: a cadaveric study. J Hand Surg Am. 2019;44(6):473–9. [DOI] [PubMed] [Google Scholar]
- 14.May MM, Lawton JN, Blazar PE. Ulnar styloid fractures associated with distal radius fractures: incidence and implications for distal radioulnar joint instability. J Hand Surg Am. 2002;27(6):965–71. [DOI] [PubMed] [Google Scholar]
- 15.Velmurugesan PS, Nagashree V, Devendra A, Dheenadhayalan J, Rajasekaran S. Should ulnar styloid be fixed following fixation of a distal radius fracture? Injury. 2023;54(7):110768. [DOI] [PubMed] [Google Scholar]
- 16.Mulders MAM, Fuhri Snethlage LJ, de Muinck Keizer RO, Goslings JC, Schep NWL. Functional outcomes of distal radius fractures with and without ulnar styloid fractures: a meta-analysis. J Hand Surg Eur Vol. 2018;43(2):150–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mulders MA, Rikli D, Goslings JC, Schep NW. Classification and treatment of distal radius fractures: a survey among orthopaedic trauma surgeons and residents. Eur J Trauma Emerg Surg. 2017;43(2):239–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Amorosa LF, Vitale MA, Brown S, Kaufmann RA. A functional outcomes survey of elderly patients who sustained distal radius fractures. Hand (N Y). 2011;6(3):260–7. [DOI] [PMC free article] [PubMed]
- 19.Ayalon O, Marcano A, Paksima N, Egol K. Concomitant Ulnar Styloid fracture and distal Radius fracture portend poorer outcome. Am J Orthop (Belle Mead NJ). 2016;45(1):34–7. [PubMed] [Google Scholar]
- 20.Nypaver C, Bozentka DJ. Distal Radius fracture and the distal Radioulnar Joint. Hand Clin. 2021;37(2):293–307. [DOI] [PubMed] [Google Scholar]
- 21.Dy CJ, Jang E, Taylor SA, Meyers KN, Wolfe SW. The impact of coronal alignment on distal radioulnar joint stability following distal radius fracture. J Hand Surg Am. 2014;39(7):1264–72. [DOI] [PubMed] [Google Scholar]
- 22.Ross M, Di Mascio L, Peters S, Cockfield A, Taylor F, Couzens G. Defining residual radial translation of distal radius fractures: a potential cause of distal radioulnar joint instability. J Wrist Surg. 2014;3(1):22–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nakamura T, Iwamoto T, Matsumura N, Sato K, Toyama Y. Radiographic and Arthroscopic Assessment of DRUJ Instability due to Foveal Avulsion of the Radioulnar Ligament in Distal Radius fractures. J Wrist Surg. 2014;3(1):12–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mirarchi AJ, Hoyen HA, Knutson J, Lewis S. Cadaveric biomechanical analysis of the distal radioulnar joint: influence of wrist isolation on accurate measurement and the effect of ulnar styloid fracture on stability. J Hand Surg Am. 2008;33(5):683–90. [DOI] [PubMed] [Google Scholar]
- 25.Bombaci H, Polat A, Deniz G, Akinci O. The value of plain X-rays in predicting TFCC injury after distal radial fractures. J Hand Surg Eur Vol. 2008;33(3):322–6. [DOI] [PubMed] [Google Scholar]
- 26.Cole DW, Elsaidi GA, Kuzma KR, Kuzma GR, Smith BP, Ruch DS. Distal radioulnar joint instability in distal radius fractures: the role of sigmoid notch and triangular fibrocartilage complex revisited. Injury. 2006;37(3):252–8. [DOI] [PubMed] [Google Scholar]
- 27.Scheker LR, Ozer K. Ligamentous stabilization of the distal radioulnar joint. Tech Hand Up Extrem Surg. 2004;8(4):239–46. [DOI] [PubMed] [Google Scholar]
- 28.Ward LD, Ambrose CG, Masson MV, Levaro F. The role of the distal radioulnar ligaments, interosseous membrane, and joint capsule in distal radioulnar joint stability. J Hand Surg Am. 2000;25(2):341–51. [DOI] [PubMed] [Google Scholar]
- 29.Jupiter JB. Commentary: the effect of ulnar styloid fractures on patient-rated outcomes after volar locking plating of distal radius fractures. J Hand Surg Am. 2009;34(9):1603–4. [DOI] [PubMed] [Google Scholar]
- 30.Clementsen SØ, Jakobsen RB, Hammer OL, Randsborg PH. The Effect of Ulnar Styloid fractures on patient-reported outcomes after surgically treated distal radial fractures. JB JS Open Access. 2022;7(3):e2200021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Afifi A, Mansour A. Is it necessary to fix basal fractures of the ulnar styloid after anterior plate fixation of distal radius fractures? A randomized controlled trial. J Hand Surg Eur Vol. 2023;48(6):544–50. [DOI] [PubMed] [Google Scholar]
- 32.Liu J, Wu Z, Li S, Li Z, Wang J, Yang C, et al. Should distal radioulnar joint be fixed following volar plate fixation of distal radius fracture with unstable distal radioulnar joint? Orthop Traumatol Surg Res. 2014;100(6):599–603. [DOI] [PubMed] [Google Scholar]
- 33.Mikić ZD. Age changes in the triangular fibrocartilage of the wrist joint. J Anat. 1978;126(Pt 2):367–84. [PMC free article] [PubMed] [Google Scholar]
- 34.Xing SG, Chen YR, Xie RG, Tang JB. In vivo contact characteristics of distal Radioulnar Joint with Malunited Distal Radius during wrist motion. J Hand Surg Am. 2015;40(11):2243–8. [DOI] [PubMed] [Google Scholar]
- 35.Wijffels MM, Krijnen P, Schipper IB. Clinical DRUJ instability does not influence the long-term functional outcome of conservatively treated distal radius fractures. Eur J Trauma Emerg Surg. 2017;43(2):227–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ajit Singh V, Jia TY, Devi Santharalinggam R, Gunasagaran J. Relationship of ulna styloid fracture to the distal radio-ulnar joint stability. A clinical, functional, and radiographic outcome study. PLoS ONE. 2023;18(1):e0279210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Arora R, Lutz M, Fritz D, Zimmermann R, Oberladstätter J, Gabl M. Palmar locking plate for treatment of unstable dorsal dislocated distal radius fractures. Arch Orthop Trauma Surg. 2005;125(6):399–404. [DOI] [PubMed] [Google Scholar]
- 38.Xiao AX, Graf AR, Dawes A, Daley C, Wagner ER, Gottschalk MB. Management of Acute Distal Radioulnar Joint Instability following a distal Radius fracture: a systematic review and Meta-analysis. J Hand Surg Glob Online. 2021;3(3):133–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pajares S, Martínez-Catalán N, Novo-Rivas U. Stabilization for acute distal radioulnar instability: a novel surgical technique. Injury. 2021;52(Suppl 4):S137–44. [DOI] [PubMed] [Google Scholar]
- 40.Rodríguez-Merchán EC, Shojaie B, Kachooei AR. Distal Radioulnar Joint instability: diagnosis and treatment. Arch Bone Jt Surg. 2022;10(1):3–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bachinskas AJ, Helsper EA, Morris HA, Hearon BF. Nonsurgical treatment for Acute Posttraumatic Distal Radioulnar Joint instability: a Case Series. J Hand Surg Glob Online. 2020;2(1):35–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Spies CK, Langer MF, Müller LP, Unglaub F. Reconstruction of the deep fibers of the distal radioulnar ligaments facilitating a tendon graft-Adams’ procedure. Oper Orthop Traumatol. 2020;32(3):262–70. [Article in German]. [DOI] [PubMed] [Google Scholar]
- 43.Park YC, Shin SC, Kang HJ, Jeon SY, Song JH, Kim JS. Arthroscopic foveal repair of the triangular Fibrocartilage Complex improved the clinical outcomes in patients with Persistent Symptomatic Distal Radio-Ulnar Joint Instability after plate fixation of distal Radius fractures: Minimum 2-Year Follow-Up. Arthroscopy. 2022;38(4):1146–e531. [DOI] [PubMed] [Google Scholar]
- 44.Chunye Tan Z, Wang L, Li. Association between imaging parameter changes and triangular fibrocartilage complex injury after distal radius fractures. J Orthop Surg Res. 2023;18(1):946. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All Data is contained within the article.