Abstract
Background
In older adults, diminished balance is associated with reduced physical functioning and an increased risk of falling. This is an update of a Cochrane review first published in 2007.
Objectives
To examine the effects of exercise interventions on balance in older people, aged 60 and over, living in the community or in institutional care.
Search methods
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register, CENTRAL (The Cochrane Library 2011, Issue 1), MEDLINE and EMBASE (to February 2011).
Selection criteria
Randomised controlled studies testing the effects of exercise interventions on balance in older people. The primary outcomes of the review were clinical measures of balance.
Data collection and analysis
Pairs of review authors independently assessed risk of bias and extracted data from studies. Data were pooled where appropriate.
Main results
This update included 94 studies (62 new) with 9,821 participants. Most participants were women living in their own home.
Most trials were judged at unclear risk of selection bias, generally reflecting inadequate reporting of the randomisation methods, but at high risk of performance bias relating to lack of participant blinding, which is largely unavoidable for these trials. Most studies only reported outcome up to the end of the exercise programme.
There were eight categories of exercise programmes. These are listed below together with primary measures of balance for which there was some evidence of a statistically significant effect at the end of the exercise programme. Some trials tested more than one type of exercise. Crucially, the evidence for each outcome was generally from only a few of the trials for each exercise category. 1. Gait, balance, co‐ordination and functional tasks (19 studies of which 10 provided primary outcome data): Timed Up & Go test (mean difference (MD) ‐0.82 s; 95% CI ‐1.56 to ‐0.08 s, 114 participants, 4 studies); walking speed (standardised mean difference (SMD) 0.43; 95% CI 0.11 to 0.75, 156 participants, 4 studies), and the Berg Balance Scale (MD 3.48 points; 95% CI 2.01 to 4.95 points, 145 participants, 4 studies).
2. Strengthening exercise (including resistance or power training) (21 studies of which 11 provided primary outcome data): Timed Up & Go Test (MD ‐4.30 s; 95% CI ‐7.60 to ‐1.00 s, 71 participants, 3 studies); standing on one leg for as long as possible with eyes closed (MD 1.64 s; 95% CI 0.97 to 2.31 s, 120 participants, 3 studies); and walking speed (SMD 0.25; 95% CI 0.05 to 0.46, 375 participants, 8 studies).
3. 3D (3 dimensional) exercise (including Tai Chi, qi gong, dance, yoga) (15 studies of which seven provided primary outcome data): Timed Up & Go Test (MD ‐1.30 s; 95% CI ‐2.40 to ‐0.20 s, 44 participants, 1 study); standing on one leg for as long as possible with eyes open (MD 9.60 s; 95% CI 6.64 to 12.56 s, 47 participants, 1 study), and with eyes closed (MD 2.21 s; 95% CI 0.69 to 3.73 s, 48 participants, 1 study); and the Berg Balance Scale (MD 1.06 points; 95% CI 0.37 to 1.76 points, 150 participants, 2 studies).
4. General physical activity (walking) (seven studies of which five provided primary outcome data). 5. General physical activity (cycling) (one study which provided data for walking speed). 6. Computerised balance training using visual feedback (two studies, neither of which provided primary outcome data). 7. Vibration platform used as intervention (three studies of which one provided primary outcome data).
8. Multiple exercise types (combinations of the above) (43 studies of which 29 provided data for one or more primary outcomes): Timed Up & Go Test (MD ‐1.63 s; 95% CI ‐2.28 to ‐0.98 s, 635 participants, 12 studies); standing on one leg for as long as possible with eyes open (MD 5.03 s; 95% CI 1.19 to 8.87 s, 545 participants, 9 studies), and with eyes closed ((MD 1.60 s; 95% CI ‐0.01 to 3.20 s, 176 participants, 2 studies); and the Berg Balance Scale ((MD 1.84 points; 95% CI 0.71 to 2.97 points, 80 participants, 2 studies).
Few adverse events were reported but most studies did not monitor or report adverse events.
In general, the more effective programmes ran three times a week for three months and involved dynamic exercise in standing.
Authors' conclusions
There is weak evidence that some types of exercise (gait, balance, co‐ordination and functional tasks; strengthening exercise; 3D exercise and multiple exercise types) are moderately effective, immediately post intervention, in improving clinical balance outcomes in older people. Such interventions are probably safe. There is either no or insufficient evidence to draw any conclusions for general physical activity (walking or cycling) and exercise involving computerised balance programmes or vibration plates. Further high methodological quality research using core outcome measures and adequate surveillance is required.
Keywords: Aged, Female, Humans, Male, Middle Aged, Breathing Exercises, Dancing, Exercise, Exercise/physiology, Exercise Therapy, Exercise Therapy/methods, Gait, Gait/physiology, Muscle Strength, Muscle Strength/physiology, Postural Balance, Postural Balance/physiology, Randomized Controlled Trials as Topic, Sensation Disorders, Sensation Disorders/rehabilitation, Tai Ji, Yoga
Plain language summary
Exercise for improving balance in older people
Balance is staying upright and steady when stationary, such as when standing or sitting, or during movement. The loss of ability to balance may be linked with a higher risk of falling, increased dependency, illness and sometimes early death. However, it is unclear which types of exercise are best at improving balance in older people (aged 60 years and over) living at home or in residential care.
This updated review includes 94 (62 new to this update) randomised controlled trials involving 9821 participants. Most participants were women living in their own home. Some studies included frail people residing in hospital or residential facilities.
Many of the trials had flawed or poorly described methods that meant that their findings could be biased. Most studies only reported outcome up to the end of the exercise programme. Thus they did not check to see if there were any lasting effects.
We chose to report on measures of balance that relate to everyday activities such as time taken to stand up, walk three metres, turn and return to sitting (Timed Up & Go test); ability to stand on one leg (necessary for safe walking in well lit and dark conditions), walking speed (better balance allows faster walking), and activities of daily living (Berg Balance Scale, comprising 14 items). These were our primary outcomes. There were eight categories of exercise programmes. These are listed below together with those measures of balance for which there was some evidence of a positive (statistically significant) effect from the specific type of exercise at the end of the exercise programme. Some trials tested more than one type of exercise. It is important to note that the evidence for each outcome was generally from only a few of the trials for each exercise category. 1. Gait, balance, co‐ordination and functional tasks (19 studies of which 10 provided data for one or more primary outcomes). Positive effects of exercise were found for the Timed Up & Go test, walking speed, and the Berg Balance Scale. 2. Strengthening exercise (including resistance or power training) (21 studies of which 11 provided data for one or more primary outcomes). Positive effects were found for the Timed Up & Go Test; standing on one leg for as long as possible with eyes closed; and walking speed. 3. 3D (3 dimensional) exercise (including Tai Chi, qi gong, dance, yoga) (15 studies of which seven provided data for one or more primary outcomes). Positive effects were found for the Timed Up & Go Test; standing on one leg for as long as possible with eyes open, and with eyes closed; and the Berg Balance Scale. 4. General physical activity (walking) (seven studies of which five provided data for one or more primary outcomes). 5. General physical activity (cycling) (one study which provided data for walking speed). 6. Computerised balance training using visual feedback (two studies, neither of which provided data for any primary outcome). 7. Vibration platform used as intervention (three studies of which one provided data for the Timed Up & Go Test).
8. Multiple exercise types (combinations of the above) (43 studies of which 29 provided data for one or more primary outcomes). Positive effects were found for the Timed Up & Go Test; standing on one leg for as long as possible with eyes open, and with eyes closed; and the Berg Balance Scale.
In general, effective programmes ran three times a week for three months and involved dynamic exercise in standing. Few adverse events were reported.
The review concluded that there was weak evidence that some exercise types are moderately effective, immediately post intervention, in improving balance in older people. However, the missing data and compromised methods of many included trials meant that further high quality research is required.
Background
NB: For an explanation of some of the terms used in this review, please see the Glossary of Terms (Table 1).
1. Glossary of terms.
| Glossary |
| 1RM ‐ One repetition maximum score 3D ‐ 3 Dimensional ADL ‐ Activities of Daily Living A/P ‐ Anterio‐Posterior BBS ‐ Berg Balance Scale BPM ‐ Balance Performance Monitor cm ‐ Centimetres CoM ‐ Centre of mass CoG ‐ Centre of gravity COP ‐ Centre of pressure COPD ‐ Chronic Obstructive Pulmonary Disease EPESE ‐ Established Populations for the Epidemiologic Studies of the Elderly short physical performance battery Ex ‐ Exercise FRT ‐ Functional Reach Test GBFT ‐ Gait, balance, functional tasks GPA ‐ General physical activity HR ‐ Heart Rate Hr ‐ Hour ICF ‐ International Classification of Functioning, Disability and Health ITT ‐ Intention‐to‐treat Km‐ Kilometres LOS ‐ Locus Of Support min ‐ Minute MD ‐ Mean difference M/L ‐ Medio‐lateral mm ‐ Millimetres MMSE ‐ Mini Mental Status Examination m/s ‐ Metres per second NSD ‐ No significant difference PNF ‐ Proprioceptive neuromuscular facilitation PRE ‐ Progressive Resistance Exercise RCT ‐ Randomised controlled trial Reps ‐ Repetitions RoB ‐ Risk of Bias ROM ‐ Range of movement RMS ‐ Root mean squared s ‐ Seconds SD ‐ Standard Deviation SEM ‐ Standard errors of the means SLS ‐ Single Legged Stance SMD ‐ Standardised mean difference STRENGTH ‐ Strength training including resistance or power training TUG ‐ Timed Up & Go Test VO2 max ‐ Maximal Oxygen Uptake WS ‐ Weight shifting |
Description of the condition
Good balance and mobility are essential to the successful performance of most activities of daily living as well as a number of recreational pursuits. Balance is the ability to stay upright and steady when stationary and during movement. Using more technical terms, balance is defined as the ability to maintain the projection of the body's centre of mass (CoM) within manageable limits of the base of support, as in standing or sitting, or in transit to a new base of support, as in walking (Winter 1995). The base of support is composed of the area between all points of contact of the body with another surface; points of contact also include extensions of the body through assistive devices (e.g. walking sticks and frames). Balance is an integral component of daily (functional) activities, however, balance control is complex and multifactorial. The task being undertaken and the environment in which it is taking place both affect an individual's ability to control balance, by altering the biomechanical and information processing needs (Huxham 2001). Balance may be measured when the body has a constant, or static, base of support, or during movement from one base of support to another. It can be analysed directly by quantifying the position of the body's centre of mass in relation to the base of support. Alternatively, balance can be measured indirectly through observation, self reporting or other reporting methods such as objective tests of functional activities.
However, the ability to undertake functional activities is complex and multifaceted involving not only balance but other internal factors such as strength, proprioception, integrity of the neuromuscular system, pain, vision and in some instances fear of falling (Menz 2007; Skelton 2001).
Physiological changes related to ageing include, for example, cognitive impairment (Nevitt 1989), reductions in muscle strength (Daubney 1999; Doherty 1993), proprioception (Skinner 1984), joint range of motion (Mills 1994), reaction time (Stelmach 1994), and changes in sensory systems (Berg 1989). These factors potentially negatively affect balance control and impact on the functional ability and activities of daily living of the older person.
Diminished ability to maintain balance may be associated with an increased risk of falling (Berg 1989;Rossat 2010). In older adults, falls commonly lead to injury, loss of independence, associated illness and early death (Baker 1985; Berg 1989; Tiedemann 2008; Tinetti 1988). Exercise interventions that concentrate on balance training have been shown to be effective in reducing the risk of falls in older adults with a prior history of falling (Sherrington 2008a;Thomas 2010).
However, poor balance is also a marker or predictor for many other outcomes, for example, poor one leg stance time predicts a higher rate of cognitive decline (Rolland 2009) and poor standing balance predicts higher all cause mortality (Cooper 2010).
Description of the intervention
Exercise interventions designed for improving balance are typically those in which participants exercise in standing and moving positions of increasing difficulty so as to challenge the body’s ability to anticipate and respond to the demands of different tasks or environments (Winter 1995). For balance to improve, participants have to exercise their muscles (and neuromuscular responses) against an external force, as a consequence of voluntary movement, or in response to an unexpected perturbation/stimulus, in order to maintain the body's centre of mass within manageable limits of the base of support or in transit to a new base of support (Rose 2005). Examples of exercise interventions include: walking, cycling, functional static and dynamic standing balance training, strengthening exercise, computerised balance training, dance, Tai Chi, yoga and whole body vibration. For most older adults, seated exercise will not improve standing or dynamic movement related balance as without practicing tasks that challenge the neuromuscular system to become more efficient, there is no improvement to balance (Rose 2005).
How the intervention might work
Irrespective of how physically active we are, throughout the life course age‐associated changes occur in the multiple body systems that contribute to balance and mobility. Changes in the peripheral and central components of the sensory and motor systems and changes in cognitive function all alter the speed and quality of task performance (Rose 2005). Older adults exhibit a tendency to over‐ or under‐respond when their balance is perturbed (Stelmach 1989). They also have more difficulty in their balance when there are other attentional demands (dual tasking) on their nervous system (Brown 1999). Research suggests that older adults are increasingly unable to activate the postural muscles required to stabilise the body before the muscles responsible for executing the movement are activated, or indeed, initiate corrective stepping strategies if they lose their balance (Maki 2005). However, the sensory systems are highly adaptive and if older adults are presented with progressively more challenging physical activities that involve the practicing of balance correcting strategies, or the altered sensory conditions, they can learn to adapt postural control strategies appropriately (Hu 1994).
However, not all types of exercise improve balance to an extent that prevents someone actually falling over. Although some exercise interventions with balance and muscle strengthening components have been shown to reduce falls (Campbell 1997; Robertson 2001; Skelton 2005;Wolf 1996), there have also been many unsuccessful exercise interventions (Sherrington 2008b). A meta‐analysis of exercise interventions suggests that at least 50 hours of highly challenging balance training and avoidance of brisk walking interventions are most successful to prevent falls (Sherrington 2008b).
Biofeedback and visual feedback have been used to improve balance control by addressing internal factors that are thought to contribute towards balance (Geiger 2001; Walker 2000). However, few of these interventions have considered falls as an outcome. A recent systematic review on biofeedback has shown some improvement in Berg Balance Scale in frail older adults but the studies are poor methodologically (Zijlstra 2010). The effects of vibration therapy on balance and mobility shows inconsistent efficacy and falls are rarely considered as an outcome (Merriman 2009). Therefore, although exercise should improve balance, this review aims to consider in more depth the types of exercise that improve balance.
Why it is important to do this review
This is an update of a Cochrane review first published in 2007. Our previous review (Howe 2007) reported that, while exercise appears to have statistically significant beneficial effects on balance ability in the short term, the strength of the evidence was limited. Thus, as noted in Howe 2007 with reference to findings from traditional literature reviews describing studies designed to improve balance in older people (Chandler 1996), there is still uncertainty surrounding the efficacy of exercise interventions, the effectiveness of the dosage (frequency, duration or intensity of delivery), the setting in which the intervention takes place, level and type of supervision, or indeed who is most likely to benefit.
Objectives
To examine the effects of exercise interventions on balance in older people, aged 60 and over, living in the community or in institutional care.
In this review, exercise interventions are compared with usual activities, usual health care, attention control or recreational activities.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled studies (RCTs), quasi‐randomised studies (e.g. randomised by date of birth or hospital record number) testing the effects of exercise interventions on balance in older people. Trials were included where participants were randomised to the following:
exercise group: a single exercise intervention or a multiple exercise intervention, versus
control group: usual activities, usual health care, or activities (such as attending recreational or educational activities or groups) that received the same attention (number of attendances at classes or contact with the research team) as the exercise group.
Trials comparing two or more exercise interventions and a control group were also included.
For cross‐over RCTs, data for the initial period were included but it was deemed inappropriate (due to potential long‐lasting effects of the intervention) for the data covering the cross‐over periods to be included. Cluster RCTs with very few clusters such that only one group of people (village; apartment block) acted as an intervention or control group were excluded.
Types of participants
We included studies with participants described as older adults, elderly, geriatric, aged, seniors or all over the age of 60, and studies that separately randomised and analysed the group described above. The participants could have included frail older people, or healthy older people, of either gender, living in the community or in institutional care. Participant characteristics of interest included age, gender, functional status at entry and residential status.
In order not to broaden the scope of this review too widely, we excluded studies of interventions targeting populations with specific conditions such as: stroke, Parkinson's disease, multiple sclerosis, labyrinthitis, Meniere's disease, amputation of upper or lower limbs, cognitive impairments, dementia, osteoporosis, rheumatoid arthritis, osteoarthritis, hip fracture or Alzheimer's disease.
Types of interventions
Exercise interventions designed to improve balance were defined as those in which participants exercise their muscles (and neuromuscular responses) against an external force as a consequence of voluntary movement, or in response to an unexpected perturbation/stimulus in order to maintain the body's centre of mass within manageable limits of the base of support or in transit to a new base of support. Examples of exercise interventions include: walking, cycling, functional static and dynamic standing balance training, computerised balance training, strengthening exercises, dance, Tai Chi, yoga and whole body vibration.
The exercise interventions could take place in the home, institutional dwelling, community, gymnasium or clinic setting and could be self‐supervised (for example using exercise sheets/video), individually supervised or as part of a supervised group. The supervisor could include for example, self, peer, physical trainer or healthcare professional.
These interventions were compared with control groups comprising usual activities, usual health care, or activities (such as attending recreational or educational activities or groups) that received the same attention (number of attendances at classes or contact with the research team) as the exercise group.
Types of outcome measures
The main outcome of interest was balance, defined as the ability to maintain the body's centre of mass within manageable limits of the base of support, as in maintaining a standing or sitting position, or in transit to a new base of support, as in walking or moving. Outcome measures were classified according to the dimensions of the ICF (International Classification of Functioning, Disability and Health) (WHO 2001): impairment, activity limitation or participation restriction.
In this update we revised the choice of our primary outcome measures from 'direct' measures of balance, such as force platform measures (as these require expensive equipment and are difficult to use and interpret in clinical or community settings) to 'indirect' quantifiable measures of balance (Table 2) (as these require minimal equipment and are easy to use in the clinical and community settings and are also easy to interpret as they relate to functional activities).
2. Primary outcome measures.
| 1. Timed Up & Go Test (time taken to stand from sitting, walk 3 m, turn and return to sitting) (Podsiadlo 1991) 2. Standing on one leg for as long as possible with eyes open 3. Standing on one leg for as long as possible with eyes closed 4. Walking speed (higher values indicate better balance) Indirect measure of balance based on observation 5. Berg Balance Scale (0 to 56 point scale) (Berg 1992) 6. Adverse events associated with the exercise intervention |
To be included, studies must have reported measures of balance performance.
Primary outcomes
Indirect measures of balance (ICF dimension activity limitation) based on quantification of functional abilities:
Timed Up & Go Test (time taken to stand from sitting, walk 3 metres, turn and return to sitting) (Podsiadlo 1991)
Standing on one leg for as long as possible with eyes open
Standing on one leg for as long as possible with eyes closed
Walking speed (higher values indicate better balance)
Berg Balance Scale (0 to 56 point scale): indirect measure of balance based on observation (Berg 1992)
Adverse events associated with the exercise intervention
Secondary outcomes
Direct measures of balance (ICF dimension impairment) include force platform indicators (centre of pressure behaviour or position, Sway, Anterior Posterior or Medio Lateral stability, Limits of Stability) (Winter 1995)
Indirect measures of balance based on quantification of functional abilities included, but were not restricted to: Functional Reach Test (Duncan 1990), tandem stance time
Level of adherence or compliance with the exercise intervention
We excluded timed walking tests such as distance walked in 3, 6 or 12 minutes, as these are indicators of aerobic capacity rather than balance ability. Trials that focused on fall rates, numbers of fallers, or other surrogate measures of balance, for example muscle strength or global functional ability, and did not report balance as a primary outcome, were excluded; these have been reviewed elsewhere (Cameron 2010; Gillespie 2009; Liu 2009).
Search methods for identification of studies
Electronic searches
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (January 2011), the Cochrane Central Register of Controlled Trials (The Cochrane Library 2011, Issue 1), MEDLINE (1966 to 1st Feb 2011), EMBASE (1980 to 1st Feb 2011), PEDro ‐ The Physiotherapy Evidence Database (accessed 27th Jan 2011), OTseeker ‐ The Occupational Therapy Systematic Evaluation of Evidence Database (accessed 18th Jan 2011), CINAHL ‐ Cumulative Index to Nursing and Allied Health Literature (from 1982 to 21st Jan 2011) and AMED ‐ Allied and Complementary Medicine Database (from 1985 to Jan 2011). No language restrictions were applied.
In MEDLINE (Ovid Web), the first two phases of the optimal trial search strategy (Robinson 2002) were combined with one subject specific search and the less precise third phase of the optimal trial search strategy was combined with a more precise subject specific search (Appendix 1). Search strategies are also shown in Appendix 1 for The Cochrane Library, CINAHL, EMBASE, AMED, PEDro, and OTseeker.
Searching other resources
Further studies were identified by contact with institutions, experts in the field and reference lists of articles.
Data collection and analysis
Selection of studies
All titles and/or abstracts generated by the searches were screened by pairs of authors for potentially relevant studies. The full‐length articles of the selected titles and/or abstracts were assessed for eligibility (for a full description, seeCriteria for considering studies for this review). Disagreement was resolved by consensus or third party adjudication.
Data extraction and management
Three pairs of members of the review team used a customised data extraction tool, tested prior to use, to independently extract data. Disagreement about data extracted was resolved by consensus or third party adjudication. We contacted authors of studies where there was inadequate reporting of data to enable clarification and where appropriate to allow pooling.
Assessment of risk of bias in included studies
In this update, assessment of risk of bias was undertaken for each included study using The Cochrane Collaboration's 'Risk of bias' tool (Higgins 2008). The following nine key domains were reported by two review authors: sequence generation, allocation concealment, incomplete outcome data, selective outcome reporting, free from other bias, blinding of participant, blinding of assessor, comparability of treatment and control groups at entry, and adequate surveillance post intervention. In cases of disagreement between the review authors, the decisions were made by consensus.
Measures of treatment effect
Where studies reported standard errors of the means (SEMs), standard deviations (SDs) were obtained by multiplying standard errors of means by the square‐root of the sample size. For each trial, risk ratios and 95% confidence intervals were calculated for dichotomous outcomes, and mean differences (MD) and 95% confidence intervals calculated for continuous outcomes (reporting mean and standard deviation or standard error of the mean). Standardised mean differences (SMD) and 95% confidence intervals were calculated when combining results from studies using different ways of measuring the same concept. Change scores have been reported separately as these cannot be incorporated into meta analyses of standardised mean differences.
Unit of analysis issues
The level at which randomisation occurred in the included studies was reported as specified by the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2008). Possible variations in study designs include cluster randomised studies, cross‐over studies, multiple observations, re‐occurring events, multiple treatments and multiple intervention groups. For cross‐over RCTs, data for the initial period were included but it was deemed inappropriate (due to potential long‐lasting effects of the intervention) for the data covering the crossover periods to be included. Cluster RCTs with very few clusters such that only one group of people (village; apartment block) acts as an intervention or control group were excluded. Where cluster randomised studies were combined with each other or with other studies in a meta‐analysis, we planned to perform sensitivity analyses to investigate the effect clustering had on the results.
Dealing with missing data
Where missing data were discovered during data extraction we attempted to contact the original investigators of the study to request the required information. The potential effect of missing data upon conclusions drawn from this review are also described.
Assessment of heterogeneity
Heterogeneity between comparable studies was tested using visual inspection of the forest plot and a standard chi2 test and considered statistically significant at P < 0.1 after due consideration of the value of the I2 statistic, a value greater than 50% may indicate substantial heterogeneity.
Assessment of reporting biases
It was intended to assess the possibility of publication bias with funnel plots. However, there were insufficient data to justify funnel plots.
Data synthesis
Appropiate statistical analysis were performed using Review Manager in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2008). Where available and appropriate, quantitative data for the outcomes listed in the inclusion criteria are presented in the Analyses. Where appropriate, results of comparable groups of studies were pooled using the fixed‐effect model and 95% confidence intervals calculated.
We complied with the recommendations put forward in the Cochrane Handbook, which determine that an I2 statistic of 0% to 40% might not be important; 30% to 60% may represent moderate heterogeneity; 50% to 90% may represent substantial heterogeneity; and 75% to 100% considerable heterogeneity (Deeks 2008). In the presence of substantial heterogeneity an I2 statistic greater than 50% the results of comparable groups of studies were pooled using the random‐effects model and 95% confidence intervals calculated.
Subgroup analysis and investigation of heterogeneity
Regardless of possible heterogeneity of the included studies, separate analyses were conducted by exercise category. On the anticipation of major differences of effect, and where the data allowed, we also planned separate subgroup analyses:
gender;
age: young old (mean age 60 to 75 years) and older old (mean age over 75 years);
frailty;
duration and/or intensity of exercise interventions;
the setting in which the exercise intervention is delivered;
level or type of supervision of the exercise intervention.
Sensitivity analysis
It was anticipated that sensitivity analyses would be undertaken, when indicated, to investigate the effects of methodological quality, for example, allocation concealment and intention‐to‐treat analysis. Where cluster randomised studies were combined with each other or with other studies in a meta‐analysis, we planned to perform sensitivity analyses to investigate the effect clustering had on the results.
Results
Description of studies
Results of the search
Since the publication of the previous version of this review (Howe 2007), 62 new trials were identified, giving a total of 94 trials that fulfilled the inclusion criteria. There are also two ongoing trials and 137 excluded studies (seeCharacteristics of excluded studies).
The search strategy identified a total of 3887 articles for potential inclusion (original search = 1297; updated search = 2590). From the title, abstract, and descriptors, pairs of members of the review team independently reviewed the results of the literature searches to identify potentially relevant studies for full review. From the full text of 274 papers (original = 158; update = 116) that appeared to meet the selection criteria, 233 full papers considered for inclusion in this review. A total of 94 studies were selected for inclusion (original = 32; update = 62). There were two ongoing studies and 137 studies were excluded. Two studies from the original review (Lichtenstein 1989; Shigematsu 2002) were excluded as they were determined to be cluster RCTs with very few clusters. See Figure 1 (PRISMA flow chart; Moher 2009) for details.
1.
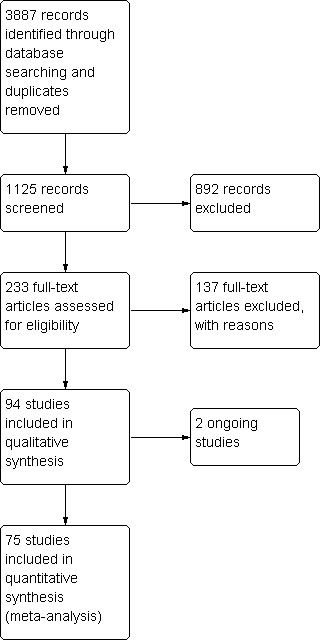
Study flow diagram.
Included studies
For the 94 included studies there were 9821 participants at entry. Two studies were published only as abstracts (Chang 2007; Gaub 2003). There was great variation across the studies in the characteristics of participants, design and content of the exercise interventions, and the outcomes assessed. A brief summary is provided here and more detailed information for individual trials is provided in the Characteristics of included studies. The trials took place in North America (n = 36), Europe (n = 29), Asia (n = 17), Australasia (n = 11), and Brazil (n = 1).
Design
There were 85 studies described as randomised controlled trials, seven cluster RCTs (Faber 2006 (15 clusters, homes randomly assigned to one of the two exercise interventions); McMurdo 1993 (four clusters: exercise = two clusters, reminiscence therapy = two clusters); MacRae 1994 (eight clusters: exercise = four clusters, attention control = four clusters); Morris 1999 (six clusters: Fit for Life exercise = two clusters, self care for seniors = two clusters, control = two clusters); Lord 2003 (20 clusters: exercise = seven self care and three intermediate care clusters, control = seven self care and three intermediate care clusters); Reinsch 1992 (16 clusters: exercise = four clusters, cognitive behavioural = four clusters, exercise‐cognitive = four clusters, discussion = four clusters); Rosendahl 2006 (34 clusters randomly assigned to exercise or control groups in a 2x2 factorial design ‐ only two groups included here) and two cross‐over trials (Baum 2003; Skelton 1996).
Participants
The participants in 66 studies were defined as healthy older people (Arai 2007; Avelar 2010; Baker 2007; Beling 2009; Beyer 2007; Bogaerts 2007; Boshuizen 2005; Brouwer 2003; Buchner 1997a; Buchner 1997b; Campbell 1997; Carvalho 2009; Cheung 2007; Chulvi‐Medrano 2009; Clemson 2010; Cress 1999; Crilly 1989; Eyigor 2009; Frye 2007; Furness 2009; Granacher 2009; Hall 2009; Hatzitaki 2009; Henwood 2006; Islam 2004; Jessup 2003; Johansson 1991; Kamide 2009; Karinkanta 2007; Kim 2009a; Logghe 2009; Lord 1995; Lord 2003; Lord 2005; MacRae 1994; McGarry 2001; McMurdo 1993; Nelson 2004; Okumiya 1996; Paillard 2004; Park 2008; Ramirez Villada 2007; Ramsbottom 2004; Reinsch 1992; Rooks 1997a; Schlicht 2001; Schoenfelder 2000; Salminen 2009; Schilling 2009; Schoenfelder 2004; Shin 2009; Skelton 1995; Suzuki 2004; Sykes 2004; Taaffe 1999; Taylor‐Piliae 2010; Topp 1993; Toraman 2004; Vogler 2009; Voukelatos 2007; Vrantsidis 2009; Wallsten 2006; Westlake 2007; Wolf 1997; Wolfson 1996; Yang 2007) and participants in the remaining 28 studies had general frailty and/or functional limitations (Baum 2003; Chandler 1998; Chang 2007; de Greef 2006; Faber 2006; Gaub 2003; Gine‐Garriga 2010; Hara 2007; Iwamoto 2009; Krebs 1998; Latham 2003; Lin 2007; Liu‐Ambrose 2008; Morris 1999; Rosendahl 2006; Rubenstein 2000; Sauvage 1992; Sherrington 2008a; Shimada 2004; Sihvonen 2004; Skelton 1996; Vestergaard 2008; Weerdesteyn 2006; Wolf 2001; Woo 2007; Worm 2001; Yoo 2010; Zhang 2006a).
A total of 25 studies included only women (Avelar 2010; Beyer 2007; Campbell 1997; Carvalho 2009; Cheung 2007; Chulvi‐Medrano 2009; Crilly 1989; Eyigor 2009; Faber 2006; Hatzitaki 2009; Karinkanta 2007; Jessup 2003; Johansson 1991; Lord 1995; MacRae 1994; Park 2008; Rosendahl 2006; Shin 2009; Sihvonen 2004; Skelton 1995; Skelton 1996; Suzuki 2004; Taylor‐Piliae 2010; Vestergaard 2008; Yoo 2010) and five studies included only men (Granacher 2009; Nelson 2004; Okumiya 1996; Rubenstein 2000; Sauvage 1992). In two trials the gender of participants was not reported (Chang 2007; Westlake 2007).The other 62 studies included both men and women in varying proportions; in the majority of studies, the proportion of women was typically greater.
The average age of participants was 60 to 75 years in 46 studies (Arai 2007; Avelar 2010; Bogaerts 2007; Carvalho 2009; Cheung 2007; Chulvi‐Medrano 2009; Eyigor 2009; Frye 2007; Furness 2009; Granacher 2009; Hall 2009; Hatzitaki 2009; Henwood 2006; Jessup 2003; Johansson 1991; Kamide 2009; Karinkanta 2007; Krebs 1998; Liu‐Ambrose 2008; Lord 1995; MacRae 1994; McGarry 2001; Nelson 2004; Paillard 2004; Park 2008; Ramirez Villada 2007; Ramsbottom 2004; Reinsch 1992; Rooks 1997a; Rubenstein 2000; Salminen 2009; Sauvage 1992; Schilling 2009; Schlicht 2001; Sherrington 2008a; Taaffe 1999; Taylor‐Piliae 2010; Topp 1993; Toraman 2004; Voukelatos 2007; Vrantsidis 2009; Weerdesteyn 2006; Woo 2007; Yoo 2010; Zhang 2006a) and over 75 years in 47 studies. The average age of participants was not reported in Westlake 2007.
Setting
Participants were residing in institutions (hospital or residential care facilities) in 11 studies (Baum 2003; Crilly 1989; Faber 2006; Morris 1999; McMurdo 1993; Rosendahl 2006; Sauvage 1992; Schoenfelder 2000; Schoenfelder 2004; Sihvonen 2004; Toraman 2004); and the community in 79 studies (Arai 2007; Avelar 2010; Baker 2007; Beling 2009; Beyer 2007; Bogaerts 2007; Boshuizen 2005; Brouwer 2003; Buchner 1997a; Buchner 1997b; Campbell 1997; Carvalho 2009; Chandler 1998; Chang 2007; Cheung 2007; Chulvi‐Medrano 2009; Clemson 2010; Cress 1999; Eyigor 2009; Frye 2007; Furness 2009; Gaub 2003; Gine‐Garriga 2010; Granacher 2009; Hall 2009; Hatzitaki 2009; Henwood 2006; Islam 2004; Iwamoto 2009; Jessup 2003; Johansson 1991; Kamide 2009; Karinkanta 2007; Kim 2009a; Krebs 1998; Lin 2007; Liu‐Ambrose 2008; Logghe 2009; Lord 1995; Lord 2003; Lord 2005; MacRae 1994; McGarry 2001; Nelson 2004; Okumiya 1996; Paillard 2004; Park 2008; Ramirez Villada 2007; Ramsbottom 2004; Reinsch 1992; Rooks 1997a; Rubenstein 2000; Salminen 2009; Schlicht 2001; Schilling 2009; Sherrington 2008a; Shin 2009; Skelton 1995; Skelton 1996; Suzuki 2004; Sykes 2004; Taaffe 1999; Taylor‐Piliae 2010; Topp 1993; Vestergaard 2008; Vogler 2009; Voukelatos 2007; Vrantsidis 2009; Wallsten 2006; Weerdesteyn 2006; Westlake 2007; Wolf 1997; Wolfson 1996; Woo 2007; Worm 2001; Yang 2007; Yoo 2010; Zhang 2006a). Type of residence was mixed in four studies (de Greef 2006; Hara 2007; Latham 2003; Wolf 2001).
Interventions
The first version of this review (Howe 2007) included seven categorisations of exercise interventions. For the current update of this review, we re‐scrutinised the original studies which resulted in a reclassification of some of the original studies, the removal of the 'General Physical Activity' category and the addition of two new categories: Computerised balance training using visual feedback, and Vibration Platform. This reclassification of the original review studies resulted in:
Three studies (168 participants) moved from Gait, balance, co‐ordination and functional tasks to the Multiple intervention types category (Brouwer 2003;Crilly 1989;MacRae 1994).
One study (72 participants) moved from Gait, balance, co‐ordination and functional tasks to the Computerised balance training using visual feedback category (Wolf 1997).
One study (56 participants) moved from the strengthening exercise (including resistance or power training) to the Multiple intervention types category (Cress 1999).
One study (34 participants) moved from the Multiple intervention types category to the Gait, balance, co‐ordination and functional tasks category (Johansson 1991).
The removal of the General Physical Activity category which originally had two studies (91 participants), both of which moved to the Multiple intervention types category (McMurdo 1993;Okumiya 1996).
The exclusion of two of the original studies from the review included Lichtenstein 1989 (50 participants) from the Gait, balance, co‐ordination and functional tasks category, and Shigematsu 2002 (38 participants) from the 3D (including Tai Chi, qi gong, dance, yoga) category.
Exercise interventions
All the exercise interventions described were land‐based except in one study (Avelar 2010), which was water‐based. We categorised exercise interventions of included studies based on the taxonomy of exercise interventions developed by ProFaNE (Lamb 2006) and included eight categories (Table 3):
3. Categories of exercise.
| We categorised exercise interventions of included studies based on the taxonomy of exercise interventions developed by ProFaNE (Lamb 2006) and included eight categories: |
|
Gait, balance, co‐ordination and functional tasks
Strengthening exercise (including resistance or power training)
3D (including Tai Chi, qi gong, dance, yoga)
General physical activity (walking)
General physical activity (cycling)
Computerised balance training using visual feedback
Vibration platform used as intervention
Multiple intervention types (combinations of the above)
(NB numbers of participants indicated are at entry to the trial. For information on numbers in each group, see the Characteristics of included studies or the Data and analyses).
Gait, balance, co‐ordination and functional tasks
Nineteen studies involving 1595 participants at entry investigated the effects of exercise programmes involving gait, balance, co‐ordination and functional task activities on balance performance. The content of the exercise programmes was varied. Avelar 2010 (46 participants) included two groups performing low intensity high repetition muscle endurance training, one in water and one on land. Beling 2009 (23 participants) included swaying, balance strategies, ankle hip and stepping flexibility and strength exercise. Clemson 2010 (34 participants) included a mix of balance (reduce base of support, move to limits of sway, shift weight from foot to foot, step over objects) and strength exercises (bending knees, on toes, on heels, up the stairs, sit to stand, move sideways, tighten muscles) embedded in normal activities (LiFE programme). Faber 2006 (158 participants) included exercises focused on balance, mobility and transfer training and Tai Chi. Gaub 2003 (50 participants) included flexibility standing and sitting, floor, static and dynamic balance, variable surfaces, with eyes open or closed. Gine‐Garriga 2010 (51 participants) included balance activities (designed to challenge the visual, vestibular and somatosensory systems) and lower body strength exercises included functional tasks and the use of ankle. Islam 2004 (43 participants) included balance exercises (visual, vestibular and somatosensory) and lower body functional strength exercises. Johansson 1991 (34 participants) involved walking in different directions at different speeds, combined with exercise to music and functional strength exercises. Karinkanta 2007 (74 participants) included jumping, balance agility and impact exercise with four different aerobics and step aerobic programs which were repeated. McGarry 2001 (22 participants) included the "Get off your Rocker" balance class, including single leg stance, exercises with Swiss balls and tandem walking. Reinsch 1992 (107 participants) included stand‐ups and step‐ups and functional exercises. Salminen 2009 (591 participants) included strengthening, balance, co‐ordination and stretching exercises (plus home exercise) within a multifactorial falls prevention programme. Schilling 2009 (19 participants) included standing balance training using VersaDisc and CorDisc devices (adjustable air filled devices). Sihvonen 2004 (28 participants) included functional strength exercise on a force platform and the use of a training device with visual feedback on movement of the centre of pressure. Vrantsidis 2009 (62 participants) included the Getting Grounded Gracefully© program, based on the Feldenkrais method, specifically targeting dynamic balance, postural and turning stability, and weight‐shift transfers. Weerdesteyn 2006 (58 participants) included balance, gait and coordination training via an obstacle course. Motor dual tasks, walking and practice of falls techniques were also included. Westlake 2007 (44 participants) included sensory‐specific balance classes followed by static and dynamic exercises using differing sensory surfaces. Wolf 2001 (94 participants) included exercise in sitting, standing and walking, in a variety of situations to test balance. Wolfson 1996 (57 participants) included exercise on a PRObalancemaster with centre of pressure feedback, in both standing and sitting, exercises using gym balls with eyes open and eyes closed, with and without perturbations, and gait on foam and narrow beams.
Strengthening exercise (including resistance or power training)
Twenty one studies involving 1929 participants at entry investigated the effects of exercise programmes involving strengthening exercise, including resistance or power training, on balance performance. Baum 2003 (20 participants) included strength and flexibility training using ankle and wrists weights and therabands. Boshuizen 2005 (73 participants) included strengthening exercises of lower limbs with theraband and increasing resistance in sitting and standing. Buchner 1997a (55 participants) included free weights and gym equipment. Chandler 1998 (100 participants) included resistive lower extremity exercises using therabands and body weight. Chang 2007 (21 participants) included a lateral trainer and high velocity resistance training. Gaub 2003 (50 participants) involved training with machines for upper and lower limbs. Granacher 2009 (40 participants) included a warm‐up, cycle, and lower limb high resistance strength training (80% 1RM (one repetition maximum score)). Henwood 2006 (67 participants) included both strength and power training on gum equipment. Karinkanta 2007 (74 participants) included progressive resistance training of the lower limbs on gym equipment and with free weights (75% to 80% 1RM). Krebs 1998 (132 participants) in the 'strong for life programme' included a home exercise video with progressive resistance training with therabands and functional movements for upper and lower body. Latham 2003 (243 participants) included high intensity quadriceps exercise programme using adjustable ankle cuff weights. Morris 1999 (468 participants) included progressive resistance training of upper and lower limbs. Rooks 1997a (91 participants) included stair climbing with resistance, seated knee extension, standing, standing knee extension. Schlicht 2001 (24 participants) included progressive resistance strength training for lower limbs at 75% 1RM. Skelton 1995 (47 participants) included progressive resistance strength training using rice bags and elastic tubing. Skelton 1996 (20 participants) included progressive resistance strengthening exercises with therabands. Taaffe 1999 (46 participants) included high intensity progressive resistance training at 80% 1RM for upper and lower limbs. Topp 1993 (63 participants) included home exercises for upper and lower limbs using surgical tubing. Vogler 2009 (120 participants) included seated exercises of the lower limbs using resistance bands and ankle weights. Wolfson 1996 (55 participants) included stretching and progressive resistive exercise with sand bags for the hip and knee. Woo 2007 (120 participants) included resistance training of upper and lower limbs using therabands.
3D exercise (including Tai Chi, qi gong, dance, yoga)
Fifteen studies involving 1863 participants at entry investigated the effects of 3D exercise programmes on balance performance. Buchner 1997b (56 participants) included exercise involving dance movement to music. Eyigor 2009 (40 participants) involved folklore dance‐sessions. Faber 2006 (162 participants) included Tai Chi. Frye 2007 (54 participants) included Tai Chi. Hall 2009 (22 participants) included Tai Chi classic Yang style (24 forms). Kim 2009a (52 participants) included 12 forms of Tai Chi. Logghe 2009 (269 participants) included Tai Chi derived from Yang style. Shin 2009 (60 participants) included rhythmic exercises to music, stretching, joint mobility, strengthening, and cardiopulmonary endurance. Taylor‐Piliae 2010 (93 participants) were taught 12 postures of the Yang short‐form style of Tai Chi, and then performed the movements at home unsupervised with a video and booklet. Voukelatos 2007 (702 participants) included different forms of Tai Chi. Wallsten 2006 (77 participants) included Tai Chi Chuan. Wolf 1997 (48 participants) included 10 forms of Tai Chi Quan. Woo 2007 (120 participants) included Tai Chi. Yang 2007 (59 participants) included Taiji Qigong. Zhang 2006a (49 participants) included a simplified form of 24 forms of Tai Chi plus 11 easy forms for home exercise.
General physical activity (walking)
Seven studies involving 287 participants at entry investigated the effects of walking on balance performance. Buchner 1997b (56 participants) involved participants walking outdoors. Gaub 2003 (50 participants) tested walking for 20 to 25 minutes at 80% estimated heart rate maximum or progressive resistance exercise (7‐8/10). Paillard 2004 (21 participants) included individual walking programmes determined by lactate levels during a VO2 max test. Rooks 1997a (91 participants) included participants walking at their own pace on level ground. Schoenfelder 2000 (16 participants) involved a walking programme of 10 minutes of sustained walking and ankle strengthening exercises (without resistance). Shimada 2004 (32 participants) involved gait training on a bilateral separated treadmill. Yoo 2010 (21 participants) included a walking exercise program with ankle weights. Exercise intensity was maintained at 60% of heart rate reserve.
General physical activity (cycling)
One study involving 54 participants at entry investigated the effects of static cycling on balance performance (Buchner 1997b).
Computerised balance training using visual feedback
Two studies involving 104 participants at entry investigated the effects of computerised balance training with visual feedback on balance performance. Hatzitaki 2009 (56 participants) included visually guided weight‐shifting tasks and stretching. One group performed anterior‐posterior movements and one group performed medio‐lateral movements. Wolf 1997 (48 participants) included standing on a force platform using exercise to move a target via a cursor on screen.
Vibration platform
Three studies involving 310 participants at entry investigated the effects of a vibration platform on balance performance. Bogaerts 2007 (160 participants) included functional lower limb strength exercises on a vibration platform. Cheung 2007 (75 participants) included standing, barefooted, on an oscillating platform. Furness 2009 (75 participants) had three groups, each standing on a vibrating plate but with three different training doses (once to three times a week).
Multiple intervention types (combinations of the above)
Forty three studies involving 3847 participants at entry investigated the effects of multiple exercise types on balance performance. Arai 2007 (171 participants) involved strengthening exercises (high intensity > 70% 1RM), highly challenging balance exercises and flexibility. Baker 2007 (38 participants) included repetitions of flexion exercises to improve strength, recumbent stepper and cycle ergometer for aerobic exercise and dynamic and static balance exercises. Beyer 2007 (53 participants) included strengthening exercises (high intensity > 70% 1RM), highly challenging balance exercises and flexibility. Bogaerts 2007 (126 participants) included a fitness group of cardiovascular, resistance and flexibility exercises with walking, running, cycling or stepping and resistance programme exercises. Brouwer 2003 (38 participants) included low resistance exercises against gravity, using therabands for legs and trunk, reaching, weight shifting, marching on spot, and a home exercise programme. Campbell 1997 (233 participants) involved moderate intensity strengthening exercises (ankle weights) for lower limb and progressively challenging standing balance exercises. Carvalho 2009 (57 participants) involved aerobic exercise, muscular endurance (circuits with functional strength exercises), agility and reaction training. Chulvi‐Medrano 2009 (28 participants) involved using a T‐Bow device, functional strength exercises and standing balance exercises. Cress 1999 (56 participants) combined endurance and resistance exercises. Crilly 1989 (50 participants) included exercise aimed at improving breathing, single and double limb balance, co‐ordination, flexibility, strength and relaxation. de Greef 2006 (45 participants) included light intensity aerobic exercises, strength training, balance training and running. Frye 2007 (53 participants) included low intensity exercises with a focus on physical fitness, strength, flexibility, endurance, and balance. Gaub 2003 (50 participants) included strength exercises (gym equipment), flexibility exercises, balance exercises, a punch bag and walking. Hara 2007 (44 participants) included sit to stands, standing up to parallel bars, light weights for seated arm strengthening and low balance challenges. Iwamoto 2009 (68 participants) included callisthenics, body balance training, muscle power training, and walking ability training. Jessup 2003 (18 participants) included progressive strength training, load‐bearing walking, stair‐climbing and balance‐training exercises. Kamide 2009 (57 participants) included stretching, moderate intensity strength training (therabands), balance and heel drop exercises. Karinkanta 2007 (75 participants) included resistance and balance jumping training; resistance and balance training were on alternate weeks. Lin 2007 (100 participants) included stretching, strengthening and balance training exercises. Liu‐Ambrose 2008 (74 participants) included moderate intensity strengthening exercises (ankle weights) for lower limb and progressively challenging standing balance exercises (same as Campbell 1997). Lord 1995 (197 participants) involved strength, flexibility, co‐ordination, and balance exercises based on the participants' falls risk profile. In Lord 2003 (461 participants), the exercise programme included aerobic exercises, strengthening exercises and activities for balance, hand‐eye and foot‐eye coordination, and flexibility. Lord 2005 (414 participants), then used a similar programme of aerobic exercises, strengthening exercises and activities for balance, hand‐eye and foot‐eye coordination, and flexibility. McMurdo 1993 (49 participants) included seated exercises aimed at improving flexibility, endurance and strength. MacRae 1994 (80 participants) included a strength and balance fitness class with steps. Nelson 2004 (72 participants) included exercise for balance and strength (free weights), plus 120 minutes of physical activity per week. Park 2008 (50 participants) included stretching, strength training, aerobic weight bearing and balance exercises. Okumiya 1996 (42 participants) included light aerobic exercise and muscle‐strengthening exercises. In Ramirez Villada 2007 (93 participants), exercise included dynamic horizontal and vertical jumps. Ramsbottom 2004 (22 participants) included free weights to strengthen upper and lower limbs and exercises to improve functional mobility, range of motion and balance. Rosendahl 2006 (95 participants) included high intensity functional exercise, strength, balance and activities of daily living. Rubenstein 2000 (59 participants) involved progressive resistance exercise (PRE) for the lower limb, endurance training on a bike and treadmill and indoor walking and balance training. Sauvage 1992 (14 participants) included PRE and aerobic conditioning (> 70% maximal heart rate) using gym equipment and ergometers. Schoenfelder 2004 (81 participants) included strength and endurance training plus 10 minutes walking. Sherrington 2008a (173 participants) included circuit style group exercises (aerobic exercise on a treadmill or bike, functional strength exercises and standing static and dynamic balance exercises). Weekly home exercises were also included. Suzuki 2004 (52 participants) included an exercise (with additional home based exercise) programme to improve strength, balance and gait and also Tai Chi. Sykes 2004 (40 participants) included leg strengthening exercises with gait and balance exercises. Toraman 2004 (42 participants) included aerobic, strength and flexibility training. Taylor‐Piliae 2010 (95 participants) included group and home based endurance, resistance/strength (hand weight and bands), and flexibility exercises. plus 30 or more minutes of walking. Vestergaard 2008 (61 participants) included exercises for flexibility, dynamic balance, strengthening and walking. Vogler 2009 (120 participants) included standing strength (weight belts) and balance exercises. Wolfson 1996 (55 participants) included exercise on a PRObalancemaster with centre of pressure feedback, strengthening exercise (sand bags), flexibility and balance exercises in standing, with a gym ball, on foam and narrow beams. Worm 2001 (46 participants) included muscle, flexibility, strength, balance and endurance training.
Exercise delivery: settings, supervision and supervisors
The exercise interventions took place in a variety of settings; in institutions ‐ 12 studies (Baum 2003; Crilly 1989; Faber 2006; Hara 2007; Morris 1999; McMurdo 1993; Rosendahl 2006; Schoenfelder 2000; Schoenfelder 2004; Shimada 2004; Sihvonen 2004; Toraman 2004); home ‐ 12 studies (Campbell 1997; Chandler 1998; Clemson 2010; Kamide 2009; Krebs 1998; Lin 2007; Liu‐Ambrose 2008; Nelson 2004; Vestergaard 2008; Vogler 2009; Wallsten 2006; Wolf 2001); community ‐ 23 studies (Boshuizen 2005; Cheung 2007; Frye 2007; Gaub 2003; Logghe 2009; Lord 1995; Lord 2003; Lord 2005; Okumiya 1996; Paillard 2004; Park 2008; Ramsbottom 2004; Reinsch 1992; Rooks 1997a; Schlicht 2001; Suzuki 2004; Taylor‐Piliae 2010; Voukelatos 2007; Weerdesteyn 2006; Worm 2001; Yang 2007; Yoo 2010; Zhang 2006a); and gymnasium or clinic ‐ 38 studies (Arai 2007; Avelar 2010; Baker 2007; Beling 2009; Beyer 2007; Bogaerts 2007; Brouwer 2003; Buchner 1997a; Buchner 1997b; Carvalho 2009; Chulvi‐Medrano 2009; Cress 1999; Eyigor 2009; Furness 2009; Gine‐Garriga 2010; Granacher 2009; Hall 2009; Hatzitaki 2009; Henwood 2006; Islam 2004; Iwamoto 2009; Jessup 2003; Johansson 1991; Kim 2009a; MacRae 1994; McGarry 2001; Rubenstein 2000; Salminen 2009; Sauvage 1992; Schilling 2009; Sherrington 2008a; Shin 2009; Taaffe 1999; Topp 1993; Vrantsidis 2009; Wolf 1997; Wolf 2001; Wolfson 1996). Note that Wolf 2001 and Avelar 2010 were factorial design studies with two arms of the study involving different interventions taking place in different settings. In one study the exercise intervention took place in a swimming pool (Avelar 2010). There were five studies which did not report the setting (Chang 2007 (abstract only); de Greef 2006; Karinkanta 2007; Westlake 2007; Woo 2007). The setting was unclear from the translation of Ramirez Villada 2007. The settings were mixed in four studies where one group exercised in a gym and the other in a pool (Avelar 2010); first two sessions were in hospital and the others at home in Latham 2003; medical school and home (Skelton 1995); home and gym/clinic (Skelton 1996); and initially in a centre then at home (Sykes 2004).
The interventions were delivered mainly as part of supervised groups (68 studies); or individually supervised ‐ 16 studies (Chandler 1998; Cheung 2007; Clemson 2010; Furness 2009; Granacher 2009; Hatzitaki 2009; Lin 2007; Liu‐Ambrose 2008; Schilling 2009; Schoenfelder 2000; Shimada 2004; Sihvonen 2004; Vestergaard 2008; Vogler 2009; Wolf 2001; Wolfson 1996); or self‐supervised (for example using exercise sheets/video) ‐ four studies (Kamide 2009; Krebs 1998; Nelson 2004; Okumiya 1996). Supervision was of a mixed type in six studies: Initial supervision over two months in the form of four home visits followed by self‐supervision (Campbell 1997); self‐supervised twice weekly and once weekly supervised during visit to their home (Latham 2003); group and unsupervised at home (Logghe 2009); once weekly in supervised group session and twice weekly in self‐supervised home sessions (Skelton 1995); supervised at gym or clinic and self supervised at home (Skelton 1996); and initial group supervision then phone calls at home (Sykes 2004). The method of supervision was not reported in two studies. (Chang 2007; de Greef 2006).There were two studies where the method of supervision was unclear (Hara 2007; Ramirez Villada 2007).
The supervisors were healthcare professionals or fitness instructors in 53 studies (Arai 2007; Baker 2007; Beling 2009; Beyer 2007; Bogaerts 2007; Boshuizen 2005; Brouwer 2003; Campbell 1997; Carvalho 2009; Chandler 1998; Chulvi‐Medrano 2009; Clemson 2010; Crilly 1989; Faber 2006; Frye 2007; Hall 2009; Henwood 2006; Islam 2004; Johansson 1991; Kamide 2009; Karinkanta 2007; Kim 2009a; Krebs 1998; Latham 2003; Lin 2007; Liu‐Ambrose 2008; Logghe 2009; Lord 1995; Lord 2003; Lord 2005; MacRae 1994; McGarry 2001; Okumiya 1996; Ramsbottom 2004; Rosendahl 2006; Salminen 2009; Sherrington 2008a; Schilling 2009; Shimada 2004; Skelton 1996; Sykes 2004; Taylor‐Piliae 2010; Toraman 2004; Vestergaard 2008; Vogler 2009; Voukelatos 2007; Vrantsidis 2009; Wallsten 2006; Weerdesteyn 2006; Wolf 1997; Wolf 2001; Yang 2007; Zhang 2006a). The background of the supervisor was not stated in 24 studies (Avelar 2010; Buchner 1997a; Buchner 1997b; Chang 2007; Cress 1999; de Greef 2006; Furness 2009; Gaub 2003; Hara 2007; Iwamoto 2009; McMurdo 1993; Paillard 2004; Park 2008; Sauvage 1992; Schlicht 2001; Sihvonen 2004; Skelton 1995; Suzuki 2004; Taaffe 1999; Westlake 2007; Wolfson 1996; Woo 2007; Worm 2001; Yoo 2010). The remaining 17 studies gave other descriptions such as researcher, exercise physiologist, dance expert, health nurse, sports scientist and students.
Exercise delivery: duration
The duration of the exercise programmes ranged from a minimum of four weeks (Sihvonen 2004) to a maximum of 12 months (Bogaerts 2007; Karinkanta 2007; Lord 1995; Lord 2003; Lord 2005; Reinsch 1992; Salminen 2009) with the most frequent being three months. The frequency of the individual sessions ranged from once every two weeks (Suzuki 2004) to every day (Zhang 2006a), the most common being three times per week. The duration of each session ranged from three minutes (Cheung 2007) to 90 minutes (Jessup 2003), the most frequent being 60 minutes. In one study (Clemson 2010), the exercise was embedded in daily activities; frequency and duration were therefore variable.
Exercise delivery: compliance
The definition of adherence or compliance with the exercise intervention and the method of recording and reporting varied considerably across studies and thus these data are difficult to interpret. Typically adherence or compliance was reported as the median or mean percentage of actual sessions completed compared with the total available sessions. This was reported in 38 studies and ranged from 25% (Liu‐Ambrose 2008) to 100% (Furness 2009; Iwamoto 2009).
Further details are provided in the Characteristics of included studies.
Comparison interventions
We compared exercise interventions with a control group. The control group was usual activities in 64 studies (Avelar 2010; Baker 2007; Beling 2009; Beyer 2007; Bogaerts 2007; Boshuizen 2005; Buchner 1997a; Buchner 1997b; Carvalho 2009; Chandler 1998; Chang 2007; Cheung 2007; Chulvi‐Medrano 2009; Clemson 2010; Cress 1999; Crilly 1989; Eyigor 2009; Faber 2006; Frye 2007; Furness 2009; Gaub 2003; Granacher 2009; Hara 2007; Hatzitaki 2009; Henwood 2006; Kamide 2009; Karinkanta 2007; Islam 2004; Iwamoto 2009; Jessup 2003; Johansson 1991; Krebs 1998; Liu‐Ambrose 2008; Logghe 2009; Lord 1995; Lord 2003; Lord 2005; McGarry 2001; Morris 1999; Okumiya 1996; Paillard 2004; Park 2008; Schilling 2009; Shin 2009; Rooks 1997a; Rubenstein 2000; Sauvage 1992; Sherrington 2008a; Shimada 2004; Sihvonen 2004; Skelton 1995; Skelton 1996; Suzuki 2004; Sykes 2004; Taaffe 1999; Voukelatos 2007; Vrantsidis 2009; Wallsten 2006; Weerdesteyn 2006; Woo 2007; Worm 2001; Yang 2007; Yoo 2010; Zhang 2006a) and attention or recreational activities in 16 studies (Baum 2003; Campbell 1997; Crilly 1989; Latham 2003; MacRae 1994; McMurdo 1993; Nelson 2004; Ramsbottom 2004; Reinsch 1992; Rosendahl 2006; Schoenfelder 2004; Taylor‐Piliae 2010; Vogler 2009; Wolf 1997; Wolf 2001; Wolfson 1996).
The control group was education sessions in nine studies (Arai 2007; Brouwer 2003; Gine‐Garriga 2010; Hall 2009; Kim 2009a; Lin 2007; Salminen 2009; Topp 1993; Westlake 2007).
It was unclear what the control group did in five studies (de Greef 2006; Ramirez Villada 2007; Schlicht 2001; Schoenfelder 2000; Toraman 2004).
Outcomes
To be included, studies must have reported measures of balance performance (Table 2). However, a wide variety of outcomes (15 broad categories described below) were assessed in these studies and often they utilised different methods of data collection and reporting.
Primary outcome measures
Timed Up & Go Test
This is the time to stand, walk three metres, turn, and return to sitting, measured in seconds (Podsiadlo 1991). It was used in 22 studies (Arai 2007; Baum 2003; Beling 2009; Boshuizen 2005; de Greef 2006; Faber 2006; Frye 2007; Furness 2009; Hara 2007; Iwamoto 2009; Kamide 2009; Latham 2003; Liu‐Ambrose 2008; McGarry 2001; Okumiya 1996; Ramsbottom 2004; Schilling 2009; Skelton 1995; Sykes 2004; Toraman 2004; Vrantsidis 2009; Wallsten 2006). Three studies used an eight foot‐up‐and‐go instead of three metres (Carvalho 2009; Chulvi‐Medrano 2009; Yoo 2010). Gine‐Garriga 2010 used a modified Timed Up and Go which included kicking a ball. Lower values on these tests indicate better balance ability
Single legged stance
Single legged stance is the ability to balance on one leg measured as the time before placing the opposite leg on the ground. This test was undertaken in a variety of conditions:
Eyes open in 23 studies (Arai 2007; Buchner 1997a; Chang 2007; Chulvi‐Medrano 2009; Clemson 2010; Gine‐Garriga 2010; Iwamoto 2009; Johansson 1991; Kamide 2009; MacRae 1994; Nelson 2004; Park 2008; Reinsch 1992; Rooks 1997a; Rubenstein 2000; Shimada 2004; Skelton 1995; Suzuki 2004; Taylor‐Piliae 2010; Weerdesteyn 2006; Wolfson 1996; Woo 2007; Zhang 2006a);
Eyes closed in eight studies (Arai 2007; Johansson 1991; Rooks 1997a; Schlicht 2001; Shin 2009; Skelton 1995; Suzuki 2004; Topp 1993).
In some cases, it was measured subject to ceiling effects with a maximum time allowed ranging from 15 seconds (Rubenstein 2000) to one minute (Suzuki 2004). Higher values indicate better balance ability.
Gait speed
Gait speed, time to walk a known pre‐determined distance, was used as an outcome in 47 studies (Avelar 2010; Baker 2007; Beyer 2007; Beling 2009; Boshuizen 2005; Brouwer 2003; Buchner 1997a; Buchner 1997b; Campbell 1997; Chang 2007; Cress 1999; de Greef 2006; Eyigor 2009; Faber 2006; Gaub 2003; Gine‐Garriga 2010; Hara 2007; Henwood 2006; Iwamoto 2009; Johansson 1991; Kamide 2009; Karinkanta 2007; Krebs 1998; Latham 2003; MacRae 1994; Nelson 2004; Paillard 2004; Park 2008; Ramsbottom 2004; Rooks 1997a; Rosendahl 2006; Sauvage 1992; Schlicht 2001; Schoenfelder 2000; Schoenfelder 2004; Sherrington 2008a; Shimada 2004; Skelton 1995; Skelton 1996; Suzuki 2004; Topp 1993; Vogler 2009; Vrantsidis 2009; Wolfson 1996; Woo 2007; Worm 2001; Zhang 2006a). This was expressed in different units of measurement; velocity (e.g. m/s, cm/min, m/min), or time (s) taken to complete the required distance. A higher value of velocity indicates faster mobility and thus better balance ability, whereas a higher time to complete a required distance indicates slower mobility. Where velocity data are pooled with time for completion of a set distance data, the negative mean values are presented for the latter so that the direction of benefit is the same. The distance walked varied from two metres (Nelson 2004) to 30 metres (Johansson 1991) and was typically measured at the participant's preferred pace of walking, usually from a standing start and finish but sometimes included acceleration and deceleration distances, or fast paced (Vogler 2009).
Berg Balance Scale
The Berg Balance Scale is a 56 point scale comprising 14 items of activities of daily living deemed safe for elderly people to perform, each item is scored 0 to 4 (Berg 1992). This was used in 15 studies (Avelar 2010; Baum 2003; Beling 2009; Beyer 2007; Eyigor 2009; Gaub 2003; Latham 2003; Logghe 2009; McGarry 2001; Rosendahl 2006; Salminen 2009; Sihvonen 2004; Sykes 2004; Wolf 2001; Worm 2001). Higher values indicate better balance ability.
Adverse events
The majority of studies either did not report on any adverse events (n = 55) or reported that there were no adverse events (n = 30). Some adverse events were reported in eight studies (Iwamoto 2009; Karinkanta 2007; Liu‐Ambrose 2008; Nelson 2004; Reinsch 1992; Rosendahl 2006; Shimada 2004; Vogler 2009) and it was unclear from translation in one study (Ramirez Villada 2007). However, it is unclear from the reporting whether these adverse events related to the exercise or control groups or the total sample. Rosendahl 2006 reported "No adverse event during the sessions led to a manifest injury or disease"; a more detailed breakdown of adverse events in the two exercise groups was given another publication of this trial (Littbrand 2006).
Secondary outcome measures
Functional reach
The distance an individual can reach forward beyond arms length while maintaining a fixed base of support in standing (Duncan 1990) was used in 18 studies (Arai 2007; Campbell 1997; Chandler 1998; Cheung 2007; Cress 1999; de Greef 2006; Granacher 2009; Hara 2007; Henwood 2006; Lin 2007; McGarry 2001; Okumiya 1996; Ramsbottom 2004; Shimada 2004; Skelton 1995; Skelton 1996; Sykes 2004; Taylor‐Piliae 2010). Higher values indicate better balance ability.
Four square step test
One study used the Four Square Step Test (Vrantsidis 2009). This involves timing participants stepping as quickly as possible in four directions over four sticks on the ground, first in one direction and then in the other. Lower scores indicate better balance ability.
Figure of eight time
Dynamic balance and agility, tested by a standardised figure of eight running test around two poles placed 10 metres apart, was used in one study (Karinkanta 2007). Participants could run or walk two laps of the course as fast as possible. Lower values indicate better balance ability.
Parallel stance
Parallel stance is the ability to stand with both feet placed beside each other measured as the time before loss of balance and movement of either leg. This outcome measure was used in four studies (Baker 2007; Buchner 1997a; Schoenfelder 2000; Schoenfelder 2004). Higher values indicate better balance ability.
Tandem (semi) stance
Tandem stance is the ability to stand with one foot placed in front of the other and touching heel to toe measured as the time before loss of balance and movement of either leg. This outcome measure was used in 11 studies (Baker 2007; Boshuizen 2005; Buchner 1997a; Clemson 2010; Iwamoto 2009; Rooks 1997a; Schoenfelder 2000; Schoenfelder 2004; Sherrington 2008a; Vestergaard 2008; Woo 2007). Semi‐tandem stance (where one foot is in front of the other but off set to the side) was used in two studies (Gine‐Garriga 2010; Salminen 2009). Higher values indicate better balance ability.
Tandem walk
Tandem walk is the ability to walk with one foot placed in front of the other and touching heel to toe, measured as the time taken to walk a set distance or the number of steps taken before loss of balance occurs. This outcome measure was used in 11 studies (Avelar 2010; Baker 2007; Clemson 2010; Granacher 2009; Iwamoto 2009; Nelson 2004; Ramirez Villada 2007; Rooks 1997a; Suzuki 2004; Taaffe 1999; Topp 1993). Higher values indicate better balance ability.
Tilt boards
The ability to maintain balance whilst standing on a tilt board that allows movement only in the anterio‐posterior direction or multiple directions, measured in time to loss of balance, was used in two studies (Buchner 1997a; Buchner 1997b). Higher values indicate better balance ability.
Balance beams
The ability to walk on wide (17 cm) and narrow (8.5 cm) beams, measured as distance completed before loss of balance (m), or speed of walking (m/s), was used in four studies (Buchner 1997a; Buchner 1997b; Cress 1999; Johansson 1991). Higher values indicate better balance ability.
Force platform and sway indicators
Force platforms allow the measurement of the movement of the centre of pressure, or limits of stability, under different conditions. Force platforms or sway meters were used in 27 studies (Brouwer 2003; Buchner 1997b; Chandler 1998; Crilly 1989; Hatzitaki 2009; Islam 2004; Jessup 2003; Kim 2009a; Lord 1995; Lord 2003; Lord 2005; McMurdo 1993; Paillard 2004; Park 2008; Ramsbottom 2004; Salminen 2009; Sauvage 1992; Schilling 2009; Sihvonen 2004; Vogler 2009; Voukelatos 2007; Vrantsidis 2009; Westlake 2007; Wolf 1997; Wolfson 1996; Woo 2007; Yang 2007). Typically, when these tests are performed under static conditions (e.g. quiet stance, one leg stance) lower values indicate better balance ability but when performed under dynamic conditions (e.g. maximal balance range, leaning forwards, backwards and sideways) higher values indicate better balance ability.
Sensory Organisational Test (SOT)
The participant stands steady during three trials of six sensory conditions: 1) eyes open fixed surface and visual surround; 2) eyes closed fixed surface; 3) eyes open fixed surface sway referenced visual surround; 4) eyes open sway referenced fixed visual surround; 5) eyes closed sway referenced surface; 6) eyes open sway referenced surface and visual surround. The test is performed on a NeuroCom computer programme with force plate. The SOT is a composite score. Higher values indicate better balance ability. The SOT was used in four studies (Beling 2009; Bogaerts 2007; Hall 2009; Yang 2007)
Stability Score
This test provides an objective score that indicates strength, proprioception and vestibular or visual impairment. The test is performed under four conditions: with or without foam and with eyes open or closed. The CAPSTM Lite programme uses a force platform as a composite balance score (Yoo 2010). Higher values indicate better balance ability.
Time able to stand normally in 5‐feet positions
This is a timed test and was used by one study (Morris 1999).
Excluded studies
There were 137 studies excluded for reasons given in the Characteristics of excluded studies. The main reasons for exclusion included: not an appropriate study design, i.e. not a randomised controlled trial, or small number of clusters in RCT; no control group or control group received some active exercise intervention; no balance outcome measures; and participants did not meet the inclusion criteria (had a specific medical condition or were younger).
Ongoing studies
Two ongoing studies were identified (Frandin 2009; Leininger 2006), details of these are given in the Characteristics of ongoing studies.
Risk of bias in included studies
The results of the risk of bias assessments for each of the nine items for each included study are summarised in Figure 2 and presented as percentages across all included studies (Figure 3). Many included trials were not of high methodological quality and were at high risk of bias for at least one of the nine items (usually performance bias relating to lack of blinding of study participants).
2.

A summary table of review authors' judgements for each risk of bias item for each study.
3.
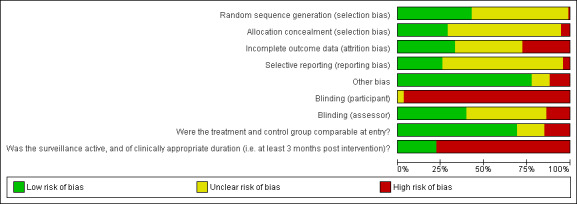
A plot of the distribution of review authors' judgements across studies for each risk of bias item.
Allocation
Sequence generation
The reported method of randomisation included random number tables, block randomisation using permuted blocks, and stratification. However, 54 studies did not state or were unclear about the method of randomisation (Arai 2007; Avelar 2010; Beling 2009; Bogaerts 2007; Boshuizen 2005; Brouwer 2003; Carvalho 2009; Chang 2007; Cheung 2007; Chulvi‐Medrano 2009; Cress 1999; Eyigor 2009; Frye 2007; Furness 2009; Gaub 2003; Granacher 2009; Hall 2009; Hara 2007; Hatzitaki 2009; Henwood 2006; Islam 2004; Iwamoto 2009; Johansson 1991; Kim 2009a; Krebs 1998; Lin 2007; MacRae 1994; McGarry 2001; Morris 1999; Okumiya 1996; Paillard 2004; Ramirez Villada 2007; Rooks 1997a;Salminen 2009; Sauvage 1992; Schilling 2009; Schlicht 2001; Schoenfelder 2004; Sherrington 2008a; Shin 2009; Suzuki 2004; Sykes 2004; Taaffe 1999; Taylor‐Piliae 2010; Topp 1993; Toraman 2004; Vrantsidis 2009; Wallsten 2006; Westlake 2007; Wolf 1997; Wolf 2001; Worm 2001;Yoo 2010; Zhang 2006a).
Concealment
Allocation concealment was adequate in 27 studies (Baker 2007; Baum 2003; Campbell 1997; Chandler 1998; Cheung 2007; Clemson 2010; Faber 2006; Gine‐Garriga 2010; Karinkanta 2007; Latham 2003; Liu‐Ambrose 2008; Logghe 2009; Lord 2003; Lord 2005; MacRae 1994; Nelson 2004; Rosendahl 2006; Rubenstein 2000; Salminen 2009; Sherrington 2008a; Vogler 2009; Voukelatos 2007; Vrantsidis 2009; Weerdesteyn 2006; Wolf 2001; Woo 2007; Yang 2007); unclear in 62 studies (Arai 2007; Avelar 2010; Beling 2009; Beyer 2007; Bogaerts 2007; Boshuizen 2005; Buchner 1997a; Buchner 1997b; Carvalho 2009; Chang 2007; Chulvi‐Medrano 2009; Cress 1999; Crilly 1989; de Greef 2006; Eyigor 2009; Frye 2007; Furness 2009; Gaub 2003; Granacher 2009; Hall 2009; Hara 2007; Hatzitaki 2009; Henwood 2006; Islam 2004; Iwamoto 2009; Jessup 2003; Johansson 1991; Kamide 2009; Kim 2009a; Krebs 1998; Lin 2007; Lord 1995; McGarry 2001; McMurdo 1993; Okumiya 1996; Paillard 2004; Park 2008; Ramirez Villada 2007; Reinsch 1992; Rooks 1997a; Sauvage 1992; Schilling 2009; Schlicht 2001; Schoenfelder 2000; Schoenfelder 2004; Shimada 2004; Shin 2009; Sihvonen 2004; Suzuki 2004; Sykes 2004; Taaffe 1999; Taylor‐Piliae 2010; Topp 1993; Toraman 2004; Vestergaard 2008; Wallsten 2006; Westlake 2007; Wolf 1997; Wolfson 1996; Worm 2001; Yoo 2010; Zhang 2006a); and not used in 5 studies (Brouwer 2003; Morris 1999; Ramsbottom 2004; Skelton 1995; Skelton 1996).
Blinding
Participants
It is difficult to ensure blinding of participants in studies of exercise interventions. We judged all trials at high risk of bias from this item except for three trials (Furness 2009; Gine‐Garriga 2010; Schilling 2009) which were rated were at unclear risk of bias. In an attempt to minimise bias, 16 studies used attention or recreational control groups (the participants received matching periods of attention or recreational activity) (Baum 2003; Campbell 1997; Crilly 1989; Latham 2003; MacRae 1994; McMurdo 1993; Nelson 2004; Ramsbottom 2004; Reinsch 1992; Rosendahl 2006; Schoenfelder 2004; Taylor‐Piliae 2010; Vogler 2009; Wolf 1997; Wolf 2001; Wolfson 1996). Nine studies used education sessions (Arai 2007; Brouwer 2003; Gine‐Garriga 2010; Hall 2009; Kim 2009a; Lin 2007; Salminen 2009; Topp 1993; Westlake 2007).
Assessors
A total of 37 studies stated that assessors for all outcomes were blind to the group allocation (Arai 2007; Avelar 2010; Baker 2007; Baum 2003; Beyer 2007; Boshuizen 2005; Buchner 1997a; Buchner 1997b; Campbell 1997; Chandler 1998; Clemson 2010; Faber 2006; Gine‐Garriga 2010; Johansson 1991; Kamide 2009; Johansson 1991; Latham 2003; Lin 2007; Liu‐Ambrose 2008; Logghe 2009; Lord 1995; Lord 2005; Morris 1999; Nelson 2004; Okumiya 1996; Rosendahl 2006; Rubenstein 2000; Sauvage 1992; Schoenfelder 2004; Suzuki 2004; Taylor‐Piliae 2010; Vogler 2009; Voukelatos 2007; Vrantsidis 2009; Wolfson 1996; Woo 2007; Worm 2001). However, 43 studies did not report the status of blinding of assessors (Beling 2009; Bogaerts 2007; Brouwer 2003; Carvalho 2009; Chang 2007; Cheung 2007; Chulvi‐Medrano 2009; Cress 1999; Crilly 1989; Eyigor 2009; Furness 2009; Gaub 2003; Granacher 2009; Hall 2009; Hara 2007; Hatzitaki 2009; Henwood 2006; Iwamoto 2009; Karinkanta 2007; Kim 2009a; Islam 2004; MacRae 1994; McGarry 2001; Paillard 2004; Park 2008; Reinsch 1992; Rooks 1997a; Schilling 2009; Schlicht 2001; Schoenfelder 2000; Shimada 2004; Shin 2009; Sihvonen 2004; Sykes 2004; Taaffe 1999; Topp 1993; Toraman 2004; Wallsten 2006; Westlake 2007; Wolf 1997; Yang 2007; Yoo 2010; Zhang 2006a). Thirteeen studies reported that the assessor was not blinded (Frye 2007; de Greef 2006; Jessup 2003; Lord 2003; McMurdo 1993; Ramsbottom 2004; Salminen 2009; Sherrington 2008a; Shimada 2004; Skelton 1995; Skelton 1996; Vestergaard 2008; Weerdesteyn 2006) and there was one study where it was unclear from the translation (Ramirez Villada 2007).
Incomplete outcome data
Incomplete outcome data
Most studies included only participants that completed the entire trial in their analysis whereas 31 studies stated that they used methods to address incomplete outcome data, for example using intention‐to‐treat analysis (Arai 2007; Baker 2007; Baum 2003; Boshuizen 2005; Brouwer 2003; Buchner 1997a; Buchner 1997b; Chandler 1998; Clemson 2010; Cress 1999; Furness 2009; Islam 2004; Iwamoto 2009; Jessup 2003; Karinkanta 2007; Latham 2003; Lin 2007: Liu‐Ambrose 2008; Lord 2003; Lord 2005; Park 2008; Ramsbottom 2004; Reinsch 1992; Rooks 1997a; Rosendahl 2006; Salminen 2009; Suzuki 2004; Vestergaard 2008; Vogler 2009; Voukelatos 2007; Yang 2007).
Surveillance
Most studies (n = 75) did not have any follow‐up beyond the end of the programme of exercise intervention. For those 19 studies reporting follow‐up (Beyer 2007; Brouwer 2003; Buchner 1997b; Campbell 1997; Carvalho 2009; Clemson 2010; Faber 2006; Gaub 2003; Gine‐Garriga 2010; Latham 2003; Lin 2007; Logghe 2009; Rosendahl 2006; Schoenfelder 2000; Schoenfelder 2004; Wallsten 2006; Westlake 2007; Wolf 2001; Wolfson 1996) the duration varied from six weeks (Brouwer 2003) to one year (Wolf 2001).
Losses
A total of 83 studies reported losses that ranged from 0% of participants (Carvalho 2009; Chulvi‐Medrano 2009; Furness 2009; Schoenfelder 2000) to 48% of participants (Wolf 2001). However, 11 studies did not report whether any losses had incurred (Baum 2003; Gaub 2003; Granacher 2009; Hatzitaki 2009; Kim 2009a; McGarry 2001; Paillard 2004; Schilling 2009; Vestergaard 2008; Wolf 1997; Wolfson 1996).
Selective reporting
Most studies (n = 66) reported insufficient information to permit judgement (Arai 2007; Avelar 2010; Beling 2009; Beyer 2007; Buchner 1997b; Carvalho 2009; Chandler 1998; Chang 2007;Cheung 2007; Chulvi‐Medrano 2009; Clemson 2010; Crilly 1989; Eyigor 2009; Frye 2007; Furness 2009; Gaub 2003; Gine‐Garriga 2010; Granacher 2009; Hall 2009; Hatzitaki 2009; Islam 2004; Iwamoto 2009; Kamide 2009; Kim 2009a; Latham 2003; Logghe 2009; MacRae 1994; McGarry 2001; Morris 1999; Paillard 2004; Park 2008; Ramirez Villada 2007; Ramsbottom 2004; Reinsch 1992; Rooks 1997a; Rosendahl 2006; Rubenstein 2000; Salminen 2009; Sauvage 1992; Schilling 2009; Schlicht 2001; Schoenfelder 2000; Schoenfelder 2004; Sherrington 2008a; Shimada 2004; Shin 2009; Sihvonen 2004; Suzuki 2004; Sykes 2004; Taaffe 1999; Taylor‐Piliae 2010; Topp 1993; Toraman 2004; Vestergaard 2008; Vogler 2009; Voukelatos 2007; Vrantsidis 2009; Wallsten 2006; Weerdesteyn 2006; Westlake 2007; Wolf 1997; Wolf 2001; Wolfson 1996; Worm 2001; Yang 2007; Yoo 2010). Some (n = 24) appear to be free of selective reporting (Baker 2007; Bogaerts 2007; Boshuizen 2005; Brouwer 2003; Buchner 1997a; Cress 1999; Faber 2006; Hara 2007; Henwood 2006; Jessup 2003; Johansson 1991; Karinkanta 2007; Krebs 1998; Lin 2007; Liu‐Ambrose 2008; Lord 1995; Lord 2003; Lord 2005; Nelson 2004; Okumiya 1996; Skelton 1995; Skelton 1996; Woo 2007; Zhang 2006a). Four studies declared selective reporting and give reasons (Baum 2003; Campbell 1997; de Greef 2006; McMurdo 1993).
Other potential sources of bias
Publication bias
It was intended to assess the possibility of publication bias with funnel plots; however, this was not undertaken due to the relatively low quality of reporting and lack of power in included studies.
Study size
A total of 24 studies had more than 100 participants at entry (Arai 2007; Bogaerts 2007; Buchner 1997a; Buchner 1997b; Campbell 1997; Faber 2006; Karinkanta 2007; Krebs 1998; Latham 2003; Lin 2007; Logghe 2009; Lord 1995; Lord 2003; Lord 2005; Morris 1999; Reinsch 1992; Rooks 1997a; Salminen 2009; Sherrington 2008a; Taylor‐Piliae 2010; Vogler 2009; Voukelatos 2007; Wolfson 1996; Woo 2007) but most were small. Nineteen studies had fewer than 40 participants at entry (Baker 2007; Baum 2003; Beling 2009; Brouwer 2003; Chulvi‐Medrano 2009; Clemson 2010; Hall 2009; Jessup 2003; Johansson 1991; McGarry 2001; Paillard 2004; Ramsbottom 2004; Sauvage 1992; Schilling 2009; Schoenfelder 2000; Shimada 2004; Sihvonen 2004; Skelton 1996; Yoo 2010). The smallest sample was Sauvage 1992 at only 14 participants.
Other bias
Seventy three studies appeared to be free from other bias (Arai 2007; Avelar 2010; Baker 2007; Baum 2003; Bogaerts 2007; Brouwer 2003; Buchner 1997a; Campbell 1997; Carvalho 2009; Chandler 1998; Chang 2007; Chulvi‐Medrano 2009; Clemson 2010; Cress 1999; Crilly 1989; Eyigor 2009; Furness 2009; Gaub 2003; Gine‐Garriga 2010; Granacher 2009; Hall 2009; Hatzitaki 2009; Islam 2004; Iwamoto 2009; Jessup 2003; Johansson 1991; Kamide 2009; Karinkanta 2007; Kim 2009a; Krebs 1998; Latham 2003; Lin 2007; Liu‐Ambrose 2008; Logghe 2009; Lord 2005; McGarry 2001; Okumiya 1996; Paillard 2004; Park 2008; Ramirez Villada 2007; Ramsbottom 2004; Rooks 1997a; Rosendahl 2006; Rubenstein 2000; Salminen 2009; Sauvage 1992; Schilling 2009; Schlicht 2001; Schoenfelder 2000; Schoenfelder 2004; Sherrington 2008a; Shimada 2004; Shin 2009; Sihvonen 2004; Skelton 1995; Suzuki 2004; Sykes 2004; Taaffe 1999; Topp 1993; Toraman 2004; Vestergaard 2008; Vogler 2009; Voukelatos 2007; Weerdesteyn 2006; Westlake 2007; Wolf 1997; Wolf 2001; Wolfson 1996; Woo 2007; Worm 2001; Yang 2007; Yoo 2010; Zhang 2006a). Eleven studies reported other bias (Beyer 2007; Faber 2006, Hara 2007; Henwood 2006; Lord 2003; MacRae 1994; McMurdo 1993; Morris 1999; Reinsch 1992; Skelton 1996; Wallsten 2006) and in seven studies it was unclear (Beling 2009; Buchner 1997b; Frye 2007; Lord 1995; Nelson 2004; Taylor‐Piliae 2010; Vrantsidis 2009). Six of the cluster RCTs failed to adjust for clustering and were judged as high risk of bias (Faber 2006; Lord 2003; MacRae 1994; McMurdo 1993; Morris 1999; Reinsch 1992).
Vibration and computerised balance training are different to the other interventions in that there is the potential for commercial gain by the producers and sellers of these devices. However, as none of the included studies reported companies as funding sources, we did not judge any study at high risk of other bias on this basis.
Treatment and control groups comparable at entry
Most trials (n = 65) reported comparability; however, there was insufficient information to permit judgement of comparability in some trials (n = 15) (Arai 2007; Bogaerts 2007; Buchner 1997b; Chang 2007; Gaub 2003; Granacher 2009; McGarry 2001; Morris 1999; Ramirez Villada 2007; Sauvage 1992; Schilling 2009; Schlicht 2001; Wallsten 2006; Westlake 2007; Wolf 2001). Treatment and control groups were not comparable at entry in 14 studies (Avelar 2010; Beyer 2007; Buchner 1997a; Campbell 1997; Chulvi‐Medrano 2009; Clemson 2010; de Greef 2006; Hara 2007; Iwamoto 2009; Liu‐Ambrose 2008; Lord 2005; MacRae 1994; Topp 1993; Woo 2007).
Effects of interventions
We categorised exercise interventions into categories (Table 3) and where appropriate data were pooled within types. Discussion relates to primary outcome measures defined in this review (Table 2). It should be noted that missing data or non‐availability of data for pooling meant that the meta‐analyses are incomplete for most primary outcomes for most exercise categories.
1. Gait, balance co‐ordination and functional tasks versus control
Appendix 2 demonstrates what actual or potential data were available for this comparison for the primary outcomes. Overall, 10 out of the 19 trials in this category contributed data to the analyses for one or more primary balance outcomes. In terms of participants, some primary outcome data were available for presentation in the analyses for 435 out of the 1595 randomised participants (27%). While reported, no primary outcome data were available for inclusion in the analyses from a further six trials (930 randomised participants).
When primary outcomes were measured immediately post intervention, the exercise programmes achieved a statistically significant reduction in time taken to perform a Timed Up & Go Test (TUG) (MD ‐0.82 s; 95% CI ‐1.56 to ‐0.08 s, 114 participants, 4 studies, Analysis 1.1), an increase in gait speed (SMD 0.43; 95% CI 0.11 to 0.75, 156 participants, 4 studies, Analysis 1.5), and an improvement in the Berg Balance Score (MD 3.48 points; 95% CI 2.01 to 4.95 points, 145 participants, 4 studies, Analysis 1.6). Although, an increase in single leg stance time with eyes open was found for exercise (MD 3.13 s; 95% CI 0.26 to 6.01 s, 206 participants, 4 studies, Analysis 1.2), a sensitivity analysis performed to examine the potential effects of unit of analysis issues on results whereby Reinsch 1992, a cluster RCT, was removed from the meta‐analysis resulted in a change to non statistically significant difference (173 participants, three studies, Analysis 1.3). There was also no statistically significant difference between the exercise or control groups for single leg stance time eyes closed (33 participants, 1 study, Analysis 1.4). One study reported adverse events (Reinsch 1992): 38.6% of participants had a fall with only 7.8% needing medical attention, with no differences in time to fall between groups. However, it is unclear from the reporting whether these adverse events relate to the exercise or control groups or the total sample.
1.1. Analysis.
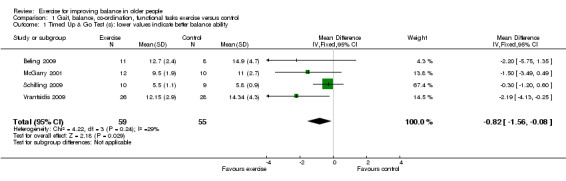
Comparison 1 Gait, balance, co‐ordination, functional tasks exercise versus control, Outcome 1 Timed Up & Go Test (s): lower values indicate better balance ability.
1.5. Analysis.
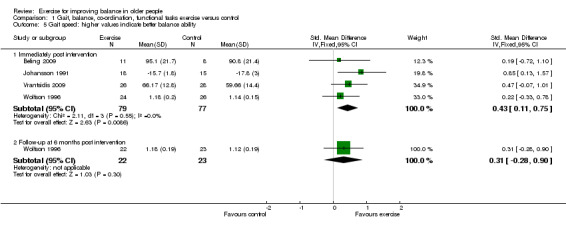
Comparison 1 Gait, balance, co‐ordination, functional tasks exercise versus control, Outcome 5 Gait speed: higher values indicate better balance ability.
1.6. Analysis.
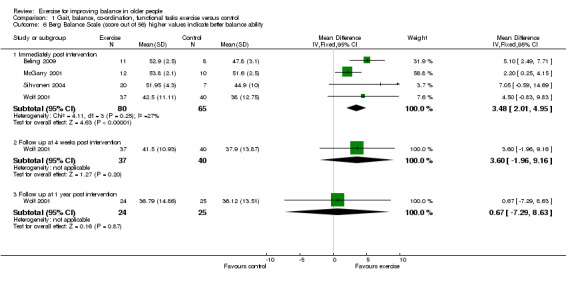
Comparison 1 Gait, balance, co‐ordination, functional tasks exercise versus control, Outcome 6 Berg Balance Scale (score out of 56) higher values indicate better balance ability.
1.2. Analysis.
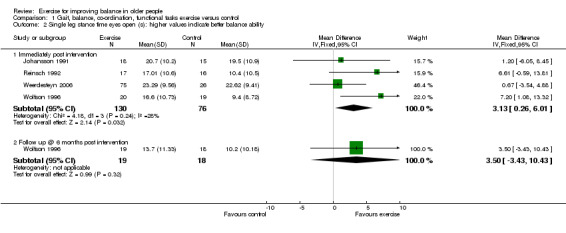
Comparison 1 Gait, balance, co‐ordination, functional tasks exercise versus control, Outcome 2 Single leg stance time eyes open (s): higher values indicate better balance ability.
1.3. Analysis.

Comparison 1 Gait, balance, co‐ordination, functional tasks exercise versus control, Outcome 3 Sensitivity analysis (cluster RCT removed): Single leg stance time eyes open (s): higher values indicate better balance ability.
1.4. Analysis.
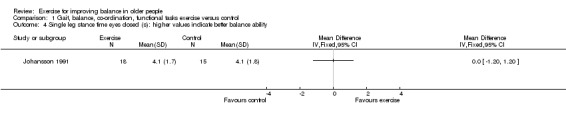
Comparison 1 Gait, balance, co‐ordination, functional tasks exercise versus control, Outcome 4 Single leg stance time eyes closed (s): higher values indicate better balance ability.
Follow‐up data were reported for some primary outcome measures but there was no statistically significant difference between the exercise or control groups for single leg stance time with eyes open or gait speed at six months (one study, Analysis 1.2, Analysis 1.5), or Berg Balance Scores at four weeks and one year (one study, Analysis 1.6).
For all other secondary outcomes there was insufficient similarity among the trials or common outcomes to pool data. Data from single trials with small numbers of participants indicated statistically significant differences in favour of exercise programmes for: maximum limits of excursion of limits of stability test (Analysis 1.13), functional base of support during a dynamic test (Analysis 1.14). For all other secondary outcome measures there was no statistically significant difference between the exercise or control groups (Analysis 1.7; Analysis 1.8; Analysis 1.9; Analysis 1.10; Analysis 1.11; Analysis 1.12; Analysis 1.15; Analysis 1.16).
1.13. Analysis.
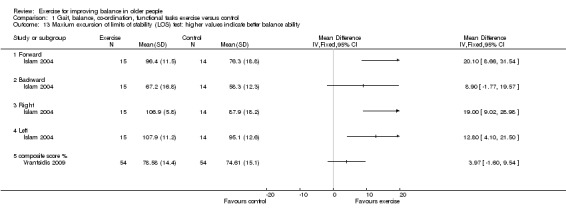
Comparison 1 Gait, balance, co‐ordination, functional tasks exercise versus control, Outcome 13 Maxium excursion of limits of stability (LOS) test: higher values indicate better balance ability.
1.14. Analysis.
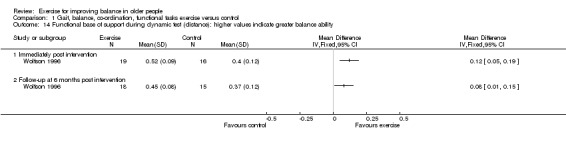
Comparison 1 Gait, balance, co‐ordination, functional tasks exercise versus control, Outcome 14 Functional base of support during dynamic test (distance): higher values indicate greater balance ability.
1.7. Analysis.

Comparison 1 Gait, balance, co‐ordination, functional tasks exercise versus control, Outcome 7 Functional Reach Test: higher values indicate better balance ability.
1.8. Analysis.
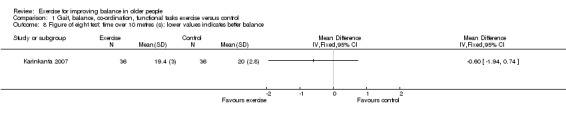
Comparison 1 Gait, balance, co‐ordination, functional tasks exercise versus control, Outcome 8 Figure of eight test: time over 10 metres (s): lower values indicates better balance.
1.9. Analysis.
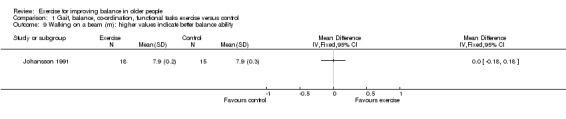
Comparison 1 Gait, balance, co‐ordination, functional tasks exercise versus control, Outcome 9 Walking on a beam (m): higher values indicate better balance ability.
1.10. Analysis.
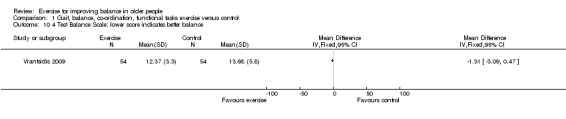
Comparison 1 Gait, balance, co‐ordination, functional tasks exercise versus control, Outcome 10 4 Test Balance Scale: lower score indicates better balance.
1.11. Analysis.
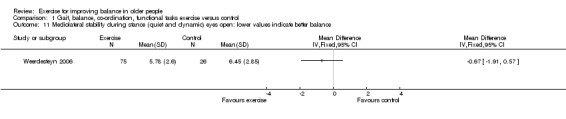
Comparison 1 Gait, balance, co‐ordination, functional tasks exercise versus control, Outcome 11 Mediolateral stability during stance (quiet and dynamic) eyes open: lower values indicate better balance.
1.12. Analysis.
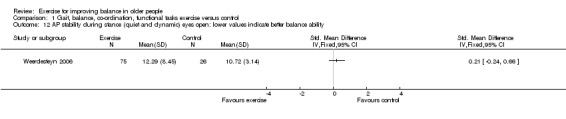
Comparison 1 Gait, balance, co‐ordination, functional tasks exercise versus control, Outcome 12 AP stability during stance (quiet and dynamic) eyes open: lower values indicate better balance ability.
1.15. Analysis.
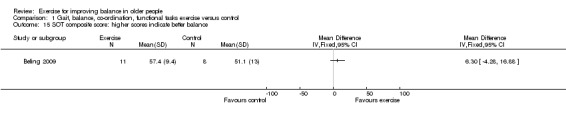
Comparison 1 Gait, balance, co‐ordination, functional tasks exercise versus control, Outcome 15 SOT composite score: higher scores indicate better balance.
1.16. Analysis.
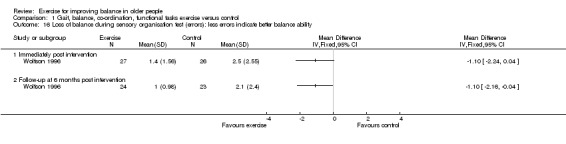
Comparison 1 Gait, balance, co‐ordination, functional tasks exercise versus control, Outcome 16 Loss of balance during sensory organisation test (errors): less errors indicate better balance ability.
2. Strengthening exercise versus control
Appendix 3 demonstrates what actual or potential data were available for this comparison for the primary outcomes. Overall, 11 out of the 21 trials in this category contributed data to the analyses for one or more primary balance outcomes. In terms of participants, some primary outcome data were available for presentation in the analyses for 590 out of the 1929 randomised participants (31%). While reported, no primary outcome data were available for inclusion in the analyses from a further six trials (571 randomised participants).
When primary outcomes were measured immediately post intervention, the exercise programmes achieved a statistically significant reduction in time taken to perform a Timed Up & Go Test (TUG) (MD ‐4.30 s; 95% CI ‐7.60 to ‐1.00 s, 71 participants, 3 studies, Analysis 2.1), an increase in single leg stance time with eyes closed (MD 1.64 s; 95% CI 0.97 to 2.31 s, 120 participants, 3 studies, Analysis 2.3), and an increase in gait speed (SMD 0.25; 95% CI 0.05 to 0.46, 375 participants, 8 studies, Analysis 2.4). However there was no statistically significant difference between the exercise or control groups for single leg stance time with eyes open (187 participants, 3 studies, Analysis 2.2) or the Berg Balance Score (20 participants, 1 study, Analysis 2.6). Two studies reported adverse events, however it is unclear from the reporting whether these relate to exercise or control groups or the total sample: Karinkanta 2007 (14 due to musculoskeletal injuries or symptoms; two falls but they returned to classes. No difference in monthly reported health problems with exercisers and controls) and Vogler 2009 (22 reported in 22 participants: soreness (lower back, hip, knee pain)).
2.1. Analysis.
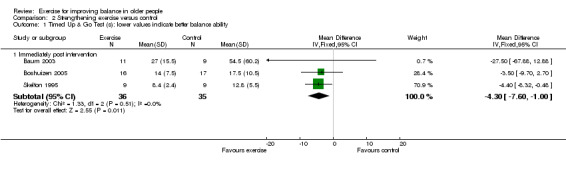
Comparison 2 Strengthening exercise versus control, Outcome 1 Timed Up & Go Test (s): lower values indicate better balance ability.
2.3. Analysis.
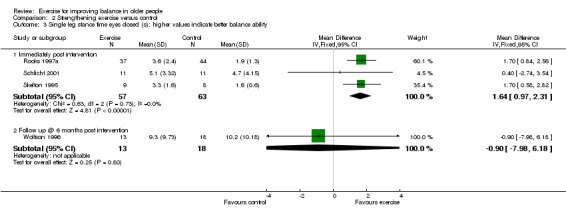
Comparison 2 Strengthening exercise versus control, Outcome 3 Single leg stance time eyes closed (s): higher values indicate better balance ability.
2.4. Analysis.
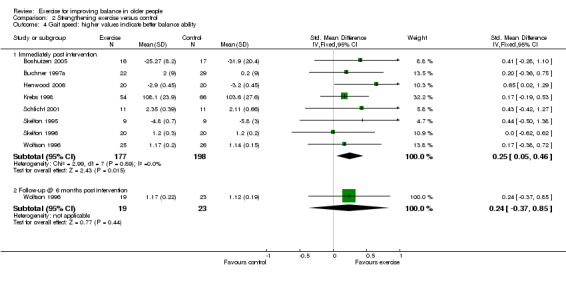
Comparison 2 Strengthening exercise versus control, Outcome 4 Gait speed: higher values indicate better balance ability.
2.2. Analysis.
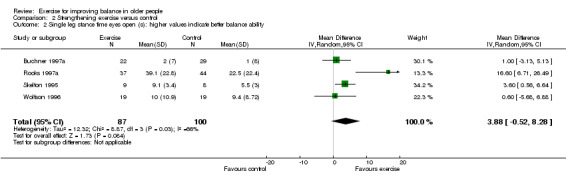
Comparison 2 Strengthening exercise versus control, Outcome 2 Single leg stance time eyes open (s): higher values indicate better balance ability.
2.6. Analysis.
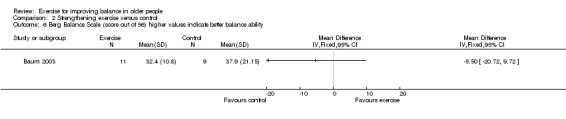
Comparison 2 Strengthening exercise versus control, Outcome 6 Berg Balance Scale (score out of 56) higher values indicate better balance ability.
Follow‐up data were reported for some primary outcome measures but there was no statistically significant difference between the exercise or control groups for single leg stance time eyes closed or gait speed at six months (one study, Analysis 2.3; Analysis 2.4) indicating that these effects were not maintained beyond the end of the exercise programme.
For secondary outcome measures, the exercise programmes achieved a statistically significant improvement compared with controls in functional reach (MD 3.27 cm; 95% CI 1.39 to 5.15 cm, Analysis 2.7), but not for the tandem stance (Analysis 2.11) or for the balance beam at any time point (Analysis 2.12).
2.7. Analysis.

Comparison 2 Strengthening exercise versus control, Outcome 7 Functional reach test (FRT) (cm): higher values indicate better balance.
2.11. Analysis.
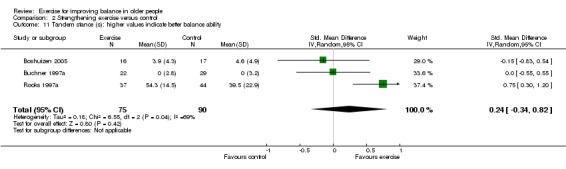
Comparison 2 Strengthening exercise versus control, Outcome 11 Tandem stance (s): higher values indicate better balance ability.
2.12. Analysis.
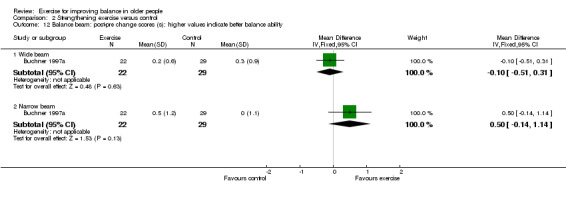
Comparison 2 Strengthening exercise versus control, Outcome 12 Balance beam: post‐pre change scores (s): higher values indicate better balance ability.
For all other secondary outcomes there was insufficient similarity among the trials or common outcomes to perform meta analysis. Data from a single trial with 51 participants indicated statistically significant differences in favour of control for omni‐directional tilt board immediately post intervention (Analysis 2.13). For all other secondary outcome measures there was no statistically significant difference between the exercise or control groups (Analysis 2.8; Analysis 2.9; Analysis 2.10; Analysis 2.13; Analysis 2.14; Analysis 2.15; Analysis 2.16; Analysis 2.17; Analysis 2.18).
2.13. Analysis.
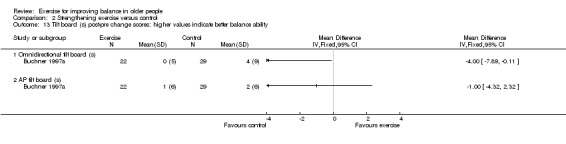
Comparison 2 Strengthening exercise versus control, Outcome 13 Tilt board (s) post‐pre change scores: higher values indicate better balance ability.
2.8. Analysis.

Comparison 2 Strengthening exercise versus control, Outcome 8 6m backward walk (s) lower value indicates better balance.
2.9. Analysis.
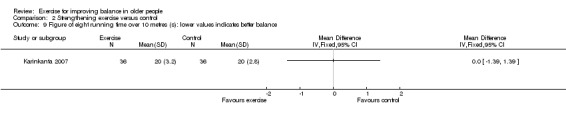
Comparison 2 Strengthening exercise versus control, Outcome 9 Figure of eight running time over 10 metres (s): lower values indicates better balance.
2.10. Analysis.
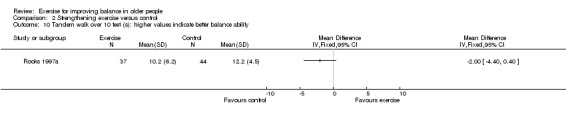
Comparison 2 Strengthening exercise versus control, Outcome 10 Tandem walk over 10 feet (s): higher values indicate better balance ability.
2.14. Analysis.
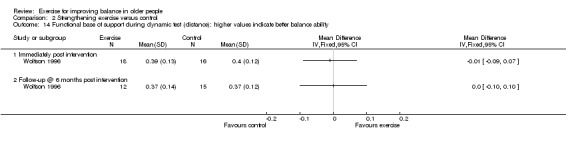
Comparison 2 Strengthening exercise versus control, Outcome 14 Functional base of support during dynamic test (distance): higher values indicate better balance ability.
2.15. Analysis.
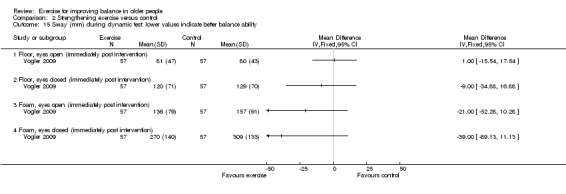
Comparison 2 Strengthening exercise versus control, Outcome 15 Sway (mm) during dynamic test: lower values indicate better balance ability.
2.16. Analysis.

Comparison 2 Strengthening exercise versus control, Outcome 16 Loss of balance during sensory organisation test (errors): less errors indicate better balance ability.
2.17. Analysis.

Comparison 2 Strengthening exercise versus control, Outcome 17 Co‐ordinated stability (errors): less errors indicate better balance ability.
2.18. Analysis.
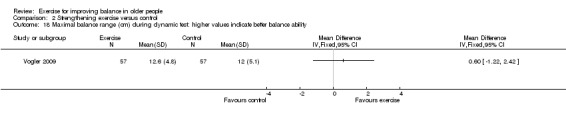
Comparison 2 Strengthening exercise versus control, Outcome 18 Maximal balance range (cm) during dynamic test: higher values indicate better balance ability.
3. 3D exercise versus control
Appendix 4 demonstrates what actual or potential data were available for this comparison for the primary outcomes. Overall, seven out of the 15 trials in this category contributed data to the analyses for one or more primary balance outcomes. In terms of participants, some primary outcome data were available for presentation in the analyses for 534 out of the 1863 randomised participants (29%). While reported, no primary outcome data were available for inclusion in the analyses from a further two trials (197 randomised participants).
When primary outcomes were measured immediately post intervention, the exercise programmes achieved a statistically significant reduction in time taken to perform a Timed Up & Go Test (TUG) (MD ‐1.30 s; 95% CI ‐2.40 to ‐0.20 s, 44 participants, 1 study, Analysis 3.1), an increase in single leg stance time with eyes open (MD 9.60 s; 95% CI 6.64 to 12.56 s, 47 participants, 1 study, Analysis 3.2), an increase in single leg stance time with eyes open change scores (MD 5.60 s; 95% CI 2.02 to 9.18 s, 93 participants, 1 study, Analysis 3.3), an increase in single leg stance time with eyes closed (MD 2.21 s; 95% CI 0.69 to 3.73 s, 48 participants, 1 study, Analysis 3.4), and an increase in Berg Balance Score (MD 1.06 points; 95% CI 0.37 to 1.76 points, 150 participants, 2 studies, Analysis 3.6). However, there was no statistically significant difference between the exercise or control groups for gait speed (Analysis 3.5). The random effects model was used to pool data in Analysis 3.5 due to significant amounts of heterogeneity: Chi² = 7.28, df = 2 (P = 0.03); I² = 73%.
3.1. Analysis.
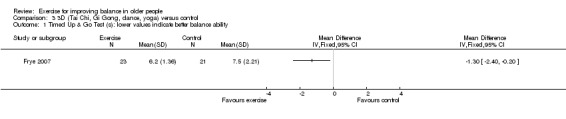
Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 1 Timed Up & Go Test (s): lower values indicate better balance ability.
3.2. Analysis.
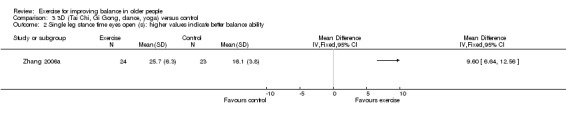
Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 2 Single leg stance time eyes open (s): higher values indicate better balance ability.
3.3. Analysis.
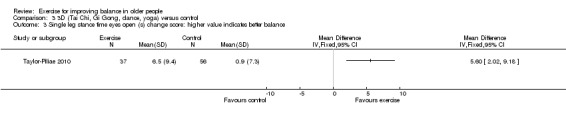
Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 3 Single leg stance time eyes open (s) change score: higher value indicates better balance.
3.4. Analysis.
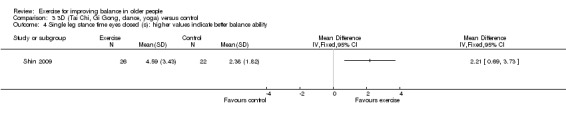
Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 4 Single leg stance time eyes closed (s): higher values indicate better balance ability.
3.6. Analysis.

Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 6 Berg Balance Scale (score out of 56) higher values indicate better balance ability.
3.5. Analysis.
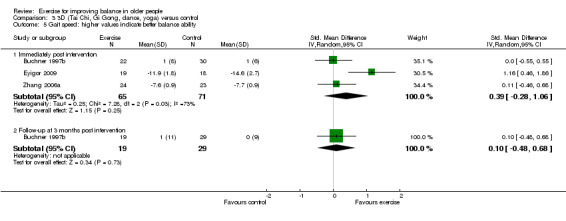
Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 5 Gait speed: higher values indicate better balance ability.
Follow‐up data were reported for some primary outcome measures but there was no statistically significant difference between the exercise or control groups for gait speed at three months (one study, Analysis 3.5) or Berg Balance Score at nine months (one study, Analysis 3.6) indicating that any effects were not maintained beyond the end of the exercise programme.
For secondary outcome measures with data for more than one study, there were no statistically significant differences between the exercise or control groups for physical performance score (Analysis 3.11), anterio‐posterior stability during stance (Analysis 3.20) and mediolateral stability during stance (Analysis 3.21).
3.11. Analysis.
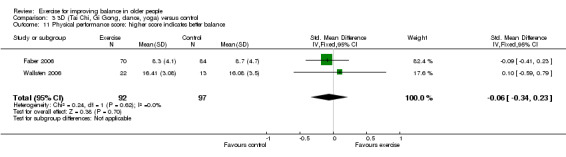
Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 11 Physical performance score: higher score indicates better balance.
3.20. Analysis.
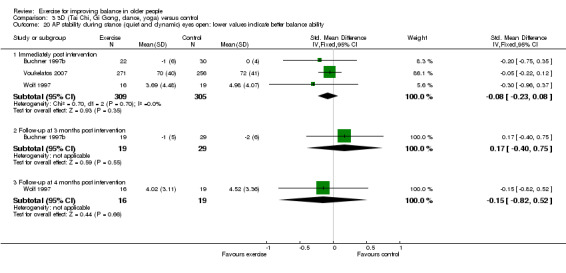
Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 20 AP stability during stance (quiet and dynamic) eyes open: lower values indicate better balance ability.
3.21. Analysis.
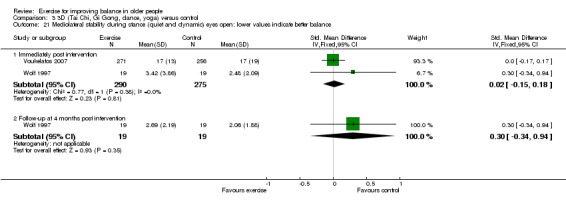
Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 21 Mediolateral stability during stance (quiet and dynamic) eyes open: lower values indicate better balance.
For all other secondary outcomes there was insufficient similarity among the trials or common outcomes to perform meta‐analysis. Data from single trials with small numbers of participants indicated statistically significant differences in favour of exercise programmes for wide balance beam (Analysis 3.13), anterio‐posterior displacement during obstacle course (Analysis 3.14), sensory organisation test (Analysis 3.16), mediolateral displacement during obstacle course (Analysis 3.17) and base of support (Analysis 3.18). Data from a single trial with 56 participants indicated statistically significant differences in favour of the control group for the functional reach test (Analysis 3.7). There were no statistically significant differences between the exercise or control groups for all other secondary outcomes at any time points (Analysis 3.8; Analysis 3.9; Analysis 3.10; Analysis 3.12; Analysis 3.15; Analysis 3.19; Analysis 3.22; Analysis 3.23; Analysis 3.24; Analysis 3.25; Analysis 3.26).
3.13. Analysis.

Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 13 Wide balance beam post‐pre change scores (m/s): lower values indicate better balance ability.
3.14. Analysis.
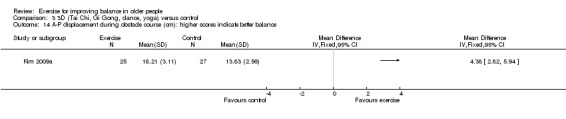
Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 14 A‐P displacement during obstacle course (cm): higher scores indicate better balance.
3.16. Analysis.
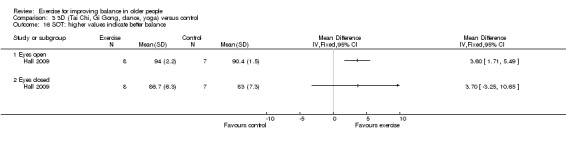
Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 16 SOT: higher values indicate better balance.
3.17. Analysis.
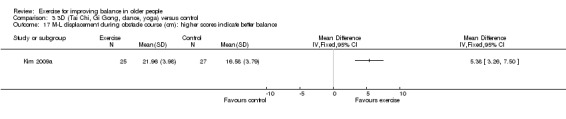
Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 17 M‐L displacement during obstacle course (cm): higher scores indicate better balance.
3.18. Analysis.

Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 18 Base of support (cm2) higher values indicate better balance.
3.7. Analysis.

Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 7 Functional Reach Test change scores (cm): higher values indicate better balance ability.
3.8. Analysis.
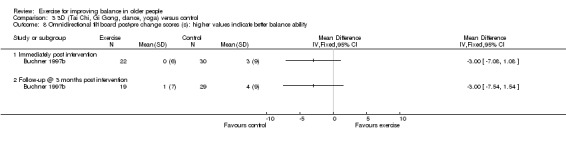
Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 8 Omnidirectional tilt board post‐pre change scores (s): higher values indicate better balance ability.
3.9. Analysis.
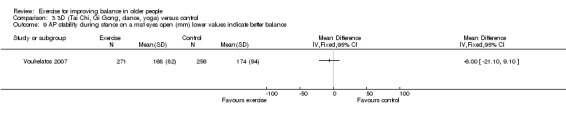
Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 9 AP stability during stance on a mat eyes open (mm) lower values indicate better balance.
3.10. Analysis.
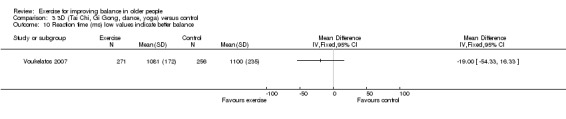
Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 10 Reaction time (ms) low values indicate better balance.
3.12. Analysis.
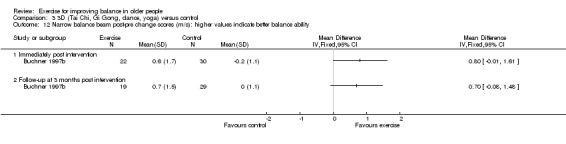
Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 12 Narrow balance beam post‐pre change scores (m/s): higher values indicate better balance ability.
3.15. Analysis.
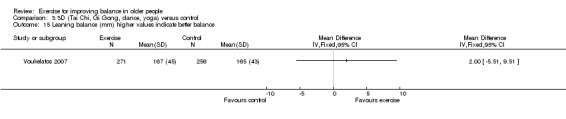
Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 15 Leaning balance (mm) higher values indicate better balance.
3.19. Analysis.
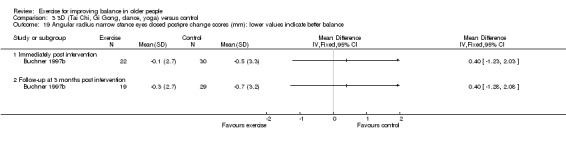
Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 19 Angular radius narrow stance eyes closed post‐pre change scores (mm): lower values indicate better balance.
3.22. Analysis.
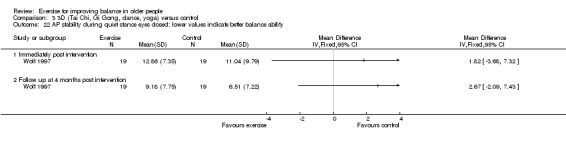
Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 22 AP stability during quiet stance eyes closed: lower values indicate better balance ability.
3.23. Analysis.
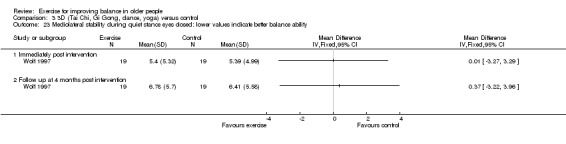
Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 23 Mediolateral stability during quiet stance eyes closed: lower values indicate better balance ability.
3.24. Analysis.
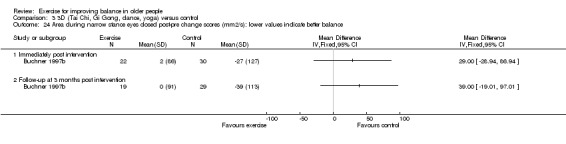
Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 24 Area during narrow stance eyes closed post‐pre change scores (mm2/s): lower values indicate better balance.
3.25. Analysis.

Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 25 Area during narrow stance eyes open post‐pre change scores (mm2/s): lower values indicate better balance.
3.26. Analysis.
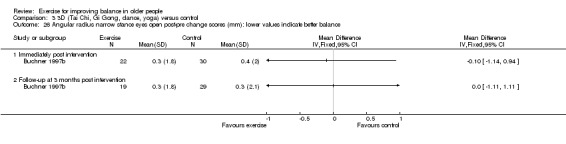
Comparison 3 3D (Tai Chi, Gi Gong, dance, yoga) versus control, Outcome 26 Angular radius narrow stance eyes open post‐pre change scores (mm): lower values indicate better balance.
4. General physical activity (walking)
Appendix 5 demonstrates what actual or potential data were available for this comparison for the primary outcomes. Overall, five out of the seven trials in this category contributed data to the analyses for one or more primary balance outcomes. In terms of participants, some primary outcome data were available for presentation in the analyses for 189 out of the 287 randomised participants (66%). While reported, no primary outcome data were available for inclusion in the analyses from a further two trials (66 randomised participants).
When primary outcomes were measured immediately post intervention or at three months follow‐up, there were no statistically significant differences between the exercise or control groups for Timed Up & Go Test (Analysis 4.1), single leg stance with eyes open (two studies, Analysis 4.2), single leg stance with eyes closed (one study, Analysis 4.3), nor in self paced gait speed (three studies, Analysis 4.4). The random effects model was used to pool data in Analysis 4.4 due to significant amounts of heterogeneity: Chi² = 11.16, df = 2 (P = 0.004); I² = 82%. No studies reported adverse events associated with the intervention.
4.1. Analysis.
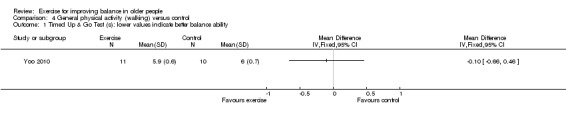
Comparison 4 General physical activity (walking) versus control, Outcome 1 Timed Up & Go Test (s): lower values indicate better balance ability.
4.2. Analysis.
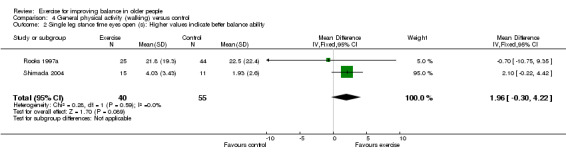
Comparison 4 General physical activity (walking) versus control, Outcome 2 Single leg stance time eyes open (s): Higher values indicate better balance ability.
4.3. Analysis.
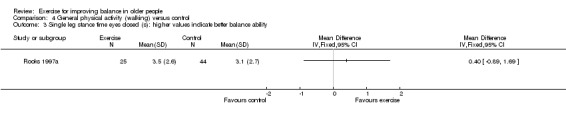
Comparison 4 General physical activity (walking) versus control, Outcome 3 Single leg stance time eyes closed (s): higher values indicate better balance ability.
4.4. Analysis.
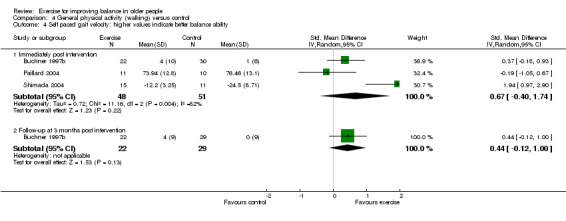
Comparison 4 General physical activity (walking) versus control, Outcome 4 Self paced gait velocity: higher values indicate better balance ability.
For other secondary outcomes, there was insufficient similarity among the trials or common outcomes to perform meta‐analysis. Data from single trials with fewer than 50 participants indicated statistically significant differences in favour of exercise programmes for the functional reach test (Analysis 4.5), tandem stance time (Analysis 4.6), tandem walk over 10 feet (Analysis 4.7), area during narrow stance eyes closed (Analysis 4.11) and stability score during static test floor eyes open (Analysis 4.14).
4.5. Analysis.

Comparison 4 General physical activity (walking) versus control, Outcome 5 Functional Reach Test (cm): higher values indicate better balance ability.
4.6. Analysis.
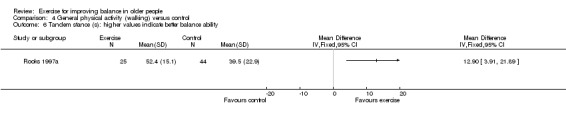
Comparison 4 General physical activity (walking) versus control, Outcome 6 Tandem stance (s): higher values indicate better balance ability.
4.7. Analysis.
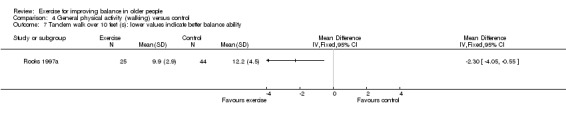
Comparison 4 General physical activity (walking) versus control, Outcome 7 Tandem walk over 10 feet (s): lower values indicate better balance ability.
4.11. Analysis.
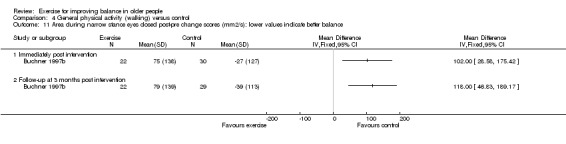
Comparison 4 General physical activity (walking) versus control, Outcome 11 Area during narrow stance eyes closed post‐pre change scores (mm2/s): lower values indicate better balance.
4.14. Analysis.

Comparison 4 General physical activity (walking) versus control, Outcome 14 Stability score during static test: higher values indicate better balance ability.
There were no statistically significant differences between the exercise or control groups for all other secondary outcomes ( Analysis 4.8; Analysis 4.9; Analysis 4.10; Analysis 4.12; Analysis 4.13; Analysis 4.15; Analysis 4.16; Analysis 4.17).
4.8. Analysis.
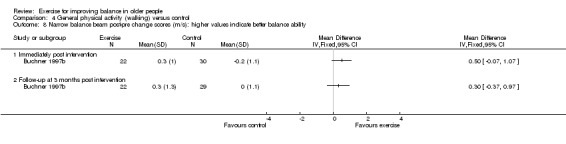
Comparison 4 General physical activity (walking) versus control, Outcome 8 Narrow balance beam post‐pre change scores (m/s): higher values indicate better balance ability.
4.9. Analysis.
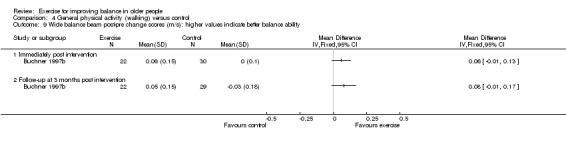
Comparison 4 General physical activity (walking) versus control, Outcome 9 Wide balance beam post‐pre change scores (m/s): higher values indicate better balance ability.
4.10. Analysis.
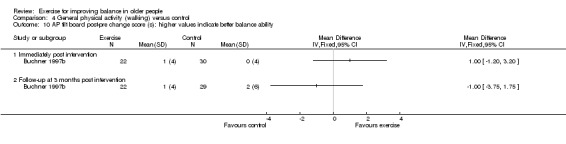
Comparison 4 General physical activity (walking) versus control, Outcome 10 AP tilt board post‐pre change score (s): higher values indicate better balance ability.
4.12. Analysis.
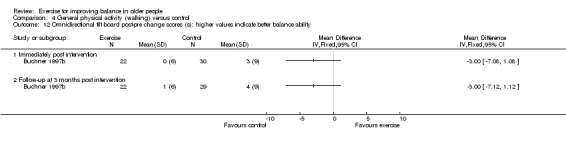
Comparison 4 General physical activity (walking) versus control, Outcome 12 Omnidirectional tilt board post‐pre change scores (s): higher values indicate better balance ability.
4.13. Analysis.

Comparison 4 General physical activity (walking) versus control, Outcome 13 Angular radius narrow stance eyes open post‐pre change scores (mm): lower values indicate better balance.
4.15. Analysis.
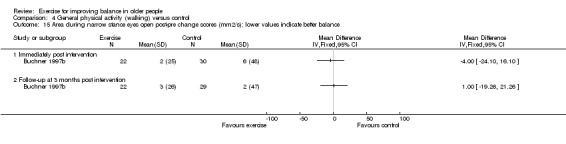
Comparison 4 General physical activity (walking) versus control, Outcome 15 Area during narrow stance eyes open post‐pre change scores (mm2/s): lower values indicate better balance.
4.16. Analysis.
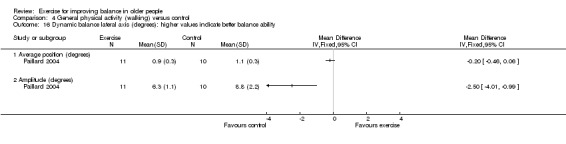
Comparison 4 General physical activity (walking) versus control, Outcome 16 Dynamic balance lateral axis (degrees): higher values indicate better balance ability.
4.17. Analysis.
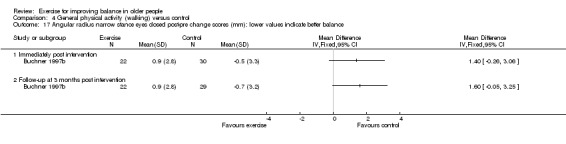
Comparison 4 General physical activity (walking) versus control, Outcome 17 Angular radius narrow stance eyes closed post‐pre change scores (mm): lower values indicate better balance.
5. General physical activity (cycling) versus control
Appendix 6 demonstrates what data were available for this comparison, for which there was only one trial (54 participants). When primary outcomes were measured immediately post intervention there were no statistically significant differences between the exercise or control groups for gait velocity (Analysis 5.1). There were no statistically significant differences between the exercise or control groups for all other secondary outcomes (Analysis 5.2; Analysis 5.3; Analysis 5.4; Analysis 5.5; Analysis 5.6; Analysis 5.7; Analysis 5.8; Analysis 5.9). Buchner 1997b did not report on adverse events.
5.1. Analysis.
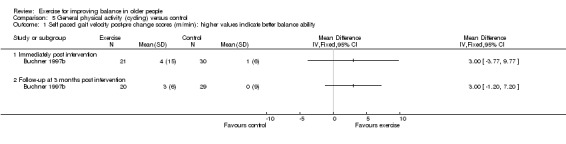
Comparison 5 General physical activity (cycling) versus control, Outcome 1 Self paced gait velocity post‐pre change scores (m/min): higher values indicate better balance ability.
5.2. Analysis.
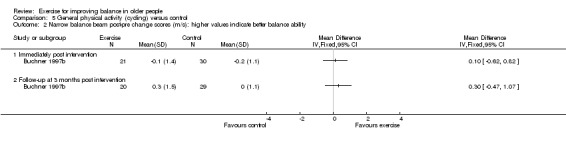
Comparison 5 General physical activity (cycling) versus control, Outcome 2 Narrow balance beam post‐pre change scores (m/s): higher values indicate better balance ability.
5.3. Analysis.

Comparison 5 General physical activity (cycling) versus control, Outcome 3 Wide balance beam post‐pre change scores (m/s): higher values indicate better balance ability.
5.4. Analysis.
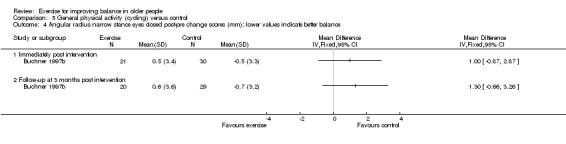
Comparison 5 General physical activity (cycling) versus control, Outcome 4 Angular radius narrow stance eyes closed post‐pre change scores (mm): lower values indicate better balance.
5.5. Analysis.
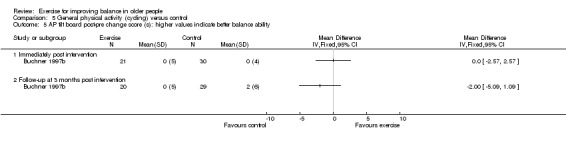
Comparison 5 General physical activity (cycling) versus control, Outcome 5 AP tilt board post‐pre change score (s): higher values indicate better balance ability.
5.6. Analysis.
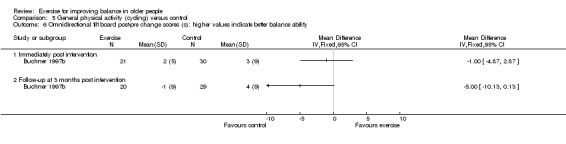
Comparison 5 General physical activity (cycling) versus control, Outcome 6 Omnidirectional tilt board post‐pre change scores (s): higher values indicate better balance ability.
5.7. Analysis.
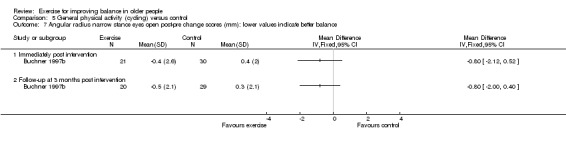
Comparison 5 General physical activity (cycling) versus control, Outcome 7 Angular radius narrow stance eyes open post‐pre change scores (mm): lower values indicate better balance.
5.8. Analysis.
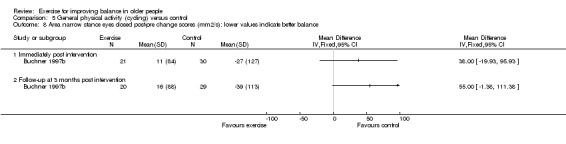
Comparison 5 General physical activity (cycling) versus control, Outcome 8 Area narrow stance eyes closed post‐pre change scores (mm2/s): lower values indicate better balance.
5.9. Analysis.
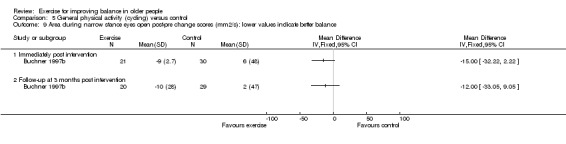
Comparison 5 General physical activity (cycling) versus control, Outcome 9 Area during narrow stance eyes open post‐pre change scores (mm2/s): lower values indicate better balance.
6. Computerised balance versus control
Neither study (Hatzitaki 2009; Wolf 1997) in this category reported data for the primary balance outcomes (seeAppendix 7), nor for adverse events. Data from Wolf 1997 (48 participants) indicated statistically significant differences in favour of exercise programmes for AP stability during stance immediately post intervention and at four months follow‐up (Analysis 6.1) and statistically significant differences in favour of control for mediolateral stability during stance eyes open at four months (Analysis 6.2). There were no statistically significant differences between the exercise or control groups for all other secondary outcomes and time points (Analysis 6.2; Analysis 6.3; Analysis 6.4).
6.1. Analysis.
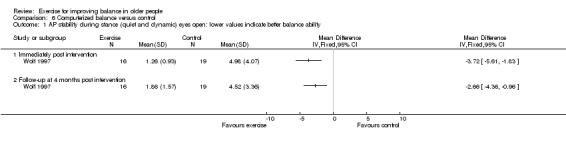
Comparison 6 Computerized balance versus control, Outcome 1 AP stability during stance (quiet and dynamic) eyes open: lower values indicate better balance ability.
6.2. Analysis.
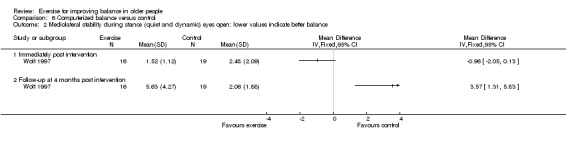
Comparison 6 Computerized balance versus control, Outcome 2 Mediolateral stability during stance (quiet and dynamic) eyes open: lower values indicate better balance.
6.3. Analysis.

Comparison 6 Computerized balance versus control, Outcome 3 AP stability during quiet stance eyes closed: lower values indicate better balance ability.
6.4. Analysis.

Comparison 6 Computerized balance versus control, Outcome 4 Mediolateral stability during quiet stance eyes closed: lower values indicate better balance ability.
7. Vibration versus control
Appendix 8 demonstrates what data were available for this comparison for the primary outcomes. Overall, one out of the three trials in this category contributed data to the analyses for just one primary balance outcome. In terms of participants, some primary outcome data were available for presentation in the analyses for 37 out of the 310 randomised participants (12%).
When measured immediately post intervention there was no statistically significant difference between the exercise or control groups for Timed Up & Go Test (Analysis 7.1). No studies reported adverse events. For other secondary outcomes there was insufficient similarity among the trials or common outcomes to perform meta analysis. Data from single trials indicated statistically significant differences in favour of exercise programmes for directional control (Analysis 7.3), maximum excursion of limits of stability (Analysis 7.4) and movement velocity (Analysis 7.5). There were no statistically significant differences between the exercise or control groups for all other secondary outcomes and time points (Analysis 7.6; Analysis 7.7; Analysis 7.8).
7.1. Analysis.
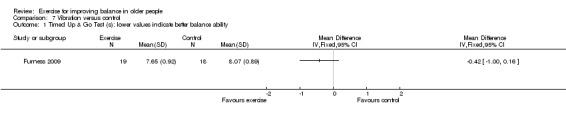
Comparison 7 Vibration versus control, Outcome 1 Timed Up & Go Test (s): lower values indicate better balance ability.
7.3. Analysis.
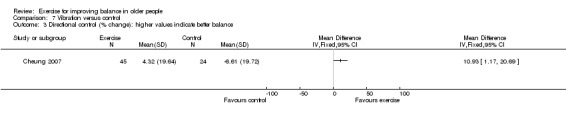
Comparison 7 Vibration versus control, Outcome 3 Directional control (% change): higher values indicate better balance.
7.4. Analysis.

Comparison 7 Vibration versus control, Outcome 4 Maxium excursion of limits of stability (LOS) test:(% change) higher values indicate better balance ability.
7.5. Analysis.

Comparison 7 Vibration versus control, Outcome 5 Movement velocity (% change): higher values indicate better balance.
7.6. Analysis.
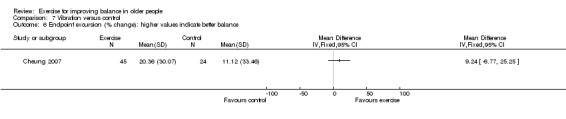
Comparison 7 Vibration versus control, Outcome 6 Endpoint excursion (% change): higher values indicate better balance.
7.7. Analysis.

Comparison 7 Vibration versus control, Outcome 7 Reaction Time (% change): lower values indicate better balance.
7.8. Analysis.
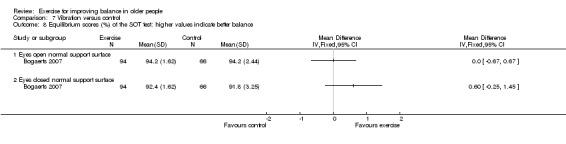
Comparison 7 Vibration versus control, Outcome 8 Equilibrium scores (%) of the SOT test: higher values indicate better balance.
8. Multiple exercise types versus control
Appendix 9 demonstrates what actual or potential data were available for this comparison for the primary outcomes. Overall, 28 out of the 43 trials in this category contributed data to the analyses for one or more primary balance outcomes. In terms of participants, some primary outcome data were available for presentation in the analyses for 1546 out of the 3847 randomised participants (40%). While reported, no primary outcome data were available for inclusion in the analyses from a further four trials (408 randomised participants).
When primary outcomes were measured immediately post intervention, the exercise programmes achieved a statistically significant reduction in time to perform a Timed Up & Go Test (TUG) (MD ‐1.63 s; 95% CI ‐2.28 to ‐0.98 s, 635 participants, 12 studies, Analysis 8.1) (note, the random‐effects model was used due to significant amounts of heterogeneity: Chi² = 61.24, df = 11 (P < 0.00001); I² = 82%); an increase in single leg stance time with eyes open (MD 5.03 s; 95% CI 1.19 to 8.87 s, 545 participants, 9 studies, Analysis 8.3) (again, the random‐effects model was used); an increase in single leg stance time with eyes closed (MD 1.60 s; 95% CI ‐0.01 to 3.20 s, 176 participants, 2 studies, Analysis 8.5). Additionally, the exercise programmes achieved a statistically significant increase in Berg Balance Score at the end of the intervention (MD 1.84 points; 95% CI 0.71 to 2.97 points, 80 participants, 2 studies, Analysis 8.9) and Berg Balance Score change score for Worm 2001 in Analysis 8.10 but not for Rosendahl 2006 at the end of the intervention; data not pooled because of excessive heterogeneity.
8.1. Analysis.
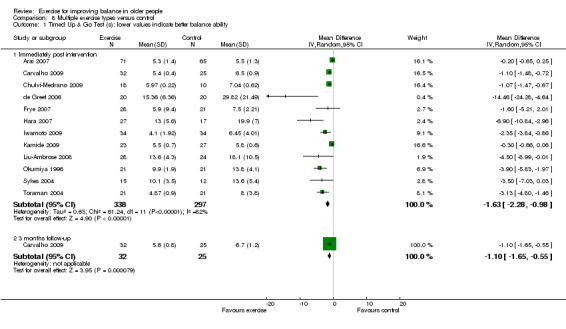
Comparison 8 Multiple exercise types versus control, Outcome 1 Timed Up & Go Test (s): lower values indicate better balance ability.
8.3. Analysis.
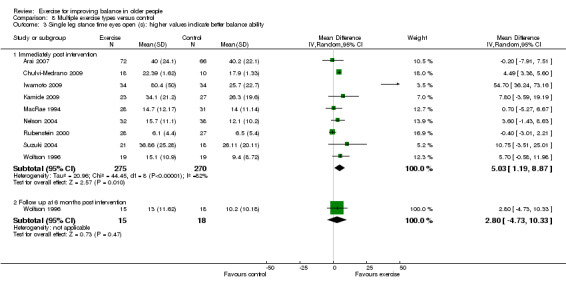
Comparison 8 Multiple exercise types versus control, Outcome 3 Single leg stance time eyes open (s): higher values indicate better balance ability.
8.5. Analysis.

Comparison 8 Multiple exercise types versus control, Outcome 5 Single leg stance time eyes closed (s): higher values indicate better balance ability.
8.9. Analysis.
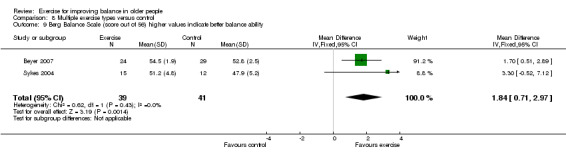
Comparison 8 Multiple exercise types versus control, Outcome 9 Berg Balance Scale (score out of 56) higher values indicate better balance ability.
8.10. Analysis.
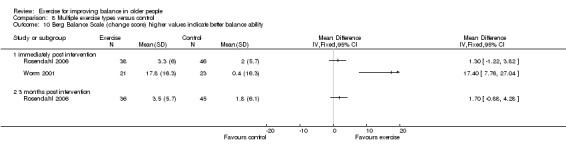
Comparison 8 Multiple exercise types versus control, Outcome 10 Berg Balance Scale (change score) higher values indicate better balance ability.
However, there was no statistically significant difference between the exercise or control groups for single leg stance times with eyes open change scores (SMD 0.00; 95% CI ‐0.31 to 0.31) (Analysis 8.2), self selected gait speed at the end of the intervention (SMD 0.04; 95% CI ‐0.10 to 0.17, 818 participants, 15 studies; Analysis 8.6), in self paced or maximum gait speed change scores (Analysis 8.7; data not pooled because of excessive heterogeneity), and gait speed at fastest pace (Analysis 8.8).
8.2. Analysis.

Comparison 8 Multiple exercise types versus control, Outcome 2 Single leg stance time eyes open (s) change score: higher value indicates better balance.
8.6. Analysis.
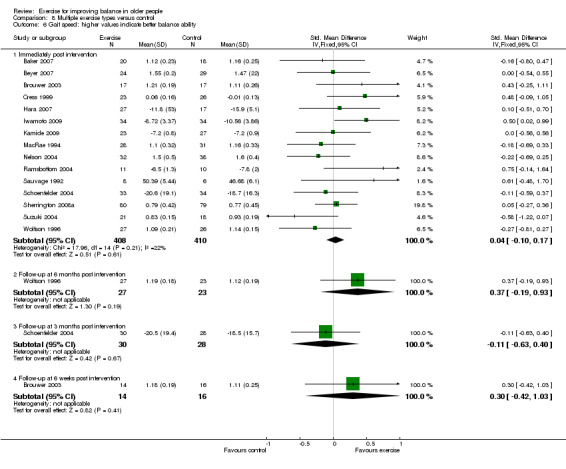
Comparison 8 Multiple exercise types versus control, Outcome 6 Gait speed: higher values indicate better balance ability.
8.7. Analysis.
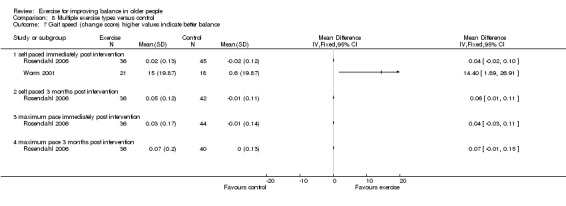
Comparison 8 Multiple exercise types versus control, Outcome 7 Gait speed (change score) higher values indicate better balance.
8.8. Analysis.
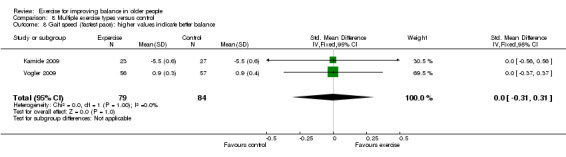
Comparison 8 Multiple exercise types versus control, Outcome 8 Gait speed (fastest pace): higher values indicate better balance.
Six studies reported adverse events; however, in five of these it is unclear from the reporting whether these relate to exercise or control groups or the total sample. In Iwamoto 2009, four participants in the control group experienced one fall each during the five months intervention period. Of four falls, one was due to a stumble of the toe, and three were caused by lurches. There were no multiple fallers during the four months intervention period. No serious adverse events, such as severe fall‐related injuries or adverse cardiovascular effects, were observed. Karinkanta 2007 reported 14 due to musculoskeletal injuries or symptoms and two falls but the participants returned to classes. No difference in monthly reported health problems with exercisers and controls. In Liu‐Ambrose 2008, two participants in the exercise group reported low back pain associated with the exercises. One resumed exercising, and the other discontinued the exercise. Nelson 2004 reported that one participant fell in the exercise group and one had food poisoning in the control group. Rosendahl 2006 stated that "No adverse event during the sessions led to a manifest injury or disease", but did not provide separate group data for adverse events. Vogler 2009 reported 22 events in 22 participants (soreness (lower back, hip, knee pain)).
Sensitivity analyses were performed to examine the potential effects of unit of analysis issues on results. Two cluster RCTs (MacRae 1994;Rosendahl 2006) were removed from the meta‐analyses (Analysis 8.3; Analysis 8.6; Analysis 8.7; Analysis 8.10). Analysis 8.4 shows the effect of removing MacRae 1994 from Analysis 8.3. The results for the random‐effects model was checked for Analysis 8.1 and Analysis 8.3, and the more conservative result selected instead of that for the fixed‐effect model.
8.4. Analysis.
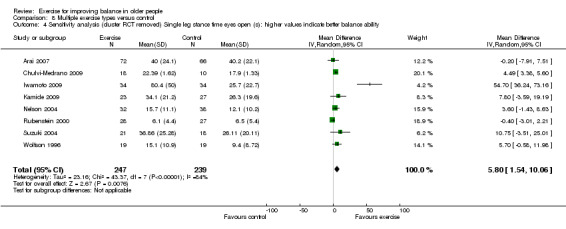
Comparison 8 Multiple exercise types versus control, Outcome 4 Sensitivity analysis (cluster RCT removed) Single leg stance time eyes open (s): higher values indicate better balance ability.
Follow‐up data were reported for some primary outcome measures. The exercise programmes achieved a statistically significant reduction in time to perform a Timed Up & Go Test at three months follow‐up (MD ‐1.10 s; 95% CI ‐1.65 to ‐0.55 s, 57 participants, one study, Analysis 8.1) but there was no statistically significant difference between the exercise or control groups for single leg stance time with eyes open at six months (33 participants, one study, Analysis 8.2), or gait speed at six weeks, three months or six months post intervention (single studies, Analysis 8.6 and Analysis 8.7). These indicated that any effects were not maintained beyond the end of the exercise programme.
For secondary outcome measures, the exercise programmes achieved a statistically significant improvement in functional reach immediately post intervention (MD 5.77 cm; 95% CI 2.70 to 8.84 cm, 350 participants, 7 trials, Analysis 8.11), tandem walk (70 participants, one study, Analysis 8.13), tandem stance time immediately post intervention (MD 2.82 s; 95% CI 1.28 to 4.36 s, 294 participants, 3 trials, Analysis 8.14) (but not at three months follow‐up), and figure of 8 time (113 participants, 2 trials, Analysis 8.17). Data were not pooled because of excessive heterogeneity in Analysis 8.15 and Analysis 8.32. Both trials in Analysis 8.15 achieved statistically significant improvement in tandem walk (number of steps), but only two of the four trials in Analysis 8.32 achieved statistically significant improvement in body sway.
8.11. Analysis.

Comparison 8 Multiple exercise types versus control, Outcome 11 Functional Reach Test (cm): higher values indicate better balance ability.
8.13. Analysis.
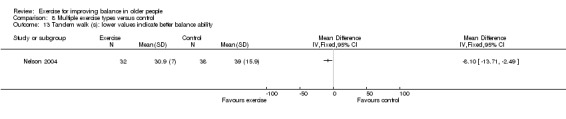
Comparison 8 Multiple exercise types versus control, Outcome 13 Tandem walk (s): lower values indicate better balance ability.
8.14. Analysis.
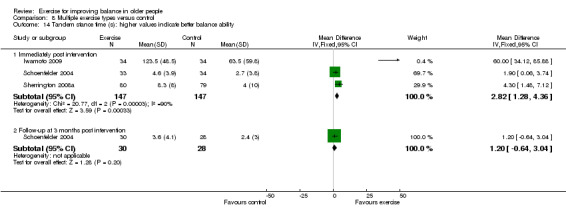
Comparison 8 Multiple exercise types versus control, Outcome 14 Tandem stance time (s): higher values indicate better balance ability.
8.17. Analysis.
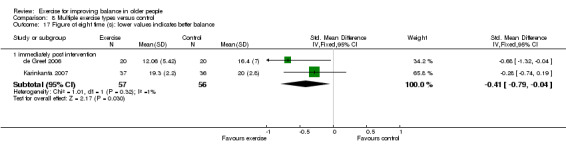
Comparison 8 Multiple exercise types versus control, Outcome 17 Figure of eight time (s): lower values indicates better balance.
8.15. Analysis.
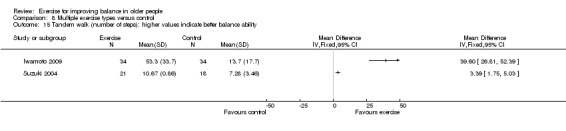
Comparison 8 Multiple exercise types versus control, Outcome 15 Tandem walk (number of steps): higher values indicate better balance ability.
8.32. Analysis.
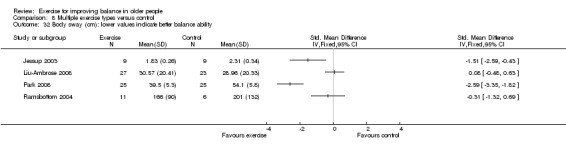
Comparison 8 Multiple exercise types versus control, Outcome 32 Body sway (cm): lower values indicate better balance ability.
For other secondary outcomes there was insufficient similarity among the trials or common outcomes to perform meta analysis. Data from single trials with fewer than 50 participants indicated statistically significant differences in favour of exercise programmes for functional reach test change score (Analysis 8.12) and functional base of support (Analysis 8.29) and in favour of controls for total distance travelled by COP during quiet stance (Analysis 8.21). There were no statistically significant differences between the exercise or control groups for all other secondary outcomes and time points (Analysis 8.16; Analysis 8.18; Analysis 8.19; Analysis 8.20; Analysis 8.22; Analysis 8.23; Analysis 8.24; Analysis 8.25; Analysis 8.26; Analysis 8.27; Analysis 8.28; Analysis 8.30; Analysis 8.31; Analysis 8.33; Analysis 8.34).
8.12. Analysis.
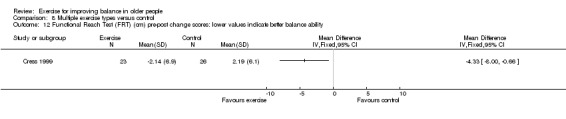
Comparison 8 Multiple exercise types versus control, Outcome 12 Functional Reach Test (FRT) (cm) pre‐post change scores: lower values indicate better balance ability.
8.29. Analysis.

Comparison 8 Multiple exercise types versus control, Outcome 29 Functional base of support (distance) during dynamic test: higher values indicate better balance ability.
8.21. Analysis.
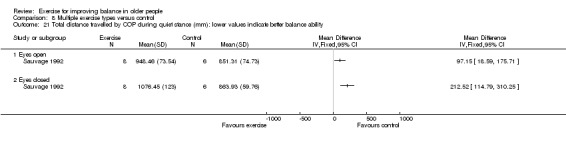
Comparison 8 Multiple exercise types versus control, Outcome 21 Total distance travelled by COP during quiet stance (mm): lower values indicate better balance ability.
8.16. Analysis.
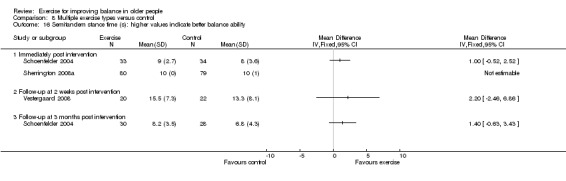
Comparison 8 Multiple exercise types versus control, Outcome 16 Semitandem stance time (s): higher values indicate better balance ability.
8.18. Analysis.
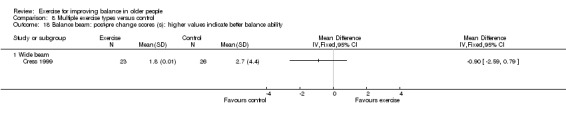
Comparison 8 Multiple exercise types versus control, Outcome 18 Balance beam: post‐pre change scores (s): higher values indicate better balance ability.
8.19. Analysis.
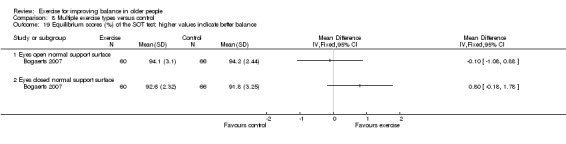
Comparison 8 Multiple exercise types versus control, Outcome 19 Equilibrium scores (%) of the SOT test: higher values indicate better balance.
8.20. Analysis.
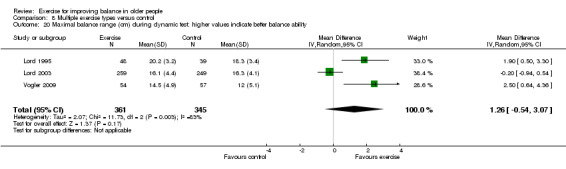
Comparison 8 Multiple exercise types versus control, Outcome 20 Maximal balance range (cm) during dynamic test: higher values indicate better balance ability.
8.22. Analysis.
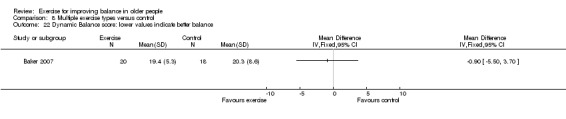
Comparison 8 Multiple exercise types versus control, Outcome 22 Dynamic Balance score: lower values indicate better balance.
8.23. Analysis.
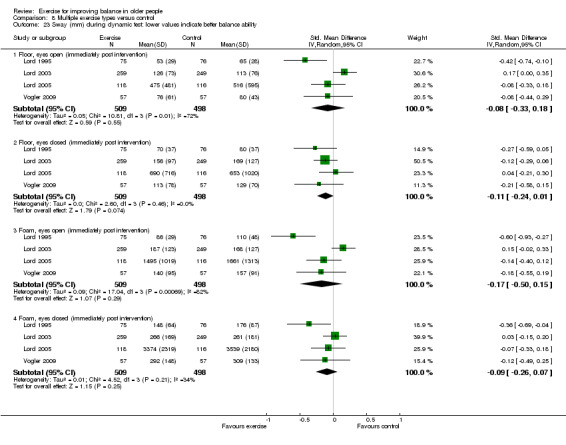
Comparison 8 Multiple exercise types versus control, Outcome 23 Sway (mm) during dynamic test: lower values indicate better balance ability.
8.24. Analysis.
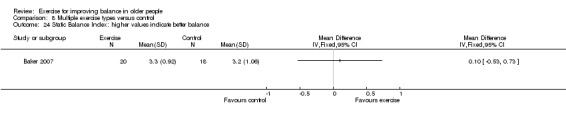
Comparison 8 Multiple exercise types versus control, Outcome 24 Static Balance Index: higher values indicate better balance.
8.25. Analysis.
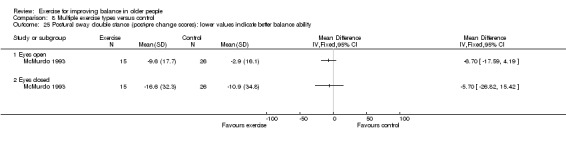
Comparison 8 Multiple exercise types versus control, Outcome 25 Postural sway double stance (post‐pre change scores): lower values indicate better balance ability.
8.26. Analysis.
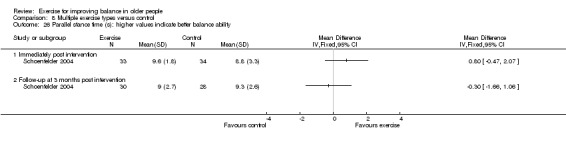
Comparison 8 Multiple exercise types versus control, Outcome 26 Parallel stance time (s): higher values indicate better balance ability.
8.27. Analysis.
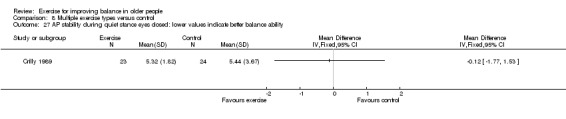
Comparison 8 Multiple exercise types versus control, Outcome 27 AP stability during quiet stance eyes closed: lower values indicate better balance ability.
8.28. Analysis.
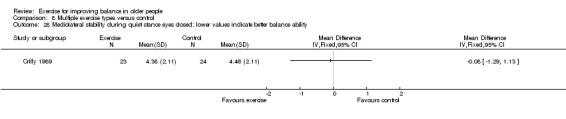
Comparison 8 Multiple exercise types versus control, Outcome 28 Mediolateral stability during quiet stance eyes closed: lower values indicate better balance ability.
8.30. Analysis.
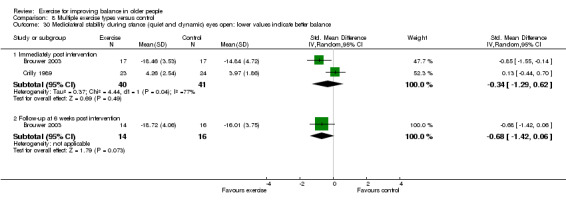
Comparison 8 Multiple exercise types versus control, Outcome 30 Mediolateral stability during stance (quiet and dynamic) eyes open: lower values indicate better balance.
8.31. Analysis.

Comparison 8 Multiple exercise types versus control, Outcome 31 Loss of balance during sensory organisation test (errors): less errors indicate better balance ability.
8.33. Analysis.
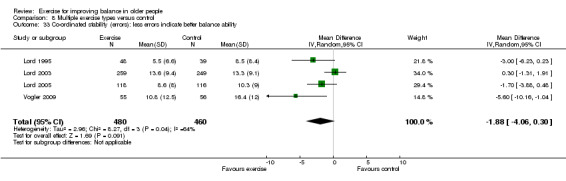
Comparison 8 Multiple exercise types versus control, Outcome 33 Co‐ordinated stability (errors): less errors indicate better balance ability.
8.34. Analysis.
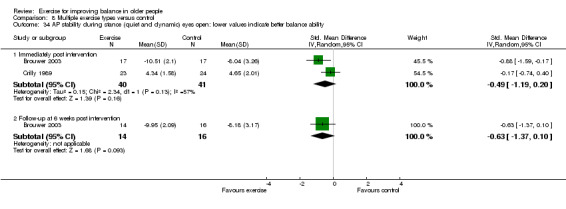
Comparison 8 Multiple exercise types versus control, Outcome 34 AP stability during stance (quiet and dynamic) eyes open: lower values indicate better balance ability.
Discussion
The objective of this review was to examine the effects of exercise interventions designed to improve balance in older people, aged 60 and over, living in the community or in institutional care. From the data available for presentation in the analyses, this review provides some evidence that some exercise types compared with usual activity are moderately effective, at least immediately post intervention, in improving clinical balance outcomes in older people. Exercise programmes involving gait, balance, co‐ordination and functional exercises; muscle strengthening exercise; 3D exercise types and multiple exercise types appear to have the greatest impact on at least some 'indirect' quantifiable measures of balance such as the Timed Up & Go (TUG) test, single leg stance, walking speed and a global subjective measure of balance, the Berg Balance Score. However, these favourable findings must be viewed in the context of the, often substantial, incompleteness of the available data and the potential for bias in the included studies.
Summary of main results
A total of 94 (62 new) studies (involving 9821 participants at entry) were included in this systematic review. Seventy five studies provided data (primary or secondary outcome) that could be presented in the analyses. There was large variation across the studies in the characteristics of participants, design and content of the exercise interventions, and the outcomes assessed. We performed meta‐analyses where there was sufficient similarity among the trials and where common outcomes had been measured.
The majority of participants were healthy community dwelling individuals and were on average aged between 60 to 75 years, in 46 studies and over 75 years in 49 studies. Most studies (n = 63) included both men and women, 25 studies only women and five studies only men. Some studies (n = 28) included participants described as frail or with activity limitations with 11 studies considering participants residing in hospital or residential facilities. Exercise interventions were heterogeneous. These were categorised into eight types: gait, balance, co‐ordination and functional tasks; strengthening exercise (including resistance or power training); 3D (including Tai Chi, qi gong, dance, yoga); general physical activity (walking); general physical activity (cycling); computerised balance training using visual feedback; vibration platforms; and multiple intervention types included combinations of the above. Exercise sessions took place mainly in gym/clinic or community settings in supervised groups delivered predominantly by healthcare professionals or fitness instructors. The duration of the exercise programmes ranged from four weeks to 12 months, the most frequent being three months. The frequency of the individual sessions ranged from once every two weeks to every day, typically three times per week for one hour each time. Control groups included mainly usual activity, or recreational or attention activities.
It should be noted that each category of exercise was analysed separately and there were over 25 types of outcome measures reported across the studies including indirect clinical measures (quantifiable functional tests) and direct (force platform) measures. Furthermore these measures were not always performed or reported in standardised ways. These relatively small samples of studies and sample sizes resulted in insufficient power for firm conclusions to be drawn from any outcome analysis, therefore these analyses should be seen primarily as hypothesis‐generating.
Direct measures of balance such as force platform measures require expensive equipment and are difficult to use and interpret in clinical or community settings. Conversely, some indirect quantifiable measures of balance such as the Timed Up & Go Test (TUG), single leg stance (SLS) (eyes open and eyes closed), walking speed and a global subjective measure of balance, such as the Berg Balance Score, require minimal equipment and are easy to use in the clinical and community settings. They are also easy to interpret as they relate to functional activities. The interventions examined demonstrated clinically important improvements in balance compared with control in some of these measures.
Timed Up & Go Test
Significant reductions were observed immediately post intervention in time taken to complete the Timed Up & Go Test in favour of exercise groups for; GBFT (MD ‐0.82 s; 95% CI ‐1.56 to ‐0.08 s, 114 participants, 4 studies, Analysis 1.1), strengthening exercise (MD ‐4.30 s; 95% CI ‐7.60 to ‐1.00s, 71 participants, 3 studies, Analysis 2.1), 3D exercise (MD ‐1.30 s; 95% CI ‐2.40 to ‐0.20 s, 44 participants, 1 study, Analysis 3.1) and multiple exercise types (MD ‐1.63 s; 95% CI ‐2.28 to ‐0.98 s), 635 participants, 12 studies, Analysis 8.1). In terms of missing data, there was a relatively small proportion missing for multiple exercise types but substantial amounts missing for other comparisons.
However, there was no statistically significant difference between the control groups and general physical activity (walking) (Analysis 4.1) or vibration (one study, Analysis 7.1) and data for this outcome were not available for general physical activity (cycling) or computerised balance exercise types.
Follow‐up data were only reported for multiple exercise programmes and a statistically significant reduction in time was maintained at three months follow up (MD ‐1.10 s; 95% CI ‐1.65 to ‐0.55 s, 57 participants, 1 study, Analysis 8.1).
Single leg stance on the floor with eyes open
Significant improvements were observed immediately post intervention for; 3D exercise (MD 9.60 s; 95% CI 6.64 to 12.56 s, 47 participants, 1 study, Analysis 3.2) and change scores (MD 5.60 s; 95% CI 2.02 to 9.18 s, 95 participants, 1 study, Analysis 3.3); and multiple exercise types (MD 5.03 s; 95% CI 1.19 to 8.87 s, 545 participants, 9 studies, Analysis 8.3). In terms of missing data there was a relatively small proportion missing for multiple exercise types but substantial amounts missing for the other comparisons.
No significant differences were observed for GBFT (173 participants, 3 studies, Analysis 1.3), strengthening exercise (187 participants, 2 studies, Analysis 2.2), GPA (walking) (one study; Analysis 4.3), and data for this outcome were not available for GPA (cycling), computerised balance or vibration.
Follow‐up data were only reported for GBFT and multiple exercise types; however, there was no statistically significant difference between these and control groups at six months.
Single leg stance on the floor with eyes closed
Significant improvements were observed immediately post intervention for strengthening exercise (MD 1.64 s; 95% CI 0.97 to 2.31 s, 120 participants, 3 studies, Analysis 2.3), 3D (MD 2.21 s; 95% CI 0.69 to 3.73 s, 48 participants, 1 study, Analysis 3.4), and multiple exercise types (MD 1.60 s; 95% CI ‐0.01 to 3.20 s, 176 participants, 2 studies, Analysis 8.5). This outcome was measured by only a small number of studies and was mainly reported and included in the analyses.
No significant differences were observed for GBFT (33 participants, 1 study, Analysis 1.4), or GPA (walking) (one study, Analysis 4.3) and data for this outcome were not available for GPA (cycling), computerised balance or vibration.
Follow‐up data were only reported for strengthening exercise and there was no statistically significant difference between exercise and control groups at six months (one study, Analysis 2.3).
Gait speed
Significant improvements were observed immediately post intervention for GBFT (SMD 0.43; 95% CI 0.11 to 0.75, 156 participants, 4 studies, Analysis 1.5) and strengthening exercise (SMD 0.25; 95% CI 0.05 to 0.46, 375 participants, 8 studies, Analysis 2.4). However there were substantial amounts of missing data, approximately 40% of the possible data, for these outcomes that may impact on these results.
No significant differences were observed for 3D exercise (Analysis 3.5), GPA (walking) (Analysis 4.4), GPA (cycling) (Analysis 5.1) and multiple exercise types (SMD 0.04; 95% CI ‐0.10 to 0.17, 818 participants, 15 studies, Analysis 8.6). Data for this outcome were not available for computerised balance or vibration.
Follow‐up data were only reported for GBFT (one study, Analysis 1.5), and strengthening exercise (one study, Analysis 2.4) at six months, and multiple exercise types at six weeks, three months or six months post intervention (single studies, Analysis 8.6); however, there was no statistically significant difference between these and control groups.
Berg Balance Scale
Significant improvements were observed immediately post intervention for GBFT (MD 3.48 points; 95% CI 2.01 to 4.95 points, 145 participants, 4 studies, Analysis 1.6), 3D exercise (MD 1.06 points; 95% CI 0.37 to 1.76 points, 150 participants, 2 studies, Analysis 3.6), and multiple exercise types (MD 1.84 points; 95% CI 0.71 to 2.97 points, 80 participants, 2 studies, Analysis 8.9). In terms of missing data, there was none missing for 3D exercise (outcome only measured in two trials), a relatively modest proportion missing for multiple exercise types but substantial amounts missing for GBFT.
No significant differences were observed for strengthening exercise (20 participants, one study, Analysis 2.6). Data for this outcome were not available for GPA (walking), GPA (cycling), computerised balance or vibration.
Follow‐up data were only reported for GBFT at four weeks and one year (one study, Analysis 1.6), and 3D exercise at nine months (one study, Analysis 3.6). However, there was no statistically significant difference between these and control groups.
Secondary outcomes
For secondary outcomes, there was generally insufficient similarity among the trials or common outcomes to perform meta‐analysis resulting mainly in data from single trials with fewer than 50 participants. When meta‐analysis was possible, significant improvements were achieved in functional reach tests in favour of exercise programmes for strengthening exercise (Analysis 2.7) and multiple exercise types (Analysis 8.11).
Effectiveness beyond the intervention
This bulk of the available evidence in this review applies to the findings at the end of the exercise intervention. Most of the included studies did not examine follow‐up and only very limited data are available from those that did. Examination of the forest plots indicates that effect sizes are often reduced at follow‐up compared with immediate post‐intervention effects. From the physiological perspective, it is unlikely that the benefits of exercise would be maintained after an exercise programme ends unless the programme included an home exercise component for continuation by the participants after the end of the exercise programme.
Overall completeness and applicability of evidence
The 94 studies included in this review were predominantly in the English language and originate mainly from North America and Europe (n = 65). Whilst this may be seen to limit the applicability of the evidence to these healthcare systems and social environments the evidence has potential generalisability. The majority of participants were healthy community dwelling women and may not have had impairment or activity limitation at baseline. This may have impacted on the capacity of these mainly small studies to reveal any differences, whether positive or negative, between the exercise intervention and control groups. The majority of participants were on average aged between 60 to 75 years in 46 studies and over 75 years in 49 studies. Most studies (n = 63) included both men and women, 25 studies included only women and five studies included only men. Some studies (n = 28) included participants described as frail or with activity limitations with 11 studies considering participants residing in hospital or residential facilities.
The applicability of these results are restricted less by difficulties in defining the intervention, which is a common problem in other studies of complex interventions, but more by the number and type of outcome measures used and inadequate reporting. The interventions investigated included many commonly utilised categories of exercise such as gait, co‐ordination, balance, function, muscle strengthening exercise, walking, cycling, Tai Chi and dance. The definition of adherence or compliance with the exercise intervention and the method of recording and reporting varied considerably across studies and thus these data are difficult to interpret. Furthermore, none of the studies included information indicating enthusiasm for uptake of exercise, or long‐term uptake of exercise among participants in the programmes.
Efficacy and adverse event outcomes were not consistently reported across the studies and when reported did not give sufficient information particularly regarding group allocation, and nature of events and this limited the analyses. Only 75 of the 94 included studies reported appropriate data (primary or secondary outcomes) that could be included in meta‐analysis this has the potential to skew the conclusions drawn in this review. Generally these studies reported positive effects of the exercise programme on balance. Where missing or inappropriately reported data were discovered during data extraction we attempted to contact the original investigators of the study to request the required information.
Incomplete and inadequate reporting of research is a widely recognised problem, which in systematic reviews hampers the critical appraisal and appropriate interpretation via meta‐analyses of research findings. This was a major issue in this review where missing or inappropriately reported data meant that the meta‐analyses are incomplete for most outcomes and comparisons. We have included tables demonstrating what actual or potential data were available for the review (Appendix 2; Appendix 3; Appendix 4; Appendix 5; Appendix 6; Appendix 7; Appendix 8; Appendix 9).
We could assume that in some instances the data were collected but not reported (purposive incomplete data reporting) due to no observed difference between the exercise or control groups, or that any differences between the groups was in opposition to the hypotheses or the results of analyses of other outcomes in the same trial. However, the outcome data may have been collected but inadequately reported for the purpose of including into meta‐analyses. For example, and for appropriate reasons, only non parametric data were provided. In other cases, there was missing information such as measures of variability and numbers in the arms of the trial, or the data were only displayed graphically. However, it must also be considered that some data may in fact be missing completely at random (random incomplete data reporting), for example, because of equipment malfunction, data corruption, staff or participant illness or incorrect data entry.
Generally, for the studies included in this review we are unable to determine for most instances why data were missing. The guidelines on the reporting of trials (CONSORT ‐ Consolidated Standards of Reporting Trials) and publication of trial protocols may improve quality of reporting and negate or highlight issues of purposive incomplete data reporting. While random incomplete data reporting cannot be completely removed, the reporting of this could be improved.
Irrespective of the reasons for the missing data, their non‐availability meant that the meta‐analyses are incomplete for most outcomes and comparisons. Thus the results of all the analyses must be viewed with caution.
The wide range of interventions and outcome measures reported across the studies made it difficult to combine outcomes in meta‐analysis. The lack of longer term follow‐up of outcomes made it difficult to determine any lasting effects. Furthermore, the lack of standardisation of measures and their relative validity, limit the interpretation of these results (for example, direct measures of balance used both force platforms and sway meters). Typically, when these tests are performed under static conditions (e.g. quiet stance, one leg stance) lower values indicate better balance ability but when performed under dynamic conditions (e.g. leaning forwards, backwards and sideways) higher values indicate better balance ability. However, there are difficulties in the interpretation of this type of data as in some populations an increased sway under static conditions may indicate better dynamic control whereas less sway may indicate that the individual is applying compensatory bracing in an effort to maintain stability. Furthermore, for some timed measures of balance, authors applied ceiling effects stipulating a maximum time allowed for the test, and this was not adjusted for in the analysis.
Quality of the evidence
Many studies demonstrate a range of methodological weaknesses, which often reflected inadequate reporting. For example, although the review was restricted to randomised controlled trials, which should limit the potential for selection bias, most trials failed to give any details of how the randomisation sequence was generated or of what precautions were taken in relation to concealment of allocation. The majority of trials were small; only 24 studies had more than 100 participants at entry, and 20 studies had fewer than 40 participants. This again makes trials susceptible to selection bias. Other major weaknesses of individual studies were the lack of blinding of participants and assessors, and not addressing incomplete outcome data.
Although we attempted to extract direct and indirect measures of balance there is a possibility that the measures reported are a biased representation of those collected by the study authors (selective reporting). Indeed there were 15 broad categories of outcome measures used across the studies, some of which were used under a variety of conditions, e.g. eyes open, eyes closed, different surfaces. Only 31 studies addressed incomplete outcome data (for example, using intention‐to‐treat analysis), with the remainder reporting the results for only those participants who completed all post‐treatment assessments. The seven studies that were cluster randomised studies did not appear to make adjustments for the cluster effect of reported data that were included in the analyses. As a result, these studies may have overly narrow confidence intervals and will receive more weight than is appropriate in a meta‐analysis.
There was limited follow‐up data to demonstrate the extent to which the effects of programmes were maintained. Some included studies reported findings based on change scores. This requires measurement of the outcome twice and can result in bias for outcomes that are difficult to measure precisely because the measurement error may be larger than the true difference between person baseline variability. These issues and the associated potential risk of bias make it difficult to draw firm conclusions on the available evidence.
The absence of publication bias (unpublished trials showing no benefit of exercise over control) can never be proven. However, publication bias is less relevant where the published studies show no effect of treatment and would only be problematic if studies (or data on outcomes) demonstrating an effect of exercise versus control in either direction (positive or deleterious) were not published.
Potential biases in the review process
Our search was comprehensive but we acknowledge that it is very likely that we may have missed some, probably small, trials, especially those published in other languages or as abstracts only. We adopted systematic processes throughout, and now assess risk of bias rather than methodological quality. This includes an assessment of selective reporting bias, which we consider is highly important in this area given the great variety of outcome measures. Although we did not explore the effects of missing data, we have presented a table for each comparison that summarises the extent of the missing data for each of the primary balance measures and we have been cautious in our interpretation of the data that were available for presentation in the analyses.
Agreements and disagreements with other studies or reviews
The objective of this review was to present the best evidence for effectiveness of exercise interventions designed to improve balance in older people living in the community or in institutional care. The general direction of findings presented (a positive effect of exercise on balance immediately post intervention, but typically not maintained on cessation of the intervention) is in keeping with those of other related systematic reviews: 'Progressive resistance strength training for improving physical function in older adults' (Liu 2009), 'Interventions for preventing falls in older people living in the community' (Gillespie 2009) and 'Interventions for preventing falls in older people in nursing care facilities and hospitals' (Cameron 2010) where the positive effects of exercise on balance were secondary findings. The same is also true of the recent systematic review on biofeedback to improve balance (Zijlstra 2010).
Authors' conclusions
Implications for practice.
A cautious interpretation of the available evidence is necessary, particularly given the extent of the missing data for primary outcomes. From the data available for presentation in the analyses, this systematic review provides some evidence that some exercise types compared with usual activity are moderately effective, at least immediately post intervention, in improving clinical balance outcomes in older people. These data show that exercise programmes involving gait, balance, co‐ordination and functional exercises; muscle strengthening exercise; 3D exercise types and multiple exercise types, appear to improve at least some 'indirect' quantifiable measures of balance such as the Timed Up and Go (TUG) test, single leg stance, walking speed and a global subjective measure of balance, the Berg Balance Score. Although the duration and frequency of these exercise programmes vary, in general, the effective programmes ran three times a week for a duration of three months and involved standing, challenging balance exercises. Where studies provided data following cessation of exercise, there was no evidence of differences between exercise and control groups, probably indicating that the positive effects on balance are only evident when engaged in programmes.
It is, however, essential to realise that the above evidence is not robust, especially because of the large amounts of missing data for many outcomes and the inadequate methodology of many, often small, trials that increased the risk of their results being biased. It is plausible that both these issues would result in exaggerated effect sizes. Additionally, the failure across the included studies to apply a core set of standardised outcome measures to determine balance ability restricts the capacity to compare or pool different studies from which firm conclusions regarding efficacy can be made. The incomplete outcome reporting compounds this issue. The lack of longer term follow‐up of outcomes makes it difficult to determine any lasting effects, although we anticipate that a component for home exercises post intervention would anyway be required.
There is insufficient evidence to draw conclusions on the effects on clinical balance outcomes of general physical activity, such as walking and cycling, and exercise involving computerised balance programmes or vibration plates.
When reported, adherence to the different exercise programmes varied from 25% to 100%. There was only limited evidence available to assess safety. The few adverse events that were reported ranged from mild discomfort to musculoskeletal pain but it was unclear whether these related to the exercise or control groups or to the total sample. Only one study reported a fall that occurred during the exercise programme.
Implications for research.
Most of the existing studies in this area were found to be poorly reported and lacking sufficient and useable data for the purposes of secondary analyses and summary. Future work in this field needs to conform to the standards laid out in the revised CONSORT statement (Schulz 2010). Future trialists need to consider their choice of outcome measurement so as to ensure clinical relevance. Whilst direct measures of balance such as force platform measures may be useful, the value of indirect outcome measures, that are more functionally relevant to patients, should not be underestimated (e.g. functional activities such as getting up from being seated and walking (TUG)). Furthermore, particular consideration should be given to the use of valid and reliable methods for collecting adverse event data. Finally, trials of longer duration are required to establish the necessary length of treatment and longer term outcomes, and trials involving a diverse range of ethnic and cultural groups would ensure greater generalisability of findings.
The benefits of exercise interventions on balance may be relatively small, so the sample sizes reported need to have adequate power to answer the research question, allowing the detection of clinically significant differences between groups. Reporting should include the method of randomisation and treatment allocation concealment and an intention‐to‐treat analysis performed. The history and reasons for drop‐outs and exclusions (including appropriate adverse event data) throughout the trial should be ascertained and reported, so that factors affecting exercise adherence can be further explored. Ideally, rather than focusing on immediately post intervention, studies should include long‐term follow‐up participants (e.g. for at least one year).
To enable comparison and pooling of the results of randomised controlled trials, we suggest that future studies report means with standard deviations for continuous measures or number of events and total numbers analysed for dichotomous measures. We recommend that a consensus set of outcome measures for balance is a vital future need.
Feedback
Amendments to one study, 7 February 2012
Summary
We are pleased that our study, the Frail Older People Activity and Nutrition Study (the FOPANU Study), was included in the updated version of this review, published in Issue 11, 2011. Unfortunately, we have found significant errors in the review concerning the FOPANU Study which we would like to inform you about:
1. Incorrect reference. In the review Rosendahl et al Aging Clin Exp Res 2008; 20:67‐75 is used, but this paper does not include any result on balance. Instead Rosendahl et al Aust J Physiother 2006; 52:105‐13 should be used.
2. The results on Berg Balance Scale in the Analysis 8.10 (page 254) are not correct and seem to be taken from another study.
3. The results on walking speed (see Table 2 in Rosendahl et al Aust J Physiother 2006; 52:105‐13) are not included, although it is a primary outcome for the review (page 6).
4. The statement on page 123 that adverse effects are not reported is incorrect. Adverse events are reported in Rosendahl et al Aust J Physiother 2006; 52:105‐13 (see page 109). This paper also includes a reference to a paper focusing on the applicability of the program (Littbrand et al Phys Ther 2006; 86:489‐98), where the adverse events are presented in more detail.
5. In another Cochrane review “Rehabilitation for older people in long‐term care” our study reached the highest level of trial quality. In the present Cochrane review the trial quality was assessed lower, but the assessment reported on page 123‐124 includes incorrect decisions.
Assessors were blinded (see page 107 in Rosendahl et al Aust J Physiother 2006; 52:105‐13), but the review reports “Insufficient information to permit judgement of yes or no”.
Clustering was adjusted for in additional analyses (see page 107 in Rosendahl et al Aust J Physiother 2006; 52:105‐13), but the review reports “Failure to adjust for clustering”.
Follow‐up data are presented (see Table 2 in Rosendahl et al Aust J Physiother 2006; 52:105‐13), but the review reports “Only immediately post intervention data, no follow‐up data reported”.
Furthermore, the review reports that there is insufficient information to permit judgement concerning the risk of bias for “Random sequence generation (selection bias)” and “Selective reporting (reporting bias)”. We would like to highlight that the randomisation procedure is reported on page 106 in Rosendahl et al Aust J Physiother 2006; 52:105‐13 and that the study protocol is published (ISRCTN31631302).
Reply
We thank Professor Rosendahl for his feedback. We have given consideration to this and our responses to each point are detailed below.
1. Incorrect reference. In the review Rosendahl et al Aging Clin Exp Res 2008; 20:67‐75 is used, but this paper does not include any result on balance. Instead Rosendahl et al Aust J Physiother 2006; 52:105‐13 should be used.
We confirm that the Rosendahl 2006 paper referred to in the above was not included. In our original search undertaken for the first version (2007) of our review, this paper was excluded in an earlier round of scrutiny. This may have been due to the title of the paper 'High‐intensity functional exercise programme and protein enriched energy supplement for older persons dependent in activities of daily living: an RCT'.
Thus in our review update (2011), we reported solely on information presented in Rosendahl 2008 and our responses relate to the reporting of the trial in this paper.
2. The results on Berg Balance Scale in the Analysis 8.10 (page 254) are not correct and seem to be taken from another study.
These data are reported correctly in our analyses as Rosendahl 2008 states "balance improvement did not significantly differ between the exercise and control groups (mean± SD 7.2±4.2 vs 6.5± 3.5, p=0.4)" on page 73.
3. The results on walking speed (see Table 2 in Rosendahl et al Aust J Physiother 2006; 52:105‐13) are not included, although it is a primary outcome for the review (page 6).
No data for walking speed are reported in Rosendahl 2008.
4. The statement on page 123 that adverse effects are not reported is incorrect. Adverse events are reported in Rosendahl et al Aust J Physiother 2006; 52:105‐13 (see page 109). This paper also includes a reference to a paper focusing on the applicability of the program (Littbrand et al Phys Ther 2006; 86:489‐98), where the adverse events are presented in more detail.
We agree that in Rosendahl 2008 data are referred to on falls: "In order to observe a possible adverse event of the intervention, falls were also recorded." and "during the 3 month intervention 39 participants in the exercise group and 45 in the control group sustained a fall. Falls per participant ranged from 0‐16." However these are pooled data (see below).
5. In another Cochrane review 'Rehabilitation for older people in long‐term care' our study reached the highest level of trial quality. In the present Cochrane review the trial quality was assessed lower, but the assessment reported on page 123‐124 includes incorrect decisions.
Assessors were blinded (see page 107 in Rosendahl et al Aust J Physiother 2006; 52:105‐13), but the review reports 'Insufficient information to permit judgement of yes or no'.
Rosendahl 2008 makes no reference to 'blinding' of participants or assessors.
Clustering was adjusted for in additional analyses (see page 107 in Rosendahl et al Aust J Physiother 2006; 52:105‐13), but the review reports 'Failure to adjust for clustering'.
Rosendahl 2008 reported "The results of the outcome analyses are presented without adjustments for randomisation in clusters" on page 71.
Follow‐up data are presented (see Table 2 in Rosendahl et al Aust J Physiother 2006; 52:105‐13), but the review reports 'Only immediately post intervention data, no follow‐up data reported'.
Our assessment of risk of bias was correct as the only data for outcome measures of interest to our review were reported immediately post intervention. Rosendahl 2008 states "Amongst participants who responded during the 3 month intervention period the extent of balance improvement did not significantly differ between the exercise and control groups (mean± SD 7.2±4.2 vs 6.5± 3.5, p=0.4)" on page 73.
Furthermore, the review reports that there is insufficient information to permit judgement concerning the risk of bias for 'Random sequence generation (selection bias)' and 'Selective reporting (reporting bias)'. We would like to highlight that the randomisation procedure is reported on page 106 in Rosendahl et al Aust J Physiother 2006; 52:105‐13 and that the study protocol is published (ISRCTN31631302).
We note that this trial was retrospectively registered as ISRCTN31631302 on 09/07/2009.
Professor Rosendahl’s main concern is that we have used Rosendahl 2008 and not Rosendahl 2006 as the source of our data. On comparing these papers and the trial registration information, it is clear that these all report the same study. However, Rosendahl 2008 describes random allocation of 191 participants into two groups (exercise n = 91 and control n = 100), whereas Rosendahl 2006 describes random allocation of 191 participants into four groups (exercise plus protein n = 46, exercise plus placebo n = 46, control plus protein n = 50 and control plus placebo n = 50). Thus, Rosendahl 2008 reports pooled data for participants in groups receiving exercise plus protein with those receiving exercise plus placebo, and pooled data for participants in groups receiving control plus protein with control plus placebo.
We have now amended our review (published Issue 5, 2012) using Rosendahl 2006 as the primary source for the FOPANU Study.
Contributors
Comment from Erik Rosendahl, Sweden Reply from Tracey Howe, Corresponding Author, with advice from Bill Gillespie, Feedback Editor, Cochrane Bone, Joint and Muscle Trauma Group.
What's new
| Date | Event | Description |
|---|---|---|
| 29 March 2012 | Feedback has been incorporated | Response to feedback relating to Rosendahl 2008 (now Rosendahl 2006). Data from Rosendahl 2006 paper as the primary source entered and the review amended accordingly. There was no change to the conclusions. |
History
Protocol first published: Issue 4, 2004 Review first published: Issue 4, 2007
| Date | Event | Description |
|---|---|---|
| 13 September 2011 | New citation required and conclusions have changed | 1. There has been a change in authorship. 2. The conclusions have changed. As well as reflecting the inclusion of more evidence, the changed conclusions reflect the change in the primary outcomes, in the categorisation of the exercise interventions, and consideration of the potential consequences of the missing data. |
| 13 September 2011 | New search has been performed | For this update, published in Issue 11, 2011, the following changes were made: 1. The search was updated to January 2011 and 62 new trials were included; 2. The methodology has been updated to include the reclassification of outcome measures and exercise categories and the reclassification of some interventions from original studies. New comparisons are included; 3. Risk of bias is now assessed; 4. All analyses are now based on the new categories of outcome measures and exercise interventions; 5. The conclusions have changed. |
| 7 July 2008 | Amended | Converted to new review format. |
Acknowledgements
We would like to thank Helen Handoll, Lindsey Elstub, Peter Herbison, Catherine Sherrington and Janet Wale for critical comments on this update, Jon Godwin for methodological and statistical advice and Ogechi Ernest‐Amaziro for retrieval of papers.
In addition, we would like to thank those who made a contribution to the previously published version of this review; Pauline Banks, Alison Jackson and Val Blair who screened search results, appraised quality and extracted data from papers and commented on drafts. We would like to thank Lesley Gillespie for her valuable assistance with the search strategy, Joanne Elliott, Lindsey Elstub, Bill Gillespie, Peter Herbison, Vicki Livingstone, Rajan Madhok, Janet Wale and Wiebren Zijlstra for critical comments and the stimulating discussions that resulted from these, Mark Waters for input into the protocol, Sallie Lamb for assistance with the taxonomy of exercise interventions, Philip Rowe and Danny Rafferty for advice on outcome measures, Daniel Soule for drafting the original plain language summary and Jayne Elms who co‐ordinated data collection, searching and retrieval of papers and additional information, entered data into RevMan and commented on drafts and Pam Dawson who screened search results, appraised quality and extracted data from papers.
Appendices
Appendix 1. Search strategies
MEDLINE (Ovid Web) (levels 1 and 2)
1 exp Aged/ not Adolescent/ 2 (parkinson$ or stroke$1 or multiple sclerosis or amput$ or meniere$ or Alzheimer$ or dementia).ti. 3 Exercise Movement Techniques/ or Dance Therapy/ or Exercise/ or Exercise Therapy/ or Tai Ji/ or Walking/ or Yoga/ or "Biofeedback (Psychology)"/ 4 (exercis$ or training or biofeedback or Tai Chi).tw. 5 (balance adj3 (retraining or re‐training or reeducation or re‐education)).tw. 6 or/3‐5 7 Musculoskeletal Equilibrium/ or Posture/ 8 (balance or functional reach or sway).tw. 9 (postur$ adj3 (stability or instability)).tw. 10 posturograph$.tw. 11 (cent$3 adj (pressure or mass)).tw. 12 or/7‐11 13 and/1,6,12 14 13 not 2 15 Randomized controlled trial.pt. 16 Controlled clinical trial.pt. 17 Randomized Controlled Trials/ 18 Random Allocation/ 19 Double‐Blind Method/ 20 Single‐Blind Method/ 21 or/15‐20 22 Animals/ not Humans/ 23 21 not 22 24 clinical trial.pt. 25 exp Clinical Trials as topic/ 26 (clinic$ adj25 trial$).tw. 27 ((singl$ or doubl$ or trebl$ or tripl$) adj (mask$ or blind$)).tw. 28 Placebos/ 29 placebo$.tw. 30 random$.tw. 31 Research Design/ 32 (latin adj square).tw. 33 or/24‐32 34 33 not 22 35 34 not 23 36 and/14,23 37 and/14,35
MEDLINE (Ovid Web) (level 3)
1. *Aged/ or *"Aged, 80 and over"/ or *Frail elderly/ 2. (elderly or seniors or geriatric or frail).ti. 3. (older adj (adult or people or person$1)).ti. 4. or/1‐3 5. Exercise Movement Techniques/ or Dance Therapy/ or Exercise/ or Exercise Therapy/ or Tai Ji/ or Walking/ or Yoga/ or "Biofeedback (Psychology)"/ 6. (exercis$ or training or biofeedback or Tai Chi).tw. 7. (balance adj3 (retraining or re‐training or reeducation or re‐education)).tw. 8. or/5‐7 9. Musculoskeletal Equilibrium/ or Posture/ 10. (balance or functional reach or sway).tw. 11. (postur$ adj3 (stability or instability)).tw. 12. posturograph$.tw. 13. (cent$3 adj (pressure or mass)).tw. 14. or/9‐13 15. and/4,8,14 16 Comparative Study.pt 17 exp Evaluation Studies.pt 18 Follow‐Up Studies/ 19 Prospective Studies/ 20 (control$ or prospectiv$ or volunteer$).tw. 21 Cross‐Over Studies/ 22 Animals/ not Humans/ 23 or/16‐21 24 23 not 22 25 15 and24
The Cochrane Library (Wiley Online Library)
#1. AGED explode tree 1 (MeSH) #2. ADOLESCENT single term (MeSH) #3. (#1 and (not #2)) #4. (parkinson* or stroke* or (multiple next sclerosis) or amput* or meniere* or alzheimer* or dementia):ti #5. EXERCISE MOVEMENT TECHNIQUES single term (MeSH) #6. DANCE THERAPY single term (MeSH) #7. EXERCISE single term (MeSH) #8. EXERCISE THERAPY single term (MeSH) #9. TAI JI single term (MeSH) #10. YOGA single term (MeSH) #11. BIOFEEDBACK (PSYCHOLOGY) single term (MeSH) #12. (exercis* or training or biofeedback or (tai next chi)) #13. ((balance near retraining) or (balance near (re next training)) or (balance near reeducation) or (balance near (re next education))) #14. (#5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13) #15. POSTURE single term (MeSH) #16. (balance or (functional next reach) or sway) #17. ((postur* near stability) or (postur* near instability)) #18. posturograph* #19. ((cent* next pressure) or (cent* next mass)) #20. (#15 or #16 or #17 or #18 or #19) #21. (#3 and #14 and #20) #22. (#21 and not #4)
CINAHL (Ebsco)
1. (MH "Aged+") 2. (MH "Yoga") OR (MH "Tai Chi") 3. (MH "Exercise+") 4. (MH "Therapeutic Exercise+") 5. TI ( exercis* or training or Tai Chi ) or AB ( exercis* or training or Tai Chi ) 6. TX (balance N3 retrain*) or TX (balance N3 re‐train*) or TX (balance N3 reeducation) or TX (balance N3 re‐education) 7. S2 or S3 or S4 or S5 or S6 8. (MH "Balance, Postural") OR (MH "Posture") 9. TI ( balance or functional reach or sway or posturog* ) or AB ( balance or functional reach or sway or posturog* 10. TX (postur* N3 stability) or TX (postur* N3 instability) 11. TX (cent* N6 pressure) or TX (cent* N6 mass) 12. S8 or S9 or S10 or S11 13. S1 and S7 and S12 14. (MH "Clinical Trials+") 15. (MH "Comparative Studies") 16. (MH "Prospective Studies+") 17. (MH "Crossover Design") 18. (MH "Double‐Blind Studies") or (MH "Single‐Blind Studies") or (MH "Triple‐Blind Studies") 19. (MH "Placebos") 20. (MH "Random Assignment") 21. PT Clinical Trial 22. TI ( (clinical or controlled or comparative or placebo or prospective or randomised or randomized) and (trial or study) ) or AB ( (clinical or controlled or comparative or placebo or prospective or randomised or randomized) and (trial or study) ) 23. TI ( random* and (allocat* or allot* or assign* or basis* or divid* or order*) ) or AB ( random* and (allocat* or allot* or assign* or basis* or divid* or order*) ) 24. TI (singl* N1 blind*) or TI (doubl* N1 blind*) or TI (trebl* N1 blind*) or TI (tripl* N1 blind*) or TI (singl* N1 mask*) or TI (doubl* N1 mask*) or TI (trebl* N1 mask*) or TI (tripl* N1 mask*) or AB (singl* N1 blind*) or AB (doubl* N1 blind*) or AB (trebl* N1 blind*) or AB (tripl* N1 blind*) or AB (singl* N1 mask*) or AB (doubl* N1 mask*) or AB (trebl* N1 mask*) or AB (tripl* N1 mask*) 25. TI ( crossover or cross‐over or "cross over" ) or AB ( crossover or cross‐over or "cross over" ) 26. S14 or S15 or S16 or S17 or S18 or S19 or S20 or S21 or S22 or S23 or S24 or S25 27. S13 and S26
EMBASE (Ovid Web)
1. Aged/ not Adolescent/ 2. Parkinson Disease/ 3. Stroke/ 4. Multiple Sclerosis/ 5. Meniere Disease/ 6. Dementia/ or Senile Dementia/ 7. exp Amputation/ 8. or/2‐7 9. 1 not 8 10. exp Exercise/ 11. exp Kinesiotherapy/ 12. Training/ 13. Qigong/ or Qigong Therapy/ 14. (exercis$ or training or Tai Chi).tw. 15. (balance adj3 (retrain$ or re‐train$ or reeducat$ or re‐educat$)).tw. 16. or/10‐15 17. Body Equilibrium/ or Body Posture/ or Body Position/ 18. (balance or functional reach or sway or posturog$).tw. 19. (postur$ adj3 (stability or instability)).tw. 20. (cent$ adj (pressure or mass)).tw. 21. or/17‐20 22. and/9,16,21 23. exp Randomized Controlled trial/ 24. exp Double Blind Procedure/ 25. exp Single Blind Procedure/ 26. exp Crossover Procedure/ 27. Controlled Study/ 28. or/23‐27 29. ((clinical or controlled or comparative or placebo or prospective$ or randomi#ed) adj3 (trial or study)).tw. 30. (random$ adj7 (allocat$ or allot$ or assign$ or basis$ or divid$ or order$)).tw. 31. ((singl$ or doubl$ or trebl$ or tripl$) adj7 (blind$ or mask$)).tw. 32. (cross?over$ or (cross adj1 over$)).tw. 33. ((allocat$ or allot$ or assign$ or divid$) adj3 (condition$ or experiment$ or intervention$ or treatment$ or therap$ or control$ or group$)).tw. 34. or/29‐33 35. or/28,34 36. limit 35 to human 37. and/22,36
AMED (Ovid Web)
1. exp Aged/ 2. exp Exercise/ 3. exp Tai chi/ 4. exp Yoga/ 5. (exercis$ or training or Tai Chi).tw. 6. exp Exercise therapy/ 7. (balance adj3 (retrain$ or re‐train$ or reeducation or re‐education)).tw. 8. (balance or functional reach or sway or posturog$).tw. 9. (postur$ adj3 (stability or instability)).tw. 10. (cent$ adj3 (pressure or mass)).tw. 11. exp Kinematics/ 12. or/2‐7 13. or/8‐11 14. and/1,12‐13 15. Randomized controlled trial.pt. 16. Controlled clinical trial.pt. 17. Randomized Controlled Trials/ 18. Random Allocation/ 19. Double‐Blind Method/ 20. or/15‐19 21. Animals/ not Humans/ 22. 20 not 21 23. clinical trial.pt. 24. exp Clinical Trials/ 25. (clinic$ adj25 trial$).tw. 26. ((singl$ or doubl$ or trebl$ or tripl$) adj (mask$ or blind$)).tw. 27. Placebos/ 28. placebo$.tw. 29. random$.tw. 30. Research Design/ 31. (latin adj square).tw. 32. or/23‐31 33. 32 not 21 34. and/14,22 35. and/14,33 36. or/34‐35
PEDro
Abstract & Title: exercise and balance Therapy: no selection Body part: no selection Subdiscipline: gerontology Method: clinical trial When searching: match all search terms (AND)
OTSeeker
Keywords:balance Intervention:exercise/strength training Diagnosis/Subdiscipline:Gerontology ‐ General Method:Clinical Trial Options:Do a "fuzzy logic" search if precise search finds nothing
Appendix 2. Data table: Gait, balance, co‐ordination and functional tasks
| N | TUG | SLS(o) | SLS(c) | Gait | Berg | Other outcomes | |
| Avelar 2010 | 46 | M | M | M | |||
| Beling 2009 | 23 | 19 | 19 | 19 | A | ||
| Clemson 2010 | 34 | M | M | ||||
| Faber 2006 | 158 | M | M | ||||
| Gaub 2003 ** | 50 | M | M | M | |||
| Gine‐Garriga 2010 | 51 | M | M | M | M | ||
| Islam 2004 | 43 | A | |||||
| Johansson 1991 | 34 | 33 | 33 | 33 | A | ||
| Karinkanta 2007 | 74 | A | |||||
| McGarry 2001 | 22 | 22 | 22 | A | |||
| Reinsch 1992 | 107 | 33 | |||||
| Salminen 2009 | 591 | M | M | ||||
| Schilling 2009 | 19 | 19 | M | ||||
| Sihvonen 2004 | 28 | 27 | M | ||||
| Vrantsidis 2009 | 62 | 54 | 54 | A | |||
| Weerdesteyn 2006 | 58 | 101 | A | ||||
| Westlake 2007 | 44 | M | |||||
| Wolf 2001 | 94 | 77 | |||||
| Wolfson 1996 ** | 57 | 39 | 50 | A | |||
| Total participants randomised in trials with data in analyses (numbers of trials) | 114 (4) | 206 (4) | 33 (1) | 156 (4) | 145 (4) | ||
| Total participants randomised in trials without data in analyses (numbers of trials) | 329 (2) | 85 (2) | 0 (0) | 425 (4) | 687 (3) | ||
| Total participants randomised in trials measuring outcome (numbers of trials) | 1595 (19) | 443 (6) | 291 (6) | 33 (1) | 581 (7) | 832 (7) |
N = number of participants randomised in trials M = measured but no data in analyses A = other outcome measured with data available for analyses ** = trial examined more than one intervention TUG = timed up and go test SLS(o) = single leg stance eyes open SLS(c) = single leg stance eyes closed BBS = Berg Balance Score
Appendix 3. Data table: Strengthening exercise
| N | TUG | SLS(o) | SLS(c) | Gait | Berg | Other outcomes | |
| Baum 2003 | 20 | 19 | 20 | ||||
| Boshuizen 2005 | 73 | 33 | 33 | A | |||
| Buchner 1997a | 55 | 51 | 51 | A | |||
| Chandler 1998 | 100 | M | |||||
| Chang 2007 | 21 | M | M | ||||
| Gaub 2003 ** | 50 | M | M | M | |||
| Granacher 2009 | 40 | M | |||||
| Henwood 2006 | 67 | 40 | A | ||||
| Karinkanta 2007 ** | 74 | M | A | ||||
| Krebs 1998 | 132 | 120 | |||||
| Latham 2003 | 243 | M | M | M | |||
| Morris 1999 | 468 | M | |||||
| Rooks 1997a ** | 91 | 81 | 81 | M | A | ||
| Schlicht 2001 | 24 | 22 | 22 | ||||
| Skelton 1995 | 47 | 18 | 17 | 17 | 18 | A | |
| Skelton 1996 | 20 | 40 | A | ||||
| Taaffe 1999 | 46 | M | |||||
| Topp 1993 | 63 | M | M | M | M | ||
| Vogler 2009 ** | 120 | 114 | A | ||||
| Wolfson 1996 ** | 55 | 38 | 51 | A | |||
| Woo 2007 ** | 120 | M | M | ||||
| Total participants randomised in trials with data in analyses (numbers of trials) | 70 (3) | 187 (4) | 120 (3) | 489 (9) | 20 (1) | ||
| Total participants randomised in trials without data in analyses (numbers of trials) | 243 (1) | 264 (3) | 63 (1) | 545 (6) | 293 (2) | ||
| Total participants randomised in trials measuring outcome (numbers of trials) | 1929 (21) | 313 (4) | 451 (7) | 183 (4) | 1034 (15) | 313 (3) |
N = number of participants randomised in trials M = measured but no data in analyses A = other outcome measured with data available for analyses ** = trial examined more than one intervention TUG = timed up and go test SLS(o) = single leg stance eyes open SLS(c) = single leg stance eyes closed BBS = Berg Balance Score
Appendix 4. Data table: 3D (Tai Chi, Gi Gong, dance, yoga)
| N | TUG | SLS(o) | SLS(c) | Gait | Berg | Other outcomes | |
| Buchner 1997b ** | 56 | 52 | A | ||||
| Eyigor 2009 | 40 | 37 | 37 | ||||
| Faber 2006 | 162 | A | |||||
| Frye 2007 ** | 54 | 44 | |||||
| Hall 2009 | 22 | A | |||||
| Kim 2009a | 52 | A | |||||
| Logghe 2009 | 269 | 213 | |||||
| Shin 2009 | 60 | 48 | |||||
| Taylor‐Piliae 2010 ** | 93 | 93 | A | ||||
| Voukelatos 2007 | 702 | A | |||||
| Wallsten 2006 | 77 | M | |||||
| Wolf 1997 ** | 48 | A | |||||
| Woo 2007 ** | 120 | M | M | M | |||
| Yang 2007 | 59 | A | |||||
| Zhang 2006a | 49 | 47 | 47 | ||||
| Total participants randomised in trials with data in analyses (numbers of trials) | 44 (1) | 140 (2) | 48 (1) | 136 (3) | 250 (2) | ||
| Total participants randomised in trials without data in analyses (numbers of trials) | 77 (1) | 180 (1) | 180 (1) | ||||
| Total participants randomised in trials measuring outcome (numbers of trials) | 1863 (15) | 121 (2) | 320 (3) | 48 (1) | 315 (4) | 250 (2) |
N = number of participants randomised in trials M = measured but no data in analyses A = other outcome measured with data available for analyses ** = trial examined more than one intervention TUG = timed up and go test SLS(o) = single leg stance eyes open SLS(c) = single leg stance eyes closed BBS = Berg Balance Score
Appendix 5. Data table: General physical activity (walking)
| N | TUG | SLS(o) | SLS(c) | Gait | Berg | Other outcomes | |
| Buchner 1997b ** | 56 | 52 | A | ||||
| Gaub 2003 ** | 50 | M | M | M | |||
| Paillard 2004 | 21 | 21 | A | ||||
| Rooks 1997a ** | 91 | 69 | 69 | A | |||
| Schoenfelder 2000 | 16 | M | M | ||||
| Shimada 2004 | 32 | 26 | 26 | A | |||
| Yoo 2010 | 21 | 21 | A | ||||
| Total participants randomised in trials with data in analyses (numbers of trials) | 21 (1) | 95 (2) | 69 (1) | 99 (3) | |||
| Total participants randomised in trials without data in analyses (numbers of trials) | 66 (2) | 50 (1) | |||||
| Total participants randomised in trials measuring outcome (numbers of trials) | 287 (7) | 21 (1) | 95 (2) | 69 (1) | 165 (4) | 50 (1) |
N = number of participants randomised in trials M = measured but no data in analyses A = other outcome measured with data available for analyses ** = trial examined more than one intervention TUG = timed up and go test SLS(o) = single leg stance eyes open SLS(c) = single leg stance eyes closed BBs = Berg Balance Score
Appendix 6. Data table: General physical activity (cycling)
| N | TUG | SLS(o) | SLS(c) | Gait | Berg | Other outcomes | |
| Buchner 1997b ** | 54 | 51 | A | ||||
| Total participants randomised in trials with data in analyses (numbers of trials) | 51 (1) | ||||||
| Total participants randomised in trials without data in analyses (numbers of trials) | |||||||
| Total participants randomised in trials measuring outcome (numbers of trials) | 54 (1) | 51 (1) |
N = number of participants randomised in trials M = measured but no data in analyses A = other outcome measured with data available for analyses ** = trial examined more than one intervention TUG = timed up and go test SLS(o) = single leg stance eyes open SLS(c) = single leg stance eyes closed BBS = Berg Balance Score
Appendix 7. Data table: Computerized balance
| N | TUG | SLS(o) | SLS(c) | Gait | Berg | Other outcomes | |
| Hatzitaki 2009 (56 participants) | 56 | M | |||||
| Wolf 1997 (72 participants) ** | 48 | A | |||||
| Total participants randomised in trials with data in analyses (numbers of trials) | |||||||
| Total participants randomised in trials without data in analyses (numbers of trials) | |||||||
| Total participants randomised in trials measuring outcome (numbers of trials) | 104 (2) |
N = number of participants randomised in trials M = measured but no data in analyses A = other outcome measured with data available for analyses ** = trial examined more than one intervention TUG = timed up and go test SLS(o) = single leg stance eyes open SLS(c) = single leg stance eyes closed BBS = Berg Balance Score
Appendix 8. Data table: Vibration
| N | TUG | SLS(o) | SLS(c) | Gait | Berg | Other outcomes | |
| Bogaerts 2007 ** | 160 | A | |||||
| Cheung 2007 | 75 | A | |||||
| Furness 2009 | 75 | 37 | |||||
| Total participants randomised in trials with data in analyses (numbers of trials) | 37 (1) | ||||||
| Total participants randomised in trials without data in analyses (numbers of trials) | |||||||
| Total participants randomised in trials measuring outcome (numbers of trials) | 310 (3) | 37 (1) |
N = number of participants randomised in trials M = measured but no data in analyses A = other outcome measured with data available for analyses ** = trial examined more than one intervention TUG = timed up and go test SLS(o) = single leg stance eyes open SLS(c) = single leg stance eyes closed BBS = Berg Balance Score
Appendix 9. Data table: Multiple exercise types
| N | TUG | SLS(o) | SLS(c) | Gait | Berg | Other outcomes | |
| Arai 2007 | 171 | 136 | 138 | 137 | A | ||
| Baker 2007 | 38 | 38 | A | ||||
| Beyer 2007 | 53 | 53 | 53 | M | |||
| Bogaerts 2007 ** | 126 | A | |||||
| Brouwer 2003 | 38 | 34 | A | ||||
| Campbell 1997 | 233 | M | M | ||||
| Carvalho 2009 | 57 | 57 | |||||
| Chulvi‐Medrano 2009 | 28 | 28 | 28 | ||||
| Cress 1999 | 56 | 49 | A | ||||
| Crilly 1989 | 50 | A | |||||
| de Greef 2006 | 45 | 40 | M | A | |||
| Frye 2007 | 53 | 49 | |||||
| Gaub 2003 | 50 | M | M | ||||
| Hara 2007 | 44 | 44 | 44 | A | |||
| Iwamoto 2009 | 68 | 68 | 68 | 68 | A | ||
| Jessup 2003 | 18 | A | |||||
| Kamide 2009 | 57 | 50 | 50 | 50 | |||
| Karinkanta 2007 ** | 75 | M | A | ||||
| Lin 2007 | 100 | A | |||||
| Liu‐Ambrose 2008 | 74 | 52 | |||||
| Lord 1995 | 197 | A | |||||
| Lord 2003 | 461 | A | |||||
| Lord 2005 | 414 | A | |||||
| McMurdo 1993 | 49 | A | |||||
| MacRae 1994 | 80 | 59 | 59 | ||||
| Nelson 2004 | 72 | 70 | 70 | A | |||
| Park 2008 | 50 | M | M | A | |||
| Okumiya 1996 | 42 | 42 | A | ||||
| Ramirez Villada 2007 | 93 | M | |||||
| Ramsbottom 2004 | 22 | M | 21 | A | |||
| Rosendahl 2006 | 95 | 81 | 84 | ||||
| Rubenstein 2000 | 59 | 55 | |||||
| Sauvage 1992 | 14 | 14 | A | ||||
| Schoenfelder 2004 | 81 | 67 | A | ||||
| Sherrington 2008a | 173 | 159 | A | ||||
| Suzuki 2004 | 52 | 39 | 39 | 39 | A | ||
| Sykes 2004 | 40 | 27 | 27 | A | |||
| Toraman 2004 | 42 | 42 | |||||
| Taylor‐Piliae 2010 ** | 95 | 95 | M | ||||
| Vestergaard 2008 | 61 | A | |||||
| Vogler 2009 ** | 120 | 113 | A | ||||
| Wolfson 1996 ** | 55 | 38 | 53 | A | |||
| Worm 2001 | 46 | 39 | 44 | ||||
| Total participants randomised in trials with data in analyses (numbers of trials) | 635 (12) | 640 (10) | 176 (2) | 1051 (18) | 208 (4) | ||
| Total participants randomised in trials without data in analyses (numbers of trials) | 22 (1) | 50 (1) | 403 (5) | 50 (1) | |||
| Total participants randomised in trials measuring outcome (numbers of trials) | 3873 (43) | 657 (13) | 690 (11) | 176 (2) | 1454 (23) | 258 (5) |
N = number of participants randomised in trials M = measured but no data in analyses A = other outcome measured with data available for analyses ** = trial examined more than one intervention TUG = timed up and go test SLS(o) = single leg stance eyes open SLS(c) = single leg stance eyes closed BBS = Berg Balance Score
Data and analyses
Comparison 1. Gait, balance, co‐ordination, functional tasks exercise versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Timed Up & Go Test (s): lower values indicate better balance ability | 4 | 114 | Mean Difference (IV, Fixed, 95% CI) | ‐0.82 [‐1.56, ‐0.08] |
| 2 Single leg stance time eyes open (s): higher values indicate better balance ability | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Immediately post intervention | 4 | 206 | Mean Difference (IV, Fixed, 95% CI) | 3.13 [0.26, 6.01] |
| 2.2 Follow up @ 6 months post intervention | 1 | 37 | Mean Difference (IV, Fixed, 95% CI) | 3.50 [‐3.43, 10.43] |
| 3 Sensitivity analysis (cluster RCT removed): Single leg stance time eyes open (s): higher values indicate better balance ability | 3 | 173 | Mean Difference (IV, Fixed, 95% CI) | 2.48 [‐0.65, 5.61] |
| 4 Single leg stance time eyes closed (s): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Gait speed: higher values indicate better balance ability | 4 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Immediately post intervention | 4 | 156 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.43 [0.11, 0.75] |
| 5.2 Follow‐up at 6 months post intervention | 1 | 45 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.31 [‐0.28, 0.90] |
| 6 Berg Balance Scale (score out of 56) higher values indicate better balance ability | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Immediately post intervention | 4 | 145 | Mean Difference (IV, Fixed, 95% CI) | 3.48 [2.01, 4.95] |
| 6.2 Follow up at 4 weeks post intervention | 1 | 77 | Mean Difference (IV, Fixed, 95% CI) | 3.60 [‐1.96, 9.16] |
| 6.3 Follow up at 1 year post intervention | 1 | 49 | Mean Difference (IV, Fixed, 95% CI) | 0.67 [‐7.29, 8.63] |
| 7 Functional Reach Test: higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8 Figure of eight test: time over 10 metres (s): lower values indicates better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9 Walking on a beam (m): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10 4 Test Balance Scale: lower score indicates better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11 Mediolateral stability during stance (quiet and dynamic) eyes open: lower values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 12 AP stability during stance (quiet and dynamic) eyes open: lower values indicate better balance ability | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 13 Maxium excursion of limits of stability (LOS) test: higher values indicate better balance ability | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 13.1 Forward | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.2 Backward | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.3 Right | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.4 Left | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.5 composite score % | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Functional base of support during dynamic test (distance): higher values indicate greater balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 14.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 Follow‐up at 6 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 SOT composite score: higher scores indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16 Loss of balance during sensory organisation test (errors): less errors indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 Follow‐up at 6 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Physical performance score: higher score indicates better balance | 1 | 154 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.09 [‐0.41, 0.23] |
1.17. Analysis.

Comparison 1 Gait, balance, co‐ordination, functional tasks exercise versus control, Outcome 17 Physical performance score: higher score indicates better balance.
Comparison 2. Strengthening exercise versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Timed Up & Go Test (s): lower values indicate better balance ability | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Immediately post intervention | 3 | 71 | Mean Difference (IV, Fixed, 95% CI) | ‐4.30 [‐7.60, 1.00] |
| 2 Single leg stance time eyes open (s): higher values indicate better balance ability | 4 | 187 | Mean Difference (IV, Random, 95% CI) | 3.88 [‐0.52, 8.28] |
| 3 Single leg stance time eyes closed (s): higher values indicate better balance ability | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Immediately post intervention | 3 | 120 | Mean Difference (IV, Fixed, 95% CI) | 1.64 [0.97, 2.31] |
| 3.2 Follow up @ 6 months post intervention | 1 | 31 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐7.98, 6.18] |
| 4 Gait speed: higher values indicate better balance ability | 8 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Immediately post intervention | 8 | 375 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.25 [0.05, 0.46] |
| 4.2 Follow‐up @ 6 months post intervention | 1 | 42 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.24 [‐0.37, 0.85] |
| 5 Gait speed (fastest pace): higher values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6 Berg Balance Scale (score out of 56) higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7 Functional reach test (FRT) (cm): higher values indicate better balance | 3 | 98 | Mean Difference (IV, Fixed, 95% CI) | 3.27 [1.39, 5.15] |
| 8 6m backward walk (s) lower value indicates better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9 Figure of eight running time over 10 metres (s): lower values indicates better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10 Tandem walk over 10 feet (s): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11 Tandem stance (s): higher values indicate better balance ability | 3 | 165 | Std. Mean Difference (IV, Random, 95% CI) | 0.24 [‐0.34, 0.82] |
| 12 Balance beam: post‐pre change scores (s): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 12.1 Wide beam | 1 | 51 | Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.51, 0.31] |
| 12.2 Narrow beam | 1 | 51 | Mean Difference (IV, Fixed, 95% CI) | 0.5 [‐0.14, 1.14] |
| 13 Tilt board (s) post‐pre change scores: higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 13.1 Omnidirectional tilt board (s) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.2 AP tilt board (s) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Functional base of support during dynamic test (distance): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 14.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 Follow‐up @ 6 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Sway (mm) during dynamic test: lower values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15.1 Floor, eyes open (immediately post intervention) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.2 Floor, eyes closed (immediately post intervention) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.3 Foam, eyes open (immediately post intervention) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.4 Foam, eyes closed (immediately post intervention) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Loss of balance during sensory organisation test (errors): less errors indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 Follow‐up @ 6 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Co‐ordinated stability (errors): less errors indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 18 Maximal balance range (cm) during dynamic test: higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
2.5. Analysis.
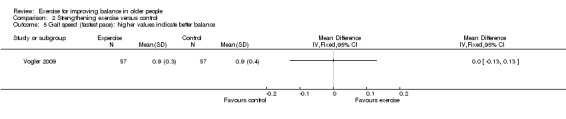
Comparison 2 Strengthening exercise versus control, Outcome 5 Gait speed (fastest pace): higher values indicate better balance.
Comparison 3. 3D (Tai Chi, Gi Gong, dance, yoga) versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Timed Up & Go Test (s): lower values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Single leg stance time eyes open (s): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Single leg stance time eyes open (s) change score: higher value indicates better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Single leg stance time eyes closed (s): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Gait speed: higher values indicate better balance ability | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Immediately post intervention | 3 | 136 | Std. Mean Difference (IV, Random, 95% CI) | 0.39 [‐0.28, 1.06] |
| 5.2 Follow‐up at 3 months post intervention | 1 | 48 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.48, 0.68] |
| 6 Berg Balance Scale (score out of 56) higher values indicate better balance ability | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Immediately post intervention | 2 | 250 | Mean Difference (IV, Fixed, 95% CI) | 1.06 [0.37, 1.76] |
| 6.2 Follow up at 9 months post intervention | 1 | 202 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐1.21, 1.61] |
| 7 Functional Reach Test change scores (cm): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8 Omnidirectional tilt board post‐pre change scores (s): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Follow‐up @ 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 AP stability during stance on a mat eyes open (mm) lower values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10 Reaction time (ms) low values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11 Physical performance score: higher score indicates better balance | 2 | 189 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.06 [‐0.34, 0.23] |
| 12 Narrow balance beam post‐pre change scores (m/s): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 12.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Wide balance beam post‐pre change scores (m/s): lower values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 13.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 A‐P displacement during obstacle course (cm): higher scores indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15 Leaning balance (mm) higher values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16 SOT: higher values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16.1 Eyes open | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 Eyes closed | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 M‐L displacement during obstacle course (cm): higher scores indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 18 Base of support (cm2) higher values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 19 Angular radius narrow stance eyes closed post‐pre change scores (mm): lower values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 19.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 AP stability during stance (quiet and dynamic) eyes open: lower values indicate better balance ability | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 20.1 Immediately post intervention | 3 | 614 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.08 [‐0.23, 0.08] |
| 20.2 Follow‐up at 3 months post intervention | 1 | 48 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.17 [‐0.40, 0.75] |
| 20.3 Follow‐up at 4 months post intervention | 1 | 35 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.15 [‐0.82, 0.52] |
| 21 Mediolateral stability during stance (quiet and dynamic) eyes open: lower values indicate better balance | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 21.1 Immediately post intervention | 2 | 565 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.15, 0.18] |
| 21.2 Follow‐up at 4 months post intervention | 1 | 38 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐0.34, 0.94] |
| 22 AP stability during quiet stance eyes closed: lower values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 22.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 22.2 Follow up at 4 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23 Mediolateral stability during quiet stance eyes closed: lower values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 23.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.2 Follow up at 4 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 24 Area during narrow stance eyes closed post‐pre change scores (mm2/s): lower values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 24.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 24.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 25 Area during narrow stance eyes open post‐pre change scores (mm2/s): lower values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 25.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 25.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 26 Angular radius narrow stance eyes open post‐pre change scores (mm): lower values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 26.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 26.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 4. General physical activity (walking) versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Timed Up & Go Test (s): lower values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Single leg stance time eyes open (s): Higher values indicate better balance ability | 2 | 95 | Mean Difference (IV, Fixed, 95% CI) | 1.96 [‐0.30, 4.22] |
| 3 Single leg stance time eyes closed (s): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Self paced gait velocity: higher values indicate better balance ability | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Immediately post intervention | 3 | 99 | Std. Mean Difference (IV, Random, 95% CI) | 0.67 [‐0.40, 1.74] |
| 4.2 Follow‐up at 3 months post intervention | 1 | 51 | Std. Mean Difference (IV, Random, 95% CI) | 0.44 [‐0.12, 1.00] |
| 5 Functional Reach Test (cm): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6 Tandem stance (s): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7 Tandem walk over 10 feet (s): lower values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8 Narrow balance beam post‐pre change scores (m/s): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Wide balance beam post‐pre change scores (m/s): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 AP tilt board post‐pre change score (s): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Area during narrow stance eyes closed post‐pre change scores (mm2/s): lower values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Omnidirectional tilt board post‐pre change scores (s): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 12.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Angular radius narrow stance eyes open post‐pre change scores (mm): lower values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 13.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Stability score during static test: higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 14.1 Floor, eyes open (immediately post intervention) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 Floor, eyes closed (immediately post intervention) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.3 Foam, eyes open (immediately post intervention) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.4 Foam, eyes closed (immediately post intervention) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Area during narrow stance eyes open post‐pre change scores (mm2/s): lower values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Dynamic balance lateral axis (degrees): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16.1 Average position (degrees) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 Amplitude (degrees) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Angular radius narrow stance eyes closed post‐pre change scores (mm): lower values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 17.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 5. General physical activity (cycling) versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Self paced gait velocity post‐pre change scores (m/min): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Narrow balance beam post‐pre change scores (m/s): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Wide balance beam post‐pre change scores (m/s): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Angular radius narrow stance eyes closed post‐pre change scores (mm): lower values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 AP tilt board post‐pre change score (s): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Omnidirectional tilt board post‐pre change scores (s): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Angular radius narrow stance eyes open post‐pre change scores (mm): lower values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Area narrow stance eyes closed post‐pre change scores (mm2/s): lower values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Area during narrow stance eyes open post‐pre change scores (mm2/s): lower values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 6. Computerized balance versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 AP stability during stance (quiet and dynamic) eyes open: lower values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Follow‐up at 4 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Mediolateral stability during stance (quiet and dynamic) eyes open: lower values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Follow‐up at 4 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 AP stability during quiet stance eyes closed: lower values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Follow‐up at 4 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Mediolateral stability during quiet stance eyes closed: lower values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Follow‐up at 4 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 7. Vibration versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Timed Up & Go Test (s): lower values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Functional reach test (% change): higher values indicates better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Directional control (% change): higher values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Maxium excursion of limits of stability (LOS) test:(% change) higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Movement velocity (% change): higher values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6 Endpoint excursion (% change): higher values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7 Reaction Time (% change): lower values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8 Equilibrium scores (%) of the SOT test: higher values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.1 Eyes open normal support surface | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Eyes closed normal support surface | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
7.2. Analysis.
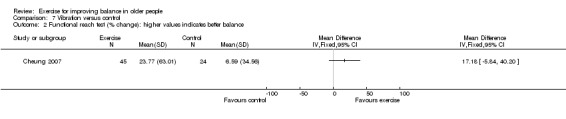
Comparison 7 Vibration versus control, Outcome 2 Functional reach test (% change): higher values indicates better balance.
Comparison 8. Multiple exercise types versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Timed Up & Go Test (s): lower values indicate better balance ability | 12 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Immediately post intervention | 12 | 635 | Mean Difference (IV, Random, 95% CI) | ‐1.63 [‐2.28, ‐0.98] |
| 1.2 3 months follow‐up | 1 | 57 | Mean Difference (IV, Random, 95% CI) | ‐1.10 [‐1.65, ‐0.55] |
| 2 Single leg stance time eyes open (s) change score: higher value indicates better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Single leg stance time eyes open (s): higher values indicate better balance ability | 9 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Immediately post intervention | 9 | 545 | Mean Difference (IV, Random, 95% CI) | 5.03 [1.19, 8.87] |
| 3.2 Follow up at 6 months post intervention | 1 | 33 | Mean Difference (IV, Random, 95% CI) | 2.80 [‐4.73, 10.33] |
| 4 Sensitivity analysis (cluster RCT removed) Single leg stance time eyes open (s): higher values indicate better balance ability | 8 | 486 | Mean Difference (IV, Random, 95% CI) | 5.80 [1.54, 10.06] |
| 5 Single leg stance time eyes closed (s): higher values indicate better balance ability | 2 | 176 | Mean Difference (IV, Fixed, 95% CI) | 1.60 [‐0.01, 3.20] |
| 6 Gait speed: higher values indicate better balance ability | 15 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Immediately post intervention | 15 | 818 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.04 [‐0.10, 0.17] |
| 6.2 Follow‐up at 6 months post intervention | 1 | 50 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.37 [‐0.19, 0.93] |
| 6.3 Follow‐up at 3 months post intervention | 1 | 58 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.11 [‐0.63, 0.40] |
| 6.4 Follow‐up at 6 weeks post intervention | 1 | 30 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐0.42, 1.03] |
| 7 Gait speed (change score) higher values indicate better balance | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1 self paced immediately post intervention | 2 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 self paced 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 maximum pace immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.4 maximum pace 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Gait speed (fastest pace): higher values indicate better balance | 2 | 163 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.31, 0.31] |
| 9 Berg Balance Scale (score out of 56) higher values indicate better balance ability | 2 | 80 | Mean Difference (IV, Fixed, 95% CI) | 1.84 [0.71, 2.97] |
| 10 Berg Balance Scale (change score) higher values indicate better balance ability | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 immediately post intervention | 2 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Functional Reach Test (cm): higher values indicate better balance ability | 8 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 11.1 Immediately post intervention | 7 | 350 | Mean Difference (IV, Random, 95% CI) | 5.77 [2.70, 8.84] |
| 11.2 2 months post intervention | 1 | 80 | Mean Difference (IV, Random, 95% CI) | 3.9 [0.70, 7.10] |
| 11.3 4 months post intervention | 1 | 79 | Mean Difference (IV, Random, 95% CI) | 3.20 [‐0.13, 6.53] |
| 12 Functional Reach Test (FRT) (cm) pre‐post change scores: lower values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 13 Tandem walk (s): lower values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 14 Tandem stance time (s): higher values indicate better balance ability | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 14.1 Immediately post intervention | 3 | 294 | Mean Difference (IV, Fixed, 95% CI) | 2.82 [1.28, 4.36] |
| 14.2 Follow‐up at 3 months post intervention | 1 | 58 | Mean Difference (IV, Fixed, 95% CI) | 1.20 [‐0.64, 3.04] |
| 15 Tandem walk (number of steps): higher values indicate better balance ability | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16 Semitandem stance time (s): higher values indicate better balance ability | 3 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16.1 Immediately post intervention | 2 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 Follow‐up at 2 weeks post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.3 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Figure of eight time (s): lower values indicates better balance | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 17.1 immediately post intervention | 2 | 113 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.41 [‐0.79, ‐0.04] |
| 18 Balance beam: post‐pre change scores (s): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 18.1 Wide beam | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 Equilibrium scores (%) of the SOT test: higher values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 19.1 Eyes open normal support surface | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.2 Eyes closed normal support surface | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 Maximal balance range (cm) during dynamic test: higher values indicate better balance ability | 3 | 706 | Mean Difference (IV, Random, 95% CI) | 1.26 [‐0.54, 3.07] |
| 21 Total distance travelled by COP during quiet stance (mm): lower values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 21.1 Eyes open | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 21.2 Eyes closed | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 22 Dynamic Balance score: lower values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 23 Sway (mm) during dynamic test: lower values indicate better balance ability | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 23.1 Floor, eyes open (immediately post intervention) | 4 | 1007 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.33, 0.18] |
| 23.2 Floor, eyes closed (immediately post intervention) | 4 | 1007 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.24, 0.01] |
| 23.3 Foam, eyes open (immediately post intervention) | 4 | 1007 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.50, 0.15] |
| 23.4 Foam, eyes closed (immediately post intervention) | 4 | 1007 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.26, 0.07] |
| 24 Static Balance Index: higher values indicate better balance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 25 Postural sway double stance (post‐pre change scores): lower values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 25.1 Eyes open | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 25.2 Eyes closed | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 26 Parallel stance time (s): higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 26.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 26.2 Follow‐up at 3 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 27 AP stability during quiet stance eyes closed: lower values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 28 Mediolateral stability during quiet stance eyes closed: lower values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 29 Functional base of support (distance) during dynamic test: higher values indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 29.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 29.2 Follow‐up at 6 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 30 Mediolateral stability during stance (quiet and dynamic) eyes open: lower values indicate better balance | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 30.1 Immediately post intervention | 2 | 81 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐1.29, 0.62] |
| 30.2 Follow‐up at 6 weeks post intervention | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.68 [‐1.42, 0.06] |
| 31 Loss of balance during sensory organisation test (errors): less errors indicate better balance ability | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 31.1 Immediately post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 31.2 Follow‐up at 6 months post intervention | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 32 Body sway (cm): lower values indicate better balance ability | 4 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 33 Co‐ordinated stability (errors): less errors indicate better balance ability | 4 | 940 | Mean Difference (IV, Random, 95% CI) | ‐1.88 [‐4.06, 0.30] |
| 34 AP stability during stance (quiet and dynamic) eyes open: lower values indicate better balance ability | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 34.1 Immediately post intervention | 2 | 81 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐1.19, 0.20] |
| 34.2 Follow‐up at 6 weeks post intervention | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.63 [‐1.37, 0.10] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Arai 2007.
| Methods | Type of study: RCT single‐blinded | |
| Participants | Number of participants randomised: 171 Losses: 34 (14 intervention, 20 control; (12 men, 22 women) Age: mean (SD) 74.1 for both groups. Exercise 73.9 (5.0) control 74.4 (6.2) Sex: women and men (N = not reported). Residential status of participants: community dwelling Health status as defined by authors: healthy Setting: Japan. Inclusion: Age 65 and older; community dwelling; ambulatory Exclusion: cerebrovascular and cardiovascular accident in last 6 months; liver disease; diabetes; high BP; heart disease; depression; restriction of activity on the advice of the GP |
|
| Interventions | EXERCISE GROUP (MULTIPLE) (n = 86): strengthening exercises (high intensity >70% 1 RM (repetition maximum)), highly challenging balance exercises, flexibility; daily functions CONTROL GROUP (n = 85): health education Duration and intensity: 3 months of 2 x 1.5 hour supervised classes per week. Supervisor: fitness staff. Supervision: group exercise classes 1:10 staff:participant Setting: university gym | |
| Outcomes | Timed Up and Go (s) One Legged Stand Time (OLST) eyes open and closed (s) Functional Reach (cm) Compliance/adherence:There was a difference in completers versus drop outs in knee extension strength Adverse events: No adverse events reported. |
|
| Notes | The Education Group met 2 x per month and had lectures on the benefits of exercise, but no diaries of activity or reporting on change in activity as a result of education | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis; knee extension strength different in completers versus drop outs |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Reported |
| Were the treatment and control group comparable at entry? | Unclear risk | Insufficient information to permit judgement |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
Avelar 2010.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 46 Losses: 2 aquatic (AG), 1 non aquatic (NAG) and 7 controls (CG) Age:mean age was 69 years (SD = 5.6; range 60 to 80) in the NAG, 68 years (SD = 5.7; range 62 to 78) in the AG and 71 years (SD = 3.9; range 65 to 78) in the CG Sex: women %: AG 36%; NAG 83%; CG 70% Health status as defined by authors:healthy Residential status of participants:community dwelling Setting: Brazil Inclusion:60 years of age or older, and able to perform the Get Up and Go Test Exclusion:undergoing physical therapy treatments; respiratory diseases or heart or metabolic diseases; cognitive deficit according to the Mini‐Mental State Examination (MMSE) 20; contagious skin abnormalities; using lower limb prostheses; use of drugs or medicines that might interfere with balance (nicotine, caffeine, alcohol, sedatives and tranquillizers); and no anal or vesical sphincter control. |
|
| Interventions | EXERCISE GROUP therapeutic pool intervention (GBFT) (n = 14): muscle endurance training, 4 sets of 20 reps in water for lower limb muscles with warm up and cool down. EXERCISE GROUP non‐aquatic intervention (GBFT) (n = 15): muscle endurance training, 4 sets of 20 reps on land for lower limb muscles with warm up and cool down. CONTROL GROUP (n = 17): usual activity, weekly telephone call Duration and intensity: twice a week for six weeks Supervisor: not stated Supervision: group Setting: pool and physical therapy gym |
|
| Outcomes | Berg Balance Scale (0 to 56 points) Tandem gait (number of steps) Gait speed (m/s) Compliance/adherence: not reported Adverse events: No adverse events reported. |
|
| Notes | Data not reported appropriately for analysis purposes. Data expressed graphically as medians | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation mentioned but Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Losses not accounted for, only those who completed |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Appraisers had no access to the allocation of the volunteers to the groups |
| Were the treatment and control group comparable at entry? | High risk | No significant age difference or outcome variables between the groups before the intervention. The proportion of male subjects was significantly larger in the AG, comprising 64% (P < 0.05), whereas the NAG and CG consisted mainly of women individuals (respectively, 83% and 70%). The AG and CG reported greater incidence of falls; however, there was no statistically significant difference among the groups (P > 0.05). |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data at 6 weeks, no follow‐up data reported. |
Baker 2007.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 38 (20 in intervention and 18 in control) Losses: 6 (2 drop outs from control and 4 intervention did not complete training) Age:76.6 (6.1) Sex: 14 men and 24 women Health status as defined by authors: not reported but healthy according to criteria Residential status of participants: residential village Setting:retirement village, USA Inclusion:age 60 or over; resident in retirement village, willing to be randomised Exclusion: acute or terminal illness, unstable metabolic or cardiovascular disease, contraindications to planned exercise, inability to commit to 10 week exercise programme. |
|
| Interventions | EXERCISE GROUP: (MULTIPLE) (n = 20): strength, endurance and balance components. Aerobic 2 days/week, balance 1 day week, strength training 3 times per week. Strength: 2 x 8 reps of knee flex, knee ext, hip flex and ext, hip abduction, chest press, seated row, lat pull down (80% of 1 RM (repetition maximum) ) adjusted over training period. Aerobic: 20 mins recumbent stepper or cycle ergometer. Balance: Static exs (single leg stand, side to side weight shift, forward backward weight shift), Dynamic exs (A‐P and lateral stepping over objects, 20 ft tandem walk, heel walk, toe walk). 8 exs performed in sequence twice. CONTROL GROUP: (n = 18): No exercise Duration and intensity: 3 to 4 hours a week for 10 weeks in 3 sessions a week Supervisor: experienced trainer Supervision: 1 to 5 participants in a group Setting: gymnasium in retirement village |
|
| Outcomes | Static balance measured using a progressive test protocol (balance index) Dynamic balance: tandem walk (time and errors recorded) Gait velocity : 2 m at normal pace (m/s) Short Physical Performance Battery ‐ calculated from 3 measures above Compliance/adherence:.Median compliance was 86.6% including drop outs. Adverse events: No adverse events reported. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised programme using randomly permuted blocks stratified by gender in blocks of 4 by investigator not on site and not involved in testing or training. Opaque enveloped used to conceal allocation. Randomised after baseline assessment |
| Allocation concealment (selection bias) | Low risk | But 80% of time assessor guessed correctly the allocation suggesting incomplete maintenance of blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | All measures intended were reported on |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Reported |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
Baum 2003.
| Methods | Type of study: Cross over trial, crossed over at 6/12 | |
| Participants | Number of participants randomised: 20 Losses: not reported N = 20 Age: mean 88 years Sex: 82% women, 12% men. Health status as defined by authors:not reported Residential status of participants: institutional dwelling, long term facility Setting: USA Inclusion: > 65 living in the facility for more than 3/12, able to ambulate with device or one person Exclusion:acute unstable illness, chronic illness, unable to follow 2 step command, assaultive behaviour pattern, unwillingness to discontinue existing therapy |
|
| Interventions | EXERCISE GROUP (STRENGTH): n = 11 strength and flexibility training, ankle and wrist weights, theraband CONTROL GROUP: n = 9 recreational activity, drawing and painting, puzzles, cards Duration and intensity: 1 hr 3 x per week for 6/12 Supervisor: exercise physiologist and trained staff Supervision:group Setting: institution (home) | |
| Outcomes | Berg balance scale (0 to 56 points) TUG (s) Physical Performance Test (7 point scale) Compliance/Adherence: at exercise group 80%, recreational group 56% Adverse events: not reported |
|
| Notes | Data not reported appropriately for analysis purposes. (Our approach for cross‐over RCTs, data for the initial periods were included but it was deemed inappropriate (due to potential long lasting effects of the intervention) for the crossover data to be included.) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers supplied in sequence by co‐ordinator |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis performed |
| Selective reporting (reporting bias) | High risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Cross over study |
| Blinding (assessor) | Low risk | Assessors blind to group allocation |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
Beling 2009.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 23 Losses: 4 (3 control, 1 exercise) Age: mean age 80 years Sex: 42% women Residential status of participants: community dwelling Health status as defined by authors: healthy Setting: USA Inclusion: over 65 years, community dwelling, English speaking, minimal vision and hearing limitations Exclusion:history of cardiac conditions, musculoskeletal/neurological conditions affecting balance, fracture in past year. |
|
| Interventions | EXERCISE GROUP (GBFT) (n = 11): CoG exercises (closed chain), balance strategies, ankle hip and stepping; treatment of sensory impairments to use visual inputs and somatosensory inputs; exercise for ROM and strength. CONTROL GROUP (n = 8): usual activity Duration and intensity: 1 hour 3 x per week 12 weeks Supervisor: Physical therapist Supervision:group Setting: clinic | |
| Outcomes | SOT composite score TUG (s) Berg Balance Scale (0 to 56 points) gait speed (cm/s) Compliance/adherence: Subjects "expected" to attend 30/36 classes but compliance not reported Adverse events: No adverse events reported. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation mentioned but Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Losses not accounted for, only those who completed |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | No follow‐up after the intervention year of the study |
Beyer 2007.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 53 completers in two arms Losses: 12 (8 intervention, 4 control) from 65 Age: mean (SD) 78.6 (5.1) exercise group, 77.6 (4.4) control group. Sex: women Residential status of participants: community dwelling Health status as defined by authors: healthy but fallers Setting: Denmark. Inclusion: Aged 70 to 90; community dwelling; fall requiring hospital visit not admission Exclusion: fracture of lower limbs within 6 months; neurological diseases; cognitive impairment (MMSE <24) |
|
| Interventions | EXERCISE GROUP (MULTIPLE) (n = 24): strengthening exercises (high intensity >70% 1 RM (repetition maximum)), highly challenging balance exercises, flexibility. CONTROL GROUP (n = 29): usual activity. Duration and intensity: 6 months of 2 x 1 hour supervised classes per week. Supervisor: physical therapist for exercise groups. Supervision: group exercise classes for exercise groups Setting: community therapy gym | |
| Outcomes | Berg Balance Scale (0 to 56 points) Maximal walking speed (m/s) Compliance/adherence:Compliance in exercise group 79% (42 to 100%). Adverse events: No adverse events reported. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised generation |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Losses not accounted for, only those who completed |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | High risk | Exercise group had three controls in it that wanted to exercise so potential bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Yes, reported independent |
| Were the treatment and control group comparable at entry? | High risk | Yes in most tests, but had more chronic diseases and had lower balance confidence (ABC) |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | Low risk | Detraining was looked at 6 months after intervention training |
Bogaerts 2007.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 220 Losses: 33 (but an additional 23 subjects who did not reach minimal compliance were not included) WBV : n = 94; (aged 66.08 (0.5) years old); FIT: n = 60 (aged 66.8 (0.6) years old) CON: n = 66 (aged 67.8 (0.6) years old) Age: 60 to 80 Sex: WBV: 46 women and 48 men FIT: 30 women and 30 men CON: 30 women and 36 men Health status defined by authors: healthy older people Residential status of participants: community Setting: Belgium Inclusion: aged 60 to 80 years and non‐institutionalised Exclusion: diseases or medications known to affect bone metabolism or muscle strength and engagement with moderate intensity exercise programmes for more than 2 hours per week. Suffering from diabetes, neuromuscular disorder or neurodegenerative disease, stroke, heart disease |
|
| Interventions | EXERCISE GROUP (VIBRATION) Whole Body Vibration (WBV) (n = 94) exercise on vibration platform, squat, deep squat, wide stance squat, toes‐stand, toes = stand deep, 1 legged squat and lunge. 40 minute sessions. EXERCISE GROUP (MULTIPLE) (n = 60) cardiovascular, resistance and flexibility exercises for approximately 1.5 hours. CV programme of walking, running cycling or stepping. Resistance programme exercises for whole body including leg press and leg extension; balance exercise included single leg and double leg on stable and unstable surfaces. CONTROL GROUP (n = 66): no changes in lifestyle including exercise for 12 months Duration and intensity: Both groups trained 3 x week for 12 months Supervisor: exercise instructors Supervision: group Setting: university training centre |
|
| Outcomes | Sensory Organisation Test (SOT) Compliance/adherence: attendance 87.9% WBV group, 86.5% FIT group Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | Although data difficult to access |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Not stated |
| Were the treatment and control group comparable at entry? | Unclear risk | Insufficient information to permit judgement |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | No follow‐up after the intervention year of the study |
Boshuizen 2005.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 73 Losses: 23 of 72 from 3 arms (plus 1 drop out before pre‐test) N = 33 completers in two arms plus 17 controls = 50 Age: mean (SD) 80.0 (6.7) high guidance group, 79.3 (7) medium guidance group, 77.2 (6.5) control group. Sex: high guidance group ‐ all women, medium guidance group ‐ 2 men, control group ‐ 2 men. Health status defined by authors: Healthy Residential status of participants: Community living (inc blocks with apartments for elderly) Setting: Netherlands. Inclusion: difficulty getting up from chair. Exclusion: maximum knee extensor torque over 87.5 Nm, self reported disease adversely affected by exercise. |
|
| Interventions | EXERCISE GROUP High guidance Intervention group (STRENGTH) (n = 16): strengthening exercises of lower limbs with theraband and increasing resistance in sitting and standing 2 exercise classes supervised by therapist plus 1 unsupervised. EXERCISE GROUP Medium guidance intervention group (STRENGTH) (n = 16): strengthening exercises of lower limbs with theraband and increasing resistance in sitting and standing 1 exercise class supervised by therapist plus 2 unsupervised home sessions CONTROL GROUP (n = 17): usual activity. Duration and intensity: HG ‐ 10 weeks of 2 x 1hour supervised classes per week and 1 self supervised home session, MG ‐ 10 weeks of 1 x 1hour supervised classes per week and 2 self supervised home session Supervisor: physical therapist for exercise groups. Supervision: group exercise classes for exercise groups and self home exercises. Setting: community. |
|
| Outcomes | 20 metre walk test (s).
TUG (s).
Tandem stance (s) Compliance/adherence: in high guidance exercise group 73% In medium guidance 76% Adverse events: not reported |
|
| Notes | Trial had 3 arms but NSD between 2 interventions therefore data taken from 'High guidance' group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Characteristics of participants and drop‐outs presented in a table |
| Selective reporting (reporting bias) | Low risk | Intervention described and outcomes presented as prespecified |
| Other bias | Unclear risk | Randomisation adjusted to have fewer in control group |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Assessors blinded |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Pre and post ‐ no follow‐up after 10 week intervention |
Brouwer 2003.
| Methods | Type of study: RCT. | |
| Participants | Number of participants randomised: 38 Losses: 4 of 38 (2 in exercise and 2 in control (education)) N = 38 Age: mean (SD) 77.1 (5.1) ‐ exercise group, 78.0 (5.5) ‐ control group (education). Sex: 5 men, 12 women ‐ exercise group, 4 men, 13 women ‐ control group. Health status defined by authors: healthy (no history of falls) Residential status of participants: independent community living Setting: Canada. Inclusion: fear of falling. Exclusion: co‐morbidities (neuropathy, vestibular deficits, mobility arthritis, neurological conditions). |
|
| Interventions | EXERCISE GROUP (MULTIPLE): (n = 17) low resistance exercises against gravity, theraband for legs and trunk, reaching, weight shifting, marching on spot, and home exercise programme. EXERCISE GROUP (Education): (n = 17) discussion about concerns relating to falling, education about environment. Duration and intensity: 1 hour per week x 8 weeks both groups. Exercise group additional 40 minutes x 2 week unsupervised home exercise programme. Supervisor: physiotherapist. Supervision: group. Setting: gym. | |
| Outcomes | Force platform: LOS AP and ML (cm).
Walking speed (middle 10 of 20 metres) (m/s) Compliance/Adherence: not reported Adverse events: Not reported. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | High risk | Paper states 'blinded to group allocation' but method unclear. Same physiotherapist delivered both interventions |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Balanced across groups 4 lost to follow‐up: 2 ill, 2 unavailable for retesting |
| Selective reporting (reporting bias) | Low risk | Protocol described in detail |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Blinding not known |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Baseline, post intervention, plus follow‐up only at 6 weeks |
Buchner 1997a.
| Methods | Type of study: RCT. | |
| Participants | Number of participants randomised: 105.
Losses: 5 of 105. Age: mean 75, range 68 to 85 Sex: 51% women. Health status as defined by authors: Frail with history of falls Residential status of participants: enrolled from health maintenance organisation Setting: USA. Inclusion: 68 to 85 years unable to do 8 step tandem gait with no errors, below 50th centile for knee extensor strength for height and weight. Exclusion: cardiovascular, pulmonary, vestibular and bone disease, dependency terminal illness, unable to speak English, positive cardiac stress test, body weight greater than 180% of ideal. |
|
| Interventions | EXERCISE GROUP (STRENGTH): weight machines (n = 25)
EXERCISE GROUP: endurance training (n = 25) EXERCISE GROUP: strength and endurance training (n = 25) CONTROL GROUP: usual activities (n = 30). Duration and intensity: intervention groups ‐ 1 hour x 3 days a week (24 to 26 weeks). Supervisor: not stated. Supervision: group. Setting: gym/ clinic. |
|
| Outcomes | Ability to walk on wide and narrow beams.
Balance in parallel, semi tandem and tandem stance (s).
Single legged stance (s)
Gait speed (m/min).
Tilt board AP and OMNI directional (s) Compliance/adherence : Adherence: 14 of 75 randomised to exercise dropped out (described and reasons given), 1 drop out from control group Adverse events: not reported |
|
| Notes | Trial had 4 arms. Part of FICSIT study see Buchner 1993. Only strength and control groups included in our analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random permuted blocks |
| Allocation concealment (selection bias) | Unclear risk | Not clear who carried out above |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | Protocols and outcomes all available |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Assessors blinded |
| Were the treatment and control group comparable at entry? | High risk | Home care visits greater in control group, inpatient costs greater in exercise group, self reported health lower in exercise group, formal education higher in exercise group. |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | Low risk | Measured at 6 and 9 months follow‐up |
Buchner 1997b.
| Methods | Type of study: RCT. | |
| Participants | Number of participants randomised: 106 Losses: 4 of 106 N = 106. Age: mean 75 control, 75 cycle, 74 walk, 75 aerobic. Sex: females ‐ 50% control, 54% cycle, 54% walk, 54% aerobic. Health status as defined by authors: frail Residential status of participants: enrolled from health maintenance organisation Setting: USA. Inclusion: sedentary, 68 to 85 years, mild balance deficit. Exclusion: regular exercise, cardiovascular, pulmonary, vestibular and bone disease, dependency terminal illness, unable to speak English, positive cardiac stress test, body weight greater than 180% of ideal. |
|
| Interventions | EXERCISE GROUP (CYCLING): (n = 24) static cycle
EXERCISE GROUP (WALKING): (n = 26) outdoors
EXERCISE GROUP (3D): Aerobic dance movement group: (n = 26) to music
CONTROL GROUP: (n = 30) usual activity Duration and intensity: intervention groups ‐ 1 hour x 3 per week for 3 months plus self directed exercise for 3 months. Supervisor: not stated. Supervision: group. Setting: gym/clinic. |
|
| Outcomes | OMNI tilt board (s).
Walking on wide beam (m/s).
Walking on narrow beam (m/s).
Force plate ‐ eyes open, eyes closed (area mm2/s: average radius mm).
AP tilt board (s)
Gait speed (m/min) Compliance/Adherence:Insufficient information to permit judgement of yes or no Adverse events: Part of FICSIT study see Buchner 1993 |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random permuted blocks |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Assessors blinded |
| Were the treatment and control group comparable at entry? | Unclear risk | Insufficient information to permit judgement |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | Low risk | A follow‐up assessment occurs 3 months after end of exercise |
Campbell 1997.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised:233 (116 exercise group, 117 control) Losses: 1 in control, 7 in exercise group at 6/12 N = 233 Age: mean 84.1 Sex: women Health status as defined by authors: healthy, Residential status of participants: community dwelling Setting: New Zealand Inclusion: women aged 80 years and over, able to move around own home, not receiving physiotherapy Exclusion:<7/10 on mental status questionnaire |
|
| Interventions | EXERCISE GROUP (MULTIPLE) (N=116): moderate intensity strengthening exercises including ankle cuff weights for lower limb, tandem and parallel standing, sitting and standing. CONTROL GROUP (N=117): social visits 4 times in 2 months Duration and intensity: 30 mins 3 times per week for 6 months Supervisor: exercise group, physiotherapist; control group, nurse Supervision: home visits 4 times over 2 months then self supervision Setting:home | |
| Outcomes | FRT (cm) 4 test balance scale time to walk 8 feet (s) Compliance/Adherence: not reported Adverse events: not reported |
|
| Notes | Data not fully reported: attempted to contact author for clarification | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated random numbers |
| Allocation concealment (selection bias) | Low risk | Allocation by telephone contact |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Losses reported but not clear how these were addressed in analysis |
| Selective reporting (reporting bias) | High risk | Outcomes of interest not fully reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Assessor blind to group allocation |
| Were the treatment and control group comparable at entry? | High risk | Differences in total number of medications and history of knee arthritis |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | Low risk | Immediately post intervention (6 months) and 1 year |
Carvalho 2009.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 57 Losses: none Age: Mean = 68.4 (ex) and 69.6 (control) Sex: all women Residential status of participants: community dwelling Health status as defined by authors: healthy Setting: Portugal Inclusion: 64 to 85 years Exclusion: being active 2 days per week for 20 minutes or more vigorous exercise, smoking, blindness, severe hearing impairment, uncontrolled hypertension/diabetes, cardiorespiratory disease, severe renal disease, uncontrolled epilepsy, progressive neurological disease and chronic disabling arthritis. |
|
| Interventions | EXERCISE GROUP (MULTIPLE) (n = 32): warm up, aerobic exercises (jogging, dancing and step), muscular endurance (circuit for upper and lower limbs including weight resistance); agility and reaction (games and walking heel to toe etc.); cool down CONTROL GROUP (n = 25): usual activity Duration and intensity: 1 hr, 2 x week, 8 months, Supervisor: physical education instructor Supervision: group Setting: clinic | |
| Outcomes | 8 foot up and go (s) Compliance/adherence: exercise group completed 91% of sessions (84‐100%) Adverse events: No adverse events reported. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation mentioned but insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | As‐treated analysis done. No drop‐outs reported but differences in size between groups 32 exercise and 25 control. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | Low risk | Outcomes assessed immediately post interventions and 3 months follow‐up. |
Chandler 1998.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 100 Losses:13 (7 control, 6 exercise) Age: mean 77.6 years Sex: 50 men, 50 women Health status as defined by authors: functionally impaired/frail Residential status of participants: community dwelling Setting:USA Inclusion: inability to descend stairs, step over step without holding on Exclusion: <18 on MMSE, unable to follow 3 step command, 3 or more on Reubens advanced ADL, terminal illness, diseases, blindness, amputation |
|
| Interventions | EXERCISE GROUP (STRENGTH): (N=50) resistive lower extremity exercises, theraband and body weight CONTROL GROUP: (N=50) usual activity Duration and intensity: 3x week for 10 weeks Supervisor: physical therapist Supervision: individual Setting:home | |
| Outcomes | Functional Reach Test (inches) Spontaneous postural sway (cm) Compliance/adherence: not reported Adverse events: not reported |
|
| Notes | Data not reported appropriately for analysis purposes. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation, stratified by two levels of functioning |
| Allocation concealment (selection bias) | Low risk | Persons conducting pre and post tests were blind to group allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Losses reported |
| Selective reporting (reporting bias) | Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Both pre and post intervention assessors blinded to which groups subjects in and baseline test results respectively |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately (within 5 days) post intervention |
Chang 2007.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 21 Losses: one reported in exercise group Age: 74 to 93 years Sex: not reported Health status as defined by authors: at increased risk of falls Residential status of participants: community dwelling Setting: USA Inclusion: at increased risk of falls Exclusion:not reported |
|
| Interventions | EXERCISE GROUP (STRENGTH): lateral trainer, high velocity resistance training CONTROL GROUP: usual activity Duration and intensity: 3 x per week for 10 weeks Supervisor: not stated Supervision: not stated Setting:not reported | |
| Outcomes | Four square step test Walking Speed Single leg stance Compliance/adherence:exercise group attended at least 85% of sessions (at least 25 sessions) Adverse events: No adverse events reported |
|
| Notes | Abstract only available. No appropriate data reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | Unclear risk | Insufficient information to permit judgement |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Cheung 2007.
| Methods | Type of study:RCT | |
| Participants | Number of participants randomised:75 Losses: 6 Age: 60 or above Sex: women Health status defined by authors: healthy Residential status of participants: community living elderly women Setting: Hong Kong Inclusion: 60 years or over; able to stand independently without aids Exclusion: hormonal replacement or drug treatment affecting normal metabolism; hypo or hyper thyroidism renal liver or chronic disease; previous or current smokers or drinkers; habitual exercise or participate in exercise. |
|
| Interventions | EXERCISE GROUP (VIBRATION) (n = 50): Whole body vibration CONTROL GROUP (n = 25): No intervention Duration and intensity: 3mins/day; 3days/week; 3 months Supervisor: research assistant Supervision: one to one Setting: community centre |
|
| Outcomes | Limits of stability assessed on a Basic Balance Master system. Measured parameters included: reaction time (s); movement velocity (deg/s); endpoint excursion (% limits of stability); maximum point excursion (% limits of stability); directional control (% accuracy) Functional reach (cm) Compliance/adherence:defined as number of treatment sessions attended over total number of treatment sessions was recorded by research assistant. Described = 93.3% compliance in exercise group Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Low risk | Independent RA using sealed envelope |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Drop outs described but not addressed in data analysis |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Different group size (50 and 25) |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
Chulvi‐Medrano 2009.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 28 Losses: none Age: Ex = 69.5 (0.99) Control = 70.7 (2.18) Sex: women Residential status of participants:community dwelling Health status as defined by authors:healthy Setting:Spain Inclusion: age 65+, community dwelling, healthy with no history of significant cardiovascular, pulmonary, metabolic, musculoskeletal or neurological disease, no prior history of falls, no use of medication impairing balance Exclusion: |
|
| Interventions | EXERCISE GROUP (MULTIPLE) (n = 18): using a T‐Bow device, squats, side and frontal swinging, frontal lunges, plantar flexo‐extensions. Variable exposure time and modification of base of support and perceived exertion. CONTROL GROUP (n = 10): usual activity Duration and intensity:30 min 2 x week for 8 weeks. Supervisor:professional with a degree in physical activity and sport Supervision:group Setting:clinic | |
| Outcomes | Single leg stance (s) 8 foot up and go (s) Compliance/adherence: not reported Adverse events: No adverse events reported. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation mentioned with non‐equilibrated design with 20% more in exercise group. Method of randomisation not mentioned. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No drop outs mentioned. Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | High risk | Appear to be differences between the groups at pre‐test in all balance outcome measures but no significance reported. |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Clemson 2010.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 34 Losses: 25% controls, 6% exercise group Age: Ex = 81 (5.6) Control = 82 (6.3) Sex: 16 women, 18 men Residential status of participants: community dwelling Health status as defined by authors: healthy but at least 2 previous falls Setting: Australia Inclusion: community dwelling, aged 70 years or over, 2 or more previous falls Exclusion: moderate to severe cognitive problems, no conversational English, inability to ambulate independently, unstable or terminal medical illnesses, neurological conditions resulting in motor performance difficulties. |
|
| Interventions | EXERCISE GROUP (GBFT) (n = 16): LiFE programme. Four balance strategies (reduce base of support, move to limits of sway, shift weight from foot to foot, step over objects) and seven strength strategies (bending knees, on toes, on heels, up the stairs, sit to stand, move sideways, tighten muscles). Embedded in normal activities.
CONTROL GROUP (n = 18): usual activity Duration and intensity: 5 home visits, 2 booster visits over 3 month period and 2 follow‐up phone calls. Activities meant to be performed in everyday life (i.e. daily) Supervisor: physiotherapist Supervision: individual for first five visits then two booster visits over next three months Setting: home |
|
| Outcomes | Tandem walk over 3 m (s) One leg stance max 15 s (s) Tandem stand (s) Compliance/adherence: not reported Adverse events: No adverse events reported. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table, stratified by age and falls history |
| Allocation concealment (selection bias) | Low risk | Investigator blind to allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis, unequal rate of drop outs 25% controls, 6% exercise group) |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Blinded outcome assessor |
| Were the treatment and control group comparable at entry? | High risk | Significant differences in tandem stance eyes open (control group lower values) |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | Low risk | Assessments at immediately post intervention and 3 months follow‐up. |
Cress 1999.
| Methods | Type of study: RCT. | |
| Participants | Number of participants randomised: 56 Losses: 7 of 56 (7 dropped out of exercise, 0 dropped out of control) Age: Exercise group: 75.6 (3.6), Control group 76 (5.1) Sex: not stated Health status as defined by authors: healthy Residential status of participants: independently living in community Setting: USA. Inclusion: 70 years and above, good health, living in retirement community or apartment. Exclusion: unstable cardiovascular or metabolic disease, recent unhealed fractures, other disorders, life expectancy less than 1 year, excessive alcohol, non English speaking. |
|
| Interventions | EXERCISE GROUP (MULTIPLE): combined endurance and resistance. CONTROL GROUP: no exercising. Duration and intensity: 1 hour x 3 per week for 6 months. Supervisor: not stated. Supervision: group. Setting: community. | |
| Outcomes | Usual walking speed (m/s).
Time on 9 m beam (s).
FRT (cm). Compliance/Adherence: not reported Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis. |
| Selective reporting (reporting bias) | Low risk | all initial intended outcomes reported on |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Crilly 1989.
| Methods | Type of study: RCT. | |
| Participants | Number of participants randomised: 50 Losses: 3 out of the 50 (2 exercise dropped out (23) and 1 control dropped out (24)) N = 50 Age: mean 82, range 71 to 92 (not per arm) Sex: women. Health status as defined by authors: Frail Residential status of participants: Sheltered apartments, rest homes or nursing homes Setting: Canada. Inclusion: over 70 years, ability to ambulate independently, good eyesight and hearing, understand instruction, ability to participate in exercise programmes. Exclusion: no specific criteria. |
|
| Interventions | EXERCISE GROUP (MULTIPLE): exercise aimed at improving breathing, single and double limb balance, co‐ordination, flexibility, strength and relaxation. CONTROL GROUP: usual activity. Duration and intensity: exercise group ‐ 15 to 35 minutes x 3 week for 3 months. Supervisor: physiotherapist. Supervision: group. Setting: institutional ‐ sheltered rest/nursing home. | |
| Outcomes | Postural sway during quiet standing on force plate ‐ eyes open, eyes closed ‐ RMS ML and AP (mm) Compliance/Adherence: 15 exercisers attended 24 out of a possible 36 classes Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised by random tables |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
de Greef 2006.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 45 Losses: 5 (2 from exercise group and 3 from control group) N = 45 Age: 85.3 years (exercise) 86.2 years (control) Sex: 33% men (exercise group) 9% men (control group) Health status as defined by authors: frail Residential status of participants: 74% nursing home residents; 26% sheltered housing residents Setting:The Netherlands Inclusion: over 75 years of age; independently mobile Exclusion:dementia; unable to give informed consent; physio assesses as "do not mobilise" |
|
| Interventions | EXERCISE GROUP (MULTIPLE) (n = 22) : light intensity training programme with exercises from the "Dutch Institute for Sports Improvement" . Strength training, balance training and running. CONTROL GROUP: (n = 23): not stated Duration and intensity: I hour per week for 8 weeks. Intensity was 10 to 12 Borg Scale, equivalent to 50 ti 60 % max HR Supervisor: not reported Supervision: not reported Setting: not reported | |
| Outcomes | Dynamic Balance TUG (s) Static balance Functional Reach (cm) Walking Speed 10 metre walk test (s) Functional Abilities Physical Performance Test Compliance/adherence: not reported Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 45 randomised by drawing of lots |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Set out to look at between group change but reports on within group changes |
| Other bias | Unclear risk | Paper not in English language and was translated |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | High risk | Assessor aware of group assignments. |
| Were the treatment and control group comparable at entry? | High risk | Differences noted by authors at baseline. These are described but not analysed. |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
Eyigor 2009.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 40 Losses: 3 (1 exercise, 2 control) Age: over 65 years (mean 73.5 exercise, 71.2 control) Sex: women Residential status of participants: community dwelling Health status as defined by authors: healthy Setting: Turkey Inclusion: over 65 years, physically active Exclusion: neurological impairment, severe cardiovascular disease, unstable chronic or terminal illness, major depression, severe cognitive impairment or musculoskeletal impairment. |
|
| Interventions | EXERCISE GROUP (3D) (n = 19): The dance‐sessions were divided into the following three sections: a warm‐up period, a special folklore dance stepping period, a stretching and a cool‐down period. During movement to movement knees were regularly flexed, shoulders were elevated and depressed and participants walked in a circle. CONTROL GROUP (n = 18): usual activity Duration and intensity: 1 hour sessions, 3 x week, 8 weeks, encouraged to walk half an hour twice a week Supervisor:senior folklore dance expert Supervision: group Setting: clinic | |
| Outcomes | Gait 20 m (s) Berg Balance Score (score 0 ‐ 56) Compliance/adherence: not reported Adverse events: No adverse events reported. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation mentioned but insufficient information about the sequence generation process to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | ‘As‐treated’ analysis done, drop outs reported |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Faber 2006.
| Methods | Type of study: cluster RCT ‐ 15 clusters homes randomly assigned to 1 of the 2 exercise interventions | |
| Participants | Number of participants randomised: 278 Losses: 76 Age: FW = 85.4 (5.9); IB = 84.4 (6.4); CON = 84.9 (5.9) Sex: 188 women Health status defined by authors: frail and pre‐frail Residential status of participants: care homes Setting: 16 care homes, the Netherlands Inclusion: not specified Exclusion: unable to walk 6m independently (use of walking aid allowed); impaired cognition preventing compliance with intervention; medical condition the contraindicated. |
|
| Interventions | EXERCISE GROUP (GBFT) : Functional walking (FW) (n = 66) = 10 exercises focus on balance, mobility and transfer training e.g.. Sit‐stand, reaching, stepping forward and sideways, step on or over obstacle, stair walking, heel and toe stands, walking and turning, tandem and single leg standing EXERCISE GROUP (3D) (n = 80) = Tai Chi principles CONTROL GROUP (n = 92): no exercise Duration and intensity: 1 session per week for 4 weeks, 2x week for 16 weeks. Each session lasts 90 mins, including 30 min social. Supervisor: instructor and assistant Supervision: maximum size of group was 15. Setting: care homes |
|
| Outcomes | Physical Performance Scale (PPS) comprised (walking speed test (ms), timed chair stands (s), TUG (s), FICSIT‐4 balance test (s)) Compliance/Adherence: on average 32 out of 36 sessions completed, median relative compliance was 88% for FW and 84% for IB Adverse events: not reported |
|
| Notes | Data for outcomes were reported as a composite score PPS and individual components were not reported separately | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 2 levels of block‐wise randomisation. Homes randomly assigned to 1 of the 2 exercise interventions using sealed envelopes; participants in each of the homes randomised across intervention and control using computer generated random numbers |
| Allocation concealment (selection bias) | Low risk | Reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Used linear regression models which account for missing data but not in mean and SD values reported in table. The analysis may have accounted for this? |
| Selective reporting (reporting bias) | Low risk | Intended measures reported on |
| Other bias | High risk | Failure to adjust for clustering |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Reported |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | Low risk | 52 week follow‐up for primary outcome of falls not other measures |
Frye 2007.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 84 (31 in Tai Chi group 30 in LIE group and 23 in control) N = 84 Losses: 8 from TC; 2 from LIE and 2 from control Age: 69.2 ± 9.26 (M ± SD) years with an age range of 52 to 82 years. Sex: 30 men and 54 women. Health status as defined by authors: not reported but inferred from inclusion criteria below Residential status of participants:community dwellers Setting: New Jersey, USA presumed. Inclusion: individuals had to be at least 50 years old, to have not regularly exercised for at least 3 months (less than 1hour of purposeful exercise per week), and to provide a note from their personal physician stating that they were physically fit to participate in a low to moderate intensity exercise program. Exclusion: not specified |
|
| Interventions | EXERCISE GROUP (MULTIPLE): (N=30) Low Intensity Exercises (LIE) focusing on enhancing the main elements of physical fitness: strength, flexibility,endurance, and balance. EXERCISE GROUP (3D): (N=31) Tai Chi was taught using a 10‐posture choreography made up of basic and classic postures from the Yang family style CONTROL GROUP: (N=23) non exercise Duration and intensity: expected to attend three 60‐minute classes per week over 12weeks classes (offered at multiple times during the day, five times a week.) Supervisor: experienced instructors Supervision: at classes Setting: local martial arts studio. |
|
| Outcomes | 8‐foot up‐and‐go test (s) Compliance/adherence:Class attendance ranged from 72.2% to 100.0%. Adverse events: not reported |
|
| Notes | Other comments: Data for over 50s, unable to extract data for over 60s only. However we estimated that the number of people under the age of 60 was 17% therefore all data was included in analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | High risk | Reported as study limitation |
| Were the treatment and control group comparable at entry? | Low risk | Comparisons are reported. Only statistical significant difference was on the sit‐to‐stand test at baseline measurement but reported as clinically non‐significant. |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
Furness 2009.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 75 Losses: none Age: mean 72 years (SD 8) Sex: 38 women, 35 men Residential status of participants: community dwelling Health status as defined by authors: healthy Setting: Australia Inclusion: 65 years plus living independently Exclusion: fallen in past 2 months, reactive arthritis, vascular disease, vertigo, high risk thromboembolism |
|
| Interventions | EXERCISE GROUP (VIBRATION) (n = 18): vibrating plate 1 x week (6 sessions) 5 1‐minute bout with 1‐minute rest. Frequency of vibration 15 Hz week 1 to 25 Hz week 6. EXERCISE GROUP (VIBRATION) (n = 18): vibrating plate 2 x week (12 sessions) as above EXERCISE GROUP (VIBRATION) (n = 19): vibrating plate 3 x week (18 sessions) as above CONTROL GROUP (n = 18): usual activity Duration and intensity: as above for groups Supervisor: not reported Supervision: individual Setting: clinic |
|
| Outcomes | TUG (s) Compliance/adherence: 100% for all groups. Adverse events: No adverse events reported. |
|
| Notes | The data for the 3 x per week group were used in the analyses | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation mentioned but insufficient information about the sequence generation process to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No drop outs |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | Unclear risk | Not possible |
| Blinding (assessor) | Unclear risk | Not reported |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
Gaub 2003.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 80 to 4 groups Losses: not stated N = 75 Age: average 85, range 77 to 102 Sex: 80% women Health status as defined by authors: frail Residential status of participants: community dwelling Setting: USA Inclusion: score 30 or less on modified physical performance test Exclusion:not stated |
|
| Interventions | EXERCISE GROUP (STRENGTH): with machines for upper and lower limbs; EXERCISE GROUP: (GPA‐WALKING) 20 to 25 mins at 80% estimated HR max or PRE 7‐8/10 EXERCISE GROUP (GBFT): flexibility standing and sitting, floor, static and dynamic balance, variable surfaces, eyes open/closed, ball toss/kick, punch bag. CONTROL GROUP: usual activity (3 month wait). Duration and intensity: 36 sessions Supervisor: not stated Supervision: group Setting: wellness centre |
|
| Outcomes | Berg Balance Scale (0 to 56 points) 15 m preferred and fast gait speed (s) Compliance/adherence:not stated Adverse events: not reported |
|
| Notes | Other comments: only abstract and platform presentation papers available. Data not reported appropriately for analysis purposes. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | Unclear risk | Insufficient information to permit judgement |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | Low risk | 3 and 6 month follow‐up |
Gine‐Garriga 2010.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 51 Losses: at end of intervention 6 control, 4 exercise; at 6 months FU a further 12 control, 4 exercise Age: 84 (± 2.9) yr Sex: 31 women, 20 men Health status as defined by authors: frail Residential status of participants: community‐dwelling Setting:Spain Inclusion: one randomly selected primary health care centre, 80 to 90 years Exclusion:unable to walk, undergoing an exercise program, severe dementia (not able to understand or follow verbal commands), or had had a stroke, hip fracture, myocardial infarction or hip‐ or knee‐ replacement surgery within the previous 6 months |
|
| Interventions | EXERCISE GROUP (GBFT) (n = 26): 1 day of balance‐based activities and 1 day of lower body strength‐based exercises; both were combined with function focused activities. Balance activities were designed to challenge the visual (e.g. eyes open/closed), vestibular (e.g., move head), and somatosensory (e.g., stand on foam) systems. Balance exercises included function‐focused activities such as walking with obstacles, while wearing standard sunglasses (worn over corrective lenses as needed) to mimic a semidark environment, walking while carrying a package that obstructed the view of the feet, and walking while picking up objects from the floor. Lower body exercises included functional tasks such as rising from a chair, stair climbing, knee bends, floor transfer, lunges, leg squat, leg extension, leg flexion, calf raise, and abdominal curl using ankle weights. initially 8 reps increased to 15. The load was increased 0.5 kg when a participant could perform 15 repetitions at a lower perceived exertion intensity, up to a maximum of 2 kg. CONTROL GROUP (n = 25): met once a week for health education meetings, four health education sessions of 60 min over the 12 visits. Duration and intensity: 45 mins twice a week for 12 weeks Supervisor: investigator (not stated) Supervision: group Setting: primary care facility |
|
| Outcomes | Gait speed 8 m of a 12‐m (m/s) Modified Timed Up‐and‐Go Test (includes kicking a ball) (s) Semi tandem stance (s) Tandem Stands (s) Single‐Leg stand (s) Compliance/adherence: Exercise group: compliance 90%; all participants were compliant with the exercise prescription except for 1 woman who required rest (sitting on a chair) after each exercise during the first 3 weeks. Control Group: compliance 76% Adverse events: No adverse events reported. |
|
| Notes | Sample‐size calculations: thirty‐eight participants (19 per group) were needed to detect a 20% improvement in the rapid‐gait test, at a power of 80% and an α of .05, and a 20% dropout rate. Forty‐four participants (22 per group) were needed to detect a 15% improvement in the stand‐up test, analysed with the same criteria as the rapid‐gait test. These data produce extreme results in the meta‐analyses. The SE may have been reported in error. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A computer‐generated algorithm was used |
| Allocation concealment (selection bias) | Low risk | Personnel who maintained the randomisation log were not involved in screening, testing, or training procedures |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | Unclear risk | Not possible |
| Blinding (assessor) | Low risk | An assistant who had no role in the intervention and was unaware of the study hypothesis and of the participants’ group assignments |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | Low risk | Immediately post intervention and six months after the end of the program |
Granacher 2009.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 40 Losses: none reported Age: 67 (SD 1) years Sex: men Residential status of participants: community dwelling Health status as defined by authors: healthy Setting: Switzerland Inclusion: age 60 to 80 years, healthy with no history of serious muscular, neurological, cardiovascular, metabolic or inflammatory diseases. Exclusion: |
|
| Interventions | EXERCISE GROUP (STRENGTH) (n = 20): warm up, cycle. 80% 1 RM (repetition maximum) leg press, leg extension, calf raise, foot dorsi flexors. 3 sets of 10 reps. CONTROL GROUP (n = 20): usual activity Duration and intensity:1hr sessions, 3 x week, 13 weeks Supervisor: sport scientist Supervision: individual Setting: clinic | |
| Outcomes | FRT (cm) Tandem walk forward (number of steps) Tandem walk backwards (number of steps) Compliance/adherence: not reported Adverse events: none reported |
|
| Notes | Data not reported appropriately for analysis purposes. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Radmomisation mentioned but method not stated |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Data reported for total sample |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Not reported |
| Were the treatment and control group comparable at entry? | Unclear risk | Insufficient information to permit judgement |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Hall 2009.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 22 Losses: 7 (n = 3 health; n = 3 time; n = 1 polypharmacy) Age: 72.2 (SD 7) years (range 62 to 85) Sex: 10 women, 5 men Residential status of participants: community dwelling Health status as defined by authors: healthy Setting: USA Inclusion: over 60 years, community dwelling, at risk of falls or experienced a fall, good vision. Exclusion: score less than 24 on MMSE, inability to hear tones, excessive medication, inability to walk without assistance. |
|
| Interventions | EXERCISE GROUP (3D) (n = 8): Tai Chi classic Yang style (24 forms) CONTROL GROUP (n = 7): Duration and intensity: 1.5 hr class, 2x week 12 weeks Supervisor: certified Wu Dang Tai Chi instructor Supervision: group Setting:clinic | |
| Outcomes | SOT eyes open, eyes closed Compliance/adherence: not reported Adverse events: none reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation mentioned but insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | ‘As‐treated’ analysis done, drop outs not reported |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Not reported |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Hara 2007.
| Methods | Type of study: RCT. | |
| Participants | Number of participants randomised: 52 Losses: 8 of 52 (6 exercise and 2 control) Age: Exercise 84.4 (5.6) Control 85.6 (4.8). Sex: women (n = 35) and men (n = 10). Setting: Japan, Health of participants: frail Residential Status: residential care facilities or frail visitors. Inclusion: walk independently or with an aid Exclusion: no specific criteria. |
|
| Interventions | EXERCISE GROUP (MULTIPLE): Sit to stands, standing up to parallel bars, light weights for seated arm strengthening ‐ low balance challenge CONTROL GROUP: usual activity. Duration and intensity: 2 or 3 times a week for 6 months.‐ duration of exercise not reported, estimated at 30 mins a session Supervisor: not known. Supervision: not clear if in a group or on a one to one basis. Setting: gym in care home. | |
| Outcomes | Functional Reach (cm) Timed Up and Go (clockwise and anticlockwise) (s) Walking time (s) Compliance/adherence: not reported. Adverse events: not reported |
|
| Notes | Subjects in both groups also attended other group activities in the home. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No randomisation method reported |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Differences between drop outs and completers not reported |
| Selective reporting (reporting bias) | Low risk | All outcome measures addressed |
| Other bias | High risk | Both groups attended other group activities which may have influenced results as no account of how many or what |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Not reported |
| Were the treatment and control group comparable at entry? | High risk | Only reported on age, weight and height (no differences) but although measured did not report on balance and strength |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Hatzitaki 2009.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 56 Losses: none reported Age: 70.9 (SD 5.7) years Sex: women Residential status of participants: community dwelling Health status as defined by authors: healthy Setting: Greece Inclusion: free from any neurological and/or musculoskeletal impairment, voluntarily participated in the study. They had no prior physical practice or experience in sports‐related activities. Exclusion: |
|
| Interventions | EXERCISE GROUP (COMPUTERISED BALANCE) (n = 20): A/P training visually guided WS task, warm‐up (5 min stretching), main phase (15 min, 3 sets of 5 WS trials separated by 1‐min intervals) and recovery phase, (5 min stretching). EXERCISE GROUP (COMPUTERISED BALANCE) (n = 20) M/L training visually guided WS task, warm‐up (5 min stretching), main phase (15 min, 3 sets of 5 WS trials separated by 1‐min intervals) and recovery phase, (5 min stretching). CONTROL GROUP (n = 16): usual activity Duration and intensity: 12 x 25 min sessions (3 sessions/week, 4 weeks) Supervisor: researcher Supervision:individual Setting: clinic |
|
| Outcomes | Force platform data (multiple variables) Compliance/adherence: not reported Adverse events: No adverse events reported. |
|
| Notes | Data from the 2 exercise groups were excluded the meta‐analysis as groups were trained in the outcome measures and data was not able to be combined. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation mentioned but insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Probably ‘As‐treated’ analysis done, no drop outs reported but groups unequal sizes |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Not reported |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Henwood 2006.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 67 Losses: drop outs described HV = 2; CT = 2; CO = 2; CB = 1. Were not different from other subjects and dropped out for a variety of reasons. Age: 65 to 84 years: HV 70.7+5.5; CT 70.2+5.0; CO 69.1+3.6; CB 69.3+4.1; Sex: HV N = 23; men = 9; women = 14; CT N = 22; men = 11; women = 11; CO N = 22; men = 10; women = 12 Health status defined by authors: healthy Residential status of participants: independent living ‐ community Setting: Australia Inclusion: not reported Exclusion: acute or terminal illness; moderator severe cognitive impairment; unstable or ongoing cardiovascular/respiratory disorder; neurological or musculoskeletal disease or impairment; resistance training experience within the previous 12 months; inability to commit to a period of time equivalent to the duration of the study |
|
| Interventions | EXERCISE GROUP (STRENGTH): High‐velocity, varied‐resistance training and gym based functional training (HV) = (n = 23); Twice weekly for 8 weeks EXERCISE GROUP (STRENGTH): Slow to moderate‐velocity constant‐resistance training (CT) = (N = 22).Twice weekly for 8 weeks CONTROL GROUP (n = 22): no training The resistance training consisted of 6 exercises using resistance equipment : chest press; supported row; biceps curl; leg press; leg curl; leg extension. 10 min warm up ; exercise and then cool down. All exercise groups started with 2 weeks of conditioning then 6 weeks of training; 2 weeks conditioning 8 reps x 3 of each exercise; training = 10 reps x 3 of each exercise. HV and CT did same reps but HV performed concentric part explosively and 3 s eccentric e.g. as fast as possible; while CT did 3 s concentric and 3 s eccentric. Exercise group (CB): Combined high‐velocity varied‐resistance and once weekly gym‐based functional training (CB) = 15. Once weekly for 8 weeks. CB : combined resistance and functional training N = 15.This group was the control group who after exiting the study were invited to take part in this phase, accounting for fewer subjects. This group were then compared to the other randomised groups and therefore not strictly randomised and definitely unblended. This group did functional strength training: fit ball squats; chair rise to standing; stair climb; calf raises; chair dips; lateral shoulder exercise. 3 x 10 reps. Duration and intensity: 8 weeks for HV and CT; CO = 24 weeks. The 8 weeks programme for HV and CT = 2 visits of approximately 1 hour. Supervisor: exercise instructor Supervision: group exercise of up to 6 persons Setting: gymnasium |
|
| Outcomes | 6 metre usual, fast and backward walk (s) Chair rise to standing (s) Floor rise to standing (s) Functional reach (cm) Timed stair climb (s) (Above are reported as Functional Performance measures) Compliance/adherence:all subjects completed 16 training sessions within a 9 week period. Adverse events: not reported |
|
| Notes | 2 intervention groups both classified as strength training however one focused on power and the other on strength therefore the latter data was used in analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement |
| Selective reporting (reporting bias) | Low risk | All outcomes appear to be reported |
| Other bias | High risk | Control group became one of intervention groups |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Not mentioned nor was the identity of the assessor |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
Islam 2004.
| Methods | Type of Study: RCT | |
| Participants | Number of participants randomised: 43
Losses: 4 prior to testing N = 43 Age: 69 to 89 years Sex: 20 men, 19 women. Health Status defined by authors: healthy Residential Status of participants: Community Setting: Japan Inclusion: healthy Exclusion: taking medication, signs or symptoms of diagnosed disease. |
|
| Interventions | EXERCISE GROUP (GBFT): (N = 29) balance exercises designed to challenge the visual (e.g. opened /closed eyes), vestibular (e.g. move head), somatosensory (e.g. stand on foam) and muscular (e.g. standing on one leg, bending body in different directions) systems. Exercises were initially performed while standing on the floor (first 4 weeks) and then progressed to standing. CONTROL GROUP: (N = 14) usual activity. Duration and intensity: 2 sessions per week for 60 minutes for 12 weeks. Supervisor: fitness instructor Supervision: individual Setting: gym | |
| Outcomes | Maximum excursion of LOS (forward, backward, right, left) Compliance/adherence: not reported Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Withdrawals well described and accounted for in analysis |
| Selective reporting (reporting bias) | Unclear risk | Insufficient reporting to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
Iwamoto 2009.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 68 Losses: 1 in control group Age: 76.4 years (range, 66 to 88 years). Sex: seven men and 61 women Residential status of participants: community dwelling Health status as defined by authors: frail Setting: Japan Inclusion: age of more than 50 years, fully ambulatory, and being able to measure parameters. Exclusion:severe gait disturbance with some aids, severe round back due to osteoporotic vertebral fractures, acute phase of diseases, and severe cardiovascular disease. |
|
| Interventions | EXERCISE GROUP (MULTIPLE) (n = 34):callisthenics, body balance training, muscle power training, and walking ability training CONTROL GROUP (n = 34): usual activities Duration and intensity: 30 minutes, 3 x week for 5 months Supervisor: not reported Supervision: group Setting: hospital clinic | |
| Outcomes | Single leg stance (s) Tandem gait (steps) Tandem standing time (s) TUG (s) 10m walk time (s) Compliance/adherence: 100% in exercise group Adverse events: Four participants in the control group experienced one fall each during the 5 months intervention period. Of four falls, one was due to a stumble of the toe, and three were caused by lurches. There were no multiple fallers during the 5 months intervention period. No serious adverse events, such as severe fall‐related injuries or adverse cardiovascular effects, were observed. |
|
| Notes | Data not reported appropriately for analysis purposes. Data only presented graphically | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation mentioned but Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis undertaken |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Not reported |
| Were the treatment and control group comparable at entry? | High risk | Significant age difference between groups |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Jessup 2003.
| Methods | Type of study: RCT. | |
| Participants | Number of participants randomised: 18
Losses: 1 from exercise group and 1 from control group N = 18 Age: mean (SD) 69.2 (3.5). Sex: women. Setting: USA Health status defined by authors: healthy Residential status of participants: community Inclusion: healthy women not taking hormone or osteoporosis medication, or done so in the last 12 months, no regular exercise in the last 12 months. Exclusion: medical history or physical examination revealing cardiac or pulmonary, endocrine, neuromuscular or orthopaedic conditions or dextra results indicating contra indication, visual acuity test less than 20/50, mini mental test less than 20, inability to retain Romberg stance for 20 seconds without losing balance, alcohol or drug abuse, smokers, psychiatric conditions. |
|
| Interventions | EXERCISE GROUP (MULTIPLE): (N = 9) Strength exercises began with 8 to 10 repetitions at 50% of pretest 1 RM (repetition maximum) score on progressed to 75%. Load‐bearing walking, stair‐climbing and balance ‐training exercises, wearing weighted vests after 2 weeks. Balance‐training exercises, in walking. CONTROL GROUP: (N = 9) usual activities of daily living. Duration and intensity: 3 sessions (60 to 90 minutes) per week for 32 weeks Supervisor: research assistant and co investigator Supervision: group Setting: gym | |
| Outcomes | Body sway (cm) Compliance/adherence : not reported Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Parallel design, random number designed by Burns and Grove |
| Allocation concealment (selection bias) | Unclear risk | Unclear, insufficient reporting to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Withdrawals well described and accounted for |
| Selective reporting (reporting bias) | Low risk | All main outcomes reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | High risk | Assessors blinded to randomisation but aware of which group participants were allocated to |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
Johansson 1991.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 34 Losses: 1 in exercise group N = 34 Age: 70 years old Sex: women Setting: Sweden Health status defined by authors: healthy Residential status of participants: Community Inclusion: healthy volunteers aged 70 years. Exclusion: neurological disease, amputation, severe pain in legs. |
|
| Interventions | EXERCISE GROUP (GBFT): (N = 18) walking different directions at different speeds, combined with movement of the arms, neck and trunk. Exercise to music including weight transfer exercises while sitting and standing and rising from and sitting down in a chair, were performed. CONTROL GROUP: (N = 16) usual activity Duration and intensity: exercise group ‐ 1 hour, twice a week, for 5 weeks. Supervisor: physiotherapist Supervision: group Setting: gym | |
| Outcomes | Single legged stance ‐ eyes open, eyes closed (s)
Walking along a beam (m)
Walking for 30 metres (s) Compliance/adherence : not reported Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear, insufficient reporting to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Withdrawals described, analysis not possible |
| Selective reporting (reporting bias) | Low risk | All main outcomes measures described |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Assessors blinded to experimental design and pre test scores. |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
Kamide 2009.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 57 Losses: 7 (5 exercise group, 2 control group) Age: mean age 71 years Sex: women Residential status of participants: community dwelling Health status as defined by authors: Setting: Japan Inclusion: 65 years and over, walk independently, no history of cerebrovascular disease, neuromuscular disease, fractures of spine or lower limbs, no restrictions in physical activity. Exclusion: cardio pulmonary, liver, kidney disease, hyperthyroidism, unstable diabetes, hypertension or steroids or performing regular exercise. |
|
| Interventions | EXERCISE GROUP (MULTIPLE) (n = 23): stretching, strength training at moderate intensity (theraband), balance (stepping forward, backwards, sideways), heel drop exercises. CONTROL GROUP (n = 27): usual activity Duration and intensity: 3 x week for 6 months Supervisor: physical therapist (only for 1 hour intro. instruction) Supervision: none (telephone calls for motivation and support) Setting: home | |
| Outcomes | Single leg stance (s) TUG (s) Gait speed preferred over 10 m (s) Gait speed fastest 10 m (s) Compliance/adherence: 82.6% completed programme 3 days per week, 91.3% completed 2 days per week. Adverse events: No adverse events reported. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated randomisation |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | ‘As‐treated’ analysis done, drop outs reported |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Assessors blinded |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Karinkanta 2007.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 149 Losses: Total = 5. (4 from the training groups and 1 from control.) (Drop out rate 3.4%) Age: RES = 72.7 (2.5); BAL = 72.9 (2.3); COMB = 72.9 (2.2); CON = 72 (2.1) Sex: women Health status defined by authors: healthy older (< 70) females Residential status of participants: community dwelling Setting: Finland Inclusion: Willing to participate; age between 70 to 79 years; full understanding of study procedures; no history of illness contraindicating exercise or limiting participation in exercise programs, no history of illness affecting balance or bones; no uncorrected vision problems; no medications known to affect balance or bone metabolism (12 months before enrolment). Exclusion: Involved in intense exercise more than 2x week or t‐score for femoral neck bone mineral density (BMD) lower than ‐2.5 |
|
| Interventions | EXERCISE GROUP (STRENGTH) (n = 37) = resistance training. 75‐80% 1 RM (repetition maximum) 3 sets of 8‐10. Large muscle group ex = sit‐stand with weighted vest, squats, leg press, hip abduct, hip extension, calf raise, rowing with resistance machines. Different combinations of above were used in 10 week cycle to prevent monotony. EXERCISE GROUP (GBFT) (n = 37) = balance jumping training. Balance agility and impact exercise. 4 different aerobics and step aerobic programs which were repeated EXERCISE GROUP (MULTIPLE) (n = 38) = resistance and balance jumping training. Reistance and balance training on alternate weeks as above CONTROL GROUP: (N=37) no training Duration and intensity: 3x weekly for 12 months, 50 mins. Warm up 7‐10 mins; 25‐30 mins exercise; 8 to 10 minutes cool down Supervisor: exercise leaders of UKK institute Supervision: groups but uncertain of number in each as not stated Setting: not described |
|
| Outcomes | Figure‐of‐8 running test 10 m (s) Compliance/adherence:mean training compliance = attendance 67% (RES = 74%; COMB = 67%; BAL = 59%) Adverse events:14 due to musculoskeletal injuries or symptoms ‐ 2 falls but they returned to classes. No difference in monthly reported health problems with exercisers and controls. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated randomisation list drawn up by statistician, blinded to study participants and their characteristics, randomly allocated participants into 4 groups. |
| Allocation concealment (selection bias) | Low risk | Statistician, blinded to study participants and their characteristics, randomly allocated participants into 4 groups |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat and per protocol analysis |
| Selective reporting (reporting bias) | Low risk | All main outcome measures reported on |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | Low risk | Statistics reported groups equivalent at baseline |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | Low risk | Immediately post intervention data, and follow‐up data at 1 year post intervention reported |
Kim 2009a.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 52 completed study Losses: not reported Age: mean age 78 years Sex: 22 men, 30 women Residential status of participants: assisted living facilities (assumed community dwellers) Health status as defined by authors: healthy but fall prone Setting: Korea Inclusion: Berg Balance Scale < 44, Frenchay IADL < 36, PFS < 20, MMSE > 24, good visual acuity, no neurological or orthopaedic problems preventing activity. Self report of at least one fall in previous year. Exclusion: MMSE < 20; inability to complete 12 weeks exercise, previous training in any form of Tai Chi or current exercise programme, unable to walk independently. |
|
| Interventions | EXERCISE GROUP (3D) (n = 25): 12 forms of Tai Chi CONTROL GROUP (n = 27): 1 hour weekly 12 weeks health education lectures. Duration and intensity: 1 hour, 3 x week for 12 weeks Supervisor: Certified Tai Chi Grand Master and 3 assistants Supervision: group Setting: gym | |
| Outcomes | Force platform Obstacle crossing A‐P displacement (cm) Force platform Obstacle crossing M‐L displacement (cm) Compliance/adherence: not reported Adverse events: No adverse events reported. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation mentioned but insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | ‘As‐treated’ analysis done, drop outs existed but no detail reported |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Krebs 1998.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 132
Losses: 12 of 132 ‐ reports 'similar' drop‐outs in each group N = 132 Age: mean 74.3 years Sex: 31 men, 89 women. Health Status defined by authors: no medical contraindications to exercise, functionally limited Residential Status of participants: Community Dwelling Setting: USA Inclusion: Community dwelling, 60 years plus, reported one or more functional limitations on SF36 physical function scale, no medical history contraindicating exercise, no current rehab. Exclusion: |
|
| Interventions | EXERCISE GROUP (STRENGTH): (n = 54) strong for life programme, 35 minute video of 11 exercises, resistance elastic bands, functional movement patterns simulate to PNF, arms and legs, therapists supervised 2 home visits then telephone contact. CONTROL GROUP: (n = 66) usual activity. Duration and intensity: 6 months Supervisor: therapist Supervision: self and therapist (therapists supervised 2 home visits then telephone contact). Setting: home | |
| Outcomes | Gait velocity (cm/s) Compliance/adherence: Compliance 78% Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear, insufficient reporting to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Withdrawals described, analysis not possible |
| Selective reporting (reporting bias) | Low risk | All main outcome measures addressed |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Assessors blinded. Small but moderate chance of unblinding |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
Latham 2003.
| Methods | Type of study:RCT | |
| Participants | Number of participants randomised: 243 Losses:21 Age: 79.1 ‐/+ 6.9 Sex: 129 women, 114M Health status as defined by authors: frail Residential status of participants: mixed ‐ inpatient and outpatient Setting: New Zealand and Australia Inclusion: aged 65 or over; frail; no clear indication or contraindication to either of the study treatments Exclusion: not trial; treatment considered potentially hazardous; poor prognosis i.e. unlikely to survive 6 months; severe cognitive impairment; scores less than 20 on a 30 point MMSE; physical limitations that could limit adherence to the exercise program; not fluent in English |
|
| Interventions | EXERCISE GROUP (STRENGTH): high intensity quadriceps exercise program using adjustable ankle cuff weights ‐ (warm‐up stretches followed by knee extension repetitions CONTROL GROUP: telephone calls or visits where general health discussed and advice re recovery/problems Duration and intensity: three times per week over 10 weeks Supervisor: experienced physiotherapist Supervision: weekly phone call or visit Setting: first two sessions in hospital and then at home | |
| Outcomes | Berg Balance Scale (0 to 56 scale) TUG (s) Time taken to walk 4 metres (s) Compliance/Adherence: 82% of prescribed exercise sessions (mean 24.6 of 30 sessions) Adverse events: not reported |
|
| Notes | Insufficient data presented for meta‐analysis (non‐parametric data presented). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer central randomisation scheme ‐ stratified block |
| Allocation concealment (selection bias) | Low risk | Only biostatistician aware of allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis ‐ withdrawals described and accounted for |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Reported |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | Low risk | Follow‐up 6 months post randomisation i.e. approximately 3 or 4 months after the 10 week exercise intervention. |
Lin 2007.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 150 Losses: 25 Age: 76.8 mean age Sex: 49% men. Health status defined by authors: aged 65 or over and had suffered an injury as a result of a fall in the past 4 weeks Residential status of participants: community Setting: Taiwan Inclusion: residents aged 65 and over who has required medical attention due to a fall in the previous 4 weeks. Exclusion: none stated |
|
| Interventions | EXERCISE GROUP (MULTIPLE) (n = 50 ): stretching, strengthening and balance training exercises. An individualised exercise program was given by a physio and individuals were asked to do this 3x week. The programme was checked every 2 weeks during a home visit. Stretching as of major joints of body; strengthening of the legs and trunk muscles and balance (sit to stand, single leg and tandem standing backward and sideways walking and turning 360) Home Safety Assessment and Modification group (n = 50) a visit every 2 weeks of 30‐40 mins. List of specially recommended modifications of the individuals home environmental hazards provided. 14 inexpensive modifications designed for study were completed in first week. CONTROL GROUP (n = 50): Education with social visit to persons home every 2 weeks for 30‐40 mins with leaflets provided on balance stretching strengthening and home environmental improvements. Duration and intensity: 4 month study with a home visit every 2 weeks lasting for 30‐40 mins for each group Supervisor: Physio supervised exercise and public health workers supervised the other groups Supervision: as above individual supervision Setting: individuals own home and assessments in home |
|
| Outcomes | Tinetti balance scores (score 0 to 26) Functional reach (cm) Compliance/adherence: not reported Adverse events:not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Used mixed linear models which account for missing data and reported characteristics of missing subjects. However the mean values reported are of the subjects they could measure data on. No significant differences in baseline characteristics were observed between drop‐outs of any group. |
| Selective reporting (reporting bias) | Low risk | Main outcome measures reported on |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Reported |
| Were the treatment and control group comparable at entry? | Low risk | No difference between groups apart from alcohol use. |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | Low risk | 2 and 4 months after the 4 month intervention ended |
Liu‐Ambrose 2008.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 74 Losses:14/38 from control and 8/36 from exp group Age: aged 70 and older Sex: 22 women and 9 men in experimental and 19 women and 9 men in control Health status as defined by authors: At risk of falls Residential status of participants:community dwellers Setting: Vancover, Canada Inclusion:aged 70 or older; referred to and attended a dedicated falls clinic; had fallen and at risk of further falls; had one of the following criteria 1. one additional nonsyncopal fall in the previous year for those whose index fall was suspected to have been due to carotid sinus syndrome 2. A TUG test time of greater than 15 seconds 3. A Physiological Profile assessment (PPA) z‐score of 1 or greater; able to walk at least 3 metres. Exclusion:progressive neurological condition; life expectancy of less than 12 months; MMSE score less than 24 |
|
| Interventions | EXERCISE GROUP (MULTIPLE): (N=36) Home based Otago Exercise programme CONTROL GROUP: (N=38) usual care through clinics. Assumed no exercise. Duration and intensity: 30 mins OEP exercise 3 times a week and walk twice per week, over 6 months Supervisor: 2 physiotherapists Supervision: initial home visit then 3 additional visits (every other week) then final visit at 6 months Setting: Participants homes | |
| Outcomes | Timed‐Up and Go test (s) Postural Sway (mm) Compliance/Adherence: Twenty‐five percent (7/28) of all participants completed the exercise program three or more, 57% (16/28) two or more times per week, and 68% (19/28) at least once per week. From data extracted from geriatricians notes at 6 months and 1 year, no participants in control group took up recommendations to exercise. Adverse Events:Two participants in the OEP group reported low back pain associated with the exercises. One resumed exercising, and the other discontinued the exercises. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated three strata (sex; falls which necessitated visit to emergency dept; falls clinic physician) in blocks of 6 |
| Allocation concealment (selection bias) | Low risk | Allocation held externally and remotely |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All analyses were 'full analysis set' |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | Well reported paper |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | All assessments and telephone interviews |
| Were the treatment and control group comparable at entry? | High risk | Baseline characteristics of groups were significantly different for postural sway and TUG. |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Logghe 2009.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 269 Losses: 26 (12 in the intervention and 14 in the control) Age: mean 77 years Sex: 71% women Residential status of participants: community dwelling Health status as defined by authors: healthy but at risk of falling Setting: Netherlands Inclusion: age 70 and over, community dwelling, high fall risk (1 or more self reported falls in previous year, or at least 2 self reported risk factors: disturbed balance, mobility problems, dizziness use of benzodiazepines or diuretics) Exclusion: |
|
| Interventions | EXERCISE GROUP (3D) (n = 138): Tai Chi derived from Yang style CONTROL GROUP (n = 131): usual activity Duration and intensity: 1hr 2x week for 13 weeks Supervisor: 4 Professional Tai Chi instructors Supervision: group and unsupervised at home (2 x week for 15 minutes) Setting: community | |
| Outcomes | Berg Balance Scale (0 to 56 points) Compliance/adherence: 47% attended at least 21 (80%) of sessions Adverse events: No adverse events reported. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Independent pre‐stratified block randomisation (sex and falls) |
| Allocation concealment (selection bias) | Low risk | Assessors blinded and independent, GPs not told allocation, statistical analysis blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Participants were analysed in the group to which they were assigned |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Blind assessor |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention except "Living alone" status. |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | Low risk | At immediately post intervention (3 months), 6 months, 1 year follow‐up |
Lord 1995.
| Methods | Type of study: RCT. | |
| Participants | Number of participants randomised: 197
Losses: 25 from exercise group and 21 from control group N = 197. Age: 60 to 85 years mean (SD) 71.6 (5.4) Sex: females Health status defined by authors: healthy Residential status of participants: community Setting: Australia Inclusion: 60 years plus in community dwelling. Exclusion: not living at dwelling of time of study, little English. |
|
| Interventions | EXERCISE GROUP (MULTIPLE): (N = 100) improving strength, flexibility, co‐ordination, and balance, the individualised exercise regimes were based on participant's falls risk profile. CONTROL GROUP: (N = 97) no information assumed usual activity Duration and intensity: sessions 1 hour 2 x week for 12 months Supervisor: accredited fitness instructor Supervision: group Setting: community | |
| Outcomes | Postural sway eyes open and eyes closed on floor and foam (cm) (Lord sway meter)
Maximal balance range (cm)
Co‐ordinated stability test (errors) Compliance/adherence: mean 73.2% across the groups Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants drawn from a health insurance database and randomised in matched blocks n = 20 |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Withdrawals described but analysis not possible |
| Selective reporting (reporting bias) | Low risk | Main outcome measures addressed |
| Other bias | Unclear risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Assessors blinded |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
Lord 2003.
| Methods | Type of study: cluster RCT (20 clusters; 7 self care and 3 intermediate care exercise clusters and 7 self care and 3 intermediate care control clusters). | |
| Participants | Number of participants randomised: 551 factorial design Losses: 21 from intervention group 22 from control N = 551 Age: range 62‐95 mean (sd) 79.5 (6.4) years Sex: 77 men, 474 women Health Status defined by authors: mixed healthy and frail Residential Status: Retirement Village Setting: Australia Inclusion: living in retirement village, Exclusion: mini mental score < 20, mental condition involving neuromuscular, skeletal, or cardiovascular system, in hospital or not present at the time of recruitment, already attending exercise class of equivalent intensity |
|
| Interventions | EXERCISE GROUP (MULTIPLE): (N = 280) warm‐up period, conditioning period including aerobic exercises, specific strengthening exercises, and activities for balance, hand‐eye and foot‐eye coordination, and flexibility. CONTROL GROUP 1: (N = 290) Took part in a flexibility and relaxation program. CONTROL GROUP 2: (N = 181) No input assumed usual activity Duration and intensity: exercise group and control group 1: sessions 1 hour twice a week for 12 months. Supervisor: exercise group: trained instructor, control group 1 ‐ yoga instructor. Supervision: group Setting: community | |
| Outcomes | Postural sway on floor and foam eyes open and eyes closed (mm) (Lord sway meter)
Co‐ordinated stability test (errors).
Maximum balance range (cm) Compliance/adherence: not reported Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was stratified by accommodation status (self care or intermediate care) and cluster size. There were 20 clusters; 7 self care and 3 intermediate care exercise clusters and 7 self care and 3 intermediate care control clusters |
| Allocation concealment (selection bias) | Low risk | Blinded person organising randomisation not involved in rest of trial |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All addressed |
| Selective reporting (reporting bias) | Low risk | All main outcome measures reported |
| Other bias | High risk | Failure to adjust for clustering |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | High risk | Not blinded |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
Lord 2005.
| Methods | Type of study: RCT. | |
| Participants | Number of participants randomised: 620
Losses: at six month assessment losses n = 41 for exercise group 35 from minimal, 26 from control at 12 month follow‐up n = 18 exercise, n = 17 minimal, n = 7 control N = 620 Age: 75 to 98, mean (SD) 80.4 (4.5). Sex: females 409, males 211. Health Status defined by authors: mixed healthy and frail Residential Status of participants: Community Setting: Australia Inclusion: 75 years plus, community living Exclusion: minimal English language skills, blind, Parkinson, short portable mini mental test less than 7, and not considered risk of falling. |
|
| Interventions | EXERCISE GROUP (MULTIPLE): (n = 210) based on falls risk profile, individualised exercises aimed at improving strength, and balance and or vision if a problem, peripheral warm up, conditioning, strength, flexibility, coordination and balance. Minimal intervention group: (n = 206) instruction sheets for home exercise. CONTROL GROUP: (n = 204) usual activity Duration and intensity: sessions 1 hour x 2 week for 12 months (only data for initial 6 months reported) Supervisor: trained supervisor Supervision: group Setting: community | |
| Outcomes | Postural sway on floor and foam eyes open and eyes closed (mm) (Lord sway meter)
Co‐ordinated stability test (errors) Compliance/adherence: Compliance with exercise: median 21 of 78. Adverse events: not reported |
|
| Notes | Three arms to this study: we have reported the enhanced intervention group only data on balance outcomes for initial 6 months reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised in matched blocks using concealed allocation drawing lots |
| Allocation concealment (selection bias) | Low risk | Yes adequately concealed |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | Main outcome measures reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Assessors blinded |
| Were the treatment and control group comparable at entry? | High risk | Small differences in number and fear of falling |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
MacRae 1994.
| Methods | Type of Study: cluster RCT (exercise = 4 clusters, attention control = 4 clusters). | |
| Participants | Number of participants randomised: 80
Losses: 14 from exercise group and 7 from control group N = 80 Age: exercise group ‐ mean 72.4, control group ‐ mean 70. Sex: females Health Status defined by authors: mixed healthy and frail Residential Status of participants: Community Setting: USA Inclusion: medical clearance, 60 years plus attending a senior centre. Exclusion: physicians advice. |
|
| Interventions | EXERCISE GROUP (MULTIPLE): (n = 42) stand up/step up routine designed to improve strength and balance with warm up and cool down. CONTROL GROUP: (n = 38) attention control group Duration and intensity: exercise group ‐ 1 hour sessions 3 days a week for 12 months, control group ‐ one hour weekly for 12 months. Supervisor: exercise instructor Supervision: group Setting: gym | |
| Outcomes | Single legged stance (s)
Self paced gait velocity (m/s) Compliance/adherence : not reported Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised by senior centre but method of randomisation not stated |
| Allocation concealment (selection bias) | Low risk | Yes adequately concealed |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Not addressed |
| Selective reporting (reporting bias) | Unclear risk | Insufficient reporting to permit judgement |
| Other bias | High risk | Failure to adjust for clustering |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Assessors blinded |
| Were the treatment and control group comparable at entry? | High risk | Significant differences, control better balance and ankle strength. |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
McGarry 2001.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 22
Loss: not stated N = 22 Age: mean 74.77 (range 60 to 87) years Sex: 16 women, 6 males Health Status defined by authors: healthy Residential Status of participants: community dwelling Setting: USA Inclusion: not stated Exclusion: not stated |
|
| Interventions | EXERCISE GROUP (GBFT): (N = 12) "Get off your Rocker" balance class, including single leg stance, Swiss ball, tandem walking. CONTROL GROUP: (N = 10) usual activity. Duration and intensity: 3 sessions per week for 6 weeks. Supervisor: physical therapist Supervision: group Setting: ?gym | |
| Outcomes | Berg Balance Scale (0 to 56 points)
FRT (cm)
TUG (s) Compliance/adherence : not reported Adverse events: not reported |
|
| Notes | Abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear, insufficient reporting to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | Unclear risk | No data reported for comparison |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
McMurdo 1993.
| Methods | Type of study: Cluster RCT (exercise = 2 clusters, reminiscence therapy = 2 clusters) | |
| Participants | Number of participants randomised: 49
Losses: 5 from exercise group and 3 from control group N = 49 Age: mean 81 (range 64 to 91) years. Sex: 33 females, 8 males. Health status defined by authors: frail Resisdential status of participants: old peoples home Setting: UK Inclusion: in residential care Exclusion: residents with severe communication difficulties. |
|
| Interventions | EXERCISE GROUP (MULTIPLE): (n = 20) All exercises were performed seated. Warm‐up, exercises designed to put joints in upper and lower limbs through their full range of movements. As the study progressed participants were encouraged to sustain muscle contractions for longer and increase number of repetitions. CONTROL GROUP: (n = 24) attended reminiscence sessions Duration and intensity: exercise group ‐ 45 minutes twice weekly for six months, control group ‐ for 45 minutes twice weekly for 6 months. Supervisor: not stated. Supervision: group Setting: residential home | |
| Outcomes | Postural sway ‐ eyes open and eyes closed (Wrights ataxiameter) Compliance/adherence: mean 91% exercise sessions Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised homes by sealed envelopes based on computer generated numbers, participants allocated in blocks of 4 by gender and age (70‐79 and 80+) |
| Allocation concealment (selection bias) | Unclear risk | Unclear, insufficient reporting to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Withdrawals described, analysis not possible |
| Selective reporting (reporting bias) | High risk | Inadequate description of all measures |
| Other bias | High risk | Failure to adjust for clustering |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | High risk | Assessors not blinded. |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
Morris 1999.
| Methods | Type of study: cluster RCT (6 clusters, Fit for Life exercise = 2 clusters, self care for seniors = 2 clusters, control = 2 clusters). Homes matched in triplets based on reviewing 40 most recent minimum data set resident assessments. | |
| Participants | Number of participants randomised: 468 Losses: Control 31, exercise 18, nursing rehabilitation 27 Age: 84.7 Sex: 79% women. Health status as defined by authors:not defined Residential status of participants:long stay nursing beds Setting: USA Inclusion: all residents in long stay beds Exclusion:a terminal prognosis, projected length of stay greater than 90 days or health complications that prohibited contact. |
|
| Interventions | EXERCISE GROUP (STRENGTH) (n = 142): progressive resistance training of upper and lower limbs CONTROL GROUP (n = 155): usual activities Duration and intensity: 10 months Supervisor:specially trained staff Supervision:group Setting: institutional | |
| Outcomes | Time able to stand normally in 5‐feet positions (s) Compliance/Adherence: not reported Adverse events:not reported |
|
| Notes | Data not reported appropriately for analysis purposes. Also a third group was included 'self care for seniors'. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Reported that homes were matched in triplets and in each triplet one home was randomly assigned to one of three groups. method of randomisation not stated. |
| Allocation concealment (selection bias) | High risk | Not possible as allocation by home |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | High risk | Failure to adjust for clustering |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | All blind to allocation status |
| Were the treatment and control group comparable at entry? | Unclear risk | Insufficient information to permit judgement |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
Nelson 2004.
| Methods | Type of Study: RCT. | |
| Participants | Number of participants randomised: 72
Losses: 2 from control group N = 72 Age: over 70 years Sex: 27 women Health status defined by authors: healthy Residential status of participants: community dwelling Setting: USA Inclusion: > 70 exercising no more than 1 day/week community dwelling must have 2 functional limitations and score 10 or less on EPESE. Exclusion: Unstable cardiovascular disease, psychiatric disorders, neurological or muscular diseases, terminal illness, cognitive impairment. |
|
| Interventions | EXERCISE GROUP (MULTIPLE): (N = 34) balance and strength using free weights working at 7/8 on a 10 point Borg Scale, tandem walks, running etc, plus 120 minutes physical activity per week CONTROL GROUP: (N = 38) attention via nutritional education booklet. Duration and intensity: exercise programme ‐ 3 times a week for 6 months plus 120 minutes physical activity per week. Supervisor: exercise physiologist Supervision: exercise group ‐ individual self paced, 6 home visits in the 1st month and then monthly, attention control ‐ 2 home visits in 1st month and then monthly. Setting: home. | |
| Outcomes | Tandem walk (over 20 feet) (s).
Single legged stance (max 30 s).
Maximum gait speed (over 2 m) Compliance/adherence: mean 82%. Adverse events 1 fell in exercise group and 1 food poisoning in control group. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified block randomisation by gender and age (70 to 79 and 80+) |
| Allocation concealment (selection bias) | Low risk | Yes, adequately |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Withdrawals described analysis not possible |
| Selective reporting (reporting bias) | Low risk | Main outcome measures described |
| Other bias | Unclear risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Assessors blinded |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
Okumiya 1996.
| Methods | Type of study: RCT. | |
| Participants | Number of participants randomised: 42
Losses: none N = 42 Age: 75 to 87 years, mean 79 Sex: 18 males, 24 females. Health Status defined by authors: healthy Residential Status of participants: Community Setting: Japan. Inclusion: 75 years and over. Exclusion: evidence of coronary artery disease or severe obstructive airways. |
|
| Interventions | EXERCISE GROUP (MULTIPLE): (N = 21) warm up, light aerobic exercise, exercises aimed at improving neuromotor co‐ordination, and muscle‐strengthening exercises, cool down. CONTROL GROUP: (N = 21) usual activity. Duration and intensity: exercise group ‐ 60 minute session twice a week for 24 weeks. Supervisor: one physical educator, one medical doctor, and 5 nurses. Supervision: group Setting: community | |
| Outcomes | TUG (s)
Functional Reach Test (cm) Compliance/adherence: mean 86% (59 to 100%) Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear, insufficient reporting to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Withdrawals described, analysis not possible |
| Selective reporting (reporting bias) | Low risk | Main outcomes measures adequately reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Assessors blinded |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
Paillard 2004.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 21
Losses: not stated. N = 21 Age: 63 to 72 years Sex: males Health status as defined by authors: healthy Residential status of participants: community Setting: France Inclusion: active in physical exercise 3 hours per week, good condition for their age. Exclusion: medical contra indications. |
|
| Interventions | EXERCISE GROUP (WALKING): (n = 11) individual walking programme determined by lactate levels during VO2 max test CONTROL GROUP (n = 10): usual activities Duration and intensity: 45 to 60 minutes x 5 times a week x 12 weeks. Supervisor: not stated. Supervision: self. Setting: home. | |
| Outcomes | Force platform ‐ dynamic test, lateral and AP. Compliance/adherence : not reported Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient reporting to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Not stated |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Outcomes immediately post intervention only with no follow‐up |
Park 2008.
| Methods | Type of study: RCT after age‐matching | |
| Participants | Number of participants randomised: 50
Losses: 5 of 50 (3 exercise gp and 2 control gp)
Age: over 65 years. Exercise Gp 68.4 (3.4) yrs; Control Gp 68.3 (3.6) yrs.
Sex: Females. Health status as defined by authors: healthy Residential status of participants: community dwelling Setting: Korea. Inclusion: over 65 years old, community dwelling, women and ambulatory. Exclusion: <5 yrs postmenopause, chronic diseases or medications affecting bone mineral density or metabolism, obese, physically active >7 hrs per week. |
|
| Interventions | EXERCISE GROUP (MULTIPLE): (n = 25) stretching, strength training, aerobic weight bearing and balance exercises. CONTROL GROUP (n = 25): usual activities Duration and intensity: 48 weeks, 3 times 1 hour per week Supervisor: not stated. Supervision: group exercise sessions. Setting: community centre. | |
| Outcomes | Body Sway (measured by Dynamic Posturography) measurements: mean length (cm) mean length/time (cm/s) mean of deviation of mean X and mean Y) (cm) Eyes open one legged single stance (EOLST) (s) 10 meter maximal walk time (10MWT) (s) Compliance/adherence: not reported Adverse events: not reported |
|
| Notes | Other comments: Also assessed bone mineral density, % body fat, VO2 max and falls experience. Data not presented for control group for Single legged stance or 10 metre walk test. Body sway (mean of LNG) was used in analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Pairs age matched and then randomised into groups using computer generated randomised number table |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data for losses was substituted |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention except for bone mineral density |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
Ramirez Villada 2007.
| Methods | Type of study: RCT of two groups of men | |
| Participants | Number of participants randomised:93 Losses: 33 Age: mean 69.2 (5.1) Sex: 45 men in exp group; 48 men in control (another control group of 45 women) Health status as defined by authors: healthy Residential status of participants: community dwelling Setting:Cordoba, Spain Inclusion: healthy and physically active, with a practical activity. Regular physical least 2 times a week (walk, fitness gym, dance) not less than one year. Exclusion: deformity of the spine, upper limb or less, amputations, sequelae of fractures, prosthesis, steroid treatment, disease cardiovascular and joint conditions. |
|
| Interventions | EXERCISE GROUP (MULTIPLE): continuous vertical and horizontal jumping CONTROL GROUP: not clear from translation Duration and intensity: two training sessions per week for 22 weeks (with sessions separated by 2 to 3 days and duration per session of 50 to 60 minutes, including warm up and cool down) Supervisor: not clear from translation Supervision: not clear from translation Setting: not clear from translation | |
| Outcomes | Backward tandem walk test over 6 metres (s) Compliance/adherence: not clear from translation Adverse events: not clear from translation |
|
| Notes | Data presented in graphical form as point estimates only. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | Unclear risk | Insufficient information to permit judgement |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Ramsbottom 2004.
| Methods | Type of study: RCT. | |
| Participants | Number of participants randomised: 22
Losses: 7 of 22 (1 for a fall, 2 arthritis and 1 illness, 1 stomach ulcer, 2 noncompliance: 3 from treatment and 4 from control) N = 22 Age: over 70 years. Sex: 7 males, 15 females. Health status as defined by authors: sedentary Residential status of participants: community dwelling Setting: UK. Inclusion: Normal, sedentary over 70 years, community dwelling. Exclusion: risk of taking PRE, physically active. |
|
| Interventions | EXERCISE GROUP (MULTIPLE): (n = 11) free weights to strengthen and develop power in shoulder, hip adductors/abductors/flexors/extensors, knee flexor/extensors, increasing in repetitions, functional mobility, stretching and balance exercises. CONTROL GROUP: (n = 10) usual activities. Duration and intensity: 2 x a week for 24 weeks. Supervisor: keep fit association registered teacher. Supervision: group. Setting: community. | |
| Outcomes | Postural sway on BPM
TUG (s)
FRT (cm) Compliance/adherence : mean (SD) 43 (3) classes (max 48) Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised by random number tables |
| Allocation concealment (selection bias) | High risk | Individuals were informed of group allocation and assessors were not blind to group allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | Insufficient reporting to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | High risk | Assessors not blinded |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Outcomes immediately post intervention only with no follow‐up |
Reinsch 1992.
| Methods | Type of study: cluster RCT (16 clusters, exercise = 4 clusters, cognitive behavioural = 4 clusters, exercise‐cognitive = 4 clusters, discussion = 4 clusters) | |
| Participants | Number of participants randomised = 230 to 4 arms of study
Losses: 46 of 230 (exercise = 13, cognitive 14, exercise‐cognitive = 11, control = 8). N = 230. Age: 60 years plus. Sex: 185 women, 45 men. Health status as defined by authors: not stated Residential status of participants: community dwelling Setting: USA. Inclusion: 60 years and over, attending senior centres (n = 16). Exclusion: none reported. |
|
| Interventions | EXERCISE GROUP (GBFT): (n = 57) stand up and step ups functional exercises. CONTROL GROUP: (n = 50) discussion. Duration and intensity: both groups 1 hour, 3 times per week for 12 months. Supervisor: college students. Supervision: group Setting: community in senior centres. | |
| Outcomes | Single legged stance (s) Compliance/adherence : not reported Adverse events: 38.6% of participants had a fall only 7.8% needing medical attention, no differences in time to fall between groups |
|
| Notes | Trial had 4 arms: others included CBT only, exercise plus CBT. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised by senior centre (n clusters = 16) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient reporting to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | Insufficient reporting to permit judgement |
| Other bias | High risk | Failure to adjust for clustering |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient reporting to permit judgement |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Outcomes immediately post intervention only with no follow‐up |
Rooks 1997a.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised = 131 Losses: 25 of 131 (strength group = 3, walking group = 15, control group = 7). N = 131. Age: 65 to 95 years. Sex: % women = 59 resistance group, 52 walking group, 82 control group. Health status as defined by authors: healthy Residential status of participants: community dwelling Setting: USA Inclusion: 65 years plus, climb a flight of stairs, participate in regular activities outside home a minimum 2 x week, transport to community centre. Exclusion: use of medication comprising safety or ability to complete study, uncontrolled or unstable chronic conditions. |
|
| Interventions | EXERCISE GROUP (STRENGTH): (n = 40) stair climbing with resistance, seated knee extension, standing, standing knee extension. EXERCISE GROUP (WALKING): (n = 40) walking own pace on level ground. CONTROL GROUP: (n = 51) on a waiting list for exercise programme. Duration and intensity: resistance training group and walking group ‐ 1 hour, 3 times per week for 10 months. Supervisor: research assistant. Supervision: group (5 to 6). Setting: community. | |
| Outcomes | Tandem stance (s).
Single legged stance ‐ eyes open and eyes closed (s).
Timed forward tandem walk (10 feet) Compliance/adherence : % Compliance resistance training group ‐ 85 (47 to 100), walking group ‐ 82 (29 to 97) Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomised by unbalanced 3 group block randomisation (due to expected higher attrition rate in control group every 13th volunteer was allocated to control group). One in 5 in the control group were not randomly assigned. |
| Allocation concealment (selection bias) | Unclear risk | Iinsufficient reporting to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | insufficient reporting to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | not possible |
| Blinding (assessor) | Unclear risk | insufficient reporting to permit judgement |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Outcomes immediately post intervention only with no follow‐up |
Rosendahl 2006.
| Methods | Type of study: RCT stratified cluster (34 clusters randomly assigned to exercise or control groups) 2x2 factorial model | |
| Participants | Number of participants randomised: 95 (191 to 4 groups ‐ see Notes) Losses: 7 at end of intervention and 9 at 6 months in exercise group; and 3 and 5 in control group Age: mean 85.5±5.5 years exercise group and 85.6±7.0 years control group Sex: 68 (71%) women Health status as defined by authors: dependent in ADL Residential status of participants: residential care Setting: Sweden Inclusion: 65 year and older, dependent on one person for at least 1 category of Katz, able to sit to stand with one person, MMSE ≥ 10, physicians approval. Exclusion: not reported |
|
| Interventions | EXERCISE GROUP (MULTIPLE): High intensity functional exercise, strength, balance, ADL (n = 45)
CONTROL GROUP: seen by an occupational therapist for seated activities, watching TV reading, etc. (n = 50) Duration and intensity: 29 sessions over 3 months, each session 45 minutes, delivered 5 times every 2 weeks Supervisor: physiotherapists Supervision: groups of 3 to 9 people Setting: residential care facilities |
|
| Outcomes | Berg Balance Scale (0 to 56 points) change score Gait speed (self paced) change score m/s Gait speed (maximum) change score m/s Adherence/compliance: reported as combined groups. 72% exercise plus exercise and supplement groups, and 70% control and control plus supplement group. Adverse effects: No adverse event during the sessions led to a manifest injury or disease. |
|
| Notes | Trial was composed of 4 groups: exercise versus control versus nutrition intervention versus exercise + nutrition. (The second 2 groups (96 participants in total) were not included in this review; however, Rosendahl 2006 reported that "No interaction effects were seen between the exercise and nutrition interventions.") | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | To reduce contamination by the exercise intervention, 34 clusters, comprising three to nine participants living on the same floor, wing, or unit, were randomly assigned to exercise or control activity. To minimise the risk of impact by factors associated with the facility, the randomisation was stratified in order to have both groups in each facility. |
| Allocation concealment (selection bias) | Low risk | Sealed non transparent envelopes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | Trial protocol published but retrospectively therefore insufficient information to permit judgement |
| Other bias | Low risk | Cluster effect was examined in additional analyses by adjusting the outcome regression analyses for clustering |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Trained physiotherapists blinded to group allocation and previous test results. |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | Low risk | Immediately post intervention and 3 months post intervention follow‐up data reported. |
Rubenstein 2000.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 59 Losses: up to 7 of 59 (actual number and groups not stated) N = 59. Age: mean (SD) 74.4 (43.4) ‐ control group, 76.4 (4.9) ‐ exercise group. Sex: men. Health status as defined by authors: frail Residential status of participants: Community dwelling Setting: USA. Inclusion: 70 years plus, lower extremity weakness, impaired gait, impaired balance, one fall in previous 6 months. Exclusion: regular exercises, severe cardiac or pulmonary disease, terminal illness, severe joint pain, dementia, medical unresponsive depression, progressive neurological disease. |
|
| Interventions | EXERCISE GROUP (MULTIPLE): (n = 31) PRE, hip, knee and ankle, endurance training bike, treadmill, indoor walking and balance training. CONTROL GROUP: (n = 28) usual activities. Duration and intensity: exercise group ‐ 90 minutes, 3 times per week x 12 weeks. Supervisor: exercise physiology students. Supervision: group. Setting: clinic. | |
| Outcomes | Single legged stance (s) (for max 15 s) Compliance/adherence : not reported Adverse events: not reported |
|
| Notes | SD 43.4 years for control group age, might be a typo in original paper | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly generated sequence of cards in sealed envelopes |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Data for completers only |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Assessors blinded. |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Outcomes immediately post intervention only with no follow‐up |
Salminen 2009.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 591 Losses: 66 (37 exercise, 29 control) Age: intervention: men 72 (69 to 76); women 72 (68 to 76); control: men 74 (70 to 77); women 71.5 (68 to 76) Sex: 86 men, 439 women Residential status of participants: community dwelling Health status as defined by authors: healthy Setting:Finland Inclusion:65 and over, at least one fall during last 12 months, MMSE ≥ 17, able to walk 10 m independently, community dwelling Exclusion: |
|
| Interventions | EXERCISE GROUP (GBFT) (n = 293): individual geriatric assessment, fall prevention, home hazard assessment, physical exercise (strengthening, balance, co‐ordination, stretching), lectures, psychosocial activity groups, home exercise. CONTROL GROUP (n = 298): Duration and intensity: 40‐50 mins every 2nd week 12 months (home exercises 3 x week). Supervisor: physical therapists Supervision: group Setting: clinic | |
| Outcomes | AP velocity (mm/s) in 3 different standing balance tests (eyes open; eyes closed and semitandem) ML velocity (mm/s) in 3 different standing balance tests (eyes open; eyes closed and semitandem) Berg Balance Scale (0 ‐ 56 points) Compliance/adherence: 64% men and 63% women completed all sessions 26% men and 38% women attended lectures, 22% men and 29% women attended psychosocial groups; 2.5 (2.2) men and 2.6 (2) women home exercise sessions per week Adverse events: No adverse events reported. |
|
| Notes | Insufficient data presented for meta‐analysis (non‐parametric data presented). Data reported separately for men and women. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation method not mentioned but consecutively numbered envelopes used |
| Allocation concealment (selection bias) | Low risk | Consecutively numbered envelopes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | High risk | Not blinded |
| Were the treatment and control group comparable at entry? | Low risk | NNo differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Outcomes immediately post intervention only with no follow‐up |
Sauvage 1992.
| Methods | Type of study: RCT. | |
| Participants | Number of participants randomised:14 Losses: 2 of 14 (no details given) N = 14 Age: mean (SD) exercise group ‐ 73.38 (4.04), control group ‐ 73.83 (4.74). Sex: men. Health status as defined by authors: deconditioned Residential status of participants: Veterans Nursing Home Setting: USA. Inclusion: Recruited from Veterans Nursing Home. Aged over 60 years, independently mobile, gait and balance difficulties (Tinetti score less than 30), lower extremity weakness. Exclusion: moderate to severe dementia, asymmetrical focal neurolic deficits, lower extremity amputation, leg length discrepancies, significant systemic disease. |
|
| Interventions | EXERCISE GROUP (MULTIPLE): (n = 8) PRE and aerobic conditioning (> 70% exercise stress tested maximal HR) using gym equipment and ergometers. CONTROL GROUP: (n = 6) usual activity. Duration and intensity: 45 to 75 minutes, 3 times per week x 12 weeks. Supervisor: not stated Supervision: group (3 to 4). Setting: Institutional. | |
| Outcomes | Average gait velocity (cm/s) over 20 feet. (right and left).
COP movement during quiet stance ‐ eyes open, eyes closed (mm). Compliance/adherence: Compliance 95% for exercise group Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Completers only |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Assessors blinded |
| Were the treatment and control group comparable at entry? | Unclear risk | Insufficient information to permit judgement |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Outcomes immediately post intervention only with no follow‐up |
Schilling 2009.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 19 Losses: none reported Age: 60 to 68 years Sex: 10 men, 9 women Residential status of participants: community dwelling Health status as defined by authors: healthy Setting: USA Inclusion: healthy with no orthopaedic limitations or vestibular problems, active but not partaking in structured exercise. Exclusion: |
|
| Interventions | EXERCISE GROUP (GBFT) (n = 10): standing balance training using VersaDisc and CorDisc devices adjustable air filled devices. progressively challenging CONTROL GROUP (n = 9): usual activities Duration and intensity: 15 to 30 min, 3 x week, 5 weeks Supervisor: Certified Strength and conditioning specialist. Supervision: Individual Setting: clinic | |
| Outcomes | TUG (s) Force plate, left leg and right leg, eyes open, eyes closed LOP (cm) Compliance/adherence: not reported Adverse events: No adverse events reported. |
|
| Notes | only TUG data reported, other data reported graphically only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation mentioned but Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | ‘As‐treated’ analysis done, unclear whether drop outs existed but no detail reported |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | Unclear risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | Unclear risk | Insufficient information to permit judgement |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Schlicht 2001.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 24 (12 in control and 12 in intervention) Losses: 2, 1 from each group Age: 61 to 87 years Sex: 14 women, 10 men Health status as defined by authors:healthy Residential status of participants: community dwelling Setting: USA Inclusion: 60 years and above, moderately active Exclusion: dependent living status, involvement in strength training or physiological disorders preventing exercise, vestibular disorders |
|
| Interventions | EXERCISE GROUP (STRENGTH): (N = 12) Progressive resistance training for leg flexion and extension, hip ab/adduction/extension, ankle extension 75% 1 RM (repetition maximum) CONTROL GROUP: (N = 12) assumed usual activity Duration and intensity: 3 x per week, 8 week Supervisor: not stated Supervision: group Setting: community | |
| Outcomes | Max gait velocity over 25 feet (m/s) one leg stance eyes closed (s) Compliance/adherence: 99% Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | Unclear risk | Insufficient information to permit judgement |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
Schoenfelder 2000.
| Methods | Type of study:RCT | |
| Participants | Number of participants randomised: 16 Losses: none immediately post intervention, 2 at 6 month follow‐up Age: mean 82.8 (65‐95) Sex: 12 females, 4 males Health status as defined by authors: healthy Residential status of participants: nursing homes Setting: USA Inclusion:over 65 years, able to ambulate, speak English score 20 or over on MMSE Exclusion: unstable physical condition, evidence of terminal illness, history of abusive behaviour |
|
| Interventions | EXERCISE GROUP (GPA ‐ walking): (n = 9) ankle strengthening exercises and walking programme of 10 minutes sustained walking CONTROL GROUP: (n = 7) assumed usual activity Duration and intensity: 20 min sessions, 3 x per week for 3 months, low intensity Supervisor: researcher Supervision:individual Setting:nursing home | |
| Outcomes | parallel stance (s) semi‐tandem stance (s) tandem stance (s) 6 metre walk test (s) Complaince/Adherence: exercise programme was well received and tolerated Adverse events: exercise well tolerated by participants. Number of falls. Control group: 6 during intervention period (3 months) and 6 in 3 month follow‐up period. Exercise group 22 during intervention period (3 months) and 20 in 3 month follow‐up period. |
|
| Notes | Means but no SDs presented. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants matched in pairs based on falls assessment then randomly assigned within each pair |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Completer analysis |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | Low risk | Immediately post intervention and 6 month follow‐up |
Schoenfelder 2004.
| Methods | Type of study: RCT. | |
| Participants | Number of participants randomised: 81
Losses: At 3 months, exercise n = 9, control n = 6; at 6 months, exercise n = 3, control n = 5 N = 81 Age: 64 ‐ 100 years, mean 84.1. Sex: 62 women, 19 men. Health Status defined by authors: frail Residential status of participants: nursing home Setting: USA. Inclusion: Recruited from nursing homes, 65 years and over, independent ambulators, English speakers, scored 20 plus on MMSE. Exclusion: unstable physical conditions. |
|
| Interventions | EXERCISE GROUP (MULTIPLE): (N = 42) strength and endurance training plus 10 minutes walking. CONTROL GROUP: (N = 39) attention placebo. Duration and intensity: exercise group ‐ 15 ‐20 minutes, 3 times per week x 3 months. Control group ‐ 30 minutes weekly x 3 months. Supervisor: student nurses. Supervision: individual. Setting: institutional. | |
| Outcomes | Parallel stance (max 10s) (s).
Semi tandem stance (max 10s) (s).
Tandem stance (max 10s) (s).
Walking speed over 6 metres (m/s). Compliance/adherence: not reported Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomisation not known (matched pairs by risk assessment for falls) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient reporting to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Not adequately addressed |
| Selective reporting (reporting bias) | Unclear risk | Insufficient reporting to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Assessors blinded. |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | Low risk | Follow‐up at 3 months post intervention |
Sherrington 2008a.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 173
Losses: 14 of 173 (8 exercise gp and 6 control gp) Age: Exercise Gp 73.4 (11.1) yrs; Control Gp 76.4 (10.2) yrs. Sex: Females n = 99 (57%) and males. Health status as defined by authors: frail Residential status of participants: community dwelling Setting: Australia. Inclusion: mobility impairment, unsuitability to join other group exercise. Exclusion: receiving other rehabilitation, severe respiratory or cardiac disease. |
|
| Interventions | EXERCISE GROUP (MULTIPLE): (n = 85) circuit style group exercises, sit to stand, walking over/around obstacles, stepping in different directions, heel raises, side steps onto blocks, step ups, side taps, treadmill or exercise bike. Moved stations every 3 to 4 minutes. Tailored to suit different levels of ability. Plus home exercises every week. CONTROL GROUP (n = 88): waiting list Duration and intensity: 5 weeks, 2 times 1 hour per week plus home exercise Supervisor: physiotherapist. Supervision: group exercise sessions. Setting: outpatient hospital rehabilitation gym. | |
| Outcomes | Step test (reps in 15 s) gait 6m walk test (m/s) semi tandem stand (s) tandem stand (s) Compliance/adherence: not reported but no registers of attendance were kept and no diaries for home exercise. Adverse events: No adverse events reported. |
|
| Notes | Also assessed muscle strength and sit to stand ability. Only 50% referred would take part in the study. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation method not stated |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered opaque sealed envelopes |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Intention‐to‐treat on those who came for follow‐up but no analysis of missing data. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | High risk | Reported as blind to baseline results but not to group allocation |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Shimada 2004.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 32
Losses: exercise n = 3, control n = 3 Age: 66 to 98 years Sex: 25 women, 7 men Health of participants defined by authors: frail Residential status of participants: residential care facility Setting: Japan Inclusion: ambulatory residents or attending a geriatric health facility, high risk for falls, decreased balance, gait and muscle strength Exclusion: unable to walk for 3 minutes at 0.5 km/hr, health problems or dementia |
|
| Interventions | EXERCISE GROUP (WALKING): (N = 18) gait training on a bilateral separated treadmill CONTROL GROUP: (N = 14) usual care Duration and intensity: 1 to 3 times per week for 6 months Supervisor: physiotherapist. Supervision: individual. Setting: institutional. | |
| Outcomes | Single legged stance (s).
FRT (cm).
Walking speed over 10 m (m/s) Compliance/adherence: not reported Adverse events: fall rate usual care 54.5% (number of falls = 11) and exercise group 33.3% (number of falls = 15). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables used |
| Allocation concealment (selection bias) | Unclear risk | Insufficient reporting to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No analysis on withdrawals |
| Selective reporting (reporting bias) | Unclear risk | Insufficient reporting to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | High risk | Assessors not blind |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only one month follow‐up |
Shin 2009.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 60 Losses: 12 (4 in exercise group, 8 in control) Age: 75 plus Sex: women Residential status of participants: community dwelling Health status as defined by authors: healthy Setting: Korea Inclusion: low income women, able to communicate without difficulties. Exclusion: |
|
| Interventions | EXERCISE GROUP (3D) (n = 30):rhythmic exercises to music, stretching, joint mobility, strengthening, and cardiopulmonary endurance. CONTROL GROUP (n = 30): wait list usual activity, Duration and intensity: 30‐50 mins 2 x week for 8 weeks (15 mins 1x week for first 4 weeks only) Supervisor:public health nurse, student nurses. Supervision:group Setting:clinic | |
| Outcomes | single leg stand eyes closed (s) Compliance/adherence: not reported Adverse events: No adverse events reported. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation mentioned but Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | ‘As‐treated’ analysis done, drop outs existed but no detail reported |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Not reported |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Sihvonen 2004.
| Methods | Type of study: RCT. | |
| Participants | Number of participants randomised: 28
Losses: exercise = 3; control = 3 N = 28 Age: mean (SD) 80.7 (6.1) ‐ exercise group, 82.9 (4.2) control group. Sex: women. Health of participants defined by authors: frail Residential status of participants: care home Setting: Finland. Inclusion: resident at two care homes, 70 years and over, able to stand and walk without walking aid. Exclusion: health problems. |
|
| Interventions | EXERCISE GROUP (GBFT): (N = 18) dynamic exercise on force platform and training device with visual feedback on movement on COP.
CONTROL GROUP: (N = 14) usual activity. Duration and intensity: 20 to 30 minutes session, 3 times per week for 4 weeks. Supervisor: not stated. Supervision: individual. Setting: institutional. |
|
| Outcomes | AP and ML velocities of sway and velocity moment in 6 standing balance tests.
Performance time and distance in 3 dynamic balance tests.
Berg Balance Scale (0 to 56 points) Compliance/adherence: not reported Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised in blocks by drawing of lots |
| Allocation concealment (selection bias) | Unclear risk | Insufficient reporting to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No, completers only |
| Selective reporting (reporting bias) | Unclear risk | Insufficient reporting to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | insufficient reporting to permit judgement |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
Skelton 1995.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 47 Losses: 5 before randomisation and 7 during study. N = 52 Age: 75 and over (Median of 79.5 in exercise with range 76 to 93 and median of 79.5 in control with range 75 to 90) Sex: women Health status as defined by authors: healthy; medically stable and living independently with no help required for washing cleaning or cooking and no help form external services. Residential status of participants: community dwellers Setting: UK Inclusion: women, over 75 years of age, living in community and response to health questionnaire indicated healthy and medically stable Exclusion: no recent history of cardiovascular, cerebrovascular, respiratory, systemic, muscular or uncontrolled metabolic disease or any impairment that interfered with mobility |
|
| Interventions | EXERCISE GROUP (STRENGTH): Progressive resistance strength training: 10 min warm‐up and stretch; 30 ‐ 40 minutes training session comprised of 3 sets of 4‐8 repetitions of each exercise using rice bags (1‐1.5kg) or elastic tubing for resistance; 10 minutes warm down. CONTROL GROUP: no exercise intervention and asked not to alter their usual exercise regime. Kept home exercise diaries and recorded any moderate strenuous activity. (guidelines given) Duration and intensity: 1 hour training session per week in medical centre and 2 hours unsupervised training sessions at home over 12 weeks. A home exercise diary was kept Supervisor: not stated Supervision: one hour per week at training session in medical school in groups of 4 to 6 people; two unsupervised home sessions (but supported by exercise tape and booklet) Setting: medical school and home sessions | |
| Outcomes | Functional reach (cm) Corridor walk over 118m. (HR and number of steps reach half way) Compliance/adherence :7 dropped out during study (4 exercisers and 3 controls) Adverse events: No adverse events reported. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Paired and matched for age and habitual physical activity. Randomly allocated using numbers table. |
| Allocation concealment (selection bias) | High risk | Participants, supervisor and assessors not blind |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Losses: 5 before randomisation and 7 during study. No adjustment made for losses. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported as per protocol |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | High risk | Assessor not blind |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | No follow‐up data reported |
Skelton 1996.
| Methods | Type of study: cross over RCT | |
| Participants | Number of participants randomised: 20 randomised in pairs Losses: Recruited 25; 5 could not manage class times due to other commitments; 20 were matched in pairs by age; 2 drop out (1 from 1TG and 1 from 2TG) but not because of exercises. 1 from the 1CG was excluded due to BP problems before baseline measures done. N = 20 Age: 74 years old or more (median 81 with range of 74 to 89) Sex: females Health status as defined by authors: frail Residential status of participants: community dwellers Setting: UK Inclusion: aged 75 or more having attended GP in recruitment period and having minor or major functional or mobility difficulties. Exclusion:any disease or condition that would be adversely affected by exercise |
|
| Interventions | EXERCISE GROUP (Strengthening):10 mins warm up and stretch; 30 to 40 mins strengthening exercises following progressive resistance protocol. Exercises performed in sets and repetitions; 10 mins cool down. Followed exercises prescribed for older people and active aging. (book referenced) CONTROL GROUP: asked to perform no more or less activity than usual Duration and intensity:over 8 weeks attended one supervised class session at physio gym/clinic and two sessions unsupervised at home. Supervisor: health care professional i.e. physiotherapist Supervision: one session/week at gym clinic; 2 sessions/week at home not supervised by other (exercise booklet and diary given to record sets and repetitions) Setting: home and also gym/clinic wherever physio worked. | |
| Outcomes | functional reach (cm) chair rise (s) TUG (s) 6.1 m walk (s) floor rise (s) one leg stance eyes open (s) one leg stance eyes closed (s) walk backwards (steps) Compliance/adherence:14 out of 19 exercises attended all classes and performed all home sessions; no one attended fewer than 6 classes and the diaries indicated that non one performed fewer than 11 home sessions. Adverse events: No adverse events reported. |
|
| Notes | (Our approach for cross‐over RCTs, data for the initial periods were included but it was deemed inappropriate (due to potential long lasting effects of the intervention) for the crossover data to be included.) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly allocated using numbers table. |
| Allocation concealment (selection bias) | High risk | Participants, supervisor and assessors not blind |
| Incomplete outcome data (attrition bias) All outcomes | High risk | completer analysis. Recruited 25; 5 could not manage class times due to other commitments; 20 were matched in pairs by age; 2 drop out (1 from 1TG and 1 from 2TG) but not because of exercises. 1 from the 1CG was excluded due to BP problems before baseline measures done |
| Selective reporting (reporting bias) | Low risk | All outcomes reported as per protocol |
| Other bias | High risk | Cross over study |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | High risk | Assessors not blind to group |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Suzuki 2004.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 52
Losses: 8 of 52; 6 month control = 2, exercise n = 6 N = 52 Sex: women Age: mean (SD) 77.31 (3.4) exercise, 78.64 (4.39) control Health of participants defined by authors: healthy Residential status of participants: community Setting: Japan Inclusion: 73‐90 years, participants in longitudinal study on aging. Exclusion: marked decline in ADL, hemiplegia, missing baseline data. |
|
| Interventions | EXERCISE GROUP (MULTIPLE): (n = 28) exercise centred falls prevention programme with home based exercise aimed at enhancing muscle strength, balance and gait. Included resistance exercise and Tai Chi. CONTROL GROUP: (n = 24) usual activity and a pamphlet and advice on falls prevention. Duration and intensity: 1 exercise session every 2 weeks for 6 months (10 hours). Supervisor: not stated. Supervision: group and self. Setting: community | |
| Outcomes | Single legged stance (s), eyes open (max 1 min), eyes closed (max 30 s) (s)
Walking speed (over 11 m) (m/s).
Tandem walk (over 2.5m) (steps) Compliance/adherence : not reported Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | insufficient reporting to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | insufficient reporting to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | insufficient reporting to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Assessors blinded. |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | Low risk | follow‐up at 8 months and 20 months |
Sykes 2004.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 40 Losses:13 (5 in exercise and 8 control) N = 40 Age: 80 +/‐ 4.5 years (Exercise group 79.5 +/‐ 3.6 : Control 80.8 +/‐ 7.3) Sex: 7 males, 20 females Health status as defined by authors: healthy Residential status of participants: community dwellers Setting: Hong Kong Inclusion:aged 75 years and older; ambulatory independent with or without aids for short distance of 20 metres; fell one or more times in previous 12 months Exclusion: terminal illness or severe dementia; nonambulatory status; amputations or severe arthritis problems; major impairment of sensorimotor function due to neurological disease; unstable cardiovascular or pulmonary conditions or diseases; episodes of unconsciousness reported in the past year; mini mental status examination (MMSE) score less than 23. |
|
| Interventions | EXERCISE GROUP (MULTIPLE): n = 20 Exercise session described as: 5 min warm up followed by leg strengthening exercises (using cuff weights and therabands and repetitions), Balance and Gait exercises (with progression) and 5 min cool down. CONTROL GROUP: n = 20 not reported assumed usual activity Duration and intensity: Introductory hour long class in centre with talk and demonstration of exercises. Then over the next 8 weeks : 45 minute daily exercise sessions at home 6 days a week and 30 minute walk twice a week. Daily activity diaries. Supervisor: physiotherapist Supervision: initial group session then phone calls weeks 1, 2, 4 and 6 Setting: initial class in centre then at home | |
| Outcomes | Berg Balance Scale (0 to 56 points) Time to get‐up and go (TUG) (s) Functional Reach (cm) Compliance/adherence: not reported Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Taaffe 1999.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 46 Losses:7 (5 in exercise and 2 control) N = 46 Age: 65 to 79 years Sex: 29 males, 17 females Health status as defined by authors: healthy Residential status of participants: community dwellers Setting: USA Inclusion: BMI < 30 Kg/m2 Exclusion: musculoskeletal disorders inhibiting exercise, participation in weight training in past 12 months |
|
| Interventions | EXERCISE GROUP (STRENGTH): high intensity progressive resistance training at 80% of 1 RM (repetition maximum) (repetition maximum) for upper and lower limbs. CONTROL GROUP: usual activity Duration and intensity: Ex1 = 1 day per week for 24 weeks, Ex2 = 2 days per week for 24 weeks, Ex3 = 3 days per week for 24 weeks Supervisor: not stated Supervision: group with direct supervision Setting: gym | |
| Outcomes | backward tandem walk over 6 m Compliance/adherence: similar across interventions Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Taylor‐Piliae 2010.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 132 Losses: 9 Tai Chi, 3 endurance, 5 control Age: 69 (± 5.8) years old (range = 60 to 84 years), Sex: % women (65% Tai Chi, 72% endurance, 73% control) Health status as defined by authors: healthy Residential status of participants: community dwelling Setting: USA Inclusion: 60 years or older, living within a reasonable commute to community exercise facilities, understanding the English language sufficiently to give study consent and follow intervention instructions, signed written consent, being sedentary (no regular exercise > 60 min/week), and being able to walk without assistive devices. Exclusion: major medical diagnoses that would interfere with participation in moderate‐intensity exercise, for example, myocardial infarction, cardiac surgery, or stroke in past 3 months; congestive heart failure, angina pectoris, serious cardiac arrhythmias, or blood pressure >160/100 mm Hg; or active treatment for cancer, alcoholism, recreational drug abuse, or severe cognitive impairment |
|
| Interventions | EXERCISE GROUP (3D) (n = 37): Participants were taught 12 postures of the Yang shortform style of Tai Chi. Provided with written instructions, illustrations of the postures, and a videotape for use during practice on home‐based exercise days. Daily practice was encouraged. EXERCISE GROUP (MULTIPLE) (n = 39) endurance, resistance/strength, and flexibility exercises. 8–10 min of warm‐up activities consisting of stretching, light callisthenics, and slow walking. Cardiorespiratory‐endurance activities lasting for 15–25 min consisting of more vigorous walking and callisthenics performed to music and then a session of both resistance/strength and flexibility exercises lasting 15–20 min. The resistance exercises included selected callisthenics and the use of light hand weights and rubber exercise bands. Home‐based exercise sessions included ≥30 min of walking and 10–25 min of resistance and flexibility exercises three times per week. CONTROL GROUP (n = 56): attention‐control group met once a week for approximately 90 min Duration and intensity: 45 mins, 3 per week classes 6 months with daily home exercise Supervisor: Gand Master, YMCA exercise instructor Supervision: group Setting: community |
|
| Outcomes | single‐leg‐stance (s) functional‐reach test (cm). Compliance/adherence:median adherence rate was highest in the Tai Chi group (77%), with slightly lower rates for the WE (68%) and control (67%) groups. Tai Chi group 75% of participants attended more than 66% of the class sessions, and 56% of WE participants attended 66% of prescribed classes Adverse events: No adverse events reported. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation mentioned but method not reported. Participants randomised in a disproportionate manner, with approximately 30% assigned to each of the two exercise groups and 40% to control |
| Allocation concealment (selection bias) | Unclear risk | Trained and certified staff obtained baseline and all follow‐up data and were blinded to participants’ group assignment. Method of concealment not reported. Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Losses noted but not accounted for in analysis. Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Trained and certified staff obtained baseline and all follow‐up data and were blinded to participants’ group assignment |
| Were the treatment and control group comparable at entry? | Low risk | No statistically significant differences between the groups at baseline, except for self‐reported history of angina |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data provided; follow‐up data only given for intervention group |
Topp 1993.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 63 Losses:7 (2 control, 5 exercise) Age: mean 71.1 Sex: 39 females, 24 males Health status as defined by authors: healthy Residential status of participants: community dwelling Setting: USA Inclusion:over 65 years Exclusion: cardiopulmonary/cardiovascular disease, intolerance to exercise, functional disabilities contraindicating strength training, unable to commit to programme, current strength training. |
|
| Interventions | EXERCISE GROUP (STRENGTH): (n = 25) 12 exercise for upper and lower limbs using surgical tubing and exercise booklet CONTROL GROUP: (n = 30) group driver education class Duration and intensity: EXERCISE 60 mins, 3x per week, 12 weeks; CONTROL 2x 3hour Supervisor:project staff Supervision:groups (10‐15) Setting:gym | |
| Outcomes | Gait velocity 3 m of 10m barefoot (m/s) Single legged stance eyes open/eyes closed (s) backward tandem walk 8 feet (errors) Compliance/adherence:diaries for exercise group indicated 90% for supervised sessions, 86.6% unsupervised sessions Adverse events: No adverse events reported. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | High risk | Significant difference is reported for age and gait velocity |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
Toraman 2004.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 42 Losses:no losses N = 42 Age: 60 to 86; EX: 72.5 (7.4), CO: 72.3 (6.0) Sex: 18 men; 3F ‐ Control and 17M; 4 women ‐ Exercise Health status as defined by authors: healthy Residential status of participants:residential care Setting: Turkey Inclusion: aged 60 or over; live in retirement home; independent; perform ADL without mobility aids; healthy; MMSE score of 20 or greater; volunteered for study Exclusion: serious cardiovascular or musculoskeletal diseases |
|
| Interventions | EXERCISE GROUP (MULTIPLE): 9 week multi component comprehensive training programme included a warm‐up 10 mins and cool down 10 mins. Components were: 1. aerobic (50% HR increasing 5% weekly) 2. Strength ‐ circuits ‐ 80%IRM and 3. Flexibility training CONTROL GROUP: Duration and intensity: 3 sessions per week for 9 weeks Supervisor: exercise instructor and daily monitoring by nurses of activity levels Supervision: in groups Setting: residential home | |
| Outcomes | TUG over 8 feet (s) Compliance/adherence:all 21 completed though only 6 participated regularly. Others not regularly. Adverse events: No adverse events reported. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Vestergaard 2008.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 61 Losses: 8 (5 from exercise and 3 from control) N = 61 Age: 75 and over mean 81 (3.3) exercise, 82.7 (3.8) control Sex: all women Health status as defined by authors: frail Residential status of participants: community dwelling Setting: Denmark Inclusion: unable to get outdoors without walking aid in last 2 weeks, not participating in regular exercise programmes, scoring 3 or less on mobility tiredness scale, able to communicate by telephone, able to get out of bed/chair, self reported sufficient visual capabilities to follow exercises on TV screen. Exclusion: |
|
| Interventions | EXERCISE GROUP (MULTIPLE): 30 min video, booklet and elastic resistance band. 15 mins warm up, flexibility and dynamic balance, strengthening, aerobic 'walking on spot'. seated or standing CONTROL GROUP: usual activity Duration and intensity: 26 mins 3x week for 5 months Supervisor: trained exercise instructor for first session, then video plus bi‐weekly telephone call Supervision: individual Setting: community | |
| Outcomes | Semi‐tandem balance (s) Compliance/adherence: not stated Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Matched randomisation based on max leg extensor power at baseline, ranked and matched in pairs, one randomly allocated to each group. Final unpaired participant was allocated based on coin toss. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis but dropouts not imputed |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | High risk | Personnel not blind to group allocation |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Outcome at 2 weeks after intervention |
Vogler 2009.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 180 Losses: 9 (3 in each group) Age: 80+/‐ 7 years Sex: 79% women Residential status of participants:community dwelling Health status as defined by authors: healthy Setting: Australia Inclusion: 65 or older Exclusion:medical contraindications to exercise, if they were cognitively impaired (Mini‐Mental State Examination score 24 out of 30), or if they were to be discharged to a high‐care residential facility for the aged. |
|
| Interventions | EXERCISE GROUP (STRENGTH) (n = 60): Seated exercises. Hip flexion, extension, abduction, knee flexion and extension, and ankle plantar‐ and dorsiflexion. An increasing amount of resistance from cuff weights and exercise bands was added to the exercises with the aim of a 10 to 12 repetition maximum load. EXERCISE GROUP (MULTIPLE) (n = 60): Standing exercises. Lower‐limb strength was targeted with exercises such as heel raises, partial squats, sit‐to‐stand, and stepping forward and sideways up onto blocks. Resistance was provided with weight‐loaded waist belts, aiming for a 10 to 12 repetition maximum load. CONTROL GROUP (n = 60): social visits Duration and intensity: physical therapist visited 8 times in 12 weeks, subjects were asked to exercise 3 times a week Supervisor: Three experienced physical therapists Supervision:individual Setting: home |
|
| Outcomes | Maximal balance range (mm) Co‐ordinated Stability test (errors) Sway in four conditions (mm) Gait speed; fast pace (m/s) Compliance/adherence: seated group 70% and weigh bearing group 62% of 36 recommended sessions. Adverse events: 22 reported in 22 participants, soreness (lower back, hip, knee pain) |
|
| Notes | Some data not reported appropriately for analysis purposes. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization (independent of baseline assessment results) was performed in blocks of 15 subjects by computer‐generated random numbers. |
| Allocation concealment (selection bias) | Low risk | Opaque envelopes. The outcome assessor remained unaware of group allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Blinding reported |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Voukelatos 2007.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 702 (EX: 353 CO:349 ) Losses: 18 Age: 69 (SD 6.5) Sex: 84% women Health status defined by authors: healthy Residential status of participants: community dwelling Setting: Sydney, Australia Inclusion: aged 60 or over; living in community; not practiced tai‐chi in last 12 months; Exclusion: degenerative neurological condition; severe arthritis; marked vision impairment; unable to walk across room unaided |
|
| Interventions | EXERCISE GROUP (3D) (n = 353): Tai‐chi in community based classes around city consisting of different forms of tai‐chi CONTROL GROUP (n = 349): no intervention Duration and intensity: 1 hour tai‐chi class for 16 weeks 1x weekly Supervisor: tai‐chi instructor (22 in total) Supervision: group Setting: community venues 24 in total |
|
| Outcomes | Sway on floor (mm): Sway on foam rubber mat (mm) Lateral stability (mm) Leaning balance (mm) using maximal balance range Leaning balance (mm) coordinated stability tests Choice stepping reaction time (ms) Compliance/adherence: 76 tai‐chi did not complete post intervention balance assessments and 81 controls did not 71% of classes attended in total of classes offered. Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation list, details unknown to assessors, randomly permuted blocks of four or six, randomisation after baseline assessment. |
| Allocation concealment (selection bias) | Low risk | Randomisation results unknown to assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | 4 research assistants blinded to allocation |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Vrantsidis 2009.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 62 Losses: 14 (6 in exercise and 8 in control) Age: mean 75 years Sex: 85% women Residential status of participants:community dwelling Health status as defined by authors: have at least one functional impairment or one fall in last 6 months; assumed "healthy status" Setting: Australia Inclusion: age 55 years or over; and have at least one functional impairment (based on Questions 1–11 on the Frenchay Activity Index) or have a history of one or more falls in the preceding 6 months. Able to stand unsupported for at least 1 min and walk short distances indoors (at least 5 m) without a walking aid. Exclusion: cognitive impairment (<7 on the Abbreviated Mental Test Score), inability to understand English (the program was conducted in English), and a marked mobility impairment (unable to walk at least 5 m indoors without a walking aid). |
|
| Interventions | EXERCISE GROUP (GBFT) (n = 26):Getting Grounded Gracefully© program, based on the Awareness Through Movement lessons of the Feldenkrais method, specifically target dynamic balance, postural and turning stability, and weight‐shift transfers. CONTROL GROUP (n = 29): Usual activity Duration and intensity: two 40‐ to 60‐min sessions per week over an 8‐week period (16 sessions in all). Supervisor:experienced Feldenkrais practitioner Supervision:group Setting:community clinic | |
| Outcomes | 4 step square test TUG (s) Gait speed preferred pace (m/min) Force platform Compliance/adherence: Exercise group, class attendance ranged from 9 to 16 classes (16 classes in all). Most participants (19 of 26; 73%) attended 14–16 classes. Overall attendance was 87.7%, and 40 individual class CDs were provided to participants who had missed one or more classes. Adverse events: not reported |
|
| Notes | Power analysis indicated an overall sample size of 42 per group (or 84 overall) was required. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation mentioned but Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Low risk | Randomly ordered opaque envelopes |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | ‘As‐treated’ analysis done, drop outs existed but no detail reported |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | The program was designed (copyright) by article’s authors |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | ‘Blinded to group allocation’ |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Wallsten 2006.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 77 Losses: confusing ‐ state 31 withdrew in table (46 remain), but present data suggesting 53 remain Age: mean (range) 81.2 (61 to 92 yrs) Sex: men N = 20; women N = 57. Setting: USA. Health status as defined by authors: healthy Residential status of participants: independently in continuing care retirement community Inclusion: Community dwelling, GP approval Exclusion: history of hip fracture or hip or knee replacement; Parkinsons Disease, stroke or other neurological disease, receiving therapy for cancer; using assistive devices for walking more than 25 feet. |
|
| Interventions | EXERCISE GROUP(3D): (n = 41) Tai Chi Chuan Moderate (10 same forms used by Wolf 1997). CONTROL GROUP (n = 36): usual activities Duration and intensity: 20 weeks, 2 times 1 hour per week Supervisor: Tai Chi instructor. Supervision: group exercise sessions. Setting: Room in retirement community. | |
| Outcomes | Timed Up and Go as part of an "Overall Performance Score" This is an overall performance score result of combining and summing results of the following tests:10m walk; TUG; side by side stance; semi tandem stance; tandem stance. Compliance/adherence: not reported Adverse events:not reported |
|
| Notes | Also looked at detraining. All benefit lost 20 weeks after the intervention. Control group undertook Tai Chi at the end of the 20 weeks intervention. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement N = 24 missing balance measures, no explanation |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | High risk | Balance measures reported on incomplete data set |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | Unclear risk | Balance measures not considered, but no differences in age, height and weight |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | Low risk | Measurements made at 20 weeks post intervention to look at detraining |
Weerdesteyn 2006.
| Methods | Type of study: Part RCT Exercise group 2 and control were randomised. Exercise group 1 wasn't. |
|
| Participants | Number of participants randomised: 58 (Out of 113 recruits, the first 49 recruits went into Ex1 with the rest then being randomised :‐ 30 into Ex2 and 28 into Control) Losses: drop out = 6 before randomisation into Exercise 2 and Control 1 person in Ex2 and 2 in Control could not comply due to medical issues (2), with one declining involvement. Age: EX1: 73.7 (4.5) EX2: 73.2 (6.2) CO: 74.9 (6.5) Sex: 76.7% females in Ex2 and 67.9% females in Control Health status as defined by authors: fallers Residential status of participants: community dwellers Setting:The Netherlands Inclusion:history of at least one fall in the year prior to participation and able to walk for 15minutes without use of a walking aid Exclusion:severe cardiac, pulmonary or musculoskeletal disorders, pathologies associated with an increase fall risk, osteoporosis and the use of psychotropic drugs. |
|
| Interventions | EXERCISE GROUP (GBFT): (N=30) 1st session of a week: balance, gait and coordination training via obstacle course. Motor dual tasks involved. 2nd session of a week: walking exercises and practicing of fall techniques. CONTROL GROUP: (N=28) usual activities Duration and intensity:1.5 hours of an exercise session, twice weekly for 5 weeks Supervisor: experienced physiotherapist Supervision:group 2‐3 supervisors per group of 10 participants Setting: Rehabilitation centre | |
| Outcomes | Timed one‐leg stance eyes open AP (mm/s) Timed one‐leg stance eyes closed AP (mm/s) Timed one‐leg stance eyes open Lateral (mm/s) Timed one‐leg stance eyes open Lateral (mm/s) Single legged stance (s) Compliance/adherence: attendance rate of 87% Adverse events:not reported |
|
| Notes | Authors provided additional data for exercise group 2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation with equal probability for exercise or control group |
| Allocation concealment (selection bias) | Low risk | Participants drew an envelope (from 20 sealed non‐see through envelopes per block) after completed baseline assessment |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | High risk | Assessors not blind |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Westlake 2007.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 44 Losses: 8 (5 from intervention group and 3 from control) Age: not stated other than over 65 Sex: not stated Health status defined by authors: healthy Residential status of participants: community Setting: not stated though presumed USA or Canada Inclusion: aged 65 or over Exclusion: pre‐existing major lower‐extremity pathology, neurological disability that would prevent taking part in testing and health conditions that would preclude and exercise programme |
|
| Interventions | EXERCISE GROUP (GBFT) (n = 22): Sensory‐specific balance classes followed the "FallProof Programme" which emphasises static and dynamic exercises with transition between different sensory conditions. Tasks included standing or walking on different surfaces such as a rocker board, foam, narrow beam, tandem, semitandem, or on one leg. Progressions to these tasks included simultaneous alterations of vestibular and visual information. CONTROL GROUP (n = 22): Falls prevention education programme. Appears to be discussion based and aims to increase awareness of falls hazards. Paper does not describe the detail of this programme. Seems that they may have had same number of visits ? group work mentioned Duration and intensity: 8 weeks, 3 x week for 1 hour each time Supervisor: not mentioned Supervision: group work Setting: not stated |
|
| Outcomes | Centre of Pressure (COP) velocity change score (cm/s) Fullerton Advanced Balance Scale (FAB) (score 0 to 40) Physical Activity Scale for the Elderly (PACE) (score 0 to > 400) Compliance/adherence: sessions attended ‐ 89.9% for exercise group and 66.3% for the education group Adverse events:not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only included subjects who attended for assessment |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Stated single blind study but no specific description of assessor or process |
| Were the treatment and control group comparable at entry? | Unclear risk | Insufficient information to permit judgement |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Evaluated pre, post and follow‐up only at 8 weeks following intervention and only for exercise group. |
Wolf 1997.
| Methods | Type of study: RCT. | |
| Participants | Number of participants randomised: 72
Losses: Balance Gp n = 8; education n = 5; Tai Chi n = 5 N = 72. Age: mean (SD) 77.7 (6.5) balance group, 75.2 (4.9) education group, 77.7 (5.2) Tai Chi group. Sex: 60 females, 12 males. Health of participants defined by authors: Healthy Residential status of participants: Community Setting: USA. Inclusion: over 70 years, free from progressive debilitating processes, able to walk across a room independently, residing in independent living centre. Exclusion: Progressive debilitating processes such as Alzheimers, Parkinson's, cancers and severe arthritis |
|
| Interventions | EXERCISE GROUP (COMPUTERISED BALANCE): (N = 24) force platform standing moving target via cursor excursions eyes open and closed.
EXERCISE GROUP (3D): (N = 24) Tai Chi quan ‐ 10 forms. CONTROL GROUP: (N = 24) discussion of topics and socialisation. Duration and intensity: 1 hour every week x 15 weeks. Supervisor: instructor. Supervision: group. Setting: gym. |
|
| Outcomes | Chattex balance system to measure: quiet standing eyes open, eyes closed Compliance/adherence : not reported Adverse events: not reported |
|
| Notes | Part of Atlanta FICSIT site study. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient reporting to permit judgement but stated random allocation |
| Allocation concealment (selection bias) | Unclear risk | Insufficient reporting to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No, only on completers |
| Selective reporting (reporting bias) | Unclear risk | Insufficient reporting to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient reporting to permit judgement |
| Were the treatment and control group comparable at entry? | Low risk | Slight differences but data analysed appropriately |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | Low risk | Follow‐up at 4 months |
Wolf 2001.
| Methods | Type of study: RCT. | |
| Participants | Number of participants randomised: 94
Losses: exercise n = 23, control n = 22 N = 94. Age: mean (SD) exercise group ‐ 84.5 (6.1), control group ‐ 83.6 (5.1). Sex: 56 women, 21 men. Health of participants defined by authors: frail Residential status of participants: residential care Setting: Netherlands. Inclusion: 75 years and over, minimal loss of visual acuity, no acute illness, no physical therapy in previous month, minimum of 17 on MMSE, Berg Balance Scale < 52, impaired balance during function. Exclusion: not stated |
|
| Interventions | EXERCISE GROUP (GBFT): exercise in sitting, standing and walking, in a variety of situations to test balance. (n = 25) CONTROL GROUP: (N = 24) reading and board games. Duration and intensity: 30 minutes 2‐3 times per week x 4‐6 weeks (10 sessions). Supervisor: therapist and trainers. Supervision: individual. Setting: gym or home. | |
| Outcomes | Berg Balance Score (points) out of 56. Compliance/adherence: not reported Adverse events: not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants assigned to 2 strata based on baseline data then randomly allocated but method not stated |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes selected by blindfolded researcher |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Some baseline data characteristics given after drop outs |
| Selective reporting (reporting bias) | Unclear risk | Insufficient reporting to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient reporting to permit judgement |
| Were the treatment and control group comparable at entry? | Unclear risk | Comparable and adjusted in analysis but baseline data characteristics given after drop outs |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | Low risk | One year follow‐up |
Wolfson 1996.
| Methods | Type of study: RCT. | |
| Participants | Number of participants randomised: 110
Losses: GBFT n = 2; STRENGTH n = 2, MULTIPLE n = 2 N = 110. Age: mean (SD) 79 (5). Sex: 58% men. Health of participants defined by authors: healthy Residential status of participants : community Setting: USA. Inclusion: 75 years and over, community dwelling, free of clinically detectable disease affecting balance. Exclusion: inability to walk 8 metres without assistance, other diseased affecting mobility, dementia. |
|
| Interventions | EXERCISE GROUP (GBFT): (N = 27) PRObalancemaster with COP feedback, standing and sitting including gym ball eyes open and eyes closed with and without perturbations and gait on foam and narrow beams.
EXERCISE GROUP (STRENGTH): (N = 28) stretching and PRE with sand bags for hip and knee.
EXERCISE GROUP (MULTIPLE): (N = 28) PRObalancemaster with COP feedback, standing and sitting including gym ball eyes open and eyes closed with and without perturbations and gait on foam and narrow beams and stretching and PRE with sand bags for hip and knee.
CONTROL GROUP: (N = 27) usual activities, sessions on fall prevention and stress management. Duration and intensity: balance only and strength only groups 45 mins x 3 times per week x 3 months. Balance and strength group ‐ 45 mins (strength) plus 45 mins (balance) x 3 times per week x 3 months. Educational control group ‐ 5 x 90 minute education sessions. All groups ‐ 6 months Tai Chi maintenance. Supervisor: not stated. Supervision: balance training ‐ individual, strength training ‐ group. Setting: gym. |
|
| Outcomes | Loss of Balance during sensory organisation test.
Functional base of support.
Single legged stance time (s).
Usual gait velocity (m/s) Compliance/adherence : mean (SD) balance 74 % (26), strength 82 % (21), balance and strength 82 % (16), control near perfect. Adverse events: not reported |
|
| Notes | Part of FICSIT studies. All subjects including those in control group participated in 6 month Tai Chi following the 3 month intervention phase. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised by blocked allocation schedule stratified by gender and generated using Moses‐Oakford algorithm |
| Allocation concealment (selection bias) | Unclear risk | Insufficient reporting to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Completer analysis only |
| Selective reporting (reporting bias) | Unclear risk | Insufficient reporting to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Assessors blinded. |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | Low risk | 6 month follow‐up |
Woo 2007.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 180 Losses: 4 Age: 68.2 (2.4) males; 69.67 (2.8) females Sex: mixed (90 men : 90 women) Health status defined by authors: healthy ‐ elderly Residential status of participants: community Setting: Hong Kong, China Inclusion: Exclusion: unable to walk 8m without assistance, neurological disease which impaired mobility, cardiovascular disease resulting in shortness of breath or angina when walking up a flight of stairs, dementia, already regularly performing tai‐chi exercise |
|
| Interventions | EXERCISE GROUP (3D): (N = 30) Tai‐Chi EXERCISE GROUP (STRENGTH): (n = 60) using theraband with 30 reps of arm lifting, hip abduction, heel raise, hip flexion, hip extension, squatting ankle dorsiflexion CONTROL GROUP: (n = 60) no exercise Duration and intensity: 3 x week for 12 months ‐ length of each session not stated. Supervisor: not stated Supervision: group exercise but not clear how many in each group Setting: not clearly stated Community assumed. |
|
| Outcomes | Balance measured by a SMART Balance Master (1 to 100) Semi‐tandem stance(s) Tandem stance (s) Single legged stance (s) (barefoot and arms crossed) Gait velocity over 8m (s) Compliance/adherence: attendance rate 3D = 81%; STRENGTH = 76.3% with no attrition between 6 and 12 months Adverse events:not reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Blocked randomisation with stratification by sex |
| Allocation concealment (selection bias) | Low risk | Randomisation by independent person |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only 4 drop outs but data not included in final analysis |
| Selective reporting (reporting bias) | Low risk | Detail available in appendices accessed online. |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Assessors blind to allocation and results |
| Were the treatment and control group comparable at entry? | High risk | Some differences noted : men and women analysed separately for each group .Some differences in demographic variables including quadriceps strength |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Worm 2001.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 46 Losses: Control 1 and Exp 1 Age: Control 81.9 +/‐ 3.6 Ex 80.5 +/‐ 4.9 Sex: Control 13 women; 11men; Exp 14 women; 8 men Health status as defined by authors: frail Residential status of participants: community dwellers Setting: Denmark Inclusion: 74 years or older; community dwellers; not able to leave home without assistance or mobility aid. Exclusion: Life threatening, symptomatic somatic disease or confined to bed |
|
| Interventions | EXERCISE GROUP (MULTIPLE): Training classes (flexibility training; aerobics, rhythm, balance and reaction exercises, and muscle training (strength and endurance) and a home based programme (muscle and flexibly training) of 10 mins/morning. CONTROL GROUP: usual care Duration and intensity: 60 minute sessions twice a week over 12 weeks Supervisor: not stated Supervision: group Setting:classes in community | |
| Outcomes | Berg Balance Scale (0 to 56 points) Walking time over 10 metres (m/s) Compliance/adherence: 81% nonattendance rate due to 2 participants Adverse events: No adverse events reported. |
|
| Notes | NB. Data presented as confidence intervals and p values provided. SDs estimated from the P values. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Low risk | Same observers without reference to pre‐intervention values |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Yang 2007.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 59 non equal randomisation to allow for more dropouts in exercise group Losses: 10 of 59 (7 exercise gp and 3 control gp) Age: mean (SD) 80.2 (9.02) Taiji Qigong, 80.9 (7.97) control. Sex: men and women, no numbers given. Health status as defined by authors: healthy Residential status of participants: community dwelling and senior living facilities Setting: USA. Inclusion: Community dwelling, aged > 60 Exclusion: < age 60, Berg balance score < 40, MSQ < 5 out of 8, Parkinsons Disease, stroke or other neurological disease, certain medications. |
|
| Interventions | EXERCISE GROUP (3D): (n = 33) Moderate Taiji Qigong (same form used by Wolf 1997). CONTROL GROUP (n = 16): usual activities Duration and intensity: 6 months, 3 times 1 hour per week Supervisor: Taiji instructor. Supervision: group exercise sessions. Setting: senior centres. | |
| Outcomes | SOT ‐ Sensory organisation Test ‐ vestibular ratio and visual ratio Quiet stance (cm2) Compliance/adherence: not reported Adverse events:not reported |
|
| Notes | Also assessed feet opening angle on standing (degrees) and base of support (BoS) Another 19 participants in exercise group not randomised as wanted to do Taiji but their data was not included in analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer randomisation |
| Allocation concealment (selection bias) | Low risk | Participants assigned by unique number |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Generalised Estimate Equations used to compute ‐ estimates of effect used for missing data |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Not reported, nurse did tests but unclear as to whether blinded. |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported. |
Yoo 2010.
| Methods | Type of study: RCT | |
| Participants | Number of participants randomised: 21 Losses: Exercise group 3, control group 4 Age: mean age 71 years Sex: all females Health status as defined by authors:healthy Residential status of participants: community‐dwelling Setting: Korea Inclusion: women over the age of 65 yrs, the capability to participate safely in moderate intensity aerobic and resistance exercise, and no more than one risk factor for cardiovascular disease. Exclusion: difficulty with activities of daily living (ADL), uncontrolled hypertension, a history of metabolic disorders known to influence bone (e.g., diabetes, hyperparathyroidism), a history of irregular menstrual cycles or amenorrhea, (e) a history of hip or vertebral fracture, or currently taking hormones or hormonal medication. |
|
| Interventions | EXERCISE GROUP (GPA ‐ WALKING) (n = 11): walking exercise program with ankle weights 10‐minute warm‐up without ankle weights, 45 minutes of walking with ankle weights, and a 5‐minute cool‐down without ankle weights. Exercise intensity was maintained at 60% of heart rate reserve CONTROL GROUP (n = 10): usual activity Duration and intensity: 3 x per week for 3 months Supervisor: stated but not specified Supervision: group Setting: community outdoors |
|
| Outcomes | 8‐foot up‐and‐go test (s) stability scores (with or without foam and with eyes open or closed) Compliance/adherence: not reported Adverse events: No adverse events reported. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation mentions but method not stated insufficient information to permit judgement of yes or no |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient information to permit judgement |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Immediately post intervention at 3 months, no follow‐up data reported |
Zhang 2006a.
| Methods | Type of study: RCT. | |
| Participants | Number of participants randomised: 49
Losses: 2 of 49. one from each group. N = 49. Age: mean (SD) 70.2 (3.6) Tai Chi, 70.6 (4.9) control. Sex: 25 men, 24 women. Health of participants defined by authors: frail Residential status of participants:community Setting: Japan. Inclusion: Community dwelling, scoring 20 to 25 seconds on Single legged stance time. Exclusion: |
|
| Interventions | EXERCISE GROUP (3D): (N = 25) Tai Chi simplified form of 24 forms plus 11 easy forms at home. CONTROL GROUP: (N = 24) usual activities. Duration and intensity: 1 hour, 7 times per week for 8 weeks. Supervisor: Tai Chi instructor. Supervision: group and self. Setting: community in park and home. | |
| Outcomes | Single legged stance eyes open (max 60 s).
Walking speed (10 metres) Compliance/adherence: 91.7% practiced 4 plus hours per week Adverse events: not reported |
|
| Notes | Subjects from earlier study by Zhang et al 2003. Assumption that there was no intervention in the wait control group (for 6 months). GEE point estimate was used. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient reporting to permit judgement although stated 49 subjects divided into 24 pairs according to sex, experience of falling and exercise habits. Randomised one from each pair by tossing a coin. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient reporting to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient reporting to permit judgement |
| Selective reporting (reporting bias) | Low risk | The study appears to be free of other sources of bias |
| Other bias | Low risk | The study appears to be free of other sources of bias |
| Blinding (participant) | High risk | Not possible |
| Blinding (assessor) | Unclear risk | Insufficient reporting to permit judgement |
| Were the treatment and control group comparable at entry? | Low risk | No differences reported on baseline characteristics with a potential to influence the effect of the intervention |
| Was the surveillance active, and of clinically appropriate duration (i.e. at least 3 months post intervention)? | High risk | Only immediately post intervention data, no follow‐up data reported |
ABBREVIATIONS AND ACRONYMS: 1RM: One Repetition Maximum score 3D: 3D exercise including Tai Chi, qi gong, dance, yoga ADL: Activities of Daily Living. AP: Anterior‐Posterior BBS: Berg Balance Scale BPM: Balance Performance Monitor cm: Centimetres CoM: Body's Centre of Mass COMPUTERISED BALANCE: Computerised balance training using visual feedback COP: Centre of pressure. COPD: Chronic Obstructive Pulmonary Disease EPESE: Established Populations for the Epidemiologic Studies of the Elderly short physical performance battery Ex: Exercise FRT: Functional Reach Test GBFT: Gait, Balance, Functional Tasks GEN ACTIVITY: General physical activity HR: Heart Rate hr: Hour km: Kilometres LOS: Locus Of Support MD: Mean difference min: Minute ML: Medio‐Lateral mm: Millimetres MMSE: Mini Mental Status Examination. m/s: Metres per second MULTIPLE: Multiple forms of exercise type included in intervention NSD: No significant difference PNF: Proprioceptive Neuromuscular Facilitation PRE: Progressive Resistance Exercise. RCT: Randomised Controlled Trial RMS: Root mean squared s: Seconds SD: Standard Deviation SE: Standard Error SLS: Single Legged Stance SMD: Standardised Mean Difference STRENGTH: Strength training including resistance or power training TUG: Timed Up & Go Test VIBRATION: Vibration platform used as intervention
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Alexander 2001a | RCT but no specific balance outcomes |
| Alexander 2001b | RCT no suitable outcome measures |
| Allen 1999 | Description of study no data reported |
| Annesi 2004 | No control group |
| Anonymous 2002 | Summary of Day 2002 |
| Au‐Yeung 2002 | Control group received some exercise |
| Ballard 2004 | Control group received some exercise |
| Barnett 2003 | Control group had home exercise |
| Barrett 2002 | Control group received some exercise |
| Bean 2004 | Comparison of different exercise types , no control group |
| Binder 2002 | Control group had home exercise |
| Bissonnette 2010 | Not an RCT |
| Bonnefoy 2003 | Trial of energy supplements all participants received supplement or placebo |
| Brown 2000 | Control group received some exercise |
| Bruyere 2005 | Intervention not exercise |
| Buchner 1993 | Description of methodology no data |
| Campbell 1999 | No suitable balance outcome measures |
| Chen 2010 | Not an RCT |
| Conroy 2010 | No balance outcomes |
| Cornillon 2002 | Not appropriate outcome measures |
| Cristopoliski 2009 | Only passive stretching included in intervention |
| Csapo 2009 | Not an RCT |
| Day 2002 | No control group |
| De Vreede 2004 | Comparison of exercise types, no control group |
| Delbaere 2006 | Not truly randomised |
| Delbaere 2010 | Intervention groups did not include exercise |
| Devereux 2005 | Osteoporotic participants |
| DeVito 2003 | No balance measures |
| Dyer 2004 | Multifactorial falls programme |
| Earles 2001 | No control group |
| Fiatarone 1993 | FICSIT study multi‐nutrient supplementation no data presented |
| Gatts 2007 | Condition specific population ‐ hip knee and back surgery were inclusion criteria |
| Gill 2002 | No specific balance outcome measures |
| Gitlin 2006 | No specific balance outcome measures |
| Granacher 2010 | This is a balance intervention with a focus on cognitive motor interference (CMI) using stride to stride variability as a surrogate marker of CMI. As such the outcome is not in our listed outcomes (e.g. this is not a measure of spatio‐temporal characteristics) |
| Gras 2004 | No control group |
| Greendale 2000 | Comparison of weighted vests |
| Gu 2006 | Korean translators (via Cochrane) confirm not an RCT |
| Haines 2007 | Usual care control group received one hour physio 5 times/week. |
| Hallage 2010 | Not an RCT |
| Hauer 2003 | 61% of participants had hip fracture or lower extremity fracture |
| Helbostad 2004a | No specific balance outcome measures |
| Helbostad 2004b | No control group |
| Hinman 2002 | No control group |
| Hinman 2006 | Not an RCT |
| Hornbrook 1993 | Description of study |
| Hu 1994 | No exercise intervention |
| Huang 2010 | Cluster randomised with small number of clusters in each intervention |
| Jones 1992 | No appropriate outcome measures of balance |
| Judge 1993a | Control group received flexibility training |
| Judge 1993b | No specific balance outcome measures |
| Judge 1994 | No specific balance outcome measures |
| Kamijo 2009 | Not an RCT |
| Kato 2006 | Not randomised, nurses chose participants for exercise group |
| Kawanabe 2007 | Not an RCT |
| Kim 2009b | No balance outcomes |
| King 2002 | Control group had home exercise |
| Kloubec 2010 | Participants were middle aged, ranging from 26 to 59 years |
| Kolbe‐Alexander 2006 | Cluster randomised with small number of clusters in each intervention |
| Kovacs 2004 | No specific balance outcome measures |
| Kutner 1997 | No specific balance outcome measures |
| LaStayo 2003 | Participants had received cardiopulmonary rehabilitation for prior medical conditions. |
| Latham 2001 | Control group had physiotherapy |
| Lazowski 1999 | Control group had exercise |
| Lee 2010 | Not an RCT (convenience grouping of participants) |
| Lelard 2010 | Both groups included exercise, no control group |
| Li 2002 | No specific balance outcome measures |
| Li 2005a | Intervention under investigation: cobblestone mat |
| Li 2005b | Control group had stretching |
| Li 2007 | Not an RCT |
| Lichtenstein 1989 | Cluster randomised with one cluster in each intervention |
| Lin 2006 | Not an RCT |
| Lindemann 2004 | Control group had exercise programme |
| Liu‐Ambrose 2004 | All participants had low bone mass |
| Liu‐Ambrose 2010 | All groups included exercise, no control |
| Luukinen 2007 | No appropriate measures for balance outcomes and age range over 85 years |
| Mahoney 2007 | No measures of balance. No exercise only intervention (was exercise plus occupational therapist home visits) |
| Marigold 2005 | Participants were chronic stroke patients |
| McMurdo 1994 | No measures of balance |
| McMurdo 2000 | Primary outcome falls no primary outcome measure for balance |
| Means 1996 | No specific balance outcome measures |
| Means 2005 | No specific balance outcome measures |
| Messier 2000 | Participants had osteoarthritis |
| Morey 2008 | No measures, study protocol only |
| Morgan 2004 | No measures of balance |
| Mulrow 1994 | No measures of balance |
| Nakamura 2007 | Not an RCT |
| Nitz 2004 | Control group had exercise |
| Nnodim 2006 | No control group: Tai Chi versus combined balance and step training |
| Ourania 2003 | Not an RCT |
| Paillard 2005 | Investigating effects of electrical stimulation |
| Pijnappels 2008 | Controlled study only, no randomisation |
| Prasansuk 2004 | Participants had balance disorders |
| Ramsey 2003 | Participants were visually impaired |
| Rees 2007 | Control group received low intensity exercise |
| Ribeiro 2009 | Not an RCT: control group did not wish to partake in the exercise programme |
| Robbins 2001 | Commentary on another study |
| Rochat 2008 | No control group |
| Rooks 1997b | No control group |
| Rugelj 2010 | Contamination of randomisation |
| Ryushi 2000 | Age range from 41 years to 53 years. |
| Sattin 2005 | Insufficient data presented ‐ excluded as only presents self report. |
| Sayers 2003 | Two groups: high versus low intensity exercise |
| Shaughnessy 1998 | Commentary on Campbell 1997 |
| Shigematsu 2002 | Cluster randomised with small number of clusters in each intervention |
| Shimada 2003 | Control groups received exercise |
| Shumway‐Cook 2006 | Intervention was multifactorial exercise was only one component |
| Signorile 2002 | No specific balance outcome measures |
| Simmons 1996 | Water versus land based exercise |
| Simons 2006 | No appropriate outcome measures of balance |
| Siqueira Rodrigues 2010 | No outcome measures |
| Siu 2007 | Control group also received exercise for upper body |
| Skelton 1999 | Description of FAME programme no data reported |
| Sohng 2003 | Control group had video programme |
| Steadman 2003 | Control group had physiotherapy |
| Steinberg 2000 | No specific balance outcome measures |
| Suarez 2006 | No control group |
| Sung 2007 | Korean translators (via Cochrane) confirmed this was not an RCT |
| Szturm 1994 | Participants with chronic peripheral vestibular dysfunction |
| Taguchi 2010 | Not an RCT |
| Timonen 2002 | Control group had home exercise |
| Timonen 2006 | Control group had a home exercise programme |
| Tinetti 1994 | No specific balance outcome measures |
| Udani 1998 | Commentary on Wolf 1996 |
| Ullmann 2010 | Contamination of randomisation |
| Urbscheit 2001 | Control group did exercise |
| Vamos 2001 | Not an RCT ‐ controls were age matched with intervention group |
| Verfaillie 1997 | No control group |
| Williams 2002 | Control group had exercise |
| Wolf 1996 | No specific balance outcome measures |
| Wolf 2003 | No specific balance outcome measures |
| Wu 2010 | All groups included exercise, no control group |
| Yan 2005 | Not an RCT: groups selected on basis of previous exercise regime. |
| Yan 2009 | Not an RCT |
| Yates 2001 | Multifactorial intervention |
| Zhang 2006b | Control group had exercise |
| Zisi 2001 | Not an RCT; control group were age and sex matched. |
Characteristics of ongoing studies [ordered by study ID]
Frandin 2009.
| Trial name or title | "A Nordic multi‐center study on physical and daily activities for residents in nursing home settings: design of a randomized, controlled trial" |
| Methods | Type of study: RCT |
| Participants | Number of participants randomised: 322 N = exercise = 170; control = 152 Age: 64 or over Sex: 85 men and 237 women Health status as defined by authors: healthy Residential status of participants: community dwelling Setting: Sweden, Norway and Denmark Inclusion: age over 64 years, need of daily assistance in a minimum of one P‐ADL activity; expected stay in nursing home in the intervention period. Exclusion: residents in a terminal stage of disease |
| Interventions | Exercise group (GBFT): personalised activity programme (treatment goals, ADL training, exercise including transfers, walking, balance, muscle strength and endurance, outdoor activity) Control group: traditional care and treatment Duration and intensity: 3 months daily with 6 month follow‐up Supervisor: physiotherapist and occupational therapist Supervision: individual and group Setting:nursing home |
| Outcomes | Gait speed (m/s) Berg Balance Scale (0 to 56 points) |
| Starting date | March 2006 |
| Contact information | Kerstin Frandin; kerstin.frandin@ki.se |
| Notes |
Leininger 2006.
| Trial name or title | Physical and psychological effects of yoga exercise on healthy community‐dwelling older adult women. |
| Methods | Type of study: RCT |
| Participants | Number of participants randomised: 92 Losses: 3 from exercise group and 7 from control N = 44 = exercise control = 48 Age: 60 or over Sex: all women Health status as defined by authors: healthy Residential status of participants: community dwelling Setting: Inclusion: Exclusion: |
| Interventions | Exercise group: Hatha yoga exercise Control group: education (met 4 times = 1 hour every other week for 10 weeks) Duration and intensity: 1 hour twice per week for 10 weeks Supervisor: Supervision: Setting: |
| Outcomes | Limits of Stability test Unilateral Stance test |
| Starting date | |
| Contact information | |
| Notes | Adherence: PhD thesis abstract |
Differences between protocol and review
For this update, published in Issue 11, 2011, the following changes were made: 1. The methodology has been updated to include the reclassification of outcome measures and exercise categories and the reclassification of some interventions from original studies. New comparisons are based on the reclassification of outcome measures and exercise categories. 2. Risk of bias (instead of methodological quality) is now assessed; 3. All analyses are now based on the new categories of exercise interventions.
Contributions of authors
TEH ‐ conceived the review, coordinated data collection, searching and retrieval of papers and additional information, screened all search results, appraised quality and extracted data from all papers, entered data into RevMan, analysed and interpreted data and wrote review. TEH is the guarantor for this review.
LR ‐ conceived the review, screened search results, appraised quality, extracted data from papers, assisted in interpretation of data and critically commented on drafts.
FN ‐ co‐ordinated searching and retrieval of papers and additional information, screened search results, appraised quality and extracted data from papers, entered data into RevMan and commented on drafts.
DS ‐ screened search results, appraised quality, extracted data from papers, entered data into RevMan, assisted in interpretation of data and critically commented on drafts
CB ‐ screened search results, appraised quality and extracted data from papers and commented on drafts.
Sources of support
Internal sources
Glasgow Caledonian University, UK.
University of Northumbria, UK.
University of Newcastle, UK.
University of Southampton, UK.
External sources
Scottish Funding Council, UK.
Scottish Executive Health Department, UK.
NHS Education for Scotland, UK.
Chief Scientist Office, UK.
-
National Institute of Health Research, UK.
Cochrane Incentive Award
Declarations of interest
Dawn Skelton is the principal investigator on two studies considered within the review. She is also a Director of Later Life Training Ltd, an educational not for profit training company that delivers exercise delivery training to health and leisure professionals (accredited by Skills Active, the Register of Exercise Professionals and has endorsed training status from the Chartered Society of Physiotherapy). The training courses include two programmes of exercise that have been shown to reduce falls.
Edited (no change to conclusions), comment added to review
References
References to studies included in this review
Arai 2007 {published data only}
- Arai T, Obuci S, Inaba Y, Nagasawa H, Shiba Y, Watanabe S, et al. The effects of short‐term exercise intervention on falls self‐efficacy and the relationship between changes in physical function and falls self‐efficacy in Japanese older people: a randomized controlled trial. American Journal of Physical Medicine & Rehabilitation 2007;86(2):133‐41. [DOI] [PubMed] [Google Scholar]
Avelar 2010 {published data only}
- Avelar NC, Bastone AC, Alcantara MA, Gomes WF. Effectiveness of aquatic and non‐aquatic lower limb muscle endurance training in the static and dynamic balance of elderly people. Revista Brasileira de Fisioterapia 2010;14(3):229‐36. [PubMed] [Google Scholar]
Baker 2007 {published data only}
- Baker MK, Kennedy DJ, Bohle PL, Campbell DS, Knapman L, Grady J, et al. Efficacy and feasibility of a novel tri‐modal robust exercise prescription in a retirement community: A randomized, controlled trial. Journal of the American Geriatrics Society 2007;55(1):1‐10. [DOI] [PubMed] [Google Scholar]
Baum 2003 {published data only}
- Baum EE, Jarjoura D, Polen AE, Faur D, Rutecki G. Effectiveness of a group exercise program in a long‐term care facility: a randomized pilot trial. Journal of the American Medical Directors Association 2003;4(2):74‐80. [DOI] [PubMed] [Google Scholar]
Beling 2009 {published data only}
- Beling J, Roller M. Multifactorial intervention with balance training as a core component among fall‐prone older adults. Journal of Geriatric Physical Therapy 2009;32(3):125‐33. [DOI] [PubMed] [Google Scholar]
Beyer 2007 {published data only}
- Beyer N, Simonsen L, Bulow J, Lorenzen T, Jensen DV, Larsen L, et al. Old women with a recent fall history show improved muscle strength and function sustained for six months after finishing training. Aging‐Clinical & Experimental Research 2007;19(4):300‐9. [DOI] [PubMed] [Google Scholar]
Bogaerts 2007 {published data only}
- Bogaerts A, Verschueren S, Delecluse C, Claessens AL, Boonen S. Effects of whole body vibration training on postural control in older individuals: A 1 year randomized controlled trial. Gait and Posture 2007;26(2):309‐16. [DOI] [PubMed] [Google Scholar]
Boshuizen 2005 {published data only}
- Boshuizen HC, Stemmerik L, Westhoff MH, Hopman‐Rock M. The effects of physical therapists' guidance on improvement in a strength‐training program for the frail elderly. Journal of Aging & Physical Activity 2005;13(1):5‐22. [DOI] [PubMed] [Google Scholar]
Brouwer 2003 {published data only}
- Brouwer BJ, Walker C, Rydahl SJ, Culham EG. Reducing fear of falling in seniors through education and activity programs: A randomized trial. Journal of the American Geriatrics Society 2003;51(6):829‐34. [DOI] [PubMed] [Google Scholar]
Buchner 1997a {published data only}
- Buchner DM, Cress ME, Lateur BJ, Esselman PC, Margherita AJ, Price R, et al. The effect of strength and endurance training on gait, balance, fall risk, and health services use in community‐living older adults. Journals of Gerontology Series A‐Biological Sciences & Medical Sciences 1997;52A(4):M218‐24. [DOI] [PubMed] [Google Scholar]
Buchner 1997b {published data only}
- Buchner DM, Cress ME, Lateur BJ, Esselman PC, Margherita AJ, Price R, et al. A comparison of the effects of three types of endurance training on balance and other fall risk factors in older adults. Aging‐Clinical & Experimental Research 1997;9(1‐2):112‐9. [DOI] [PubMed] [Google Scholar]
Campbell 1997 {published data only}
- Campbell AJ, Robertson MC, Gardner MM, Norton RN, Tilyard MW, Buchner DM. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ 1997;315(7115):1065‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carvalho 2009 {published data only}
- Carvalho MJ, Marques E, Mota J. Training and detraining effects on functional fitness after a multicomponent training in older women. Gerontology 2009;55(1):41‐8. [DOI] [PubMed] [Google Scholar]
Chandler 1998 {published data only}
- Chandler JM, Duncan PW, Kochersberger G, Studenski S. Is lower extremity strength gain associated with improvement in physical performance and disability in frail, community‐dwelling elders?. Archives of Physical Medicine & Rehabilitation 1998;79(1):24‐30. [DOI] [PubMed] [Google Scholar]
Chang 2007 {published data only}
- Chang SJ, Mercer VS, Giuliani CA, Morey MC, Sloane C, Williams S. Hip abductor exercise and lateral stability in older adults at risk of falls... Combined Sections Meeting 2008: section on geriatrics poster and platform presentations. February 6‐9, 2008, Nashville, TN. Journal of Geriatric Physical Therapy 2007;30(3):146‐7. [Google Scholar]
Cheung 2007 {published data only}
- Cheung W‐H, Mok H‐W, Qin L, Sze P‐C, Lee K‐M, Leung K‐S. High‐frequency whole‐body vibration improves balancing ability in elderly women. Archives of Physical Medicine and Rehabilitation 2007;88(7):852‐7. [DOI] [PubMed] [Google Scholar]
Chulvi‐Medrano 2009 {published data only}
- Chulvi‐Medrano I, Colado JC, Pablos C, Naclerio F, Garcia‐Masso X. A lower‐limb training program to improve balance in healthy elderly women using the T‐bow device. Physician & Sportsmedicine 2009;37(2):127‐35. [DOI] [PubMed] [Google Scholar]
Clemson 2010 {published data only}
- Clemson L, Singh MF, Bundy A, Cumming RG, Weissel E, Munro J, et al. LiFE Pilot Study: a randomised trial of balance and strength training embedded in daily life activity to reduce falls in older adults. Australian Occupational Therapy Journal 2010;57(1):42‐50. [DOI] [PubMed] [Google Scholar]
Cress 1999 {published data only}
- Cress ME, Buchner DM, Questad KA, Esselman PC, Lateur BJ, Schwartz RS. Exercise: effects on physical functional performance in independent older adults. Journals of Gerontology Series A‐Biological Sciences & Medical Sciences 1999;54A(5):M242‐8. [DOI] [PubMed] [Google Scholar]
Crilly 1989 {published data only}
- Crilly RG, Willems DA, Trenholm KJ, Hayes KC, Delaquerriere‐Richardson LF. Effect of exercise on postural sway in the elderly. Gerontology 1989;35(2‐3):137‐43. [DOI] [PubMed] [Google Scholar]
de Greef 2006 {published data only}
- Greef MH, WeeningDijksterhuis B, Buren M, Hardeman F, Slutter K. The effect of a physiotherapeutic exercise programme on disability in older adults. Nederlands Tijdschrift voor Fysiotherapie 2006;116(5):106‐10. [Google Scholar]
Eyigor 2009 {published data only}
- Eyigor S, Karapolat H, Durmaz B, Ibisoglu U, Cakir S. A randomized controlled trial of Turkish folklore dance on the physical performance, balance, depression and quality of life in older women. Archives of Gerontology & Geriatrics 2009;48(1):84‐8. [DOI] [PubMed] [Google Scholar]
Faber 2006 {published data only}
- Faber MJ, Bosscher RJ, Chin A Paw MJ, Wieringen PC. Effects of exercise programs on falls and mobility in frail and pre‐frail older adults: A multicenter randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2006;87(7):885‐96. [DOI] [PubMed] [Google Scholar]
Frye 2007 {published data only}
- Frye B, Scheinthal S, Kemarskaya T, Pruchno R. Tai chi and low impact exercise: Effects on the physical functioning and psychological well‐being of older people. Journal of Applied Gerontology 2007;26(5):433‐53. [Google Scholar]
Furness 2009 {published data only}
- Furness TP, Maschette WE. Influence of whole body vibration platform frequency on neuromuscular performance of community‐dwelling older adults. Journal of Strength & Conditioning Research 2009;23(5):1508‐13. [DOI] [PubMed] [Google Scholar]
Gaub 2003 {published data only}
- Gaub M, Prost E, Bomar M, Farid R, Langland G, Brown M. Exercise specificity for physical frailty [abstract]. Journal of Geriatric Physical Therapy 2003;26(3):36. [Google Scholar]
Gine‐Garriga 2010 {published data only}
- Gine‐Garriga M, Guerra M, Pages E, Manini TM, Jimenez R, Unnithan VB. The effect of functional circuit training on physical frailty in frail older adults: a randomized controlled trial. Journal of Aging & Physical Activity 2010;18(4):401‐24. [DOI] [PubMed] [Google Scholar]
Granacher 2009 {published data only}
- Granacher U, Gruber M, Gollhofer A. Resistance training and neuromuscular performance in seniors. International Journal of Sports Medicine 2009;30(9):652‐7. [DOI] [PubMed] [Google Scholar]
Hall 2009 {published data only}
- Hall CD, Miszko T, Wolf SL. Effects of Tai Chi intervention on dual‐task ability in older adults: a pilot study. Archives of Physical Medicine & Rehabilitation 2009;90(3):525‐9. [DOI] [PubMed] [Google Scholar]
Hara 2007 {published data only}
- Hara T, Shimada T. Effects of exercise on the improvement of the physical functions of the elderly. Journal of Physical Therapy Science 2007;19(1):15‐26. [Google Scholar]
Hatzitaki 2009 {published data only}
- Hatzitaki V, Amiridis IG, Nikodelis T, Spiliopoulou S. Direction‐induced effects of visually guided weight‐shifting training on standing balance in the elderly. Gerontology 2009;55(2):145‐52. [DOI] [PubMed] [Google Scholar]
- Hatzitaki V, Voudouris D, Nikodelis T, Amiridis IG. Visual feedback training improves postural adjustments associated with moving obstacle avoidance in elderly women. Gait & posture 2009;29(2):296‐9. [DOI] [PubMed] [Google Scholar]
Henwood 2006 {published data only}
- Henwood TR, Taaffe DR. Short‐term resistance training and the older adult: The effect of varied programmes for the enhancement of muscle strength and functional performance. Clinical Physiology and Functional Imaging 2006;26(5):305‐13. [DOI] [PubMed] [Google Scholar]
Islam 2004 {published data only}
- Islam MM, Nasu E, Rogers ME, Koizumi D, Rogers NL, Takeshima N. Effects of combined sensory and muscular training on balance in Japanese older adults. Preventative Medicine 2004;39(6):1148‐55. [DOI] [PubMed] [Google Scholar]
Iwamoto 2009 {published data only}
- Iwamoto J, Suzuki H, Tanaka K, Kumakubo T, Hirabayashi H, Miyazaki Y, et al. Preventative effect of exercise against falls in the elderly: a randomized controlled trial. Osteoporosis International 2009;20(7):1233‐40. [DOI] [PubMed] [Google Scholar]
Jessup 2003 {published data only}
- Jessup JV, Horne C, Vishen RK, Wheeler D. Effects of exercise on bone density, balance, and self‐efficacy in older women. Biological Research for Nursing 2003;4(3):171‐80. [DOI] [PubMed] [Google Scholar]
Johansson 1991 {published data only}
- Johansson G, Jarnlo G. Balance training in 70‐year‐old women. Physiotherapy Theory and Practice 1991;7(2):121‐5. [Google Scholar]
Kamide 2009 {published data only}
- Kamide N, Shiba Y, Shibata H. Effects on balance, falls, and bone mineral density of a home‐based exercise program without home visits in community‐dwelling elderly women: a randomized controlled trial. Journal of Physiological Anthropology 2009;28(3):115‐22. [DOI] [PubMed] [Google Scholar]
Karinkanta 2007 {published data only}
- Karinkanta S, Heinonen A, Sievanen H, Uusi‐Rasi K, Fogelholm M, Kannus P. Maintenance of exercise‐induced benefits in physical functioning and bone among elderly women. Osteoporosis International 2009;20(4):665‐74. [DOI] [PubMed] [Google Scholar]
- Karinkanta S, Heinonen A, Sievanen H, Uusi‐Rasi K, Pasanen M, Ojala K, et al. A multi‐component exercise regimen to prevent functional decline and bone fragility in home‐dwelling elderly women: Randomized, controlled trial. Osteoporosis International 2007;18(4):453‐62. [DOI] [PubMed] [Google Scholar]
Kim 2009a {published data only}
- Kim H‐D. Effects of Tai Chi exercise on the center of pressure trace during obstacle crossing in older adults who are at a risk of falling. Journal of Physical Therapy Science 2009;21(1):49‐54. [Google Scholar]
Krebs 1998 {published data only}
- Krebs DE, Jette AM, Assmann SF. Moderate exercise improves gait stability in disabled elders. Archives of Physical Medicine & Rehabilitation 1998;79(12):1489‐95. [DOI] [PubMed] [Google Scholar]
Latham 2003 {published data only}
- Latham NK, Anderson CS, Lee A, Bennett DA, Moseley A, Cameron ID. A randomized, controlled trial of quadriceps resistance exercise and vitamin D in frail older people: the Frailty Interventions Trial in Elderly Subjects (FITNESS). Journal of the American Geriatrics Society 2003;51(3):291‐9. [DOI] [PubMed] [Google Scholar]
Lin 2007 {published data only}
- Lin M‐R, Wolf SL, Hwang H‐F, Gong S‐Y, Chen C‐Y. A randomized, controlled trial of fall prevention programs and quality of life in older fallers. Journal of the American Geriatrics Society 2007;55(4):499‐506. [DOI] [PubMed] [Google Scholar]
Liu‐Ambrose 2008 {published data only}
- Liu‐Ambrose T, Donaldson MG, Ahamed Y, Graf P, Cook WL, Close J, et al. Otago home‐based strength and balance retraining improves executive functioning in older fallers: a randomized controlled trial. Journal of the American Geriatrics Society 2008;56(10):1821‐30. [DOI] [PubMed] [Google Scholar]
Logghe 2009 {published data only}
- Logghe IH, Zeeuwe PE, Verhagen AP, Wijnen‐Sponselee RM, Willemsen SP, Bierma‐Zeinstra SM, et al. Lack of effect of Tai Chi Chuan in preventing falls in elderly people living at home: a randomized clinical trial. Journal of the American Geriatrics Society 2009;57(1):70‐5. [DOI] [PubMed] [Google Scholar]
Lord 1995 {published data only}
- Lord S, Ward J, Williams P, Zivanovic E. The effects of a community exercise program on fracture risk factors in older women. Osteoporosis International 1996;6(5):361‐7. [DOI] [PubMed] [Google Scholar]
- Lord SR, Ward JA, Williams P, Strudwick M. The effect of a 12‐month exercise trial on balance, strength, and falls in older women: a randomized controlled trial. Journal of the American Geriatrics Society 1995;43(11):1198‐206. [DOI] [PubMed] [Google Scholar]
- Lord SR, Ward JA, Williams P. Exercise effect of dynamic stability in older women: a randomized controlled trial.. Archives of Physical Medicine & Rehabilitation 1996;77(3):232‐236. [DOI] [PubMed] [Google Scholar]
Lord 2003 {published data only}
- Lord SR, Castell S, Corcoran J, Dayhew J, Matters B, Shan A, et al. The effect of group exercise on physical functioning and falls in frail older people living in retirement villages: a randomized, controlled trial. Journal of the American Geriatrics Society 2003;51(12):1685‐92. [DOI] [PubMed] [Google Scholar]
Lord 2005 {published data only}
- Lord SR, Tiedemann A, Chapman K, Munro B, Murray SM, Sherrington C. The effect of an individualized fall prevention program on fall risk and falls in older people: a randomized, controlled trial. Journal of the American Geriatrics Society 2005;53(8):1296‐304. [DOI] [PubMed] [Google Scholar]
MacRae 1994 {published data only}
- MacRae PG, Feltner ME, Reinsch S. A 1‐year exercise program for older women: Effects on falls, injuries, and physical performance. Journal of Aging & Physical Activity 1994;2(2):127‐145. [Google Scholar]
McGarry 2001 {published and unpublished data}
- McGarry ST, McGuire SK, Magee TM, Bethard HK, FlomMeland CK. The effects of "The Get Off Your Rocker" exercise class on balance. Journal of Geriatric Physical Therapy 2001;24(3):21‐5. [Google Scholar]
McMurdo 1993 {published data only}
- McMurdo ME, Rennie L. A controlled trial of exercise by residents of old people's homes. Age & Ageing 1993;22(1):11‐5. [DOI] [PubMed] [Google Scholar]
Morris 1999 {published data only}
- Morris JN, Fiatarone M, Kiely DK, Belleville Taylor P, Murphy K, et al. Nursing rehabilitation and exercise strategies in the nursing home. Journals of Gerontology Series A‐Biological Sciences & Medical Sciences 1999;54(10):M494‐500. [DOI] [PubMed] [Google Scholar]
Nelson 2004 {published data only}
- Nelson ME, Layne JE, Bernstein MJ, Nuernberger A, Castaneda C, Kaliton D, et al. The effects of multidimensional home‐based exercise on functional performance in elderly people. Journals of Gerontology Series A‐Biological Sciences & Medical Sciences 2004;59(2):154‐60. [DOI] [PubMed] [Google Scholar]
Okumiya 1996 {published data only}
- Okumiya K, Matsubayashi K, Wada T, Kimura S, Doi Y, Ozawa T. Effects of exercise on neurobehavioral function in community‐dwelling older people more than 75 years of age. Journal of the American Geriatrics Society 1996;44(5):569‐72. [DOI] [PubMed] [Google Scholar]
Paillard 2004 {published data only}
- Paillard T, Lafont C, Costes‐Salon M, Rivière D, Dupui P. Effects of brisk walking on static and dynamic balance, locomotion, body composition, and aerobic capacity in ageing healthy active men. International Journal of Sports Medicine 2004;25(7):539‐546. [DOI] [PubMed] [Google Scholar]
Park 2008 {published data only}
- Park H, Kim KJ, Komatsu T, Park SK, Mutoh Y. Effect of combined exercise training on bone, body balance, and gait ability: a randomized controlled study in community‐dwelling elderly women. Journal of Bone & Mineral Metabolism 2008;26(3):254‐9. [DOI] [PubMed] [Google Scholar]
Ramirez Villada 2007 {published data only}
- Ramirez Villada JF, Silva ME, Lancho Alonso JL. Influence of a training programme with jumps on explosive force, speed of movement and dynamic balance in the elderly [Influencia de un programa de entrenamiento con saltos en la fuerza explosiva, la velocidad de movimiento y el equilibrio dinamico de personas mayores]. Revista Espanola de Geriatria y Gerontologia 2007;42(4):218‐26. [Google Scholar]
Ramsbottom 2004 {published data only}
- Ramsbottom R, Ambler A, Potter J, Jordan B, Nevill A, Williams C. The effect of 6 months training on leg power, balance, and functional mobility of independently living adults over 70 years old. Journal of Aging & Physical Activity 2004;12(4):497‐510. [DOI] [PubMed] [Google Scholar]
Reinsch 1992 {published data only}
- Reinsch S, MacRae P, Lachenbruch P, Tobis J. Attempts to prevent falls and injury: a prospective community study. Gerontologist 1992;32(4):450‐6. [DOI] [PubMed] [Google Scholar]
Rooks 1997a {published data only}
- Rooks DS, Kiel DP, Parsons C, Hayes WC. Self‐paced resistance training and walking exercise in community‐dwelling older adults: Effects on neuromotor performance. Journals of Gerontology Series A‐Biological Sciences & Medical Sciences 1997;52(3):M161‐8. [DOI] [PubMed] [Google Scholar]
Rosendahl 2006 {published data only}
- Littbrand H, Rosendahl E, Lindelöf N, Lundin‐Olsson L, Gustafson Y, Nyberg L. A high‐intensity functional weight‐bearing exercise program for older people dependent in activities of daily living and living in residential care facilities: evaluation of the applicability with focus on cognitive function. Physical Therapy 2006;86(4):489‐98. [PubMed] [Google Scholar]
- Rosendahl E, Gustafson Y, Nordin E, Lundin‐Olsson L, Nyberg L. A randomized controlled trial of fall prevention by a high‐intensity functional exercise program for older people living in residential care facilities. Aging Clinical and Experimental Research 2008;20(1):67‐75. [DOI] [PubMed] [Google Scholar]
- Rosendahl E, Lindelöf N, Littbrand H, Yifter‐Lindgren E, Lundin‐Olsson L, Håglin L, et al. High‐intensity functional exercise program and protein‐enriched energy supplement for older persons dependent in activities of daily living: A randomised controlled trial. Australian Journal of Physiotherapy 2006;52:105–13. [DOI] [PubMed] [Google Scholar]
Rubenstein 2000 {published data only}
- Rubenstein LZ, Josephson KR, Trueblood PR, Loy S, Harker JO, Pietruszka FM, et al. Effects of a group exercise program on strength, mobility, and falls among fall‐prone elderly men. Journals of Gerontology Series A‐Biological Sciences & Medical Sciences 2000;55(6):M317‐21. [DOI] [PubMed] [Google Scholar]
Salminen 2009 {published data only}
- Salminen M, Vahlberg T, Sihvonen S, Sjosten N, Piirtola M, Isoaho R, et al. Effects of risk‐based multifactorial fall prevention on postural balance in the community‐dwelling aged: a randomized controlled trial. Archives of Gerontology & Geriatrics 2009;48(1):22‐7. [DOI] [PubMed] [Google Scholar]
Sauvage 1992 {published data only}
- Sauvage LR Jr, Myklebust BM, CrowPan J, Novak S, Millington P, Hoffman, et al. A clinical trial of strengthening and aerobic exercise to improve gait and balance in elderly male nursing home residents. American Journal Physical Medicine & Rehabilitation 1992;71(6):333‐42. [DOI] [PubMed] [Google Scholar]
Schilling 2009 {published data only}
- Schilling BK, Falvo MJ, Karlage RE, Weiss LW, Lohnes CA, Chiu LZ. Effects of unstable surface training on measures of balance in older adults. Journal of Strength & Conditioning Research 2009;23(4):1211‐6. [DOI] [PubMed] [Google Scholar]
Schlicht 2001 {published data only}
- Schlicht J, Camaione DN, Owen SV. Effect of intense strength training on standing balance, walking speed, and sit‐to‐stand performance in older adults. Journals of Gerontology Series A‐Biological Sciences & Medical Sciences 2001;56(5):M281‐6. [DOI] [PubMed] [Google Scholar]
Schoenfelder 2000 {published data only}
- Schoenfelder DP. A fall prevention program for elderly individuals. Exercise in long‐term care settings. Journal of Gerontology Nursing 2000;26(3):43‐51. [DOI] [PubMed] [Google Scholar]
Schoenfelder 2004 {published data only}
- Schoenfelder DP, Rubenstein LM. An exercise program to improve fall‐related outcomes in elderly nursing home residents. Applied Nursing Research 2004;17(1):21‐31. [DOI] [PubMed] [Google Scholar]
Sherrington 2008a {published data only}
- Sherrington C, Pamphlett PI, Jacka JA, Olivetti LM, Nugent JA, Hall JM, et al. Group exercise can improve participants' mobility in an outpatient rehabilitation setting: a randomized controlled trial. Clinical Rehabilitation 2008;22(6):493‐502. [DOI] [PubMed] [Google Scholar]
Shimada 2004 {published and unpublished data}
- Shimada H, Obuchi S, Furuna T, Suzuki T. New intervention program for preventing falls among frail elderly people: the effects of perturbed walking exercise using a bilateral separated treadmill. American Journal Physical Medicine & Rehabilitation 2004;83(7):493‐9. [DOI] [PubMed] [Google Scholar]
Shin 2009 {published data only}
- Shin KR, Kang Y, Park HJ, Heitkemper M. Effects of exercise program on physical fitness, depression, and self‐efficacy of low‐income elderly women in South Korea. Public Health Nursing 2009;26(6):523‐31. [DOI] [PubMed] [Google Scholar]
Sihvonen 2004 {published data only}
- Sihvonen S, Sipila S, Taskinen S, Era P. Fall incidence in frail older women after individualized visual feedback‐based balance training. Gerontology 2004;50(6):411‐6. [DOI] [PubMed] [Google Scholar]
- Sihvonen SE, Sipila S, Era PA. Changes in postural balance in frail elderly women during a 4‐week visual feedback training: a randomized controlled trial. Gerontology 2004;50(2):87‐95. [DOI] [PubMed] [Google Scholar]
Skelton 1995 {published and unpublished data}
- Skelton DA, Young A, Greig CA, Malbut KE. Effects of resistance training on strength, power, and selected functional abilities of women aged 75 and older. Journal of the American Geriatrics Society 1995;43(10):1081‐7. [DOI] [PubMed] [Google Scholar]
Skelton 1996 {published and unpublished data}
- Skelton DA, McLaughlin AW. Training functional ability in old age. Physiotherapy 1996;82(3):159‐67. [Google Scholar]
Suzuki 2004 {published and unpublished data}
- Suzuki T, Kim H, Yoshida H, Ishizaki T. Randomized controlled trial of exercise intervention for the prevention of falls in community‐dwelling elderly Japanese women. Journal of Bone & Mineral Metabolism 2004;22(6):602‐11. [DOI] [PubMed] [Google Scholar]
Sykes 2004 {published data only}
- Sykes K, Ling WM. Exercise training and fall‐risk prevention for community‐dwelling elders. American Journal of Recreation Therapy 2004;3(2):36‐42. [Google Scholar]
Taaffe 1999 {published data only}
- Taaffe DR, Duret C, Wheeler S, Marcus R. Once‐weekly resistance exercise improves muscle strength and neuromuscular performance in older adults. Journal of the American Geriatrics Society 1999;47(10):1208‐14. [DOI] [PubMed] [Google Scholar]
Taylor‐Piliae 2010 {published data only}
- Taylor‐Piliae RE, Newell KA, Cherin R, Lee MJ, King AC, Haskell WL. Effects of Tai Chi and Western exercise on physical and cognitive functioning in healthy community‐dwelling older adults. Journal of Aging & Physical Activity 2010;18(3):261‐79. [DOI] [PMC free article] [PubMed] [Google Scholar]
Topp 1993 {published data only}
- Topp R, Mikesky A, Wigglesworth J, Holt W Jr, Edwards JE. The effect of a 12‐week dynamic resistance strength training program on gait velocity and balance of older adults. Gerontologist 1993;33(4):501‐6. [DOI] [PubMed] [Google Scholar]
Toraman 2004 {published data only}
- Toraman NF, Erman A, Agyar E. Effects of multicomponent training on functional fitness in older adults. Journal of Aging & Physical Activity 2004;12(4):538‐53. [DOI] [PubMed] [Google Scholar]
Vestergaard 2008 {published data only}
- Vestergaard S, Kronborg C, Puggaard L. Home‐based video exercise intervention for community‐dwelling frail older women: a randomized controlled trial. Aging‐Clinical & Experimental Research 2008;20(5):479‐86. [DOI] [PubMed] [Google Scholar]
Vogler 2009 {published data only}
- Vogler CM, Sherrington C, Ogle SJ, Lord SR. Reducing risk of falling in older people discharged from hospital: a randomized controlled trial comparing seated exercises, weight‐bearing exercises, and social visits. Archives of Physical Medicine & Rehabilitation 2009;90(8):1317‐24. [DOI] [PubMed] [Google Scholar]
Voukelatos 2007 {published data only}
- Voukelatos A, Cumming RG, Lord SR, Rissel C. A randomized, controlled trial of tai chi for the prevention of falls: The central sydney tai chi trial. Journal of the American Geriatrics Society 2007;55(8):1185‐91. [DOI] [PubMed] [Google Scholar]
Vrantsidis 2009 {published data only}
- Vrantsidis F, Hill KD, Moore K, Webb R, Hunt S, Dowson L. Getting Grounded Gracefully: effectiveness and acceptability of Feldenkrais in improving balance. Journal of Aging & Physical Activity 2009;17(1):57‐76. [DOI] [PubMed] [Google Scholar]
Wallsten 2006 {published data only}
- Wallsten SM, Bintrim K, Denman DW, Parrish JM, Hughes G. The effect of Tai Chi Chuan on confidence and lower extremity strength and balance in residents living independently at a continuing care retirement community. Journal of Applied Gerontology 2006;25(1):82‐95. [Google Scholar]
Weerdesteyn 2006 {published data only}
- Weerdesteyn V, Rijken H, Geurts AC, Smits‐Engelsman BC, Mulder T, Duysens J. A five‐week exercise program can reduce falls and improve obstacle avoidance in the elderly. Gerontology 2006;52(3):131‐41. [DOI] [PubMed] [Google Scholar]
Westlake 2007 {published data only}
- Westlake KP, Culham EG. Sensory‐specific balance training in older adults: Effect on proprioceptive reintegration and cognitive demands. Physical Therapy 2007;87(10):1274‐83. [DOI] [PubMed] [Google Scholar]
Wolf 1997 {published data only}
- Wolf SL, Barnhart HX, Ellison GL, Coogler CE. The effect of Tai Chi Quan and computerized balance training on postural stability in older subjects. Physical Therapy 1997;77(4):371‐81. [DOI] [PubMed] [Google Scholar]
- Wolf SL, Kutner NG, Green RC, McNeely E. The Atlanta FICSIT study: Two exercise interventions to reduce frailty in elders. Journal of the American Geriatrics Society 1993;41(3):329‐32. [DOI] [PubMed] [Google Scholar]
Wolf 2001 {published data only}
- Wolf B, Feys H, De W, Meer J, Noom M, Aufdemkampe G, et al. Effect of a physical therapeutic intervention for balance problems in the elderly: a single‐blind, randomized, controlled multicentre trial. Clinical Rehabilitation 2001;15(6):624‐36. [DOI] [PubMed] [Google Scholar]
Wolfson 1996 {published data only}
- Wolfson L, Whipple R, Derby C, Judge J, King M, Amerman P, et al. Balance and strength training in older adults: intervention gains and Tai Chi maintenance. Journal of the American Geriatrics Society 1996;44(5):498‐506. [DOI] [PubMed] [Google Scholar]
- Wolfson L, Whipple R, Judge J, Amerman P, Derby C, King M. Training balance and strength in the elderly to improve function. Journal of the American Geriatrics Society 1993;41(3):341‐3. [DOI] [PubMed] [Google Scholar]
Woo 2007 {published data only}
- Woo J, Hong A, Lau E, Lynn H. A randomised controlled trial of Tai Chi and resistance exercise on bone health, muscle strength and balance in community‐living elderly people. Age and Ageing 2007;36(3):262‐8. [DOI] [PubMed] [Google Scholar]
Worm 2001 {published data only}
- Vad E, Worm C, Lauritsen JM, Poulsen PB, Puggaard L, Stovring H, et al. Physical training as treatment of reduced functional ability in frail 75+ year‐olds living at home. A randomized intervention study in general practice with technological assessment elements [Fysisk traening som behandling af nedsat funktionsevne hos svage, hjemmeboende 75+ ‐arige. Et randomiseret interventionsstudie i almen praksis omfattende elementer til en teknologivurdering]. Ugeskrift for Laeger 2002;164(44):5140‐4. [PubMed] [Google Scholar]
- Worm CH, Vad E, Puggaard L, Stovring H, Lauritsen J, Kragstrup J. Effects of a multicomponent exercise program on functional ability in community‐dwelling, frail older adults. Journal of Aging & Physical Activity 2001;9(4):414‐24. [Google Scholar]
Yang 2007 {published data only}
- Yang Y, Verkuilen JV, Rosengren KS, Grubisich SA, Reed MR, Hsiao‐Wecksler ET. Effect of combined Taiji and Qigong training on balance mechanisms: A randomized controlled trial of older adults. Medical Science Monitor 2007;13(8):CR339‐48. [PubMed] [Google Scholar]
Yoo 2010 {published data only}
- Yoo EJ, Jun TW, Hawkins SA. The effects of a walking exercise program on fall‐related fitness, bone metabolism, and fall‐related psychological factors in elderly women. Research in Sports Medicine 2010;18(4):236‐250. [DOI] [PubMed] [Google Scholar]
Zhang 2006a {published data only}
- Zhang JG, Ishikawa‐Takata K, Yamazaki H, Morita T, Ohta T. The effects of Tai Chi Chuan on physiological function and fear of falling in the less robust elderly: An intervention study for preventing falls. Archives of Gerontology and Geriatrics 2006;42(2):107‐16. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Alexander 2001a {published data only}
- Alexander NB, Galecki AT, Grenier ML, Nyquist LV, Hofmeyer MR, Grunawalt JC, et al. Task‐specific resistance training to improve the ability of activities of daily living‐impaired older adults to rise from a bed and from a chair. Journal of the American Geriatrics Society 2001;49(11):1418‐27. [DOI] [PubMed] [Google Scholar]
Alexander 2001b {published data only}
- Alexander NB, Gross MM, Medell JL, Hofmeyer MR. Effects of functional ability and training on chair‐rise biomechanics in older adults. Journals of Gerontology Series A‐Biological Sciences & Medical Sciences 2001;56(9):M538‐47. [DOI] [PubMed] [Google Scholar]
Allen 1999 {published data only}
- Allen A, Simpson JM. A primary care‐based fall prevention programme. Physiotherapy Theory and Practice 1999;15(2):121‐33. [Google Scholar]
Annesi 2004 {published data only}
- Annesi JJ, Gann S, Westcote WW. Preliminary evaluation of a 10‐wk. resistance and cardiovascular exercsie protocol on physiological and psychological measures for a sample of older women. Perceptual and motor skills 2004;98(1):163‐70. [DOI] [PubMed] [Google Scholar]
Anonymous 2002 {published data only}
- Anonymous. Balance is best to prevent falls in the elderly. Medicine Today 2002;3(10):7. [Google Scholar]
Au‐Yeung 2002 {published data only}
- Au‐Yeung SSY, Ho HPY, Lai JWC, Lau RWK, Wong AYL, Lau SK. Did mobility and balance of residents living in private old age homes improve after a mobility exercise programme? A pilot study. Hong Kong Physiotherapy Journal 2002;20:16‐21. [Google Scholar]
Ballard 2004 {published data only}
- Ballard JE, McFarland C, Wallace LS, Holiday DB, Roberson G. The effect of 15 weeks of exercise on balance, leg strength, and reduction in falls in 40 women aged 65 to 89 years. Journal of the American Medical Womens Association 2004;59(4):255‐61. [PubMed] [Google Scholar]
Barnett 2003 {published data only}
- Barnett A, Smith B, Lord SR, Williams M, Baumand A. Community‐based group exercise improves balance and reduces falls in at‐risk older people: A randomised controlled trial. Age & Ageing 2003;32(4):407‐14. [DOI] [PubMed] [Google Scholar]
Barrett 2002 {published data only}
- Barrett C, Smerdely P. A comparison of community‐based resistance exercise and flexibility exercise for seniors. Australian Journal of Physiotherapy 2002;48(3):215‐9. [DOI] [PubMed] [Google Scholar]
Bean 2004 {published data only}
- Bean JF, Herman S, Kiely DK, Frey IC, Leveille SG, Fielding RA, et al. Increased Velocity Exercise Specific to Task (InVEST) training: a pilot study exploring effects on leg power, balance, and mobility in community‐dwelling older women. Journal of the American Geriatrics Society 2004;52(5):799‐804. [DOI] [PubMed] [Google Scholar]
Binder 2002 {published data only}
- Binder EF, Schechtman KB, Ehsani AA, StegerMay K, Brown M, Sinacore DR, et al. Effects of exercise training on frailty in community‐dwelling older adults: results of a randomized, controlled trial. Journal of the American Geriatrics Society 2002;50(12):1921‐8. [DOI] [PubMed] [Google Scholar]
Bissonnette 2010 {published data only}
- Bissonnette DR, Weir PL, Leigh L, Kenno K. The Effects of a Whole‐Body Advanced Vibration Exercise Program on Flexibility, Balance, and Strength in Seniors. Physical & Occupational Therapy in Geriatrics 2010;28(3):225‐34. [Google Scholar]
Bonnefoy 2003 {published data only}
- Bonnefoy M, Cornu C, Normand S, Boutitie F, Bugnard F, Rahmani A, et al. The effects of exercise and protein‐energy supplements on body composition and muscle function in frail elderly individuals: a long‐term controlled randomised study. British Journal of Nutrition 2003;89(5):731‐8. [DOI] [PubMed] [Google Scholar]
Brown 2000 {published data only}
- Brown M, Sinacore DR, Ehsani AA, Binder EF, Holloszy JO, Kohrt WM. Low‐intensity exercise as a modifier of physical frailty in older adults. Archives of Physical Medicine & Rehabilitation 2000;81(7):960‐5. [DOI] [PubMed] [Google Scholar]
Bruyere 2005 {published data only}
- Bruyere O, Wuidart M, Di P, Gourlay M, Ethgen O, Richy F, et al. Controlled whole body vibration to decrease fall risk and improve health‐related quality of life of nursing home residents. Archives of Physical Medicine and Rehabilitation 2005;86(2):303‐7. [DOI] [PubMed] [Google Scholar]
Buchner 1993 {published data only}
- Buchner DM, Cress ME, Wagner EH, Lateur BJ, Price R, Abrass IB. The Seattle FICSIT/MoveIt study: the effect of exercise on gait and balance in older adults. Journal of the American Geriatrics Society 1993;41(3):321‐5. [DOI] [PubMed] [Google Scholar]
Campbell 1999 {published data only}
- Campbell AJ, Robertson MC, Gardner MM, Norton RN, Buchner DM. Falls prevention over 2 years: a randomized controlled trial in women 80 years and older. Age & Ageing 1999;28(6):513‐8. [DOI] [PubMed] [Google Scholar]
Chen 2010 {published data only}
- Chen KM, Fan JT, Wang HH, Wu SJ, Li CH, Lin HS. Silver yoga exercises improved physical fitness of transitional frail elders. Nursing Research 2010;59(5):364‐70. [DOI] [PubMed] [Google Scholar]
Conroy 2010 {published data only}
- Conroy S, Kendrick D, Harwood R, Gladman J, Coupland C, Sach T, et al. A multicentre randomised controlled trial of day hospital‐based falls prevention programme for a screened population of community dwelling older people at high risk of falls. Age and Ageing 2010;39(6):704‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cornillon 2002 {published data only}
- Cornillon E, Blanchon M, Ramboatsisetraina P, Braize C, Beauchet O, Dubost V, et al. Effectiveness of falls prevention strategies for elderly subjects who live in the community with performance assessment of physical activities (before‐after). Annales de Readaptation et de Medecine Physique 2002;45(9):493‐504. [DOI] [PubMed] [Google Scholar]
Cristopoliski 2009 {published data only}
- Cristopoliski F, Barela JA, Leite N, Fowler NE, Rodacki AL. Stretching exercise program improves gait in the elderly. Gerontology 2009;55(6):614‐20. [DOI] [PubMed] [Google Scholar]
Csapo 2009 {published data only}
- Csapo R, Gormasz C, Baron R. Functional performance in community‐dwelling and institutionalized elderly women. Wiener Klinische Wochenschrift 2009;121(11‐12):383‐90. [DOI] [PubMed] [Google Scholar]
Day 2002 {published data only}
- Day L, Fildes B, Gordon I, Fitzharris M, Flamer H, Lord S. Randomised factorial trial of falls prevention among older people living in their own homes. BMJ 2002;325(7356):128. [DOI] [PMC free article] [PubMed] [Google Scholar]
Delbaere 2006 {published data only}
- Delbaere K, Bourgois J, Noortgate N, Vanderstraeten G, Willems T, Cambier D. A home‐based multidimensional exercise program reduced physical impairment and fear of falling. Acta Clinica Belgica 2006;61(6):340‐50. [DOI] [PubMed] [Google Scholar]
Delbaere 2010 {published data only}
- Delbaere K, Close JC, Heim J, Sachdev PS, Brodaty H, Slavin MJ, et al. A multifactorial approach to understanding fall risk in older people. Journal of the American Geriatrics Society 2010;58(9):1679‐85. [DOI] [PubMed] [Google Scholar]
Devereux 2005 {published data only}
- Devereux K, Robertson D, Briffa NK. Effects of a water‐based program on women 65 years and over: a randomised controlled trial. Australian Journal of Physiotherapy 2005;51(2):102‐8. [DOI] [PubMed] [Google Scholar]
DeVito 2003 {published data only}
- DeVito CA, Morgan RO, Duque M, Abdel‐Moty E, Virnig BA. Physical performance effects of low‐intensity exercise among clinically defined high‐risk elders. Gerontology 2003;49(3):146‐54. [DOI] [PubMed] [Google Scholar]
De Vreede 2004 {published data only}
- Vreede PL, Samson MM, Meeteren NL, Bom JG, Duursma SA, Verhaar HJ. Functional tasks exercise versus resistance exercise to improve daily function in older women: a feasibility study. Archives of Physical Medicine and Rehabilitation 2004;85(12):1952‐61. [DOI] [PubMed] [Google Scholar]
Dyer 2004 {published data only}
- Dyer CAE, Taylor GJ, Reed M, Dyer CA, Robertson DR, Harrington R. Falls prevention in residential care homes: a randomised controlled trial. Age & Ageing 2004;33(6):596‐602. [DOI] [PubMed] [Google Scholar]
Earles 2001 {published data only}
- Earles DR, Judge JO, Gunnarsson OT. Velocity training induces power‐specific adaptations in highly functioning older adults. Archives of Physical Medicine and Rehabilitation 2001;82(7):872‐8. [DOI] [PubMed] [Google Scholar]
Fiatarone 1993 {published data only}
- Fiatarone MA, O'Neill EF, Doyle N, Clements KM, Roberts SB, Kehayias JJ, et al. The Boston FICSIT study: the effects of resistance training and nutritional supplementation on physical frailty in the oldest old. Journal of the American Geriatrics Society 1993;41(3):333‐7. [DOI] [PubMed] [Google Scholar]
Gatts 2007 {published data only}
- Gatts SK, Woollacott MH. How Tai Chi improves balance: Biomechanics of recovery to a walking slip in impaired seniors. Gait and Posture 2007;25(2):205‐14. [DOI] [PubMed] [Google Scholar]
Gill 2002 {published data only}
- Gill TM, Baker DI, Gottschalk M, Peduzzi PN, Allore H, Byers A. A program to prevent functional decline in physically frail, elderly persons who live at home. New England Journal of Medicine 2002;347(14):1068‐74. [DOI] [PubMed] [Google Scholar]
Gitlin 2006 {published data only}
- Gitlin LN, Winter L, Dennis MP, Corcoran M, Schinfeld S, Hauck WW. A randomized trial of a multicomponent home intervention to reduce functional difficulties in older adults. Journal of the American Geriatrics Society 2006;54(5):809‐16. [DOI] [PubMed] [Google Scholar]
Granacher 2010 {published data only}
- Granacher U, Muehlbauer T, Bridenbaugh S, Bleiker E, Wehrle A, Kressig RW. Balance training and multi‐task performance in seniors. International Journal of Sports Medicine 2010;31(5):353‐8. [DOI] [PubMed] [Google Scholar]
Gras 2004 {published data only}
- Gras LZ, Levangie PK, GoodwinSegal M, Lawrence DA. A comparison of hip versus ankle exercises in elders and the influence on balance and gait. Journal of Geriatric Physical Therapy 2004;27(2):39‐46. [Google Scholar]
Greendale 2000 {published data only}
- Greendale GA, Salem GJ, Young JT, Damesyn M, Marion M, Wang M, et al. A randomized trial of weighted vest use in ambulatory older adults: strengths, performance, and quality of life outcomes. Journal of the American Geriatrics Society 2000;48(3):305‐11. [DOI] [PubMed] [Google Scholar]
Gu 2006 {published data only}
- Gu MO, Jeon MY, Eun Y. The development & effect of a tailored fall prevention exercise for older adults. Journal of Korean Academic Nursing 2006;36(2):341‐352. [DOI] [PubMed] [Google Scholar]
Haines 2007 {published data only}
- Haines TP, Hill KD, Bennell KL, Osborne RH. Additional exercise for older subacute hospital inpatients to prevent falls: Benefits and barriers to implementation and evaluation. Clinical Rehabilitation 2007;21(8):742‐53. [DOI] [PubMed] [Google Scholar]
Hallage 2010 {published data only}
- Hallage T, Krause MP, Haile L, Miculis CP, Nagle EF, Reis RS, et al. The effects of 12 weeks of step aerobics training on functional fitness of elderly women. Journal of Strength and Conditioning Research 2010;24(8):2261‐6. [DOI] [PubMed] [Google Scholar]
Hauer 2003 {published data only}
- Hauer K, Pfisterer M, Schuler M, Bartsch P, Oster P. Two years later: a prospective long‐term follow‐up of a training intervention in geriatric patients with a history of severe falls. Archives of Physical Medicine & Rehabilitation 2003;84(10):1426‐32. [DOI] [PubMed] [Google Scholar]
Helbostad 2004a {published data only}
- Helbostad JL, Moe‐Nilssen R, Sletvold O. Comparison of two types of exercise regimes on selected functional abilities for community‐dwelling elderly at risk of falling. XVI th Conference of the International Society for Postural and Gait Research; 2003 Mar 23‐27; New South Wales (Australia). www.powmri.edu.au/ispg2003/ISPG2003/ISPG2003.htm.
- Helbostad JL, Sletvold O, MoeNilssen R. Home training with and without additional group training in physically frail old people living at home: effect on health‐related quality of life and ambulation. Clinical Rehabilitation 2004;18(5):498‐508. [DOI] [PubMed] [Google Scholar]
Helbostad 2004b {published data only}
- Helbostad JL, Sletvold O, Moe‐Nilssen R. Effects of home exercises and group training on functional abilities in home‐dwelling older persons with mobility and balance problems. A randomized study. Aging‐Clinical & Experimental Research 2004;16(2):113‐21. [DOI] [PubMed] [Google Scholar]
Hinman 2002 {published data only}
- Hinman MR. Comparison of two short‐term balance training programs for community‐dwelling older adults. Journal of Geriatric Physical Therapy 2002;25(3):10‐15, 20. [Google Scholar]
Hinman 2006 {published data only}
- Hinman MR, O'Connell JK, Graves L, Maples J, Staton K. Comparison of changes in upper extremity strength, function, and balance in older adults who exercise with Thera‐Band(Tm) vs. Bodyblade(Tm). Journal of Geriatric Physical Therapy 2006;29(3):123‐4. [Google Scholar]
Hornbrook 1993 {published data only}
- Hornbrook MC, Stevens VJ, Wingfield DJ. Seniors' Program for Injury Control and Education. Journal of the American Geriatrics Society 1993;41(3):309‐14. [DOI] [PubMed] [Google Scholar]
Hu 1994 {published data only}
- Hu M, Woollacott MH. Multisensory training of standing balance in older adults: I. Postural stability and one‐leg stance balance. Journal of Gerontology 1994;49(2):M52‐61. [DOI] [PubMed] [Google Scholar]
Huang 2010 {published data only}
- Huang H, Liu C, Huang Y, Kernohan WG. Community‐based interventions to reduce falls among older adults in Taiwan ‐ long time follow‐up randomised controlled study. Journal of Clinical Nursing 2010;19(7‐8):959‐68. [DOI] [PubMed] [Google Scholar]
Jones 1992 {published data only}
- Jones CJ, Robichaux J, Williams P, Rikli R. The effects of a 16‐week exercise program on the dynamic balance of older adults. Journal of Clinical & Experimental Gerontology 1992;14(2):165‐82. [Google Scholar]
Judge 1993a {published data only}
- Judge JO, Lindsey C, Underwood M, Winsemius D. Balance improvements in older women: effects of exercise training. Including commentary by Keshner EA with author response. Physical Therapy 1993;73(4):254‐265. [DOI] [PubMed] [Google Scholar]
Judge 1993b {published data only}
- Judge JO, Underwood M, Gennosa T. Exercise to improve gait velocity in older persons. Archives of Physical Medicine & Rehabilitation 1993;74(4):400‐6. [PubMed] [Google Scholar]
Judge 1994 {published data only}
- Judge JO, Whipple RH, Wolfson LI. Effects of resistive and balance exercises on isokinetic strength in older persons. Journal of the American Geriatrics Society 1994;42(9):937‐46. [DOI] [PubMed] [Google Scholar]
Kamijo 2009 {published data only}
- Kamijo T, Murakami M. Regular physical exercise improves physical motor functions and biochemical markers in middle‐age and elderly women. Journal of Physical Activity & Health 2009;6(1):55‐62. [DOI] [PubMed] [Google Scholar]
Kato 2006 {published data only}
- Kato M, Izumi K, Hiramatsu T, Shogenji M. Development of an exercise program for fall prevention for elderly persons in a long term care facility. Japan Journal of Nursing Science 2006;3(2):107‐17. [Google Scholar]
Kawanabe 2007 {published data only}
- Kawanabe K, Kawashima A, Sashimoto I, Takeda T, Sato Y, Iwamoto J. Effect of whole‐body vibration exercise and muscle strengthening, balance, and walking exercises on walking ability in the elderly. Keio Journal of Medicine 2007;56(1):28‐33. [DOI] [PubMed] [Google Scholar]
Kim 2009b {published data only}
- Kim H‐D, Han J‐T, Cho Y‐H. The effectiveness of community‐based Tai Chi training on balance control during stair descent by older adults. Journal of Physical Therapy Science 2009;21(4):317‐23. [Google Scholar]
King 2002 {published data only}
- King MB, Whipple RH, Gruman CA, Judge JO, Schmidt JA, Wolfson LI. The performance enhancement project: Improving physical performance in older persons. Archives of Physical Medicine & Rehabilitation 2002;83(8):1060‐9. [DOI] [PubMed] [Google Scholar]
Kloubec 2010 {published data only}
- Kloubec JA. Pilates for improvement of muscle endurance, flexibility, balance, and posture. Journal of Strength & Conditioning Research 2010;24(3):661‐7. [DOI] [PubMed] [Google Scholar]
Kolbe‐Alexander 2006 {published data only}
- Kolbe‐Alexander TL, Lambert EV, Charlton KE. Effectiveness of a community based low intensity exercise program for older adults. Journal of Nutrition, Health & Aging 2006;10(1):21‐9. [PubMed] [Google Scholar]
Kovacs 2004 {published data only}
- Kovacs C, Williams K. Sensory training effects on obstacle avoidance in healthy older adults. Physical Occupational Therapy in Geriatrics 2004;22(3):1‐17. [Google Scholar]
Kutner 1997 {published data only}
- Kutner NG, Barnhart H, Wolf SL, McNeely E, Xu T. Self‐report benefits of Tai Chi practice by older adults. Journals of Gerontology Series B‐Psychological Sciences & Social Sciences 1997;52B(5):P242‐6. [DOI] [PubMed] [Google Scholar]
LaStayo 2003 {published data only}
- LaStayo PC, Ewy GA, Pierotti DD, Johns RK, Lindstedt S. The positive effects of negative work: increased muscle strength and decreased fall risk in a frail elderly population. Journals of Gerontology Series A‐Biological Sciences & Medical Sciences 2003;58(5):M419‐24. [DOI] [PubMed] [Google Scholar]
Latham 2001 {published data only}
- Latham NK, Stretton C, Ronald M. Progressive resistance strength training in hospitalised older people: a preliminary investigation. New Zealand Journal of Physiotherapy 2001;29(2):41‐8. [Google Scholar]
Lazowski 1999 {published data only}
- Lazowski DA, Ecclestone NA, Myers AM, Paterson DH, Tudor Locke C, Fitzgerald C, et al. A randomized outcome evaluation of group exercise programs in long‐term care institutions. Journal of Gerontology 1999;54(12):M621‐8. [DOI] [PubMed] [Google Scholar]
Lee 2010 {published data only}
- Lee E. The effect of Self‐Help Tai Chi over 16 weeks in community program for older adults Korean American women [Korean].. Korean Journal of Women Health Nursing 2010;16(1):87‐94. [DOI] [PubMed] [Google Scholar]
Lelard 2010 {published data only}
- Lelard T, Doutrellot PL, David P, Ahmaidi S. Effects of a 12‐week Tai Chi Chuan program versus a balance training program on postural control and walking ability in older people. Archives of Physical Medicine & Rehabilitation 2010;91(1):9‐14. [DOI] [PubMed] [Google Scholar]
Li 2002 {published data only}
- Li F, Fisher KJ, Harmer P, Mcauley E. Delineating the impact of Tai Chi training on physical function among the elderly. American Journal of Preventive Medicine 2002;23(2 Suppl):92‐7. [DOI] [PubMed] [Google Scholar]
Li 2005a {published data only}
- Li F, Fisher KJ, Harmer P. Improving physical function and blood pressure in older adults through cobblestone mat walking: A randomized trial. Journal of the American Geriatrics Society 2005;53(8):1305‐12. [DOI] [PubMed] [Google Scholar]
Li 2005b {published data only}
- Li F, Harmer P, Fisher KJ, Mcauley E, Chaumeton N, Eckstrom E, et al. Tai Chi and fall reductions in older adults: A randomized controlled trial. Journals of Gerontology Series A‐Biological Sciences & Medical Sciences 2005;60(2):187‐94. [DOI] [PubMed] [Google Scholar]
- Li F, Harmer P, Fisher KJ, Mcauley E. Tai Chi: Improving functional balance and predicting subsequent falls in older persons. Medicine & Science in Sports & Exercise 2004;36(12):2046‐52. [DOI] [PubMed] [Google Scholar]
Li 2007 {published data only}
- Li Y, Devault C N, Oteghen S. Effects of extended Tai Chi intervention on balance and selected motor functions of the elderly. American Journal of Chinese Medicine 2007;35(3):383‐91. [DOI] [PubMed] [Google Scholar]
Lichtenstein 1989 {published data only}
- Lichtenstein MJ, Shields SL, Shiavi RG, Burger MC. Exercise and balance in aged women: a pilot controlled clinical trial. Archives of Physical Medicine & Rehabilitation 1989;70(2):138‐43. [PubMed] [Google Scholar]
Lin 2006 {published data only}
- Lin M‐R, Hwang H‐F, Wang Y‐W, Chang S‐H, Wolf SL. Community‐based tai chi and its effect on injurious falls, balance, gait, and fear of falling in older people. Physical Therapy 2006;86(9):1189‐201. [DOI] [PubMed] [Google Scholar]
Lindemann 2004 {published data only}
- Lindemann U, Rupp K, Muche R, Nikolaus T, Becker C. Improving balance by improving motor skills. Zeitschrift fur Gerontologie und Geriatrie 2004;37(1):20‐6. [DOI] [PubMed] [Google Scholar]
Liu‐Ambrose 2004 {published data only}
- Liu‐Ambrose T, Khan KM, Eng JJ, Lord SR, McKay HA. Balance confidence improves with resistance or agility training. Increase is not correlated with objective changes in fall risk and physical abilities. Gerontology 2004;50(6):373‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liu‐Ambrose 2010 {published data only}
- Liu‐Ambrose T, Nagamatsu LS, Graf P, Beattie BL, Ashe MC, Handy TC. Resistance training and executive functions: a 12‐month randomized controlled trial. Archives of Internal Medicine 2010;170(2):170‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Luukinen 2007 {published data only}
- Luukinen H, Lehtola S, Jokelainen J, Vaananen‐Sainio R, Lotvonen S, Koistinen P. Pragmatic exercise‐oriented prevention of falls among the elderly: A population‐based, randomized, controlled trial. Preventive Medicine 2007;44(3):265‐71. [DOI] [PubMed] [Google Scholar]
- Luukinen H, Lehtola S, Jokelainen J, Vaananen‐Sainio R, Lotvonen S, Koistinen P. Prevention of disability by exercise among the elderly: A population‐based, randomized, controlled trial. Scandinavian Journal of Primary Health Care 2006;24(4):199‐205. [DOI] [PubMed] [Google Scholar]
Mahoney 2007 {published data only}
- Mahoney JE, Shea TA, Przybelski R, Jaros L, Gangnon R, Cech S, et al. Kenosha County falls prevention study: a randomized, controlled trial of an intermediate‐intensity, community‐based multifactorial falls intervention. Journal of the American Geriatrics Society 2007;55(4):489‐98. [DOI] [PubMed] [Google Scholar]
Marigold 2005 {published data only}
- Marigold DS, Eng JJ, Dawson AS, Inglis JT, Harris, Gylfadottir S. Exercise leads to faster postural reflexes, improved balance and mobility, and fewer falls in older persons with chronic stroke. Journal of the American Geriatrics Society 2005;53(3):416‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
McMurdo 1994 {published data only}
- McMurdo ME, Rennie LM. Improvements in quadriceps strength with regular seated exercise in the institutionalized elderly. Archives of Physical Medicine & Rehabilitation 1994;75(5):600‐3. [PubMed] [Google Scholar]
McMurdo 2000 {published data only}
- McMurdo M, Millar A, Daly F. A randomized controlled trial of fall prevention strategies in old peoples' homes. Gerontology 2000;46(2):83‐7. [DOI] [PubMed] [Google Scholar]
Means 1996 {published data only}
- Means KM, Rodell DE, O'Sullivan PS, Cranford LA. Rehabilitation of elderly fallers: pilot study of a low to moderate intensity exercise program. Archives of Physical Medicine & Rehabilitation 1996;77(10):1030‐6. [DOI] [PubMed] [Google Scholar]
Means 2005 {published data only}
- Means KM, Rodell DE, O'Sullivan PS. Balance, mobility, and falls among community‐dwelling elderly persons: effects of a rehabilitation exercise program. American Journal of Physical Medicine & Rehabilitation 2005;84(4):238‐50. [DOI] [PubMed] [Google Scholar]
Messier 2000 {published data only}
- Messier SP, Royer TD, Craven TE, O'Toole ML, Burns R, Ettinger WH Jr. Long‐term exercise and its effect on balance in older, osteoarthritic adults: Results from the fitness, arthritis, and seniors trial (FAST). Journal of the American Geriatrics Society 2000;48(2):131‐8. [DOI] [PubMed] [Google Scholar]
Morey 2008 {published data only}
- Morey MC, Peterson MJ, Pieper CF, Sloane R, Crowley GM, Cowper P, et al. Project LIFE ‐ Learning to Improve Fitness and Function in Elders: Methods, design and baseline characteristics of randomized trial. Journal of Rehabilitation Research & Development 2008;45(1):31‐42. [DOI] [PubMed] [Google Scholar]
Morgan 2004 {published data only}
- Morgan RO, Virnig BA, Duque M, Abdel‐Moty E, deVito CA. Low‐intensity exercise and reduction of the risk for falls among at‐risk elders. Journals of Gerontology Series A‐Biological Sciences & Medical Sciences 2004;59(10):1062‐7. [DOI] [PubMed] [Google Scholar]
Mulrow 1994 {published data only}
- Mulrow CD, Gerety MB, Kanten D, Cornell JE, DeNino LA, Chiodo L, et al. A randomized trial of physical rehabilitation for very frail nursing home residents. JAMA 1994;271(7):519‐24. [PubMed] [Google Scholar]
Nakamura 2007 {published data only}
- Nakamura Y, Tanaka K, Yabushita N, Sakai T, Shigematsu R. Effects of exercise frequency on functional fitness in older adult women. Archives of Gerontology and Geriatrics 2007;44(2):163‐73. [DOI] [PubMed] [Google Scholar]
Nitz 2004 {published data only}
- Nitz JC, Choy NL. The efficacy of a specific balance‐strategy training programme for preventing falls among older people: A pilot randomised controlled trial. Age & Ageing 2004;33(1):52‐8. [DOI] [PubMed] [Google Scholar]
Nnodim 2006 {published data only}
- Nnodim JO, Strasburg D, Nabozny M, Nyquist L, Galecki A, Chen S, et al. Dynamic balance and stepping versus tai chi training to improve balance and stepping in at‐risk older adults. Journal of the American Geriatrics Society 2006;54(12):1825‐31. [DOI] [PubMed] [Google Scholar]
Ourania 2003 {published data only}
- Ourania M, Yvoni H, Christos K, Ionannis T. Effects of a physical activity program. The study of selected physical abilities among elderly women. Journal of Gerontological Nursing 2003;29(7):50‐5. [DOI] [PubMed] [Google Scholar]
Paillard 2005 {published data only}
- Paillard T, Lafont C, Soulat JM, Montoya R, Costes‐Salon MC, Dupui P. Short‐term effects of electrical stimulation superimposed on muscular voluntary contraction in postural control in elderly women. Journal of Strength & Conditioning Research 2005;19(3):640‐6. [DOI] [PubMed] [Google Scholar]
Pijnappels 2008 {published data only}
- Pijnappels M, Reeves ND, Maganaris CN, Dieen JH. Tripping without falling; lower limb strength, a limitation for balance recovery and a target for training in the elderly. Journal of Electromyography & Kinesiology 2008;18(2):188‐96. [DOI] [PubMed] [Google Scholar]
Prasansuk 2004 {published data only}
- Prasansuk S, Siriyananda C, Nakorn AN, Atipas S, Chongvisal S. Balance disorders in the elderly and the benefit of balance exercise. Journal of the Medical Association of Thailand 2004;87(10):1225‐33. [PubMed] [Google Scholar]
Ramsey 2003 {published data only}
- Ramsey VK, Blasch BB, Kita A. Effects of mobility training on gait and balance. Journal of Visual Impairment & Blindness 2003;97(11):720‐6. [Google Scholar]
Rees 2007 {published data only}
- Rees S, Murphy A, Watsford M. Effects of vibration exercise on muscle performance and mobility in an older population. Journal of Aging & Physical Activity 2007;15(4):367‐81. [DOI] [PubMed] [Google Scholar]
Ribeiro 2009 {published data only}
- Ribeiro F, Teixeira F, Brochado G, Oliveira J. Impact of low cost strength training of dorsi‐ and plantar flexors on balance and functional mobility in institutionalized elderly people. Geriatrics & Gerontology International 2009;9(1):75‐80. [DOI] [PubMed] [Google Scholar]
Robbins 2001 {published data only}
- Robbins JA. A home‐based, nurse‐delivered exercise program reduced falls and serious injuries in persons greater than or equal to 80 years of age. American College of Physicians Journal Club 2001;135(3):100. [Google Scholar]
Rochat 2008 {published data only}
- Rochat S, Martin E, Piot‐Ziegler C, Najafi B, Aminian K, Bula CJ. Falls self‐efficacy and gait performance after gait and balance training in older people. Journal of the American Geriatrics Society 2008;56(6):1154‐6. [DOI] [PubMed] [Google Scholar]
Rooks 1997b {published data only}
- Rooks DS, Ransil BJ, Hayes WC. Self‐paced exercise and neuromotor performance in community‐dwelling older adults. Journal of Aging & Physical Activity 1997;5(2):135‐49. [Google Scholar]
Rugelj 2010 {published data only}
- Rugelj D. The effect of functional balance training in frail nursing home residents. Archives of Gerontology & Geriatrics 2010;50(2):192‐7. [DOI] [PubMed] [Google Scholar]
Ryushi 2000 {published data only}
- Ryushi T, Kumagai K, Hayase H, Abe T, Shibuya K, Ono A. Effect of resistive knee extension training on postural control measures in middle aged and elderly persons. Journal of Physiological Anthropology & Applied Human Science 2000;19(3):143‐9. [DOI] [PubMed] [Google Scholar]
Sattin 2005 {published data only}
- Sattin RW, Easley KA, Wolf SL, Chen Y, Kutner MH. Reduction in fear of falling through intense tai chi exercise training in older, transitionally frail adults. Journal of the American Geriatrics Society 2005;53(7):1168‐78. [DOI] [PubMed] [Google Scholar]
- Wolf B, Feys H, Weerdt W, Meer J, Noom M, Aufdemkampe G, et al. Effect of a physical therapeutic intervention for balance problems in the elderly: a single‐blind, randomized, controlled multicentre trial. Clinical Rehabilitation 2001;15(6):624‐36. [DOI] [PubMed] [Google Scholar]
- Wolf SL, Sattin RW, Kutner M, O'Grady M, Greenspan AI, Gregor RJ. Intense tai chi exercise training and fall occurrences in older, transitionally frail adults: a randomized, controlled trial. Journal of American Geriatrics Society 2003;51(12):1693‐701. [DOI] [PubMed] [Google Scholar]
Sayers 2003 {published data only}
- Sayers SP, Bean J, Cuoco A, LeBrasseur NK, Jette A, Fielding RA. Changes in function and disability after resistance training: does velocity matter? A pilot study. American Journal of Physical Medicine & Rehabilitation 2003;82(8):605‐13. [DOI] [PubMed] [Google Scholar]
Shaughnessy 1998 {published data only}
- Shaughnessy A. Can an in‐home exercise program decrease falls and injuries in elderly women?. Evidence Based Practice 1998;1(2):7, insert 2. [Google Scholar]
Shigematsu 2002 {published data only}
- Shigematsu R, Chang M, Yabushita N, Sakai T, Nakagaichi M, Nho H, et al. Dance‐based aerobic exercise may improve indices of falling risk in older women. Age & Ageing 2002;31(4):261‐6. [DOI] [PubMed] [Google Scholar]
Shimada 2003 {published data only}
- Shimada H, Uchiyama Y, Kakurai S. Specific effects of balance and gait exercises on physical function among the frail elderly. Clinical Rehabilitation 2003;17(5):472‐9. [DOI] [PubMed] [Google Scholar]
Shumway‐Cook 2006 {published data only}
- Shumway‐Cook A, Silver IF, LeMier M, York S, Cummings P, Koepsell TD. The effectiveness of a community‐based multifactorial intervention on falls and fall risk factors in community living older adults: a randomized, controlled trial. Journal of Geriatric Physical Therapy 2006;29(3):117. [DOI] [PubMed] [Google Scholar]
Signorile 2002 {published data only}
- Signorile JF, Carmel MP, Czaja SJ, Asfour SS, Morgan RO, Khalil TM, et al. Differential increases in average isokinetic power by specific muscle groups of older women due to variations in training and testing. Journals of Gerontology Series A‐Biological Sciences & Medical Sciences 2002;57(10):M683‐90. [DOI] [PubMed] [Google Scholar]
Simmons 1996 {published data only}
- Simmons V, Hansen PD. Effectiveness of water exercise on postural mobility in the well elderly: An experimental study on balance enhancement. Journals of Gerontology Series A‐Biological Sciences & Medical Sciences 1996;51(5):M233‐8. [DOI] [PubMed] [Google Scholar]
Simons 2006 {published data only}
- Simons R, Andel R. The effects of resistance training and walking on functional fitness in advanced old age. Journal of Aging & Health 2006;18(1):91‐105. [DOI] [PubMed] [Google Scholar]
Siqueira Rodrigues 2010 {published data only}
- Siqueira Rodrigues BG, Cader SA, Torres NVOB, Oliveira EM, Dantas EHM. Pilates method in personal autonomy, static balance and quality of life of elderly females. Journal of Bodywork & Movement Therapies 2010;14(2):195‐202. [DOI] [PubMed] [Google Scholar]
Siu 2007 {published data only}
- Siu E, Li T‐Y, Lau C‐K, Lam MWF, Lam K‐S, Fung S‐W, et al. An evaluation on the efficacy of "General Exercise for the Elders" on endurance, strength, balance, flexibility and quality of life. Hong Kong Practitioner 2007;29(9):334‐45. [Google Scholar]
Skelton 1999 {published data only}
- Skelton DA, Dinan SM. Exercise for falls management: rationale for an exercise programme aimed at reducing postural instability. Physiotherapy Theory & Practice 1999;15(2):105‐20. [Google Scholar]
Sohng 2003 {published data only}
- Sohng K, Moon J, Song H, Lee K, Kim Y. Fall prevention exercise program for fall risk factor reduction of the community‐dwelling elderly in Korea. Yonsei Medical Journal 2003;44(5):883‐91. [DOI] [PubMed] [Google Scholar]
Steadman 2003 {published data only}
- Steadman J, Donaldson N, Kalra L. A randomized controlled trial of an enhanced balance training program to improve mobility and reduce falls in elderly patients. Journal of the American Geriatrics Society 2003;51(6):847‐52. [DOI] [PubMed] [Google Scholar]
Steinberg 2000 {published data only}
- Steinberg M, Cartwright C, Peel N, Williams G. A sustainable programme to prevent falls and near falls in community dwelling older people: results of a randomised trial [with consumer summary]. Journal of Epidemiology & Community Health 2000;54(3):227‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Suarez 2006 {published data only}
- Suarez H, Suarez A, Lavinsky L. Postural adaptation in elderly patients with instability and risk of falling after balance training using a virtual‐reality system. International Tinnitus Journal 2006;12(1):41‐4. [PubMed] [Google Scholar]
Sung 2007 {published data only}
- Sung K W. The effect of a health maintenance program on physical function and mental health of the elderly in nursing homes. Daehan Ganho Haghoeji 2007;37(4):478‐89. [DOI] [PubMed] [Google Scholar]
Szturm 1994 {published data only}
- Szturm T, Ireland D, Lessing‐Turner M. Comparison of different exercise programs in the rehabilitation of patients with chronic peripheral vestibular dysfunction. Journal of Vestibular Research 1994;4(6):461‐79. [PubMed] [Google Scholar]
Taguchi 2010 {published data only}
- Taguchi N, Higaki Y, Inoue S, Kimura H, Tanaka K. Effects of a 12‐month multicomponent exercise program on physical performance, daily physical activity, and quality of life in very elderly people with minor disabilities: an intervention study. Journal of Epidemiology 2010;20(1):21‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Timonen 2002 {published data only}
- Timonen L, Rantanen T, Ryynanen OP, Taimela S, Timonen TE, Sulkava R. A randomized controlled trial of rehabilitation after hospitalization in frail older women: effects on strength, balance and mobility. Scandinavian Journal of Medicine & Science in Sports 2002;12(3):186‐92. [DOI] [PubMed] [Google Scholar]
Timonen 2006 {published data only}
- Timonen L, Rantanen T, Makinen E, Timonen TE, Tormakangas T, Sulkava R. Effects of a group‐based exercise program on functional abilities in frail older women after hospital discharge. Aging‐Clinical & Experimental Research 2006;18(1):50‐6. [DOI] [PubMed] [Google Scholar]
Tinetti 1994 {published data only}
- Tinetti ME, Baker DI, McAvay G, Claus EB, Garrett P, Gottschalk M, et al. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. New England Journal of Medicine 1994;331(13):821‐27. [DOI] [PubMed] [Google Scholar]
Udani 1998 {published data only}
- Udani JK, Ofman JJ. Tai Chi for the prevention of falls in the elderly. Integrative Medicine 1998;1(4):167‐9. [Google Scholar]
Ullmann 2010 {published data only}
- Ullmann G, Williams HG, Hussey J, Durstine JL, McClenaghan BA. Effects of Feldenkrais exercises on balance, mobility, balance confidence, and gait performance in community‐dwelling adults age 65 and older. Journal of Alternative & Complementary Medicine 2010;16(1):97‐105. [DOI] [PubMed] [Google Scholar]
Urbscheit 2001 {published data only}
- Urbscheit NL, Wiegand MR. Effect of two exercise programs on balance scores in elderly ambulatory people. Physical and Occupational Therapy in Geriatrics 2001;19(4):49‐58. [Google Scholar]
Vamos 2001 {published data only}
- Vamos L, Riach C. Strength training and postural stability in healthy older adults. Clinical Kinesiology 2001;55(2):28‐36. [Google Scholar]
Verfaillie 1997 {published data only}
- Verfaillie DF, Nichols JF, Turkel E, Hovell MF. Effects of resistance, balance, and gait training on reduction of risk factors leading to falls in elders. Journal of Aging & Physical Activity 1997;5(3):213‐28. [Google Scholar]
Williams 2002 {published data only}
- Williams K, Mustian K, Kovacs C. A home‐based intervention to improve balance, gait and self‐confidence. Activities, Adaptation & Aging 2002;27(2):1‐16. [Google Scholar]
Wolf 1996 {published data only}
- Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler C, Xu T. Reducing frailty and falls in older persons: an investigation of Tai Chi and computerized balance training. Atlanta FICSIT Group. Frailty and Injuries: Cooperative Studies of Intervention Techniques. Journal of the American Geriatrics Society 1996;44(5):489‐97. [DOI] [PubMed] [Google Scholar]
Wolf 2003 {published data only}
- Wolf SL, Sattin RW, Kutner M, O'Grady M, Greenspan AI, Gregor RJ. Intense Tai Chi exercise training and fall occurrences in older, transitionally frail adults: a randomized, controlled trial. Includes commentary by Lavery L and Studenski S. Journal of the American Geriatrics Society 2003;51(12):1693‐701, 1804‐5. [DOI] [PubMed] [Google Scholar]
Wu 2010 {published data only}
- Wu G, Keyes L, Callas P, Ren X, Bookchin B. Comparison of telecommunication, community, and home‐based Tai Chi exercise programs on compliance and effectiveness in elders at risk for falls. Archives of Physical Medicine & Rehabilitation 2010;91(6):849‐56. [DOI] [PubMed] [Google Scholar]
Yan 2005 {published data only}
- Yan T‐B, Xie R‐H, Guo Y‐H, Jin D‐M, Cao Y‐L. Comparison of the effects of shadowboxing on equilibrium function of healthy elderly women. Zhongguo Linchuang Kangfu (Chinese Journal of Clinical Rehabilitation) 2005;9(4):159‐61. [Google Scholar]
Yan 2009 {published data only}
- Yan T, Wilber KH, Aguirre R, Trejo L. Do sedentary older adults benefit from community‐based exercise? Results from the Active Start program. Gerontologist 2009;49(6):847‐55. [DOI] [PubMed] [Google Scholar]
Yates 2001 {published data only}
- Yates SM, Dunnagan, TA. Evaluating the effectiveness of a home‐based fall risk reduction program for rural community‐dwelling older adults. Journals of Gerontology Series A‐Biological Sciences & Medical Sciences 2001;56(4):M226‐30. [DOI] [PubMed] [Google Scholar]
Zhang 2006b {published data only}
- Zhang T‐M, Tan Y‐M. Comparison of Yangko and Taijiquan in body building in the middle‐ages and elderly women. Chinese Journal of Clinical Rehabilitation 2006;10(36):76‐8. [Google Scholar]
Zisi 2001 {published data only}
- Zisi V, Michalopoulou M, Tzetzis G, Kioumourtzoglou E. Effects of a short‐term exercise program on motor function and whole body reaction time in the elderly. Journal of Human Movement Studies 2001;40(2):145‐60. [Google Scholar]
References to ongoing studies
Frandin 2009 {published data only}
- Frandin K, Borell L, Gronstedt H, Bergland A, Helbostad JL, Puggaard L, et al. A Nordic multi‐center study on physical and daily activities for residents in nursing home settings: design of a randomized, controlled trial. Aging‐Clinical & Experimental Research 2009;21(4‐5):314‐22. [DOI] [PubMed] [Google Scholar]
Leininger 2006 {published data only}
- Leininger P. Physical and psychological effects of yoga exercise on healthy community‐dwelling older adult women. Philadelphia, USA: Temple University, 2006. [Google Scholar]
Additional references
Baker 1985
- Baker SP, Harvey AH. Fall injuries in the elderly. Clinics in Geriatric Medicine 1985;1(3):501‐12. [PubMed] [Google Scholar]
Berg 1989
- Berg K. Balance and its measure in the elderly: A review. Physiotherapy Canada 1989;41(5):240‐6. [Google Scholar]
Berg 1992
- Berg KO, Wood‐Dauphinee SL, Williams JI, Maki B. Measuring balance in the elderly: Validation of an instrument. Canadian Journal of Public Health 1992;83(Suppl 2):S7‐11. [PubMed] [Google Scholar]
Brown 1999
- Brown LA, Shumway‐Cook A, Woollacott MH. Attentional demands and postural recovery: the effects of aging. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 1999;54(4):M165‐71. [DOI] [PubMed] [Google Scholar]
Cameron 2010
- Cameron ID, Murray GR, Gillespie LD, Robertson MC, Hill KD, Cumming RG, Kerse N. Interventions for preventing falls in older people in nursing care facilities and hospitals. Cochrane Database of Systematic Reviews 2010, Issue 1. [DOI: 10.1002/14651858.CD005465.pub2] [DOI] [PubMed] [Google Scholar]
Campbell 1997
- Campbell AJ, Robertson MC, Gardner MM, Norton RN, Tilyard MW, Buchner DM. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ 1997;315(7115):1065‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chandler 1996
- Chandler JM, Hadley EC. Exercise to improve physiologic and functional performance in old age. Clinics in Geriatric Medicine 1996;12(4):761‐84. [PubMed] [Google Scholar]
Cooper 2010
- Cooper R, Kuh D, Hardy R, Mortality Review Group, FALCon and HALCyon Study Teams. Objectively measured physical capability levels and mortality: systematic review and meta‐analysis. BMJ 2010;341:c4467. [DOI: 10.1136/bmj.c4467.] [DOI] [PMC free article] [PubMed] [Google Scholar]
Daubney 1999
- Daubney ME, Culham EG. Lower‐extremity muscle force and balance performance in adults aged 65 years and older. Physical Therapy 1999;79(12):1177‐85. [PubMed] [Google Scholar]
Deeks 2008
- Deeks JJ, Higgins JPT, Altman DG. Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1 (updated September 2008). The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org.
Doherty 1993
- Doherty TJ, Vandervoort AA, Brown WF. Effects of ageing on the motor unit: a brief review. Canadian Journal of Applied Physiology 1993;18(4):331‐58. [DOI] [PubMed] [Google Scholar]
Duncan 1990
- Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: a new clinical measure of balance. Journal of Gerontology 1990;45(6):M192‐7. [DOI] [PubMed] [Google Scholar]
Geiger 2001
- Geiger RA, Allen JB, O'Keefe J, Hicks RR. Balance and mobility following stroke: effects of physical therapy interventions with and without biofeedback/forceplate training. Physical Therapy 2001;81(4):995‐1005. [PubMed] [Google Scholar]
Gillespie 2009
- Gillespie LD, Robertson MC, Gillespie WJ, Lamb SE, Gates S, Cumming RG, Rowe BH. Interventions for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews 2009, Issue 2. [DOI: 10.1002/14651858.CD007146.pub2] [DOI] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated September 2008]. The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org. [Available from www.cochrane‐handbook.org.]
Huxham 2001
- Huxham FE, Goldie PA, Patla AE. Theoretical considerations in balance assessment. Australian Journal of Physiotherapy 2001;47(2):89‐100. [DOI] [PubMed] [Google Scholar]
Lamb 2006
- Lamb S. personal communication 27 November 2006.
Littbrand 2006
- Littbrand H, Rosendahl E, Lindelöf N, Lundin‐Olsson L, Gustafson Y, Nyberg L. A high‐intensity functional weight‐bearing exercise program for older people dependent in activities of daily living and living in residential care facilities: evaluation of the applicability with focus on cognitive function. Physical Therapy 2006;86(4):489‐98. [PubMed] [Google Scholar]
Liu 2009
- Liu CJ, Latham NK. Progressive resistance strength training for improving physical function in older adults. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD002759.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Maki 2005
- Maki BE, McIlroy WE. Change‐in‐support balance reactions in older persons: an emerging research area of clinical importance. Neurologic Clinics 2005;23(3):751‐83. [DOI] [PubMed] [Google Scholar]
Menz 2007
- Menz HB, Lord SR, Fitzpatrick RC. A structural equation model relating impaired sensorimotor function, fear of falling and gait patterns in older people. Gait Posture 2007;25(2):243‐9. [DOI] [PubMed] [Google Scholar]
Merriman 2009
- Merriman H, Jackson K. The effects of whole‐body vibration training in aging adults: a systematic review. Journal of Geriatric Physical Therapy 2009;32(3):134‐45. [DOI] [PubMed] [Google Scholar]
Mills 1994
- Mills EM. The effect of low‐intensity aerobic exercise on muscle strength, flexibility, and balance among sedentary elderly persons. Nursing Research 1994;43(4):207‐11. [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Medicine 2009; Vol. 6, issue 7:e1000097. [DOI: 10.1371/journal.pmed1000097] [DOI] [PMC free article] [PubMed]
Nevitt 1989
- Nevitt MC, Cummings SR, Kidd S, Black D. Risk factors for recurrent nonsyncopal falls: a prospective study. JAMA 1989;261:2663‐8. [PubMed] [Google Scholar]
Podsiadlo 1991
- Podsiadlo D, Richardson S. The timed 'Up and Go': A test of basic functional mobility for frail elderly persons. Journal of the American Geriatric Society. 1991;39(2):142‐8. [DOI] [PubMed] [Google Scholar]
Robertson 2001
- Robertson MC, Devlin N, Gardner MM, Campbell AJ. Effectiveness and economic evaluation of a nurse delivered home based exercise programme to prevent falls. 1: Randomised controlled trial. BMJ 2001;322(7288):697‐701. [DOI] [PMC free article] [PubMed] [Google Scholar]
Robinson 2002
- Robinson KA, Dickerson K. Development of a highly sensitive search strategy for the retrieval of reports of controlled trials using PubMed. International Journal of Epidemiology 2002;31(1):150‐3. [DOI] [PubMed] [Google Scholar]
Rolland 2009
- Rolland Y, Abellan van Kan G, Nourhashemi F, Andrieu S, Cantet C, Guyonnet‐Gillette S, Vellas B. An abnormal "one‐leg balance" test predicts cognitive decline during Alzheimer's disease. Journal of Alzheimers Disease 2009;16(3):525‐31. [DOI] [PubMed] [Google Scholar]
Rose 2005
- Rose DJ. Balance and Mobility Training. In: Jones CJ, Rose DJ editor(s). Physical Activity Instruction of Older Adults. Champaign, Illinois: Human Kinetics, 2005:211‐227. [Google Scholar]
Rosendahl 2008
- Rosendahl E, Gustafson Y, Nordin E, Lundin‐Olsson L, Nyberg L. A randomized controlled trial of fall prevention by a high‐intensity functional exercise program for older people living in residential care facilities. Aging Clinical and Experimental Research 2008;20(1):67‐75. [DOI] [PubMed] [Google Scholar]
Rossat 2010
- Rossat A, Fantino B, Nitenberg C, Annweiler C, Poujol L, Herrmann FR, et al. Risk factors for falling in community‐dwelling older adults: which of them are associated with the recurrence of falls?. Journal of Nutrition, Health and Aging 2010;14(9):787‐91. [DOI] [PubMed] [Google Scholar]
Schulz 2010
- Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. Trials 2010;11:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sherrington 2008b
- Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, Close JC. Effective exercise for the prevention of falls: a systematic review and meta‐analysis. Journal of the American Geriatrics Society 2008;56(12):2234‐43. [DOI] [PubMed] [Google Scholar]
Skelton 2001
- Skelton DA. Effects of physical activity on postural stability. Age and Ageing 2001;30(Suppl 4):33‐9. [DOI] [PubMed] [Google Scholar]
Skelton 2005
- Skelton D, Dinan S, Campbell M, Rutherford O. Tailored Group Exercise (Falls Management Exercise ‐ FaME) reduces falls in community‐dwelling older frequent fallers (an RCT). Age and Ageing 2005;34(6):636‐9. [DOI] [PubMed] [Google Scholar]
Skinner 1984
- Skinner HB, Barrack RL, Cook SD. Age‐related decline in proprioception. Clinical Orthopedics and Related Research 1984;(184):208‐11. [PubMed] [Google Scholar]
Stelmach 1989
- Stelmach GE, Phillips J, DiFabio RP, Teasdale N. Age, functional postural reflexes, and voluntary sway. Journal of Gerontology 1989;44:B100‐6. [DOI] [PubMed] [Google Scholar]
Stelmach 1994
- Stelmach GE. Physical activity and aging: Sensory and perceptual processing. In: Bouchard C, Shepard RJ, Stephens T editor(s). Physical fitness and health. Champaign: Human Kinetics, 1994. [Google Scholar]
Thomas 2010
- Thomas S, Mackintosh S, Halbert J. Does the 'Otago exercise programme' reduce mortality and falls in older adults?: A systematic review and meta analysis. Age and Ageing 2010;39(6):681‐7. [DOI] [PubMed] [Google Scholar]
Tiedemann 2008
- Tiedemann AC, Murray SM, Munro B, Lord SR. Hospital and non‐hospital costs for fall‐related injury in community‐dwelling older people. New South Wales Public Health Bulletin 2008;19(9‐10):161‐5. [DOI] [PubMed] [Google Scholar]
Tinetti 1988
- Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. New England Journal of Medicine 1988;319:1701‐7. [DOI] [PubMed] [Google Scholar]
Walker 2000
- Walker C, Brouwer BJ, Culham EG. Use of visual feedback in retraining balance following acute stroke. Physical Therapy 2000;80(9):886‐95. [PubMed] [Google Scholar]
WHO 2001
- World Health Organization. ICF: International classification of functioning, disability and health. Geneva: World Health Organisation, 2001. [ISBN 9241545429. m] [Google Scholar]
Winter 1995
- Winter DA. ABC: Anatomy, biomechanics and control of balance during standing and walking. Waterloo, Ont: Waterloo Biomechanics, 1995. [Google Scholar]
Wolf 1996
- Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler C, Xu T. Reducing frailty and falls in older persons: an investigation of Tai Chi and computerized balance training. Atlanta FICSIT Group. Frailty and Injuries: Cooperative Studies of Intervention Techniques. Journal of the American Geriatrics Society 1996;44(5):489‐97. [DOI] [PubMed] [Google Scholar]
Zijlstra 2010
- Zijlstra A, Mancini M, Chiari L, Zijlstra W. Biofeedback for training balance and mobility tasks in older populations: a systematic review. Journal of NeuroEngineering and Rehabilitation 2010;7:58‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Howe 2007
- Howe TE, Rochester L, Jackson A, Banks PMH, Blair VA. Exercise for improving balance in older people. Cochrane Database of Systematic Reviews 2007, Issue 4. [DOI: 10.1002/14651858.CD004963.pub2] [DOI] [PubMed] [Google Scholar]


