Abstract
Background:
Brisk walking exercise is an aerobic exercise with the moderate intensity that can reduce the risk in people with hypertension. This systematic review and meta-analysis aimed to investigate the effects of interventions related to brisk walking and blood pressure reduction in hypertensive patients.
Methods:
Search strategy through the PubMed, Science Direct, ProQuest, and Google Scholar databases limited from 2018 to 2023. The components measured are systolic blood pressure and diastolic blood pressure. This study uses the Black and Downs checklist to measure the quality of the study, which consists of 3, namely high quality, medium quality, and low quality. Effect size analysis of the study used the standard mean difference between brisk walking exercise and not doing brisk walking exercise.
Results:
The results of the identification of the database obtained 1700 articles, then limited by title, year, abstract (n = 381), and full-text article feasibility (n = 76) to obtain nine articles included. Nine articles were included in the systematic review and meta-analysis by study quality: six studies of high quality, 2 of medium quality, and 1 of low quality. Systolic blood pressure had a substantial effect size in all studies (P<0.05; SMD: −0.55) while diastolic blood pressure had an effect medium size (P=0.05; SMD: 0.13).
Conclusion:
Brisk walking exercise can significantly reduce blood pressure in people with hypertension—recommendations for the future to carry out community-based physical activity in improving physical health, including heart health.
Keywords: Blood pressure, Brisk walking exercise, Cardiovascular, Hypertension
Introduction
Hypertension is a non-communicable disease and the most critical risk factor for cardiovascular disease related to morbidity and mortality (1).
Hypertension is responsible for death rates worldwide, with as many as 8.5 million deaths from stroke, ischemic heart disease, other vascular diseases, and kidney disease (2). The prevalence of hypertension was found as many as 82% of hypertension sufferers from all over the world live in areas of low and middle-income countries. In India, the prevalence of hypertension was recorded at 30.7%, and in Indonesia, there were 34.1% of hypertension sufferers (1, 3). Hypertension is defined as systolic blood pressure ≥ 140 mmHg and diastolic blood pressure ≥ 90 mmHg or being on hypertension treatment (3).
Based on the theory, hypertension occurs due to pressure changes caused by systemic changes in the peripheral blood flow system and pathogenic mechanisms, namely increased cardiac output (CO) and total peripheral vascular resistance (TPR). In addition, several causes of hypertension are changes in the sympathetic and hormonal nervous system acting to disrupt blood pressure regulation, increased intracellular calcium levels, sodium retention, reversal of hypoxia-induced vasodilation, and increased activity of the renin-angiotensin-aldosterone system (RAAS) (4). Treatment of hypertension is the most critical prevention for cardiovascular and cerebrovascular disease (5).
Hypertension is a lifestyle-related disease; changing unhealthy lifestyles and regular and moderate exercise can help prevent and improve hypertension (6). Pharmacological and nonpharmacological interventions can be carried out in managing hypertension. Non-pharmacological interventions have the benefit of helping to reduce the daily dose of antihypertensive drugs and delay the development of pre-hypertension to hypertension, including lifestyle modifications such as diet, exercise, and avoiding stress (7).
The person’s lifestyle behavior impacts the risk of developing hypertension (8). A healthy lifestyle is a practical approach to preventing and controlling high blood pressure. Physical activity is one of the lifestyle behaviors that can support the prevention of high blood pressure (9). This is based on the two main pillars of proactive disease control by patients and reducing the burden of care recommended by the WHO, namely by establishing healthy eating behaviors and regular involvement in physical exercise (10).
A person lacking physical activity or exercise can cause a buildup of cholesterol, especially LDL (low-density lipoprotein), in the artery walls. Lipoproteins that enter the lining of the blood vessel walls can increase with high blood pressure and increased permeability of the blood vessel walls. Thus, performance on the lining of the blood vessel walls can cause it to malfunction. In people who rarely do physical activity, the heart muscle will work faster every time there is a contraction, and the arteries will be harder when the heart muscle is pumped (11).
Walking is a form of aerobic exercise that can be done daily at moderate or vigorous intensity (12). A brisk, moderate-intensity walking program is recommended and effectively reduces metabolic risk factors (13). Brisk walking training has many benefits for physical fitness with minimal side effects. Doing brisk walking exercises can strengthen leg muscles, increase flexibility and stability of cardinal joints, and improve cardiovascular and respiratory function. The Centers for Disease Control and Prevention (CDC) defines brisk walking as requiring a minimum walking speed of 3.0 miles per hour or 20 min per mile (14).
A limited review of the literature on quasi-experimental research designs showed that performing brisk walking exercises reduced blood pressure in hypertensive patients, with a reduction in systolic blood pressure of approximately 10 mm Hg and diastolic blood pressure of approximately 20 mmHg (11). Recently, various guidelines have recommended walking as many as 10,000 steps a day to improve heart health. Recent systematic reviews and meta-analyses evaluated the relationship between the number of steps and clinical outcomes such as lipid profile or blood pressure. The number of steps is associated with decreased blood pressure (15).
We aimed to conduct a systematic review and meta-analysis of data to evaluate the effects of interventions related to brisk walking and lowering blood pressure in hypertensive patients.
Materials and Methods
This systematic review and meta-analysis was conducted according to the Preferred Reporting Statement Items for Systematic Review and Meta-Analysis Protocol (PRISMA-P) 2015 (16).
Search Strategy
Online literature searches were conducted through PubMed, Science Direct, ProQuest, and Google Scholar databases. The terms used in the search are brisk walking training AND hypertension, brisk walking training AND blood pressure, in English. The search strategy in the database carried out by researchers is limited from 2018 to 2023.
Eligibility criteria
The articles included in this study were full text (original article), an experimental study with a control group, a complete explanation of the intervention provided, and articles published in English. Articles with abstracts without full articles, review articles, conference articles, articles containing poor data on the duration of intervention, and non-randomized controlled trials were excluded from the study.
Study selection
The researcher assessed the eligibility criteria, namely considering the appropriate title, abstract, and year and then included in the study. References and study abstracts are stored in alphabetical order using EndNote software version 21; if repeated references are found, they are deleted. Next, researchers evaluated the full text for eligibility based on inclusion and exclusion criteria. Finally, the articles that entered the final stage to be included in the review left nine articles.
Quality assessment of included studies
Researchers independently assessed study quality using a modified Downs & Black checklist (Table 1). Articles included in this systematic review were evaluated to assess methodological quality and minimize bias. This study used 15 items of the Black and Downs list consisting of reporting (items 1, 2, 3, 5, 6, 7, and 10), external validity (items 11 and 12), internal validity (items 16, 18, and 20), and internal fact confounding (items 21, 22, and 25). Items were scored as 0 (“no”), 1 (“yes”), or 0 (“unable to determine”), except for item 5, scored 0 (“no”), 1 (“partially”), 2 (“yes”). The total score in the study was categorized as high quality with a quality score of ≥ 75%, medium quality, namely 60–74%, and low quality, namely ≤ 60% (17).
Table 1:
Methodological quality of studies based on the Black and Downs checklist
| Author (yr) | Reporting | External Validity | Internal Validity-Bias | Internal Validity - Confounding | Total | Percent (%) | Quality | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||||
| 1 | 2 | 3 | 5 | 6 | 7 | 10 | 11 | 12 | 16 | 18 | 20 | 21 | 22 | 25 | ||||
| Chen et al. (2021) (18) | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 14 | 87,5 | H |
| He et al. (2018) (19) | 1 | 1 | 1 | 2 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 11 | 68,8 | M |
| Humphrey & Ogu (2021) (20) | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 10 | 62,5 | M |
| Kumaravelu (2019) (21) | 1 | 1 | 0 | 2 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 12 | 75 | H |
| Omar et al. (2021) (22) | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 14 | 87,5 | H |
| Rachmawati et al. (2019) (23) | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 9 | 56,3 | L |
| Saavedra et al. (2021) (24) | 1 | 1 | 0 | 2 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 13 | 81,3 | H |
| Xu et al. (2021) (25) | 1 | 0 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 14 | 87,5 | H |
| Zhao & Wang (2021) (6) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 12 | 75 | H |
Abbreviations: H: High, M: Medium, L: Low
Data extraction and analyses
Researchers extracted article information from study data characteristics consisting of the author (year), country, design, sample, intervention description, duration, and outcome. All statistical analyzes, namely heterogeneity and effect size tests in this study, used REVMAN software version 5. The results model used was a 95% confidence interval (CI).
Results
Study characteristics
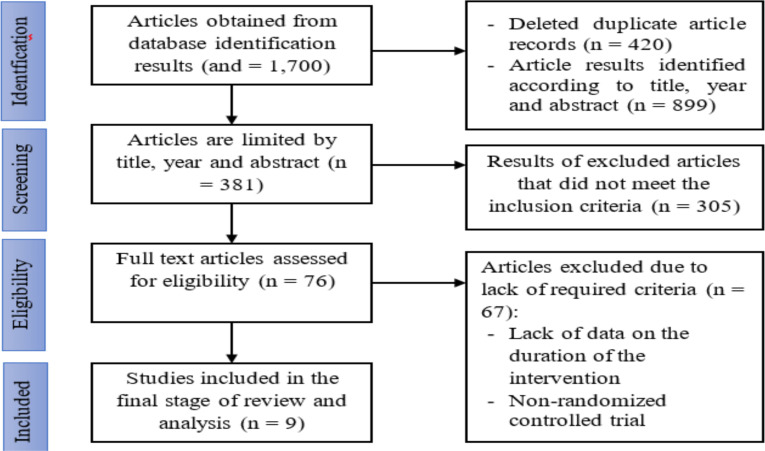
An initial database search identified 1,700 studies (PubMed n = 455, Science Direct n = 421, ProQuest n = 368, and Google Scholar n = 456), 420 of deleted due to duplication. Then, it was re-selected based on title, year, and abstract, leaving 381 studies. We then screened 381 studies based on inclusion criteria, resulting in the deletion of 305 suitable studies. Overall, 76 studies were included as full articles assessed for eligibility, including this systematic review, of which 67 were excluded because they did not meet the eligibility criteria. Finally, nine studies were selected for systematic review and meta-analysis (Fig. 1) (6, 18–25).
Fig. 1:
Literature search flowchart based on PRISMA
Quality assessment of studies
The average score for the quality of the research methodology was 75.7% (range 56.3% - 87.5%), indicating that the quality of the research was high. There were six studies (66.7%) that had a high-quality methodology, two studies (22.2%) had a medium-quality method, and one study (11.1%) had a low-quality procedure. All studies described the research objectives, the statistical tests used were appropriate, and the outcome measures were accurately described. Only four studies reported that study groups were recruited from the same population, and three studies recruited different study groups during a period.
Characteristics of studies
An article search was conducted in Jul 2023. After applying inclusion and exclusion criteria in evaluating the included articles and critically assessing them, nine articles were included in this systematic review and meta-analysis. All selected studies were experimental with a sample population of 908 hypertensive patients (minimum–maximum age of 20–79 yr), with a minimum sample range of 26 people and a maximum of 421 people. One study was published in 2018, two in 2019, and six in 2021. In addition, three studies were conducted in China, 1 in Nigeria, 2 in Malaysia, 1 in India, and 1 in Spain. And 1 in Indonesia (Table 2).
Table 2:
Characteristics of the data from the selected studies
| Author (Year) | Study Quality* | Country | Design | Sample | Intervention Description | Intervention Duration | Outcome | ||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Amount | Gender | Age | |||||||
| Chen et al. (2021) (18) | High | Malaysia | Experimental study | 38 | Female | 20–35 yr | Walk briskly at a distance of 2.2 km for 25–35 min with an intensity of 55% to 75% of the maximum heart rate | 1 time | Resting systolic blood pressure was significantly lower in brisk walking than not brisk walking (P< 0.05) |
| He et al. (2018) (19) | Medium | China | A Pilot study | 26 | Female | 55–60 yr | Fast walking exercise is carried out for 60 min/exercise and is carried out three times a week, 30 meters long, with the Improved six-minute walk test (6MWT) method | 12 wk | Brisk walking can significantly reduce blood pressure and the risk of acute cardiovascular events in elderly patients with essential hypertension (P < 0.05) |
| Humphrey & Ogu (2021) (20) | Medium | Nigeria | Experimental study pre- test and post-test control group | 42 | Male | 36–45 yr | Fast walking exercises are carried out routinely for 150 min daily with an intensity of 50% - 70%. | 12 wk | Shows significant mean reduction in systolic blood pressure (SBP) and diastolic blood pressure (DBP) (P < 0.05) |
| Kumaravelu (2019) (21) | High | India | Experimental study | 30 | Male | 30–40 yr | Exercise consists of a warmup, brisk walking, and cool down for 20–45 min/day | 12 wk | A brisk walking exercise program for 12 wk significantly reduced systolic and diastolic blood pressure at rest (P < 0.01) |
| Omar et al. (2021) (22) | High | Malaysia | Randomized controlled trial study | 70 | Male | 20–40 yr | Exercise brisk walking of 1000 to 8000 steps/day | 12 wk | Pedometer-based brisk walking can significantly reduce blood pressure (P < 0.05) |
| Rachmawati et al. (2019) (23) | Low | Indonesia | Quasi-experiment with non-equivalent control group design pretest and post- test approach | 116 | Female and Male | 40–60 yr | Fast walking exercise for 8 min per session and carried out as many as eight sessions | 2 wk | The brisk walking exercise showed that the average decrease in blood pressure was significant (P < 0.001) |
| Saavedra et al. (2021) (24) | High | Spanish | Quasi-experimental study | 47 | Male | 45 yr | Frequency 3 sessions/week of 30 min duration in the middle of the weekday with > 100 steps/minute throughout the session. | 12 wk | Brisk walking exercises can lower blood pressure |
| Xu et al. (2021) (25) | High | China | A Prospective Study | 421 | Female and Male | 55–79 yr | Fast walking training using the Graded Brisk Walking Test (GBWT) method | 24 wk | A brisk walking program significantly reduced blood pressure (P < 0.05) |
| Zhao & Wang (2021) (6) | High | China | Experimental study pre- test and post-test with the control group | 98 | Female | 55–65 yr | The brisk walking exercise for 30–40 min with an intensity of 65–75% | 3–5 times a week | Effective brisk walking exercise can increase the therapeutic effect on essential hypertension and improve self-management ability for chronic diseases (P < 0.05) |
Quality of studies based on results methodological quality of studies in Table 1
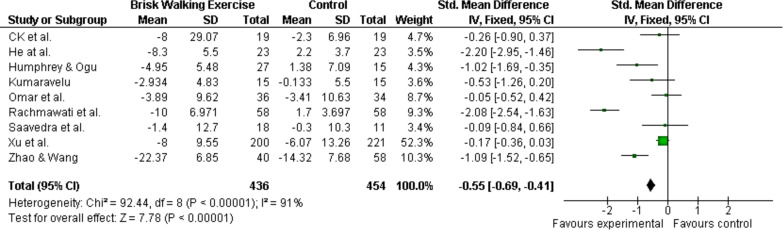
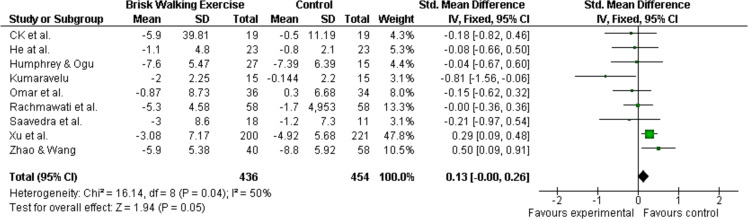
The nine studies evaluated in a meta-analysis, based on solid evidence from the results of the forest plot, showed that hypertensive patients who did brisk walking had a better reduction in blood pressure, both systolic and diastolic blood pressure, compared to the control group. The forest plot of systolic blood pressure shows a strong effect size in all studies (P < 0.05; SMD: −0.55; 95 % CI [−0.69 to −0.41]) (Fig. 2). Whereas in the forest plot, the diastolic blood pressure showed that the effect size was moderate (P = 0.05; SMD: 0.13; 95% CI [−0.00 to 0.26]), that is, out of nine studies, two studies had results better effect size in the control group than the group that did the brisk walking exercise (Fig. 3).
Fig. 2:
The forest plot of systolic blood pressure
Fig. 3:
The forest plot of diastolic blood pressure
Discussion
The current study conducted a systematic review and meta-analysis to evaluate the effects of brisk walking exercise on blood pressure in people with hypertension. The literature search identified a total of nine studies (890 subjects). The results obtained for blood pressure were a significant decrease in systolic blood pressure (systolic blood pressure: −0.55 mmHg) and a reduction in diastolic blood pressure (0.13 mmHg). The difference in mean blood pressure changes to systolic blood pressure was associated with the duration of brisk walking and the number of brisk walking steps.
In these nine studies, four studies did brisk walking exercises of > 10,000 steps in each exercise session (18, 20, 21, 25), and five studies did brisk walking exercises of <10,000 steps (6, 19, 22–24). Walking 10,000 steps improves health-related quality of life (26). In addition, the 10,000-step program also has the efficacy and potential to improve one’s mental health and well-being (26). Other findings reveal that brisk walking can effectively control blood pressure. Still, there is no significant dose-effect relationship between a higher number of steps (> 12,000 steps) with a decrease in blood pressure (27). Other findings reveal that brisk walking can effectively control blood pressure. Still, there is no significant dose-effect relationship between a higher number of steps (> 12,000 steps) with a decrease in blood pressure (28).
Brisk walking exercise is an aerobic exercise with a moderate intensity that can be done at all ages and reduces the risk of hypertension sufferers by helping the body relax, calorie-burning mechanisms, maintaining body weight, and increasing beta-endorphins which can reduce stress. Regular brisk walking exercises will train the muscles, blood, and oxygen circulation in the body to run smoothly so that the body’s metabolism becomes optimal. The body will feel refreshed, and the brain, as the central nervous system, will work better (29, 30). Meanwhile, brisk walking significantly impacts two organ systems, namely the musculoskeletal and cardiovascular, allowing for more efficient oxygen delivery, endurance capacity, and increased performance (31).
Brisk walking is performed by standing straight and looking straight ahead while walking heel to toe on a soft surface (20). Several studies on brisk walking exercises have been carried out; the findings in one of the studies were that the walking speed category is divided into three, namely slow, average, and fast. People who walk fast have a significant association with reduced systolic and diastolic blood pressure, increased levels of vitamin D, and increased glycemia (32).
The results of this study found that the mean difference in systolic blood pressure reduction was better (SMD: −0.55; 95% CI [−0.69 to −0.41]) compared to diastolic blood pressure reduction (SMD: 0.13; 95% CI [−0.00 to 0.26]). Similar findings suggest that brisk walking exercises of 4,000–12,000 steps per day (80–100 m/min) can effectively control blood pressure. There is a significant dose-effect relationship between the number of steps and changes in systolic blood pressure. Still, there is no meaningful dose-effect relationship between the number of steps and diastolic blood pressure (33). This may be possible because, during repeated training sessions, there is a regular decrease in peripheral vascular resistance in diastolic blood pressure (34).
Furthermore, the findings showed that of the nine studies, brisk walking exercises with the Improved six-minute walk test (6MWT) method were carried out for 60 min each time you exercise and three times a week and 12 wk better results in reducing diastolic blood pressure in the intervention group. Compared to the control group. The six-minute walk test is a simple cardiopulmonary functional testing method through interaction between the lungs and the heart (35). 6MWT has been shown to have benefits in lowering blood pressure in hypertensive patients (19).
The decrease in blood vessel resistance during brisk walking occurs through increasing nitric oxide production in several parts of the body, known as vasodilation. Vasodilation is also a process of relaxing smooth muscles in the walls of blood vessels, increasing blood vessel diameter (20). The European Society of Cardiology (ESC) guidelines recommend that patients with hypertension perform at least moderate-intensity aerobic exercise or the equivalent of brisk walking of at least 3000 steps per day for 30 min 5–7 times per week (36).
A systematic review of longitudinal studies reported that higher physical activity levels were associated with a lower risk of developing obesity, coronary heart disease, or diabetes. However, the results stated that physical activity and hypertension had an inconsistent relationship (37). In addition, a meta-analysis of previous observational studies found that walking briskly at a normal or maximal pace of ≤ 20 m is associated with cardiovascular health (38). Rapid walking, a relatively inexpensive, safe, and readily available non-pharmacological method, has been recommended for preventing/treating hypertension (39).
There were limitations to the systematic review and meta-analysis of this study. First, the difference in the number of sessions and the number of steps taken between studies means that the study results cannot be generalized. Second, although we applied study selection to experimental studies with pre-test and post-test and randomized methods as strengths in this study, we found evidence of heterogeneity between studies in the primary outcome. Therefore, the researcher recommends that future clinical trials consider the effect of the number of steps in doing brisk walking exercises to lower blood pressure.
Conclusion
The best available evidence suggests that a brisk walking exercise intervention can reduce blood pressure statistically significantly in people with hypertension. Regular brisk walking exercises can reduce the risk of dependence on anti-hypertensive drugs. However, brisk walking is not recommended as monotherapy for hypertension but as prevention of hypertension. These findings provide recommendations for the future to carry out community-based physical activity to improve physical health, including heart health.
Journalism Ethics considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
The researcher appreciates the wholehearted collaboration of all parties involved in attending this research. The manuscript preparation was supported by Bina Bangsa Getsempena University.
Footnotes
Conflict of interest
The authors declare that there is no conflict of interests.
References
- 1.Kurnianto A, Sunjaya DK, Rinawan FR, et al. (2020). Prevalence of Hypertension and its Associated Factors among Indonesian Adolescents. Int J Hypertens, 2020: 4262034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou B, Carrillo-Larco RM, Danaei G, et al. (2021). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet, 398(10304):957–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramakrishnan S, Zachariah G, Gupta K, et al. (2019). Prevalence of Hypertension among Indian Adults: Results from the Great India Blood Pressure Survey. Indian Heart J, 71(4):309–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ku E, Lee BJ, Wei J, Weir MR. (2019). Hypertension in CKD: Core Curriculum 2019. Am J Kidney Dis, 74(1):120–31. [DOI] [PubMed] [Google Scholar]
- 5.Pescatello LS, MacDonald HV, Lamberti L, et al. (2015). Exercise for Hypertension: A Prescription Update Integrating Existing Recommendations with Emerging Research. Curr Hypertens Rep, 17(11):87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhao B, Wang H. (2021). Effect of Abdominal Breathing Combined with Brisk Walking on Intervention Effect of Female Patients with Essential Hypertension. Global Journal of Health Science, 13(3): 76–80. [Google Scholar]
- 7.Mahmood S, Shah KU, Khan TM, et al. (2019). Non-Pharmacological Management of Hypertension: in the Light of Current Research. Ir J Med Sci, 188(2):437–52. [DOI] [PubMed] [Google Scholar]
- 8.Walther D, Curjuric I, Dratva J, et al. (2017). Hypertension, Diabetes and Lifestyle in the Long-Term—Results from a Swiss Population-Based Cohort. Prev Med, 97:56–61. [DOI] [PubMed] [Google Scholar]
- 9.Aljuraiban GS, Gibson R, Chan DSM, et al. (2023). Lifestyle Score and Risk of Hypertension in the Airwave Health Monitoring Study of British Police Force Employees. Int J Environ Res Public Health, 20(5):4029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO (2017). Global Diffusion of eHealth: Making Universal Health Coverage Achievable: Report of the Third Global Survey on eHealth: World Health Organization.
- 11.Wijaya IK, Tahir MY, Talib MT, et al. (2022). The Effect of Brisk Walking on Blood Pressure in Hypertension Patients: A Literature Review. KnE Life Sciences, 7(2):327–334. [Google Scholar]
- 12.Igarashi Y, Akazawa N, Maeda S. (2018). The Required Step Count for a Reduction in Blood Pressure: a Systematic Review and Meta-Analysis. J Hum Hypertens, 32(12):814–24. [DOI] [PubMed] [Google Scholar]
- 13.Chan AWK, Chair SY, Lee DTF, et al. (2018). Tai Chi Exercise is more Effective than Brisk Walking in Reducing Cardiovascular Disease Risk Factors among Adults with Hypertension: A Randomised Controlled Trial. Int J Nurs Stud, 88:44–52. [DOI] [PubMed] [Google Scholar]
- 14.Lan Y-S, Feng Y-J. (2022). The Volume of Brisk walking is the Key Determinant of BMD Improvement in Premenopausal Women. PLoS One, 17(3):e0265250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baskerville R, Ricci-Cabello I, Roberts N, et al. (2017). Impact of Accelerometer and Pedometer Use on Physical Activity and Glycaemic Control in People with Type 2 Diabetes: a Systematic Review and Meta-Analysis. Diabet Med, 34(5):612–20. [DOI] [PubMed] [Google Scholar]
- 16.Moher D, Shamseer L, Clarke M, et al. (2015). Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 Statement. Syst Rev, 4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yalfani A, Ahmadi M. (2023). Patients with Patellofemoral Pain Exhibiting Decrease Vertical Ground Reaction Force Compared to Healthy Individuals during Weight Bearing Tasks: A Systematic Reviews and Meta-Analysis. Iran J Public Health, 52(2):254–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen C, NS KH, Jeffri N. (2021). Effects of Brisk Walking on Plasma Lipoprotein (a), Total Antioxidant Status, Aerobic Fitness, Percent Body Fat, Waist Circumference and Resting Blood Pressure in Overweight and Obese Females. IIUM Medical Journal Malaysia, 20(1): doi.org/ 10.31436/imjm.v20i1.1760 [DOI] [Google Scholar]
- 19.He L, Wei WR, Can Z. (2018). Effects of 12-Week Brisk Walking Training on Exercise Blood Pressure in Elderly Patients with Essential Hypertension: a Pilot Study. Clin Exp Hypertens, 40(7):673–679. [DOI] [PubMed] [Google Scholar]
- 20.Humphrey O, Ogu C. (2021). 12-Week Brisk-Walking Intervention on Middle-Aged Mild-Hypertensive Population in Asaba, Delta state, Nigeria. American Journal of Health, Medicine and Nursing Practice, 6(2):1–9. [Google Scholar]
- 21.Kumaravelu P. (2019). Effect Of Moderate Intensity Walking On Blood Pressure In Prehypertensive Adults. Think India Journal, 22(14):14362–6. [Google Scholar]
- 22.Omar N, Ahmad R, Shah MSM, et al. (2021). Effect of Brisk Walking Workplace Programme on Cardiorespiratory Fitness in Young Men With Cardiovascular Risks. Malaysian Journal of Sport Science and Recreation, 17(2):138–53. [Google Scholar]
- 23.Rachmawati ID, Sugiarto A, Hastuti TP. (2019). Influence of Brisk Walking Exercise on Blood Pressure Among Essential Hypertension Patients. Midwifery and Nursing Research, 1(1):10–5. [Google Scholar]
- 24.Saavedra JM, Kristjánsdóttir H, Gunnarsson SB, et al. (2021). Effects of 2 Physical Exercise Programs (Circuit Training and Brisk Walk) Carried Out during Working Hours on Multidimensional Components of Workers’ Health: a Pilot Study. Int J Occup Med Environ Health, 34(1):39–51. [DOI] [PubMed] [Google Scholar]
- 25.Xu M, Sun X-T, Zhu A-Y, et al. (2021). Effects of a Graded Brisk Walking Test at Different Levels of Intensity on Elderly Patients with Essential Hypertension: a Prospective Study In Shanghai, China. J Health Commun, 6(S6):34. [Google Scholar]
- 26.Castres I, Tourny C, Lemaitre F, Coquart J. (2017). Impact of a Walking Program of 10,000 Steps per Day and Dietary Counseling on Health-Related Quality of Life, Energy Expenditure and Anthropometric Parameters in Obese Subjects. J Endocrinol Invest, 40(2):135–41. [DOI] [PubMed] [Google Scholar]
- 27.Hallam KT, Bilsborough S, de Courten M. (2018). “Happy Feet”: Evaluating the Benefits of a 100-Day 10,000 Step Challenge on Mental Health and Wellbeing. BMC Psychiatry, 18(1):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yu Y, Chang C, Wu Y, et al. (2021). Dose-Effect Relationship between Brisk Walking and Blood Pressure in Chinese Occupational Population with Sedentary Lifestyles: Exercise and Blood Pressure. J Clin Hypertens (Greenwich), 23(9):1734–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mak MKY, Wong-Yu ISK. (2021). Six-Month Community-Based Brisk Walking and Balance Exercise Alleviates Motor Symptoms and Promotes Functions in People with Parkinson’s Disease: A Randomized Controlled Trial. J Parkinsons Dis, 11:1431–41. [DOI] [PubMed] [Google Scholar]
- 30.Rachmatullah R, Widyatuti W, Sukihananto S. (2022). Effect of Brisk Walking Exercise on Lowering Blood Pressure: Systematic Review. Faletehan Health Journal, 9(01):100–10. [Google Scholar]
- 31.Opoku B, de Beer-Brandon CR, Quartey J, et al. (2023). Effects of Brisk Walking on Fasting Blood Glucose and Blood Pressure in Diabetic Patients. J Insul Resist, 6(1):a77. [Google Scholar]
- 32.Cigarroa I, Bravo-Leal M, Petermann-Rocha F, et al. (2023). Brisk Walking Pace Is Associated with Better Cardiometabolic Health in Adults: Findings from the Chilean National Health Survey 2016–2017. Int J Environ Res Public Health, 20(8):5490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yu Y, Chang C, Wu Y, et al. (2020). Effects of Brisk Walking on Blood Pressure in the Chinese Han Occupational Population with a Sedentary Lifestyle: A Baseline Control Trial. Research Square, 10.21203/rs.3.rs-23564/v1. [DOI] [Google Scholar]
- 34.Farrell C, Turgeon DR. (2023). Normal Versus Chronic Adaptations To Aerobic Exercise: StatPearls Publishing, Treasure Island (FL), 2022. [PubMed] [Google Scholar]
- 35.Casano HAM, Anjum F. (2020). Six Minute Walk Test. StatPearls [Internet]: StatPearls Publishing. [PubMed] [Google Scholar]
- 36.Bolbrinker J, Touis LZ, Gohlke H, et al. (2018). European Guidelines on Lifestyle Changes for Management of Hypertension. Herz, 43(4):352–8. [DOI] [PubMed] [Google Scholar]
- 37.Cleven L, Krell-Roesch J, Nigg CR, et al. (2020). The Association Between Physical Activity with Incident Obesity, Coronary Heart Disease, Diabetes and Hypertension in Adults: a Systematic Review of Longitudinal Studies Published After 2012. BMC Public Health, 20(1):726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fonseca Alves DJ, Bartholomeu-Neto J, Júnior ER, et al. (2017). Walking Speed, Risk Factors, and Cardiovascular Events in Older Adults—Systematic Review. The J Strength Cond Res, 31(11):3235–44. [DOI] [PubMed] [Google Scholar]
- 39.Esmailiyan M, Amerizadeh A, Vahdat S, et al. (2023). Effect of Different Types of Aerobic Exercise on Individuals With and Without Hypertension: An Updated Systematic Review. Curr Probl Cardiol, 48(3):101034. [DOI] [PubMed] [Google Scholar]