Dear Editor,
Introduction
Standardized pain intensity scales are often adapted for cross-cultural use by translating descriptive labels from English to non-English languages, with limited to no consideration of how cultural groups conceptualize, describe, and rate their pain.1,2 Research shows that pain intensity is described differently for the Hmong compared with other cultural groups because of their oral culture and communication style (ie, storytelling).3 Consequently, clinicians and interpreters experience challenges understanding Hmong patients’ pain.4,5 Previous research highlighted the need for a specific pain intensity scale for the Hmong population.6 The present study’s aims were (1) to characterize outward expressions of pain intensity among Hmong patients with limited English proficiency (LEP) and (2) to co-design a pain intensity scale to improve pain communication for them.
Methods
This study was approved by the University of Wisconsin Institutional Review Board and was conducted in two phases to design and refine the pain intensity scale.
Phase I involved individual in-person interviews that occurred from November 2020 to March 2021 to understand how Hmong patients conceptualized outward expressions of pain intensity. Specifically, we asked Hmong participants, “When you or someone you know is in pain, how do they show it?” If participants discussed pain expression related to the full body or face, we asked follow-up questions to further clarify the descriptions and obtain a range of pain intensity expressions. For example, we asked, “You mentioned the facial expression for when someone is in a lot of pain. How does someone who is not in pain or has mild or moderate pain express their pain, either through facial expression or body cues?”
Phase II involved participatory design sessions comprising 3 to 5 individuals at a time to develop and iteratively refine the pain intensity scale with participants (ie, LEP Hmong and bilingual interpreters) in person. Some LEP Hmong from Phase I participated in the beginning of Phase II to come up with initial pain intensity visuals. Subsequently, those visuals were put into different scales and shown to new participants for refinement throughout Phase II. Because of the COVID-19 pandemic, Phase II data were collected via virtual focus groups. The pain intensity scale was iteratively refined, incorporating their feedback on color, accuracy of the infographics for representing the pain descriptions obtained in Phase I, and other suggestions for improvements. We named the final pain intensity scale the Lor Hmong Pain Intensity Scale. All interviews and design sessions were digitally recorded, transcribed, and analyzed via thematic analysis in the Hmong language.
Results
A total of 46 participants took part in this study, with five individuals participating in both study phases; however, they were counted only once in the overall count. Phase I consisted of individual interviews with 20 LEP Hmong people, and Phase II involved 31 participants distributed across 5 design sessions (n = 8 LEP Hmong, n = 10 bilingual Hmong, and n = 13 Hmong-speaking interpreters). The majority of the participants were female (n = 30, 65.21%) with a mean age of 53.31 years (SD = 17.24).
Phase I: Characterization of outward expressions of pain intensity
There were two main themes with regard to how LEP Hmong conceptualized outward expressions of pain intensity—physical traits and structure of scale. Participants associated physical characteristics, such as skin color and facial expressions, with levels of pain intensity. Specifically, participants associated a pale yellow hue on a person’s face with more severe pain, compared with other skin colors. With regard to facial expressions, nearly all of the participants, regardless of gender, agreed that crying and angry facial expressions indicate severe pain, whereas happy and laughing faces signal the absence of pain. See exemplary quotes in Table 1.
Table 1.
Example themes and quotes across study phases.
| Themes | Quote |
|---|---|
| Phase I | |
| Physical traits | |
| Facial expression | Yes, because when there is pain, the face that it makes is mean. When you are hurting and it has a mean face, then that is not good for you. The face is grimacing and crying. (Participant 25) |
| Skin color |
|
| Structure of scale | |
| Use scale of 0–10 and include numbers under each face |
|
| Include Hmong | Writing in Hmong would help those who don’t know how to read in English. So, writing in Hmong would help. (Participant 23) |
| Six faces and no body needed | 6 faces is fine. 10 is too much …. Just the face is fine. (Participant 25) |
| Phase II | |
| Facial expression | That the facial expression, like the frowning and stuff is helpful, but I feel like looking at the scale, it doesn't help me to like to describe. Like I can see the level of changes if I look at them all together. But if I were to look at number 6, that could potentially be normal. You know, and number 8, it doesn't look like they're in a lot of pain to me. It doesn’t translate into a lot of pain. And 10, because of the tears, it does help but you can’t really see it. (Participant 43) |
| Use of color |
|
| Facial features | |
| Change shape of face | I think you should make the face less oval and more face-shaped with a chin. (Participant 45) |
| Increase wrinkle lines | When they barely open their eyes. And maybe, I think the mouth makes a difference too umm, trying to think of how’d that change. I think maybe some changes in the nose, a little more scrunchy? Yea, the mouths are all different so you can kinda see there's a difference in everything. And also, even the wrinkles on the forehead, it changes too. (Participant 43) |
| Lip coloring and open mouth | When you are doing good, you are healthy, and the cheeks are not as pale. When you are experiencing a little more pain, the person is burning or not healthy, so the cheeks are a little redder and then become paler. When it hurts a lot, then it will go home [metaphor for dying] and become pale. (Participant 1) |
When we asked participants about the structure of the pain scale, they suggested using the familiar 0–10 rating system with 6 faces instead of the usual 10 for simplicity. Additionally, they suggested including the number representing pain intensity under each face to provide more clarity compared with having no number. They also shared that including the whole body might not be necessary; a scale with faces is sufficient. Most participants also expressed a preference for having Hmong text anchoring the numbers referencing at both ends of scale (ie, 0 and 10).
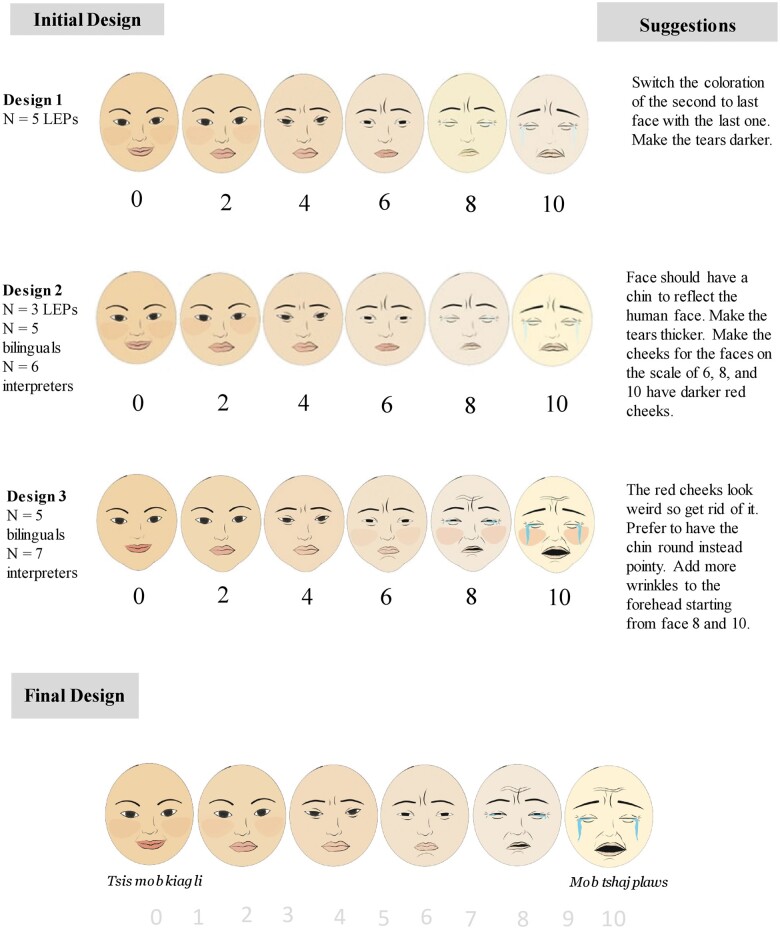
We created Design 1 for the participatory design sessions on the basis of participants' descriptions of their pain in this phase (Figure 1).
Figure 1.
Evolution of Hmong pain intensity scale across participatory design sessions. © Maichou Lor, 2023, All rights reserved.
Phase II: Design and iterative refinement of pain intensity scale
The feedback revealed three major themes of changes to (1) the facial expressions, (2) use of color, and (3) details of facial features. Most participants agreed that the facial expressions were appropriate for the respective pain levels, but they wanted more dramatic changes between pain levels 6–10, such as facial grimacing with lines and wrinkles on the forehead and below the mouth, as well as mouths progressing from shut to open. In terms of color, participants wanted more vibrancy in the no pain to mild pain range, with rosy cheeks and a normal skin tone. They also proposed switching faces 8 and 10 as the pale yellow hue is more indicative of severe pain (Figure 1).
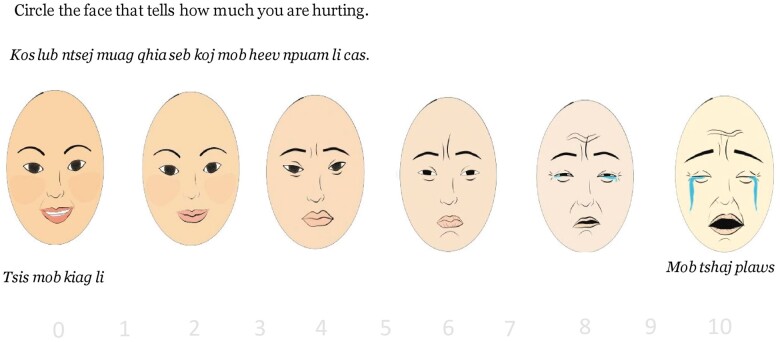
Finally, participants had a variety of comments on the structure of the scale. The suggestions that were incorporated into the updated Lor Hmong Pain Intensity Scale are outlined in Table 1, and they include changing the shape of the face, the color of the lips, and the features around the eyes. The final version of the facial expressions is presented in Figure 2.
Figure 2.
Finalized Lor Hmong pain intensity scale with instructions. © Maichou Lor, 2023, All rights reserved.
Conclusion
To our knowledge, this is the first study with LEP Hmong to characterize their outward expressions of pain intensity and to create a culturally appropriate pain intensity scale for them. We plan to promote the use of the Lor Hmong Pain Intensity Scale through additional publications, conference presentations, local Hmong community groups, health care systems, and interpreter service agencies. Although our Lor Hmong Pain Intensity Scale is similar to commonly used scales (eg, Wong Baker or Revised-Faces Scale) in having 6 faces and tears, but there are also culturally distinct features, such as having more consistent skin tone that is realistic to Asian features and cultural expectations of pain severity (ie, change in faces’ pale yellow hue). This study did not test the psychometric properties validation of the Lor Hmong Pain Intensity Scale on LEP Hmong patients. A national efficacy study is our next step to assess and evaluate the Lor Hmong Pain Intensity Scale on LEP Hmong patients’ communication with providers.
Acknowledgments
We thank our illustrators Mai Joua Yang and Nancy Yang for creating and revising the images in this study. We also thank Mayhoua Moua, Shannon Sparks, and the Milwaukee Consortium for Hmong Health, Inc., for their assistance with participant recruitment and for providing us with a private space to conduct the design session interviews with some of the Hmong participants.
Contributor Information
Maichou Lor, University of Wisconsin-Madison, School of Nursing, Madison, WI 53705, United States.
Abby M Hammes, University of Wisconsin-Madison, School of Nursing, Madison, WI 53705, United States.
Adriana Arcia, University of San Diego Hahn School of Nursing and Health Science, San Diego, CA 92110, United States.
Funding
The research reported in this publication was supported by the National Institute of Nursing Research of the National Institutes of Health under Award Number K23NR019289. The content is solely the authors’ responsibility and does not necessarily represent the official views of the National Institutes of Health.
Conflicts of interest: While conducting this research and preparing this article, the authors have strived to maintain objectivity and impartiality. No conflicts of interest, whether financial or non-financial, exist that might undermine the integrity of our findings or the objectivity of our conclusions.
References
- 1. “Star” BS, Herr K. The state-of-“cultural validity” of self-report pain assessment tools in diverse older adults: table 1. Pain Med. 2015;16(2):232-239. 10.1111/pme.12496 [DOI] [PubMed] [Google Scholar]
- 2. Narayan MC. Culture’s effects on pain assessment and management. Am J Nurs. 2010;110(4):38-47. [DOI] [PubMed] [Google Scholar]
- 3. Lor M, Kim KS, Brown RL, Rabago D, Backonja M. Comparison of four pain scales among Hmong patients with limited English proficiency. Pain Manag Nurs. 2021;22(2):205-213. 10.1016/j.pmn.2020.08.001 [DOI] [PubMed] [Google Scholar]
- 4. Lor M, Rabago D, Backonja M. “There are so many nuances …”: health care providers’ perspectives of pain communication with Hmong patients in primary care settings. J Transcult Nurs. 2021;32(5):575-582. 10.1177/1043659620959437 [DOI] [PubMed] [Google Scholar]
- 5. Lor M, Badenoch N, Yang MJ. Technical meets traditional: language, culture, and the challenges faced by Hmong medical interpreters. J Transcult Nurs. 2022;33(1):96-104. 10.1177/10436596211039553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lor M, Vang X, Rabago D, Brown RL, Backonja M. “It hurts as if …”: pain-associated language, visual characterization, and storytelling in Hmong adults. Pain Med (Malden, Mass.). 2020;21(8):1690-1702. 10.1093/pm/pnz268 [DOI] [PubMed] [Google Scholar]