Abstract
Objective
This study aimed to develop a Korean version of the Nonsuicidal Self-injury Inventory (K-NSSI) through the Deliberate Self-harm Inventory (DSHI) developed by Gratz for the Korean context and confirm its reliability and validity for clinical application.
Methods
A total of 188 participants were analyzed utilizing the DSHI, the Korean version of the Self-harm Inventory, the Personality Assessment Inventory-Borderline Features (PAI-BOR), and the DSM-5 Level-2-Depression scale (Level-2-Dep). Cronbach’s α assessed their reliability, while frequency analysis examined the items of the K-NSSI scales. Validity of the K-NSSI was confirmed through correlation analyses between K-NSSI (tendency for and frequency of nonsuicidal self-injury [NSSI] behavior) and SHI, PAI-BOR total scale, four subscales of PAI-BOR, and Level-2-Dep scale. Polyserial correlations analyzed the correlation between the presence of NSSI behavior and other scales. Confirmatory factor analysis and structural equation modeling explored the relationship between borderline personality features and self-harm.
Results
Cronbach’s α was 0.71, indicating an “acceptable” level of reliability. Statistically significant correlations were observed between the presence of NSSI behavior and the total scores of SHI and PAI-BOR, and the four subscales of PAI-BOR. The frequency of NSSI showed statistically significant correlations with the total score of SHI and PAI-BOR, and its four subscales. Notably, 13.8% of participants reported engaging in self-harm behaviors, 26.9% reported a single occurrence, and 73.1% reported two or more instances. Structural equation modeling demonstrated that self-harm adequately predicted borderline personality traits.
Conclusion
This study successfully validated the adaptation of DSHI into K-NSSI. The K-NSSI can facilitate interventions for self-harm incidents.
Keywords: Nonsuicidal self-injury, Self-harm scale, Deliberate self-harm scale, Scale validation, Self-injurious behavior
INTRODUCTION
The self-harming behavior prevalence in South Korea is currently alarming, with 22.8% of adolescents reported to have experienced self-harm. This rate surpasses figures in other countries, including the United States (14%), China (17%), and the United Kingdom (10%) [1]. This indicates that “one in five adolescents in South Korea have engaged in self-harm.” Notably, the actual prevalence is likely higher, as self-harming behaviors are often concealed, and individuals may hesitate to disclose such behaviors. Further, the gravity of the situation is underscored because 60% of adolescents with self-harm attempts are prone to repeat this behavior. Additionally, 70% of adolescents with a history of self-harm have made suicide attempts, which is concerning [2]. Hence, it is crucial to treat self-harming behavior with the utmost seriousness, recognizing it as a potential precursor to suicide. According to the 2022 White Paper on Suicide Prevention, suicide has consistently ranked as the leading cause of death among Korean adolescents for over a decade [3]. The recent coronavirus disease 2019 (COVID-19) pandemic has exacerbated the situation, causing a surge in suicide incidents and attempts [4]. Studies in Korea have further supported these findings, indicating an uptick in emergency room visits and hospitalizations related to self-harm among children and adolescents during the COVID-19 pandemic [5,6].
People engage in self-harm for various reasons. Nock and Prinstein [7]’s four-function model posits mechanisms involving automatic negative reinforcement, automatic positive reinforcement, social negative reinforcement, and social positive reinforcement. Alternatively, Jacobson and Batejan [8]’s modified integrative model suggests that biological, psychological, and environmental factors interact, leading individuals to resort to “self-harm” as a coping mechanism when stressed. Edmondson et al. [9] conducted a synthesis of 152 studies, identifying reasons for self-harm, such as the control of emotional distress, a way of seeking help or expressing distress, and as a form of self-punishment. Hooley and Franklin [10]’s research delves into self-harm, highlighting the perceived benefits and the reasons individuals may be hesitant to engage in such behavior.
Preventing self-harm is indeed a crucial challenge. Self-harm resembles an addiction, persisting and evolving in various methods if left unchecked [11]. Consequently, identifying and intervening with individuals who have engaged in self-harm at an early stage is crucial.
In Korea, few instruments facilitate a thorough and qualitative examination of self-harming behavior. Currently, the Self-harm Inventory (SHI) and the Inventory of Statement About Self-injury (ISAS) are commonly employed domestically. However, their reliance on a Likert scale for self-harm assessment limits their adequacy in thoroughly examining the content, timing, and frequency of self-harm [12,13]. Regarding the SHI, the assessment of self-harm severity relies on a straightforward total score assigned on a Likert scale, which may not precisely distinguish when the self-harm began, its frequency, and the specific methods employed. The ISAS offers a comprehensive assessment by encompassing the frequency and methods of self-harm. However, it is perceived as time-consuming because of its extensive content, comprising 48 questions. Gratz’s Deliberate Self-harm Inventory (DSHI) optimizes the advantages of both the SHI and ISAS while mitigating their drawbacks [14].
Gratz introduced DSHI in 2001, designed to gather detailed information on self-harm. This inventory inquires about the initiation and frequency of self-harm, the most recent occurrence, its duration, and any subsequent post-injury interventions. Notably, the DSHI classifies self-harm into 16 distinct methods and systematically repeats the same set of questions for each method employed [14]. Gratz conducted a validation study involving 150 individuals and determined that DSHI demonstrated satisfactory levels of reliability and validity.
Validation studies of the DSHI have been conducted in Asia. In a Japanese validation study involving 149 individuals, the DSHI demonstrated satisfactory reliability and validity [15]. This study affirmed the DSHI utility for a comprehensive understanding of an individual’s past and present self-harm history, potentially aiding therapeutic interventions. Although it has been adapted and employed in domestic theses, no dedicated study has assessed its validity in the Korean context [16,17].
Hence, this study aimed to validate the Korean version of the DSHI. As the DSHI aligns with the concept of nosuicidal self-injury as defined in the diagnostic statistical manual-5 (DSM-5), the study translated the DSHI into the Nonsuicidal Self-injury Inventory (NSSI) for use. The anticipated outcome of this research is the introduction of the Korean version of NSSI (K-NSSI), which is envisioned to be employed in clinical settings. K-NSSI can aid in identifying the extent, nature, and severity of self-harm, facilitating the development of treatment plans for self-harming behavior and contributing to the prevention of such behaviors.
METHODS
Development of the Korean Version of the Nonsuicidal Self-injury Inventory
Before commencing the validation study for the K-NSSI, the initial steps involved reaching out to the original author of the DSHI to obtain permission for a validation study of the Korean version, which was granted via email. Subsequently, two psychiatrists and one clinical psychologist collaborated to adapt the DSHI into the Korean version. To ensure linguistic fidelity, an American PhD holder, proficient in both English and Korean, conducted the back-translation of the Korean version into English. Subsequently, the translated versions were subjected to a meticulous review process involving one psychiatrist and one clinical psychologist, who compared the Korean version with the back-translated edition. Following the comprehensive review, the final items for the K-NSSI were determined.
Noteworthy modifications included allowing respondents to specify each type of self-harm independently. The yes or no response format was replaced with a checkbox method, and respondents were prompted to indicate the frequency and the beginning and end periods of self-harm across different educational stages (elementary school, middle school, high school, and university). Further, the representation method for indicating the presence or absence of medical treatment was also transitioned to a checkbox format.
Research Subjects
Approval for this study was obtained from the Institutional Review Board of Wonkwang University Hospital (WKUH IRB No. 2019-05-011-006). Before study commencement, all participants provided written informed consent. The research, initiated in June 2019 following institutional review board approval, concluded in August 2022. The study enrolled healthy adults aged 19−64 years who attended mental health-related workshops and educational programs organized by the Jeollabuk-do Mental Health and Welfare Center. A total of 205 individuals initially agreed to participate and completed the questionnaires. However, 17 participants provided incomplete questionnaire responses, resulting in a final analysis being conducted on the data of 188 individuals.
Assessment Tools
Deliberate Self-harm Inventory
Developed by Gratz in 2001, the DSHI is a comprehensive scale that conceptually characterizes self-harming behavior while providing a psychometric measure of such behavior. Gratz’s research established its robust psychometric properties, including adequate test–retest reliability, construct validity, convergent validity, and discriminant validity. The DSHI comprises 17 items, each addressing different modes of intentional self-harm. Beyond identifying the presence or absence of self-harming behavior, the inventory delves into details, such as the timing, frequency, and duration of the initial and most recent self-harming incidents. Additionally, it explores whether hospitalization or medical treatment was sought. In the original paper, Cronbach’s alpha was 0.82.
Self-harm Inventory
The SHI is a self-report scale originally developed by Sansone et al. [18] in 1998 to assess intentional self-harming behavior. This study utilized the Korean version developed by Lee and Lee [19] in 2015. This adaptation was derived from the work of Kong et al. [12] and received approval from the original authors [19]. The scale comprises 20 questions assessing self-harming behaviors, utilizing a 4-point Likert scale (1 for “rarely,” 2 for “sometimes,” 3 for “often,” and 4 for “always”). Higher total scores on the items indicate a greater frequency of self-harming behavior, with no reverse-scored items. In Lee and Lee [19]’s (2015) study, Cronbach’s alpha was reported as 0.76, and in the current study it was determined to be 0.79.
Personality Assessment Inventory-Borderline Features
The PAI-BOR is the borderline features scale within the clinical version of the PAI, developed by Morey [20]. The elevation of PAI-BOR scores above a clinically significant level may suggest the presence of borderline personality disorder from a psychiatric diagnostic perspective. Comprising 24 questions, the responses on the Likert scale range from 0 to 3 (0 for “never,” 1 for “rarely,” 2 for “occasionally,” and 3 for “frequently”). The PAI-BOR includes reverse-scored questions 3, 5, 12, 16, 18, and 24. This scale is further divided into four subscales: BOR-Affective Instability (BOR-A), BOR-Identity Problem (BOR-I), BOR-Negative Relationships (BOR-N), and BOR-Self-Harm (BOR-S). In a study on the Korean version of the PAI, Cronbach’s alpha for PAI-BOR was 0.87 [21]. In this study as well, Cronbach’s alpha for PAI-BOR was determined to be 0.87.
Level-2-Depression
The Level-2-Depression scale (Level-2-Dep) is a component of the self-assessment DSM-5 Level 1 Cross-Cutting Symptom Assessment provided by the DSM-5. This assessment addresses various symptoms, including depression, anxiety, anger, psychosis, and others. If any of these symptoms are present, the patient progresses to the next level, Level 2 [22]. The Level-2-Dep focuses specifically on depression and comprises eight questions. Participants rate their responses on a 1−5 Likert scale (1 for “never,” 2 for “rarely,” 3 for “sometimes,” 4 for “often,” and 5 for “always”). Notably, there are no reverse-scored items in Level-2-Dep. Originally integrated into the emotional distress short forms of the Patient-Reported Out-comes Measurement Information System, this scale encompasses eight questions related to depression and seven questions on anxiety. The original study reported an internal consistency of 0.72, and in the present study the internal consistency reached 0.93, denoting “excellent” reliability.
Statistical Analysis
Initially, descriptive statistics were applied to the demographic variables of the study population, encompassing mean and standard deviation calculations, along with frequency analyses. The reliability of the scales was assessed using Cronbach’s α, with the following interpretation criteria: an α value of 0.7 ≦ α < 0.8 is considered “acceptable,” 0.8 ≦ α < 0.9 is deemed “good,” and 0.9 ≦ α is regarded as “excellent” [23]. Subsequently, frequency analysis was conducted on the items of the K-NSSI scales. Consistent with previous studies, a detailed frequency analysis was performed for self-harm by question and sex. The reliability of the K-NSSI was further scrutinized through internal consistency analysis, employing Cronbach’s alpha. To affirm the validity of the K-NSSI, correlation analyses were performed between the K-NSSI (presence and frequency of NSSI behavior) and other relevant scales, including the SHI, PAI-BOR total scale, four subscales of the PAI-BOR, and Level-2-Dep.
Polyserial correlation analysis was employed using the statistical software R Studio (version 4.3.1) to examine the association between the presence of self-harm behavior and other scales. In addition, the present study conducted structural equation modeling to explore the relationship between borderline personality features and actual self-harming behaviors. While the DSM-5 typically divides borderline personality features into nine diagnostic criteria, the outcomes of factor analysis on these features may vary depending on the scale used. In this study, the “borderline personality features” scale from the Personality Assessment Inventory was employed, and in its original paper it was segmented into four subfactors [20]. There-fore, the study performed a confirmatory factor analysis of this four-factor structure and examined the impact of self-harm on borderline personality features through a structural equation model. The R Studio’s Lavaan package was employed for testing the structural equation model regarding the relationship between borderline personality features and self-harming behavior. All other analyses were conducted using IBM SPSS Statistics 21 (IBM Co.).
RESULTS
Participants’ Demographic Characteristics
Table 1 presents the participants’ demographic characteristics. A total of 188 subjects were analyzed. The average age of the participants was 24.93 years; 40.4% (76 participants) were male and 59.6% (112 participants) were female. Regarding marital status, 93.1% (175 participants) were single, 6.4% (12 participants) were married, and 0.5% (1 participant) were widowed. Regarding education levels, 27.1% (51 participants) had completed high school, 2.7% (5 participants) had completed a two-year community college program, and 70.2% (132 participants) had completed a four-year university program or higher.
Table 1.
Demographic characteristics and descriptive statistics of measures for participants (n = 188)
| Variable | Value |
|---|---|
| Age, yr | 24.93 ± 6.84 |
| Sex | |
| Male | 76 (40.4) |
| Female | 112 (59.6) |
| Marital status | |
| Single | 175 (93.1) |
| Married | 12 (6.4) |
| Separated | 0 (0.0) |
| Divorced | 0 (0.0) |
| Lost | 1 (0.5) |
| Education level | |
| Elementary school | 0 (0.0) |
| Middle school | 0 (0.0) |
| High school | 51 (27.1) |
| 2-year college | 5 (2.7) |
| 4-year college | 132 (70.2) |
| Measures | |
| SHI | 21.57 ± 2.91 |
| BOR-Total | 44.01 ± 9.22 |
| BOR-A | 10.61 ± 3.04 |
| BOR-I | 12.36 ± 3.18 |
| BOR-N | 11.20 ± 2.41 |
| BOR-S | 9.85 ± 2.86 |
| Level-2-Dep | 12.49 ± 5.63 |
Values are presented as number (%) or mean ± standard deviation.
SHI, Self-harm Inventory; BOR, Personality Assessment Inventory-Borderline Features; BOR-A, BOR-Affective Instability; BOR-I, BOR-Identity Problems; BOR-N, BOR-Negative Relationships; BOR-S, BOR-Self-Harm; Level-2-Dep, Level-2-Depression.
Descriptive Statistics for Measurement Tools
Descriptive statistics for measurement tools are presented in Table 1, The SHI score was 21.57 ± 2.91, while the BOR-Total score was 44.01 ± 9.22. Descriptive statistics for the BOR subscales were as follows: 10.61 ± 3.04 for BOR-A, 12.36 ± 3.18 for BOR-I, 11.20 ± 2.41 for BOR-N, and 9.85 ± 2.86 for BOR-S. Lastly, Level-2-Dep received a score of 12.49 ± 5.63.
Sex Difference Analysis in K-NSSI and Frequency Analysis by Question Content
The statistical analysis did not find a significant difference in the presence of self-harm behavior between sexes [χ2 (1, n = 188) = 0.42, p = 0.515]. Specifically, a frequency analysis of responses related to self-harm revealed the following results. The percentage of individuals who reported engaging in self-harming behavior at least once was 13.8% in this study. Among these participants, 46.2% employed a single method, followed by 23.1% using two methods, 3.8% using three methods, 23.1% using four methods, and 3.8% using five methods (Table 2).
Table 2.
Demographic characteristics and descriptive statistics of measures for participants (n = 188)
| Number of self-harm behavior type | Value |
|---|---|
| Only one type attempted | 12 (46.2) |
| Two types attempted | 6 (23.1) |
| Three types attempted | 1 (3.8) |
| Four types attempted | 6 (23.1) |
| Five types attempted | 1 (3.8) |
| Total | 26 (100.0) |
Values are presented as number (%).
The percentage of people who have experienced self-harm behavior even once is 13.8%.
Regarding self-harm, severe scratching was the most common at 28.6%, followed by biting at 14.3%, cutting at 12.5%, and preventing wounds from healing at 10.7% (Table 3).
Table 3.
The frequency rate according to the type of self-harm behavior
| Type of self-harm behavior | Value |
|---|---|
| Severe scratching | 16 (28.6) |
| Biting | 8 (14.3) |
| Cutting | 7 (12.5) |
| Prevented wounds from healing | 6 (10.7) |
| Carving pictures into skin | 5 (8.9) |
| Banging head | 4 (7.1) |
| Carving words into skin | 3 (5.4) |
| Sticking pins, needles, staples into skin | 3 (5.4) |
| Punching self | 2 (3.6) |
| Rubbing glass into skin | 1 (1.8) |
| Breaking bones | 1 (1.8) |
| Total | 56 (100.0) |
Values are presented as number (%).
Additionally, 26.9% of individuals had self-harmed once and 73.1% had self-harmed two or more times (Table 4). Further, 36.0% of individuals began self-harming during elementary school, 28.0% during middle school, 22.0% during high school, and 14.0% during college (Table 5). Finally, out of those who self-harmed, 57.7% sought medical attention (Table 6).
Table 4.
The ratio of individuals who self-harmed once and those who self-harmed two or more times
| Number of attempts | Value |
|---|---|
| Only once | 7 (26.9) |
| More than two times | 19 (73.1) |
| Total | 26 (100.0) |
Values are presented as number (%).
Table 5.
The ratio based on the time of initiating self-harm behavior
| The time of initiating self-harm | Value |
|---|---|
| Since elementary school | 9 (36.0) |
| Since middle school | 7 (28.0) |
| Since high school | 6 (22.0) |
| Since college | 4 (14.0) |
| Total | 26 (100.0) |
Values are presented as number (%).
Table 6.
Correlation analysis between variables for concurrent validity verification
| Dichotomous NSSI | NSSI frequency | SHI | BOR-A | BOR-I | BOR-N | BOR-S | BOR-Total | Level-2-Dep | |
|---|---|---|---|---|---|---|---|---|---|
| Dichotomous NSSI | 1.00 | ||||||||
| NSSI frequency | - | 1.00 | |||||||
| SHI | 0.213** | 0.437** | 1.00 | ||||||
| BOR-A | 0.180* | 0.233** | 0.546** | 1.00 | |||||
| BOR-I | 0.228** | 0.336** | 0.540** | 0.536** | 1.00 | ||||
| BOR-N | 0.136 | 0.212** | 0.397** | 0.507** | 0.552** | 1.00 | |||
| BOR-S | 0.150* | 0.175* | 0.494** | 0.551** | 0.540** | 0.433** | 1.00 | ||
| BOR-Total | 0.213** | 0.302** | 0.623** | 0.818** | 0.834** | 0.753** | 0.792** | 1.00 | |
| Level-2-Dep | 0.159* | 0.198** | 0.538** | 0.613** | 0.651** | 0.501** | 0.404** | 0.683** | 1.00 |
NSSI, Nonsuicidal Self-injury Inventory; SHI, Self-harm Inventory; BOR, Personality Assessment Inventory-Borderline Features; BOR-A, BOR-Affective Instability; BOR-I, BOR-Identity Problems; BOR-N, BOR-Negative Relationships; BOR-S, BOR-Self-Harm; Level-2-Dep, Level-2-Depression; -, not available.
*p < 0.05, **p < 0.01.
Verifying Reliability
Reliability was assessed by calculating Cronbach’s α values. Excluding the dichotomous “yes/no” questions with zero variance (questions 2, 3, 8, 9, and 10), the Cronbach’s α coefficient was 0.71, which is considered acceptable.
Verifying Validity
To validate the study, the presence and frequency of NSSI behavior, total scores of SHI and PAI-BOR, and its four subscales, and the total score of Level-2-Dep, were correlated to assess concurrent validity.
In correlational analyses, the presence of NSSI behavior demonstrated statistical significance with the total scores of SHI and PAI-BOR, and the four subscales of PAI-BOR (r = 0.213 for SHI-Total, p < 0.01; r = 0.180 for BOR-A, p < 0.05; r = 0.228 for BOR-I, p < 0.01; r = 0.150 for BOR-S, p < 0.05; r = 0.213 for BOR-Total, p < 0.01; r = 0.159 for Level-2-Dep, p < 0.05).
The frequency of NSSI exhibited statistical significance in correlations with the total scores of SHI and PAI-BOR, and the four subscales of PAI-BOR (r = 0.437 for SHI-Total, p < 0.01; r = 0.233 for BOR-A, p < 0.01; r = 0.336 for BOR-I, p < 0.01; r = 0.212 for BOR-N, p < 0.01; r = 0.175 for BOR-S, p < 0.05; r = 0.302 for BOR-Total, p < 0.01; r = 0.198 for Level-2-Dep, p < 0.01). This is shown at Table 7.
Table 7.
The frequency based on whether individuals who self-harm received medical treatment or not
| Presence or absence of medical treatment | Value |
|---|---|
| Received medical treatment | 11 (42.3) |
| Didn’t receive any medical treatment | 15 (57.7) |
| Total | 26 (100.0) |
Values are presented as number (%).
Correlation analysis of the other scales (SHI, BOR-A, BOR-I, BOR-N, BOR-S, BOR-Total, and Level-2-Dep) revealed statistically significant correlations at the 0.01 significance level.
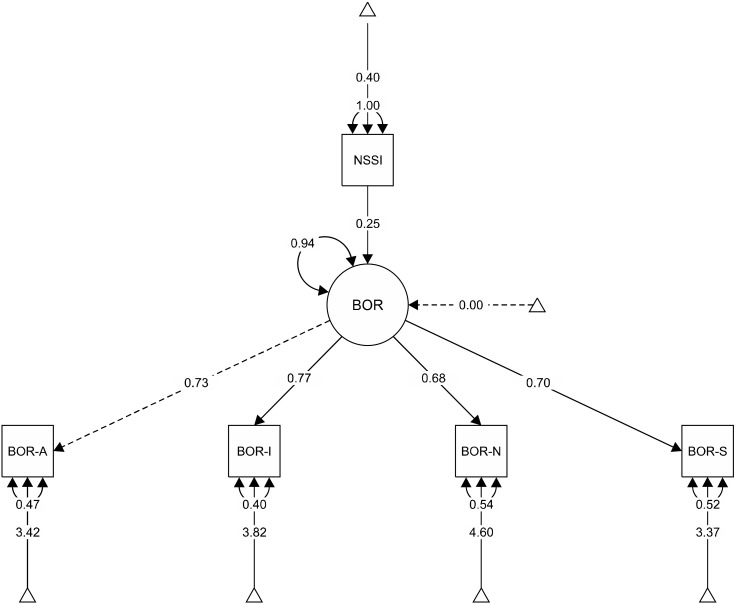
Validation of the Relationship between Borderline Personality Features and Actual Self-harm Behavior
Confirmatory factor analysis of the four-factor structure of the borderline personality scale, as presented in the original paper, demonstrated the appropriateness of the model [comparative fit index (CFI) = 0.992, Tucker-Lewis index (TLI) = 0.977, root mean square error of approximation (RMSEA) = 0.070, standardized root mean square residual (SRMR) = 0.022]. Consequently, a structural equation model assessing the relationship between borderline personality features and actual self-injurious behavior indicated a good fit for the structure of self-injury concerning borderline personality features (CFI = 1.00, TLI = 1.00, RMSEA = 0.000, SRMR = 0.019). This is shown in Table 8 and Figure 1.
Table 8.
The validation of the relationship between borderline personality features and actual self-harm behavior
| Analysis solution | df | CFI | TLI | RMSEA | SRMR |
|---|---|---|---|---|---|
| CFA | 6 | 0.991 | 0.977 | 0.070 | 0.022 |
| SEM | 10 | 1.00 | 1.00 | 0.000 | 0.019 |
CFA, confirmatory factor analysis, SEM, structural equation modeling; df, degree of freedom; CFI, comparative fit index; TLI, Tucker-Lewis index; RMSEA, root mean square error of approximation; SRMR, standardized root mean square residual.
Fig. 1.
A structural equation model path diagram of relationship between borderline personality fea-tures and actual self-harm behavior.
NSSI, Nonsuicidal Self-injury Inventory; BOR, Personality Assess-ment Inventory-Borderline Features; BOR-A, BOR-Affective Instability; BOR-I, BOR-Identity Problems; BOR-N, BOR-Negative Relation-ships; BOR-S, BOR-Self-Harm.
DISCUSSION
This study validated the Korean version of the DSHI by adapting Gratz’s DSHI into the Korean language.
The sample size for this study was 188, surpassing the original paper’s sample size of 159 [14]. In contrast to the original study, which included individuals of various ethnicities, this study focused exclusively on Korean participants. The demographic analysis revealed an approximate 2:3 male-to-female ratio, with over 90% of participants being single. Regarding education, approximately 73% of the study participants held a college degree or higher.
The SHI scores averaged 21.57, closely aligning with the average score of individuals in other studies categorized as regular (21.36 ± 0.65) [24]. The BOR-Total average score in this study was 19.98 points, closely resembling the regular average score (20.15 ± 8.70) as indicated in the PAI guidelines [21]. In this study, the average raw score for Level-2-Dep was 12.49, translating to a T-score of 50, indicative of an average level compared with a regular person [25].
Among 188 healthy adults, 13.8% reported having attempted self-harm at least once, aligning with previous research, which identified a prevalence of self-harm ranging between 10% and 20% [26,27]. Nonetheless, the true incidence of self-harm is anticipated to surpass the 10 to 20% range, given the pronounced inclination to conceal such behaviors. Expanding this perspective to the school environment, approximately 20% of students in the class engage in self-harming behaviors. When considering self-harming behavior within the framework of addiction, it becomes evident that prompt intervention is imperative.
An examination of various self-harm methods revealed that approximately 46% of individuals engage in self-harm using a single method. This typically involves severe scratching, biting, cutting, or preventing wounds from healing, aligning with findings in a comparable category to previous studies [27-29]. Among individuals who engaged in self-harm, over half (approximately 53.8%) employed five distinct methods, aligning with earlier studies [27-29], wherein over 70% of individuals attempting self-harm exhibited repetition and employed two to four different methods [28]. Individuals may explore different self-harm methods when the perceived benefits of one approach diminish, mirroring mechanisms observed in addiction.
The predominant type of NSSI was severe scratching (28.6%), followed by biting, cutting, and preventing wounds from healing. This aligns with previous findings and is likely the highest percentage because of its relative ease of execution [27]. It is theorized that scratching and biting are daytime behaviors in contrast to cutting, which necessitates the use of tools.
While 26.9% of individuals engaged in self-harm only once, over two-thirds of those attempting self-harm repeated the behavior, aligning with previous findings [30-33], which may signify the intensity of addiction to self-injurious behavior.
In the examination of the age at onset of self-harm, the sequence was as follows: elementary school, middle school, high school, and college students, representing 36.0%, 28.0%, 22.0%, and 14.0%, respectively. The onset age of self-harm may be decreasing, occurring at a much younger age than in previous studies from the 2000s, which reported it between 12 and 14 years [29]. Notably, the initiation rates during high school and college are 22.0% and 14.0%, respectively. This implies that self-harm is prevalent among college students and also during early adulthood, extending up to the age of 30 [30]. Another Korean study showed that 20.2% of adults initiated self-harming behavior between the ages of 20 and 24, a higher percentage than observed in the current study [5]. This may be from elevated stress levels during early adulthood and the likelihood that vulnerabilities not apparent during adolescence may surface in adulthood due to challenges in coping with emerging conflicts [31].
Lastly, the analysis of medical treatment received revealed that over half of the individuals attempting self-harm did not receive medical treatment following their self-harming behavior. This may be because of feelings of shame and a desire to conceal self-injurious behavior [10].
The reliability analysis indicated that Cronbach’s α was deemed “acceptable.” In the original paper, a Cronbach’s α of 0.82 was reported [14]. The fact that the study was based on a dichotomous question focusing on the presence or absence of NSSI behavior is likely the reason it did not attain the “excellent” level of 0.90. In the Japanese version of DSHI, this was determined to be 0.57, possibly attributable to the factors mentioned earlier.
The validation analysis results indicated that the correlation between the presence and frequency of NSSI behaviors and SHI was 0.213 and 0.437, respectively, both statistically significant at the 0.01 level. In the original study, DSHI exhibited significant correlations with the Interview for Borderlines-Revised, Suicide Behaviors Questionnaire, and Borderline Personality Organization Scale at 0.43, 0.35, and 0.48, respectively. The Japanese version of the DSHI also exhibited notable correlations with the BDI-II at 0.412 and 0.45. In this study, the Level-2-Dep was employed to help assess depression, demonstrating significance at 0.159 and 0.198.
In this study, a correlation analysis was also conducted with the subscales of BOR, revealing significant findings for all of them. The item with the highest correlation coefficient was BOR-I, indicating that “identity problems” exhibited the strongest correlation with the presence and frequency of NSSI behavior. Considering that the average age of the study participants was early 20s, this period often coincides with the heightened prevalence of identity concerns. This confusion may be closely associated with offending behavior. Empirical studies have demonstrated that individuals exhibiting borderline personality characteristics, coupled with identity confusion, may exhibit a heightened frequency of self-harming behavior [32,33].
The implications of the results for confirmatory factor analysis and the validation of structural equation models are as follows. The confirmatory factor analysis of the borderline personality features scale, comprising four measures, demonstrated a good fit, encompassing “emotional instability,” “identity problems,” “negative relationships,” and “self-destructive behaviors.” Specifically, “identity problems” were identified as having the most significant impact on “borderline personality features.” Moreover, upon scrutinizing the influence of the presence or absence of actual self-harm experience on these borderline personality characteristics, the comprehensive structural model was deemed suitable. Explicitly, we observed that the BOR score could be 1.607 points higher in the presence of actual NSSI behavior. This suggests an interpretation that borderline personality traits are accentuated when self-harm is present.
In this study, the reliability and validity of the Korean version of the NSSI were affirmed, indicating its potential utility in the clinical assessment and intervention of nonsuicidal self-harm patients in Korea in the future.
In summary, this study adapted the Korean version of DSHI, which can effectively measure self-harm behavior within a short timeframe and encompass diverse information (frequency, start and end time, type of self-harm method, the presence of medical treatment). The reliability analysis showed an “acceptable” level, and in the concurrent validity analysis, statistically significant correlations with similar scales were established. Moreover, the analysis of frequency data from the 188 participants yielded statistical insights into the prevalence of self-harm in Korea, the recurrence rate, the prevalence of various self-harm methods, the distribution by age at onset, and the utilization of medical treatment. Expectations are that K-NSSI can enable prompt intervention against self-harm.
Funding Statement
Funding This study was supported by Wonkwang University in 2022.
Footnotes
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Conceptualization: Sang-Yeol Lee, Kyu-Sic Hwang. Data acquisition: Hye-Jin Lee, Sang-Cheol Choi. Formal analysis: Kyu-Sic Hwang, Chan-Mo Yang. Funding: Sang-Yeol Lee, Hye-Jin Lee. Supervision: Sang-Yeol Lee, Sang-Cheol Choi. Writing−original draft: Kyu-Sic Hwang, Chan-Mo Yang. Writing−review & editing: Sang-Yeol Lee, Kyu-Sic Hwang.
References
- 1.Ahn YS. Song HJ. Non-suicidal self-injury in adolescents. J Emot Behav Disord. 2017;33:257–281. doi: 10.33770/JEBD.33.4.13. [DOI] [Google Scholar]
- 2.Nock MK, Kessler RC. Prevalence of and risk factors for suicide attempts versus suicide gestures: analysis of the National Comorbidity Survey. J Abnorm Psychol. 2006;115:616–623. doi: 10.1037/0021-843X.115.3.616. [DOI] [PubMed] [Google Scholar]
- 3.Ministry of Health and Welfare, author. White Paper on Suicide Prevention [Internet] Korea Foundation for Suicide Prevention; 2022. Jun 14, [cited at 2024 Apr 14]. https://seoulmentalhealth.kr/library/paper-collections/347. [Google Scholar]
- 4.Ammerman BA, Burke TA, Jacobucci R, McClure K. Prelimi-nary investigation of the association between COVID-19 and suicidal thoughts and behaviors in the U.S. J Psychiatr Res. 2021;134:32–38. doi: 10.1016/j.jpsychires.2020.12.037. [DOI] [PubMed] [Google Scholar]
- 5.Gu M, Lim S, Kim J, Lee D. Non-suicidal self-injury (NSSI) of Korean adults: gender differences in types and functions of NSSI. Korea J Couns. 2019;20:41–62. doi: 10.15703/kjc.20.5.201910.41. [DOI] [Google Scholar]
- 6.Park S, Choi SC, Yang CM, Jang SH, Lee SY. The Korean version of Pandemic Stress Questionnaire: validation in Korean population. Clin Psychopharmacol Neurosci. 2023;21:377–385. doi: 10.9758/cpn.2023.21.2.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nock MK, Prinstein MJ. A functional approach to the assessment of self-mutilative behavior. J Consult Clin Psychol. 2004;72:885–890. doi: 10.1037/0022-006X.72.5.885. [DOI] [PubMed] [Google Scholar]
- 8.Jacobson CM, Batejan K. In: The Oxford handbook of suicide and self-injury. Nock MK, editor. Oxford University Press; 2014. Comprehensive theoretical models of nonsuicidal self-injury; pp. 308–320. [Google Scholar]
- 9.Edmondson AJ, Brennan CA, House AO. Non-suicidal reasons for self-harm: a systematic review of self-reported accounts. J Affect Disord. 2016;191:109–117. doi: 10.1016/j.jad.2015.11.043. [DOI] [PubMed] [Google Scholar]
- 10.Hooley JM, Franklin JC. Why do people hurt themselves? A new conceptual model of nonsuicidal self-injury. Clin Psychol Sci. 2018;6:428–451. doi: 10.1177/2167702617745641. [DOI] [Google Scholar]
- 11.Blasco-Fontecilla H, Fernández-Fernández R, Colino L, Fajardo L, Perteguer-Barrio R, de Leon J. The addictive model of self-harming (non-suicidal and suicidal) behavior. Front Psychiatry. 2016;7:8. doi: 10.3389/fpsyt.2016.00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kong SS, Lee JH, Shin MY. Impact of childhood trauma on self-harm behavior in patients with eating disorders and the mediating effect of parental conflict. J Korean Acad Psychiatr Ment Health. 2009;18:31–40. doi: 10.12934/jkpmhn.2009.18.1.31. [DOI] [Google Scholar]
- 13.Chu E, Lee Y. Validation of Korean version of Self-injury Inventory (ISAS) Korean J Youth Stud. 2018;25:95–124. doi: 10.21509/KJYS.2018.11.25.11.95. [DOI] [Google Scholar]
- 14.Gratz KL. Measurement of deliberate self-harm: preliminary data on the Deliberate Self-Harm Inventory. J Psychopathol Behav Assess. 2001;23:253–263. doi: 10.1023/A:1012779403943. [DOI] [Google Scholar]
- 15.Ohira T, Munesue T, Oi M, Suzuki K, Saito D. Investigation of the reliability and validity of the Japanese Deliberate Self-Harm Inventory. J Brain Sci. 2018;48:14–42. [Google Scholar]
- 16.Seo Y. Exploration of complex trauma and complex posttraumatic stress syndrome influencing non-suicidal self- injury. Chungbuk National University; Cheongju: 2014. [Dissertation] [Google Scholar]
- 17.Im SY, Lee YH. The effects of negative urgency, negative affect, and emotion regulation difficulties on self- harm behavior in borderline personality disorder. Korean J Health Psychol. 2017;22:565–585. doi: 10.17315/kjhp.2017.22.3.006. [DOI] [Google Scholar]
- 18.Sansone RA, Wiederman MW, Sansone LA. The Self-Harm Inventory (SHI): development of a scale for identifying self-destructive behaviors and borderline personality disorder. J Clin Psychol. 1998;54:973–983. doi: 10.1002/(SICI)1097-4679(199811)54:7<973::AID-JCLP11>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 19.Lee HL, Lee YH. Influence of reward sensitivity/punishment sensitivity on anxiety, depression, and self-harm behavior: the role of stress and controllable attribution style. Korean J Youth Stud. 2015;22:567–593. [Google Scholar]
- 20.Morey LC. In: Personality assessment. 2nd ed. Archer RP, Smith SR, editors. Routledge; 2014. The Personality Assessment Inventory; pp. 181–228. [Google Scholar]
- 21.Morey LC, Kim YH, Kwon HS, Kim JH, Park EY, Park JK, et al. PAI Manual for Professionals. Inpsyt 2019
- 22.American Psychiatric Association, author. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Hakjisa; 2013. [DOI] [Google Scholar]
- 23.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. doi: 10.1007/BF02310555. [DOI] [Google Scholar]
- 24.Jeong K. Seoul Cyber University; Seoul: 2016. Study on medication effect of distress tolerance between adolescents' stress, self-harm behavior and depression. [Dissertation] [Google Scholar]
- 25.Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT Cella D; PROMIS Cooperative Group, author. Item banks for measuring emotional distress from the Patient-Reported Outcomes Measure-ment Information System (PROMIS®): depression, anxiety, and anger. Assessment. 2011;18:263–283. doi: 10.1177/1073191111411667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hawton K, Rodham K, Evans E, Weatherall R. Deliberate self harm in adolescents: self report survey in schools in England. BMJ. 2002;325:1207–1211. doi: 10.1136/bmj.325.7374.1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Whitlock J, Eckenrode J, Silverman D. Self-injurious behaviors in a college population. Pediatrics. 2006;117:1939–1948. doi: 10.1542/peds.2005-2543. [DOI] [PubMed] [Google Scholar]
- 28.Tracy N. 10 Ways people self-harm, self-injure [Internet] HealthyPlace; 2022. Dec 15, [cited at 2024 Apr 14]. Available from: https://www.healthyplace.com/abuse/self-injury/10-ways-people-self-harm-self-injure . [Google Scholar]
- 29.Klonsky ED, Muehlenkamp JJ. Self-injury: a research review for the practitioner. J Clin Psychol. 2007;63:1045–1056. doi: 10.1002/jclp.20412. [DOI] [PubMed] [Google Scholar]
- 30.Klonsky ED. Non-suicidal self-injury in United States adults: prevalence, sociodemographics, topography and functions. Psychol Med. 2011;41:1981–1986. doi: 10.1017/S0033291710002497. [DOI] [PubMed] [Google Scholar]
- 31.Whitlock J, Muehlenkamp J, Eckenrode J. Variation in nonsuicidal self-injury: identification and features of latent classes in a college population of emerging adults. J Clin Child Adolesc Psychol. 2008;37:725–735. doi: 10.1080/15374410802359734. [DOI] [PubMed] [Google Scholar]
- 32.Homan KJ, Sim LA, Fargo JD, Twohig MP. Five-year prospective investigation of self-harm/suicide-related behaviors in the development of borderline personality disorder. Personal Disord. 2017;8:183–188. doi: 10.1037/per0000169. [DOI] [PubMed] [Google Scholar]
- 33.Reichl C, Kaess M. Self-harm in the context of borderline personality disorder. Curr Opin Psychol. 2021;37:139–144. doi: 10.1016/j.copsyc.2020.12.007. [DOI] [PubMed] [Google Scholar]