Abstract
Objective
Dermatologic office procedures involving needles including injection of local anesthetic both cutaneously and intraorally, botulinum toxin, fillers and keloids, as well as venipuncture and a plethora of other procedures can often cause pain that ranges from mild to severe. The technique of utilizing vibration frequently lessens pain. Vibration anesthesia is a non-invasive, inexpensive, virtually side-effect free, and well-established method of lessening pain during dermatologic procedures. We conducted a review of prior studies which used vibration anesthesia in a variety of invasive procedures.
Methods
A comprehensive search was performed using PubMed and EMBASE (Ovid) to look for original studies related to the usage of vibration to reduce pain in invasive procedures. Terms searched were “vibration anesthesia”, “vibration analgesia”, “vibratory anesthesia”, and “vibratory analgesia.” Since these terms, especially the most commonly accepted, “Vibration Anesthesia”, are generally but not universally recognized, a small number of journal articles were found by searching references of acceptable papers. A total of 35 papers were included for analysis.
Results
Many studies have reported that vibration anesthesia is a useful method for reducing uncomfortable symptoms before dermatologic procedures.
Limitations
A small number of suitable papers, especially in the dermatologic literature, met the criteria. The instrumentation and techniques used are not standardized.
Conclusion
Studies involving injection of local anesthesia as well as venipuncture in pediatric populations show vibration anesthesia as a useful method to minimize pain. There is additional literature suggesting that vibration is able to help minimize discomfort associated with injections of botox, fillers, intramuscular antibiotic injections and intralesional cortisone for keloids.
Keywords: Vibration anesthesia, vibration analgesia, vibratory anesthesia, vibratory analgesia
Pain is described as the body’s reaction to an unpleasant stimulus, which can cause both sensory and emotional distress.1 Many patients report experiencing pain during injection of local anesthesia for invasive procedures or other needle sticks, such as for vaccination. While some patients experience mild to moderate pain, others are more sensitive and report a higher severity of pain. Brain scans of people who reported higher levels of pain had increased activation in the primary somatosensory cortex and the anterior cingulate cortex.2 Moreover, brain scans showed that those with a thinner cortex were more sensitive to pain.2
Avoidance of vaccines due to fear of pain was seen in 27 percent of hospital employees and 18 percent in health care workers at long-term care facilities.3 It was also observed in 16 percent of adult patients and 8 percent of hospital health care workers. The outcomes were similar for other vaccines, where approximately 19 percent of people overall did not want to receive a pneumococcal vaccination and about 20 percent did not want to obtain a tetanus vaccination.3
Fear of pain can prevent patients from undergoing necessary procedures such as venipuncture. While it is reported that about 10 percent of individuals in the United States have a fear of needles, the number of unreported cases may be even higher. Trypanophobia (fear of needles) is common among approximately 20 to 50 percent of adolescents and 20 to 30 percent of young adults.3
Many methods can be used to minimize procedural pain. These include using vibration, applying cold, buffering and warming anesthetic to room temperature, using thinner needles, regional nerve blocks, using a dermajet, freezing sprays, topical anesthetic, or simply distractions such as talking.4,5 Some physicians use a combination of these methods.
Vibration anesthesia, which was first described in the literature by Smith and Comite in 2004, has been used countless times and is an established, though non-standardized, technique to help reduce pain associated with invasive procedures.6 It involves applying a vibratory device near the site of injection a few seconds before the procedure begins. Vibration anesthesia is inexpensive and non-invasive, with extremely rare and transitory side effects.
Pathophysiologically, the transmission of pain involves reception of noxious stimuli via nociceptors. These fibers are classified based on size and myelination, the most prominent being C-fibers and A-δ fibers. A-δ fibers are responsible for the initial perception of pain due to their smaller receptive fields and larger degree of myelination in comparison to C fibers, which are unmyelinated and have larger receptive fields and are thus capable of relaying the intensity of pain.7 In response to stimulation, these fibers relay signals to second-order neurons located in the dorsal horn of the spinal cord, where the signal is then relayed by projection neurons into the brainstem.8
In addition to these nociceptive fibers, there are also non-nociceptive fibers, such as A-ß fibers, which are larger in diameter, myelinated, and are receptive to pressure and vibration. Vibration stimulates the Meissner and Pacinian corpuscles, which are the two major A-ß mechanoreceptors involved in sensing vibration. Low-frequency vibration is detected by Meissner corpuscles, which are located in the cutaneous parts of the body such as the skin that covers both the fingertips and eyelids.9 Higher frequency vibration is detected by the Pacinian corpuscles, which are found subcutaneously. The pathway of perceiving vibration also goes via the dorsal column of the spinal cord. The signals are passed along to the VPL nucleus, located in the thalamus, and are then passed on to the primary somatosensory area of the cortex.9
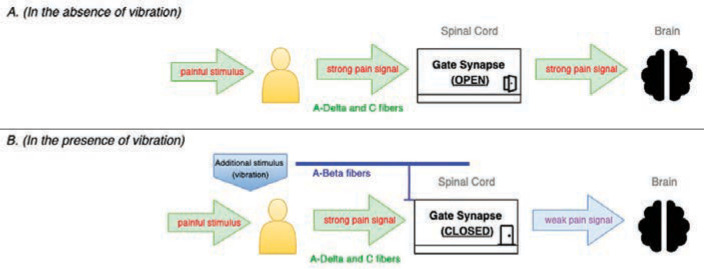
According to the gate-control theory of pain, as A-ß fibers are stimulated by vibration or pressure, pain signals are less able to be transmitted by A-δ or C fibers.10 The dorsal horn in the spinal cord has a gate that can either allow or prevent action potentials from being sent. The facilitation of action potentials depends on how active the A-δ and C-fibers are. These fibers have the ability to open the gate, which would allow for pain signals to be transmitted and received (Figure 1A).
FIGURE 1.
The gate control theory of pain
FIGURE 2.
Index of common devices used to provide vibration anesthesia
The gate becomes closed when larger diameter fibers such as A-ß fibers become stimulated. During homeostasis, the gate is closed at the spinal cord and hence no pain signals are passed along. The action of vibration causes the gate to remain closed and prevents pain signals from being transmitted (Figure 1B).
Extensive research is being performed to identify exactly how the body senses and reacts to changes in our environment. In 2021, the Nobel Prize in Physiology was awarded to Dr. David Julius and Dr. Ardem Patapoutian for their findings of genes responsible for sensing changes in temperature and touch, respectively. Dr. Julius’s work centered around noxious heat, which can be felt with capsaicin peppers, and how our body responds to such stimuli. The TRP family of ion channels were discovered to be activated when stimuli reached a high threshold of temperature, indicating they may play a pivotal role in thermosensation.11 During separate investigations, Dr. Patapoutian successfully identified the genes responsible for detecting changes in mechanical force known as Piezo1 and Piezo2. The Piezo ion channels become activated by the presence of pressure on the skin.12 These medical breakthroughs have been essential to further understand physiological functions and to develop methods to minimize the perception of pain.
OBJECTIVES
In this review, we aim to examine multiple studies that all use the technique of vibration anesthesia and compare its effectiveness to other methods or no methods.
METHODS
Articles published from 1964 to the present were searched in the PubMed, Ovid, and Cochrane (via Ovid) databases. A search was performed using the term “vibration anesthesia” which yielded 444 results. A further search was done with the term “vibration analgesia” which had 169 results. An additional search with the term “vibratory anesthesia” showed 80 results, while “vibratory analgesia” provided 38 results.
RESULTS
We deemed 35 papers to be relevant and were available in full and in English.
Injection of fillers. To determine whether vibration devices are able to minimize pain during cosmetic filler injections, 32 subjects were recruited. Twenty patients received hyaluronic acid injections Restylane® (Galderma S.A.; Lausanne, Switzerland) while twelve patients received injections with Juvederm Vista® (Allergan, Irvine, California). One side of the face received injections while using a Y-shaped vibration device (Blaine Labs, Inc, Santa Fe Springs, California) while the other half received injections without vibration. Whether each patient received treatment with or without vibration first was randomized. The device provided 9,000 continuous vibrations per minute to the area adjacent to the injection site. The Numeric Rating Scale (NRS) was used by patients to report the intensity of pain, where a rating of 0 indicates no pain and a rating of 10 indicates the worst possible pain. There was a statistically significant difference (P<0.001) in the average NRS score for injections received without vibration (4.5±1.5) and with vibration (2.3±0.9). Of the 32 patients, 28 reported that vibration partially relieved their symptoms of pain while three stated that it did not help reduce pain and one stated feeling increased pain.13 Overall, vibration helped to reduce symptoms of pain associated with injections of both fillers.
Vibration anesthesia was used on 41 patients that were treated with dermal fillers, all hyaluronic acids. There were 29 patients treated with Restylane-L®, 12 with Juvederm-XC Ultra®, four with Perlane-L® (Medicis, Scottsdale, Arizona), and four with Radiesse® (Merz Aesthetics, San Mateo, California) and three with Juvederm-XC Ultra Plus® (Allergan, Irvine, California), One site was treated in 22 patients, while the rest of the patients had multiple sites injected with filler. The tool used in this split-face design study was a Pin Point Personal Massager (Brookstone, Inc; Merrimack, New Hampshire) which was placed on nasolabial folds, tear troughs, cheeks, or other areas the patient was interested in getting treatment. On one side, patients received injection of the filler with the vibration device within 2cm of the injection site; no vibration was received on the opposite side of the face. While some patients received treatment in multiple different areas, the split-design was maintained in all instances. A questionnaire was administered to evaluate pain using a Likert-type scale, where 0 represented no pain while 4 represented the worst pain experienced. The mean pain score for injections received with vibration (0.9±0.6) was significantly lower (p<0.001) than the mean score without vibration (2.7±0.9). About 95 percent of patients reported a significant reduction in their symptoms of pain, with notably zero patients recording an absence of pain when treated without vibration.14
The injection of fillers can be especially painful on thinner and more sensitive areas, such as the lips. In this study, 25 patients undergoing lip augmentation using Juvederm Volift (Allergan; Irvine, California) received vibration to assess its ability to reduce pain. All patients were given topical anesthetic for 20 minutes on the lips prior to the procedure, which used a split-lip design and incorporated the Vibrata device (Beverly Hills, California). Vibration was randomly assigned during one half of the treatment, with the device operating for 2 to 3 seconds prior to the injections to stimulate the surrounding nerves. The other half received fillers without any vibration. Patients reported their pain scores for both sides after the procedure was completed using a 10-point Likert type scale, where 0 indicated no pain, 5 indicated moderate pain, and 10 represented worst pain ever felt. The average pain score on the side that received vibration (3.82±1.73) was found to be significantly lower (p<0.001) than the average pain score without vibration (5.6±1.76). Of note 23 of 25 patients stated that they would prefer to use vibration for future visits. Although two patients who were receiving filler for the first time found vibration to increase pain and anxiety levels, all of the patients who have had the procedure previously preferred using vibration in the future.15
Botulinum toxin type A injections.Botulinum toxin type A injections were utilized to investigate the efficacy of vibration in reducing pain. A split-face design was utilized on fifty patients seeking treatment to minimize rhytides of the glabella and forehead. One side of the face received conventional treatment, while the other received treatment along with vibration from a Pin Point Personal Massager before and continuously throughout the procedure. Pain was self-assessed through a five-point Likert-type scale for each side treated as described previously, where a 0 indicated no pain, and 4 indicated worst pain ever felt. There was a statistically significant (p<0.001) difference in mean pain scores for the side with vibration (1.3±0.6) compared to the side without vibration (2.4±0.8). Additionally, 86 percent of patients reported that they would prefer to have vibration during their next treatment, indicating that vibration was an effective method to reduce pain during facial injections of botulinum toxin type A.16
Botulinum toxin injections were also studied comparing the efficacy of vibration anesthesia versus ice packs. Twenty-two patients were randomized into three different groups, all receiving bilateral forehead injections. One group had ice packs placed unilaterally on the site of injection for around a minute, with no intervention on the other side. The second group had a Buzzy (MMJ Labs, Atlanta, Georgia). A Buzzy is an 8cm× 5cm× 2.5cm plastic device containing a battery-powered vibrating motor. The Buzzy device contains detachable ice wings that must be frozen in advance in order to utilize its cooling effect. The device is best used when placing it 5cm above the insertion site and maintaining it there throughout the procedure.17 In this study, the vibratory device was placed unilaterally about 2cm near the injection site, with no intervention on the other side. The third group received the vibration on one side and the cooling intervention on the other. A total of 88 injection sites were analyzed. Pain intensity of injections was evaluated using the Visual Analog Scale, (VAS) which presents a 10-point horizontal pain rating scale on paper with accompanying images for reference. The mean VAS score for injections received without any intervention (29.4) was higher than the mean score for injections received with vibration (26.5) and with ice (24.4) The results demonstrated that there were no statistically significant different scores among the three groups (p=0.737). For patients that received both interventions, treatment with ice was recorded to be more painful (mean VAS=33) than treatment with vibration (mean VAS=21), but the difference was not statistically significant (p=0.223). While this study shows no efficacy of the Buzzy device prior to botulinum toxin injections, it is likely that this device is simply not powerful enough to be helpful.18
We frequently use vibration to help with botulinum toxin and filler injections, especially with patients who are pain sensitive, as they are being poked many times. Our technique is as follows: after using topical anesthetic for an appropriate amount of time, we generally place ice compresses on patients prior to botulinum toxin injections. After we remove the ice compresses, we add vibration anesthesia a few seconds prior to the injections. Occasional patients prefer neither topical anesthetic nor ice generally because of time constraints, but even most of these patients opt for vibration.We generally use a vibrating instrument with a small footprint and have a trained assistant follow the injector to place the injection about 1cm to 2cm away from the injection point. If any heme appears, we will immediately use gauze to prevent splatter. The assistant has to be well-trained, and the injection order of procedure has to be relatively standard so that the assistant can follow the injector safely and appropriately. While many of our patients have found vibration anesthesia helpful and prefer it to be used on them with each subsequent cosmetic treatment, we have not formally studied the use of vibration anesthesia prior to cosmetic procedures.
Intralesional injections for keloids. A total of 40 patients who were being treated for keloids with corticosteroid injections were enrolled in the study.19 The device used was the Y- shaped vibration device (Blaine Labs, Inc; Santa Fe Springs, California) designed such that the physician can administer the injection with one hand while applying vibration with the other. Vibration was used on one half of the keloid but not on the other half. The VAS was used to assess pain scores. Patients had a statistically significant (p<0.05) lower VAS rating on the side of injection where vibration was applied (3.28±1.85) in comparison to the other side that did not receive any vibration (5.88±2.34).19
Venipuncture. To evaluate the effect of vibration to minimize pain in newborns during heel lance procedures, 58 newborns were included in this study.20 Of that total, 28 received vibration from a gray mini vibration device of 92-100 Hz to the area through which the sural nerve passes below the knee of the patient. The scale used for the study the Neonatal Infant Pain Scale (NIPS), which is used exclusively on newborns and infants. As they are unable to verbally communicate their pain, the NIPS scale assigns 0 to 1 points to the infant's facial expression, arm and leg movements, breathing patterns, and 0 to 2 points on crying, for a total of 0 to 7 points, such that 0 indicates no pain and 7 indicates extreme pain. The scale was used both prior to the procedure, 15 to 20 seconds after, and five minutes after the procedure. There were statistically significant (p<0.05) differences between the vibration and control groups at 15 to 20 seconds and five minutes after the procedures.20
An additional study on the efficacy of vibration on neonates undergoing heel lance procedures also shows positive effects from vibration.21 Of 56 eligible neonates, 30 participants received vibration anesthesia to the heel using a Norco MiniVibrator of 52 Hz during a heel lance procedure. All patients had their heel warmed for 3 to 5 minutes with a leg warmer and were also given oral sucrose two minutes before being lanced. Those in the vibration group received vibration 30 seconds before the heel stick to assess for any adverse effects such as apnea, bradycardia, or desaturation, in which case the vibration would be immediately removed. The Neonatal Pain, Agitation, and Sedation Scale (N-PASS) was used, which consisted of heart rate and oxygen. Scores obtained for vibration were compared against neonates who received no vibration. The patients in the experimental group had significantly lower N-PASS scores and more stable heart rates during heel stick (p=0.006, p=0.037) and two minutes after heel lance (p=0.002, p=0.016) than those in the control group.21
Vibration anesthesia was used on pediatric patients ranging from 4 to 17 years of age needing venipuncture and having difficulty with verbal communication.22 The vibration instrument used was the Buzzy, which was placed above the venipuncture area on the arm. Of 70 patients, vibration anesthesia was used on 34 patients while the other half received no intervention. To determine pain levels of the participants, parents were asked to use the Non Communicating Children’s Pain Checklist–postoperative version scale (NCCPC-PV). The score ranged from 0 to 80. A pain score less than or equal to 10 indicated absence of pain or mild pain. A score greater than 10 indicated the presence of moderate to severe pain. In this study, 91.4 percent of patients in the experimental group and 61.1 percent of patients in the no-intervention group reported no to mild pain. The difference in NCCPC-PV scores of the experimental group (3.0) and control group (8.0) were statistically significant (p=0.003). It was concluded that the Buzzy device effectively reduced pain from venipuncture in pediatric patients who have difficulty with verbal communication.
Vibration was paired with cooling and compared with bubble blowing in a study to determine if either was capable of reducing pain in children undergoing phlebotomy.23 From a group of 96 children aged 3 to 6 years, 32 were randomly selected to receive vibration along with external cold through a Buzzy device. The Buzzy device was placed on the arm, above the area of the phlebotomy site. Another third of participants had the distraction of blowing soap bubbles, and the rest of participants received no intervention, functioning as a control group. The Wong-Baker Faces Pain Rating Scale (WBFPRS) was used, which consisted of six facial expressions, and the rating ranged from no pain (0) to the most pain (10). This scale was recorded by parents, the nurse, and the researchers, which showed that there was a statistically significant difference (p>0.05) between both experimental groups and the control in the ability to minimize pain. However, it cannot be concluded whether vibration served as the best method of minimizing pain as there was no significant difference in WBFPRS scores between both distraction methods.23
In another study, the Buzzy device with ice was utilized to determine whether it was capable of reducing pain and anxiety in children undergoing phlebotomy. The study contained 120 pediatric participants aged 6 to 12 years; 60 received vibration anesthesia during the phlebotomy procedure while 60 served as a control group. Children’s Anxiety and Pain Scale (CAPS), was used to record anxiety levels of participants before and during the procedure. CAPS consists of five cartoon faces that range from a neutral expression associated with a number of 0 that means no anxiety, to a frightened face labeled as 5 that represents severe anxiety.24 There was a statistically significant difference between self-reported scores for patients that received vibration (1.61±0.99) and patients that did not (3.36±0.99). In addition, levels of pain post-procedure were measured using the Faces Pain Scale-Revised (FPS-R) scale, which consists of six cartoon faces that range from a neutral expression indicating no pain and is labeled as 0, to a screaming face with a numerical value of 10, indicating severe pain. There was a statistically significant difference in the ratings for pain post-procedure for patients that did receive vibration (2.78±1.94) versus those that did not (6.56±1.56), indicating that the Buzzy device with ice was effective at reducing both pain and anxiety levels of children.
In another study, 64 pediatric patients participated in the study in which 35 patients received vibration anesthesia during venipuncture. The instrument type utilized was a Buzzy device. A questionnaire containing the WBFPRS with a six-point scale was used to assess pain between the groups before and after the treatment. Out of 35 participants who received vibration, 25 stated that vibration helped reduce pain, and 28 also indicated that they would prefer vibration to be used again for their next venipuncture.25 One patient reported that they would not want it used in the future with the other six responding that they did not have a preference. Additionally, the phlebotomists that participated in the procedure mentioned that vibration made the procedure easier in 81 percent of instances where it was used.
Intramuscular antibiotic injections. Out of 100 patients who received intramuscular (IM) antibiotic injections, 32 participants received vibration through a dolphin massager device on the ventrogluteal area while 35 participants received the ShotBlocker (Bionix, Toledo, Ohio), a U-shaped plastic tool that contains multiple, blunt points designed to innervate the nerves upon contact. The rest of participants were placed in a control group, where there was no instrumental intervention. Patients’ perception of pain was measured after the procedure using a standard VAS, and the level of satisfaction the patient felt during the procedure was also measured. This was done using a Visual Satisfaction Scale, designed similarly to a VAS as it ranges from “strongly dissatisfied” (0 points) on the lower end to “strongly satisfied” (10 points) on the opposite end. There was a statistically significant difference found between the mean scores of perceived pain and satisfaction levels among the groups (p<0.001). The group receiving vibration expressed the lowest amount of pain felt, with a mean VAS score of 3.02±1.07, while the control group experienced the most pain with a mean VAS score of 7.09±0.94. When measuring satisfaction levels, the vibration group expressed the highest levels of satisfaction with a mean score of 7.80±0.90, while the control group expressed the lowest levels, with a mean score of 4.93±1.93. Vibration was more effective than the ShotBlocker. There was also a statistically significant negative correlation found between perceived pain scores and satisfaction levels, indicating that vibration anesthesia proved to be effective at minimizing pain and satisfying patients during IM injections.26
Injection of local anesthesia. Vibration anesthesia was used during the injection of local anesthesia on 80 patients undergoing eyelid surgery. The Waterproof Mini-G vibration device (California Exotic Novelties, Chino, California) was switched on and placed on the forehead during injection of one eyelid, whereas the contralateral lid had the vibrating device switched-off as the control method. Whether patients received vibration during the first injection or second was randomized. To determine the perception of pain, a subjective scale was incorporated where a rating of 0 represented no pain while 10 was the worst pain experienced. Patients that received vibration had a mean score of 3.3 on the subjective pain scale, while the placebo group reported a mean score of 4.5, with a statistically significant difference (p=0.0003). The side that used vibration was reported as better than the placebo at reducing pain in 73 percent of participants.27
Cooling the skin with ice prior to needle insertion has been found to be useful for minimizing pain to an extent, and is often used in conjunction with other methods such as vibration. The following study recruited 60 participants to compare the effectiveness of cryoanalgesia (cooling of skin) against vibration anesthesia in reducing pain before the infiltration of 1% lidocaine-epinephrine. Thirty subjects received vibration through the Buzzy device for two minutes before receiving the anesthetic injection to one arm located 7cm proximal to the olecranon process. Then the other arm was given ice to apply to the area for two minutes prior to injection. The other 30 patients received the same treatment in the opposite order. Patients were asked to rate their pain intensity immediately after each injection using the Visual Analog Scale. The mean score was 30±23.14 after skin cooling and 25.5±24.1 after vibration, which was not statistically significant.28 This may be due to the fact that unlike in other studies described here, the patients did not receive vibration during the injection, but rather solely before.
The anticipation of pain prior to a procedure may cause psychological distress to some patients, and can affect the amount of pain experienced by the patient postoperatively. During pain catastrophization, patients will focus on the negative consequences upon perceiving noxious stimuli as a coping mechanism. The following study was designed to determine whether applying vibration during anesthetic injections would be equally beneficial for patients that tended to catastrophize pain and for patients that did not.29 A total of 87 patients who were undergoing skin cancer removal were included in the study. The patients were grouped into those that received vibration and patients that did not receive any intervention. The vibratory anesthetic device (VAD) was a 10-cm, handheld, battery-operated device (Finever Inc) that was used during local anesthetic injections to the areas after applying a cotton ball to the tip and encasing the device in a glove. The NRS scale was utilized to assess anticipated pain (aNRS) as well as pain during five seconds into the injection (iNRS). Participants that catastrophize pain were defined as those with an aNRS>4. There was a significant difference (p=0.03) in mean iNRS scores between participants who catastrophize pain (2.27) before the injections compared to those that did not (1.44). Vibration anesthesia proved to be slightly effective on participants that catastrophized pain and significantly more effective on participants that did not catastrophize pain.29
Intraoral anesthesia. A meta-analysis consisting of seven studies that were all performed on pediatric dental patients evaluating injection of anesthesia in this cohort. In six of the studies, the WBFPRS was utilized to measure pain. The vibration device was the DentalVibe® (Bing Innovations, Boca Raton, Florida), a vibration tool with a U-shaped tip that provides controlled waves of vibratory stimulus and is designed for intraoral procedures. In five of the seven studies, vibration anesthesia proved to be effective. In two studies, there were no significant differences between the DentalVibe® vibration anesthesia and the placebo group.30
A second meta-analysis reviewed six studies of pediatric patients requiring the use of local anesthetic for dental procedures. Four of the six studies included use of the Dentalvibe, while the other two used the Buzzy. All of the studies contained an experimental group with the device and a conventional treatment group, and assessed for pain using the WBFPRS, with four also using the Face, Legs, Activity, Cry, Consolability (FLACC) scale. If a patient receives a score of 0 on the FLACC scale, they are considered comfortable and relaxed; a score of 1 to 3 indicates mild discomfort, 4 to 6 indicates moderate pain, and 7 to 10 signals severe pain. Due to variation in the techniques used in each study, the correlation between the vibration devices used and the injection method was found to be inconclusive. Among the studies utilizing the DentalVibe, it was found that the device was not effective at reducing pain perception, with only one of the four studies stating otherwise. On the other hand, the Buzzy showed consistent results in effectively minimizing pain perception, which was attributed to not only the cooling effect but also as a means of distraction for children.31
A study consisting of 99 adults in need of bilateral local intraoral anesthetic injections were treated conventionally on one side of the mouth, and with DentalVibe® on the other half. Treatments were randomized and separated by visits, with a total of 256 injections performed, indicating that some patients received treatment in multiple different areas. The areas treated included inferior alveolar, long buccal, palatal, and infraorbital nerves, and all of the patients had at least one pair of injections in a similar area. Not infrequently, dermatologists anesthetize the infraorbital nerve for facial procedures. Pain was assessed both before and immediately after the procedures using a VAS. The results indicated that regardless of the area of injection, the mean anticipated pain scores with vibration were significantly lower (p<0.001) compared to anticipated pain scores without vibration. Similarly, the mean score for actual pain experienced with vibration was also significantly lower (p<0.001) than the mean score without vibration among all areas of injection. Given that mean anticipated pain scores were also lower for the side treated with vibration, it was concluded that not only is DentalVibe effective at reducing pain during intraoral procedures, it was effective at decreasing anxiety prior to the procedure as well.32
The effectiveness of DentalVibe® vibration was compared against a topical anesthetic, 2% lidocaine gel, in their ability to reduce pain during tooth extractions. Using a randomized split-mouth study with 50 participants, DentalVibe® was placed intraorally on one site, while the second site received 2% lidocaine gel, followed by local anesthetic injection for both. The VAS was used to record the outcome of pain after local anesthetic injection. Scores for the site using the DentalVibe ranged from 0 to 6 with a median score of 3, while the side with lidocaine gel scored from 4 to 10 with a median of 7. There was a statistically significant difference (p<0.001) in scores between the two sites. With lower pain scores from the side treated with vibration, it was concluded that vibration can be a viable tool for painful intraoral procedures.33
Vibration was utilized in the administration of two different anesthesia injections in 60 patients requiring two-step endodontic treatment to determine if it was effective at reducing pain.34 Half of the patients received labial infiltration (LI) anesthesia in the anterior maxilla while the rest received inferior alveolar nerve block (IANB). Vibration anesthesia consisted of the DentalVibe® device being placed intraorally, and whether patients received vibration during the first or second injection was determined randomly. The VAS was used to evaluate pain perception in participants during needle insertion and the anesthetic injection. Mean VAS scores were significantly (p<0.0001) lower with the use of vibration during needle insertion and anesthetic injection than those treated conventionally, for both LI and IANB sites. The results indicated that the use of DentalVibe® during the injection of local anesthesia was effective at pain reduction during intraoral procedures.34
There is variable literature in regards to the success of the DentalVibe® device in its ability to reduce pain during the administration of local anesthetic injections for intraoral procedures. For this particular study, thirty-one patients requiring two sessions of maxillary anterior infiltration local anesthetic administration were selected.35 During one session, patients received local anesthetic injections in a conventional manner, and received the same injection with vibration via DentalVibe® for the other session. Both sessions were randomized in order for each patient and separated from one another between two weeks. During conventional treatment, the patient’s lip would be retracted using the DentalVibe® while the device itself was turned off. After each session, patients were presented with a VAS to self assess their pain in addition to the WBFPRS. It was found that there was no statistically significant difference between the mean VAS scores in both the conventional and vibrational treatment groups (p=0.196); similarly, there was no statistically significant difference in the mean WBFPRS scores as well (p=0.192). When patients were asked about their preferred method of treatment, 15 patients showed preference towards the conventional method, while 15 others stated they preferred the vibrational method; the last patient showed no particular preference for either method. The use of DentalVibe was thus not justifiable in its ability to reduce pain during intraoral injections.35
The following study utilized different techniques during the administration of local dental anesthesia in 9 to 12 year old children to evaluate differences in pain, anxiety, and disruptive behavior.36 A total of 105 participants were separated into three groups that received infiltrative anesthesia using three techniques: conventional, vibrational, and computer-controlled. Vibration anesthesia was performed using the DentalVibe® device, which was applied on the mucosa at the puncture site after topical anesthesia and turned on 10 seconds before the anesthetic injection. Both the WBFPRS and NRS were used to evaluate self pain perception. Additionally, physiological parameters such as respiration rate and heart rate were measured, and disruptive behavior during the procedure was scored using the FLACC scale. While physiological parameters remained consistent among all patients, conventional anesthesia provided the lowest pain reports compared to VBA in both the WPS (p=0.018) and NRS (p=0.006) scales. It was concluded that the DentalVibe® was ineffective at reducing pain during intraoral procedures.36
In a similar study, the efficacy of DentalVibe® was investigated in pediatric patients requiring buccal infiltration anesthesia (BIA). Fully 60 patients between the ages of 6 to 12 years in need of BIA were split into two groups, with one group receiving traditional BIA and the other group receiving BIA with vibration via DentalVibe®. Subjective pain was measured immediately after the procedure using the WBFPRS, and pain was also objectively assessed by two trained observers using the FLACC sale. It was found that the DentalVibe® did not significantly decrease pain in patients compared to the traditional method.37
To determine whether vibration can assist in the minimization of injection pain during dental procedures, 40 children aged 4 to 8 years were recruited. The experimental group was determined randomly and consisted of 20 children that received vibrations of 50 Hz from a self-produced device developed with a computer mouse above the cheek. The Frankl Behavior Rating Scale, which consists of four categories ranging from complete refusal of treatment to complete acceptance of treatment, was utilized to assess behavior preoperatively, and did not show a significant difference among both groups. The Sound, Eye, and Motor (SEM) scale consisted of observations of sounds, eyes and motor to assess discomfort and pain. The level of response for each observation was given a value ranging from 1 to 4, with 1 being comfort and a rating of 4 being painful. The mean SEM score was significantly higher in the control group (6.65±1.95) than in the experimental group (3.80±1.15). The usage of vibration was described as being effective in reducing the discomfort of local anesthetic.38
The VibraJect® is a vibration device that can be attached to standard dental syringes and serves as another alternative method of vibration for patients during intraoral procedures. In a study determining the efficacy of the VibraJect® device during injection of local anesthetic, 75 children between the ages of 6-9 years in need of intraoral treatment were recruited. The participants were categorized into 3 groups of 25 patients each, depending on the area of treatment: upper buccal infiltrations, posterior palatal infiltrations, or inferior alveolar nerve block. The study utilized a split-mouth design, where each patient received treatment with the VibraJect® on one half, and the conventional treatment on the other. The order of treatment was randomized, and treatment of each side was separated between 2 visits. Assessment of pain was measured using both the VAS and FLACC scales. Patients reported lower VAS and FLACC scores for the side treated with vibration compared to the side treated conventionally for all three groups, indicating that the use of Vibraject to produce vibration was effective at reducing pain during injection of local anesthetic in intraoral procedures.39
Although topical anesthetic presents itself as a suitable alternative, the time used to apply the anesthetic can elongate the duration of anticipated pain and fear in children. This study recruited 48 children ranging from 4-10 years to determine difference in pain behavior when administered with anesthesia injections intraorally with vibration in comparison to standard topical anesthesia. In the experimental group of 25 patients, anesthesia was delivered by first drying the needle insertion area before applying a cotton ball containing topical anesthesia gel to the site. With the cotton ball still in place, the syringe was brought to the area for injection with the addition of a mild, manual vibratory stimulus provided by hand. After the injection, the cotton ball and vibration was continually applied for a few seconds afterwards while the physician provided a verbal distraction to the patient. In contrast, the other 23 patients in the control group did not receive the vibration stimulus while all other components remained identical. The author used a self-produced scale to assess pain after the procedure, in which each category has a range from 0-3 for a total range of 0-18. Scores were administered by 2 nurses present after the procedure. There was a statistically lower mean score in the experimental group (1.21 ± 1.38) compared with the control (2.44 ± 2.18), indicating that the use of the cotton-roll vibration method was effective at minimizing behavioral pain symptoms in children.40
Vibration anesthesia was compared with topical anesthesia in the ability to reduce pain during the administration of local dental anesthesia. A total of 61 patients were put into groups that received topical anesthetic with or without vibration. The topical anesthetic was applied on the buccal or palatal mucosa adjacent to the maxillary first premolar which is also where vibration anesthesia was placed using a modified shaving device. Injection pain was recorded through the use of a five-point visual analog scale where four pain ratings were obtained from each patient.41 There were some differences observed between the placebo and topical anesthetic with vibration, where the VAS scores were lower with topical anesthetic than with the placebo. However, there were no statistically significant differences between the effectiveness of either vibration anesthesia or topical anesthesia.
Placement of an intravenous (IV) catheter. A total of 100 participants undergoing intravenous propofol infusions were randomized into two groups; vibration anesthesia was used on only one of the groups. The vibration tool used on the experimental group was the Buzzy device, which was placed in a suspended position proximal to the intravenous catheter site without making contact with the patient’s skin. Vibration was received both before and during the propofol infusions. The control group received the Buzzy device while switched off to “blind” the participants. Pain was rated on a four-point scale, where 0 represented no pain at all while 3 represented severe pain which was manifested by grimacing facial gestures or a strong vocal response.42 Pain was reported by two independent-blinded observers to be lower in the treatment group compared to the group that received no intervention. From the 50 patients that were treated with vibration, 41 reported no pain felt, with the remaining 9 reporting the severity of pain as 1, equivalent to minimal pain felt. Within the control group, 31 of 50 patients felt no pain, and the median value of pain severity in the remaining 11 patients was 2. There was a significant difference in pain severity among the two groups (p<0.01), indicating the effectiveness of vibration anesthesia during propofol injections.
To compare the effects of vibration anesthesia with a lidocaine anesthetic patch on reducing pain during peripheral venous cannulation, 607 pediatric subjects participated in this study. Three hundred and two participants were placed in the group that received the Buzzy device while the rest were put in the group that had the EMLA patch. Pain scores were evaluated by the parents of the participants using the Children’s Hospital of Ontario Pain Scale (CHEOPS). This scale consists of ranking the severity of 6 different behaviors in children during treatment, with each behavior ranging from 1 to 3 points depending on the particular action. A minimum score of 4 indicates little to no pain expressed, while a 13 is the maximum score possible and indicates extreme pain felt. The behaviors scored consist of crying, verbal cues, facial cues, torso movement, touch, and legs movement.43 Participants that were treated with the EMLA patch had a mean CHEOPS score of 7.2±2.4 while the mean score with the Buzzy was 8.5±2.6, with the difference being statistically significant (p<0.01). These results indicate that the EMLA patch is a more effective method of reducing pain during cannulation than the Buzzy.
Miscellaneous. In an study of healthy volunteers, vibration anesthesia was one of the methods used for reducing pain in subcutaneous forehead injections of physiological saline; the other methods were cryoanalgesia and EMLA topical anesthetic cream. Using a design that split the forehead into four sections, 100 participants underwent vibration, cryoanalgesia via a frozen block of saline, topical anesthetic, or no anesthetic in a random order. The vibration instrument utilized was a T-shaped facial vibration device (Beauty bar, Careshow Ltd., Guangzhou, China), and pain levels were measured using a VAS. All analgesic techniques showed significantly better (p<0.001) pain control than no treatment, which had a mean score of 4.07±1.5 . When cryoanalgesia (2.16±1.19) was compared against the EMLA cream (2.14±1.33), the results were not statistically significant. Vibration anesthesia (1.78±1.34) performed significantly better than the other analgesic methods (p<0.015) against both external cold and anesthetic cream, so there was a significant difference in the effectiveness of vibration anesthesia in comparison to other methods.44
The use of vibration has been reviewed in a plastic surgery practice where 28 patients were enrolled in this study that required two consecutive visits and included procedures that are described as painful such as injections, staple removal, or suture removal. For each patient, one half of the procedures were performed using vibration, and the other half did not use vibration. The tool used was a Dentalvibe device. The NRS was utilized, where without vibration the average pain score was 3.46 and with vibration the rating was 1.93, indicating a statistically significant difference when using vibration. About 86 percent of participants claimed that vibration helped to decrease their symptoms of pain.45
A current study has been utilizing vibration during carboxytherapy in women with cellulite in the gluteal region. A total of 78 participants were placed into three groups, where 26 participants received vibratory anesthesia with the Vibrata during carboxytherapy. Another 26 received treatment with the Blaine Labs® Inc., while the remaining third were treated with carboxytherapy alone.46 The NRS was used which scaled from 0 to 10, 0 representing no pain and 10 representing the worst pain experienced. Although this is an ongoing trial, it is expected that vibration anesthesia will be effective.
Vibration for hyperhidrosis, axillae, hands and feet. The treatment of hyperhidrosis with botulinum toxin into the axillae, hands and feet significantly increases the quality of life (QOL) in patients both in the short term and long term.47,48 Although this procedure has been performed for over two decades, it can be especially painful as it involves dozens of injections. When performed upon the hands, it is uncomfortable and most patients cannot tolerate the injections without some type of anesthetic. This discomfort is magnified when botulinum toxin is injected into the feet for hyperhidrosis.
We have used vibration anesthesia while injecting botulinum toxin in countless patients suffering from hyperhidrosis who can now tolerate the procedure but could not tolerate it previously. Many practitioners are not aware of this effective use of vibration ameliorating the discomfort of injections.49 Many other techniques continue to be proposed including regional nerve blocks, topical anesthetic, and DermaJet. We have found ice to be helpful along with vibration anesthesia; it is more convenient and simpler than other pain-reducing techniques although it does require trained assistants. Most patients who desire treatment for the hyperhidrosis are very motivated and can tolerate multiple injections. They generally describe the discomfort as somewhere between a 2 to 4 on a scale of 10, but generally give an average rating of about 3. After the procedure is performed, unlike with regional blocks, patients do not have long-lasting anesthesia. They can leave on their own and drive home.
There are no controlled studies concerning the use of vibration anesthesia in hyperhidrosis. A paper by Nasser et al50 provides a meta-analysis of methods such as the usage of nerve or Bier blocks, cryoanalgesia, and topical anesthetics that could be used for reducing pain associated with injections but does not extensively discuss vibration anesthesia. It mentioned the use of an AcuVibe massager and the protocol behind it.
Vibration anesthesia use before injections in the hand or foot of corticosteroids or anesthetic. Injections of anesthesia or cortisone into the digits, palms, and dorsal feet can be very painful although often necessary in preparation for distal extremity procedures. Some of these techniques require multiple injections. For many patients, it is nearly intolerable.
While there are no controlled studies on the use of vibration anesthesia in preparation for injecting anesthetic or corticosteroids, many dermatologists who specialize in treating nails utilize vibration anesthesia. The instrument for vibration can be placed by an assistant several centimeters proximal to where the injection is taking place. The vibration device serves both as a distraction as well as stimulating the nerve fibers so it should be initiated several seconds before the injection.
While vibration anesthesia does not totally eliminate the discomfort associated with injections into the digits, toes, hands, or feet, it can serve as a helpful adjunct and make the procedure much more tolerable.
A study focused on methods to reduce pain during injections of corticosteroids to the hands and upper extremities using vibration anesthesia. This randomized study included patients experiencing arthritis, tendinopathy, or compression neuropathy of the hand, wrist, or elbow. The participants were divided into three groups with sixty injections performed in each. One group received injections without anesthesia, and the second group received injections with vibration near the injection site for 12 to 15 seconds using either an Accupal device (no longer produced) or DigiVibe (Bing Innovations, Boca Raton, Florida). The third group consisted of patients receiving injections after the injection site was covered with vapocoolant (Gebauers’s Company, Cleveland, Ohio) spray as an anesthetic. Measurements of expected pain were recorded prior to the procedure using a 10-point Likert-type scale, and the same scale was used immediately after to measure perceived pain as well. The results indicated that the group treated with vibration recorded the highest expected pain (5.73), and was the only group to have a statistically significant difference between their expected pain and perceived pain (4.18) scores. The group treated with vapocoolant spray also experienced a difference in expected pain (5.32) versus perceived pain (4.12), but the difference was not considered statistically significant. The control group recorded similar expected (5.57) and perceived pain scores (5.18). The study concluded that both vibration anesthesia and vapocoolant spray are two effective methods to reduce pain during corticosteroid injections to the hands and upper extremities.51
Injection of Kybella®. Kybella® is a common dermatologic procedure used to lessen submental lipid. This procedure can involve multiple needle injections and often significant discomfort. Although there are no controlled studies for use of vibration for Kybella, we have found it to be a very helpful adjunctive technique in minimizing discomfort for multiple patients.
Mesotherapy injections for scalp alopecia areata. Vibration was utilized to assist with the reduction of pain during mesotherapy injections on the scalp. A total of 30 patients participated in the study; 43 percent had androgenetic alopecia and 56 percent had alopecia areata. Every patient received mesotherapy with vibration via the Blaine Labs device on one randomly selected side, while the other side received treatment without vibration. To assess the perception of pain, an NRS, numerical rating scale, was used.52 In this study, the reported pain levels for the area on the scalp that received simultaneous vibration was significantly lower than the contralateral side (p<0.001). It was concluded that vibration anesthesia is an effective method for reducing pain during mesotherapy injections.
In situations where lidocaine may become a risk for interference with the procedure in question, vibration anesthesia presents itself as a safe alternative; one such procedure is the injection of platelet-rich plasma (PRP), which has become a common treatment method for those experiencing hair loss. As the procedure requires intradermal scalp injections, lidocaine is considered a risk for affecting platelet functionality, thus minimizing the benefits of the treatment. This study recruited 31 patients with alopecia to determine the most effective method of minimizing pain during inactivated PRP injections. Using a randomized split-scalp design, 10 of the patients were treated with an ice compress a few seconds prior to the injection on one half, and without ice on the other. A second group of 10 patients received vibration during the injection with a T-shaped device (Beauty bar, Careshow Ltd., Guangzhou, China) on one half, and no vibration on the other half. The last 11 patients received an ice compress on one half, and vibration on the other half. Pain was self-reported by the patients using an NRS ranging from 1 to 10 immediately after treatment for each side. Within the first group of patients, there was a statistically significant (p=0.001) decrease in pain scores when treated with the ice compress compared to no ice. Although there was no significant decrease (p=0.270) in pain scores for the vibration group, 90 percent of the patients reported that vibration was more favorable than no vibration. In the group comparing ice compresses to vibration, both sides received similar pain scores (5.0±2.8 with ice; 5.2±3.1 with vibration), and 55 percent of patients favored vibration while 9 percent found both methods equally favorable. The study concluded that both vibration and ice are two methods to be considered in the future for pain reduction during inactivated PRP injections.53
Limitations. This review is limited in the small number of suitable papers that met the specific focus, inclusion, and exclusion criteria. The instrumentations used for vibration anesthesia are non-standardized. A plethora of instruments were used during these papers. It is also not standardized as to the placement of vibration devices in relation to the procedure being performed. Additionally, the timing of when to use vibration was often not detailed.
CONCLUSION
There are various methods used by physicians that can help with the discomfort caused by certain procedures; vibration anesthesia has become much more commonplace. The technique of using vibration has been included in many invasive procedures, which target different locations on the body. The effectiveness of vibration anesthesia can be better understood through Melzack and Wall’s gate-control theory; more specifically vibration anesthesia has an impact on the Meissner and Pacinian corpuscles.
In this paper, we selected 35 papers that discussed the ability of vibration to reduce either pain, or the perception of pain and the anxiety associated with invasive procedures, the most common being the administration of local anesthesia. Upon reviewing these papers, it is evident that vibration anesthesia can be used for a wide variety of procedures and areas ranging from facial cosmetic injections to venipuncture on the extremities. Despite the variation in technique and tools in these procedures, a majority of these papers concluded vibration anesthesia as an effective means of pain reduction. A bulk of the literature focused on the use of vibration for intraoral patients, particularly the use of DentalVibe® during local anesthesia injections; this particular area within the literature also contained the most heterogeneity in results, with some deeming the instrument to be useful, while others did not. However, given the success of other instruments utilized during invasive intraoral procedures, the reliability of vibration anesthesia cannot be diminished simply due to possible lower efficaciousness from one device.
In most instances, the use of vibration lessened the pain associated with use of needles. Vibration anesthesia, however, did not reduce all of the pain but made it more palatable.
There were no long term side effects in any of the papers we reviewed; there were virtually no transitory side effects either. In one of the studies, two patients reported transitory tingling of teeth.16 In our experience a rare patient has transitory urticaria where the vibration was placed, which resolved within 30 to 60 minutes with no sequelae.
Further studies should be done in the future that involve using vibration on patients and should be performed with more standardized instruments. Moreover the placement of where the instrument should be in relation to the procedure should be better examined. In addition, further research should be done on the utilization of vibration on patients that undergo cosmetic procedures such as botulinum injections or fillers.
TABLE 1.
Summary of clinical applications involving the use of vibration anesthesia
| AUTHORS | N | PROCEDURE | LOCATION(S) | VIBRATORY DEVICE VS. COMPARISON | PAIN MEASUREMENT | OUTCOME | VIBRATION CONCLUDED AS EFFECTIVE/PREFERRED? |
|---|---|---|---|---|---|---|---|
| Kuwahara & Ogawa13 | 32 | Filler injections | Face | Blaine Labs vs. placebo | NRS | Mean NRS score with vibration: 2.3 ± 0.9; Mean score without vibration: 4.5 ± 1.5 | Yes (p<0.05) |
| Mally et al14 | 41 | Filler injections | Nasolabial Folds, cheeks, or tear troughs | Pin Point Personal Massager vs. placebo | Likert-type scale | Mean score with vibration: 0.9 ± 0.6; Mean score without vibration: 2.7 ± 0.9 | Yes (p<0.05) |
| Guney et al15 | 25 | Filler injections | Lips | Vibrata vs. placebo | Likert-type scale | Mean score with vibration: 3.82 ± 1.73; Mean score without vibration: 5.6 ± 1.76 | Yes (p<0.05) |
| Sharma et al16 | 50 | BTX | Glabella | Pin Point Personal Massager vs. placebo | Likert-type scale | Mean score with vibration: 1.3 ± 0.6; Mean score without vibration: 2.4 ± 0.8 | Yes (p<0.05) |
| Chorney et al18 | 22 | BTX | Forehead | (Ice vs. placebo) vs. (Buzzy vs. placebo) vs. (Ice vs. Buzzy) | VAS | Mean VAS score with vibration: 26.5; Mean VAS score without intervention: 29.4; Mean VAS score with ice: 24.4 | No (p>0.05) |
| Park et al19 | 40 | Corticosteroid injections to keloids | Varied | Blaine Labs vs. placebo | VAS | Mean VAS score with vibration: 3.28 ± 1.85; Mean score without vibration: 5.88 ± 2.34 | Yes (p<0.05) |
| Antepli et al20 | 56 | Heel lance procedures | Heel | Gray mini vibrator vs. placebo | NIPS | Patients treated with vibration scored significantly lower than those treated without vibration after the procedure | Yes (p<0.05) |
| McGinnis et al21 | 56 | Heel lance procedures | Heel | Norco MiniVibrator vs. placebo | N-PASS | Patients that received vibration had lower N-PASS scores 2 minutes after heel lance compared to those that did not receive vibration | Yes (p<0.05) |
| Schreiber et al22 | 70 | Venipuncture | Arms | Buzzy vs. placebo | NCCPC-PV | Mean score with vibration: 8.0; Mean score without vibration: 3.0 | Yes (p<0.05) |
| Binay et al23 | 96 | Venipuncture | Arms | Buzzy vs. distraction vs. placebo | WBFPRS | Patients experienced less pain when provided with distraction compared to no intervention. | Yes (p<0.05) |
| Inal & Kelleci24 | 120 | Venipuncture | Arms | Buzzy vs. placebo | CAPS, FPS-R | Mean CAPS score with vibration: 1.61 ± 0.99; Mean FPS-RS score with vibration: 2.78 ± 1.94; Mean CAPS score without vibration: 3.36 ± 0.99; Mean FPS-RS score without vibration 2.78 ± 1.94 | Yes (p<0.05) |
| Whelan et al25 | 64 | Venipuncture | Arms | Buzzy vs. placebo | WBFPRS | 71.4% of patients who received vibration (n = 35) stated it helped reduce pain and 80% would prefer having it again for their next visit. | Yes but (p>0.05) |
| Savcı et al26 | 100 | IM antibiotic injections | Intramuscular, ventrogluteal region | Dolphin massager device vs. ShotBlocker vs. placebo | VAS | Patients receiving vibration displayed the lowest mean pain score (3.02 ± 1.07) and highest mean satisfaction score (7.80 ± 0.90) compared to the other two groups. | Yes (p<0.001) |
| Fayers et al27 | 80 | LAI | Upper eyelids | Waterproof Mini-G vs. placebo | NRS | Mean score with vibration = 3.3; mean score without vibration = 4.5. | Yes (p<0.05) |
| Alshahwan28 | 80 | LAI | Arms | Buzzy vs. cooling | VAS | Mean score after vibration = 25.5 ± 24.1; mean score after cooling = 30 ± 23.14. | No (p>0.05) |
| Govas et al29 | 87 | LAI | Treatment site varied | VAD vs. placebo | NRS | Mean score with vibration = 1.24; mean score without vibration = 2.04. | Yes (p<0.05) |
| Tirupathi et al30 | 376 (across 7 studies) | ILAI | Intraoral | 6/7 studies used Dentalvibe; 1 study used a modified electric toothbrush | Varied among FLACC, VAS, or WBFPRS | 5/7 studies showed statistically significant results in vibration minimizing pain. 2 studies did not have significant differences | Yes in 5 studies, No in 2 studies |
| Faghihian et al31 | 373 (across 6 studies) | ILAI | Intraoral | 4/7 studies used Dentalvibe; 2 studies used Buzzy vs. placebo | FLACC or WBFPRS | The Buzzy effectively minimized pain during procedures; the DentalVibe produced inconsistent results across all 4 studies | Yes in 3 studies, No in 3 DentalVibe studies |
| Nasehi et al32 | 99 | ILAI | Intraoral | Dentalvibe vs. placebo | VAS | Mean anticipated pain scores with vibration were significantly lower compared to anticipated pain scores without vibration. Mean score for actual pain experienced with vibration was significantly lower. | Yes (p<0.001) |
| Joshi et al33 | 50 | ILAI | Intraoral | Dentalvibe vs. Lidocaine 2% gel | VAS | Median score with vibration = 3; median score without vibration = 7. | Yes (p< 0.05) |
| Ghorbanzadeh et al34 | 60 | ILAI | Intraoral | Dentalvibe vs. placebo | VAS | Mean score with vibration < 20; mean score without vibration > 35. | Yes (p< 0.05) |
| Erdogan et al35 | 31 | ILAI | Intraoral | Dentalvibe vs. placebo | VAS; WBFPRS | There were no statistically significant differences in mean VAS and WBFPRS scores between both groups | No (p>0.05) |
| de Camargo Smolarek et al36 | 105 | ILAI | Intraoral | Dentalvibe vs. Computer controlled techniques vs. placebo | FLACC; NRS; WBFPRS | The conventional method promoted significantly less self-reported pain than vibrational and computer-controlled techniques | No (p<0.05) |
| Felemban et al37 | 60 | ILAI | Intraoral | Dentalvibe vs. placebo | FLACC; WBFPRS | There were no statistically significant differences in mean FLACC and WBFPRS scores between both groups | No (p>0.05) |
| Subramaniam & Ghai38 | 40 | ILAI | Intraoral | Buzzy vs. placebo | SEM scale | Mean sore with vibration = 3.80 ± 1.15; mean score without vibration = 6.65 ± 21.95 | Yes (p<0.05) |
| Albouni et al39 | 75 | ILAI | Intraoral | VibraJect vs. placebo | FLACC; VAS | Patients that received vibration reported lower mean VAS and FLACC scores | Yes (p<0.001) |
| Bagherian et al40 | 48 | ILAI | Intraoral | Cotton-roll vibration vs. placebo (no vibration) | Self-produced scale | Mean score with vibration = 1.21 ± 1.38, mean score without vibration 2.44 ± 2.18 | Yes (p<0.05) |
| Hutchins et al41 | 61 | ILAI | Intraoral | Topical Anesthetic vs. Dentalvibe vs. placebo | VAS | Mean score with vibration = 1.21 ± 1.38, mean score without vibration 2.44 ± 2.18 | Yes (p< 0.05) |
| Hwang et al42 | 100 | IV cannulation | Cannulation area varied | Buzzy vs. placebo | 4-point scale | Patients that received vibration scored lower on the pain scale | Yes (p<0.05) |
| Bourdier et al43 | 607 | IV cannulation | Cannulation area varied | Buzzy vs. EMLA patch | CHEOPS | Mean CHEOPS score with EMLA = 7.2 ± 2.4, Mean CHEOPS score with Buzzy = 8.5 ± 2.6 | No (p<0.05) |
| Salmerón-González et al44 | 100 | Saline injections | Forehead | Beauty bar vs. cryoanalgesia vs. EMLA vs. placebo | VAS | Mean VAS score with vibration = 1.78 ± 1.34, Mean VAS score with EMLA = 2.14 ± 1.33, Mean VAS with external cold = 2.16 ± 1.19, Mean VAS without treatment = 4.07 ± 1.5. | Yes (p<0.05) |
| Eichhorn et al45 | 28 | Local dental anesthetic injection | Intraoral | Dentalvibe vs. placebo | NRS | Mean NRS score with vibration: 1.93, Mean score wthout vibration: 3.52. | Yes (p<0.05) |
| Weeks and Falliace51 | 180 | Corticosteroid injections | Hand, wrist, or elbow | DigiVibe vs. vapocoolant vs. placebo | Likert-type scale | Perceived pain with vibration = 4.18, Perceived pain with cooling 4.12, Perceived pain with no treatment = 5.18 | Yes but (p>0.05) |
| Carvalho et al52 | 30 | Mesotherapy injections | Scalp | VAD vs. placebo | NRS | Range of scores with vibration: 5-9, range of scores without vibration: 0.5-6 | Yes (p<0.05) |
| Suh et al53 | 31 | Platelet rich plasma injections | Scalp | Split scalp design: ice compress vs. placebo; vibration vs. placebo; ice compress vs. vibration | NRS | Mean score with vibration = 1.93, Mean score without vibration = 3.46 | Yes but (p>0.05) |
BTX: Botulinum toxin injections; ILAI: Intraoral local anesthetic injection; LAI: Local anesthetic injection; IM: Intramuscular; IV: Intravenous; NRS: Numeric Rating Scale; FLACC: Face, Legs, Activity, Cry, Consolability; WBFPRS: Wong-Baker Faces Pain Rating Scale; VAS: Visual Analog Scale; SEM: Sound, Eye, and Motor; CHEOPS: Children’s Hospital of Ontario Pain Scale; CAPS: Children’s Anxiety and Pain Scale; NIPS: Neonatal Infant Pain Scale; NCCPC-PV: Non Communicating Children’s Pain Checklist–postoperative version scale; FPS-R: Faces Pain Scale-Revised; N-PASS: Neonatal Pain, Agitation, and Sedation Scale
REFERENCES
- Garland EL. Pain processing in the human nervous system: a selective review of nociceptive and biobehavioral pathways. Prim Care. 2012;39:561–571. doi: 10.1016/j.pop.2012.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- https://newsroom.wakehealth.edu/news-releases/2003/06/brain-imaging-confirms-that-people-feel-pain-differently-report-researchers-at-wake Brain imaging confirms that people feel pain differently, report researchers at Wake Forest University Baptist Medical Center. News release. Atrium Health Wake Forest Baptist. June 23, 2003. Accessed July 17 2024.
- McLenon J, Rogers MAM. The fear of needles: a systematic review and meta-analysis. J Adv Nurs. 2019;75:30–42. doi: 10.1111/jan.13818. [DOI] [PubMed] [Google Scholar]
- Smith KC, Comite SL, Storwick GS. Ice minimizes discomfort associated with injection of botulinum toxin type A for the treatment of palmar and plantar hyperhidrosis. Dermatol Surg. 2007;33:S88–91. doi: 10.1111/j.1524-4725.2006.32337.x. [DOI] [PubMed] [Google Scholar]
- Comite S, Greene A, Cieszynski SA et al. Minimizing discomfort during the injection of radiesse with the use of either local anesthetic or ice. Dermatol Online J. 2007;13:5. [PubMed] [Google Scholar]
- Smith KC, Comite SL, Balasubramanian S et al. Vibration anesthesia: a noninvasive method of reducing discomfort prior to dermatologic procedures. Dermatol Online J. 2004;10:1. [PubMed] [Google Scholar]
- Kendroud S, Fitzgerald LA, Murray I . Treasure Island (FL): StatPearls Publishing; 2021. Physiology, nociceptive pathways. In: StatPearls. [PubMed] [Google Scholar]
- Garcia K, Wray JK, Kumar S. Treasure Island (FL): StatPearls Publishing; 2022. Spinal cord stimulation. In: StatPearls. [PubMed] [Google Scholar]
- Bajwa H, Al Khalili Y. Treasure Island (FL): StatPearls Publishing; 2023. Physiology, vibratory sense. In: StatPearls. [PubMed] [Google Scholar]
- Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;150(3699):971–979. doi: 10.1126/science.150.3699.971. [DOI] [PubMed] [Google Scholar]
- Caterina MJ, Schumacher MA, Tominaga M et al. The capsaicin receptor: a heat-activated ion channel in the pain pathway. Nature. 1997;389:816–824. doi: 10.1038/39807. [DOI] [PubMed] [Google Scholar]
- Coste B, Mathur J, Schmidt M et al. Piezo1 and Piezo2 are essential components of distinct mechanically activated cation channels. Science. 2010;330(6000):55–60. doi: 10.1126/science.1193270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuwahara H, Ogawa R. Using a vibration device to ease pain during facial needling and injection. Eplasty. 2016;16:e9. [PMC free article] [PubMed] [Google Scholar]
- Mally P, Czyz CN, Chan NJ et al. Vibration anesthesia for the reduction of pain with facial dermal filler injections. Aesthetic Plast Surg. 2014;38:413–418. doi: 10.1007/s00266-013-0264-4. [DOI] [PubMed] [Google Scholar]
- Guney K, Sezgin B, Yavuzer R. The efficacy of vibration anesthesia on reducing pain levels during lip augmentation: worth the buzz? Aesthet Surg J. 2017;37:1044–1048. doi: 10.1093/asj/sjx073. [DOI] [PubMed] [Google Scholar]
- Sharma P, Czyz CN, Wulc AE. Investigating the efficacy of vibration anesthesia to reduce pain from cosmetic botulinum toxin injections. Aesthet Surg J. 2011;31:966–971. doi: 10.1177/1090820X11422809. [DOI] [PubMed] [Google Scholar]
- Ballard A, Khadra C, Adler S et al. Efficacy of the buzzy device for pain management during needle-related procedures: a systematic review and meta-analysis. Clin J Pain. 2019;35:532–543. doi: 10.1097/AJP.0000000000000690. [DOI] [PubMed] [Google Scholar]
- Chorney SR, Villwock JA, Suryadevara AC. Vibration versus ice to reduce cosmetic botulinum toxin injection pain-a randomized controlled trial. Ear Nose Throat J. 2019;98:351–355. doi: 10.1177/0145561319839839. [DOI] [PubMed] [Google Scholar]
- Park KY, Lee Y, Hong JY et al. Vibration anesthesia for pain reduction during intralesional steroid injection for keloid treatment. Dermatol Surg. 2017;43:724–727. doi: 10.1097/DSS.0000000000001040. [DOI] [PubMed] [Google Scholar]
- Avan Antepli N, Bilsin Kocamaz E, Güngörmüş Z. The effect of vibration on pain during heel lance procedures in newborns: a randomized controlled trial. Adv Neonatal Care. 2022;22:E43–47. doi: 10.1097/ANC.0000000000000918. [DOI] [PubMed] [Google Scholar]
- McGinnis K, Murray E, Cherven B et al. Effect of vibration on pain response to heel lance: a pilot randomized control trial. Adv Neonatal Care. 2016;16:439–448. doi: 10.1097/ANC.0000000000000315. [DOI] [PubMed] [Google Scholar]
- Schreiber S, Cozzi G, Rutigliano R et al. Analgesia by cooling vibration during venipuncture in children with cognitive impairment. Acta Paediatr. 2016;105:e12–6. doi: 10.1111/apa.13224. [DOI] [PubMed] [Google Scholar]
- Binay Ş, Bilsin E, Gerçeker GÖ et al. Comparison of the effectiveness of two different methods of decreasing pain during phlebotomy in children: a randomized controlled trial. J Perianesth Nurs. 2019;34:749–756. doi: 10.1016/j.jopan.2018.11.010. [DOI] [PubMed] [Google Scholar]
- Inal S, Kelleci M. Relief of pain during blood specimen collection in pediatric patients. MCN Am J Matern Child Nurs. 2012;37:339–345. doi: 10.1097/NMC.0b013e31825a8aa5. [DOI] [PubMed] [Google Scholar]
- Whelan HM, Kunselman AR, Thomas NJ et al. The impact of a locally applied vibrating device on outpatient venipuncture in children. Clin Pediatr. 2014;53:1189–1195. doi: 10.1177/0009922814538494. [DOI] [PubMed] [Google Scholar]
- Savcı C, Özkan B, Açıksarı K et al. Effectiveness of two different methods on the perceived pain and satisfaction during intramuscular antibiotic injection: shotblocker and local vibration. Clin Nurs Res. 2022;31:812–819. doi: 10.1177/10547738211051877. [DOI] [PubMed] [Google Scholar]
- Fayers T, Morris DS, Dolman PJ. Vibration-assisted anesthesia in eyelid surgery. Ophthalmology. 2010;117:1453–1457. doi: 10.1016/j.ophtha.2009.11.025. [DOI] [PubMed] [Google Scholar]
- Alshahwan M. A prospective comparison between skin cooling and skin vibration in reducing the pain of local anesthetic infiltration. J Cosmet Dermatol. 2020;19:1490–1493. doi: 10.1111/jocd.13160. [DOI] [PubMed] [Google Scholar]
- Govas P, Kazi R, Slaugenhaupt RM et al. Effect of a vibratory anesthetic device on pain anticipation and subsequent pain perception among patients undergoing cutaneous cancer removal surgery: a randomized clinical trial. JAMA Facial Plast Surg. 2019;21:480–486. doi: 10.1001/jamafacial.2019.0733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tirupathi SP, Nanda N, Pallepagu S et al. The combined effect of extraoral vibratory stimulus and external cooling on pain perception during intra-oral local anesthesia administration in children: a systematic review and meta-analysis. J Dent Anesth Pain Med. 2022;22:87–96. doi: 10.17245/jdapm.2022.22.2.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faghihian R, Rastghalam N, Amrollahi N et al. Effect of vibration devices on pain associated with dental injections in children: a systematic review and meta-analysis. Australian Dental Journal. 2021;66:4–12. doi: 10.1111/adj.12811. [DOI] [PubMed] [Google Scholar]
- Nasehi A, Bhardwaj S, Kamath A-T et al. Clinical pain evaluation with intraoral vibration device during local anesthetic injections. J Clin Exp Dent. 2015;7:e23–27. doi: 10.4317/jced.51643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joshi S, Bhate K, Kshirsagar K et al. DentalVibe reduces pain during the administration of local anesthetic injection in comparison to 2% lignocaine gel: results from a clinical study. J Dent Anesth Pain Med. 2021;21:41–47. doi: 10.17245/jdapm.2021.21.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghorbanzadeh S, Alimadadi H, Zargar N et al. Effect of vibratory stimulation on pain during local anesthesia injections: a clinical trial. Restor Dent Endod. 2019;44:e40. doi: 10.5395/rde.2019.44.e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erdogan O, Sinsawat A, Pawa S et al. Utility of vibratory stimulation for reducing intraoral injection pain. Anesth Prog. 2018;65:95–99. doi: 10.2344/anpr-65-02-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Camargo Smolarek P, da Silva LS, Martins PRD et al. The influence of distinct techniques of local dental anesthesia in 9- to 12-year-old children: randomized clinical trial on pain and anxiety. Clin Oral Investig. 2021;25:3831–843. doi: 10.1007/s00784-020-03713-7. [DOI] [PubMed] [Google Scholar]
- Felemban O, Oghli AR, Alsaati I et al. The effect of DentalVibe on pain and discomfort during local anesthesia in children: a randomized clinical trial. Quintessence Int. 2021;0:434–443. doi: 10.3290/j.qi.b912695. [DOI] [PubMed] [Google Scholar]
- Subramaniam P, Ghai SK. Efficacy of an innovative device in reducing discomfort during local anesthesia administration in children: a clinical study. Int J Clin Pediatr Dent. 2021;14:353–356. doi: 10.5005/jp-journals-10005-1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albouni MA, Kouchaji C, Al-Akkad M et al. Evaluation of the injection pain with the use of vibraject during local anesthesia injection for children: a randomized clinical trial. J Contemp Dent Pract. 2022;23:749–754. [PubMed] [Google Scholar]
- Bagherian A, Sheikhfathollahi M. Children’s behavioral pain reactions during local anesthetic injection using cotton-roll vibration method compared with routine topical anesthesia: a randomized controlled trial. Dent Res J. 2016;13:272–277. doi: 10.4103/1735-3327.182189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchins HS, Jr, Young FA, Lackland DT et al. The effectiveness of topical anesthesia and vibration in alleviating the pain of oral injections. Anesth Prog. 1997;44:87–89. [PMC free article] [PubMed] [Google Scholar]
- Hwang LK, Nash DW, Yedlin A et al. The effect of vibration on pain during intravenous injection of propofol: a randomized controlled trial. Ann Plast Surg. 2021;87:S36–39. doi: 10.1097/SAP.0000000000002827. [DOI] [PubMed] [Google Scholar]
- Bourdier S, Khelif N, Velasquez M et al. Cold vibration (buzzy) versus anesthetic patch (emla) for pain prevention during cannulation in children: a randomized trial. Pediatr Emerg Care. 2021;37:86–91. doi: 10.1097/PEC.0000000000001867. [DOI] [PubMed] [Google Scholar]
- Salmerón-González E, García-Vilariño E, Sánchez-García A et al. A randomized controlled trial of three noninvasive analgesic techniques for the prevention of pain during facial injections. Aesthet Surg J. 2021;41:74–79. doi: 10.1093/asj/sjz380. [DOI] [PubMed] [Google Scholar]
- Eichhorn MG, Karadsheh MJ, Krebiehl JR et al. Vibration for pain reduction in a plastic surgery clinic. Plast Surg Nurs. 2016;36:63–68. doi: 10.1097/PSN.0000000000000134. [DOI] [PubMed] [Google Scholar]
- Sadala AY, Rampazo ÉP, Liebano RE. Vibration anesthesia during carboxytherapy for cellulite: a study protocol. Pain Manag. 2022;12:401–408. doi: 10.2217/pmt-2021-0080. [DOI] [PubMed] [Google Scholar]
- Campanati A, Penna L, Guzzo T et al. Quality-of-life assessment in patients with hyperhidrosis before and after treatment with botulinum toxin: results of an open-label study. Clin Ther. 2003;25:298–308. doi: 10.1016/s0149-2918(03)90041-5. [DOI] [PubMed] [Google Scholar]
- Lynch OE, Aherne T, Gibbons J et al. Five-year follow-up of patients treated with intra-dermal botulinum toxin for axillary hyperhidrosis. Ir J Med Sci. 2020;189:1023–1026. doi: 10.1007/s11845-019-02131-3. [DOI] [PubMed] [Google Scholar]
- Comite SL, Smith K. Commenting on: “Duration of efficacy increases with the repetition of botulinum toxin A injections in primary palmar hyperhidrosis.”. J Am Acad Dermatol. 2015;72:201. doi: 10.1016/j.jaad.2014.08.053. [DOI] [PubMed] [Google Scholar]
- Nasser S, Farshchian M, Kimyai-Asadi A et al. Techniques to relieve pain associated with botulinum injections for palmar and plantar hyperhidrosis. Dermatol Surg. 2021;47:1566–1571. doi: 10.1097/DSS.0000000000003182. [DOI] [PubMed] [Google Scholar]
- Weeks DW, Faillace JJ. Vibratory anesthesia’s effect on pain perception in upper extremity corticosteroid injections. Hand (N Y). 2024;19(2):321–326. doi: 10.1177/15589447221109910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carvalho R, de M, Barreto T, de M, Weffort F et al. Use of vibrating anesthetic device reduces the pain of mesotherapy injections: a randomized split-scalp study. J Cosmet Dermatol. 2021;20:425–428. doi: 10.1111/jocd.13554. [DOI] [PubMed] [Google Scholar]
- Suh S, Casale FS, Atanaskova Mesinkovska N. Effective strategies to reduce pain during platelet-rich plasma scalp injections: a randomized split-scalp study. J Am Acad Dermatol. 2022;86:654–655. doi: 10.1016/j.jaad.2021.02.029. [DOI] [PubMed] [Google Scholar]